Abstract
Introduction:
Fatigue has been cited as a common problem associated with traumatic brain injury. A positive association of fatigue has been suggested with insomnia and depression which are also considered to be significantly associated with traumatic brain injury.
Aims and Objectives:
The present study in post-traumatic brain injury patients is planned to assess the prevalence of fatigue, depression and insomnia, the correlation of fatigue with depression and insomnia and the risk factors associated with fatigue.
Material and Methodology:
Total 100 patients were recruited in the present study. Interview was focused on assessment of severity of traumatic brain injury, fatigue, insomnia and depression using Glasgow Coma Scale, Fatigue Severity Scale, Insomnia Severity Index and Patients Health Questionnaire(PHQ-9) respectively.
Results:
Prevalence of depression was found 84% while that of fatigue and insomnia was 50% and 49% respectively. All patients with fatigue had depression whereas those patients without fatigue were also found to have depression (68%) and this correlation was found statistically significant. Similarly, insomnia was reported in 70% of patients who were fatigued against 28% of patients with no fatigue. This was also found statistically significant (P <0.0002).
Conclusion:
Fatigue in common in post TBI patients. Insomnia and depression are closely associated with fatigue. Clinical and research investigations of fatigue in post-traumatic brain injury should include concomitant screening for treatable depressive symptoms and sleep disorders.
Keywords: Depression, fatigue, insomnia, traumatic brain injury
Introduction
Traumatic brain injury (TBI), defined as “an alteration in brain function, or other evidence of brain pathology, caused by an external force,”[1] is considered to be one of the most serious, disabling neurological conditions across the globe. In recent past, fatigue has been cited as a common, long-lasting problem after TBI ranging between 21% and 73%, depending on the characteristics of the study population.[2,3] In several studies, fatigue has been reported to have a negative effect on social, physical, and cognitive functioning[4] and participation in everyday activities.[5]
The term “fatigue” has several meanings. Physiological fatigue refers to the state of general tiredness due to physical or mental exertion, which can be improved by rest.[6] Psychological fatigue has been defined “as a state of wariness related to reduced motivation, prolonged mental fatigue, or boredom.”[7] A state that refers to tiredness not linked with previous exertion level, and not ameliorated by rest, is termed “pathological fatigue.”[8]
Sleep disturbances, such as insomnia, are very common following TBI and have been reported in frequencies from 40.2%[9] to as high as 84%.[10] A positive association between fatigue and insomnia has been suggested in several studies in recent past.[11,12,13] Similarly, fatigue in TBI patients has also been reported to have a close correlation with depression as suggested by Kempf et al.[14] and Englander et al.[12] Depressive disorders develop commonly among individuals with TBI, with estimated frequencies ranging from 6% to 77%.[14] Within this range, most experts on this subject accept an estimated 1st-year post-TBI depression frequency in the range of 25%–50%.[14,15] In a recent clinical trial, Sharma et al.[17] had reported the prevalence of depression in 42.15% post-TBI population. Considering these facts, the present study was designed to assess the presence of depression, insomnia, and fatigue in post-TBI patients. This study was also aimed to explore the association between fatigue and insomnia and to assess risk factors associated with fatigue.
Materials and Methods
Participants included both new and follow-up TBI patients regardless of severity of trauma from the Neurosurgery Ward and OPD of SMS Medical College and Group of Hospitals, a 3000-bedded super-specialty tertiary care center. The institutional ethical committee approval was obtained. The nature and purpose of the study were explained to the participants, and written informed consent was obtained from the participants. All the participants were evaluated for eligibility. To be included in the study, participants had to be 18 years or older, had at least 2-week old injury, had a history of TBI with a documented loss of consciousness or other evidence of a TBI (i.e., pathology on neuroimaging), and were able to comprehend or answer verbal or written questionnaires. Participants were excluded from the study if they were known (1) to have a serious medical illness, (2) had a current substance abuse disorder using Diagnostic and Statistical Manual, Fourth Edition (DSM-IV) criteria, (3) had mass brain lesions or other neurologic diagnoses other than TBI, and (4) had a history of current or past psychosis or mania, major depressive disorder (MDD), or any other mental disorders except current insomnia or depression using DSM-IV criteria.
Measures
Demographic and injury characteristics of the participants were assessed on a self-designed semi-structured proforma by interviewing the participants and exploring the medical records and neuroradiological investigations. Preinjury history of their insomnia, depression and substance abuse, if any was also taken into account from the participant or their next of kin. Interview was focused on assessment and severity of TBI, fatigue, insomnia, and depression using Glasgow Coma Scale (GCS), Fatigue Severity Scale (FSS), Insomnia Severity Index (ISI), and Patients Health Questionnaire-9 (PHQ-9), respectively.
GCS[17] is an extensively used clinical scale for assessing the depth and duration of impaired consciousness and coma.
FSS[18] is the most commonly used fatigue-specific questionnaire. The FSS emphasizes the impact of fatigue on daily life in terms of accumulation of functional fatigue effects, which appears suitable for detecting the presence and severity of fatigue.
ISI[19] is one of the most commonly used disease-specific measures for self-perceived insomnia severity. The psychometric properties of the ISI have been evaluated in earlier studies and have been reported to have sound measurement quality for measuring perceived insomnia severity and the impact of insomnia in different populations.[20,21] We used Hindi version of the ISI.[22]
PHQ-9 is a self-report version of PRIME-MD11, which assesses the presence of MDD using modified DSM-IV criteria.[23,24] In this study, Hindi version of PHQ-9 was used. We considered PHQ-9 score of 10 or more as depression in this study.
Assessment of lesion location was obtained via computed tomography scans conducted as part of the clinical workup. For this analysis, the results were characterized as the presence or absence of contusions, intracerebral bleed, subarachnoid hemorrhage, epidural bleed, and subdural bleed in different brain regions grouped as frontal, temporal, parietal, occipital subcortical, and/or cerebellar sites.
Statistical analyses
Data were analyzed using SPSS version 20 (IBM Corporation, Armonk, NY, United States of America), with a 2-tailed level of 5%. The qualitative data were analyzed using Chi-square test, and the quantitative data were analyzed, using Z-test. The criterion for statistical significance was set at P < 0.05.
Results
A total of 100 patients were recruited in the present study. The mean age of patients was 35.07 ± 12.88 years. 71% were male (n = 71) and 29% were female (n = 29). Road traffic accident was the most common cause (75%) of TBI, followed by falls and assaults each accounting for 19% (n = 19) and 4% (n = 4), respectively. Fifty (50%) patients reported to have fatigue in our study sample. Of these, 24 patients (48%) had moderate fatigue whereas severe fatigue was reported in 26 participants (52%).
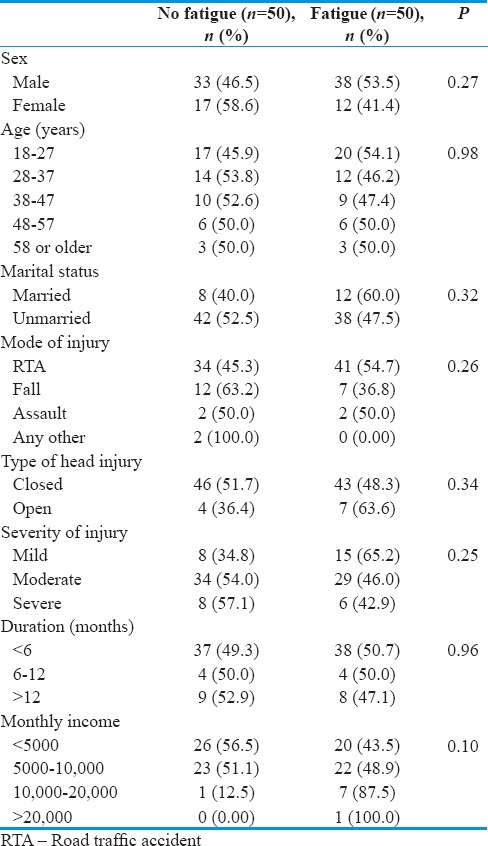
A majority of the study population comprised young age between 18 and 47 years, both with fatigue and without fatigue groups. Most of the cases with fatigue had moderate TBI (58%), and almost similar was the proportion of those without fatigue who had moderate TBI. However, none of these sociodemographic variables were statistically associated with fatigue [Table 1].
Table 1.
Sociodemographic and injury characteristics of study sample (n=100) including fatigue and without fatigue
In this study population, the prevalence of depression was found to be 84% while that of fatigue and insomnia was 50% and 49%, respectively.
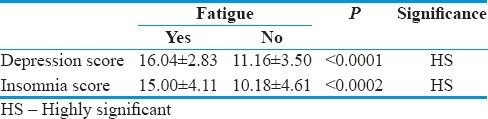
Depression was found associated in all patients with fatigue (100%). Majority of the patients without fatigue also reported to have depression (68%), and this correlation was found statistically significant. Similarly, insomnia was reported in 70% of patients who were fatigued against 28% of patients with no fatigue. This was again statistically significant (P < 0.0002) [Table 2].
Table 2.
Correlation of fatigue with depression and insomnia in traumatic brain injury patients
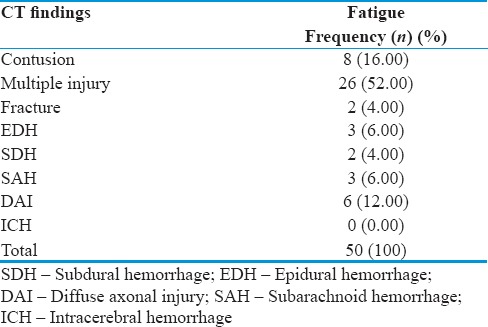
Neuroanatomical localization was also correlated with fatigue. Multiple injury including contusions was the most common (52%) site of impact, followed by cerebral contusions alone in 16% of the cases. Other areas such as extradural, subdural, subarachnoid hemorrhage, and even fracture were also found to be implicated though in lesser frequency [Table 3].
Table 3.
Distribution of computed tomography findings in fatigue patients
Discussion
Our study population was closed to the age and sex distribution of TBI in general adult population. The age range was 18–76 years with a mean of 35.07 years and sex distribution was roughly 3:1, similar to general adult population with TBI. Jain et al.[10] had also reported similar findings with regard to age and sex distribution in their study on chronic TBI patients evaluated for sleep disorders.
When we searched evidence of a temporal relationship between clinically important factors and fatigue, we focused on (1) TBI population characteristics (e.g., time since injury, severity of injury, and comorbid conditions) and (2) fatigue – its frequency, severity, and definition, with the goal of obtaining a set of risk factors that can be used for prognosis and its correlation with insomnia and depression.[9]
Fatigue was significantly associated with TBI. This figure is somewhat comparable to that reported in studies that have examined fatigue among a variety of residual symptoms following TBI.[2,5] However, the bulk of these studies involved individuals with minor TBIs and were conducted mainly in the 1st year following the accident. This study represents the efforts to concentrate specifically on fatigue and to characterize this symptom in a sample of individuals with TBI of varying levels of injury severity and covering a broad span of time elapsed since the injury.
Fatigue is thought to be caused by diffuse axonal injury, and particularly injury in brain regions which regulate arousal, attention, and speed of response, including the ascending reticular activating system, limbic system, anterior cingulate, middle frontal, and basal ganglia areas.[25] Due to the presence of impairments of speed of information processing, attention, memory, and executive function performance of mentally demanding tasks is more effortful for many people with brain injury, which find most cognitively demanding tasks more effortful. It has been suggested that fatigue results from the increased effort needed to keep up with complex everyday demands in the presence of impaired attention, processing speed, and other cognitive functions. Fatigue levels are related to severity of attentional problems. Moreover, while people with brain injury may be able to maintain task performance over time, this is associated with a disproportional increase in blood pressure, consistent with greater effort, and this is associated with fatigue levels, and subsequent emotional distress.[26] It has also been suggested that neuroendocrine abnormalities, such as growth hormone deficiency, present in many people with brain injury, may underpin fatigue.[27] Baumann et al.[28] had argued that fatigue is caused by lower levels of the wake-promoting neurotransmitter cerebrospinal fluid hypocretin-1, caused by loss of hypocretin neurons. This may cause daytime sleepiness.
Research into the relation between fatigue and depression is lacking. The prevalence of depression after TBI is variable among studies (6%–77%).[14] In our study sample, all participants who had fatigue were depressed. In a study of 666 patients at 3 years on average after injury, Seel et al.[29] found that 29% of patients with depression complained of fatigue. Kreutzer et al.[30] in a study of 722 patients with TBI found that 42% of patients were depressed, with 46% complaining of fatigue. Ziino and Ponsford[31] reported complex relationships between fatigue and depression after brain injury. They found moderate-to-strong correlations between depression (as assessed with the Hospital Anxiety and Depression Scale) and the VAS-F energy and subjective fatigue items. Depression was related to mental effort as the main cause of fatigue according to the cause of fatigue scale. However, depression was not significantly correlated with the impact of fatigue on daily-life (FSS) or with physical effort as the main cause of fatigue. In addition, the authors also found a moderate-to-strong correlation between anxiety and fatigue.
Insomnia was significantly associated with fatigue. Fatigue is one of the most prominent consequences of sleep disturbances and appears in a wide range of sleep disorders (Lichstein et al.[32]). Reports of fatigue almost systematically accompany insomnia complaints. Because between 30 and 70% of individuals with TBI report being affected by some insomnia symptoms, and about 30% fulfill the criteria for an insomnia syndrome (Ouellet et al.[33]), insomnia probably plays an important part in causing or exacerbating post-TBI fatigue.
None of the other variables including sociodemographic or injury characteristics were found to be associated with fatigue. TBI severity was not found to be predictive of the presence of significant fatigue. This result suggests that fatigue is not proportional to the severity or extent of detectable brain damage. Thus, it seems that any significant blow to the head, be it considered minor or severe, may lead to post-TBI fatigue. This result fits with the literature on other neurological conditions, indicating that fatigue does not seem related to the severity of neurological abnormalities (Ingles et al., 1999;[34] van der Werf et al., 1998[35]).
Limitations and directions for future research
Since it was a cross-sectional study and follow-up cases were also included, many parameters were determined by relying on medical record available. A prospective study of individuals postinjury should give a better idea of the natural history of fatigue; it would also have been better capture injury severity with more precise measures of length of coma or posttraumatic amnesia. Longitudinal research could also help clarify to what extent perceptions of deficits change over time and are associated with changes in fatigue, including specific types of fatigue.
Conclusion
Post-TBI fatigue is a common symptom. Its frequency may change over time, but fatigue can persist even many years after injury. Fatigue is commonly associated with symptoms of depression or sleep disturbance. Therefore, clinical and research investigations of fatigue post-TBI should include concomitant screening for treatable depressive symptoms and sleep disorders.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Brain Injury Association of America. About Brain Injury. [Last accessed on 2018 Feb 11]. Available from: http://www.biausa.org/about-brain-injury.htm .
- 2.Belmont A, Agar N, Hugeron C, Gallais B, Azouvi P. Fatigue and traumatic brain injury. Ann Readapt Med Phys. 2006;49:283. doi: 10.1016/j.annrmp.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A. Long-term outcomes after uncomplicated mild traumatic brain injury: A comparison with trauma controls. J Neurotrauma. 2011;28:937–46. doi: 10.1089/neu.2010.1516. [DOI] [PubMed] [Google Scholar]
- 4.Ziino C, Ponsford J. Selective attention deficits and subjective fatigue following traumatic brain injury. Neuropsychology. 2006;20:383–90. doi: 10.1037/0894-4105.20.3.383. [DOI] [PubMed] [Google Scholar]
- 5.Cantor JB, Ashman T, Gordon W, Ginsberg A, Engmann C, Egan M, et al. Fatigue after traumatic brain injury and its impact on participation and quality of life. J Head Trauma Rehabil. 2008;23:41–51. doi: 10.1097/01.HTR.0000308720.70288.af. [DOI] [PubMed] [Google Scholar]
- 6.Schillings ML, Kalkman JS, Janssen HM, van Engelen BG, Bleijenberg G, Zwarts MJ, et al. Experienced and physiological fatigue in neuromuscular disorders. Clin Neurophysiol. 2007;118:292–300. doi: 10.1016/j.clinph.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Jha A, Weintraub A, Allshouse A, Morey C, Cusick C, Kittelson J, et al. A randomized trial of modafinil for the treatment of fatigue and excessive daytime sleepiness in individuals with chronic traumatic brain injury. J Head Trauma Rehabil. 2008;23:52–63. doi: 10.1097/01.HTR.0000308721.77911.ea. [DOI] [PubMed] [Google Scholar]
- 8.Jason LA, Evans M, Brown M, Porter N. What is fatigue? Pathological and nonpathological fatigue. PM R. 2010;2:327–31. doi: 10.1016/j.pmrj.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 9.Fellus JL, Elovic EP. Fatigue: Assessment and treatment. In: Zasler ND, Katz DI, Zafonte RD, editors. Brain Injury Medicine: Principles and Practice. New York: Demos Medical Publishing; 2007. pp. 545–55. [Google Scholar]
- 10.Jain A, Mittal RS, Sharma A, Sharma A, Gupta ID. Study of insomnia and associated factors in traumatic brain injury. Asian J Psychiatr. 2014;8:99–103. doi: 10.1016/j.ajp.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 11.Lew HL, Poole JH, Vanderploeg RD, Goodrich GL, Dekelboum S, Guillory SB, et al. Program development and defining characteristics of returning military in a VA Polytrauma Network Site. J Rehabil Res Dev. 2007;44:1027–34. [PubMed] [Google Scholar]
- 12.Englander J, Bushnik T, Oggins J, Katznelson L. Fatigue after traumatic brain injury: Association with neuroendocrine, sleep, depression and other factors. Brain Inj. 2010;24:1379–88. doi: 10.3109/02699052.2010.523041. [DOI] [PubMed] [Google Scholar]
- 13.Cantor JB, Bushnik T, Cicerone K, Dijkers MP, Gordon W, Hammond FM, et al. Insomnia, fatigue, and sleepiness in the first 2 years after traumatic brain injury: An NIDRR TBI model system module study. J Head Trauma Rehabil. 2012;27:E1–14. doi: 10.1097/HTR.0b013e318270f91e. [DOI] [PubMed] [Google Scholar]
- 14.Kempf J, Werth E, Kaiser PR, Bassetti CL, Baumann CR. Sleep-wake disturbances 3 years after traumatic brain injury. J Neurol Neurosurg Psychiatry. 2010;81:1402–5. doi: 10.1136/jnnp.2009.201913. [DOI] [PubMed] [Google Scholar]
- 15.Seel RT, Macciocchi S, Kreutzer JS. Clinical considerations for the diagnosis of major depression after moderate to severe TBI. J Head Trauma Rehabil. 2010;25:99–112. doi: 10.1097/HTR.0b013e3181ce3966. [DOI] [PubMed] [Google Scholar]
- 16.Kim E, Lauterbach EC, Reeve A, Arciniegas DB, Coburn KL, Mendez MF, et al. Neuropsychiatric complications of traumatic brain injury: A critical review of the literature (a Report by the ANPA Committee on Research) J Neuropsychiatry Clin Neurosci. 2007;19:106–27. doi: 10.1176/jnp.2007.19.2.106. [DOI] [PubMed] [Google Scholar]
- 17.Sharma A, Jain A, Sharma A, Mittal RS, Gupta ID. Prevalence and determinants of depression and its association with quality of life in Traumatic Brain Injury (TBI) patients. Rom Neurosurg. 2015;XXIX(3):353–62. [Google Scholar]
- 18.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 19.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 20.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 21.Sierra JC, Guillén-Serrano V, Santos-Iglesias P. Insomnia severity index: Some indicators about its reliability and validity on an older adults sample. Rev Neurol. 2008;47:566–70. [PubMed] [Google Scholar]
- 22.Yu DS. Insomnia severity index: Psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66:2350–9. doi: 10.1111/j.1365-2648.2010.05394.x. [DOI] [PubMed] [Google Scholar]
- 23.Lahan V, Gupta R. Translation and validation of the insomnia severity index in Hindi language. Indian J Psychol Med. 2011;33:172–6. doi: 10.4103/0253-7176.92060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the patient health questionnaire: A systematic review. Gen Hosp Psychiatry. 2007;29:388–95. doi: 10.1016/j.genhosppsych.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Chaudhuri A, Behan PO. Fatigue in neurological disorders. Lancet. 2004;363:978–88. doi: 10.1016/S0140-6736(04)15794-2. [DOI] [PubMed] [Google Scholar]
- 27.Ziino C, Ponsford J. Vigilance and fatigue following traumatic brain injury. J Int Neuropsychol Soc. 2006;12:100–10. doi: 10.1017/S1355617706060139. [DOI] [PubMed] [Google Scholar]
- 28.Baumann CR, Werth E, Stocker R, Ludwig S, Bassetti CL. Sleep-wake disturbances 6 months after traumatic brain injury: A prospective study. Brain. 2007;130:1873–83. doi: 10.1093/brain/awm109. [DOI] [PubMed] [Google Scholar]
- 29.Seel RT, Kreutzer JS, Rosenthal M, Hammond FM, Corrigan JD, Black K, et al. Depression after traumatic brain injury: A National Institute on Disability and Rehabilitation Research Model Systems Multicenter investigation. Arch Phys Med Rehabil. 2003;84:177–84. doi: 10.1053/apmr.2003.50106. [DOI] [PubMed] [Google Scholar]
- 30.Kreutzer JS, Seel RT, Gourley E. The prevalence and symptom rates of depression after traumatic brain injury: A comprehensive examination. Brain Inj. 2001;15:563–76. doi: 10.1080/02699050010009108. [DOI] [PubMed] [Google Scholar]
- 31.Ziino C, Ponsford J. Measurement and prediction of subjective fatigue following traumatic brain injury. J Int Neuropsychol Soc. 2005;11:416–25. doi: 10.1017/s1355617705050472. [DOI] [PubMed] [Google Scholar]
- 32.Lichstein KL, Means MK, Noe SL, Aguillard RN. Fatigue and sleep disorders. Behav Res Ther. 1997;35:733–40. doi: 10.1016/s0005-7967(97)00029-6. [DOI] [PubMed] [Google Scholar]
- 33.Ouellet MC, Savard J, Morin CM. Insomnia following traumatic brain injury: A review. Neurorehabil Neural Repair. 2004;18:187–98. doi: 10.1177/1545968304271405. [DOI] [PubMed] [Google Scholar]
- 34.Ingles JL, Eskes GA, Phillips SJ. Fatigue after stroke. Arch Phys Med Rehabil. 1999;80:173–8. doi: 10.1016/s0003-9993(99)90116-8. [DOI] [PubMed] [Google Scholar]
- 35.van der Werf SP, Jongen PJ, Lycklama à Nijeholt GJ, Barkhof F, Hommes OR, Bleijenberg G, et al. Fatigue in multiple sclerosis: Interrelations between fatigue complaints, cerebral MRI abnormalities and neurological disability. J Neurol Sci. 1998;160:164–70. doi: 10.1016/s0022-510x(98)00251-2. [DOI] [PubMed] [Google Scholar]


