Abstract
Background
Migration may impact the mental health of family members who remain in places of origin. We examined longitudinal associations between having an adult child migrant and mental health, for middle-aged and older Mexican adults accounting for complex time-varying confounding.
Methods
Mexican Health and Aging Study cohort (N = 11 806) respondents ≥50 years completed a 9-item past-week depressive symptoms scale; scores of ≥5 reflected elevated depressive symptoms. Expected risk differences (RD) for elevated depressive symptoms at each wave due to having at least one (versus no) adult child migrant in the US or in another Mexican city were estimated with longitudinal targeted maximum likelihood estimation.
Results
Women with at least one adult child in the US had a higher adjusted baseline prevalence of elevated depressive symptoms (RD: 0.063, 95% CI: 0.035, 0.091) compared to women with no adult children in the US. Men with at least one child in another Mexican city at all three study waves had a lower adjusted prevalence of elevated depressive symptoms at 11-year follow-up (RD: −0.042, 95% CI: −0.082, −0.003) compared to those with no internal migrant children over those waves. For men and women with ≤3 total children, adverse associations between having an adult child in the US and depressive symptoms persisted beyond baseline.
Conclusions
Associations between having an adult child migrant and depressive symptoms varied by respondent gender, family size, and the location of the child migrant. Trends in population aging and migration bring new urgency to examining associations with other outcomes and in other settings.
Keywords: Migration, aging, depressive symptoms, Mexico, longitudinal analyses
Key Messages
No prior studies have estimated the effect of time-varying adult child out-migration on time-varying health outcomes among older adults who remain in low and middle-income countries.
The present study used longitudinal targeted maximum likelihood estimation (TMLE) to identify the associations between having an adult child migrant and depressive symptoms among Mexican adults ≥50 years with at least one living child followed over an 11-year period.
There was limited evidence of adverse associations between having an adult child migrant and depressive symptoms in the overall analytic sample.
Among women with small family sizes (i.e. ≤3 total children), the estimated prevalence of elevated depressive symptoms was 6.3% points higher at 11-year follow-up for those with an adult child in the US across all study waves compared to those with no children in the US.
Among men with ≤3 total children, the estimated prevalence of elevated depressive symptoms was 6.5% points higher at 2-year follow-up for those with an adult child in the US at both baseline and follow-up waves compared to those with no adult children in the US for the same time period. The association was not observed at 11-year follow-up.
The estimated prevalence of elevated depressive symptoms at the 11-year follow-up was 4.2% points lower for men who had an adult child in another city in Mexico at all three study waves compared to men with no adult children elsewhere in Mexico.
Introduction
While scholarship on migration and population mental health has typically focused on those who move,1–5 there is growing interest in the impact of migration on family members who remain in places of origin.6–10 Remittances sent by migrant family members may result in improved material circumstances for those who remain in places of origin11,12 with potential benefits for psychological wellbeing.13 However, family-member out-migration may result in the loss of key emotional and instrumental supports for older adults, contributing to poorer mental health.
Quantifying the effects of family-member out-migration on those who remain presents a substantial methodological challenge, principally due to concerns about endogeneity in the relationship between family-member migration and mental health.14–16 For example, while the migration of adult children may impact the mental health of parents who remain, adult children may make migration decisions based on their parents’ mental health status.17 Scholars have used a variety of methodological approaches to estimate the impact of adult child migration on health outcomes of older adults who remain while addressing these concerns about endogeneity,15,18–22 including instrumental variables analyses;18,20 fixed effects regression models;10,19 and propensity score matching methods.21,22
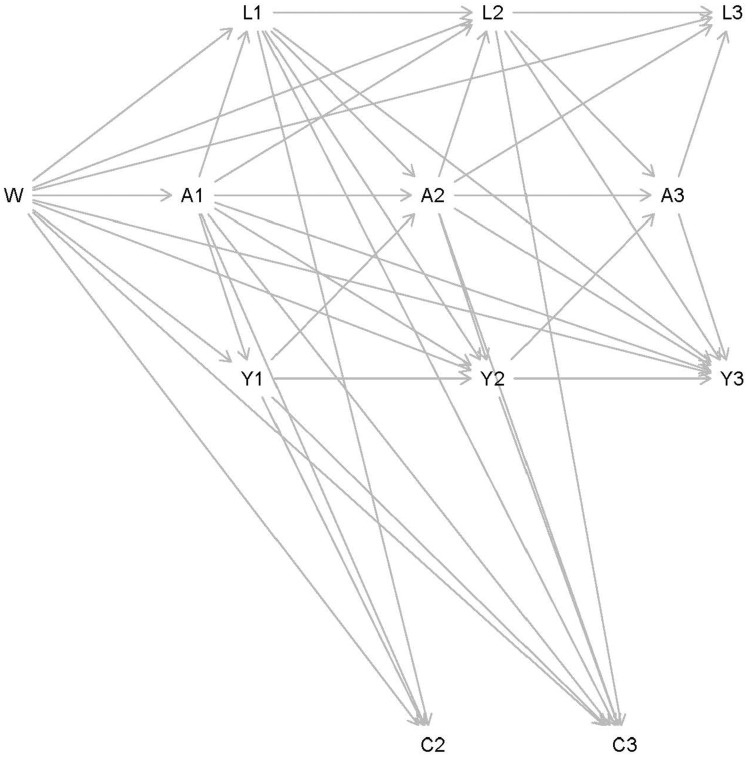
No prior approach allows for evaluation of the longitudinal relationship between adult child out-migration and depressive symptoms of older adults in a way that allows for both exposure and outcome to vary over time –while also accounting for time-varying confounders affected by prior exposure. The directed acyclic graph in Figure 1 demonstrates potential reciprocal associations between having an adult child migrant, depressive symptoms, and time-varying confounders in a longitudinal study setting with respondent attrition.
Figure 1.
Directed Acyclic Graph (DAG) depicting potential relationships between having an adult child migrant (A1, A2, A3) and depressive symptoms (Y1, Y2, Y3) over three waves of the Mexicali Health and Aging Study (2001-2012). Time-invariant (W) and time-varying confounders (L1, L2, L3) and censoring (C2, C3). are also considered.
The present study estimates the associations between having an adult child migrant and depressive symptoms among middle-aged and older adults in Mexico followed over an 11-year period. The approach overcomes methodological challenges in research on the health effects of family member migration. First, the analyses appropriately adjust for time-varying confounding variables affected by prior exposure. Second, the analyses use longitudinal targeted maximum likelihood estimation (TMLE)23 to estimate the associations between time-varying exposures and outcomes. TMLE is doubly robust, meaning that estimation will be consistent under misspecification of either the treatment or outcome model. TMLE has the added advantage of providing valid statistical inference when using data adaptive estimation approaches, further reducing reliance on correct specification of multiple parametric models.24
Mexico is an important setting for this work. While the US-Mexico migration corridor has historically been the world’s busiest, Mexican migration to the US slowed dramatically in the aftermath of the 2008 Great Recession.25 Mexico is also facing rapid population aging in the context of historically limited formal programs to support long-term medical care and support services.26 Nevertheless, the landscape has shifted over the present study period with the initiation of national health reform as well as the introduction of financial supports for older adults through the 70 y más program.27,28 The analytic strategy better accounts for these dynamic patterns compared to conventional approaches.
Methods
Data
Data come from three waves of the Mexican Health and Aging Study (MHAS). At baseline (2001), the MHAS was a nationally representative sample of Mexican adults aged ≥50 years.29 Briefly, the MHAS selected households with adults ≥50 years that were previously included in the nationally representative 2000 Mexican Employment Survey. Within each household, a target respondent was interviewed. Spouses or cohabitating partners were also interviewed regardless of age, as well as proxy respondents for older adults who could not respond on their own. Response rates were 91.8% in 2001, 93.3% in 2003, and 88.1% in 2012. The MHAS surveyed 15 186 respondents at baseline. Proxy respondents, spouse-respondents younger than 50, and respondents who had no living children at baseline were excluded from the analytic sample, which included 11 806 respondents (see flowchart in the Supplementary Appendix, available as Supplementary data at IJE online).
Exposure
The exposures at each survey wave are binary indicators of 1) whether or not any of the respondents’ children were in the US, and 2) whether or not any of the respondents’ children were in another city or town in Mexico. These measures were constructed from a detailed household roster that solicited the location of each of the respondents’ children. At baseline, over 99% of migrant children were ≥18 years; the remaining few were in mid to late-adolescence.
Outcomes
Depressive symptoms were measured with a modified 9-item Center for Epidemiological Studies – Depression (CES-D) scale.30 The scale was adapted in the style of the 8-item CES-D scale used for the Health and Retirement Study, which reduced responses to ‘yes’ or ‘no’ for ease of use with low-education older adults.31 This scale has been validated for use among older adults in Mexico; a cut-off of ≥5 depressive symptoms was suggested to have 80% sensitivity and 69% specificity when compared to clinically-diagnosed depression.32 Models using both the binary outcome of elevated (≥5) depressive symptoms and a continuous outcome of depressive symptoms (range: 0–9) were estimated.
Covariates
Models were stratified by gender given prior evidence of potentially distinct psychosocial impacts of family-member migration for older men and women in Mexico.33 Covariates were selected based on their expected contribution to both the likelihood of having an adult child migrant and to respondents’ depressive symptoms in middle to older adulthood. Time-invariant covariates included baseline age and indicators of early life socio-economic status and health; a measure of prior US migration was included for men only given that few women in the cohort were US migrants. Time-varying covariates included measures of physical and cognitive functioning, a count of self-reported chronic diseases, past-year health care utilization, health insurance coverage, monthly income, household assets, employment status, marital status, the total number of living children and grandchildren, the presence of adult children in the household and the availability of support within the community. Further details on the measurement of select covariates are available in the Supplementary Appendix, available as Supplementary data at IJE online.
Analytic strategy
The application of longitudinal targeted maximum likelihood estimation (TMLE)23,24 involved first estimating outcome models for the conditional probability of elevated depressive symptoms at each of the three study waves (t = 1, 2, 3) for different regimes of prior exposure. For example, for the third study wave (2012, t = 3), models estimated the conditional probability of elevated depressive symptoms in 2012 for two contrasting exposure regimes: 1) having at least one adult child migrant in 2001, 2003, and 2012 (i.e. at time point t and all prior ts) and 2) having no adult child migrants in 2001, 2003, or 2012, conditional on time-invariant covariates and lagged (2003 or t-1, 2001 t-2) time-varying covariates (including the confounders and the lagged value of depressive symptoms) and inclusion in the survey wave. This estimation procedure was carried out analogously for the other two study waves. There was not support in the data to model other regimes; adult child migration status was largely stable across study waves. Baseline models were conditional only on time-invariant covariates; lagged values of time-varying indicators or prior values of the outcome are not available for these models.
The TMLE algorithm then updated the outcome model at each wave with cumulative inverse probability weights of 1) exposure at each wave conditional on time-invariant covariates, lagged time-varying covariates (including values of the outcome), prior exposure, and inclusion in the survey wave, and 2) inclusion in survey wave conditional on time-invariant covariates, lagged time-varying covariates (including outcome values), and prior exposure. For example, the cumulative weights applied to the outcome model for the third wave (2012, t = 3) were evaluated as the product of the exposure weights generated for 2001, 2003, and 2012 study waves. Weights for inclusion in the survey were generated using separate models to account for attrition due to 1) death, 2) having a proxy interview, or 3) loss-to-follow-up. A small group of respondents who no longer had living children at follow-up waves were combined with those who had a proxy interview.
Exposure, outcome, and attrition models were estimated data-adaptively via an ensemble modeling approach known as the SuperLearner.34 For a given library of machine learning algorithms (candidate estimators), this approach selects the weighted combination of candidate estimators with the lowest cross-validated mean squared error (via 10-fold cross-validation). In these analyses, LASSO,35 gradient boosting machine,36,37 and generalized linear models were used as candidate estimators in the SuperLearner. Cumulative inverse probability weights were truncated at the 99th percentile.38 Models were estimated using the stremr and sl3 packages for R;39,40 code sample is available in the Supplementary Appendix, available as Supplementary data at IJE online.
The results are presented as adjusted marginal risk differences (RDs), contrasting at each time point, t (where t = 1, 2, 3), the expected prevalence of elevated depressive symptoms at time t if respondents had an adult child migrant at t and all prior ts compared to the expected prevalence of elevated depressive symptoms at t if respondents had no adult child migrant during the same time points (i.e. t and all prior ts).41 For example, at time point 3 (i.e. the 2012 study wave), we present the RD contrasting the expected prevalence of elevated depressive symptoms in 2012 if respondents had an adult child migrant in 2001, 2003, and 2012 compared to the expected prevalence of elevated depressive symptoms in 2012 if respondents had no adult children who were migrants in 2001, 2003, or 2012.
Multiple imputation was used to address missing data using the Amelia package for R.42 Ten multiply imputed datasets were created for the baseline wave, and mean values from multiply imputed baseline models were incorporated into the multiple imputation of time-varying measures at successive follow-up waves. Estimates were combined using Rubin’s rules.43
Results
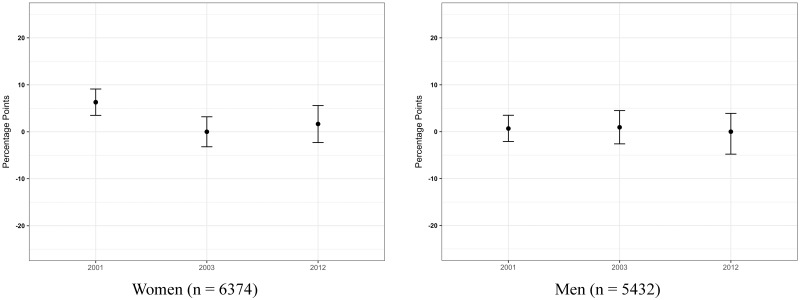
Roughly a quarter of respondents had at least one child in the US and a third had at least one child living elsewhere in Mexico (Table 1). The results of primary analyses for women (Table 2, Figure 2), indicate that the estimated prevalence of elevated depressive symptoms at baseline was 6.3% points higher (95% CI: 0.035, 0.091) for those who had at least one adult child in the US at baseline compared to those who had no adult children in the US. There were similar patterns when depressive symptoms were instead analyzed as a continuous outcome (Table 3). There were no associations between having an adult child in the US and depressive symptoms in the other study waves for women, or in any of the study waves for men.
Table 1.
Baseline (2001) descriptive characteristics for respondents with at least one living child, Mexican Health and Aging Study
| Women | Men | |
|---|---|---|
| N | 6374 | 5432 |
| Outcome | ||
| ≥5 depressive symptoms | 3004 (47.13) | 2060 (37.92) |
| Exposures | ||
| At least one child in US | 1532 (24.04) | 1237 (22.77) |
| At least one child in different city/town in Mexico | 2329 (36.53) | 1868 (34.39) |
| Covariates | ||
| Demographic Characteristics | ||
| Age (in years) | 61.73 (9.22) | 62.17 (9.42) |
| Urban residence | 4323 (67.82) | 3546 (65.28) |
| Residence in high US out-migration state | 1779 (27.91) | 1488 (27.39) |
| US migrant | 209 (3.28) | 896 (16.49) |
| Married | 3795 (59.54) | 4658 (85.75) |
| Life-course Socio-Economic Status | ||
| Education (in years) | 3.99 (3.92) | 5.05 (4.83) |
| No sanitation facilities during childhood | 4175 (65.50) | 3753 (69.09) |
| Total household income (in pesos) | 4510 (53 384) | 6083 (65 977) |
| Total household net worth (in pesos) | 362 000 (697 264) | 429 593 (889 858) |
| Currently working | 1493 (23.42) | 3787 (69.72) |
| Material items in household, range (0-6) | 4.36 (1.69) | 4.35 (1.70) |
| Health and Health Care Utilization | ||
| Major illness or injury during childhood | 717 (11.25) | 609 (11.21) |
| Health coverage | 4101 (64.34) | 3316 (61.05) |
| Past year medical visit | 4578 (71.82) | 3083 (56.76) |
| Lower-body functional limitations, range (0-8) | 3.07 (2.46) | 2.11 (2.32) |
| Cognitive function, range (0-80) | 35.80 (16.94) | 38.32 (17.04) |
| Chronic health conditions, range (0-6) | 0.80 (0.81) | 0.58 (0.78) |
| Family and Community | ||
| At least one adult child living in the household | 4512 (70.79) | 3953 (72.77) |
| Number of living children | 5.57 (2.95) | 5.59 (2.98) |
| Number of living grandchildren | 11.44 (10.72) | 9.41 (10.23) |
| Can count on neighbors/friends for help with daily activities | 4092 (64.20) | 3482 (64.10) |
Data presented as a. Mean (SD) or b. N (%).
Table 2.
Marginal risk differences in the prevalence of ≥5 depressive symptoms for adults ≥50 years in the Mexican Health and Aging Study (2001–2012) with at least one adult migrant child versus no migrant children
| Women (n = 6374) | ||||
|---|---|---|---|---|
| Adult child in the US |
Adult child elsewhere in Mexico |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.063 | (0.035, 0.091) | −0.007 | (−0.033, 0.018) |
| 2003 | 0.000 | (−0.032, 0.032) | 0.001 | (−0.030, 0.032) |
| 2012 | 0.017 | (−0.023, 0.056) | 0.010 | (−0.021, 0.044) |
|
Men (n=5432) | ||||
|
Adult child in the US |
Adult child elsewhere in Mexico |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.007 | (−0.021, 0.035) | −0.004 | (−0.027, 0.020) |
| 2003 | 0.009 | (−0.026, 0.045) | 0.013 | (−0.017, 0.044) |
| 2012 | 0.000 | (−0.048, 0.039) | −0.042 | (−0.082, −0.003) |
Source: Mexican Health and Aging Study.
Figure 2.
Marginal risk differences in the expected prevalence of ≥ 5 depressive symptoms at each time point (t) given counterfactual outcomes of having at least one child in the US versus having no child in the US at t and all prior ts.
Table 3.
Marginal risk difference in average depressive symptoms (range: 0-9) for adults ≥50 years in the Mexican Health and Aging Study (2001-2012) with at least one adult migrant child versus no migrant children
| Women (n = 6374) | ||||
|---|---|---|---|---|
| Adult child in the US |
Adult child elsewhere in Mexico |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.308 | (0.155, 0.461) | −0.053 | (−0.188, 0.082) |
| 2003 | 0.037 | (−0.146, 0.221) | 0.019 | (−0.143, 0.181) |
| 2012 | 0.153 | (−0.066, 0.371) | 0.059 | (−0.132, 0.250) |
|
Men (n=5432) | ||||
|
Adult child in the US |
Adult child elsewhere in Mexico |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.125 | (−0.032, 0.283) | −0.039 | (−0.174, 0.096) |
| 2003 | −0.042 | (−0.239, 0.154) | 0.078 | (−0.098, 0.255) |
| 2012 | 0.061 | (−0.185, 0.307) | −0.134 | (−0.391, 0.124) |
Source: Mexican Health and Aging Study.
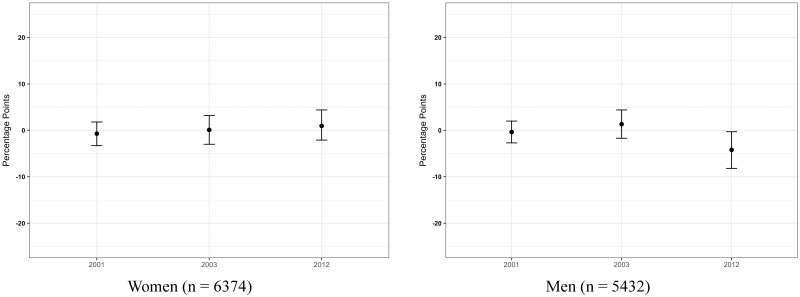
There were no associations between having an adult child elsewhere in Mexico and depressive symptoms at any time points for women or for men at baseline or two-year follow-up. The expected prevalence of elevated depressive symptoms at the 11-year follow-up was 4.2% points lower for men who had an adult child elsewhere in Mexico in 2001, 2003, and 2012 compared to their counterparts who did not have an adult child elsewhere in Mexico in any year (95% CI: −0.082, −0.003) (Figure 3). The estimated association was weaker although in the same protective direction when depressive symptoms were analyzed as a continuous outcome.
Figure 3.
Marginal risk differences in the expected prevalence of ≥ 5 depressive symptoms at each time point (t) given counterfactual outcomes of having at least one child in another city/town in Mexico versus having no adult children in another city/town in Mexico at t and all prior ts.
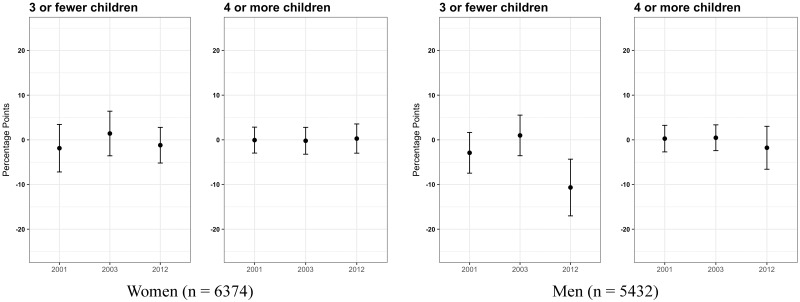
Additional un-prespecified analyses were estimated separately for respondents at or below the 25th percentile of family size (i.e. ≤3 total living children) and for respondents with larger family sizes (i.e. ≥4 total living children). Women with ≤3 children had higher expected prevalence of elevated depressive symptoms at baseline (RD: 0.054; 95% CI: -0.023, 0.130) and in the final study wave (RD: 0.063; 95% CI: 0.000, 0.126) (Table 4, Figure 4). Among men, those with ≤ 3 children had higher expected prevalence of elevated depressive symptoms at baseline (RD: 0.059; 95% CI: −0.025, 0.142) and two-year follow-up (RD: 0.065; 95% CI: −0.010, 0.140). Patterns for both women and men with ≥4 total children were similar as those reported for primary analyses. The protective association between having an adult child elsewhere in Mexico throughout the study and depressive symptoms in the final wave was observed for men with ≤3 total children (RD: −0.107; 95% CI: −0.170, −0.043) but not for men with ≥4 children (Table 5, Figure 5). There were similar results when using the continuous measure of depressive symptoms (Appendix Tables B and C, available as Supplementary data at IJE online).
Table 4.
Marginal risk differences in the prevalence of ≥5 depressive symptoms for adults ≥50 years in the Mexican Health and Aging Study (2001–2012) with at least one adult child in the US versus no adult children in the US, by total number of living children
| Women | ||||
|---|---|---|---|---|
| ≤3 total children (n = 1744) |
≥4 total children (n = 4630) |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.054 | (−0.023, 0.130) | 0.072 | (0.041, 0.103) |
| 2003 | 0.007 | (−0.060, 0.074) | 0.002 | (−0.030, 0.034) |
| 2012 | 0.063 | (0.0004, 0.126) | 0.007 | (−0.025, 0.039) |
| Men | ||||
|
≤3 total children (n=1498) |
≥4 total children (n=3934) |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | 0.059 | (−0.025, 0.142) | 0.004 | (−0.027, 0.034) |
| 2003 | 0.065 | (−0.010, 0.140) | 0.004 | (−0.028, 0.035) |
| 2012 | 0.000 | (−0.056, 0.057) | −0.004 | (−0.035, 0.027) |
Source: Mexican Health and Aging Study.
Figure 4.
Marginal risk differences in the expected prevalence of ≥ 5 depressive symptoms at each time point (t) given counterfactual outcomes of having at least one child in the US versus having no adult children in the US at t and all prior ts, stratified by total number of living children (≤3 children versus ≥ 4 children).
Table 5.
Marginal risk differences in the prevalence of ≥5 depressive symptoms for adults ≥50 years in the Mexican Health and Aging Study (2001–2012) with at least one adult child elsewhere in Mexico versus no adult children elsewhere in Mexico, by total number of living children
| Women | ||||
|---|---|---|---|---|
| ≤3 total children (n = 1744) |
≥4 total children (n = 4630) |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | −0.019 | (−0.072, 0.034) | −0.001 | (−0.030, 0.028) |
| 2003 | 0.014 | (−0.036, 0.064) | −0.002 | (−0.032, 0.028) |
| 2012 | −0.012 | (−0.052, 0.028) | 0.003 | (−0.030, 0.036) |
| Men | ||||
|
≤3 total children (n=1498) |
≥4 total children (n=3934) |
|||
| Marginal RD | 95% CI | Marginal RD | 95% CI | |
| 2001 | −0.029 | (−0.075, 0.017) | 0.003 | (−0.027, 0.032) |
| 2003 | 0.010 | (−0.036, 0.055) | 0.005 | (−0.024, 0.034) |
| 2012 | −0.107 | (−0.170, −0.043) | −0.018 | (−0.066, 0.030) |
Source: Mexican Health and Aging Study.
Figure 5.
Marginal risk differences in the expected prevalence of ≥ 5 depressive symptoms at each time point (t) given counterfactual outcomes of having at least one child elsewhere in Mexico versus having no adult children elsewhere in Mexico at t and all prior ts, stratified by total number of living children (≤3 children versus ≥4 children).
Discussion
Trends of accelerated global migration and population aging have contributed to growing interest in the potential mental health impacts of family-member migration on those who remain in places of origin. Prior research on this topic has not considered how the relationship between having a migrant family member and health outcomes unfolds over time. The present study utilized longitudinal targeted maximum likelihood estimation to robustly estimate the associations between having an adult child migrant and depressive symptoms over an 11-year period for a national sample of older adults in Mexico. In the overall sample, there was limited evidence of meaningful associations between having an adult migrant child and depressive symptoms. The only exceptions were an adverse baseline association between having an adult child in the US and depressive symptoms for women and a protective association between having an adult child in Mexico and depressive symptoms for men at 11-year follow-up.
Despite overall null findings, there was some evidence suggesting adverse associations between having an adult child in the US and depressive symptoms for both men and women with relatively few total children. Moreover, these associations persisted beyond the baseline wave, even after accounting for time-varying covariates. These adverse associations are consistent with findings from prior cross-sectional studies carried out in the Mexican context,9,15,18 which have generally been explained by the potential reduction in social and instrumental support for older adults whose family members migrate. The adverse effects of family-member out-migration may be particularly acute for older adults who remain in low and middle-income country (LMIC) settings that have limited formal old-age assistance,26 and may depend critically on the financial and in-person assistance of family members. The results of these stratified analyses nevertheless add important nuance to prior research, suggesting that adverse associations were largely restricted to respondents with few total children.
There were otherwise almost no associations for the overall sample and those with larger family sizes. The exception was for a protective association between having an adult child elsewhere in Mexico at all three study waves and depressive symptoms at 11-year follow-up for men. These results coincide with other studies finding null or protective associations between having a within-country migrant child.19,21 There are likely many fewer barriers to in-person or even long-distance communication between internal migrants and their family members relative to international migrants, possibly facilitating the provision of assistance and support. In addition, MHAS respondents generally had robust networks of adult children and grandchildren, and reported high community-level support. Respondents may have continued to receive sufficient support even if one or more adult children had migrated. On the other hand, in models stratified by respondent family size the protective association between having an internal migrant child and depressive symptoms was observed only for men with ≤3 total children – suggesting that there may be benefits to the within-country migration of adult children even for those with smaller family networks.
The potential receipt of remittances from adult migrant children has also been hypothesized as a potential offsetting factor driving null or positive relationships with mental health.13,19 Remittances may support access to health care or other material resources that may be linked to improved mental wellbeing.13,44 The results of un-prespecified analyses confirm that respondents who had at least one adult child migrant were more likely to report receiving financial support from their children than those with no migrant children (Supplementary Appendix Table D, available as Supplementary data at IJE online). However, receiving financial assistance from adult children was associated with either no or greater risk of elevated depressive symptoms (Supplementary Appendix Table E, available as Supplementary data at IJE online). Future research should further examine the complex economic pathways that may link adult child migration to the wellbeing of older adults who remain.
Limitations and strengths
Results should be interpreted in light of a number of limitations. For one, the causal interpretation of the estimates hinges on a set of additional assumptions that may be unreasonable in this context. For example, unmeasured confounders, including local-level economic, environmental, or safety conditions could be driving both adult child out-migration and depressive symptoms among older adults who remain.45,46 The MHAS does not contain sufficient information on respondents’ residence to account for these factors.
Second, measures of earlier-life socio-economic and health status are subject to bias given that they are reported retrospectively. Nevertheless, prior research suggests that such retrospective measures are sufficiently reliable,47 particularly among older adults.48 We additionally controlled for factors that predict reliability of retrospective reports of early-life conditions (e.g. age, cognition).49
Third, scholars have recently drawn attention to the potential for estimates of family member migration to be underestimated in population-based data sources due in part to the out-migration of entire families, with no one remaining to report migration status.50,51 Survey respondents who do remain in Mexico may be unsure of family members’ whereabouts, and may incorrectly report on family-member migration status.51 Methods of correcting for these biases rely on data that follows migrating household members (e.g. to the US) – information that is not available in the MHAS. Nevertheless, the present study has a number of strengths, including the use of longitudinal TMLE, a doubly robust, semiparametric estimation strategy that reduces reliance on correct specification of multiple parametric models. Additionally, the analyses correctly adjust for time-varying confounders affected by prior exposure.52,53
Conclusion
There is growing interest in family-member out-migration as a determinant of global mental health, particularly in the context of population aging. The present study contributes to this literature by examining the longitudinal associations between having an adult child migrant and time-varying depressive symptoms in a population-based prospective study of older adults in Mexico using a doubly robust estimation strategy. The results suggest important heterogeneity by respondent gender, the location of migrant children, and family size, with adverse associations observed only for those with an adult child in the US – and only for respondents with few total children. Further research may extend this work to other health and aging outcomes in Mexico and other low and middle-income country settings.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers K01AG056602, RF1055486, and R01AG018016; by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R00DA042127; and by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R01AI074345. The MHAS (Mexican Health and Aging Study) is partly sponsored by the National Institutes of Health/National Institute on Aging under Award Number R01AG018016 and the INEGI in México. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the INEGI.
Conflict of interest: None declared.
Supplementary Material
References
- 1. Goldman N, Pebley AR, Creighton MJ, Teruel GM, Rubalcava LN, Chung C.. The consequences of migration to the United States for short-term changes in the health of Mexican immigrants. Demography 2014;51:1159–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zimmerman C, Kiss L, Hossain M.. Migration and health: a framework for 21st century policy-making. PLoS Med 2011;8:e1001034.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cantor-Graae E, Pedersen CB.. Full spectrum of psychiatric disorders related to foreign migration: a Danish population-based cohort study. JAMA Psychiatry 2013;70:427–35. [DOI] [PubMed] [Google Scholar]
- 4. Stillman S, McKenzie D, Gibson J.. Migration and mental health: evidence from a natural experiment. J Health Econ 2009;28:677–87. [DOI] [PubMed] [Google Scholar]
- 5. Hwang SS, Cao Y, Xi J.. Project-induced migration and depression: a panel analysis. Soc Sci Med 2010;70:1765–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nobles J, Rubalcava L, Teruel G.. After spouses depart: emotional wellbeing among nonmigrant Mexican mothers. Soc Sci Med 2015;132:236–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Breslau J, Borges G, Tancredi D. et al. Migration from Mexico to the United States and subsequent risk for depressive and anxiety disorders: a cross-national study. Arch Gen Psychiatry 2011;68:428–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Borges G, Breslau J, Su M, Miller M, Medina-Mora ME, Aguilar-Gaxiola S.. Immigration and suicidal behavior among Mexicans and Mexican Americans. Am J Public Health 2009;99:728–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Familiar I, Borges G, Orozco R, Medina-Mora ME.. Mexican migration experiences to the US and risk for anxiety and depressive disorders. J Affect Disord 2011;130:83–91. [DOI] [PubMed] [Google Scholar]
- 10. Lu Y. Household migration, social support, and psychosocial health: the perspective from migrant-sending areas. Soc Sci Med 2012;74:135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Molina Millán T. Regional Migration, Insurance and Economic Shocks: Evidence from Nicaragua. IZA Discussion Paper No. 9494. Bonn, Germany: Institute for the Study of Labor (IZA; ), 2015, p. 59. [Google Scholar]
- 12. Airola J. The use of remittance income in Mexico. Int Migr Rev 2007;41:850–59. [Google Scholar]
- 13. Silverstein M, Cong Z, Li S.. Intergenerational transfers and living arrangements of older people in rural China: consequences for psychological well-being. J Gerontol B Psychol Sci Soc Sci 2006;61:S256–66. [DOI] [PubMed] [Google Scholar]
- 14. Antman FM. The Impact of Migration on Family Left Behind. IZA Discussion Paper No. 6374. Bonn, Germany: Institute for the Study of Labor (IZA; ), 2012, p. 35. [Google Scholar]
- 15. Antman FM. How Does International Migration Affect the Health of Elderly Parents Left Behind? Evidence from Mexico Boulder, CO: Department of Economics, University of Colorado at Boulder, 2016. http://spot.colorado.edu/∼antmanf/AntmanMigration&ElderlyHealth.pdf (1 October 2017, date last accessed).
- 16. Breslau J, Borges G, Tancredi DJ. et al. Health selection among migrants from Mexico to the U.S.: childhood predictors of adult physical and mental health. Public Health Rep 2011;126:361–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Giles J, Mu R.. Elderly parent health and the migration decisions of adult children: evidence from rural China. Demography 2007;44:265–88. [DOI] [PubMed] [Google Scholar]
- 18. Antman F. Adult child migration and the health of elderly parents left behind in Mexico. Am Econ Rev 2010;100:205–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Abas M, Tangchonlatip K, Punpuing S. et al. Migration of children and impact on depression in older parents in rural Thailand, southeast Asia. JAMA Psychiatry 2013;70:226–34. [DOI] [PubMed] [Google Scholar]
- 20. Böhme MH, Persian R, Stöhr T.. Alone but better off? Adult child migration and health of elderly parents in Moldova. J Health Econ 2015;39:211–27. [DOI] [PubMed] [Google Scholar]
- 21. Kuhn R, Everett B, Silvey R.. The effects of children’s migration on elderly kin’s health: a counterfactual approach. Demography 2011;48:183–209. [DOI] [PubMed] [Google Scholar]
- 22. Downer B, González-González C, Goldman N, Pebley AR, Wong R.. The effect of adult children living in the United States on the likelihood of cognitive impairment for older parents living in Mexico. Ethn Health 2018;23:57–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Petersen M, Schwab J, Gruber S, Blaser N, Schomaker M, van der Laan M.. Targeted maximum likelihood estimation for dynamic and static longitudinal marginal structural working models. J Causal Inference 2014;2:147–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schuler MS, Rose S.. Targeted maximum likelihood estimation for causal inference in observational studies. Am J Epidemiol 2017;185:65–73. [DOI] [PubMed] [Google Scholar]
- 25. Passel JS, Cohn DV, Gonzalez-Barrera A.. Net Migration from Mexico Falls to Zero—and Perhaps Less. Washington, DC: Pew Research Center, 2012. [Google Scholar]
- 26. Wong R, Palloni A.. Aging in Mexico and Latin America In: Uhlenberg P. (ed). International Handbook of Population Aging. US: Springer Science, 2009. [Google Scholar]
- 27. Amuedo-Dorantes C, Juarez L.. Old-Age Government Transfers and the Crowding Out of Private Gifts: The 70 Plus Program for the Rural Elderly in Mexico. Banco de México Working Paper No. 2013–17. Mexico City, México: Banco de México, 2012, p. 39. [Google Scholar]
- 28. Frenk J, González-Pier E, Gómez-Dantés O, Lezana MA, Knaul FM.. Comprehensive reform to improve health system performance in Mexico. Lancet 2006;368:1524–34. [DOI] [PubMed] [Google Scholar]
- 29. Wong R, Michaels-Obregon A, Palloni A.. Cohort profile: the Mexican Health and Aging Study (MHAS). Int J Epidemiol 2017;46:e2.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Radloff LS. The CES-D scale, a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 31. Steffick DE. Documentation of Affective Functioning Measures in the Health and Retirement Study. Ann Arbor, MI: Survey Research Center, University of Michigan, 2000. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf (15 October 2017, date last accessed). [Google Scholar]
- 32. Aguilar-Navarro SM, Fuentes-Cantú A, Ávila-Funes JA, García-Mayo EJ.. Validez y confiabilidad del cuestionario del ENASEM para la depresión en adultos mayores. Salud Pública Méx 2007;49:256–62. [DOI] [PubMed] [Google Scholar]
- 33. Alvarado BE, Zunzunegui MV, Béland F, Sicotte M, Tellechea L.. Social and gender inequalities in depressive symptoms among urban older adults of Latin America and the Caribbean. J Gerontol B Psychol Sci Soc Sci 2007;62:S226–37. [DOI] [PubMed] [Google Scholar]
- 34. Polley E, LeDell E, Kennedy C, Lendle S, van der Laan M.. SuperLearner: Super Learner Prediction. R Package Version 2.0–22, 2017.
- 35. Tibshirani R. Regression shrinkage and selection via the Lasso. J R Stat Soc Ser B 1996;58:267–88. [Google Scholar]
- 36. Friedman J. Greedy boosting approximation: a gradient boosting machine. Ann Stat 2001;29:1189–232. [Google Scholar]
- 37. Chen T, Guestrin C. XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining San Francisco, CA, 2016, pp. 785–94.
- 38. Cole SR, Hernán MA.. Constructing inverse probability weights for marginal structural models. Am J Epidemiol 2008;168:656–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sofrygin O, van der Laan MJ, Neugebauer R.. Stremr: Streamlined Estimation for Static, Dynamic and Stochastic Treatment Regimes in Longitudinal Data. R package version 3.3.2, 2017.
- 40. Coyle J, Hejazi N, Sofrygin O, Malenica I.. sl3: Pipelines for Machine Learning and Super Learning. R Package Version 1.0.0., 2018.
- 41. van der Laan MJ, Gruber S.. Targeted minimum loss based estimation of causal effects of multiple time point interventions. Int J Biostat 2012;8:1–41. [DOI] [PubMed] [Google Scholar]
- 42. Honaker J, King G, Blackwell M.. Amelia II: A Program for Missing Data. R Package: version 1.7.3, 2014.
- 43. Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley, 1987. [Google Scholar]
- 44. Salinas JJ. Tapping healthcare resource by older Mexicans with diabetes: how migration to the United States facilitates access. J Cross Cult Gerontol 2008;23:301–12. [DOI] [PubMed] [Google Scholar]
- 45. Hunter LM, Murray S, Riosmena F.. Rainfall patterns and U.S. migration from rural Mexico. Int Migr Rev 2013;47:874–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Feng S, Krueger AB, Oppenheimer M.. Linkages among climate change, crop yields and Mexico-US cross-border migration. Proc Natl Acad Sci USA 2010;107:14257–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Krieger N, Okamoto A, Selby JV.. Adult female twins’ recall of childhood social class and father’s education: a validation study for public health research. Am J Epidemiol 1998;147:704–08. [DOI] [PubMed] [Google Scholar]
- 48. Haas SA. The long-term effects of poor childhood health: an assessment and application of retrospective reports. Demography 2007;44:113–35. [DOI] [PubMed] [Google Scholar]
- 49. Vuolo M, Ferraro KF, Morton PM, Yang T-Y.. Why do older people change their ratings of childhood health? Demography 2014;51:1999–2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Steinmayr A. When a Random Sample is Not Random: Bounds on the Effect of Migration on Household Members Left behind. Kiel Working Paper No. 1975. Kiel, Germany: Kiel Institute for the World Economy, 2014, pp. 54. [Google Scholar]
- 51. Hamilton ER, Savinar R.. Two sources of error in data on migration from Mexico to the United States in Mexican household-based surveys. Demography 2015;52:1345–55. [DOI] [PubMed] [Google Scholar]
- 52. Robins JM, Hernán MA, Brumback B.. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550–60. [DOI] [PubMed] [Google Scholar]
- 53. Mansournia MA, Danaei G, Forouzanfar MH. et al. Effect of physical activity on functional performance and knee pain in patients with osteoarthritis: analysis with marginal structural models. Epidemiology 2012;23:631–40. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.