Abstract
Purpose
Numerous indices have been proposed to analyse wound healing in oral soft tissues, but each has specific shortcomings. A new method of analysis, the Early Wound Healing Score (EHS), was evaluated in the present study. The aim was to assess more accurately early healing by primary intention of surgical incisions in periodontal soft tissues.
Methods
Twenty-one patients were treated with different surgical procedures comprising 1 or 2 vertical releasing incisions as part of a surgical access flap. Twenty-four hours after surgery, early wound healing at the vertical releasing incisions was assessed using the EHS. This score assessed clinical signs of re-epithelialization (CSR), clinical signs of haemostasis (CSH), and clinical signs of inflammation (CSI). Since complete wound epithelialization was the main outcome, the CSR score was weighted to be 60% of the total final score. Accordingly, a score of 0, 3, or 6 points was possible for the assessment of CSR, whereas scores of 0, 1, or 2 points were possible for CSH and CSI. Higher values indicated better healing. Accordingly, the score for ideal early wound healing was 10.
Results
Thirty vertical releasing incisions were assessed in 21 patients. At 24 hours after incision, 16 vertical releasing incisions (53.33%) received the maximum score of CSR, while 6 cases (20%) received an EHS of 10. None of the cases received 0 points.
Conclusion
The EHS system may be a useful tool for assessing early wound healing in periodontal soft tissue by primary intention after surgery.
Keywords: Gingiva, Periodontal diseases, Soft tissue injuries, Symptom assessment, Wound healing
Graphical Abstract
INTRODUCTION
A wound is defined as an injury to living tissue and a forcible interruption of the continuity of any organic tissue [1]. Therefore, the involved tissues after periodontal surgery are considered to be wounded sites. Healing, in contrast, is the process of repair or regeneration of an injured, lost, or surgically treated tissue. In particular, healing by primary intention refers to primary wound closure, where the flap margins are placed and held in direct contact until merged by tissue healing [1]. Healing itself takes place following a well-organized chronology of biological events that are crucial for the quality of the final repair of wounded tissues, beginning with initial haemostasis, early clot formation, and inflammatory cell infiltration, which, in turn, is followed by the proliferation of epithelial cells and fibroblasts that migrate into the wound [2,3,4,5].
Wound closure has been universally recognized to be crucial for periodontal wound healing, especially following regenerative procedures [2,5]. In particular, the first postoperative week appears to be critical for the maintenance of wound stability [2,6,7].
Wound healing should be monitored to identify early signs that may be related to healing complications. Such findings might be associated with problems in different surgical procedures, and surgeons should be aware of these problems to consider prompt interventions [8].
Numerous methods have been described for the assessment of wound healing in oral soft tissues. The first published index, the Healing Index (HI), was introduced by Landry et al. [9] in 1988 and evaluated the parameters of tissue colour, bleeding response to palpation, presence of granulation tissue, characteristics of the incision margins, and the presence of suppuration. This index assesses wound healing using scores from 1 to 5: a wound with very poor healing receives a score of 1, whereas excellent healing receives a score of 5.
A further index, the Early Healing Index (EHI), was developed by Wachtel et al. [10], classifying healing in 5 degrees. It rates flap closure not only as complete or incomplete, but also registers both the amount of fibrin and necrosis.
In 2004, Hagenaars et al. [11] published a 3-point score (both from 0 to 2) assessing swelling and colour of the gingival tissues. In the same year, Tonetti and colleagues [12] described a dichotomous score for evaluating healing using the following parameters: oedema, haematoma, suppuration, flap dehiscence, and patient complaints.
Then, in 2005, Huang et al. [13] introduced the Wound Healing Index (WHI), which evaluates periodontal soft tissue wound healing with scores from 1 to 3. On this scale, wounds are scored 1 in the absence of gingival oedema, erythema, suppuration, patient discomfort, and flap dehiscence; a score of 2 refers to uneventful healing with slight gingival oedema, erythema, patient discomfort, and flap dehiscence, but no suppuration; and a score of 3 corresponds to poor wound healing with significant gingival oedema, erythema, suppuration, patient discomfort, and flap dehiscence, or any suppuration.
Even though these methods have been proposed, a ready-to-use assessment system for early wound healing after surgical and intended healing by primary wound closure seems to be still missing. This fact might be explained by the complexity of biological and clinical healing procedures. Accordingly there are several specific limitations of the previously described methods: 1) not all relevant parameters are considered; 2) most indices are designed to follow wound healing no earlier than 1 or 2 weeks after surgery (i.e., not since the very beginning of the healing process, such as 24 hours after surgery); 3) some of them are excessively comprehensive, thus including many parameters assembled in an inflexible arrangement, rendering the index too complicated for clinical use; 4) some methods evaluate healing features dichotomously, thus becoming very simple without considering the effect of each single parameter of which they are composed; 5) some parameters might be difficult to assess objectively since an adequate definition of the different clinical manifestations is lacking; 6) and some are not applicable for the evaluation of different kinds of surgical incisions.
Considering these limitations, in this pilot study we developed and used a new score called the Early Wound Healing Score (EHS), in order to assess more accurately the early stage of periodontal soft tissue wound healing. The EHS aimed to: 1) adequately define and comprehensively include the clinical aspects of primary healing at incisions, evaluable from postoperative day 1 and onward; and 2) independently assess and subsequently integrate the different clinical aspects of primary healing at incisional wounds.
MATERIALS AND METHODS
Inclusion criteria
Patients requiring dental implants or periodontal surgery were selected according to the following inclusion criteria: 1) age ≥18 years; 2) no systemic disease; 3) no smoking; 4) no alcohol abuse; 5) no immunosuppressive therapy; 6) no pregnancy; 7) a full-mouth plaque score and a full-mouth bleeding score <25% as recorded at 6 sites per tooth; and 8) no history of previous periodontal surgery at the experimental sites.
The study was conducted at the Department of Dental and Maxillofacial Sciences, Section of Periodontology, “Sapienza” University of Rome, Rome, Italy. The study protocol was approved by the local ethical committee (2464/15). All patients were informed about the study and signed a consent form. Study participation was strictly voluntary. The study was performed in accordance to the Declaration of Helsinki of 1975, as revised in 2013 [14].
Surgical procedures
Patients were treated with different surgical procedures with at least 1 vertical releasing incision in the flap design. Each incision was extended from the attached gingiva at the line angles of the teeth, apically to the mucogingival line, including the alveolar mucosa for an equivalent length compared to the keratinized gingiva.
Upon completion of surgery, interrupted sutures were placed in order to obtain passive closure of the flap and healing by primary intention.
Postsurgical assessment (at 24 hours)
Patients were recalled 24 hours after surgery, and a trained examiner (LM) assessed early wound healing using the EHS. In order to standardize the assessment as much as possible for this study, only the vertical releasing incisions were assessed.
EHS
The EHS is composed of 3 parameters: clinical signs of re-epithelization (CSR), clinical signs of haemostasis (CSH), and clinical signs of inflammation (CSI).
Zero, 3, or 6 points were used to evaluate CSR, whereas 0, 1, or 2 points were used for both CSH and CSI (Table 1). The summation of the points of these 3 parameters generated the EHS. The EHS for ideal wound healing was 10 points, while the worst possible score was 0 points.
Table 1. EHS description.
| Parameter | Description | Points |
|---|---|---|
| CSR | Merged incision margins | 6 |
| Incision margins in contact | 3 | |
| Visible distance between incision margins | 0 | |
| CSH | Absence of fibrin on the incision margins | 2 |
| Presence of fibrin on the incision margins | 1 | |
| Bleeding at the incision margins | 0 | |
| CSI | Absence of redness along the incision length | 2 |
| Redness involving <50% of the incision length | 1 | |
| Redness involving >50% of the incision length and/or pronounced swelling | 0 | |
| Maximum total score: 10 | ||
EHS: Early Wound Healing Score, CSR: clinical signs of re-epithelialization, CSH: clinical signs of haemostasis, CSI: clinical signs of inflammation.
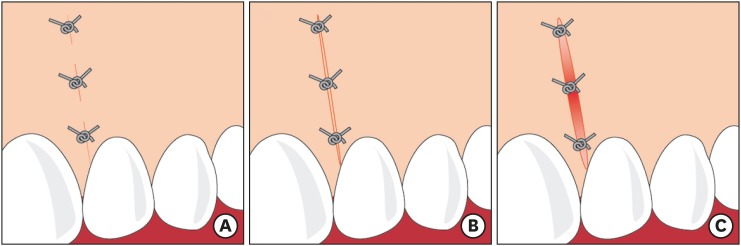
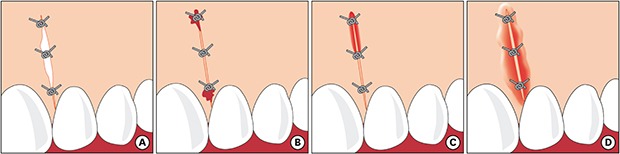
• CSR: 0 points, visible distance between incision margins; 3 points, incision margins in contact; 6 points, merged incision margins.
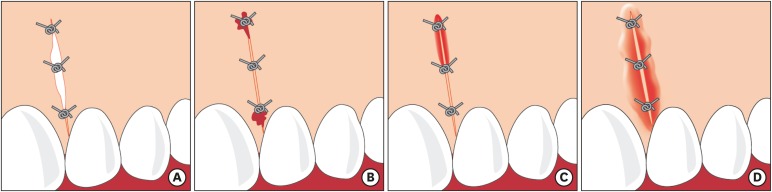
• CSH: 0 points, bleeding at the incision margins; 1 point, presence of fibrin at the incision margins; 2 points, absence of fibrin on the incision margins.
• CSI: 0 points, redness involving >50% of the incision length and/or pronounced swelling; 1 point, redness involving <50% of the incision length; 2 points, absence of redness along the incision length.
For each parameter, the worst score observable was registered.
An EHS of 0 points was assigned in the presence of suppuration, independently of the ratings for the 3 single parameters.
RESULTS
Thirty vertical releasing incisions were assessed in 21 patients (9 males and 12 females, aged from 32 to 60 years; mean age, 49.13±8.81 years). Fifteen patients received only 1 vertical releasing incision, whereas 4 patients received 2 incisions, 1 received 3 incisions, and 1 received 4 incisions. Patients who had at least 3 vertical releasing incisions underwent multiple surgical procedures. In each patient, all incisions were assessed, and the worst healing outcome was used for documentation.
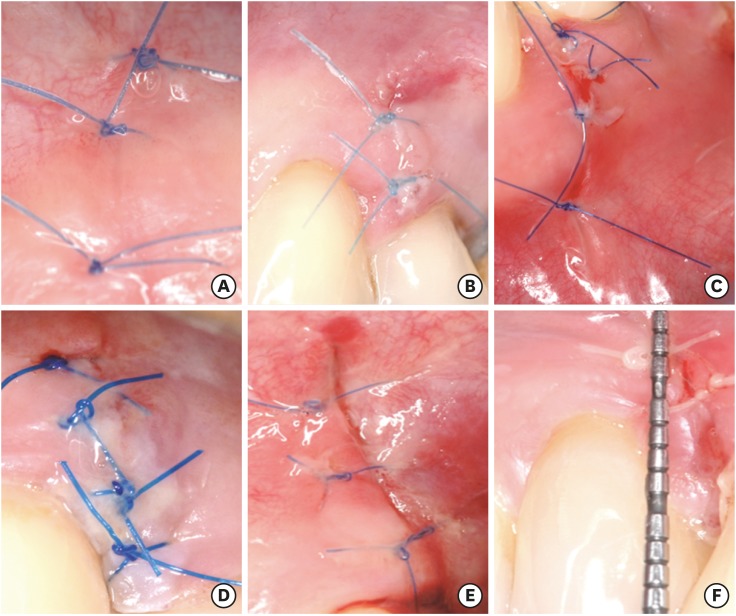
EHS was used to evaluate the wounds in the early stage of healing, at 24 hours after surgery. The mean EHS was 7.2±2.56 (range, 1–10). Six cases (20%) scored 10, whereas no case scored 0. Sixteen vertical releasing incisions (53.3%) exhibited a maximum CSR score (6). Thirteen vertical releasing incisions (43.3%) received 3 points for CSR, while only 1 (3.3%) received 0 points for CSR. Fifteen vertical releasing incisions (50%) exhibited a CSH score of 2, 7 (23.3%) had a CSH score of 1, and 8 (26.6%) had a CSH score of 0. Fifteen (50%) vertical releasing incisions exhibited a CSI score of 2, 14 (46.6%) a CSI score of 1, and 1 (3.3%) a CSI score of 0 (Table 2, Figures 1, 2, 3).
Table 2. Data on individual vertical releasing incisions with EHS parameters.
| VRIs | CSR (points) | CSH (points) | CSI (points) | EHS (points) |
|---|---|---|---|---|
| 1 | 6 | 2 | 2 | 10 |
| 2 | 6 | 2 | 1 | 9 |
| 3 | 6 | 1 | 2 | 9 |
| 4 | 3 | 1 | 1 | 5 |
| 5 | 3 | 0 | 2 | 5 |
| 6 | 3 | 2 | 1 | 6 |
| 7 | 6 | 2 | 1 | 9 |
| 8 | 6 | 2 | 1 | 9 |
| 9 | 0 | 0 | 1 | 1 |
| 10 | 6 | 2 | 2 | 10 |
| 11 | 3 | 1 | 1 | 5 |
| 12 | 3 | 0 | 1 | 4 |
| 13 | 6 | 1 | 2 | 9 |
| 14 | 3 | 2 | 1 | 6 |
| 15 | 6 | 2 | 2 | 10 |
| 16 | 6 | 2 | 2 | 10 |
| 17 | 6 | 2 | 2 | 10 |
| 18 | 6 | 2 | 2 | 10 |
| 19 | 6 | 2 | 1 | 9 |
| 20 | 3 | 0 | 2 | 5 |
| 21 | 6 | 1 | 2 | 9 |
| 22 | 3 | 0 | 1 | 4 |
| 23 | 3 | 0 | 1 | 4 |
| 24 | 3 | 2 | 2 | 7 |
| 25 | 6 | 2 | 1 | 9 |
| 26 | 6 | 1 | 1 | 8 |
| 27 | 6 | 1 | 2 | 9 |
| 28 | 3 | 2 | 2 | 7 |
| 29 | 3 | 0 | 2 | 5 |
| 30 | 3 | 0 | 0 | 3 |
EHS: Early Wound Healing Score, VRI: vertical releasing incision, CSR: clinical signs of re-epithelialization, CSH: clinical signs of haemostasis, CSI: clinical signs of inflammation.
Figure 1. Graphic representations of CSR. (A) Merged incision margins (6 points for CSR). (B) Incision margins in contact (3 points for CSR). (C) Visible distance between incision margins (0 points for CSR).
CSR: clinical signs of re-epithelialization.
Figure 2. Graphic representations of the CSH and CSI. (A) Presence of fibrin on the incision margins (1 point for CSH). (B) Bleeding at the incision margins (0 points for CSH). (C) Redness involving <50% of the incision length (1 point for CSI). (D) Redness involving >50% of the incision length and/or pronounced swelling (0 points for CSI).
CSH: clinical signs of haemostasis, CSI: clinical signs of inflammation.
Figure 3. Clinical photographs of vertical releasing incisions exhibiting decreasing values of the EHS. (A) The value of EHS is 10 (merged incision margins: 6; absence of fibrin on the incision margins: 2; absence of redness along the incision length: 2). (B) The value of EHS is 9 (merged incision margins: 6; absence of fibrin on the incision margins: 2; redness involving <50% of the incision length: 1). (C) The value of EHS is 5 (incision margins in contact: 3; bleeding at the incision margins: 0; absence of redness along the incision length: 2). (D) The value of EHS is 5 (incision margins in contact: 3; presence of fibrin on the incision margins: 1; redness involving <50% of the incision length: 1). (E) The value of EHS is 3 (incision margins in contact: 3; bleeding at the incision margins: 0; redness involving >50% of the incision length and/or pronounced swelling: 0). (F) The value of EHS is 1 (visible distance between incision margins: 0; bleeding at the incision margins: 0; redness involving <50% of the incision length: 1).
EHS: Early Wound Healing Score.
DISCUSSION
Even though numerous systems have been proposed to evaluate wound healing in oral soft tissues, a new method —EHS — was introduced in the present study in order to assess healing by primary intention 24 hours following surgical interventions.
In this study, the EHS was only assessed in vertical releasing incisions in order to better standardize the evaluation. However, the authors suggest that the EHS should be used to evaluate primary wound healing in other settings, such as papillary horizontal incisions and crestal linear incisions.
The EHS was intended to be used starting on the first postoperative day. It is thought to be important to start the evaluation at day 1 because, simultaneously with the haemostatic and inflammatory phases, re-epithelialization begins at 24 hours following tissue injury [2,8,15]. Even though this healing interval might seem too short for a clinical evaluation, since periodontal wound healing is not completed before 2–3 weeks of healing and even then is followed by further remodelling and tissue maturation, the purpose of the authors was specifically to assess the healing process of the wound surface at this early time interval [8].
The EHS was developed to analyse incision wounds in the early stages of healing by applying 3 parameters that correspond to the biological processes of oral soft tissue healing (haemostasis, inflammation, and re-epithelialization). Since these processes can only be definitively assessed histologically, the parameters of EHS were respectively named CSH, CSI, and CSR.
The present system allows for a strictly independent scoring of CSR, CSH, and CSI. The summation of the scores of each parameter generates the EHS score. The EHS for perfect wound healing is 10 points, and the worst EHS is 0 points. However, a score of 10 points is not intended to indicate the completion of the wound healing process, but rather uneventful early healing, which reflects a sequence of well-orchestrated, innate temporal and spatial events that dictate the outcomes of wound healing [8].
For CSR, the clinical signs assessed were merging, approximation, and distance of margins, which represent the progress of re-epithelialization. Since wound closure is essential for healing by primary intention, especially for periodontal wound healing, CSR was considered the main outcome [8]. Therefore, the CSR component was weighed to be 60% of the EHS. Accordingly, the following scores were assigned to CSR: 0 points if visible distance was present between the incision margins; 3 points if the incision margins were in contact; and 6 points if the incision margins had merged.
For CSH the clinical signs assessed were bleeding, fibrin, and the absence thereof, representing haemostasis in its schematic subdivisions (primary, secondary, and tertiary). Primary haemostasis, subclassified into a vascular and a platelet phase, is a crucial step in would healing, since the interruption of blood flow and clotting allow further steps of healing [16,17,18]. Slight bleeding is common for the first few hours after surgery, but it may occur for some additional hours or for 2–3 days due to suture loosening, flap instability, or dehiscence, which impede outcomes in the course of further wound healing [8]. Secondary haemostasis, through fibrinogen conversion, leads to fibrin clot formation. A thin fibrin clot is essential for rapid healing by primary intention and forms the initial seal between the oral environment and the wound edges. However, healing is delayed by the formation of a large coagulum, which occupies excessive space and is associated with inadequate re-approximation of wound edges [19]. Tertiary haemostasis, as the final stage in the process, occurs when the fibrinolytic system disrupts the fibrin clot. A delay of the haemostatic phase may result in increased swelling, pain, and delayed postoperative healing [20]. Accordingly, the following scores were assigned to CSH: 0 points in the presence of bleeding at the incision margins; 1 point in the presence of fibrin on the incision margins; and 2 points in the absence of fibrin on the incision margins. CSH was scored as 1 point in the presence of fibrin covering necrotic tissue, due to insufficient blood supply during postoperative healing.
For CSI, the clinical signs assessed were redness and swelling, representing 2 visually distinguishable cardinal signs of inflammation. Healing is considered to be dependent on the inflammatory process to create a favourable environment for cellular metabolism by removing microorganisms, necrotic or damaged tissue, and particulate matter [3,4]. However, poor flap closure, excessive tissue injury during surgical manipulation, and prolonged retention of sutures in the tissues prolong the debridement activities of the inflammatory process and delay the onset of healing mechanisms [17,19,20,21]. Accordingly, the following scores were assigned for CSI: 0 points in the presence of redness involving >50% of the incision length and/or pronounced swelling; 1 point in the presence of redness involving <50% of the incision length; and 2 points in the absence of redness along the incision length. The adjacent healthy gingiva was used as the reference to judge changes in tissue colour and swelling, while the incision area was defined between 2 mm along each side of the incision margins.
Pain perception, a third cardinal sign of inflammation, was not taken into consideration for the evaluation. Although pain is of high clinical importance, this symptom was considered too subjective for a clinical score and could negatively interfere with the objective assessment [22].
Suppuration, identified as a turbid or creamy exudate, is caused by white blood cells and bacteria, and therefore is indicative of an infection [23]. Since infection was considered to be a major adverse event during early wound healing, if suppuration was present, the EHS was scored as 0.
In the present study, clinical cases are presented to illustrate the use of the EHS system.
Several clinical cases (16 of 30; 53.33%) achieved the maximum CSR score at 24 hours of follow-up and 6 achieved the highest EHS (10 points), demonstrating perfect early wound healing. Within their limits, the results concerning the present score have shown that periodontal soft tissues have a remarkable early wound healing ability, which has also been observed when the EHI [10] and WHI [13] were used to evaluate wound healing.
Conversely, other vertical releasing incisions (13 of 30; 43.33%) received 3 points for CSR at 24 hours post-surgery, suggesting incomplete re-epithelialization. In most cases, this was a consequence of incomplete closure at the tooth surface. Flap dehiscence only occurred in 1 case.
Concerning the clinical signs of haemostasis, 15 cases (50%) did not present fibrin on the incision margins (CSH score of 2), 7 cases (23.3%) exhibited fibrin (CSH score of 1), and 8 cases (26.6%) showed bleeding from the incision margins (CSH score of 0).
Regarding the clinical signs of inflammation, half of the total vertical releasing incisions (15 of 30; 50%) did not exhibit any redness (CSI score of 2), while most others (14 of 30; 46.6%) revealed moderate redness (CSI score of 1). One vertical releasing incision (3.3%) presented pronounced redness and swelling (CSI score of 0). Taken together, the distribution of the given scores over a broad range, with few cases reaching the maximal score of 10, shows the applicability of the component sub-scores and the EHS itself.
Among the limitations of EHS, as for the above-mentioned indices, it should be emphasized that all parameters were arbitrarily weighted. However, this is an essential simplification for an approximate estimation of the early healing of incisional wounds. The approach used for the EHS was inspired by previously published assessment methods [24].
Finally, no sample size calculation was possible for this pilot study. Considering the novel nature of EHS, no previous equivalent or sufficiently comparable data were available for a reasonable calculation. However, the authors consider that the information presented herein could be useful to preliminarily illustrate the different clinical presentations of the early healing of periodontal soft tissue wounds and their assessment by using the proposed system. For future studies, data from the present study are available and might be considered for sample size calculations.
In conclusion, the EHS system may be a useful tool for assessing wound healing by primary intention in periodontal soft tissues after surgical incisions, and would also be of significant aid for communications between clinicians and researchers, thereby promoting a better understanding of the clinical presentation of early wound healing.
Footnotes
Author Contributions: Conceptualization: Lorenzo Marini, Andrea Pilloni; Data curation: Lorenzo Marini; Formal analysis: Lorenzo Marini; Investigation: Lorenzo Marini, Andrea Pilloni; Methodology: Rustam Aghazada, Lorenzo Marini, Mariana Andrea Rojas, Philipp Sahrmann; Project administration: Andrea Pilloni; Supervision: Andrea Pilloni; Visualization: Rustam Aghazada, Mariana Andrea Rojas, Philipp Sahrmann, Andrea Pilloni; Writing - original draft: Lorenzo Marini; Writing - review & editing: Rustam Aghazada, Mariana Andrea Rojas, Philipp Sahrmann, Andrea Pilloni.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.American Academy of Periodontology. Glossary of periodontal terms. 4th ed. Chicago (IL): American Academy of Periodontology; 2001. [Google Scholar]
- 2.Wikesjö UM, Selvig KA. Periodontal wound healing and regeneration. Periodontol 2000. 1999;19:21–39. doi: 10.1111/j.1600-0757.1999.tb00145.x. [DOI] [PubMed] [Google Scholar]
- 3.Aukhil I. Biology of wound healing. Periodontol 2000. 2000;22:44–50. doi: 10.1034/j.1600-0757.2000.2220104.x. [DOI] [PubMed] [Google Scholar]
- 4.Häkkinen L, Uitto VJ, Larjava H. Cell biology of gingival wound healing. Periodontol 2000. 2000;24:127–152. [PubMed] [Google Scholar]
- 5.Polimeni G, Xiropaidis AV, Wikesjö UM. Biology and principles of periodontal wound healing/regeneration. Periodontol 2000. 2006;41:30–47. doi: 10.1111/j.1600-0757.2006.00157.x. [DOI] [PubMed] [Google Scholar]
- 6.Hiatt WH, Stallard RE, Butler ED, Badgett B. Repair following mucoperiosteal flap surgery with full gingival retention. J Periodontol. 1968;39:11–16. doi: 10.1902/jop.1968.39.1.11. [DOI] [PubMed] [Google Scholar]
- 7.Werfully S, Areibi G, Toner M, Bergquist J, Walker J, Renvert S, et al. Tensile strength, histological and immunohistochemical observations of periodontal wound healing in the dog. J Periodontal Res. 2002;37:366–374. doi: 10.1034/j.1600-0765.2002.01375.x. [DOI] [PubMed] [Google Scholar]
- 8.Susin C, Fiorini T, Lee J, De Stefano JA, Dickinson DP, Wikesjö UM. Wound healing following surgical and regenerative periodontal therapy. Periodontol 2000. 2015;68:83–98. doi: 10.1111/prd.12057. [DOI] [PubMed] [Google Scholar]
- 9.Landry RG, Turnbull RS, Howley T. Effectiveness of benzydamyne HCl in the treatment of periodontal post-surgical patients. Res Clin Forums. 1988;10:105–118. [Google Scholar]
- 10.Wachtel H, Schenk G, Böhm S, Weng D, Zuhr O, Hürzeler MB. Microsurgical access flap and enamel matrix derivative for the treatment of periodontal intrabony defects: a controlled clinical study. J Clin Periodontol. 2003;30:496–504. doi: 10.1034/j.1600-051x.2003.00013.x. [DOI] [PubMed] [Google Scholar]
- 11.Hagenaars S, Louwerse PH, Timmerman MF, Van der Velden U, Van der Weijden GA. Soft-tissue wound healing following periodontal surgery and Emdogain application. J Clin Periodontol. 2004;31:850–856. doi: 10.1111/j.1600-051X.2004.00571.x. [DOI] [PubMed] [Google Scholar]
- 12.Tonetti MS, Fourmousis I, Suvan J, Cortellini P, Brägger U, Lang NP, et al. Healing, post-operative morbidity and patient perception of outcomes following regenerative therapy of deep intrabony defects. J Clin Periodontol. 2004;31:1092–1098. doi: 10.1111/j.1600-051X.2004.00615.x. [DOI] [PubMed] [Google Scholar]
- 13.Huang LH, Neiva RE, Wang HL. Factors affecting the outcomes of coronally advanced flap root coverage procedure. J Periodontol. 2005;76:1729–1734. doi: 10.1902/jop.2005.76.10.1729. [DOI] [PubMed] [Google Scholar]
- 14.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 15.Woodley DT. Reepithelialization. In: Clark RAF, editor. The molecular and cellular biology of wound repair. New York (NY): Plenum Press; 1996. pp. 339–354. [Google Scholar]
- 16.Gale AJ. Continuing education course #2: current understanding of hemostasis. Toxicol Pathol. 2011;39:273–280. doi: 10.1177/0192623310389474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Politis C, Schoenaers J, Jacobs R, Agbaje JO. Wound healing problems in the mouth. Front Physiol. 2016;7:507. doi: 10.3389/fphys.2016.00507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larjava H. Oral wound healing: cell biology and clinical management. Chichester: John Wiley & Sons, Inc.; 2012. [Google Scholar]
- 19.Harrison JW. Healing of surgical wounds in oral mucoperiosteal tissues. J Endod. 1991;17:401–408. doi: 10.1016/S0099-2399(06)81994-1. [DOI] [PubMed] [Google Scholar]
- 20.Kumar KR, Kumar J, Sarvagna J, Gadde P, Chikkaboriah S. Hemostasis and post-operative care of oral surgical wounds by hemcon dental dressing in patients on oral anticoagulant therapy: a split mouth randomized controlled clinical trial. J Clin Diagn Res. 2016;10:ZC37–ZC40. doi: 10.7860/JCDR/2016/17275.8462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin P, Leibovich SJ. Inflammatory cells during wound repair: the good, the bad and the ugly. Trends Cell Biol. 2005;15:599–607. doi: 10.1016/j.tcb.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Young EE, Lariviere WR, Belfer I. Genetic basis of pain variability: recent advances. J Med Genet. 2012;49:1–9. doi: 10.1136/jmedgenet-2011-100386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pippi R. Post-surgical clinical monitoring of soft tissue wound healing in periodontal and implant surgery. Int J Med Sci. 2017;14:721–728. doi: 10.7150/ijms.19727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cairo F, Rotundo R, Miller PD, Jr, Pini Prato GP. Root coverage esthetic score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J Periodontol. 2009;80:705–710. doi: 10.1902/jop.2009.080565. [DOI] [PubMed] [Google Scholar]