Abstract
A 1-year-old female toddler who was under a great amount of psychological stress presented with acute hematemesis. She had no significant medical history; she displayed lethargy and was anemic. Although blood transfusion and famotidine were administered for upper gastrointestinal bleeding (UGIB), the anemia did not improve. Thus, early endoscopy was performed under general anesthesia, revealing a gastric ulcer with exposed vessels in the supra-angular region. Cauterization via bipolar hemostatic forceps was performed on the exposed vessels, and the bleeding was controlled successfully. We diagnosed the patient with hemorrhagic stress-induced gastric ulcer due to psychological stress. Three months later, endoscopy revealed that the gastric ulcer had healed.
Keywords: stress-induced gastric ulcer, upper gastrointestinal bleeding, toddler
Introduction
Stress-induced ulcers may develop during the neonatal period due to birth asphyxia, prolonged labor, Caesarean deliveries, respiratory distress syndrome, instrumentation, and sepsis. Such ulcers occur more frequently in the stomach than in the esophagus or duodenum (1,2). Gastric bleeding from a stress-induced ulcer is an uncommon, but previously documented, entity in neonates (3) that presents as acute onset of gastrointestinal bleeding, commonly with bloody vomitus resembling coffee grounds, hematemesis, and melena. However, hemorrhagic stress-induced gastric ulcer is even more unusual in toddlers, particularly those who are healthy. To our knowledge, hemorrhagic stress-induced gastric ulcer treated successfully by endoscopic hemostasis has never been reported in a healthy toddler.
We herein report an extremely rare case of hemorrhagic stress-induced gastric ulcer in a healthy toddler.
Case Report
A 1-year-old girl was brought to our hospital with acute hematemesis with vomitus resembling coffee grounds. She was born at full-term (Ballard score 39 weeks) with a birth weight of 2.56 kg through vaginal delivery and without birth asphyxia. She had no remarkable medical history, no allergies, and had received no drugs, such as nonsteroidal anti-inflammatory drugs. She also had no notable family history.
On an examination, she was lethargic, had a heart rate of 160 beats/min, respiratory rate of 24 breaths/min, blood pressure of 83/35 mmHg, and oxygen saturation of 100% with nasal oxygen, 2 L/min. On a physical examination, she was normal, except for facial pallor. A nasogastric (NG) tube was inserted into her stomach, and a small amount of blood mixed with gastric fluid was aspirated through the NG tube.
Her laboratory test results were as follows: white blood cell count (WBC), 9,500/μL; hemoglobin (Hb), 7.2 g/dL; platelet count, 220×103/μL; C-reactive protein (CRP) level, 0.55 mg/dL; normal liver function tests, blood coagulation ability [prothrombin time, 13.2 seconds (INR: 1.01), and activated partial thromboplastin time, 31.7 seconds (reference range 24-32 seconds)], factor XIII levels, and plasma gastrin level; erythrocyte sedimentation rate, 2 mm/h (reference range, 0-20 mm/h); and serum cytomegalovirus-IgM, Epstein-Bar virus viral-capsid antigen-IgM, and Helicobacter pylori-IgG, negative. A stool antigen test showed no H. pylori infection. Blood culture was negative. Stool testing also yielded negative results for parasitic infection. Abdominal radiography and ultrasonography findings were normal. Contrast-enhanced computed tomography revealed no active bleeding.
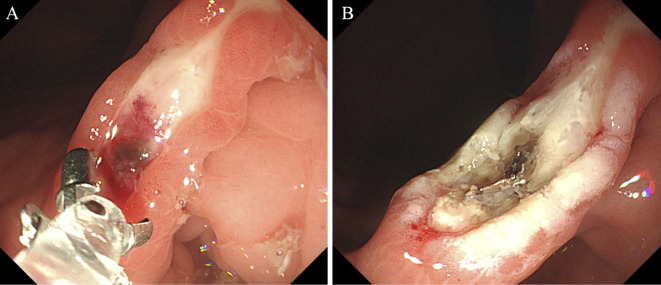
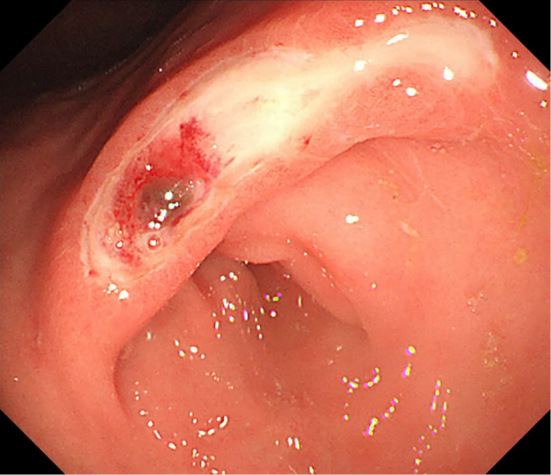
The patient was managed conservatively with fresh blood transfusion. Famotidine (10 mg/day) was added due to the suspicion of stress-induced gastric ulcer bleeding. No episodes of fresh blood vomitus or further bloody NG aspiration were observed after admission. However, her hemoglobin levels did not sufficiently recover, even after 2 units of fresh blood transfusion and initiation of famotidine treatment. Thus, on the second day of admission, early endoscopy (GIF-Q260J; Olympus, Tokyo, Japan) was performed under general anesthesia. Upper gastrointestinal (GI) endoscopy showed a gastric ulcer with exposed vessels in the supra-angular region (Fig. 1). No other mucosal lesions were observed in the stomach. The esophagus and duodenum were apparently normal. Cauterization via bipolar hemostatic forceps was performed on the exposed vessels, and the bleeding was controlled successfully (Fig. 2). No recognized complications occurred during the endoscopy procedures. On the same day after endoscopic treatment, extubation was performed successfully, and oral intake was started on the fourth day. On the 5th day, oral esomeprazol (0.5 mg/kg) was administered to replace famotidine. Subsequently, the patient had no recurrence of GI bleeding and was discharged on the seventh day.
Figure 1.
A gastrointestinal endoscopic examination. Upper gastrointestinal (GI) endoscopy showing a gastric ulcer with exposed vessels in the supra-angular region.
Figure 2.
A gastrointestinal endoscopic examination. Cauterization via bipolar hemostatic forceps was performed on the exposed vessels, and the bleeding was controlled successfully.
Her mother reported that she had vehemently refused to attend nursery school every day since approximately one month prior to the onset of hematemesis. Based on this information, her profile, and her laboratory findings, we diagnosed the patient with hemorrhagic stress-induced gastric ulcer due to psychological stress. After discharge, her mother allowed her to not attend nursery school, thereby removing her psychological stress. Hemoglobin gradually improved to the normal range, and there was no recurrence of upper GI bleeding (UGIB).
Repeat endoscopy (GIF-Q260J; Olympus) was performed three months after the cauterization. Endoscopy revealed that the gastric ulcer had healed with a white scar (Fig. 3), with no abnormal findings noted on a biopsy (Fig. 4). Narrow-band imaging also showed no obvious malignant findings. We therefore stopped administering oral esomeprazole after the second endoscopy. There has been no recurrence of symptoms and anemia suggestive of UGIB at the one-year follow-up.
Figure 3.
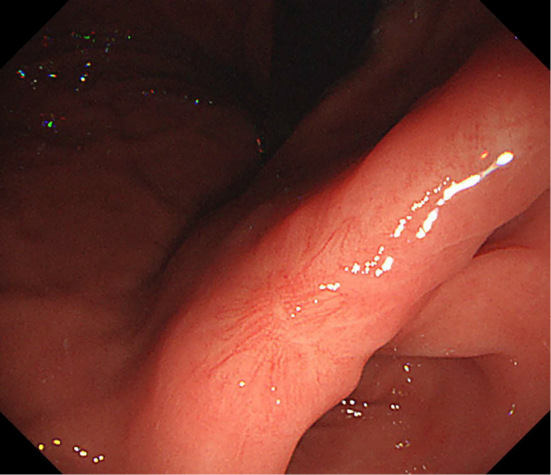
A gastrointestinal endoscopic examination. Three months after cauterization, the gastric ulcer healed with a white scar.
Figure 4.
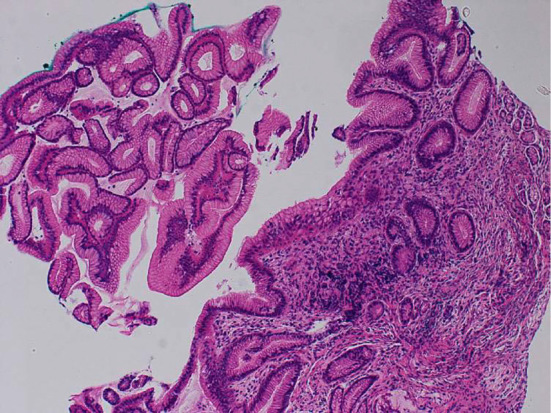
Pathological images of the biopsy specimens. A gastric biopsy showing regenerative changes, little inflammatory infiltration, and no abnormal findings in the gastric mucosal epithelium (Hematoxylin and Eosin staining, ×20).
Discussion
The occurrence of severe stress-induced lesions of the upper GI tract in the neonatal period of life, mainly in preterm newborn babies or in neonates treated in intensive-care units, is relatively frequent (4,5). Stress-induced lesions, such as erosive gastritis, gastric or duodenal ulcers, and esophagitis with or without gastric lesions, are observed in up to 75% of preterm newborn babies admitted to neonatal intensive-care units (6). However, significant UGIB is uncommon. Hemorrhagic complications are described in only 6% of children, even in intensive care (5,7). In such patients, mucosal ulcers are usually classified as secondary stress ulcers or are associated with other serious conditions, such as intracerebral bleeding, raised intracranial pressure, congenital heart disease, asphyxia, respiratory failure, and hypoglycemia (8,9). The first description of stress-induced gastric lesions in infants was published by Liebman et al. (4). Since then, there have been several case reports on stress-induced ulcers and erosions in infants, particularly in preterm infants. Furthermore, a few seemingly healthy infants were reported to have massive or even fatal UGIB that developed in the first 48 hours of life (4,10-12). In these infants, diffuse hemorrhagic gastritis with multiple gastric erosions or duodenal ulcers accounted for the bleeding (4,10,11).
The occurrence of significant UGIB in healthy toddlers is even more unusual. A search of the English literature revealed no cases of hemorrhagic stress-induced gastric ulcers in healthy toddlers. To our knowledge, this report is the first documented case of hemorrhagic stress-induced gastric ulcer in which endoscopic hemostasis was successfully achieved in a healthy toddler.
Hemorrhagic gastric ulcer shows an acute onset of GI bleeding commonly with vomitus resembling coffee grounds, hematemesis, and melena. Our patient presented with a hemorrhagic stress-induced gastric ulcer characterized by hematemesis with vomitus resembling coffee grounds. In varying percentages of patients, stress-induced ulcer leads to clinically significant GI hemorrhaging. Therefore, particularly in infants, once stress-induced ulcers cause significant hemorrhaging, the likelihood of mortality approaches 40% (13). Massive UGIB is associated with a relatively high mortality rate.
The etiology of UGIB in healthy toddlers is obscure, and stress-induced gastric ulcer is difficult to diagnose. Our patient did not undergo Caesarean delivery, nor did she experience birth asphyxia, use mechanical ventilation, exhibit an electrolyte imbalance, or develop neonatal seizures. As such, no stressful factors were present at birth; however, strong psychological stress was present. Furthermore, she did not have congenital heart disease, hemostasis disorders, inherited bleeding disorders, vascular anomalies, milk protein allergy, or sepsis. In addition, coagulopathies, serum antiparasite antibody, antinuclear antibody, and antineutrophil cytoplasmic antibody were negative. Thus, parasitic infection, collagen disease, and vasculitis were ruled out. We ultimately diagnosed the patient with a hemorrhage stress-induced gastric ulcer due to the presence of psychological stress and absence of any other precipitating factors.
Stress-induced gastric ulcers are widely attributed to circulatory disturbances in the stomach, since stress results in reflex vasospasms, thereby leading to gastric congestion and possible mucosal ischemia. This results in devitalization of the mucus membrane with subsequent peptic digestion of the damaged area (14). As a result, stress-induced gastric ulcers affect mainly the gastric body, as it is the area most vulnerable to ischemic injury (15). The pathogenesis of stress-induced ulcers due to psychological stress is unknown, but we speculated that psychological stress impaired the ability of the intact gastric mucosa to maintain homeostasis in addition to the above speculative etiology. As a result, stress-induced gastric ulcer leading to massive UGIB was diagnosed in this patient.
Proton pump inhibitors (PPIs) and histamine-2 (H2) receptor blockers used in newborns and infants have been shown to induce healing earlier than placebos (16). A gastric pH below 2.5 is a risk factor for the development of stress-induced ulcers and UGIB (17). In our patient, we first used oral esomeprazole (H2 receptor blocker) and performed blood transfusion; however, these approaches were not effective, nor did they lead to a clinical recovery of UGIB. Thus, our patient required endoscopy at an early stage. We can effectively and safely perform endoscopic examinations and endoscopic hemostasis treatments, even in young toddlers, using GIF-Q260F with an air- and water-supply system (distal portion outside diameter: 9.9 mm; forceps bore diameter: 3.2 mm). Thereafter, as the stressful event was resolved and the patient was treated with oral esomeprazol, the gastric ulcer gradually decreased in size and disappeared without significant episodes of bleeding.
Most cases of UGIB in newborns and infants are benign and self-limiting, and the outcome of UGIB after treatment with antisecretory drugs is generally rapid and favorable (8,18). They therefore usually do not warrant endoscopy; however, endoscopy must be performed in cases of acute severe hemorrhaging requiring blood transfusion or in cases of unexplained persistent bleeding even after antisecretory treatment, particularly in toddlers, as in our case.
In conclusion, hemorrhagic stress-induced gastric ulcers should always be considered in the differential diagnosis of healthy toddlers under psychological stress who present with massive UGIB. An early endoscopic examination and endoscopic hemostasis treatment should also be considered to satisfactorily stop bleeding from stress-induced gastric ulcers. We believe that the identification and treatment of hemorrhagic stress-induced gastric ulcers can significantly contribute to the prevention of morbidity and mortality in toddlers.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Mezoff AG, Balistreri WF. Peptic ulcer disease in children. Pediatr rev 16: 257-265, 1995. [DOI] [PubMed] [Google Scholar]
- 2.Shuman RB, Schuster DP, Zuckerman GR. Prophylactic therapy for stress ulcer bleeding: a reappraisal. Ann Intern Med 106: 562-567, 1987. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal AK, Saili A, Pandey KK, Saxena AK, Sarna MS, Dutta AK. Role of cimetidine in prevention and treatment of stress induced gastric bleeding in neonates. Indian Pediatr 27: 465-469, 1990. [PubMed] [Google Scholar]
- 4.Liebman WM, Thaler MM, Bujanover Y. Endoscopic evaluation of upper gastrointestinal bleeding in the newborn. Am J Gastroenterol 69: 607-608, 1978. [PubMed] [Google Scholar]
- 5.Lacroix J, Nadeau D, Laberge S, Gauthier M, Lapierre G, Farrell CA. Frequency of upper gastrointestinal bleeding in a pediatric intensive care unit. Crit Care Med 20: 35-42, 1992. [DOI] [PubMed] [Google Scholar]
- 6.de Boissieu D, Bargaoui K, Sakiroglu O, Francoual C, Dupont C, Badoual J. [Esophagogastroduodenitis in the newborn. Apropos of 32 cases]. Arch Fr Pediatr 46: 711-715, 1989(in French, Abstract in English). [PubMed] [Google Scholar]
- 7.Crill CM, Hak EB. Upper gastrointestinal tract bleeding in critically ill pediatric patients. Pharmacotherapy 19: 162-180, 1999. [DOI] [PubMed] [Google Scholar]
- 8.Goyal A, Treem WR, Hyams JS. Severe upper gastrointestinal bleeding in healthy full-term neonates. Ame J Gastroenterol 89: 613-616, 1994. [PubMed] [Google Scholar]
- 9.Oldham KT, Lobe TE. Gastrointestinal hemorrhage in children. A pragmatic update. Pediatr Clin North Am 32: 1247-1263, 1985. [DOI] [PubMed] [Google Scholar]
- 10.Pugh RJ, Newton RW, Piercy DM. Fatal bleeding from gastric ulceration during first day of life-possible association with social stress. Arch Dis Child 54: 146-148, 1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Man DW. Massive upper gastrointestinal bleeding from haemorrhagic gastritis in the newborn. Aust N Z J Surg 56: 871-872, 1986. [DOI] [PubMed] [Google Scholar]
- 12.Johnson D, L'Heureux P, Thompson T. Peptic ulcer disease in early infancy: clinical presentation and roentgenographic features. Acta Paediatr Scand 69: 753-760, 1980. [DOI] [PubMed] [Google Scholar]
- 13.Bell MJ, Keating JP, Ternberg JL, Bower RJ. Perforated stress ulcers in infants. J Pediatr Surg 16: 998-1002, 1981. [DOI] [PubMed] [Google Scholar]
- 14.Joshi A, Shrestha PS, Dangol S, Shrestha NC, Poudyal P, Shrestha AA. Stress induced gastric ulcers: presenting as massive rectal bleeding in a newborn. Kathmandu Unive Med J (KUMJ) 14: 186-189, 2016. [PubMed] [Google Scholar]
- 15.Fusamoto H, Hagiwara H, Meren H, et al. A clinical study of acute gastrointestinal hemorrhage associated with various shock states. Am J Gastroenterol 86: 429-433, 1991. [PubMed] [Google Scholar]
- 16.Sarna MS, Saili A, Dutta AK, Sharma D. Stress associated gastric bleeding in newborn-role of ranitidine. Indian Pediatr 28: 1305-1308, 1991. [PubMed] [Google Scholar]
- 17.Hawwa AF, Westwood PM, Collier PS, et al. Prophylactic ranitidine treatment in critically ill children-a population pharmacokinetic study. Br J Clin Pharmacol 75: 1265-1276, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deneyer M, Goossens A, Pipeleers-Marichal M, et al. Esophagitis of likely traumatic origin in newborns. J Pediatr Gastroenterol Nutr 15: 81-84, 1992. [DOI] [PubMed] [Google Scholar]