Abstract
Background:
Management of obstructive hydrocephalus is an important issue for the reduction of mortality and morbidity.
Objectives:
The aim of the present study was to assess the early surgical outcome of endoscopic third ventriculostomy (ETV) in the management of obstructive hydrocephalus.
Methodology:
This randomized controlled trial was conducted at the Department of Neurosurgery at Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh, from April 2009 to September 2010 for 1½ years. All patients presenting with obstructive hydrocephalus with the obstruction at or distal to the third ventricle and age 6 months and above were included in the study population. All the patients were divided into two groups named as Group A (experimental group) who were treated with ETV and Group B (control group) who were treated with ventriculoperitoneal shunt (VPS). The early surgical outcome was defined as outcomes within 1 month following surgical interventions. Pre- and post-operative outcomes of this study were measured.
Results:
A total number of sixty patients were recruited from which thirty patients were in Group A and the rest thirty patients were in Group B. The mean postoperative head circumference was 43.4 ± 7.1 cm and 47.8 ± 5.6 cm in VPS and ETV surgery, respectively (P ≤ 0.01). Postoperative vomiting was improved 24 (92.3%) in Group A and 23 (88.5%) in Group B (P < 0.05). Postoperative infection occurred in 1 (3.3%) case in Group A and 8 (26.7%) cases in Group B (P < 0.05). The success of the operation in Group A and Group B included 25 (83.3%) cases and 12 (40%) cases, respectively (P < 0.05).
Conclusion:
Early surgical outcome following ETV is better than VPS surgery in patients with obstructive hydrocephalus.
Keywords: Endoscopic third ventriculostomy, obstructive hydrocephalus, surgical outcomes, ventriculoperitoneal shunt
Introduction
Obstructive hydrocephalus is one of the common conditions in hospital settings that require surgery.[1] It is managed either by endoscopic third ventriculostomy (ETV) or by ventriculoperitoneal shunt (VPS) surgery. The morbidity of VPS surgery is very high.[2] Some patients even die following repeated shunt infection. The cost of shunt hardware, antibiotics the following infection, and increased hospital stay result in financial loss.[3] Therefore, the economic burden of shunt infection is huge.
ETV is now considered a safe and effective treatment for obstructive hydrocephalus in selected patients.[4] In addition, ETV has numerous potential benefits over the standard shunt procedure, which possesses its own set of inherent risks and complications; these include infection, slit ventricle syndrome, and mechanical malfunction.[5]
Indications for performing ETV are based on computed tomography (CT) or magnetic resonance imaging (MRI) findings that demonstrate a noncommunicating type of hydrocephalus with obstruction at the level of or distal to the posterior third ventricle.[6] Patients with hydrocephalus from aqueductal stenosis are, in general, excellent candidates for ETV. Although it is controversial, patients <6 months of age have not had good results with ETV, and most authors do not advocate the procedure in this group.[7] The management of hydrocephalus needs cerebrospinal fluid (CSF) diversion either extracranially by shunt surgery or intracranially by ETV. Extracranial shunts are subject to complications such as blockage, infection, and overdrainage often necessitating repeated surgical revisions.[8] ETV obviates all these complications. Various studies have shown that ETV has fewer complications, more cost effectiveness, and shorter hospital stay.[9] There is no similar study done in Bangladesh. This study compares the early surgical outcome following ETV and VPS surgery, which may be helpful to manage such patients in future. Therefore, this present study was conducted to see the effectiveness of ETV compared with the VPS surgery in the management of obstructive hydrocephalus.
Methodology
This study was designed as single-blind, parallel, randomized controlled trial and was conducted at the Department of Neurosurgery at Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh, from April 2009 to September 2010 for 1½ years. CT scan and MRI were used to confirm hydrocephalus. All patients presenting with obstructive hydrocephalus with the obstruction at or distal to the third ventricle and age 6 months and above were included in the study population. Communicating hydrocephalus, previously shunted patient, abnormal ventricular anatomy in imaging, severe systemic diseases, or comorbid diseases such as diabetes mellitus, hypertension, patients with the age <6 months, or postmeningitic hydrocephalus were excluded from this study. All the patients were divided into two groups by simple random sampling method with the computer-generated random number and these were named as Group A who were treated with ETV and Group B who were treated with VPS. ETV group was considered as experimental, and VPS group was considered as control group. Chhabra medium pressure VPS system was used. The rigid endoscope was used for ETV instrument. The early surgical outcome was defined as outcomes within 1 month following surgical interventions. On admission, a detailed history was taken from the patient or from patient's attendants. Preoperative record of head size, the condition of fontanelle, frequency of vomiting, and postoperative records of head size, changes of the fontanelle, frequency of vomiting, postoperative complications, infection, malfunction of shunt and ETV, procedure failure, and mortality were noted carefully. The postoperative outcomes of this study were fontanelle, head size, vomiting, infection, the presence of persisting fever in the absence of other causes, procedure failure, and mortality. Postoperative follow-up period was 30 days. Daily clinical notes were kept and analyzed to find out infection. Temperature chart was maintained daily. Complete blood count was done if the temperature was high. Before commencement of this study, the research protocol was approved by the Ethical Review Committee of the concerned institute, BSMMU. Statistical analyses of the results were obtained using window-based computer software devised with Statistical Packages for Social Sciences (SPSS-22) (IBM Corp, Armonk, NY). Statistical significance was set at P < 0.05, and confidence interval was set at 95% level.
Results
A total number of sixty patients were recruited from which thirty patients were in Group A (ETV group) and the rest thirty patients were in Group B (VPS group). Table 1 shows that the age group 0.6–10 years was predominant, which was 53.3% in Group A and 53.3% in Group B. The mean age was 18.29 ± 19.74 years in Group A and that of Group B was 17.24 ± 18.56 years. The mean age difference was not statistically significant (P > 0.05) between two groups [Table 1].
Table 1.
Age distribution of the study patients (n=60)
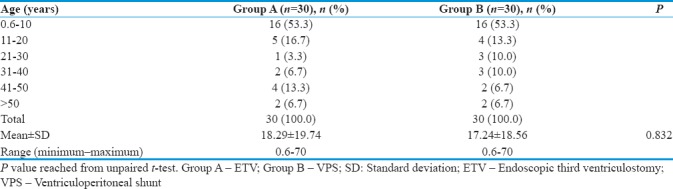
Table 1 shows that the majority of the patients had no complications in both groups, which were 22 (73.3%) and 19 (63.3%) in Group A and Group B, respectively. Complications were observed 8 (26.7%) in Group A and 11 (36.7%) in Group B. Stomal malformation, infection, and shunt malfunction were statistically significant (P < 0.05) between two groups. Others were not statistically significant (P > 0.05); however, subdural hematoma, extradural hematoma, overdrainage, and death were found only in Group B [Table 2].
Table 2.
Distribution of the patients by postoperative complications (n=60)
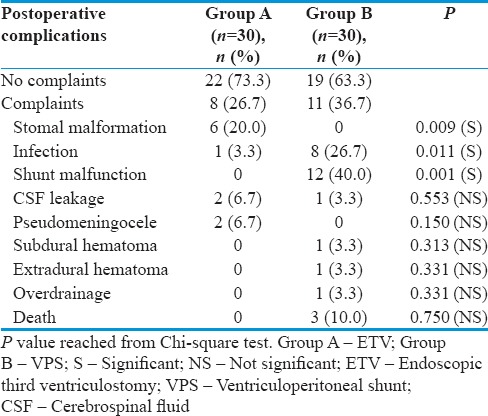
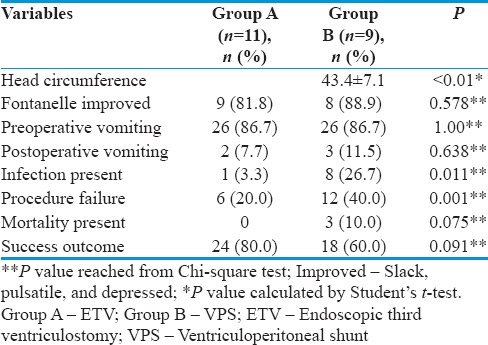
The mean postoperative head circumference was 43.4 ± 7.1 cm and 47.8 ± 5.6 cm in VPS and ETV surgery, respectively (P ≤ 0.01). From Table 2, it is seen that a total of twenty patients having bulged, tense, and nonpulsatile fontanelle underwent CSF diversion procedure by ETV and VPS, out of which 11 in Group A and 9 in Group B. Postoperatively, fontanelle of 9 (81.8%) patients became slack and pulsatile moderately in Group A and 8 (88.9%) in Group B. The difference was not statistically significant (P > 0.05) between two groups. Postoperative vomiting was found in 2 patients (7.7%) and 3 (11.50%) in Group A and Group B, respectively. Postoperative vomiting was improved in 24 patients (92.3%) in Group A and 23 (88.5%) in Group B. The difference was statistically significant (P < 0.05) between two groups. A total of nine patients had developed a postoperative infection, out of which 1 (3.3%) in Group A and 8 (26.7%) in Group B. The difference was statistically significant (P < 0.05) between two groups. The success of the procedure was defined as partial or complete relief of symptoms or no need for further surgery. Failure was defined as no change or deterioration in the clinical condition. Table 2 shows 25 (83.3%) and 12 (40%) success in Group A and Group B, respectively. The difference was statistically significant (P < 0.05) between two groups. Table 2 shows that 3 (10%) patients died in Group B but no patient died in Group A. The difference was not statistically significant (P > 0.05) between two groups regarding the mortality rate. The success of the ETV was defined as partial or complete relief of symptoms. Failure was defined as no change or deterioration in the condition. Table 2 shows that out of all patients in Group A, the success rate was 24 (80%), and in Group B, the success rate was 18 (60%). The difference was not statistically significant (P > 0.05) between two groups in respect to ultimate outcome [Table 3].
Table 3.
Outcome analysis in relation to fontanelle (n=20)
Discussion
The present study comprised sixty patients. They were divided into two groups namely ETV group and VPS group. Thirty patients were in each group of which thirty patients underwent ETV and thirty underwent VPS surgery. The age range was 6 months–70 years. The study of Koch-Wiewrodt and Wagner[10] had shown that failure of ETV occurs more frequently in the first 2–4 months of life. Although controversial, patients <6 months of age have not had good results with ETV, and most authors do not advocate the procedure in this group.
There is a clear impact of age on ETV failure rate even when etiological factors are excluded. And this is why in my study, patients having age <6 months were excluded from the study. The study of El-Ghandour[7] compared the outcome of ETV and VPS in the treatment of obstructive hydrocephalus in 53 cases where Group A (32 patients) was operated by ETV and Group B (21 patients) was operated by VPS surgery. In Group A, intraoperative bleeding occurred in two cases (6.2%) and CSF leakage in one case (3.1%). In Group B, shunt infection occurred in two cases (9.4%), one patient died from ventriculitis, subdural collection occurred in two cases (9.4%), and extradural hematoma occurred in one case (4.7%). Rezaee et al.[11] had shown that mechanical malfunction namely proximal or distal catheter obstruction, disconnection or migration, account for about 60% of the complications followed by infections (1%–40%), overdrainage (10%). In this present study, in group ETV, CSF leakage was noted in 2 (6.67%) cases, pseudo meningocele in 2 (6.67%) cases, stomal malfunction in 5 (17%) cases. In VPS group, CSF leakage was noted in one case, subdural hematoma in one case, extradural hematoma in 1 (3.33%) case, overdrainage in 1 (3.33%) case, and malfunction of the VPS in 12 (40%) cases. Infection was present in nine patients, one (3.33%) in ETV group, and eight (26.7%) in VPS group.
The study of El-Ghandour[7] has shown a lower incidence of procedure failure for ETV (6.2%) than VPS (38%). In my study, regarding procedure failure, ETV failure occurred in six patients (20%) and failure of VPS occurred in 12 patients (40%). Buxton et al.[9] have shown that at 5-year follow-up, failure rate of ETV was 26% as compared to 42% for the VPS group. In the study of El-Ghandour,[7] one patient had died due to ventriculitis following VPS surgery but there was no mortality following ETV. In the present study, three patients died following VPS surgery, two from ventriculitis, and one was due to the subdural hematoma. There was no mortality following ETV.
Feng et al.[3] elucidated that 1 month after ETV, an overall clinical improvement was observed in 45 (77.6%) of 58 patients. Early clinical pictures after the operation play an important role in predicting patient's outcome after ETV. In this study, early surgical outcome following ETV was compared to VPS surgery and follow-up period 30 days. Twenty-four (80%) patients showed clinical improvement after ETV and 18 (60%) patients showed clinical improvement after VPS. Feng et al.[3] had shown that the predictive value of an alternation in ventricle size, especially during the early stage following ETV is unsatisfactory. Therefore, any radio-imaging method has not been used for follow-up purpose.
In the present study, twenty patients had bulged, tense, and pulsatile fontanelle associated with enlarged head size and symptom of vomiting. Of these, 11 underwent ETV and nine underwent VPS surgery. Clinical improvement was satisfactory by both these procedures. However, in the case of VPS surgery, clinical improvement was more rapid than ETV. Early postoperative follow-up records were analyzed in relation to changes in the fontanelle, head size, vomiting, infection rate, procedure failure, and mortality rate. It was seen that significant postoperative changes of fontanelle, head size, and relief of vomiting occurred following both ETV and VPS surgery, but infection rate was 26.67% in VPS group and 3.33% in ETV group. There was 20% procedure failure in ETV group but 40% in VPS group, and three patients died in VPS group but no patient died in ETV group. Therefore, in this perspective, Chi-square test was done, and the P value was calculated which was statistically significant. Hence, in this study, early postoperative outcome following ETV is better than VPS surgery in patients with obstructive hydrocephalus.
Conclusion
Early surgical outcome following ETV is better than VPS surgery in patients with obstructive hydrocephalus. On the basis of the results of the present study, it is highly recommended that a longitudinal study with large sample size should be conducted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Grunert P, Charalampaki P, Hopf N, Filippi R. The role of third ventriculostomy in the management of obstructive hydrocephalus. Minim Invasive Neurosurg. 2003;46:16–21. doi: 10.1055/s-2003-37957. [DOI] [PubMed] [Google Scholar]
- 2.Buxton N, Turner B, Ramli N, Vloeberghs M. Changes in third ventricular size with neuroendoscopic third ventriculostomy: A blinded study. J Neurol Neurosurg Psychiatry. 2002;72:385–7. doi: 10.1136/jnnp.72.3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng H, Huang G, Liao X, Fu K, Tan H, Pu H, et al. Endoscopic third ventriculostomy in the management of obstructive hydrocephalus: An outcome analysis. J Neurosurg. 2004;100:626–33. doi: 10.3171/jns.2004.100.4.0626. [DOI] [PubMed] [Google Scholar]
- 4.Drake JM, Iantosca MR. Cerebrospinal fluid shunting and management of pediatric hydrocephalus. In: Schmidek HH, Roberts DW, editors. Schmidek & Sweet Operative Neurosurgical Techniques: Indications, Methods, and Results. 5th ed. Philadelphia: Saunders Elsevier; 2006. pp. 488–99. [Google Scholar]
- 5.Lindsay KW, Bone I. Neurology, and Neurosurgery Illustrated. 4th ed. London: Churchill Livingstone; 2004. pp. 370–3. [Google Scholar]
- 6.Di Rocco C, Massimi L, Tamburrini G. Shunts vs. endoscopic third ventriculostomy in infants: Are there different types and/or rates of complications? A review. Childs Nerv Syst. 2006;22:1573–89. doi: 10.1007/s00381-006-0194-4. [DOI] [PubMed] [Google Scholar]
- 7.El-Ghandour NM. Endoscopic third ventriculostomy versus ventriculo-peritoneal shunts in the treatment of obstructive hydrocephalus due to posterior fossa tumors in the children. Childs Nerv Syst. 2010;381:1263–5. doi: 10.1007/s00381-010-1263-2. [DOI] [PubMed] [Google Scholar]
- 8.Teo C, Mobbs R. Neuroendoscopy. In: Rengachary SS, Ellenbogen RG, editors. Principles of Neurosurgery. 2nd ed. London: Elsevier Mosby; 2005. pp. 146–7. [Google Scholar]
- 9.Buxton N, Ho KJ, Macarthur D, Vloeberghs M, Punt J, Robertson I. Neuroendoscopic third ventriculostomy for hydrocephalus in adults: Report of a single unit's experience with 63 cases. Surg Neurol. 2001;55:74–8. doi: 10.1016/s0090-3019(01)00352-4. [DOI] [PubMed] [Google Scholar]
- 10.Koch-Wiewrodt D, Wagner W. Success and failure of endoscopic third ventriculostomy in young infants: Are there different age distributions? Childs Nerv Syst. 2006;22:1537–41. doi: 10.1007/s00381-006-0191-7. [DOI] [PubMed] [Google Scholar]
- 11.Rezaee O, Sharifi G, Samadian M, Haddadian K, Ali-Asgari A, Yazdani M. Endoscopic third ventriculostomy for treatment of obstructive hydrocephalus. Arch Iran Med. 2007;10:498–503. [PubMed] [Google Scholar]


