Abstract
Introduction:
This study assessed young athletes’ (ages 12 to 17) concussion attitudes and behaviors, particularly their self-reported experience learning about concussion and intentions to report a concussion and disparities in these experiences.
Methods:
We used data from Porter Novelli’s 2014 YouthStyles survey that is conducted each year to gather insights about American consumers.
Results:
Of the 1,005 respondents, 57% reported sports participation. Fourteen percent reported they may have had a previous concussion, and among them 41% reported having a concussion more than once while playing sports. Males (17.7%) were significantly more likely to report having a concussion than females (10.0%; χ2 (1) = 7.01, p = 0.008). Fifty-five percent of respondents reported having learned about what to do if they think they may have a concussion, and 92% reported that they would tell their coach if they thought they sustained a concussion while playing youth or high school sports. Youth from higher income families ($75,000–$124,999) were significantly more likely than youth from lower income families (less than $35,000) to report that they learned about what do if they suspected that they had a concussion.
Conclusion:
Age of athlete, parental income level, athlete’s sex, and living in a metro versus non-metro area led to disparities in athletes’ concussion education. There is a need for increased access to concussion education and an emphasis on customizing concussion education efforts to meet the needs of different groups.
Practical application:
We identified athletes’ self-reported previously sustained concussions and predictors of education related to concussion. Further research is needed to explore the age, gender and income gaps in concussion education among athletes.
Keywords: Concussion, Knowledge, Attitude, Behavior, Adolescent
1. Introduction
According to the Centers for Disease Control and Prevention (CDC), a concussion is “a type of traumatic brain injury caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and sometimes stretching and damaging the brain cells.” (Centers for Disease Control and Prevention et al., n.d.-a) A concussion is a serious injury, and while most youth athletes have a good recovery and feel better within a few weeks, sometimes symptoms can continue for months or longer (Centers for Disease Control and Prevention et al., n.d.-b). Across the country, nearly 60 million youth (National Council of Youth Sports, n.d.) benefit physically and psychologically from participating in organized youth sports where they develop important life skills, such as leadership and teamwork, and maintain healthy bones and muscles. Sports can provide significant benefits to young athletes (Physical Activity Guidelines Advisory Committee report, 2008; The Association Between School-based Physical Activity, 2010); however, protecting the health and safety of young athletes while participating in sports is critical.
In recent years, a heightened focus on sports-related concussion has emerged. A 2016 public opinion poll of 1000 American adults found widespread awareness of concussion, with 65% agreeing that sports-related concussions are a major problem (UMASS Lowell, n.d.). However despite increased awareness and efforts to protect young athletes, research suggests that too many young athletes still do not report their concussion symptoms, are not removed from play and continue to play with symptoms, or return to play too soon (Chrisman, Quitiquit, & Rivara, 2013; Hwang, Trickey, Lormel, Bradford, et al., 2014; McLeod, Schwartz, & Bay, 2007; O’Kane et al., 2014; Register-Mihalik et al., 2013; Rivara et al., 2014; Yard & Comstock, 2009).
Further, within the growing body of research on concussion, there is a scarcity of studies about health disparities and population-based factors that contribute to concussion-related health education, attitudes, and behaviors. To inform ongoing public health interventions aimed at protecting young athletes from concussion, this study contributes an analysis of concussion-related health disparities among youth athletes ages 12 to 17 who responded to the 2014 YouthStyles survey. Specifically, we assessed young athletes’:
Self-reported previously sustained concussions,
Predictors of education related to concussion, and
Concussion reporting behavioral intention.
We included access to education and demographic factors such as race and ethnicity, sex, and geographic location in our analysis. Research indicates that Americans, including young people (Probst, Barker, Enders, & Gardiner, 2016), who live in rural areas are at higher risk of mortality from unintentional injuries when compared to Americans who live in urban areas (Centers for Disease Control and Prevention, n.d.), and we hypothesized that concussion-related health disparities would exist among young athletes based on geographic factors such that young athletes who live in rural areas would report less access to concussion education when compared with young athletes who live in urban areas. We also explored whether concussion attitudes and behaviors varied between male and female athletes.
2. Methods
This study used data from Porter Novelli’s 2014 YouthStyles survey. Porter Novelli Public Services is a public relations firm contracted by CDC to design and implement the YouthStyles survey. The YouthStyles survey is part of a series of web-based surveys conducted each year to gather insights about American consumers, including information about their health attitudes and behaviors. Broadly, the YouthStyles survey explores relationships with friends, health behaviors, sources of influence, media habits, and media usage. The YouthStyles survey is fielded from June to July each year.
In June and July 2014, 1614 youth ages 12 to 17 residing with parents who are members of GfK’s Knowledge Panel® were invited to answer the YouthStyles survey. GfK’s KnowledgePanel® members are randomly recruited using probability-based sampling and include respondents regardless of whether or not they have landline phones or Internet access. If needed, households are provided with a laptop computer and access to the Internet. The panel is continuously replenished and maintains approximately 50,000 panelists. Adult panel members participated in a corresponding survey immediately prior to the youth’s participation and provided electronic consent for the youth to participate. Respondents were not required to answer individual questions and could exit the survey at any time for any reason. Of the 2153 households sampled, a total of 1005 YouthStyles surveys were returned, representing a response rate of 47%. Households that completed both the adult and youth surveys received reward points worth approximately $5 and were entered into a monthly sweepstakes.
The CDC was provided a license to access data from the 2014 YouthStyles survey post-collection from Porter Novelli, and analysis of these data was exempt from institutional review board approval because personal identifiers were not included in the data file.
The resulting data were weighted to match the U.S. Current Population Survey proportions for sex, age, race/ethnicity, number of youth ages 12 to 17 in the household, household income, parent education level, census region, metro status, and whether or not the household had internet access prior to joining the panel.
Seven questions about concussion in sports were included in the 2014 YouthStyles survey (see Table 1). The purpose of these questions was to assess young athletes’ attitudes and behavioral intention related to concussion.
Table 1.
2014 YouthStyles survey questions about concussion in sports.
| 1. | If you play youth or high school sports, what are the reasons that you play? |
| 2. | A concussion can be caused by a bump, blow, or jolt to the head that can cause things like headaches and dizziness and/or may make you feel sick to your stomach, confused, or sleepy. Please tell us if you may have gotten a concussion while playing youth or high school sports. |
| 3. | If you answered Yes to question 2, please tell us how many times you may have gotten a concussion while playing youth or high school sports. |
| 4. | Have you learned about what to do if you think you may have gotten a concussion while playing sports? |
| 5. | If you answered Yes to question 4, please tell us how you learned about what to do if you think you may have gotten a concussion while playing sports. |
| 6. | If you think you got a concussion while playing youth or high school sports, would you tell your coach? |
| 7. | If you answered No to question 6, please tell us why you wouldn’t tell your coach. |
To explore the context of potential health disparities among young athletes, backward stepwise logistic regression was used to examine the effects of socio-demographic factors influencing the likelihood of having received concussion education. The independent variables included were: a binary variable indicating whether or not a participant had ever received a concussion; the age of the participant; the gender of the participant; a categorical variable for the participant’s race/ethnicity; a categorical variable for the household income of the participant; a binary variable for whether or not a participant was located in a metropolitan area; and a binary variable for whether or not a participant had internet access. Lastly, variables examining a categorical by categorical interaction effect between metro status and both income and race/ethnicity category were included in the model to control for possible moderating factors.
3. Results
Among the 1005 respondents, over half (57%) reported sports participation and were included in the analysis. This study reports results among youth who indicated sports participation, or 573 of a total 1005 respondents. The remaining 422 respondents replied to Q1 that “I do not play youth or high school sports” and were therefore excluded from this analysis. Table 2 presents the self-reported demographic characteristics of youth who had played youth or high school sports.
Table 2.
Participants’ socio-demographics (n = 573).
| n | % | ||
|---|---|---|---|
| Child age | |||
| 12 | 109 | 19.0 | |
| 13 | 110 | 19.2 | |
| 14 | 109 | 19.0 | |
| 15 | 87 | 15.2 | |
| 16 | 84 | 14.7 | |
| 17 | 74 | 12.9 | |
| Child race/ethnicity | |||
| White, Non-Hispanic | 384 | 57.0 | |
| Black, Non-Hispanic | 48 | 8.4 | |
| Other, Non-Hispanic | 31 | 5.4 | |
| Hispanic | 80 | 14.0 | |
| Multiracial, Non-Hispanic | 30 | 5.2 | |
| Gender | |||
| Male | 300 | 52.4 | |
| Female | 273 | 47.6 | |
| Adult education | |||
| Less than high school | 17 | 3.0 | |
| High school | 82 | 14.3 | |
| Some college | 212 | 37.0 | |
| Bachelor’s degree or | 262 | 45.7 | |
| higher | |||
| Household income | |||
| Less than $35,000 | 95 | 16.6 | |
| $35,000 – $74,999 | 184 | 32.1 | |
| $75,000 – $124,999 | 203 | 20.2 | |
| $125,000 or more | 91 | 22.9 | |
| Household internet access | |||
| Yes | 564 | 98.4 |
When asked, “If you play youth or high school sports, what are the reasons that you play?” youth reported that they participate for various reasons, primarily because sports are fun (n = 514, 90%), their friends play sports (n = 314, 55%), and they want to be in shape (n = 308, 54%). Less common reasons for playing included wanting a college scholarship (n = 161, 28%), wanting to be a professional athlete (n = 103, 18%), and because their parents made them play (n = 67, 12%).
3.1. Previous concussions
Respondents were given the following definition: “A concussion can be caused by a bump, blow, or jolt to the head that can cause things like headaches and dizziness and/or may make you feel sick to your stomach, confused, or sleepy.” Following the definition, the majority of respondents (n = 491, 86%) reported that they have not had a concussion while playing youth or high school sports. Among those who did report they may have had a concussion (n = 80, 14%), over 40% reported having a concussion more than once while playing youth or high school sports (n = 32, 41%).
Both the binary and continuous measures of concussion incidence were examined across the key sociodemographic variables in the data set: household income; youth race/ethnicity; youth age; youth gender; adult education status; and whether or not they resided in a metropolitan area. The analyses used were logistic and linear regression, respectively. There were no significant relationships between the sociodemographic variables and the binary concussion incidence measure. From the results of the linear regression, being female was associated with less concussions when compared with males (Coefficient = −0.66, p value = 0.027) and identifying as race/ethnicity “other” was associated with significantly more concussions when compared to white youth. (Coefficient = 1.14, p value = 0.005).
3.2. Learning about concussions
More than half of youth athletes (n = 313, 55%) reported having learned about what to do if they think they may have a concussion while playing sports. These respondents reported learning about concussion from a range of information sources, including from: their coach (n = 185, 60%); reading a fact sheet about concussion (n = 123, 40%); their mother (n = 99, 32%); and their father (n = 84, 27%).
There was a positive and significant relationship between having received education about concussions and intention to report a concussion. This is true both in the Chi2 analysis (χ2 (1) = 14.74, p value = 0.001) and when controlling for sociodemographic factors in a logistic regression (OR =2.97, p value = 0.006) This indicates that after controlling for other factors, someone who has been educated about concussions is about three times more likely to have intentions to report a concussion, than someone who has not received education about concussion.
3.3. Sociodemographic determinants of concussion education
Table 3 shows the results of the logistic regression used to examine the effects of sociodemographic factors that influence the likelihood of having received concussion education. The relationship is positive and significant in the Fisher’s exact test (p value = 0.000) and as a coefficient in a larger logistic regression predicting concussion education OR = 1.45, p value = 0.000). Participants in the third income bracket ($75,000–$124,999) were significantly more likely to have received concussion education than those in the first income bracket (less than $34,999). There were no significant differences in education likelihood between the first income bracket and either the second income bracket ($35,000–$74,999) or the fourth income bracket ($125,000 and higher).
Table 3.
Logistic regression of sociodemographic factors and receiving concussion education.
| Odds ratio | P value | 95% CI | |
|---|---|---|---|
| Constant | 0.01 | 0.001 | [0.00,0.12] |
| Pastconcussion(s) | |||
| 0 | Reference | ||
| 1 or more | 3.19 | 0.001 | [1.64,6.21] |
| Youth age | 1.28 | 0.000 | [1.13,1.46] |
| Youth gender | |||
| Male | Reference | ||
| Female | 0.64 | 0.038 | [0.42, 0.98] |
| Adult education level | |||
| High school or less | Reference | ||
| High school | 1.53 | 0.550 | [0.38,6.23] |
| Some college | 2.13 | 0.270 | [0.55,8.19] |
| Bachelor’s degree or higher | 1.68 | 0.453 | [0.43, 6.54] |
| Metro status | |||
| Non-metro area | Reference | ||
| Metro area | 3.7 | 0.103 | [0.76,18.31] |
| Youth ethnicity | |||
| White | Reference | ||
| Black, Non-Hispanic | 1.69 | 0.760 | [0.07, 39.06] |
| Other, Non-Hispanic | 0.32 | 0.015 | [0.12,0.80] |
| Hispanic | 0.91 | 0.940 | [0.07,11.42] |
| 2 + races, Non-Hispanic | 0.473 | ||
| Youth ethnicity × metro status | |||
| Black | 0.41 | 0.586 | [0.16,10.38] |
| Other | Omitted* | ||
| Hispanic | 0.45 | 0.554 | [0.03, 6.22] |
| 2 + races, Non-Hispanic | Omitted* | ||
| Household income | |||
| $34,999 or less | Reference | ||
| $35,000 to $74,999 | 4.30 | 0.063 | [0.92,20.03] |
| $75,000 to $124,999 | 12.67 | 0.004 | [2.28,70.51] |
| $125,000 or more | 6.22 | 0.113 | [0.65,59.63] |
| Household income × metro status | |||
| $35,000 to $74,999 | 0.33 | 0.212 | [0.06,1.86] |
| $75,000 to $124,999 | 0.14 | 0.045 | [0.02, 0.96] |
| $125,000 or more | 0.30 | 0.319 | [0.03, 3.26] |
| Internet access | Omitted* |
Omitted variables due to low size.
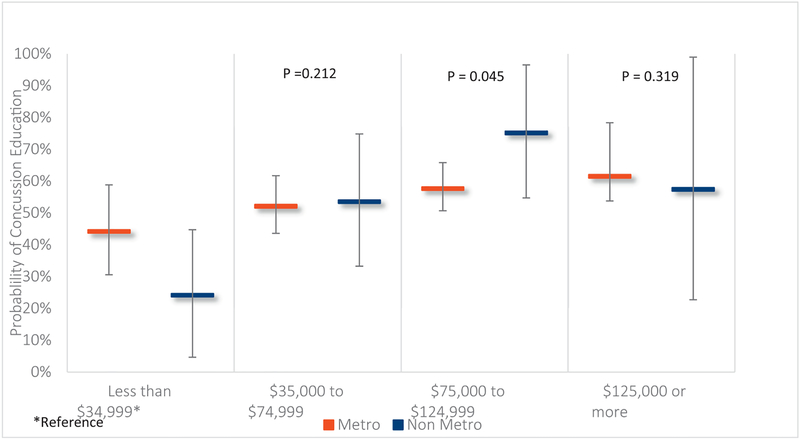
We also examined a possible moderation effect on the likelihood of receiving concussion education between the binomial measure of whether or not participants lived in a census designated metropolitan area and both their income category and race/ethnicity. While there was no evidence for a race/ethnicity moderating effect by metro status, there was significant evidence for differing effects of metro status on likelihood of education by income category.
Our analysis shows that there is a stronger positive relationship between income and concussion education among members of the non-metropolitan group compared to the metropolitan group. This trend is shown in Fig. 1, beginning with the lowest probability of concussion education among the non-metro members of the lowest income quartile (less than $34,999). The non-metro group catches and surpasses the metro groups’ members in the next two categories before decreasing in the final quartile ($125,000 and above). Statistical evidence supporting this trend is the significant interaction between the first (less than $34,999) and the third ($75,000 to $124,999) income quartiles indicating a significantly larger likelihood of concussion education for those in the non-metropolitan participants. The trend remains even with the slight decrease in probability of concussion education in the non-metropolitan group for the final income bracket.
Fig. 1.
Metro status moderates the effect of income on receiving concussion education.
3.4. Reporting concussions
The vast majority of youth athletes (n = 524, 92%) reported that they would tell their coach if they thought that they had sustained a concussion while playing youth or high school sports. There were no significant differences between youth who would tell their coach about a suspected concussion and those who would not tell their coach about a suspected concussion, in terms of age, race/ethnicity, or sex of respondent. Those who reported that they wouldn’t tell their coach about a suspected concussion reported that their reasons for not reporting were that they: didn’t want to stop playing (n = 19, 43%): didn’t want to look weak (n = 12, 27%), didn’t want to let their teammates down (n = 11, 25%), and didn’t want to lose their position on the team (n = 9, 21%). Other less common reasons for not telling a coach were “my coach would get mad” (n = 6; 14%), “my parents would get mad” (n = 4, 9%), “didn’t want to risk my future sports career” (n = 3, 7%), and “concussions aren’t that serious” (n = 3; 7%).
4. Discussion
Our study explored predictors of young athletes’ having learned about concussion. Older youth were significantly more likely than their younger peers to have learned about concussion, indicating a need for greater emphasis on concussion education that targets younger athletes. Younger athletes may also be more receptive to concussion education, and future research should evaluate outcomes of education among younger athletes relative to older athletes. A survey of young athletes found that youth ages 13–15 were significantly more likely than their older peers (ages 16–18) to strongly agree that concussion is a critical issue (Bloodgood, Inokuchi, Shawver, et al., 2013). Previous research has reported the influence of concussion education and training on concussion symptom reporting. A survey by Bramley, Patrick, Lehman, and Silvis (2012) found that the majority (72%) of high school athletes who received concussion training reported that they would always notify their coach of their concussion symptoms.
We identified several disparities among respondents related to their knowledge of what to do about a suspected concussion. First, we identified an income-level disparity among youth related to education about concussion. We found that youth from higher income families (between $75,000 to $124,999) were almost twice as likely to have learned about what to do if they suspected that they had had a concussion, compared to youth from lower income families (less than $35,000). This indicates a need to target education to ensure that youth from lower income families receive education about concussion. Future research should explore this disparity further and seek to identify opportunities to address it. Second, we identified that male respondents were significantly less likely than female respondents to report that they learned what to do if they suspected that they had had a concussion. And, at same time, males (17.7%) were significantly more likely to report having a concussion than females (10.0%; χ2 (1) = 7.01, p = .008). Our findings that males were more likely to report having a previous concussion and less likely to receive education about concussion are concerning. There are numerous potential explanations for this disparity that merit further study such as males being more likely to engage in unhealthy or risky behaviors or males being more likely to play with concussion symptoms prior to reporting them. Research is necessary to explore this gender gap, the basis for it, and potential strategies to overcome it and increase knowledge of what to do about a suspected concussion among both male and female athletes.
In addition, we found a significant interaction effect between income and metro status in relation to the likelihood of young athletes receiving education about concussion. The higher income group ($75,000 to $124,999) who live in a non-metro area were more likely to receive education about concussion than the lower income group (less than $34,999) who live in a non-metro area. There are several potential explanations for these differences, including lack of resources available to people with low income in non-metro areas and differences in lifestyle among the high income in both categories. This interaction also could explain differences in future studies and should be accounted for whenever possible. Further research is needed to explore geographic differences in access to and participation in concussion education. There was also a slight decrease in the probability of concussion education in the highest income bracket ($125,000 and above), and this requires further study. In particular, our sample included a smaller number of participants in this income bracket, and a sample that includes more prominent participation from individuals in this income bracket will contribute to understanding of the interaction between education and income.
In our study, the incidence of sustained concussions, self-reported by youth athletes, was low. Only 14% of youth athletes reported that they have had a concussion, based on the definition that they were provided. Similar studies have provided other definitions for concussion and found varying self-reported incidence rates of concussion. McDonald, Burghart, and Nazir (2016) assessed the concussion reporting behaviors among female high school athletes and found the reported incidence rate to be much higher than our findings, with approximately 40% of athletes reporting a suspected concussion. A cross-sectional survey by Register-Mihalik et al. (2013), using a convenience sample of high school athletes from nine different states, found that more than half (53%) of athletes recalled sustaining at least one possible concussion. Using existing databases, Bryan, Rowhani-Rahbar, Comstock, Rivara, et al. (2016) estimated the annual incidence of sports- and recreation-related concussion among youth ages 18 and younger and found that between 1.1 and 1.9 million occurred each year.
There are no national large scale surveillance systems that comprehensively measure the full range of youth sports concussion. In the absence of a national surveillance system, current efforts to collect data about the incidence of concussion via athlete self-report is needed (Bell, Breiding, & DePadilla, 2017). Wojtowicz, Iverson, Silverberg, Mannix, et al. (2017) found that high school athletes reliably and consistently reported their concussion histories when they were surveyed during high school. Limited research is available on the self-reported concussion incidence among younger elementary school aged athletes who participate in organized sports.
A potential explanation for the lower self-reported concussion incidence rate in our study is that we included youth and high school athletes who participated in all sports whereas some other studies, such as Register-Mihalik et al. (2013), that found higher incidence rates, included athletes who participate in specific sports with increased contact.
Overall, more accurate reporting mechanisms are needed to identify the incidence of concussion in youth and high school sports. The CDC is currently pilot testing a concussion surveillance system to track, monitor, and accurately determine how many Americans sustain a concussion each year and how the injury happened (Bell et al., 2017). After a planned pilot phase is complete, the hope is to scale up to a national concussion surveillance system that will be administered on an ongoing basis.
Another potential explanation for the lower self-reported concussion incidence rate in our study is based on the definition that we provided. Our definition was limited in that it did not include every sign and symptom of concussion, but rather named a few categories of symptoms (headaches, dizziness, sick to your stomach, confused, or sleepy). If respondents were provided with a more specific and comprehensive list of signs and symptoms, it is possible that a higher number of respondents would have reported a previous concussion.
Our study assessed concussion reporting intentions among young athletes and found that most youth athletes (92%) reported that they would tell their coach if they suspected that they had sustained a concussion. While encouraging, it’s evident from existing literature that in reality too many athletes do not report their concussion symptoms when they are injured. Rivara et al. (2014) found that 69% of concussed athletes reported playing with symptoms and 40% said that their coach wasn’t aware of their injury. Similarly, McDonald et al. (2016) found that nearly a third of athletes did not report their concussion symptoms to athletic training staff after their injury. This points to the complexity of concussion as a public health issue and the discrepancies between behavioral intentions and actual behavior. Closely examining the reasons athletes shared for not reporting their concussion symptoms points to several potential considerations for the breakdown between behavioral intentions and behavior.
We found that the most common reason that athletes chose not to report their concussion symptoms was that the athletes wanted to keep playing (43%), which signals the strength of this internal pressure and its influence on behavior. Additionally, athletes were concerned that reporting their concussion would translate into losing their position on their team (21%). These findings are consistent with a retrospective survey conducted by McCrea, Hammeke, Olsen, Leo, and Guskiewicz (2004) that found that motivation to continue competition was a common reason for athletes not to report a suspected concussion. Register-Mihalik et al. (2013) also found that athletes did not report their concussion symptoms because they did not want to be removed from practice. Combined, these underlying attitudes reflect the intensity of youth and high school sports, and the innate pressure that young athletes face to “tough it out” and play through injury (Kroshus, Garnett, Hawrilenko, Baugh, et al., 2015; O’Connell & Manschreck, 2012).
Further research is needed to assess the gap between young athletes’ intention to report concussion symptoms and actual reporting behavior. There are potential external (e.g., policies, social pressures, environmental contributors) and internal (e.g., biological) factors that may lead to this discrepancy. Additional research is needed to uncover the real-life barriers that interfere with concussion reporting behavior among youth athletes.
There are several limitations of our study. Our survey uncovered income, sex, and geographic factors that related to receipt of concussion education; however more research is needed to explore these health disparities. It is apparent that health disparities exist among youth athletes of various backgrounds. We lack an understanding of the relationship of these demographic factors, how they contribute to these gaps, and what role they play as facilitators or barriers to concussion education. Further, the concussion definition that was provided to participants in this study may have limited the number of participants who reported a previous concussion because the definition did not provide every concussion sign and symptom. Future studies would benefit from using a consistent definition that includes a comprehensive list of the potential signs and symptoms of concussion. Health disparities in concussion education and related behaviors remain an understudied area of concussion research and these findings provide initial data that can inform initial research and future studies.
5. Practical application
Most Americans are concerned about sports-related concussion. We assessed young athletes’ self-reported previously sustained concussions, predictors of education related to concussion, and concussion-reporting behavior, with a focus on uncovering concussion-related health disparities among youth athletes.
Acknowledgments
The Journal of Safety Research has partnered with the Office of the Associate Director for Science, Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control at the CDC in Atlanta, Georgia, USA, to briefly report on some of the latest findings in the research community. This report is the 50th in a series of “From the CDC” articles on injury prevention.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Biographies
Zoe Donnell, MA, Manager, ICF.
Roseanne Hoffman, MPH, Senior Manager, ICF.
Kelly Sarmiento, MPH, Health Communication Specialist, CDC.
Cameron Hays, MHS, Associate, ICF.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Bell JM, Breiding MJ, & DePadilla L (2017, September). CDC’s efforts to improve traumatic brain injury surveillance. Journal of Safety Research, 62, 253–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloodgood B, Inokuchi D, Shawver W, et al. (2013). Exploration of awareness, knowledge, and perceptions of traumatic brain injury among American youth athletes and their parents. Journal of Adolescent Health, 53(1), 34–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramley H, Patrick K, Lehman E, & Silvis M (2012). High school soccer players with concussion education are more likely to notify their coach of a suspected concussion. La Clinica Pediatrica, 51(4), 332–336. [DOI] [PubMed] [Google Scholar]
- Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F, et al. (2016, July). Sports- and recreation-related concussions in US youth. Pediatrics, 138(1). 10.1542/peds.2015-4635 (pii: e20154635). [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (d). Rural Americans at higher risk of death from five leading causes. (Available at) https://www.cdc.gov/media/releases/2017/p0112-rural-death-risk.html, Accessed date: 13 April 2017.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, & Division of Unintentional Injury Prevention (d). What is a concussion? (Available at) http://www.cdc.gov/headsup/basics/concussion_whatis.html, Accessed date: 8 November 2016. [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, & Division of Unintentional Injury Prevention (d). Recovery from concussion. (Available at) http://www.cdc.gov/headsup/basics/concussion_recovery.html, Accessed date: 8 November 2016.
- Chrisman SP, Quitiquit C, & Rivara FP (2013). Qualitative study of barriers to concussive symptom reporting in high school athletics. The Journal of Adolescent Health, 52(3), 330–335. [DOI] [PubMed] [Google Scholar]
- Hwang V, Trickey AW, Lormel C, Bradford, et al. (2014). Are pediatric concussion patients compliant with discharge instructions? Journal of Trauma and Acute Care Surgery, 77(1), 117–122. [DOI] [PubMed] [Google Scholar]
- Kroshus E, Garnett B, Hawrilenko M, Baugh C, et al. (2015, June). Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Social Science & Medicine, 134, 66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrea M, Hammeke T, Olsen G, Leo P, & Guskiewicz K (2004, January). Unreported concussion in high school football players: implications for prevention. Clinical Journal of Sport Medicine, 14(1), 13–17. [DOI] [PubMed] [Google Scholar]
- McDonald T, Burghart MA, & Nazir N (2016, Sep-Oct). Underreporting of concussions and concussion-like symptoms in female high school athletes. Journal of Trauma Nursing, 23(5), 241–246. 10.1097/JTN.0000000000000227. [DOI] [PubMed] [Google Scholar]
- McLeod TCV, Schwartz C, & Bay RC (2007, March). Sport-related concussion misunderstanding among youth coaches. Clinical Journal of Sport Medicine, 17(2), 140–141. [DOI] [PubMed] [Google Scholar]
- National Council of Youth Sports (d). National Council of Youth Sports. (Available at) http://www.ncys.org/, Accessed date: 8 November 2016. [Google Scholar]
- O’Connell S, & Manschreck C (2012, July). Playing through the pain: Psychiatric risks among young athletes. Current Psychiatry, 11(7), 16–20. [Google Scholar]
- O’Kane JW, Spieker A, Levy MR, Neradilek M, Polissar NL, & Schiff MA (2014). Concussion among female middle-school soccer players. JAMA Pediatrics, 168, 258–264. [DOI] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee report (2008). Washington, DC: U.S. Department of Health and Human Services, 2008. [Google Scholar]
- Probst JC, Barker JC, Enders A, & Gardiner P (2016, September 8). Current state of child health in rural America: How context shapes children’s health. The Journal of Rural Health (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Register-Mihalik JK, Guskiewicz KM, McLeod TC, Linnan LA, Mueller FO, & Marshall SW (2013, Sep-Oct). Knowledge, attitude, and concussion-reporting behaviors among high school athletes: A preliminary study. Journal of Athletic Training, 48(5), 645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivara FP, Schiff MA, Chrisman SP, Chung SK, Ellenbogen RG, & Herring SA (2014, May). The effect of coach education on reporting of concussions among high school athletes after passage of a concussion law. The American Journal of Sports Medicine, 42(5), 1197–1203. [DOI] [PubMed] [Google Scholar]
- The Association Between School-based Physical Activity (2010). Including physical education, and academic performance. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. [Google Scholar]
- UMASS Lowell (d). Attitudes towards sports and concussion. (Available at) https://www.uml.edu/Research/public-opinion/polls/2016/concussion.aspx, Accessed date: 8 November 2016.
- Wojtowicz M, Iverson GL, Silverberg ND, Mannix R, et al. (2017, January 15). Consistency of self-reported concussion history in adolescent athletes. Journal of Neurotrauma, 34(2), 322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yard EE, & Comstock RD (2009, October). Compliance with return to play guidelines following concussion in US high school athletes, 2005–2008. Brain Injury, 23(11), 888–898. [DOI] [PubMed] [Google Scholar]