Abstract
Skull base osteomyelitis (SBO) is a complex and fatal clinical entity that is often misdiagnosed for malignancy. SBO is commonly a direct complication of otogenic, sinogenic, odontogenic, and rhinogenic infections and can present as central, atypical, or pediatric clival SBO. This review describes the clinical profile, investigational approach, and management techniques for these variants. A comprehensive literature review was performed in PubMed, MEDLINE, Research Gate, EMBASE, Wiley Online Library, and various Neurosurgical and Neurology journals with the keywords including: SBO, central or atypical SBO, fungal osteomyelitis, malignant otitis externa, temporal bone osteomyelitis, and clival osteomyelitis. Each manuscript's reference list was reviewed for potentially relevant articles. The search yielded a total of 153 articles. It was found that with early and aggressive culture guided long-term intravenous broad-spectrum antibiotic therapy decreases post-infection complications. In cases of widespread soft tissue involvement, an early aggressive surgical removal of infectious sequestra with preferentially Hyperbaric Oxygen (HBO) therapy is associated with better prognosis of disease, less neurologic sequelae and mortality rate. Complete resolution of the SBO cases may take several months. Since early treatment can improve mortality rates, it is paramount that the reporting radiologists and treating clinicians are aware of the cardinal diagnostic signs to improve clinical outcomes of the disease. It will decrease delayed diagnosis and under treatment of the condition. However, due to rarity of the condition, complete prognostic factors have not fully been analyzed and discussed in the literature.
Keywords: Central skull base osteomyelitis, clival osteomyelitis, fungal osteomyelitis, malignant ostitis externa, pediatric osteomyelitis, skull base osteomyelitis, temproal bone osteomyelitis
Introduction
Nelton was the first to introduce the term “osteomyelitis” in 1844; Wilensky, in 1934, endorsed that term.[1,2] A century earlier, John Hunter had already recognized the mechanism of sequestrum formation by describing it as a pocket of dead cortical bone with an abscess.[3] In 1773, William Bromfield described the clinical picture of acute hematogenous osteomyelitis and termed the disease “abcessus in medulla.”[4]
In 1775, cranial osteomyelitis was first explained by surgeon Percival Pott as a collection of pus under the pericranium. Dr. Pott reported cranial osteomyelitis as a consequence of forehead trauma (bone contusion) and extradural hemorrhage.[5] One hundred years later, Lannelongue and Fischer determined that the etiology of inflammation of the skull bones is due to infectious dissemination from neighboring tissues. In 1889, Luc and Tilley reported that cranial osteomyelitis is a complication of paranasal sinusitis.[6,7,8,9] In 1959, Meltzer and Keleman described skull-base osteomyelitis (SBO) in patients with pyocyaneous chondritis and osteomyelitis of the external auditory canal (EAC).[10]
In the past few decades, extensive changes have been made in the clinical course and management of SBO. These changes were attributed to improvements in neurosurgical procedures, diagnostic modalities, and the introduction of new antibiotics and management techniques. Despite these advancements, SBO remains a great challenge, due to its increasing prevalence and high mortality rate.[11,12,13,14,15,16,17,18,19] In this review article, the epidemiology, clinical course, and diagnostic and therapeutic challenges for the management of SBO are examined. The aim of this review is to increase physician awareness of SBO by highlighting its clinical features and diagnostic modalities and emphasizing the potentially devastating complications.
Materials and Methods
A comprehensive search of the published literature was conducted in PubMed, MEDLINE, Wiley Online Library, Research Gate, EMBASE, Science Direct, Elsevier, Cambridge Journals, Cerebral Cortex, SAGE Journals, Oxford Journals, BMC Medicine, International Review of Neuroscience, JAMA Neurology, Journal of Neurosurgery, World Neurosurgery, Surgical Neurology International, Journal of Clinical Neuroscience, Journal of Neurology, Neurosurgery, and Psychiatry, Journal of Neuropathology and Experimental Neurology, European Journal of Neurology, Experimental Neurology, Annals of Neurology, and Journal of the Neurological Sciences. Cross-checking of references led to the identification of additional relevant references. Any controversies or disagreements regarding whether to include or exclude articles or extract data were resolved through discussion and consensus. Keywords for the search included skull base osteomyelitis (SBO), central SBO, fungal osteomyelitis, malignant otitis externa (MOE), temporal bone osteomyelitis, occipital bone osteomyelitis, and clival osteomyelitis. No date restrictions were used. Articles that primarily focused on SBO were included in the study. Articles with high possibility of bias and with blurred/mixed and confusing data were excluded from the study.
Results
A total of 153 articles were shortlisted, based on their relevance to SBO and its different variants [Figure 1]. We reviewed the literature to evaluate the challenges of diagnostic modalities and therapeutic techniques among SBO variants. Due to the rarity of the disease, it is a challenge for physicians to recognize the clinical features of SBO and maintain a high index of suspicion toward the disease. Our review suggests that early and aggressive culture guided long-term intravenous broad-spectrum antibiotic therapy decreases postinfection complications. In the case of widespread soft-tissue involvement, early aggressive surgical removal of infectious sequestra with hyperbaric oxygen (HBO) therapy is associated with better prognosis, fewer neurologic sequelae, and a lower mortality rate. However, treatment may be required for several months before complete resolution. In addition, imaging studies can misinterpret SBO as a malignancy. Therefore, consideration of this diagnosis, both radiologically and clinically, is preferable to biopsy, as biopsy delays treatment.
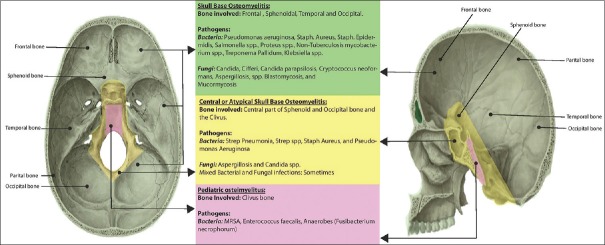
Figure 1.
Skull base osteomyelitis and its variants
Discussion
By definition, osteomyelitis is an inflammatory process of bone, primarily caused by pyogenic organisms, which can either involve just one or multiple parts of a bone, such as the cortex, periosteum, bone marrow, and the surrounding soft tissues.[11] Osteomyelitis can affect any bone of the body, but most commonly the long bones, such as the tibia and fibula.[12,13] Cranial osteomyelitis is a rare clinical entity that can involve either the cranial vault or the base of skull.[12,13]
Epidemiology and risk factors for cranial osteomyelitis
After the development of antibiotics, cranial osteomyelitis became a rare event. However, the use of antibiotics has not resulted in complete eradication of cranial osteomyelitis in developed and underdeveloped nations.[12,13,15] In developing countries with limited access to antibiotics, the most common causes of cranial osteomyelitis are paranasal sinuses, direct head injuries, and scalp infections. In developed nations, postoperative craniotomy infections are the predominant source.[12,18,19,20,21]
In a 10-year retrospective study spanning from 1994 to 2004, 84 cases of osteomyelitis involving the head and neck were observed.[12] Of the 84 cases, 24 required a cranial vault, 20 cases of frontal bone osteomyelitis involved chronic sinusitis, and 4 cases of temporal bone osteomyelitis occurred secondary to MOE.[12] There was a 1.7:1 male-to-female ratio, with an age range of 15–70 years.[12] However, according to two recent studies, the overall incidence rate of cranial osteomyelitis is reportedly higher in developing countries, with Tanzania reporting 12.7% and South Africa reporting 6.7%.[21,23] Furthermore, it is estimated that the incidence of cranial vault tuberculosis ranges from 0.2%–1.3% of all cases of skeletal tuberculosis.[24] The most important risk factor for cranial osteomyelitis with frontal bone involvement is frontal sinusitis, especially in children and adolescents.[14,15,16,17,25,26] In addition to the frontal sinus, any paranasal sinus, such as orbital, oral, or dental, infections impose a significant risk of cranial osteomyelitis.[27,28]
At present, SBO is still a rare event and mainly involves the temporal bone and the sphenoidal bone. SBO commonly occurs as a complication of MOE and chronic mastoid infections or secondary to sphenoidal sinusitis.[29,30,31] MOE primarily affects the temporal bone and is the most frequent cause of SBO.[31] A large study at the University of California Irvine from 1990 to 2000 reported a male-to-female ratio of 1:1 in 820 patients with SBO.[32] The researchers reported the overall incidence of SBO as 69.3% in whites, 13.2% in Native Americans, 6.5% in African Americans, and 2.9% in Asians.[32]
A new, rare clinical entity, central or atypical SBO may begin with otitis externa.[33,34] Central or atypical SBO primarily affects the sphenoidal bone and the occipital bone; the latter is often affected around the clivus bone.[33,32] A review of case study series from 1946 to 2013 revealed 42 cases of central or atypical SBO unrelated to ear infection, with a mean age of 52 years and a male-to-female ratio of 2.2: 1.[35]
Surgical site infections (SSIs) are infections that occur in the wound, secondary to an invasive surgical procedure. Erman et al. estimated that the frequency of SSIs after a clean neurosurgical procedure in randomized controlled trials would be 4.0% to 12.0% without prophylactic antibiotics and 0.3% to 3.0% with prophylactic antibiotics.[36] There are no available data related to prevalence and correlation of specific risk factors with iatrogenic cranial osteomyelitis.[36,37,38] However, procedure-related risk factors were reported as the strongest predictors of SSIs.[37,38] These risk factors often include longer operation time, craniotomy, dural substitute, CSF leak, and staples in wound closure.[37,38,39] Furthermore, prolonged initial hospitalizations and readmissions are significantly associated with SSIs.[37,38,39]
Many cases of cranial osteomyelitis have been reported from posttraumatic injuries secondary to minor scalp wounds such as human bites, scalp wound/laceration, and needle insertions.[19,40,41] Other direct injuries causing cranial osteomyelitis include cephalohematoma infection (particularly after vacuum extraction), craniofacial injuries, penetrating craniocerebral injury, traumatic scalp hematoma, and contaminated war wounds.[42,43,44,45,46,47]
In addition to the above-mentioned etiologic factors, cranial osteomyelitis is influenced by systemic diseases that decrease bone vascularity, the course of illness, and alter the host defense mechanism.[12,22,48,49,50,51,52,53,54,55,56,57,58] The causative infections and predisposing comorbidities are summarized in Table 1.
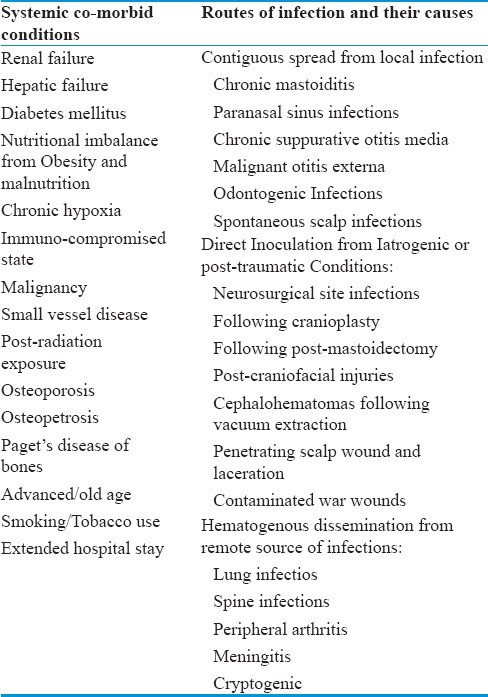
Table 1.
The main routes of infection and systemic comorbid conditions in cranial osteomyelitis
Skull base osteomyelitis and its variants
Examining the pathophysiology and neurological manifestations, along with a reevaluation of diagnostic modalities and therapeutic techniques among different variants of SBO, will allow us to understand the scope of the disease.
Skull base osteomyelitis
Association of skull base osteomyelitis with infections
SBO is an uncommon clinical entity that can lead to significant functional morbidity and mortality.[55,59] Toulmouche was the first to describe progressive osteomyelitis of temporal bone in 1838.[60] In 1959, Meltzer and Keleman described the association of osteomyelitis of EAC and temporal bone with otitis externa caused by Pseudomonas aeruginosa in a patient with poorly controlled diabetes mellitus.[10] In 1968, Chandler introduced the term “MOE,” along with a comprehensive description of a case series from 1968 to 1974.[16,61]
Many studies in the past few decades have represented MOE secondary to P. aeruginosa infection as a leading cause of SBO.[12,62] In 90%–98% of SBO cases, P. aeruginosa is the main cause.[62] Other infections causing SBO include paranasal sinusitis, chronic mastoiditis, suppurative otitis media, and odontogenic infections.[63,64] Bacteremia or fungemia may also be responsible for SBO, typically in immunocompromised patients, such as those who have prolonged neutropenia, leukemia, corticosteroid use, critical illness in Intensive Care Unit, undergone chemotherapy, acquired immunodeficiency syndrome, and diabetes mellitus.[65]
Other bacteria have been known to cause SBO in both immunocompetent and immunosuppressed individuals. These bacteria include Staphylococcus aureus, Staphylococcus epidermidis, Salmonella spp., Proteus spp., nontuberculous Mycobacterium spp., Treponema pallidum, and Klebsiella spp.[9,66,67,68,69] Fungi, such as Candida ciferri, Candida parapsilosis, Cryptococcus neoformans, Aspergillus spp., Blastomycosis, and Mucormycosis, can also cause SBO.[9,66,67,68,69] Aspergillus is the most common fungal cause of SBO in both immunosuppressed and immunocompetent patients.[70]
SBO commonly involves the temporal bone at the base of the skull.[70] Mucormycosis is another common fungus known to infiltrate the sinonasal, orbital, and deep facial soft tissues before involving the head bones.[71,72] These infections can occur through the hematogenous or contiguous spread of sinus and ear infections, or by direct inoculation through trauma or surgery.[69,70,71,73,74,75,76] A very high index of suspicion and recognition of clinical features of each organism are required for the early diagnosis and the aggressive treatment of these conditions.
Pathophysiology
Despite new investigational modalities and multiple research studies, the exact pathogenesis of SBO is unknown. Most cases have been reported in elderly diabetic or immunocompromised patients. These conditions may produce an alkaline pH in the cerumen, diminished immune response (impaired phagocytosis, poor leukocytic response, and impaired intracellular digestion of bacteria), hypoperfusion, and microangiopathy, which predispose the patient to SBO.[77] Water irrigation for cerumen disimpaction is another implicating event that increases the susceptibility to Pseudomonas infection in elderly diabetic patients by making the ear wax less acidic with lower lysozyme contents.[61] MOE can spread from the EAC to the skull base through the fissures of Santorini and the osseocartilaginous junction of the EAC.[78,79] This progressive spread of infection to the skull base foramina may lead to cranial neuropathies, along with the involvement of the parotid gland and temporomandibular joint if spread to the anterior portion of the skull base.[78,79,80,81] The inferomedial spread leads to the participation of the carotid artery and the jugular bulb. The posterior spread affects the sigmoid sinus.[78,79,80,81] In advanced untreated disease, multiple abscesses and pneumatized trabeculated bone may occur.[81] The infection can also spread to the contralateral side and involve the cervical spine.[64]
Clinical features
Prasad et al. characterized SBO into lateral and medial temporal bone osteomyelitis. Lateral temporal involves the mastoid and the middle ear cleft. Medial temporal involves the petrous apex of temporal bone.[82] Lateral temporal bone osteomyelitis is predominantly caused by MOE, acute mastoiditis, and suppurative otitis media, while medial temporal bone osteomyelitis is caused predominantly by MOE and also by sphenoid sinusitis and skull base infections.[82] The bones involved in SBO include the temporal bone, sphenoid bone, occipital bone, and sometimes the frontal bones.[33,82,83,84,85] SBO typically presents with severe and profound otalgia due to the involvement of temporal, parietal, postauricular and retro-orbital areas, spiking a fever, aural fullness, and foul purulent otorrhea.[86] In some patients, SBO shows atypical presentation with unremitting headaches in the absence of localized ear and sinus infection and usually poses a diagnostic challenge. The infection can lead to early cranial neuropathies, commonly abducens palsy, due to the extension of the infectious process to the brainstem, if not treated or diagnosed promptly.[59]
Patients with MOE usually complain of otalgia that is out of proportion and is also worse at night. Other symptoms include conductive deafness, headache, and temporomandibular joint pain.[79] The cardinal signs on examination include woody induration of pinna, preauricular cellulitis, and tender EAC with granulation tissue.[79,86,87] The involvement of the mastoid bone with granulation tissue and cutaneous fistula may occur at late stages of infection.[79,86] The diagnostic criteria set forth by Cohen and Friedman include pain, exudates, edema, and granulation tissue of EAC and positive technetium 99 m (Tc99 m) scan.[87] However, presentation of SBO with frontal bone involvement can include fever, frontal headache, frontal edema, retro-orbital pain, photophobia, purulent rhinorrhea, seizures, and focal neurological signs.[12,87,88,89,90,91] Undiagnosed SBO with frontal lobe involvement is characterized by progressive frontal headaches with decreased mentation, sinocutaneous fistulas, and infectious complications, such as meningitis and extradural, subdural or intraparenchymal abscess, with significant morbidity and mortality.[87,89,90,91]
Cranial nerve involvement commonly occurs in SBO as the disease progresses. The facial nerve is the most common and first cranial nerve involved when the infection spreads subtemporally at the stylomastoid foramen.[34,78] With further posteromedial spread, cranial nerves IX, X, and XI may be affected, with jugular foramen involvement.[78] Cranial nerves V and VI are affected when the petrous apex is involved.[78] Despite complete treatment, the facial nerve does not always recover and should not be used as an indicator of clinical improvement, whereas the other cranial nerves have good rates of recovery.[34,78] Early and aggressive antibiotic therapy has been shown to decrease the incidence of cranial nerve palsy.[34,78] Untreated SBO may lead to meningitis, brain parenchymal involvement, abscess formation (intracranial empyema), and venous sinus thrombosis.[34] These complications are commonly fatal and reflect the severity of the disease.
Investigational modalities
Diagnosis of SBO can be based on particular findings of the history, physical examination, the laboratory results, radiological evidence of infection, and isolation and identification of pathogens at the site of infection. In suspected individuals, every effort should be made for early diagnosis to prevent central nervous system complications. Laboratory investigations usually illustrate a mild elevation of erythrocyte sedimentation rate (ESR), C-reactive protein, and leukocyte counts.[91] In some cases, biopsy with histopathology and microbiology are necessary to rule out malignant disease.[35,62] Repeated biopsy and cultures may be required in those cases in which the first culture result is negative or to rule out an occult malignancy in patients who have persistent disease despite the appropriate antibiotic therapy.[35,79] For fungal pathogens, silver stain on histological sections may identify organisms.[35,79]
Imaging studies are generally used for early diagnosis and to establish the location and extension of infection. These imaging modalities include computed tomography (CT), magnetic resonance imaging (MRI), gallium-67 scintigraphy, Indium-111 (In-111) white blood cell (WBC) scan, and Tc99 m MDP bone single-photon emission CT (SPECT) scintigraphy.[93,94,95,96] Although the CT scan is sensitive to bone erosion or periosteal remodeling, it is a poor choice for SBO to represent an intracranial extension, bone marrow involvement, and to measure treatment response.[93,94] Bone SPECT scintigraphy and MRI are superior to CT scans for detecting early SBO.[93,94] MRI is also more sensitive in determining the extent of the disease.[93,95] Tc99 m methylene diphosphonate (MDP) bone scintigraphy lacks specificity to correlate with the increased osteoblastic activity seen in inflammatory, neoplastic, and postsurgical conditions.[97] In-111 WBC bone scintigraphy is useful for the anatomic localization of lesions, especially in the skull base,[98,99] and can be used to assess for active SBO after treatment.[98,99,100] Studies have shown that MRI, In-111, and WBC bone SPECT are the most sensitive techniques for detecting SBO in patients with previous skull base surgery.[93,94,95] Gallium-67 citrate scintigraphy and ESR titer can assess treatment response and evaluate recurrence and prognosis, as both of these markers rapidly revert to normal with disease resolution.[64,96,97]
Strumas et al. studied a method for multimodality image registration (fused standard CT and SPECT images) for the accurate localization of osteomyelitis in clinically challenging patients.[100] The researchers identified that the fused multimodality image technique guides the need for surgical management and limits unnecessary dissection and excessive debridement.[100] In recent years, imaging modalities have gained importance in early diagnosis. It is important that the reporting radiologist and physician are aware of detecting early improvements on radiologic images. Sometimes, these changes significantly lag behind a satisfactory clinical improvement and lead to premature discontinuation of antibiotic therapy, causing refractory and chronic osteomyelitis.[101]
Treatment techniques
The mainstay treatment for SBO includes a course of culture-guided long-term intravenous broad-spectrum antibiotic therapy.[102] In cases of widespread soft-tissue involvement, early aggressive surgical removal of infectious sequestra is required.[102] With early treatment, SBO can take several months before a complete resolution is achieved.[82,85,102,103] Early intervention can lead to a better prognosis, fewer neurologic sequelae, and a lower mortality rate.[82,85,102,103] Strict glycemic control in diabetic patients and improvements in the immune status of immunocompromised patients also play vital roles in the successful resolution of SBO.[82,85,102,103]
For bacterial or fungal SBO, 3–6 months of culture-directed antimicrobial therapy remains a general protocol.[58,82,85,102,103] For bacterial SBO, these antimicrobial therapies include aminoglycoside and a β-lactamase antibiotic, a third-generation cephalosporin, or an oral quinolone ciprofloxacin.[5,82,85,102,103] For fungal SBO, the use of high-dose amphotericin B is recommended.[58] However, the alternative treatment for fungal SBO includes liposomal amphotericin B, a new lipid formulation with lower toxicity, and equal efficacy to amphotericin B.[58]
Tissue hypoperfusion and hypoxia may lead to treatment failures in both bacterial and fungal SBO.[82,104] In these cases, HBO therapy is a recent treatment technique that improves tissue oxygen contents and host defenses.[21,104,105] It leads to increased oxygen tension at the site of infection, enhances the oxidative killing of pathogens, and promotes angioneogenesis and osteoneogenesis.[21,104,105] HBO therapy is a useful adjunct to antibiotics and surgical therapies and plays a vital role in the management of chronic, refractory SBO. Daily HBO therapy for several weeks is recommended. The reported side effects are oxygen toxicity, barotrauma, and tympanic membrane perforation.[104]
In terms of surgical treatment, there are various standard skull base approaches available for the removal of involved bones. These techniques require special care for the type of procedure and the appropriate timing of surgery. Although early aggressive treatment could result in a deforming procedure that might not be required, delayed treatment of progressive disease may lead to unnecessary morbidity and mortality.[83,101] Surgical procedures may involve debridement of necrotic tissue, bone biopsy and culture, handling of the dead space after surgery, and when required, bone stabilization.[85,87,88,89,102,103] With MOE, the EAC may need local debridement of granulation tissue and bone sequestration; in some cases, if disease extensively involves EAC, extensive meatoplasty is required.[81] Due to the variety of antibiotics available, the role of surgery is often limited to biopsy and drainage of associated abscesses. However, aggressive surgical debridement is recommended in fungal SBO.[77,106] Prompt, appropriate treatment leads to normalization of neurological deficits, early resolution of associated symptoms, and improvements on radiographic imaging.[77,78,85,87,90,91,92,102,103,106]
The management of SBO in immunosuppressed patients requires a multidimensional approach. This approach includes wide surgical debridement with prolonged parenteral antimicrobial therapy and HBO therapy in refractory and chronic patients. Management of SBO also requires control of underlying comorbid factors such as aggressive glycemic control in diabetes and improvements in immune status in immunocompromised patients.[15,107,108,109,110] Treatment in immunosuppressed patients includes intravenous administration of a combination of antimicrobial therapies such as ciprofloxacin and ceftazidime.[111,112]
Data suggested that the intravenous administration of a combination of antimicrobial agents has better mortality benefits than does the single agent used in the treatment of Pseudomonas bacteremia in AIDS patients.[112] However, third-generation cephalosporins and quinolones are also the drugs of choice in the treatment of bacterial infections in immunosuppressed patients.[113] Despite its systemic toxicity, amphotericin B is the treatment of choice for fungal SBO in immunosuppressed patients.[109] To lower the toxicity without sacrificing efficacy of amphotericin B, a new lipid formation, liposomal amphotericin B, and gamma interferon are new alternative options.[109,114] Given the rarity of fungal SBO, clinical suspicion should be high after a failure of antibacterial therapy in patients who have classic signs and symptoms with negative cultures, or in patients who initially responded to antimicrobial therapy, but later experienced recrudescence.[88]
Central or atypical skull base osteomyelitis
Recently, researchers have defined central or atypical SBO as conditions unrelated to otologic pathology. At times, central or atypical SBO has been confused with “simple” MOE. In this review, we will focus on central or atypical SBO of otogenic, sinogenic, or rhinogenic origin.
Pathophysiology
Central or atypical SBO is an uncommon condition that is significantly associated with high mortality and morbidity.[64,107] The incidence of pyogenic osteomyelitis has recently increased, especially in the aging population, patients with diabetes, immunocompromised patients, and intravenous drug abusers.[33,64,107,115,116,117,118] Delayed diagnosis, undertreatment, nonresponsiveness to antimicrobial therapy, and anaerobic infections in immunocompromised patients are significantly associated with central or atypical SBO. Partial or undertreatment of central or atypical SBO is also responsible for relapses; however, bilateral or contralateral SBO is very rare.[64,87,119,120,121]
Central or atypical SBO involves the sphenoid bone and occipital bone; the latter is often affected around the clivus bone [Figures 2 and 3]. The clivus forms a shallow depression and is located between the foramen magnum and dorsum sellae. It is the synchondrosis that later ossifies anteriorly to form the basisphenoid and the basil occiput, posteriorly.[122] This part neighbors with the prevertebral space and becomes connected to vertebral bodies, disc spaces, and the epidural space of the cervical and upper thoracic spine.[123] The prevertebral space is a compartment that spreads from the clival epidural space to the fourth thoracic vertebra and links the base of skull with the posterior mediastinum.[124]
Figure 2.
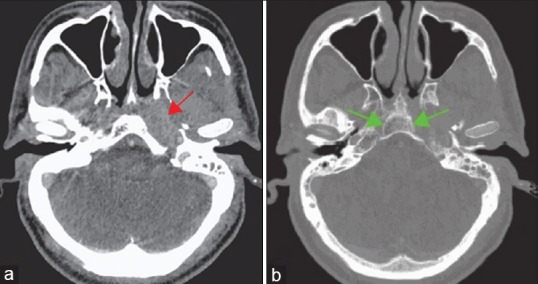
Axial computed tomography images following intravenous contrast administration (a) Soft-tissue window settings demonstrate the fullness of the posterior nasal space and posterior nasopharynx with abnormal soft tissue along the course of the Eustachian tube (red arrow). (b) Bone window settings demonstrate opacification of mastoid air cells on the left with erosive bone loss involving the inferior petrous bone. Loss of clarity of the cortical outline of the basisphenoid (green arrows) and the proximity to the carotid vessel can be noted
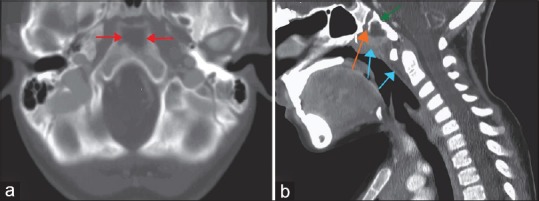
Figure 3.
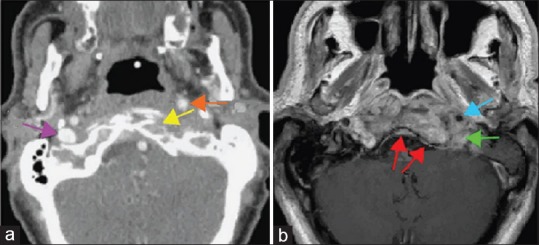
(a) Contrast-enhanced computed tomography of the skull base shows erosion of the anterior cortex of the left occipital condyle (yellow arrows), anterior displacement of the left internal carotid artery (orange arrow). A normal right internal jugular vein is visible (purple arrow), whereas the left internal jugular vein is completely occluded. (b) Magnetic resonance imaging of the skull base shows pathological contrast enhancement in the clivus extending into the soft tissues surrounding the left internal carotid artery (blue arrow) and jugular foramen (green arrow). There is thickening and enhancement of the clival dura (red arrows)
Pathologically, central or atypical SBO usually occurs due to direct spread of an infectious process involving the paranasal sinuses, EAC, mastoid, middle ear, or oral cavity. This infection has also been reported independently, without any history of infection. Those noninfectious causes are infrequent and can occur secondary to trauma or illness.[64,115,116,117] Numerous pathogens, such as Streptococcus, Pneumonia, Pseudomonas, Streptococcus spp., S. aureus, and less commonly, fungal or mixed bacterial infections, have been recognized.[123,124,125] Aspergillus and Candida are reportedly the most common fungal pathogens for central or atypical SBO.[58] The exact pathophysiology of central or atypical SBO involving the clivus remains poorly understood. In addition, there is much controversy surrounding the etiology and management of central or atypical SBO and its complications.
Clinical features
The clinical presentation of central or atypical SBO differs from patient to patient, depending on the involvement of structures and the extent of the disease. If the lesion extends superiorly into the sphenoid bone, it can lead to the erosion of floor of the sella turcica, with extension into the cavernous sinus. Headaches, atypical facial pain, and cranial nerve palsies are the common signs and symptoms at the time of initial presentation.[35,64] Conversely, an inferior extension of the lesion can involve the prevertebral region Occipito-atlantoaxial junction up to the fourth cervical vertebrae. Persistent fever, neck pain, focal pain, and tenderness in the suboccipital area may also be present. In later stages, central or atypical SBO might lead to hemiplegia and quadriparesis, dyspnea, and apnea with the inferior extension of the lesion.[64,125,126,127] Extensive disease may lead to serious complications including dural sinus thrombosis, such as thrombosis of sigmoid sinus, cavernous sinus and internal jugular vein, jugular foramen syndrome, meningitis, brain abscess, or cervical epidural abscess [Figure 3a].[35,64,123,124,125,126,127,128,129]
In contrast to the neurology literature recommendations toward anticoagulation therapy for sigmoid sinus thrombosis due to neoplasm, hypercoagulable state, trauma, or autoimmune disorder,[130,131,132,133] most otolaryngology recommendations suggest avoiding anticoagulation, especially when there is a lack of specific neurological findings.[134] In this antibiotic era, complications associated with central or atypical SBO are relatively rare; however, their presentations are subtle and require a very high index of suspicion. Furthermore, valid data on the etiology and the management of these complications are lacking.[35,64,123,124,125,126,127,128,129]
Investigational modalities
Diagnostic modalities include laboratory work, tissue sampling, and imaging studies. Occasionally, central or atypical SBO does not manifest the characteristic signs of infection, i.e., fever, leukocytosis, elevated ESR, and positive blood cultures.[127] In such cases, tissue sampling is often required for conclusive diagnosis because imaging studies are nonspecific for central or atypical SBO.[33] Tissue sampling can be done by CT-guided fine-needle aspiration, endoscopic sphenoidotomy, or open craniotomy.[33] Due to the low-grade chronic infection with less pathogen burden within the clival bone or preclival soft tissues, biopsies can yield false-negative results. Under those conditions, MR-guided biopsy may be useful.[135]
Imaging studies of central or atypical SBO in the setting of widespread disease are best accomplished with MRI, which has an advantage over CT scan. MRI is best for evaluating the extent of soft-tissue changes and assessing the bone marrow. It is also useful for the detection of osteomyelitis, particularly, at the skull base.[136] Clival marrow and preclival soft-tissue abnormalities are the customary findings on MRI studies [Figure 3b]. It is poorly understood whether these changes in preclival soft tissue are due to direct extension of an infection from the sphenoid sinus or the extension from the clivus itself.[33,136,137] Numerous granulomatous diseases and other inflammatory conditions, such as Wegener granulomatosis, tuberculosis, sarcoidosis, fibrous dysplasia, and Paget's disease of bone, may mimic the findings of central or atypical SBO on imaging studies and must also be ruled out before an accurate diagnosis is made.[33,64]
Treatment techniques
The management of central or atypical SBO entails long-term antimicrobial therapy. Debridement may be required in a significant group of patients. In recently diagnosed central or atypical SBO cases, 6–20 weeks of broad-spectrum antimicrobial agents are recommended.[35,57,95] Johnson and Batra estimated that approximately 55% of patients required aggressive parenteral antimicrobial agents over a mean period of 6.9 weeks.[35] Although diabetes increases susceptibility to infection and causes microangiopathy, there is no evidence of an association between diabetes and longer duration of antimicrobial therapy.[35] Given the high vulnerability to polymicrobial infection, multiple broad-spectrum antimicrobial therapies should be started as soon as possible, until the microbiology and histopathology studies become available. Due to the high prevalence of P. aeruginosa, double coverage is required.
Earlier, intravenous antipseudomonal penicillins and aminoglycosides were commonly used.[93] However, recent data establish carbapenems and ciprofloxacin as appropriate adjunctive therapy.[138] Empiric therapy with vancomycin is required for adequate Methicillin-resistant S. aureus (MRSA) coverage.[35] Johnson and Batra reported that broad-spectrum antifungal coverage must be considered in refractory cases in the setting of appropriate empiric antibiotics. However, empiric antifungal therapy has not been suggested in the literature.[35] HBO therapy has long been suggested to improve treatment and reduce morbidity and mortality.[56,139] However, several discrepancies have been reported due to the limited amount of analyzable data; future studies are needed to overcome current limitations.[56,139]
There are several arguments regarding the role of surgical management in central or atypical SBO. The available literature has not demonstrated the effectiveness of surgery or the required duration of antimicrobial treatment.[138,139,140] The aggressive surgical debridement of affected tissues may still be considered as an important adjunctive therapy for the treatment of central or atypical SBO.[138,139,140] The local debridement of devitalized tissues will help to decrease the infectious and inflammatory load while improving the availability of antimicrobial agents to the affected region. However, concrete guidelines for surgical treatment are not available.[35]
Pediatric clival osteomyelitis
Clival osteomyelitis is a very rare condition that affects children [Figure 4]. The clivus is usually involved in many pathogenic processes such as primary or metastatic neoplasm and vascular and infectious diseases.[137,141] Studies have shown that this condition generally occurs secondary to the direct spread of an infection from contiguous structures, involving the paranasal sinuses, or the adjacent bones of the base of skull, especially the posterior ethmoid and sphenoid bones.[30,142,143] There are little data to determine the origin of the infectious process.
Figure 4.
A contrast-enhanced computed tomography scan (a) axial and (b) sagittal views in a child with pediatric clival osteomyelitis demonstrates destruction within the anterior aspect of the clivus bone (red and green arrows in a and b) posterior to the spheno-occipital synchondrosis (orange arrow) associated with anterior soft-tissue prominence extending close to the cephalic most portion of the adenoids along with some prevertebral soft-tissue thickening (blue arrows)
Some case studies have reported a link between clival osteomyelitis and different pathogens, such as Enterococcus faecium and MRSA, and an anaerobe, Fusobacterium necrophorum.[30,142,143,144] Recently, researchers proposed that this infection could be spread through the fossa navicularis magna from the lymphatic tissue in the pharynx to the skull base, usually in patients with retropharyngeal abscess.[143,145,146] The lymphoid tissue of the pharyngeal tonsil and the presence of emissary veins in the fossa navicularis functioned as a potential route of infection spread and led to clival osteomyelitis.[143,145,146] Rusconi et al. reported clival osteomyelitis in adult patients, in addition to children.[142]
Due to the presence of several important adjacent structures, including the cranial nerves, cavernous sinus, internal carotid artery, and dura, any disease progression can lead to intracranial complications.[147,148] The most frequent complication is abducens nerve palsy in the clivus and/or paraclival pathology.[149] Contrast-enhanced imaging studies, such MRI and CT scans, are essential to evaluate the extent of the disease process.[142,143,146]
Treatment of clival osteomyelitis consists of intravenous administration of broad-spectrum antibiotic therapy over a period of 4–8 weeks, and surgical drainage through the posterior pharyngeal wall in those patients who are unresponsive to antibiotic therapy.[25,142,143,146] Together with clival osteomyelitis, the differential diagnoses for bone destruction in the pediatric population are clival chordoma, Langerhans cell histiocytosis, and small round blue cell tumors such as Ewing sarcoma or primitive neuroectodermal tumor, rhabdomyosarcoma, metastatic neuroblastoma, and lymphoma.[143,150,151,152]
Long-term prognosis of skull base osteomyelitis
Due to the rarity of SBO, it is difficult to recognize the potential epidemiological variables and the major trends of the disease. Johnson and Batra reported an overall survival rate of 90.5% at a mean 18-month follow-up.[35] In previous studies, 3-year survival rates for MOE were reported at 57%.[55] Prognosis is poor in diabetic patients, with survival rates ranging from 21% to 70%.[153] The reported overall mortality rate reaches 10%; in addition, long-term neurologic sequelae are reported in 31% of cases, despite aggressive treatment.[33] Considering the extent and aggression of the disease process, the overall survival rate indicates that advances in diagnostic procedures with aggressive antibiotic treatment and careful surgical interventions may reduce SBO-related mortality.[140] However, the prognostic factors have not been explored fully.
Conclusion
In this review, we focused on SBO and its variants, central or atypical SBO and pediatric clival osteomyelitis. SBO is a life-threatening complication that can be misdiagnosed for malignancy. However, there was no single pathognomonic feature of SBO revealed in the literature. Our review highlights several important aspects of this complication, with major implications for diagnosis and treatment. SBO can occur in elderly patients with diabetes mellitus or immunosuppression, and there are many predisposing factors. This condition often results from an ear infection with either acute or chronic presentation. Atypical SBO can be present without any sign of infection. Diagnosis can be based on a combination of clinical findings, history, imaging, microbiology, and histology. We recommend the early and aggressive use of long-term intravenous broad-spectrum antibiotic treatment for several months, along with HBO therapy and conservative surgical therapy, which seem to improve clinical outcome. Although this condition is rare, reporting radiologists and treating clinicians must be aware of the radiological findings to decrease delayed diagnosis and undertreatment of the condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nelaton A. Elements of Surgical Pathology. Vol. 586. Paris: Germer Bailliere; 1844. pp. 595–7. [Google Scholar]
- 2.Wilensky AO. Osteomyelitis; its Pathogenesis, Symptomatology and Treatment. New York: Macmillan Company; 1934. [Google Scholar]
- 3.Hunter J. Lectures on the principles of surgery. In: Palmer JF, editor. The Works of John Hunter FRS. Vol. 1. London: Longman, Rees, Orme, Brown, Green and Longman; 1835. [Google Scholar]
- 4.Bromfield W. Chirurgical Observations and Cases. II. London: T. Cadall; 1773. pp. 19–24. [Google Scholar]
- 5.Pott P. London: L Hawes, W Clarke, R Collins; 1768. Observations on the Nature and Consequences of Those Injuries to Which the Head Is Liable from External Violence. [Google Scholar]
- 6.Lannelongue OM. Acute osteomyelitis during growth. Paris: Asselin and Cie; 1879. [Google Scholar]
- 7.Fischer H. Die osteomyelitis traumatica purulenta cranii. Deut Zeit Chir. 1900;56:449–72. [Google Scholar]
- 8.Luc H. Paris: Masson & Cie; 1902. Killian's method for the radical cure of chronic frontal empyema. Annals of Ear Diseases, Larynx, Nezet of the Pharynx. [Google Scholar]
- 9.Tilley H. Remarks on the operative treatment of a case of double frontal sinus empyema, complicated by double antral suppuration. Br Med J. 1897;1:197–9. doi: 10.1136/bmj.1.1882.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meltzer PE, Kelemen G. Pyocyaneous osteomyelitis of the temporal bone, mandible and zygoma. Laryngoscope. 1959;69:1300–16. [Google Scholar]
- 11.Waldvogel FA, Medoff G, Swartz MN. Osteomyelitis: A review of clinical features, therapeutic considerations and unusual aspects 3. Osteomyelitis associated with vascular insufficiency. N Engl J Med. 1970;282:316–22. doi: 10.1056/NEJM197002052820606. [DOI] [PubMed] [Google Scholar]
- 12.Prasad KC, Prasad SC, Mouli N, Agarwal S. Osteomyelitis in the head and neck. Acta Otolaryngol. 2007;127:194–205. doi: 10.1080/00016480600818054. [DOI] [PubMed] [Google Scholar]
- 13.Peltola H, Paakkonen M. Acute osteomyelitis in children. N Engl J Med. 2014;370:352–60. doi: 10.1056/NEJMra1213956. [DOI] [PubMed] [Google Scholar]
- 14.Amedee RG, Mann WJ. Osteomyelitis of the skull base – An unusual manifestation. Am J Otol. 1989;10:402–4. [PubMed] [Google Scholar]
- 15.Balm AJ, Tiwari RM, de Rijcke TB. Osteomyelitis in the head and neck. J Laryngol Otol. 1985;99:1059–65. doi: 10.1017/s0022215100098182. [DOI] [PubMed] [Google Scholar]
- 16.Chandler JR. Malignant external otitis and osteomyelitis of the base of the skull. Am J Otol. 1989;10:108–10. [PubMed] [Google Scholar]
- 17.Chandler JR, Grobman L, Quencer R, Serafini A. Osteomyelitis of the base of the skull. Laryngoscope. 1986;96:245–51. doi: 10.1288/00005537-198603000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Nisbet M, Briggs S, Ellis-Pegler R, Thomas M, Holland D. Propionibacterium acnes: An under-appreciated cause of post-neurosurgical infection. J Antimicrob Chemother. 2007;60:1097–103. doi: 10.1093/jac/dkm351. [DOI] [PubMed] [Google Scholar]
- 19.Mortazavi MM, Khan MA, Quadri SA, Suriya SS, Fahimdanesh KM, et al. Cranial Osteomyelitis: A Comprehensive Review of Modern Therapies. World Neurosurg. 2017 doi: 10.1016/j.wneu.2017.12.066. pii: S1878-8750(17)32182-4. [DOI] [PubMed] [Google Scholar]
- 20.Phillips NI, Robertson IJ. Osteomyelitis of the skull vault from a human bite. Br J Neurosurg. 1997;11:168–9. doi: 10.1080/02688699746582. [DOI] [PubMed] [Google Scholar]
- 21.Larsson A, Engström M, Uusijärvi J, Kihlström L, Lind F, Mathiesen T, et al. Hyperbaric oxygen treatment of postoperative neurosurgical infections. Neurosurgery. 2002;50:287–95. [PubMed] [Google Scholar]
- 22.Ali AM, Maya E, Lakhoo K. Challenges in managing pediatric osteomyelitis in the developing world: Analysis of cases presenting to a tertiary referral centre in Tanzania. Afr J Paediatr Surg. 2014;11:308–11. doi: 10.4103/0189-6725.143136. [DOI] [PubMed] [Google Scholar]
- 23.Nathoo N, Nadvi SS, Gouws E, van Dellen JR. Craniotomy improves outcomes for cranial subdural empyemas: Computed tomography-era experience with 699 patients. Neurosurgery. 2001;49:872–7. doi: 10.1097/00006123-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Patankar T, Varma R, Krishnan A, Prasad S, Desai K, Castillo M, et al. Radiographic findings in tuberculosis of the calvarium. Neuroradiology. 2000;42:518–21. doi: 10.1007/s002340000317. [DOI] [PubMed] [Google Scholar]
- 25.Gallagher RM, Gross CW, Phillips CD. Suppurative intracranial complications of sinusitis. Laryngoscope. 1998;108:1635–42. doi: 10.1097/00005537-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Bambakidis NC, Cohen AR. Intracranial complications of frontal sinusitis in children: Pott's puffy tumor revisited. Pediatr Neurosurg. 2001;35:82–9. doi: 10.1159/000050395. [DOI] [PubMed] [Google Scholar]
- 27.Clayman GL, Adams GL, Paugh DR, Koopmann CF., Jr Intracranial complications of paranasal sinusitis: A combined institutional review. Laryngoscope. 1991;101:234–9. doi: 10.1288/00005537-199103000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Adams JR, Bryant DG. Cranial osteomyelitis: A late complication of a dental infection. Br J Oral Maxillofac Surg. 2008;46:673–4. doi: 10.1016/j.bjoms.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 29.Niv A, Nash M, Slovik Y, Fliss DM, Kaplan D, Leibovitz E, et al. Acute mastoiditis in infancy: The Soroka experience: 1990-2000. Int J Pediatr Otorhinolaryngol. 2004;68:1435–9. doi: 10.1016/j.ijporl.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 30.Laurens MB, Becker RM, Johnson JK, Wolf JS, Kotloff KL. MRSA with progression from otitis media and sphenoid sinusitis to clival osteomyelitis, pachymeningitis and abducens nerve palsy in an immunocompetent 10-year-old patient. Int J Pediatr Otorhinolaryngol. 2008;72:945–51. doi: 10.1016/j.ijporl.2008.02.025. [DOI] [PubMed] [Google Scholar]
- 31.Chen JC, Yeh CF, Shiao AS, Tu TY. Temporal bone osteomyelitis: The relationship with malignant otitis externa, the diagnostic dilemma, and changing trends. Scientific World Journal 2014. 2014:591714. doi: 10.1155/2014/591714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rothholtz VS, Lee AD, Shamloo B, Bazargan M, Pan D, Djalilian HR, et al. Skull base osteomyelitis: The effect of comorbid disease on hospitalization. Laryngoscope. 2008;118:1917–24. doi: 10.1097/MLG.0b013e31817fae0d. [DOI] [PubMed] [Google Scholar]
- 33.Chang PC, Fischbein NJ, Holliday RA. Central skull base osteomyelitis in patients without otitis externa: Imaging findings. AJNR Am J Neuroradiol. 2003;24:1310–6. [PMC free article] [PubMed] [Google Scholar]
- 34.Adams A, Offiah C. Central skull base osteomyelitis as a complication of necrotizing otitis externa: Imaging findings, complications, and challenges of diagnosis. Clin Radiol. 2012;67:e7–16. doi: 10.1016/j.crad.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Johnson AK, Batra PS. Central skull base osteomyelitis: An emerging clinical entity. Laryngoscope. 2014;124:1083–7. doi: 10.1002/lary.24440. [DOI] [PubMed] [Google Scholar]
- 36.Erman T, Demirhindi H, Göçer AI, Tuna M, Ildan F, Boyar B, et al. Risk factors for surgical site infections in neurosurgery patients with antibiotic prophylaxis. Surg Neurol. 2005;63:107–12. doi: 10.1016/j.surneu.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 37.Chiang HY, Kamath AS, Pottinger JM, Greenlee JD, Howard MA, 3rd, Cavanaugh JE, et al. Risk factors and outcomes associated with surgical site infections after craniotomy or craniectomy. J Neurosurg. 2014;120:509–21. doi: 10.3171/2013.9.JNS13843. [DOI] [PubMed] [Google Scholar]
- 38.Abu Hamdeh S, Lytsy B, Ronne-Engström E. Surgical site infections in standard neurosurgery procedures – A study of incidence, impact and potential risk factors. Br J Neurosurg. 2014;28:270–5. doi: 10.3109/02688697.2013.835376. [DOI] [PubMed] [Google Scholar]
- 39.Korinek AM, Golmard JL, Elcheick A, Bismuth R, van Effenterre R, Coriat P, et al. Risk factors for neurosurgical site infections after craniotomy: A critical reappraisal of antibiotic prophylaxis on 4,578 patients. Br J Neurosurg. 2005;19:155–62. doi: 10.1080/02688690500145639. [DOI] [PubMed] [Google Scholar]
- 40.Pickering SA, Ashpole RD, Wallace ME, Paul SH. Osteomyelitis of calvarium after trivial scalp laceration. J Accid Emerg Med. 1998;15:430. doi: 10.1136/emj.15.6.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGregor JA, McFarren T. Neonatal cranial osteomyelitis: A complication of fetal monitoring. Obstet Gynecol. 1989;73:490–2. [PubMed] [Google Scholar]
- 42.Nakwan N, Nakwan N, Wannaro J, Dissaneevate P, Kritsaneepaiboon S, Chokephaibulkit K, et al. Septicemia, meningitis, and skull osteomyelitis complicating infected cephalhematoma caused by ESBL-producing Escherichia coli. Southeast Asian J Trop Med Public Health. 2011;42:148–51. [PubMed] [Google Scholar]
- 43.Metzinger SE, Guerra AB, Garcia RE. Frontal sinus fractures: Management guidelines. Facial Plast Surg. 2005;21:199–206. doi: 10.1055/s-2005-922860. [DOI] [PubMed] [Google Scholar]
- 44.Domingo Z, Peter JC, de Villiers JC. Low-velocity penetrating craniocerebral injury in childhood. Pediatr Neurosurg. 1994;21:45–9. doi: 10.1159/000120813. [DOI] [PubMed] [Google Scholar]
- 45.Valerón-Almazán P, Gómez-Duaso AJ, Rivero P, Vilar J, Dehesa L, Santana N, et al. Extensive, non-healing scalp ulcer associated with trauma-induced chronic osteomyelitis. Ann Dermatol. 2011;23:S364–7. doi: 10.5021/ad.2011.23.S3.S364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Margorin EM. Cranium osteomyelitis following gunshot. Voen Med Zh. 1946;1-2:10–21. [PubMed] [Google Scholar]
- 47.Ramakrishnan V, Dahlin R, Hariri O, Quadri SA, Farr S, Miulli D, et al. Anti-epileptic prophylaxis in traumatic brain injury: A retrospective analysis of patients undergoing craniotomy versus decompressive craniectomy. Surg Neurol Int. 2015;6:8. doi: 10.4103/2152-7806.149613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rerolle JP, Szelag JC, Diaconita M, Paraf F, Aldigier JC, Le Meur Y, et al. Intracranial granuloma and skull osteolysis: Complication of a primary cutaneous cryptococcosis in a kidney transplant recipient. Am J Kidney Dis. 2005;46:e113–7. doi: 10.1053/j.ajkd.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 49.Levitt MR, Benedict WJ, Barton K, Melian E, Gamelli RL, Vandevender D, et al. Management of scalp toxic epidermal necrolysis and cranial osteomyelitis with serratus anterior myocutaneous pedicle flap: A case report. J Burn Care Res. 2007;28:524–9. doi: 10.1097/BCR.0B013E318053DA97. [DOI] [PubMed] [Google Scholar]
- 50.McClelland S, 3rd, Hall WA. Postoperative central nervous system infection: Incidence and associated factors in 2111 neurosurgical procedures. Clin Infect Dis. 2007;45:55–9. doi: 10.1086/518580. [DOI] [PubMed] [Google Scholar]
- 51.Topazian RG. Osteomyelitis of jaws. In: Topazian RG, Goldberg MH, editors. Oral and Maxillofacial Infections. 3rd ed. Philadelphia, PA: Saunders; 1994. pp. 251–86. [Google Scholar]
- 52.Wickenhauser C, Tsironis K, Zirbes TK, Larena-Avellanda A, Dienes HP. Highly differentiated squamous epithelial carcinoma as a late complication of post-traumatic osteomyelitis. Pathologe. 1999;20:236–41. doi: 10.1007/s002920050351. [DOI] [PubMed] [Google Scholar]
- 53.Pincus DJ, Armstrong MB, Thaller SR. Osteomyelitis of the craniofacial skeleton. Semin Plast Surg. 2009;23:73–9. doi: 10.1055/s-0029-1214159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tuon FF, Russo R, Nicodemo AC. Brain abscess secondary to frontal osteomyelitis. Rev Inst Med Trop Sao Paulo. 2006;48:233–5. doi: 10.1590/s0036-46652006000400012. [DOI] [PubMed] [Google Scholar]
- 55.Lee S, Hooper R, Fuller A, Turlakow A, Cousins V, Nouraei R, et al. Otogenic cranial base osteomyelitis: A proposed prognosis-based system for disease classification. Otol Neurotol. 2008;29:666–72. doi: 10.1097/MAO.0b013e318179972f. [DOI] [PubMed] [Google Scholar]
- 56.Stodulski D, Kowalska B, Stankiewicz C. Otogenic skull base osteomyelitis caused by invasive fungal infection. Case report and literature review. Eur Arch Otorhinolaryngol. 2006;263:1070–6. doi: 10.1007/s00405-006-0118-7. [DOI] [PubMed] [Google Scholar]
- 57.Blyth CC, Gomes L, Sorrell TC, da Cruz M, Sud A, Chen SC, et al. Skull-base osteomyelitis: Fungal vs.bacterial infection. Clin Microbiol Infect. 2011;17:306–11. doi: 10.1111/j.1469-0691.2010.03231.x. [DOI] [PubMed] [Google Scholar]
- 58.Hariri OR, Minasian T, Quadri SA, Dyurgerova A, Farr S, Miulli DE, et al. Histoplasmosis with deep CNS involvement: Case presentation with discussion and literature review. J Neurol Surg Rep. 2015;76:e167–72. doi: 10.1055/s-0035-1554932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sreepada GS, Kwartler JA. Skull base osteomyelitis secondary to malignant otitis externa. Curr Opin Otolaryngol Head Neck Surg. 2003;11:316–23. doi: 10.1097/00020840-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 60.Toulmouche MA. Observations on cerebral otorrhea: latest considerations. Gaz Med Paris. 1838;6:422–6. [Google Scholar]
- 61.Chandler JR. Malignant external otitis. Laryngoscope. 1968;78:1257–94. doi: 10.1288/00005537-196808000-00002. [DOI] [PubMed] [Google Scholar]
- 62.Rubin Grandis J, Branstetter BF, 4th, Yu VL. The changing face of malignant (necrotising) external otitis: Clinical, radiological, and anatomic correlations. Lancet Infect Dis. 2004;4:34–9. doi: 10.1016/s1473-3099(03)00858-2. [DOI] [PubMed] [Google Scholar]
- 63.Magliulo G, Varacalli S, Ciofalo A. Osteomyelitis of the skull base with atypical onset and evolution. Ann Otol Rhinol Laryngol. 2000;109:326–30. doi: 10.1177/000348940010900316. [DOI] [PubMed] [Google Scholar]
- 64.Singh A, Al Khabori M, Hyder MJ. Skull base osteomyelitis: Diagnostic and therapeutic challenges in atypical presentation. Otolaryngol Head Neck Surg. 2005;133:121–5. doi: 10.1016/j.otohns.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 65.Auguste KI, McDermott MW. Salvage of infected craniotomy bone flaps with the wash-in, wash-out indwelling antibiotic irrigation system. Technical note and case series of 12 patients. J Neurosurg. 2006;105:640–4. doi: 10.3171/jns.2006.105.4.640. [DOI] [PubMed] [Google Scholar]
- 66.Kountakis SE, Kemper JV, Jr, Chang CY, DiMaio DJ, Stiernberg CM. Osteomyelitis of the base of the skull secondary to aspergillus. Am J Otolaryngol. 1997;18:19–22. doi: 10.1016/s0196-0709(97)90043-0. [DOI] [PubMed] [Google Scholar]
- 67.Mani R, Belcadhi M, Krifa N, Abdelkefi M, Ben Said M, Bouzouita K, et al. Fungal necrotizing external otitis. Ann Otolaryngol Chir Cervicofac. 2008;125:40–5. doi: 10.1016/j.aorl.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 68.Chan LL, Singh S, Jones D, Diaz EM, Jr, Ginsberg LE. Imaging of mucormycosis skull base osteomyelitis. AJNR Am J Neuroradiol. 2000;21:828–31. [PMC free article] [PubMed] [Google Scholar]
- 69.Bruce JN, Bruce SS. Preservation of bone flaps in patients with post craniotomy infections. J Neurosurg. 2003;98:1203–7. doi: 10.3171/jns.2003.98.6.1203. [DOI] [PubMed] [Google Scholar]
- 70.Rinaldi MG. Invasive aspergillosis. Rev Infect Dis. 1983;5:1061–77. doi: 10.1093/clinids/5.6.1061. [DOI] [PubMed] [Google Scholar]
- 71.Bahna MS, Ward PH, Konrad HR. Nasopharyngeal mucormycotic osteitis: A new syndrome characterized by initial presentation of multiple cranial nerve palsies. Otolaryngol Head Neck Surg (1979) 1980;88:146–53. doi: 10.1177/019459988008800209. [DOI] [PubMed] [Google Scholar]
- 72.Finn DG, Farmer JC., Jr Chronic mucormycosis. Laryngoscope. 1982;92:761–6. doi: 10.1288/00005537-198207000-00009. [DOI] [PubMed] [Google Scholar]
- 73.Gordon G, Giddings NA. Invasive otitis externa due to Aspergillus species: Case report and review. Clin Infect Dis. 1994;19:866–70. doi: 10.1093/clinids/19.5.866. [DOI] [PubMed] [Google Scholar]
- 74.Salaki JS, Louria DB, Chmel H. Fungal and yeast infections of the central nervous system. A clinical review. Medicine (Baltimore) 1984;63:108–32. doi: 10.1097/00005792-198403000-00004. [DOI] [PubMed] [Google Scholar]
- 75.Fuchs HA, Evans RM, Gregg CR. Invasive aspergillosis of the sphenoid sinus manifested as a pituitary tumor. South Med J. 1985;78:1365–7. doi: 10.1097/00007611-198511000-00028. [DOI] [PubMed] [Google Scholar]
- 76.Stanley RJ, McCaffrey TV, Weiland LH. Fungal mastoiditis in the immunocompromised host. Arch Otolaryngol Head Neck Surg. 1988;114:198–9. doi: 10.1001/archotol.1988.01860140096030. [DOI] [PubMed] [Google Scholar]
- 77.Alva B, Prasad KC, Prasad SC, Pallavi S. Temporal bone osteomyelitis and temporoparietal abscess secondary to malignant otitis externa. J Laryngol Otol. 2009;123:1288–91. doi: 10.1017/S0022215109005313. [DOI] [PubMed] [Google Scholar]
- 78.Unnikrishnan R, Faizal BP, Pillai MG, Paul G. Villaret's syndrome – A rare presentation of skull base osteomyelitis. Case report. Amrita J Med. 2013;9:1–44. [Google Scholar]
- 79.Carfrae MJ, Kesser BW. Malignant otitis externa. Otolaryngol Clin North Am. 2008;41:537. doi: 10.1016/j.otc.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 80.Holder CD, Gurucharri M, Bartels LJ, Colman MF. Malignant external otitis with optic neuritis. Laryngoscope. 1986;96:1021–3. [PubMed] [Google Scholar]
- 81.Slattery WH, 3rd, Brackmann DE. Skull base osteomyelitis. Malignant external otitis. Otolaryngol Clin North Am. 1996;29:795–806. [PubMed] [Google Scholar]
- 82.Prasad SC, Prasad KC, Kumar A, Thada ND, Rao P, Chalasani S, et al. Osteomyelitis of the temporal bone: Terminology, diagnosis, and management. J Neurol Surg B Skull Base. 2014;75:324–31. doi: 10.1055/s-0034-1372468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Verde RC, De Souza LA, Lessa BF, De Lima CM, Lessa MM, Lessa HA. Clinical and tomography evolution of frontal osteomyelitis: Case report. Int Arch Otorhinolaryngol. 2012;16:130–4. [Google Scholar]
- 84.Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364:369–79. doi: 10.1016/S0140-6736(04)16727-5. [DOI] [PubMed] [Google Scholar]
- 85.Minutilli E, Pompucci A, Anile C, Corina L, Paludetti G, Magistrelli P, et al. Cutaneous fistula is a rare presentation of Pott's puffy tumour. J Plast Reconstr Aesthet Surg. 2008;61:1246–8. doi: 10.1016/j.bjps.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 86.Schweitzer VG. Hyperbaric oxygen management of chronic staphylococcal osteomyelitis of the temporal bone. Am J Otol. 1990;11:347–53. [PubMed] [Google Scholar]
- 87.Marshall AH, Jones NS. Osteomyelitis of the frontal bone secondary to frontal sinusitis. J Laryngol Otol. 2000;114:944–6. doi: 10.1258/0022215001904671. [DOI] [PubMed] [Google Scholar]
- 88.Ducic Y. Management of osteomyelitis of the anterior skull base and craniovertebral junction. Otolaryngol Head Neck Surg. 2003;128:39–42. doi: 10.1067/mhn.2003.9. [DOI] [PubMed] [Google Scholar]
- 89.Bullitt E, Lehman RA. Osteomyelitis of the skull. Surg Neurol. 1979;11:163–6. [PubMed] [Google Scholar]
- 90.Goldberg AN, Oroszlan G, Anderson TD. Complications of frontal sinusitis and their management. Otolaryngol Clin North Am. 2001;34:211–25. doi: 10.1016/s0030-6665(05)70307-8. [DOI] [PubMed] [Google Scholar]
- 91.Guillén A, Brell M, Cardona E, Claramunt E, Costa JM. Potts puffy tumour: Still not an eradicated entity. Childs Nerv Syst. 2001;176:359–62. doi: 10.1007/s003810000420. [DOI] [PubMed] [Google Scholar]
- 92.Masterson L, Leong P. Potts puffy tumour: A forgotten complication of frontal sinus disease. Oral Maxillofac Surg. 2009;13:115–7. doi: 10.1007/s10006-009-0155-7. [DOI] [PubMed] [Google Scholar]
- 93.Seabold JE, Simonson TM, Weber PC, Thompson BH, Harris KG, Rezai K, et al. Cranial osteomyelitis: Diagnosis and follow-up with in-111 white blood cell and tc-99m methylene diphosphonate bone SPECT, CT, and MR imaging. Radiology. 1995;196:779–88. doi: 10.1148/radiology.196.3.7644643. [DOI] [PubMed] [Google Scholar]
- 94.Weber PC, Seabold JE, Graham SM, Hoffmann HH, Simonson TM, Thompson BH, et al. Evaluation of temporal and facial osteomyelitis by simultaneous in-WBC/Tc-99m-MDP bone SPECT scintigraphy and computed tomography scan. Otolaryngol Head Neck Surg. 1995;113:36–41. doi: 10.1016/s0194-5998(95)70142-7. [DOI] [PubMed] [Google Scholar]
- 95.Gherini SG, Brackmann DE, Bradley WG. Magnetic resonance imaging and computerized tomography in malignant external otitis. Laryngoscope. 1986;96:542–8. doi: 10.1288/00005537-198605000-00014. [DOI] [PubMed] [Google Scholar]
- 96.Stokkel MP, Takes RP, van Eck-Smit BL, Baatenburg de Jong RJ. The value of quantitative gallium-67 single-photon emission tomography in the clinical management of malignant external otitis. Eur J Nucl Med. 1997;24:1429–32. doi: 10.1007/s002590050172. [DOI] [PubMed] [Google Scholar]
- 97.Ostfeld E, Aviel A, Pelet D. Malignant external otitis: The diagnostic value of bone scintigraphy. Laryngoscope. 1981;91:960–4. [PubMed] [Google Scholar]
- 98.Uri N, Gips S, Front A, Meyer SW, Hardoff R. Quantitative bone and 67Ga scintigraphy in the differentiation of necrotizing external otitis from severe external otitis. Arch Otolaryngol Head Neck Surg. 1991;117:623–6. doi: 10.1001/archotol.1991.01870180059012. [DOI] [PubMed] [Google Scholar]
- 99.Redleaf M, Angeli S, McCabe B. Indium 111-labelled white blood cell scintigraphy as an unreliable indicator of malignant external otitisresolution. Ann Otol Rhinol Laryngol. 1994;103:444–8. doi: 10.1177/000348949410300605. [DOI] [PubMed] [Google Scholar]
- 100.Strumas N, Antonyshyn O, Caldwell CB, Mainprize J. Multimodality imaging for precise localization of craniofacial osteomyelitis. J Craniofac Surg. 2003;14:215–9. doi: 10.1097/00001665-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 101.Carr MM, Cusimano MD, Muller PJ, Bilbao J. Aspergillosis of the cranial base. Skull Base Surg. 1994;4:159–63. doi: 10.1055/s-2008-1058968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gardiner LJ. Complicated frontal sinusitis: Evaluation and management. Otolaryngol Head Neck Surg. 1986;95:333–43. doi: 10.1177/01945998860953P112. [DOI] [PubMed] [Google Scholar]
- 103.Wu CT, Huang JL, Hsia SH, Lee HY, Lin JJ. Pott's puffy tumor after acupuncture therapy. Eur J Pediatr. 2009;168:1147–9. doi: 10.1007/s00431-008-0892-x. [DOI] [PubMed] [Google Scholar]
- 104.Mader JT, Love JT. MEO cure with HBO as adjuvant therapy. Arch Otorhinolaryngol. 1982;108:38–40. doi: 10.1001/archotol.1982.00790490040011. [DOI] [PubMed] [Google Scholar]
- 105.Neovius EB, Lind MG, Lind FG. Hyperbaric oxygen therapy for wound complications after surgery in the irradiated head and neck: A review of the literature and a report of 15 consecutive patients. Head Neck. 1997;19:315–22. doi: 10.1002/(sici)1097-0347(199707)19:4<315::aid-hed10>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 106.Hsiao YC, Lee JC, Kang BH, Lin YS. Idiopathic osteomyelitis at the base of the skull. South Med J. 2006;99:1121–3. doi: 10.1097/01.smj.0000224745.75981.52. [DOI] [PubMed] [Google Scholar]
- 107.Malone DG, O’Boynick PL, Ziegler DK, Batnitzky S, Hubble JP, Holladay FP. Osteomyelitis of the skull base. Neurosurgery. 1992;30:426–31. doi: 10.1227/00006123-199203000-00021. [DOI] [PubMed] [Google Scholar]
- 108.Rubin MM, Jui V, Sadoff RS. Oral aspergillosis in a patient with acquired immunodeficiency syndrome. J Oral Maxillofac Surg. 1990;48:997–9. doi: 10.1016/0278-2391(90)90019-x. [DOI] [PubMed] [Google Scholar]
- 109.Cravens G, Robertson H, Banta C, Garcia C, Neville P. Spinal cord compression due to intradural extramedullary aspergilloma and cyst: A case report. Surg Neurol. 1989;31:315–8. doi: 10.1016/0090-3019(89)90058-x. [DOI] [PubMed] [Google Scholar]
- 110.Benecke JE., Jr Management of osteomyelitis of the skull base. Laryngoscope. 1989;99:1220–3. doi: 10.1288/00005537-198912000-00002. [DOI] [PubMed] [Google Scholar]
- 111.Pagano L, Ricci P, Tonso A, Nosari A, Cudillo L, Montillo M, et al. Mucormycosis in patients with haematological malignancies: A retrospective clinical study of 37 cases. GIMEMA infection program (Gruppo Italiano Malattie Ematologiche Maligne Dell’adulto) Br J Haematol. 1997;99:331–6. doi: 10.1046/j.1365-2141.1997.3983214.x. [DOI] [PubMed] [Google Scholar]
- 112.Mendelson MH, Gurtman A, Szabo S, Neibart E, Meyers BR, Policar M, et al. Pseudomonas aeruginosa bacteremia in patients with AIDS. Clin Infect Dis. 1994;18:886–95. doi: 10.1093/clinids/18.6.886. [DOI] [PubMed] [Google Scholar]
- 113.Hook EW. Salmonella species (including typhoid fever) In: Mandell GL, Douglas RG Jr, Bennett JE, editors. Principles and Practice of Infectious Diseases. 3rd ed. New York: Churchill Livingstone; 1990. pp. 1700–16. [Google Scholar]
- 114.Moen MD, Lyseng-Williamson KA, Scott LJ. Liposomal amphotericin B: A review of its use as empirical therapy in febrile neutropenia and in the treatment of invasive fungal infections. Drugs. 2009;69:361–92. doi: 10.2165/00003495-200969030-00010. [DOI] [PubMed] [Google Scholar]
- 115.Kothari NA, Pelchovitz DJ, Meyer JS. Imaging of musculoskeletal infections. Radiol Clin North Am. 200l;39:653–71. doi: 10.1016/s0033-8389(05)70304-3. [DOI] [PubMed] [Google Scholar]
- 116.Gupta JD, Dang M, Palacios E. Severe muscle spasm of the neck secondary to osteomyelitis of the atlantoaxial joint. Ear Nose Throat J. 2007;86:380–1. [PubMed] [Google Scholar]
- 117.Nagashima H, Yamane K, Nishi T, Nanjo Y, Teshima R. Recent trends in spinal infections: Retrospective analysis of patients treated during the past 50 years. Int Orthop. 2010;34:395–9. doi: 10.1007/s00264-009-0741-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mortazavi MM, Quadri SA, Suriya SS, Fard SA, Hadidchi S, Adl FH, et al. Rare concurrent retroclival and pan-spinal subdural empyema: Review of literature with an uncommon illustrative case. World Neurosurg. 2017 doi: 10.1016/j.wneu.2017.11.082. pii: S1878-8750(17) 32005-3. [DOI] [PubMed] [Google Scholar]
- 119.Davis JC, Gates GA, Lerner C, Davis MG, Jr, Mader JT, Dinesman A, et al. Adjuvant hyperbaric oxygen in malignant external otitis. Arch Otolaryngol Head Neck Surg. 1992;118:89–93. doi: 10.1001/archotol.1992.01880010093022. [DOI] [PubMed] [Google Scholar]
- 120.Lancaster J, Alderson DJ, McCormick M. Non-pseudomonal malignant otitis externa and jugular foramen syndrome secondary to cyclosporin-induced hypertrichosis in a diabetic renal transplant patient. J Laryngol Otol. 2000;114:366–9. doi: 10.1258/0022215001905580. [DOI] [PubMed] [Google Scholar]
- 121.Grobman LR, Ganz W, Casiano R, Goldberg S. Atypical osteomyelitis of the skullbase. Laryngoscope. 1989;99:671–6. doi: 10.1288/00005537-198907000-00001. [DOI] [PubMed] [Google Scholar]
- 122.Chaljub G, Van Fleet R, Guinto FC, Jr, Crow WN, Martinez L, Kumar R, et al. MR imaging of clival and paraclival lesions. AJR Am J Roentgenol. 1992;159:1069–74. doi: 10.2214/ajr.159.5.1414777. [DOI] [PubMed] [Google Scholar]
- 123.Vlastos IM, Helmis G, Athanasopoulos I, Houlakis M. Acute mastoiditis complicated with bezold abscess, sigmoid sinus thrombosis and occipital osteomyelitis in a child. Eur Rev Med Pharmacol Sci. 2010;14:635–8. [PubMed] [Google Scholar]
- 124.Clark MP, Pretorius PM, Byren I, Milford CA. Central or atypical skull base osteomyelitis: Diagnosis and treatment. Skull Base. 2009;19:247–54. doi: 10.1055/s-0028-1115325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zigler JE, Bohlman HH, Robinson RA, Riley LH, Dodge LD. Pyogenic osteomyelitis of the occiput, the atlas, and the axis. A report of five cases. J Bone Joint Surg Am. 1987;69:1069–73. [PubMed] [Google Scholar]
- 126.Yamane K, Nagashima H, Tanishima S, Teshima R. Severe rotational deformity, quadriparesis and respiratory embarrassment due to osteomyelitis at the occipito-atlantoaxial junction. J Bone Joint Surg Br. 2010;92:286–8. doi: 10.1302/0301-620X.92B2.22984. [DOI] [PubMed] [Google Scholar]
- 127.Medvedev G, Palacios E, Jones W. Iatrogenic occipital osteomyelitis. Ear Nose Throat J. 2009;88:720–1. [PubMed] [Google Scholar]
- 128.Lam CH, Ethier R, Pokrupa R. Conservative therapy of atlantoaxial osteomyelitis. A case report. Spine (Phila Pa 1976) 1996;21:1820–3. doi: 10.1097/00007632-199608010-00021. [DOI] [PubMed] [Google Scholar]
- 129.Go C, Bernstein JM, De Jong AL, Sulek M, Friedman EM. Intracranial complications of acute mastoiditis. Int J Pediatr Otorhinolaryngol. 2000;52:143–8. doi: 10.1016/s0165-5876(00)00283-4. [DOI] [PubMed] [Google Scholar]
- 130.Bousser MG. Cerebral venous thrombosis: Diagnosis and management. J Neurol. 2000;247:252–8. doi: 10.1007/s004150050579. [DOI] [PubMed] [Google Scholar]
- 131.Bousser MG, Chiras J, Bories J, Castaigne P. Cerebral venous thrombosis – A review of 38 cases. Stroke. 1985;16:199–213. doi: 10.1161/01.str.16.2.199. [DOI] [PubMed] [Google Scholar]
- 132.DeVeber G, Chan A, Monagle P, Marzinotto V, Armstrong D, Massicotte P, et al. Anticoagulation therapy in pediatric patients with sinovenous thrombosis: A cohort study. Arch Neurol. 1998;55:1533–7. doi: 10.1001/archneur.55.12.1533. [DOI] [PubMed] [Google Scholar]
- 133.Einhaupl KM, Villringer A, Meister W, Mehraein S, Garner C, Pellkofer M, et al. Heparin treatment in sinus venous thrombosis. Lancet. 1991;338:597–600. doi: 10.1016/0140-6736(91)90607-q. [DOI] [PubMed] [Google Scholar]
- 134.Bradley DT, Hashisaki GT, Mason JC. Otogenic sigmoid sinus thrombosis: What is the role of anticoagulation? Laryngoscope. 2002;112:1726–9. doi: 10.1097/00005537-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 135.Kacl GM, Carls FR, Moll C, Debatin JF. Interactive MR-guided biopsies of maxillary and skull-base lesions in an open-MR system: First clinical results. Eur Radiol. 1999;9:487–92. doi: 10.1007/s003300050700. [DOI] [PubMed] [Google Scholar]
- 136.Erdman WA, Tamburro F, Jayson HT, Weatherall PT, Ferry KB, Peshock RM, et al. Osteomyelitis: Characteristics and pitfalls of diagnosis with MR imaging. Radiology. 1991;180:533–9. doi: 10.1148/radiology.180.2.2068324. [DOI] [PubMed] [Google Scholar]
- 137.Azizi SA, Fayad PB, Fulbright R, Giroux ML, Waxman SG. Clivus and cervical spinal osteomyelitis with epidural abscess presenting with multiple cranial neuropathies. Clin Neurol Neurosurg. 1995;97:239–44. doi: 10.1016/0303-8467(95)00036-j. [DOI] [PubMed] [Google Scholar]
- 138.Patmore H, Jebreel A, Uppal S, Raine CH, McWhinney P. Skull base infection presenting with multiple lower cranial nerve palsies. Am J Otolaryngol. 2010;31:376–80. doi: 10.1016/j.amjoto.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 139.Narozny W, Kuczkowski J, Mikaszewski B. Infectious skull base osteomyelitis – Still a life-threatening disease. Otol Neurotol. 2006;27:1047–8. doi: 10.1097/01.mao.0000235372.39998.7c. [DOI] [PubMed] [Google Scholar]
- 140.Mani N, Sudhoff H, Rajagopal S, Moffat D, Axon PR. Cranial nerve involvement in malignant external otitis: Implications for clinical outcome. Laryngoscope. 2007;117:907–10. doi: 10.1097/MLG.0b013e318039b30f. [DOI] [PubMed] [Google Scholar]
- 141.Tahir MZ, Quadri SA, Hanif S, Javed G. Traumatic retroclival epidural hematoma in pediatric patient-case report and review of literature. Surg Neurol Int. 2011;2:78. doi: 10.4103/2152-7806.82085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rusconi R, Bergamaschi S, Cazzavillan A, Carnelli V. Clivus osteomyelitis secondary to Enterococcus faecium infection in a 6-year-old girl. Int J Pediatr Otorhinolaryngol. 2005;69:1265–8. doi: 10.1016/j.ijporl.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 143.Nabavizadeh SA, Vossough A, Pollock AN. Clival osteomyelitis. Pediatr Emerg Care. 2013;29:1030–2. doi: 10.1097/PEC.0b013e3182a37755. [DOI] [PubMed] [Google Scholar]
- 144.He J, Lam JC, Adlan T. Clival osteomyelitis and hypoglossal nerve palsy-rare complications of Lemierre's syndrome. BMJ Case Rep 2015. 2015 doi: 10.1136/bcr-2015-209777. pii: bcr2015209777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Prabhu SP, Zinkus T, Cheng AG, Rahbar R. Clival osteomyelitis resulting from spread of infection through the fossa navicularis magna in a child. Pediatr Radiol. 2009;39:995–8. doi: 10.1007/s00247-009-1283-9. [DOI] [PubMed] [Google Scholar]
- 146.Jacquemin C, Bosley TM, al Saleh M, Mullaney P. Canalis basilaris medianus: MRI. Neuroradiology. 2000;42:121–3. doi: 10.1007/s002340050029. [DOI] [PubMed] [Google Scholar]
- 147.Nemzek W, Postma G, Poirier V, Hecht S. MR features of pachymeningitis presenting with sixth-nerve palsy secondary to sphenoid sinusitis. AJNR Am J Neuroradiol. 1995;16:960–3. [PMC free article] [PubMed] [Google Scholar]
- 148.Gilony D, Talmi YP, Bedrin L, Ben-Shosan Y, Kronenberg J. The clinical behavior of isolated sphenoid sinusitis. Otolaryngol Head Neck Surg. 2007;136:610–5. doi: 10.1016/j.otohns.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 149.Fanous MM, Margo CE, Hamed LM. Chronic idiopathic inflammation of the retropharyngeal space presenting with sequential abducens palsies. J Clin Neuroophthalmol. 1992;12:154–7. [PubMed] [Google Scholar]
- 150.Hoistad DL, Duvall AJ., 3rd Sinusitis with contiguous abscess involvement of the clivus and petrous apices. Case report. Ann Otol Rhinol Laryngol. 1999;108:463–6. doi: 10.1177/000348949910800508. [DOI] [PubMed] [Google Scholar]
- 151.Balasubramaniam S, Nadkarni T, Menon R, Goel A, Rajashekaran P. Primary Ewing's sarcoma of the petroclival bone. J Clin Neurosci. 2008;15:712–4. doi: 10.1016/j.jocn.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 152.Hurley ME, O’Meara A, Fogarty E, Hayes R. Langerhans’ cell histiocytosis of the clivus: Case report and literature review. Pediatr Radiol. 2004;34:267–70. doi: 10.1007/s00247-003-1065-8. [DOI] [PubMed] [Google Scholar]
- 153.Blitzer A, Lawson W, Meyers BR, Biller HF. Patient survival factors in paranasal sinus mucormycosis. Laryngoscope. 1980;90:635–48. doi: 10.1288/00005537-198004000-00010. [DOI] [PubMed] [Google Scholar]