Abstract
Objective:
To present recommendations for athletic trainers and other health care providers regarding the identification of risk factors for and management of individuals with patellofemoral pain (PFP).
Background:
Patellofemoral pain is one of the most common knee diagnoses; however, this condition continues to be one of the most challenging to manage. Recent evidence has suggested that certain risk factors may contribute to the development of PFP. Early identification of risk factors may allow clinicians to develop and implement programs aimed at reducing the incidence of this condition. To date, clinicians have used various treatment strategies that have not necessarily benefitted all patients. Suboptimal outcomes may reflect the need to integrate clinical practice with scientific evidence to facilitate clinical decision making.
Recommendations:
The recommendations are based on the best available evidence. They are intended to give athletic trainers and other health care professionals a framework for identifying risk factors for and managing patients with PFP.
Key Words: anterior knee pain, patella, risk factors, therapeutic exercise, hip musculature, quadriceps strength
Patellofemoral pain (PFP) is one of the most common knee conditions in patients presenting to orthopaedic practices.1–4 Although frequently seen in a wide range of populations, PFP is particularly prevalent in younger people who are physically active.5–7 In addition, females are reported to be at higher risk for the development of PFP than males.7,8
The significance of PFP is highlighted by the fact that as many as 70% to 90% of individuals with this condition have recurrent or chronic symptoms.1,3,9,10 Interventions for PFP have shown positive short-term outcomes, but long-term clinical outcomes are less compelling.1,9,11,12 The apparent lack of long-term success in treating this condition may be due to an incomplete understanding of the underlying factors that contribute to its development. Due to its multifactorial causes, the treatment of PFP is complex and involves an intricate interplay of anatomical variations and biomechanical abnormalities.13
The purpose of this position statement is to present recommendations for health care providers regarding the identification of risk factors and management of PFP. The recommendations outlined here represent the best available evidence to date. Continued research is necessary to refine these recommendations and to advance our understanding of this complicated condition.
The National Athletic Trainers' Association (NATA) suggests the following guidelines to identify risk factors for and manage patients with PFP. The strength of recommendations is based on the Strength of Recommendation (SOR) Taxonomy criteria.14 In the SOR Taxonomy, the letter indicates the consistency and evidence-based strength of the recommendation (A has the strongest evidence base). For the practicing clinician, any recommendation with an A grade warrants attention and should be inherent to clinical practice. Less research supports recommendations with grade B or C; these should be discussed by the sports medicine staff. Grade B recommendations are based on inconsistent or limited controlled research outcomes. Grade C recommendations should be considered as expert guidance despite limited research support.
RECOMMENDATIONS
Risk Factors (Based on Prospective Studies)
-
1.
Hip adduction and internal rotation during dynamic tasks such as running and landing from a jump are risk factors for the development of PFP.5,15 SOR: B
-
2.
Increased knee-abduction impulses and moments during running and drop landings are risk factors for the development of PFP.16,17 SOR: B
-
3.
Novice runners who developed PFP generated greater vertical peak force to the lateral heel and second and third metatarsals. Military recruits who developed PFP walked with greater lateral foot pressure.18 SOR: B
-
4.
Reduced isometric hip-abductor, external-rotator, and hip-extensor strength are not likely risk factors for the development of PFP.19,20 SOR: B
-
5.
Quadriceps weakness is a risk factor for the development of PFP.21,22 SOR: B
-
6.
Delayed activation of the vastus medialis obliquus (VMO) relative to the vastus lateralis (VL), as identified with a patellar tendon tap or voluntary tasks (eg, rocking back on the heels), can contribute to the onset of PFP.23,24 SOR: C
-
7.
Static measures, such as the quadriceps angle (Q-angle), foot posture index, lower leg-heel alignment, and heel-to-forefoot alignment, are not predictors of PFP development.5,24–26 SOR: B
-
8.
Individuals with quadriceps tightness and decreased vertical-jump performance have developed PFP.24 SOR: B
Pain and Functional Outcome Measures
-
9.
Clinicians should use a 10-cm visual analog scale (VAS) to assess changes in pain during rehabilitation. A 2-cm or greater change in VAS score for usual or worst knee pain in the past week represents a clinically meaningful difference.27 SOR: B
-
10.
Clinicians should use patient-reported outcome measures, such as the Anterior Knee Pain Scale (AKPS) or the Lower Extremity Functional Scale (LEFS), to assess function in individuals with PFP. For the AKPS, a 10-point or greater change represents the minimal clinically important difference.27 For the LEFS, an 8-point or greater change represents the minimal detectable change.28 SOR: B
Nonsurgical Treatment
-
11.
Due to the complexity of managing PFP, clinicians should develop and implement a multimodal plan of care. The plan of care should include gluteal- and quadriceps-strengthening exercises, patient education (ie, contributing factors, importance of exercise, rehabilitation expectations), and activity modification.29 Individuals with PFP who complete an 8-week gluteal-strengthening program reported greater improvements in pain and health status 6 months after completing rehabilitation compared with those who completed an 8-week quadriceps-strengthening program.30–32 SOR: A
-
12.
For individuals with PFP, clinicians should prescribe an initial 3-week program of isolated gluteal-strengthening exercises before a program of quadriceps-strengthening exercises.31–41 SOR: B
-
13.
Clinicians should prescribe interventions that address trunk-muscle (eg, abdominal oblique, rectus abdominis, transversus abdominis, erector spinae, and multifidi) control and capacity in individuals with PFP.31,32,36,40,41 SOR: A
-
14.
To minimize patellofemoral joint stress, patients should perform nonweight-bearing quadriceps exercises between 45° and 90° of knee flexion and weight-bearing quadriceps exercises between 0° and 45° of knee flexion.42–44 SOR: C
-
15.
Patellar taping appears to be beneficial if it enables patients with PFP to exercise in a pain-free manner.29,45,46 SOR: B
-
16.
Movement-retraining programs that incorporate either real-time visual or auditory feedback can benefit individuals with altered lower extremity gait mechanics such as excessive hip adduction or hip internal rotation or increased knee valgus (or a combination of these).47,48 SOR: A
-
17.
Movement retraining that emphasizes keeping the pelvis level and the knees facing forward during dynamic activities has been beneficial for females with PFP. Providing visual and verbal feedback to the patient about keeping the pelvis level and knees facing forward appears to be an important component of this training.49,50 SOR: B
-
18.
Foot orthoses as an adjunct intervention in combination with other treatment strategies provide some benefit to patients with PFP.45 SOR: B
-
19.
Forms of electrotherapy including therapeutic ultrasound and low-level laser therapy have shown limited effectiveness in the management of PFP.51–58 SOR: B
Surgical Treatment
-
20.
Referral for surgical intervention should be considered only if an individual with PFP presents with either evident lateral patellar compression or patellar instability and has failed to improve despite exhaustive rehabilitation attempts.59–63 SOR: A
-
21.
Lateral retinacular release or lengthening can benefit individuals with PFP who present with excessive lateral patellar tilting but no patellar instability or grade III–IV articular cartilage changes.59–61,64,65 SOR: B
-
22.
Patellofemoral joint realignment procedures, such as the Fulkerson osteotomy, can benefit individuals with PFP and patellar instability.62,66–68 SOR: B
BACKGROUND AND LITERATURE REVIEW
Risk Factors
Although PFP is a common knee problem among physically active individuals, its causes have remained elusive. Dye et al69 characterized PFP as the “black hole of orthopaedics” because of its poorly identified causative factors. They believed that PFP resulted from irritation of innervated structures of the patellofemoral joint (eg, inflamed synovial and fat pad tissues) as a result of excessive joint loading.70 This theory has led to the identification of factors that can lead to increased patellofemoral joint loading, such as (1) altered lower extremity kinematics and kinetics, (2) decreased muscle strength and neuromuscular recruitment, (3) faulty structural alignment, and (4) reduced flexibility.
A limitation of many studies has been the use of retrospective data, which cannot distinguish between cause and effect.15 Although retrospective data can identify impairments to address during rehabilitation, these problems did not necessarily exist before the onset of PFP. For example, individuals with PFP responded favorably to gluteal muscle-strengthening exercises30,71; however, gluteal muscle weakness was not a risk factor.5,20 To better understand the causes of PFP, this literature review includes only findings from investigations that prospectively followed otherwise healthy individuals who eventually developed PFP.
Lower Extremity Kinematics.
Altered lower extremity movement patterns have been theorized to contribute to PFP. The term dynamic Q-angle describes the negative effect of altered lower extremity kinematics on the patellofemoral joint.72 Briefly, the Q-angle represents the resultant lateral pull of the patella and is the angle formed by 1 line drawn from the anterior-superior iliac spine to the midpatella and a second line drawn from the midpatella to the tibial tuberosity. Excessive hip adduction or internal rotation (or both) place the patella in a more medial position relative to the anterior-superior iliac spine, resulting in an increased dynamic Q-angle. Increased tibial external rotation and knee abduction place the tibial tubercle in a more lateral position relative to the patella, which also increases the Q-angle. Together, these motions can increase the laterally directed forces on the patella, leading to lateral patellofemoral joint compression and pain.73–75
To date, limited and conflicting data exist regarding an association between altered lower extremity kinematics and an increased risk of developing PFP. Inconsistent findings may reflect differences in the patient populations studied and the tasks used to assess kinematics. From a systematic review of 7 articles with meta-analysis, Pappas and Wong-Tom21 concluded that additional prospective studies were needed to better understand the risk factors associated with PFP. However, they stated that excessive knee abduction during landing tasks may contribute to the onset of PFP. Boling et al5 reported that military recruits who developed PFP demonstrated, on average, 76° ± 12° of peak knee flexion and 8° ± 9° of peak hip internal rotation during a jump landing. Participants who did not develop PFP exhibited, on average, 81° ± 14° and 7° ± 8° of peak knee flexion and hip internal rotation, respectively. Although all participants displayed similar peak hip internal rotation, the combined effect of hip internal rotation and less knee flexion could lead to increased lateral patellofemoral contact pressure.5 Myer et al76 investigated frontal-plane knee motion (eg, knee abduction) in younger female basketball players (mean age = 13.4 years) during a similar task but did not identify it as a risk factor for PFP. This finding suggested that, among younger females, different risk factors could contribute to PFP onset.77 Noehren et al15 prospectively followed a cohort of pain-free female runners over a 2-year period. Compared with those who remained asymptomatic and demonstrated 8° ± 5° of hip adduction during the stance phase of running, the individuals who eventually developed PFP demonstrated 12° ± 3° of hip adduction. However, with respect to rear-foot eversion angle, no between-groups differences existed. These results provided additional information that the PFP onset may be more attributable to altered hip kinematics than to foot kinematics.
In summary, out-of-plane motions such as hip adduction and internal rotation can increase lateral patellofemoral joint loading78,79 and most likely contribute to the onset of PFP. The relationship between sagittal-plane and out-of-plane motions also deserves further study.76 It is important to note that activities such as basketball and long-distance running may result in different patterns of altered kinematics.76 Future investigators should examine hip and knee kinematics across different activities and age groups.77,80
Lower Extremity Kinetics.
Patellofemoral pain is theorized to result from increased patellofemoral joint stress, defined as force per unit area (ie, quadriceps force applied per unit of patellofemoral joint contact area).70,81 As explained in the “Lower Extremity Kinematics” section, an increased dynamic Q-angle leads to abnormal lateral patellofemoral joint stress.72,82 Increased stress may also occur from the repetitive quadriceps force produced during running and jumping activities. For example, ground reaction forces generated during the landing phase of running and jumping cause the knee to move into flexion and abduction.78,83 In response to the ground reaction force, the quadriceps generates force to control these knee motions. If sufficient, the cumulative effect of quadriceps force generation could lead to increased patellofemoral stress and pain.70 This theory has led to research directed at understanding the role of altered lower extremity kinetics (ie, forces) in PFP onset.
Stefanyshyn et al16 assessed knee kinetics during the stance phase of running and prospectively followed these individuals over a 6-month period. Runners who developed PFP generated 19% higher knee-abduction impulses during the stance phase of running than those who remained symptom free. Myer et al17 evaluated knee kinetics during a drop-landing task in middle and high school female basketball players before their competitive season. Those who developed PFP during the season exhibited greater knee-abduction moments during the initial contact phase of the task. Results from both investigations suggested that greater frontal-plane knee loading may contribute to PFP onset.
Thijs et al25,84 examined plantar pressures during running in pain-free novice recreational runners and walking in military recruits. Novice runners who developed PFP generated greater vertical peak forces at the lateral heel and the second and third metatarsals during running.25 Thijs et al84 also found that military recruits who developed PFP walked with the foot in a more supinated position, as evidenced by a pattern of greater lateral foot pressure. The authors concluded that these plantar-pressure patterns could decrease the foot's ability to dampen ground reaction forces, resulting in increased impact loading to the knee and eventual PFP.25 However, a systematic review with meta-analysis18 provided limited evidence of an association between dynamic foot function (ie, plantar pressures) and the risk of developing PFP. Additional prospective studies are needed to better understand the role of dynamic foot function in the onset of PFP.
Lower Extremity Muscle Strength.
Clinically, hip and knee weakness has been identified in individuals with PFP85 and has led to studies of muscle weakness and PFP onset. Decreased gluteal muscle strength may result in increased hip adduction and internal rotation, motions theorized to increase patellofemoral joint stress.72 Quadriceps weakness may contribute to PFP by increasing lateral patellar tracking and patellofemoral joint loading.5,24,86
From a systematic review with meta-analysis of 24 articles, Rathleff et al19 reported moderate-to-strong evidence of no correlation between decreased isometric hip-abductor, external-rotator, and hip-extensor strength and PFP onset. They noted that hip-muscle weakness became evident after PFP developed, suggesting that hip weakness may have arisen from inactivity after symptoms began.
A limitation of prior studies that evaluated hip strength as a predictor of PFP has been little attention to other aspects of muscle performance (eg, muscle endurance and rate of force development).19 Souza and Powers87 found that reduced hip-extension endurance, not isometric strength, was the sole hip-muscle predictor of increased hip internal rotation during running in females with PFP. Although these authors used retrospective data, their findings highlighted the need to examine different strength factors.
Individuals with PFP are known to exhibit hip weakness that most likely evolved from inactivity due to pain.19,85,88 More important, those with PFP have reported improvements in pain and function from hip-strengthening exercises.30,71 This trend supports the current thought that isometric hip weakness is a result and not a cause of PFP.19 However, future prospective investigators should assess other aspects of hip strength (eg, isokinetic concentric and eccentric strength) and performance (eg, muscle endurance) to identify additional possible hip influences on PFP.
Researchers5,24,89–91 have also evaluated the isometric strength, isokinetic peak torque, and functional performance of the quadriceps and hamstrings as risk factors for PFP. They identified decreased quadriceps strength but not decreased hamstrings strength as a predictor of PFP. Using handheld dynamometry, Boling et al5 reported that asymptomatic individuals entering the US Naval Academy who developed PFP generated, on average, less isometric quadriceps force (equal to 46% ± 0.09% of body mass compared with 52% ± 0.12% of body mass in those who did not develop PFP) at baseline. Results from 2 meta-analyses21,22 further supported isometric quadriceps weakness as a risk factor. With respect to functional performance, Witvrouw et al24 found that individuals who went on to develop PFP demonstrated smaller vertical jumps at baseline compared with those who did not (52 ± 3.6 cm versus 56 ± 6.3 cm, respectively). Additional prospective studies are needed to provide more data to support the functional performance of the quadriceps and hamstrings as risk factors for the development of PFP.
Neuromuscular Factors.
Another possible contributor to PFP is a delay in activation of the VMO relative to the VL (VMO onset − VL onset). The VMO and VL provide dynamic stabilization to the patella as it tracks in the femoral trochlea.86 Therefore, an imbalance in the onset or activity level (or both) of the VMO relative to the VL could lead to patellar malalignment.92 Witvrouw et al24 observed that individuals who exhibited a delay of 0.31 ± 1.4 milliseconds in VMO activation after patellar tendon tap developed PFP. In a follow-up study, Van Tiggelen et al23 assessed VMO onset − VL onset during the volitional task of rocking back on the heels. Participants who had a 0.67-millisecond or greater delay in VMO onset developed PFP.23 These findings highlighted the importance of altered neuromuscular control as another risk factor.
Structural Alignment.
Lower limb structural alignment may also adversely influence lower limb motion in a way that increases patellofemoral joint loading.73,78 The lower limb alignment variables that have been investigated as risk factors for PFP include static Q-angle,5,24 foot posture index,84 lower leg-heel frontal-plane alignment,24 and heel-to-forefoot frontal-plane alignment.24 To date, no research21,22 has supported any of these static measures as risk factors for PFP. Neal et al26 conducted a systemic review with meta-analysis of 21 articles and reported limited evidence for increased navicular drop as a risk factor. They concluded that other factors, such as altered hip kinematics (which have been associated with the development of PFP5,15) in combination with increased navicular drop should be considered. Therefore, the authors of future prospective studies should determine if altered structural alignment combined with other risk factors influences the risk of developing PFP.
Lower Extremity Muscle Flexibility.
Lower extremity muscle tightness (eg, quadriceps, iliotibial band, hamstrings, and gastrocnemius) has been identified in individuals with PFP93,94 and theorized to cause increased patellar compression for the following reasons. First, quadriceps and iliotibial band tightness can compress the patella and promote lateral tracking.94 Second, tightness of the knee flexors, such as the hamstrings and gastrocnemius, can lead to greater quadriceps force being needed to extend the knee. This increase in quadriceps force would be another source of patellar compression. To date, only Witvrouw et al24 have described decreased quadriceps flexibility as a risk factor for the development of PFP. Additional prospective studies are needed to better understand the influence of tightness of other lower extremity muscles on the onset of PFP.
Suggestions for Future Investigations.
Although researchers have sought to identify PFP risk factors, many more prospective investigations are needed. Patellofemoral pain is a multifactorial problem with no single contributory factor.24,92 At this time, the common link among prospective study findings is that excessive patellofemoral joint loading contributes to PFP onset. Based on our literature review, combined altered kinematics (eg, decreased knee flexion and increased hip adduction and internal rotation during running and landing activities) and kinetics (eg, increased knee-abduction moments) are likely causative factors. Therefore, investigators should examine a combination of biomechanical factors to identify a risk profile for developing PFP. Isometric hip weakness has not been shown to be a risk factor, yet retrospective data87 have revealed associations between other aspects of hip-muscle function and PFP. This finding highlights the need to determine if reduced hip-muscle concentric and eccentric strength, functional performance, and endurance lead to PFP. Identifying potential risk factors among males and females, individuals participating in a sport-specific activity, and adolescents may provide further insight.80 Finally, PFP is a chronic problem.9,11 Therefore, certain psychological (eg, coping strategies, fear-avoidance beliefs95) and pain-perception (eg, central sensitization) factors may play roles and deserve attention.13
Pain and Functional Outcome Measures
Appropriate pain and functional outcome measures are needed to help determine if an individual with PFP receiving treatment is responding in a clinically meaningful manner.13 Common measures used to assess pain and function in patients with PFP include a 10-cm VAS, the AKPS, the LEFS, the Functional Index Questionnaire, and the global rating of change. Crossley et al27 examined the test-retest reliability, validity, and responsiveness of all these measures except the LEFS for this patient population. The 10-cm VAS for usual and worst pain in the past week and the AKPS represented reliable and valid measures of pain and function in individuals with PFP. Also, each measure was responsive, meaning that a change could show either an improvement in or worsening (ie, sensitivity to change28) of pain and function. The minimal clinically important difference, defined as the smallest change in a score that is clinically meaningful for a patient,96 was ≥2 cm on the VAS for pain and ≥10 points on the AKPS score for function.27
The LEFS, another popular functional outcome measure, may be an equally reliable and responsive measure for individuals with PFP. Watson et al28 reported excellent reliability and responsiveness for this scale. Unlike Crossley et al,27 they calculated the minimal detectable change. Although similar to the minimal clinically important difference, the minimal detectable change represents the smallest change not attributable to measurement error.28 The minimal detectable change for the LEFS was 8 points.
In summary, clinicians should consider a ≥2-cm change in the VAS score for usual and worst pain in the prior week clinically meaningful. A ≥10-point change in the AKPS score can be useful to identify a clinically meaningful change in function. It is noteworthy that the 8-point minimal detectable change for the LEFS suggests it is a slightly more responsive measure of change than the AKPS. Therefore, clinicians should use the LEFS to identify more subtle functional changes.28
Nonsurgical Treatment
Due to its multifactorial causes, PFP is one of the most difficult knee problems to manage.13 To date, an overwhelming amount of evidence exists for the use of nonsurgical treatment and the need to develop and implement treatment strategies based on an individual's body function and structural impairments, activity limitations, and participation restrictions.29,97,98 It cannot be overemphasized that a one-size-fits-all treatment approach is not recommended for this patient population.29,45
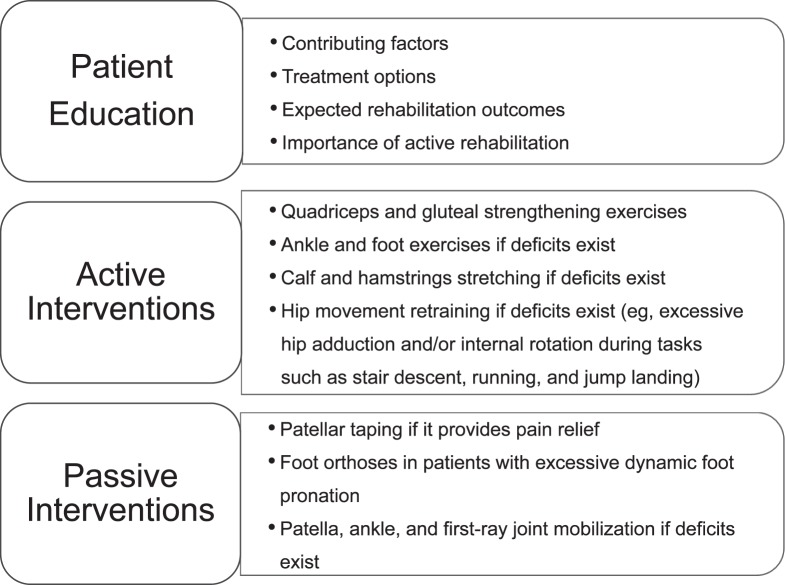
A multimodal intervention allows for the integration of various treatment strategies based on examination findings. Common components of a multimodal intervention are patient education, active interventions, and passive interventions (Figure).29 In the next section, we will summarize the available evidence supporting a multimodal intervention. A given component of a multimodal intervention (eg, knee and hip strengthening) offers the opportunity to present more evidence for a specific treatment strategy within the component (eg, weight-bearing versus nonweight-bearing quadriceps exercises). Therefore, subsequent subheadings within this section will provide evidence for the use of strategies within a specific component. This information serves as an evidence-based guide that the clinician may use when developing and implementing an individually tailored, evidence-based PFP rehabilitation program.
Figure.
Summary of “Best Practice Guide for the Conservative Management of Patellofemoral Pain.”29
Multimodal Intervention
Crossley et al99 were among the first researchers to conduct a multicenter, randomized, double-blinded, placebo-controlled trial examining the benefits of a multimodal intervention for the treatment of PFP. Participants in the treatment group pursued a program of knee and hip exercises, patellar mobilization, corrective taping, and lower extremity stretching. Participants in the placebo group donned loosely applied tape (ie, tape with no therapeutic application), received sham ultrasound, and applied a nontherapeutic gel to the knee. At the end of the 6-week intervention period, the treatment group reported greater and clinically meaningful improvements in VAS for usual (3.5-cm decrease) and worst (4-cm decrease) pain and AKPS (18-point change) scores than controls. This study's use of a true control group (ie, participants who received a placebo treatment) supplied a high level of evidence for multimodal interventions.
Collins et al100 compared the effects of multimodal physical therapy with or without either prefabricated foot orthoses or flat inserts. At the end of 6 weeks, 93% of those who participated in multimodal physical therapy and 90% of those who participated in multimodal physical therapy plus foot orthoses reported treatment success (defined as moderately or markedly improved on a 5-point Likert scale of global effect). At 12 months, participants who received multimodal physical therapy with or without foot orthoses had at least a 2.0-cm improvement in worst pain on the VAS, a 10-point improvement on the AKPS, and a 2-point improvement on the Functional Index Questionnaire. All these changes represented clinically meaningful improvements.
These results suggested that the addition of foot orthoses provided no further benefit beyond that of multimodal physical therapy. However, participants who wore foot orthoses reported improvements at the 1-year follow-up. As discussed later in the “Prophylactic Equipment and Physical Agents” section, individuals with increased midfoot mobility may benefit from foot orthoses as part of a multimodal strategy.101 Therefore, a possible limitation of the Collins et al100 study was the use of foot orthoses without regard for foot mobility. Future authors should examine the benefits of multimodal physical therapy and foot orthoses for individuals with PFP and excessive midfoot mobility.
Rathleff et al77 conducted a systematic review to examine the benefits of multimodal interventions based on investigations with a minimum of 1-year follow-up data. They concluded that exercises designed to improve hip and knee strength and neuromuscular control were the best intervention options. Interestingly, this systematic review included outcomes for adolescents,102 38% of whom responded favorably to a multimodal intervention, a smaller percentage than among adults (62%103 and 81%100). The researchers11 determined that adolescents presented with a longer duration of pain, a factor suggestive of a poor prognosis. More importantly, findings from this review highlighted the need to understand PFP in adolescents, who may not have the same underlying condition as adults and may benefit from different intervention strategies.77 At this time, much work is needed regarding the etiology and management of PFP in children and adolescents.80
Although peer-reviewed evidence has been valuable for identifying important intervention strategies, knowledge gained from clinical experience may be equally useful. Barton et al29 performed a systematic review of interventions for PFP and integrated interview data from clinicians and researchers considered experts in this field. This study was unique because its overarching purpose was to integrate findings from the scientific literature into clinical decision making. The interviewers queried respondents on their clinical reasoning, impression of the body of literature, and the need for future research. Best practices for the treatment of PFP were patient education, active interventions, and passive interventions (Figure). Their “Best Practice Guide to Conservative Management of Patellofemoral Pain” highlighted that many treatment strategies may benefit this patient population. Most important, clinicians should do their best to develop and implement individually tailored interventions based on each patient's presentation. The following sections provide information on various intervention strategies that a clinician may (or may not, depending on the patient's presentation) consider using when developing and implementing a multimodal intervention for individuals with PFP.
Therapeutic Exercise
Quadriceps Strengthening.
Quadriceps strengthening has long been considered the mainstay of treatment for individuals with PFP.104 Clinicians have prescribed these exercises based on the theory that quadriceps weakness105 or delayed VM activation (or both) relative to the VL106,107 can lead to abnormal patellar tracking and lateral patellofemoral joint compression. Furthermore, patients with PFP have responded favorably to quadriceps exercises.104,108–110
Individuals with PFP must perform quadriceps-strengthening exercises in a pain-free manner, one that reduces the amount of patellofemoral joint stress (quadriceps force per patellar contact area on the femur) and resultant pain.29,44 Powers et al43 found differences in patellofemoral joint stress during nonweight-bearing and weight-bearing quadriceps exercises. During nonweight-bearing knee-extension exercises, the quadriceps must generate greater force as the knee moves from 90° to 0° of flexion.83 As the knee approaches full extension, the patella has less contact within the femoral trochlea, leading to increased patellofemoral joint stress.42,43
The opposite effect occurs during weight-bearing knee extension, when the quadriceps generates less force as it extends the knee from 90° to 0° of flexion. Although the patella has less femoral contact area as it approaches full knee extension, less quadriceps force is required.83,111 The relatively greater decrease in quadriceps force compared with patellar contact results in less overall patellofemoral stress.42,43 Understanding these biomechanical principles is critical to promoting pain-free quadriceps exercises.
Nonweight-Bearing Quadriceps-Strengthening Exercises.
Clinicians have prescribed isometric quadriceps contraction setting and straight-leg–raise exercises to address quadriceps weakness, an approach shown to reduce pain and improve quadriceps strength.112–115 However, a significant limitation has been their relatively isometric nature and strengthening focused on a single point in the knee's range of motion.
Isokinetic exercise allows controlled movement speed within a specific arc of motion. Hazneci et al116 and Alaca et al117 prescribed a 6-week isokinetic quadriceps program at speeds of 60°/s and 180°/s. Patients displayed an average 2.4-cm improvement in VAS scores116,117 after the training.116,117 Limitations of isokinetic exercise have been equipment cost and availability.
Weight-Bearing Quadriceps-Strengthening Exercises.
Clinicians also prescribe weight-bearing exercises because they better simulate greater quadriceps eccentric loading during functional activities.44 In addition, weight-bearing exercises enable individuals to target the quadriceps in lesser degrees of knee flexion while minimizing overall patellofemoral joint stress.42,43 Because individuals with PFP demonstrated both hip85 and quadriceps21,22 weakness, weight-bearing exercise allows for the activation of multiple muscle groups simultaneously.
Weight-bearing quadriceps exercises (eg, wall slides, lateral step-downs, and mini-squats) have been shown to benefit individuals with PFP. Patients with PFP have demonstrated improvement (2.9-cm decrease) in VAS scores as soon as 4 weeks into a 6-week program.118 Specific nonweight-bearing hip-abductor and external-rotator strengthening exercises provided benefits beyond those gained from weight-bearing quadriceps exercise.35 Participants who completed a 6-week weight-bearing quadriceps program plus isolated nonweight-bearing gluteal-strengthening exercises showed greater decreases (3.2 versus 2.3 cm) in VAS and increases (13.7 versus 8.6 points) in AKPS scores than those who performed only weight-bearing quadriceps exercises.35 In summary, these findings35,118 support the use of both weight-bearing quadriceps exercises and specific nonweight-bearing gluteal-strengthening exercises.
Nonweight-Bearing Versus Weight-Bearing Quadriceps-Strengthening Exercises.
Individuals with PFP have also benefited from exercise programs incorporating both nonweight-bearing and weight-bearing quadriceps exercises.54,57,119,120 For a 5-year period, Witvrouw et al108 prospectively followed patients who had completed a 5-week protocol of either nonweight-bearing or weight-bearing quadriceps exercises. At the end of the follow-up period, all participants, regardless of exercise group, maintained AKPS scores (greater than a 10-point increase from baseline), single-legged triple-jump performance, and isokinetic knee strength similar to those values at the 3-month posttreatment time. This finding suggested that both nonweight-bearing and weight-bearing quadriceps exercises were useful. However, only 20% of all participants were pain free at the 5-year follow up. The fact that 80% had ongoing symptoms agreed with other results3,9 and indicated that a single treatment approach may be insufficient for complete symptom resolution.
In summary, nonweight-bearing and weight-bearing quadriceps-strengthening exercises can benefit individuals with PFP. Clinicians should prescribe nonweight-bearing exercises if the rehabilitation goal is to target the quadriceps; weight-bearing exercises should be used to strengthen the quadriceps in a functional manner. The most important point is that quadriceps exercises be performed in a pain-free manner44,46 and in combination with other treatment strategies (ie, multimodal approach).29
Specific Vastus Medialis Training.
Investigators106,121,122 have also examined the effects of specific VMO training on PFP. Syme et al122 conducted a randomized controlled trial to compare the effects of selective VMO activation, general quadriceps strengthening, and no treatment. All patients who received treatment exhibited similar decreases (greater than 2 cm) in VAS scores, increases in knee flexion during a step-down test, improved McGill Pain Questionnaire scores, and improved Short Form-36 Health Evaluation questionnaire scores. These findings suggested that selective VMO-activation exercise provided no additional benefit over general nonweight-bearing and weight-bearing quadriceps exercises. Historically, data have not supported the ability to selectively activate the VMO during exercise.123 Therefore, any quadriceps exercise capable of reversing muscle inhibition most likely accounted for muscle timing improvements. Generalized quadriceps-based exercises are shown in Table 1.
Table 1.
Sample Exercises Designed to Target the Quadriceps Muscles in Individuals With Patellofemoral Pain
| Study |
Exercise |
Resistance or Repetitions |
| Dolak et al34 | Straight-leg raisesa | 3 × 10 repetitions (progress resistance from 3% to 7% of body mass) |
| Supine knee extension (30° to 0°)a | ||
| Ferber et al32 | Standing terminal knee extensionb | 3 × 10 repetitions |
| Wall slide (45° knee extension) | 3 repetitions (progress hold time from 30 to 60 s and excursion to 90°) | |
| Single-legged squat (0° to 45°) | 3 × 10 repetitions (progress to 15 repetitions and excursion to 90°) | |
| Fukuda et al38 | Seated knee extension (90° to 45°)a | 3 × 10 repetitions (70% of 1-repetition maximum) |
| Seated leg press (0° to 45°) | 3 × 10 repetitions (70% of 1-repetition maximum) | |
| Herrington and Al-Sherhi124 | Seated knee extension (90° to 0°)a | Determined using the daily adjustable progressive resistance exercise program |
| Seated leg press (0° to 90°) | ||
| Khayambashi et al31 | Seated knee extension (30° to 0°)b | 3 × 20–25-repetition progressionc |
| Standing mini-squats (30° to 0°)b | 3 × 20–25-repetition progressionc | |
| Song et al121 | Unilateral seated leg press (0° to 45°) | 5 × 10 repetitions (60% of 1-repetition maximum) |
Cuff weight resistance.
Elastic band resistance (all used a progression of elastic band resistance).
Number of repetitions varied depending on the sets performed for a given level of resistance within a single bout of exercise.
Quadriceps Strengthening With Biofeedback.
Biofeedback represents another means of facilitating VMO activation. Researchers55–57 have compared changes in PFP using visual feedback (eg, electromyography biofeedback) during quadriceps exercises. Although a popular treatment strategy, biofeedback for enhanced quadriceps activation during exercise provided no more pain relief than quadriceps exercises alone.45,58
Hip and Trunk Strengthening.
Powers72,78 theorized that faulty hip kinematics, such as increased adduction and internal rotation, may increase laterally directed forces at the patellofemoral joint (as discussed in the “Lower Extremity Kinematics” subheading in the “Risk Factors” section). From a clinical standpoint, prescribing a combination of hip- and traditional quadriceps-strengthening exercises reduces pain and improves function in individuals with PFP.99,118,119
To better understand the role of the hip and trunk musculature, authors have examined the isolated effects of hip and trunk strengthening. Mascal et al125 were the first to report on the benefits of targeted trunk and hip strengthening. In this case series, they outlined the intervention used for 2 females with PFP who initially demonstrated hip weakness and faulty hip and knee kinematics during a stair-descent maneuver. After completing a 14-week trunk- and hip-focused exercise program, both patients demonstrated improved VAS (preintervention pain = 4/10 and 7/10; postintervention = 0/10 and 2/10, respectively) and AKPS (9- and 14-point improvements) scores and generated greater quadriceps, gluteus maximus, gluteus medius, hip internal-rotator, and hip external-rotator isometric force during strength testing. One participant underwent a biomechanical examination during stair descent and exhibited 4° more hip external rotation and 6.4° less hip adduction after completing the intervention. This result suggested that strength gains transferred to performing stair descent with the hip in a more optimal position, one that reduced the dynamic Q-angle. These findings provided preliminary support for the importance of trunk and hip strengthening in this patient population.
Others have continued to investigate the importance of proximal strengthening. Tyler et al126 examined 35 patients with PFP who performed 6 weeks of nonweight-bearing and weight-bearing hip-strengthening exercises. On average, VAS scores decreased by 2.2 cm. However, the effect of the weight-bearing exercises on quadriceps strength was unclear.
Fukuda et al38 randomized sedentary females with PFP into 1 of the following groups: quadriceps exercises, isolated hip and quadriceps exercises, and control (no intervention). After 4 weeks, patients in both exercise groups had greater improvements in numeric pain-rating scale (NPRS), LEFS, and AKPS scores than the control group. However, only those who performed the additional hip exercises demonstrated clinically meaningful improvements in VAS scores during stair ascent (2.2-cm decrease) and descent (2.6-cm decrease). These findings were consistent with those of other investigators33,35 who reported greater improvements in VAS scores with the addition of hip-abductor and hip external-rotator exercises to a traditional quadriceps-strengthening program. Participants in the quadriceps and isolated hip and quadriceps exercise groups showed improvements in LEFS (10- and 16.6-point increases, respectively) and AKPS (10.2- and 15-point increases, respectively) scores.
Fukuda et al40 also followed their exercise groups at 3, 6, and 12 months postintervention. Those who performed both hip and quadriceps exercises reported continued improvements in NPRS, LEFS, and AKPS scores. Those who performed only quadriceps exercises showed improvement in NPRS scores but not in LEFS and AKPS scores at 6 months. No further changes in these scores occurred between 6 and 12 months. Based on these results, clinicians should develop and implement programs that incorporate both hip- and knee-strengthening exercises.
Khayambashi et al39 examined the effect of an 8-week hip-abductor and external-rotator strengthening program on females with PFP. At the end of the program, patients displayed improvements in the VAS (6.5-cm decrease) and Western Ontario and McMaster Universities (WOMAC) questionnaire scores and greater isometric hip-abductor and external-rotator strength. Ferber et al37 reported improved VAS scores (2.5-cm decrease) and greater hip-abductor isometric strength within 3 weeks among recreational runners with PFP who performed isolated hip-abductor exercises. Together, these findings suggested the potential benefits of isolated hip strengthening for individuals with PFP.
Although evidence45,46,127 supports the importance of hip strengthening, quadriceps-strengthening exercises continue to offer a viable treatment approach. To better understand the relationship between hip and quadriceps exercises, Dolak et al34 initially instructed females with PFP to perform a 4-week program of either an isolated hip (eg, nonweight-bearing hip-abduction and external-rotation resistance exercises) or quadriceps (eg, nonweight-bearing short-arc quadriceps and straight-leg–raise resistance exercises) program. After the initial 4-week protocol, all patients completed an identical 4-week weight-bearing lower extremity strengthening (eg, single-legged balance, lateral step-downs, and lunges) program. Although all participants reported less pain after 8 weeks (2.2- and 1.6-cm decreases for the initial hip- and quadriceps-exercise groups, respectively), only those in the initial hip-exercise group had a clinically meaningful improvement. Regardless of group assignment, LEFS scores increased by 11 points. These data further support the importance of hip-strengthening exercises for patients with PFP.
Earl and Hoch36 instructed patients to perform specific trunk-endurance and isolated hip-strengthening exercises, followed by weight-bearing lower extremity strengthening exercises. As in Dolak et al,34 improvements were noted in both VAS score (3.5-cm decrease) and isometric hip strength. Findings from both investigations34,36 provided preliminary evidence for the benefits of early trunk and hip strengthening. A sample of the exercises used in these investigations is shown in Table 2.
Table 2.
Sample Exercises Designed to Target the Hip and Trunk Muscles in Individuals With Patellofemoral Pain
| Study |
Exercise |
Resistance or Repetitions |
| Dolak et al34 | Side-lying hip abductiona | 3 × 10 repetitions (3% to 7% body weight progression) |
| Seated hip external rotationb | 3 × 10 repetitions (3% to 7% body weight progression) | |
| Isometric combined hip abduction-external rotation in quadruped positionb | 3 × 10 repetitions (3% body weight) | |
| Earl and Hoch36 | Abdominal drawing | 2 × 15 repetitions (10-s hold) |
| Side-lying combined hip abduction-external rotationb | 3 × 10 repetitions (progressed up to 3 × 20 with cuff weight ranging from 2.5–5 lb [1.1–2.3 kg]) | |
| Prone planks | 2 × 15 repetitions (10-s hold) | |
| Side planks | 2 × 15 repetitions (10-s hold) | |
| Fukuda et al38 | Standing hip abductionb | 3 × 10 repetitions (10-repetition maximum) |
| Side-lying hip abductiona | 3 × 10 repetitions (70% of 1-repetition maximum) | |
| Seated hip external rotationb | 3 × 10 repetitions (10-repetition maximum) | |
| Side stepping | 3 × 1 min | |
| Khayambashi et al39 | Standing hip abductionb | 3 × 20–25-repetition progressionc |
| Seated hip external rotationb | 3 × 20–25-repetition progressionc | |
| Nakagawa et al33 | Transversus abdominis contraction in quadruped position | 2 × 15 repetitions (10-s hold) |
| Side-lying combined hip abduction-external rotationb | 2 × 15 repetitions (10-s hold) | |
| Isometric combined hip abduction-external rotation in the quadruped position | 2 × 15 repetitions (10-s hold) | |
| Pelvic drop exercise on a 20-cm (7.9-in) step | 2 × 15 repetitions (10-s hold) |
Cuff weight resistance.
Elastic band resistance (all used a progression of elastic band resistance).
Number of repetitions varied depending on the sets performed for a given level of resistance within a single bout of exercise.
Hip and Trunk Exercises Versus Quadriceps Exercises.
More recent investigators31,32,41 have specifically compared the isolated effects of hip and trunk exercises versus quadriceps exercises for individuals with PFP. Ferber et al32 assessed VAS and AKPS scores in 199 patients with PFP who participated in either a 6-week hip- and core- or quadriceps-exercise intervention. All patients, regardless of group assignment, demonstrated clinically meaningful improvements in VAS (3-cm decrease) and AKPS (11-point increase) scores. Those assigned to the hip and core group displayed a decrease in VAS score at the end of week 3, a week sooner than those in the quadriceps group. Dolak et al34 also found that individuals who initially performed hip exercises improved sooner than those who initially performed quadriceps exercises.
Khayambashi et al31 assessed changes in pain and function in patients who completed a program of either 2 hip or 2 quadriceps exercises using a progression of resistance bands. Those in the hip group performed side-lying hip-abduction and seated hip–external-rotation exercises. Patients in the quadriceps group performed a nonweight-bearing (seated knee extension from 30° to 0° of knee flexion against a resistance band) and a weight-bearing (squat from 30° to 0° of knee flexion against a resistance band) knee-extension exercise. The strengthening exercises were performed during a 20-minute session, 3 times a week for 8 weeks. Although all patients benefited, those in the hip-exercise group exhibited better outcomes with respect to VAS (5.5-cm decrease compared with 3.6-cm decrease for the quadriceps group) and WOMAC scores. At the 6-month follow-up assessment, participants in the hip group maintained their improved VAS scores (0.1-cm decrease from intervention completion to 6-month follow up), while those in the quadriceps group had slightly higher VAS scores (0.7-cm increase from intervention completion to 6-month follow up). These findings were clinically important because they demonstrated that the beneficial effect of prescribing only 2 hip exercises were maintained for at least 6 months.
A limitation of prior investigations31,32,34 has been the inability to determine the effect of strengthening on lower extremity kinematics. Baldon et al41 compared VAS scores and trunk and lower extremity kinematics during a single-legged squat in females with PFP who performed either an 8-week functional-stabilization (eg, trunk-endurance exercise, isolated hip-strengthening exercise, lunges, and single-limb stance on an unstable platform) or a traditional quadriceps-strengthening (eg, leg press, front step-up, wall squat, straight-leg raise, and nonweight-bearing knee-extension) program. Additionally, patients in the functional-stabilization program received education on optimal trunk and hip positions during functional tasks such as a squat. Similar to prior research,31,32,34 all patients benefitted regardless of the intervention, but those who completed the functional-stabilization training had greater improvements in VAS scores (5.2-cm decrease compared with a 3.0-cm decrease for the quadriceps group). Those in the functional-stabilization training group also demonstrated less ipsilateral trunk lean (3.0° decrease) and hip adduction (11.2° decrease) during a single-legged squat after completing the intervention. In a subsequent analysis, Baldon et al128 examined whether the improvement in trunk and hip kinematics resulted from increased hip strength or better motor control. Increased eccentric gluteal-muscle strength accounted for most of the improved frontal-plane kinematics of the trunk and hip during a single-legged squat. These results further support the importance of hip-strengthening exercise in managing patients with PFP.
Movement Retraining.
Researchers49,50,129 have also focused on the importance of movement-pattern modification. Noehren et al49 assessed hip mechanics in 10 female runners with PFP before, immediately after, and 1 month after completing a real-time 2-dimensional kinematic-feedback intervention. Patients ran on a treadmill 4 times a week for 2 weeks. Initially, they ran for 15 minutes and were given real-time visual kinematic feedback to minimize hip adduction. As the duration of the running session increased, the amount of real-time visual kinematic feedback decreased. After 2 weeks, patients exhibited 5.1° less hip peak adduction, 2.5° less peak hip internal rotation, and 2.3° less peak contralateral pelvic drop during the stance phase of running. Importantly, they showed improvements in VAS (4.3-cm decrease) and LEFS (11-point increase) scores. All benefits were maintained at the 1-month follow up.
However, a limitation of the Noehren et al study49 was the use of expensive motion-analysis equipment not conducive to most clinical settings. To address this concern, Willy et al50 sought to identify changes in hip mechanics during running using mirror and verbal feedback. These authors also assessed hip mechanics during a single-legged squat and a step-down task before and after training. After completing the 2-week training program, patients displayed similar improvements in VAS scores (3.2-cm decrease), LEFS scores (9-point increase), and peak hip adduction (5.9° decrease) during running as those in the Noehren et al49 study. They also exhibited 4° and 3.5° less peak hip adduction during a single-legged squat and step-down task, respectively. These findings suggested they were able to transfer the newly acquired skill (ie, less hip adduction during running, suggestive of a smaller dynamic Q-angle) to other functional tasks. Most important, patients maintained the improved VAS and LEFS scores at the 3-month follow-up assessment.
Prophylactic Equipment and Physical Agents
Patellar Taping.
The original premise of patellar taping was that tape could correct patellar positioning and tracking and facilitate VMO activation during dynamic movement. However, evidence130–132 has now suggested that patellar taping does not maintain optimal patellar position after exercise or necessarily facilitate quadriceps neuromuscular activity, although it may promote pain-free quadriceps exercise.46
Callaghan and Selfe133 conducted a systematic review of 5 articles but did not make a conclusive recommendation regarding the use of patellar taping, either with or without exercise. They noted the limited available evidence and the need for higher-quality studies, especially to measure clinically important short-term and long-term outcomes.
Despite conflicting evidence, patellar taping should be considered a treatment strategy. Clinicians with expertise in the management of individuals with PFP recommend taping, at least for an immediate short-term period, if needed for pain relief.29
Patellar Bracing.
Bracing is an alternative to patellar taping. Advantages of bracing include fewer adverse skin reactions and minimal patient education regarding application, yet currently, limited data support its use. Lun et al134 examined the use of a brace specifically designed to minimize lateral patellar movement. Patients were randomized into 1 of the following groups: (1) exercise only, (2) patellar brace only, (3) exercise and brace, and (4) exercise and knee sleeve. At the end of the intervention, all participants, regardless of group assignment, demonstrated minimal improvements (1.6- to 1.9-cm decreases) in VAS scores for pain during sport activity. Regarding pain 1 hour after sport activity, all patients experienced meaningful improvements (2.1- to 2.8-cm decrease) in VAS scores. Interestingly, those who only wore a brace had the greatest improvement (2.8-cm decrease). Although bracing alone was more beneficial in reducing some aspects of pain (eg, pain 1 hour after activity), the difference in VAS score compared with exercise alone was only 0.7 cm. Thus, bracing may play an important role in patients who cannot exercise regularly.134 However, clinicians should consider the cost of bracing because exercise alone can provide similar benefits.
Knee Bracing.
Denton et al135 compared the effect of the additional use of the Protonics knee brace (Protonics Biomechanical Balance Systems, Lincoln, NE) with weight-bearing quadriceps exercise alone. The brace was designed to decrease the quadriceps force needed to extend the knee, thereby reducing patellofemoral stress and facilitating pain-free weight-bearing quadriceps exercise. Patients demonstrated clinically meaningful improvements in AKPS scores (21- and 24-point improvements for exercise alone and exercise with the brace, respectively). Therefore, use of the Protonics brace afforded no significant benefit versus weight-bearing quadriceps exercise alone. Considering the cost of this brace, data do not support its use.
Foot Orthoses.
Results from systematic reviews45,136,137 agreed that the addition of orthoses had no greater benefit than multimodal physical therapy in improving VAS and AKPS scores at the 6-, 12-, and 52-week follow-up periods. However, orthoses should be considered an adjunctive strategy for patients who demonstrate excessive foot pronation during gait.29
Regarding the isolated use of orthoses, Barton et al138 examined the relationships among subjective pain, gait, and orthosis use. Patients initially completed a Likert pain scale and underwent a kinematic evaluation of foot and ankle motion during gait. After wearing orthoses for 12 weeks, those who demonstrated an average of 5° peak rear-foot eversion during gait at baseline reported markedly better pain. Mills et al139 compared changes in self-perceived functional improvement using a global improvement scale (6-point Likert scale) in individuals with PFP who wore orthoses for 6 weeks versus a control group (ie, no treatment). Before the orthoses were prescribed, the researchers measured patients' midfoot widths in nonweight-bearing and weight-bearing positions. At 6 weeks, those who wore the orthoses displayed better global improvement scale scores than controls. Among the patients who wore the orthoses, those who exhibited an 11-mm greater difference between nonweight-bearing and weight-bearing midfoot mobility were more likely to report a successful outcome.
These data138,139 suggested that a certain cohort of individuals with PFP may benefit from orthosis use. Vicenzino et al101 developed a clinical prediction rule for orthosis use with the following variables: (1) age greater than 25 years, (2) height less than 165 cm, (3) worst pain on a VAS less than 53.25 mm, and (4) midfoot width difference >11 mm between nonweight bearing and weight bearing. With 3 variables present, the positive likelihood ratio was 8.8, and the success rate improved from 40% to 86% with orthosis use. In summary, individuals with PFP who have increased overall foot mobility (eg, 5° peak rear-foot eversion during gait138 or increased midfoot mobility101,139) may benefit from foot orthoses as part of a multimodal intervention.29,45
Neuromuscular Electrical Stimulation.
Inhibition of the VMO may contribute to PFP,54 which has prompted the use of neuromuscular electrical stimulation (NMES) to facilitate VMO activity. Callaghan et al52,53 specifically examined the isolated effect of NMES on individuals with PFP. Their patients received NMES over a 6-week period and demonstrated improvements in quadriceps isometric and isokinetic strength, quadriceps endurance, and step-test performance (number of times the person could step up and down from a 25-cm step without pain). However, the VAS (1.5-cm or less decrease) and AKPS (7.8-point or less increase) score changes were not clinically meaningful and do not support the isolated use of NMES.
Bily et al54 investigated the potential additional benefits gained from the use of NMES with exercise. Patients in the first group performed nonweight-bearing and weight-bearing quadriceps exercises. Those in the second group performed identical exercises as the first but also received two 20-minute sessions of NMES every day. All patients demonstrated similar improvements in VAS scores at the 12-week (4.0- and 4.1-cm decreases for the exercise-only and exercise-plus-NMES groups, respectively) and 52-week (4.9- and 3.8-cm decreases for the exercise-only and exercise-plus-NMES groups, respectively) follow-ups compared with baseline. Although participants who received exercise plus NMES had a greater improvement (16-point increase) in AKPS score than those in the exercise-only group (7-point increase) from baseline at 12 weeks, all had similar total AKPS scores (95/100 and 94/100 points for the exercise-only and exercise-plus-NMES groups, respectively) at the 52-week follow-up. Based on these data,52–54 we conclude that NMES use provided minimal, if any, additional benefit over exercise alone. Its use is not recommended for the management of PFP.
Ultrasound, Cryotherapy, Phonophoresis, and Iontophoresis.
Lake and Wofford58 conducted a systematic review to address the effects of physical agents on PFP. They determined that the use of physical agents was no more effective than exercise.
Low-Level Laser Therapy.
Low-level laser therapy, approved for clinical use in the United States since 2002, is an emerging physical agent theorized to modulate tissue healing. Although it is promising for wound and fracture healing, the current evidence does not support its use in those with PFP.51,58 Future investigations are needed to determine its clinical utility.
Surgical Interventions
Nonsurgical management is the preferred treatment approach for PFP.45,109 However, cases arise in which an individual with long-term PFP may consider surgical intervention after exhausting nonsurgical interventions. For this reason, knowledge of the various surgical procedures and postoperative outcomes will facilitate the clinician's role as patient educator.
Lavage and Debridement.
Arthroscopic lavage and debridement is the least invasive surgical intervention. The risks of arthroscopy and lavage are low, but evidence140 has suggested that arthroscopic debridement is no better than conservative treatment in patients with PFP. Kettunen et al141 used the AKPS to compare 5-year outcomes for individuals with chronic PFP who were treated with knee arthroscopy and an 8-week home exercise program with those who only performed the home exercise program. All patients, regardless of intervention, showed meaningful improvements in pain (greater than 2-cm decrease in the VAS scores during stair ambulation and sit-to-stand transfer) and function (16- and 12-point improvements in AKPS scores for those who underwent arthroscopy or exercise only, respectively). No between-groups differences existed in VAS and AKPS scores, which suggested that arthroscopy did not provide any additional long-term benefit over exercise alone.
Lateral Retinacular Release.
Lateral retinacular release (LRR) is another intervention used to address the tight lateral retinacular structures thought to contribute to PFP. The decision to perform an LRR requires special attention to the pain source, which may originate from excessive lateral patellar compression, lateral patellar instability, or articular cartilage damage. Panni et al60 evaluated changes in Lysholm scores at a minimum 5-year follow-up period (range = 5–12 years) in patients who underwent LRR for either excessive lateral patellar compression or patellar instability. Although all patients reported significant improvements, 70% of those with excessive lateral patellar compression described satisfactory results, compared with 50% of those with patellar instability or significant articular cartilage damage (or both). These findings agreed with the results of others59,61,64,65 who recommended LRR for patients with PFP resulting from excessive lateral patellar tilting and no evident patellar instability or grade III or IV articular cartilage changes.
Lateral Retinacular Lengthening.
A potential complication after LRR is the development of medial patellar instability, leading some surgeons to perform lateral retinacular lengthening (LRL). The rationale is to reduce tension in the lateral retinaculum or reduce articular cartilage loading resulting from the tight lateral structures (or both) by lengthening the tissues rather than releasing them altogether.
Pagenstert et al61 prospectively followed patients over a 2-year period to compare outcomes in those with excessive lateral patellar compression but no instability who underwent open LRR or open LRL. Patients who underwent open LRL demonstrated higher Lysholm scores and experienced no medial patellar subluxation. They also exhibited less quadriceps atrophy (defined as a ≥2-cm difference in quadriceps girth) than those who underwent LRR. These findings provided preliminary evidence for the superiority of open LRL for patients with lateral patellar compression.
Realignment Procedures.
In some patients, joint or limb malalignment cannot be corrected by functional training. Therefore, an osteotomy may be considered to reduce overall patellofemoral stress (force per unit surface area83) via structural realignment. A wide variety of osteotomies have been promoted, and a thorough discussion is beyond the scope of this position statement. However, their overarching goal is to reposition the patella with respect to the femur or to reposition the patella in the trochlear groove. The specific objective is to balance or redirect forces acting at the patellofemoral articulation during active knee extension.
Laboratory testing has shown that surgery, at best, may reduce the overall magnitude of forces applied via the quadriceps to the patella. Using a cadaveric model, Ferguson et al142 measured patellar stress after elevating the patellar tendon via tibial tubercle displacement. They reported that 0.5 in (1.3 cm) of tendon elevation resulted in decreased contact stress. Elevation beyond this amount afforded little additional benefit.
Surgical realignment has been useful for redistributing rather than reducing patellofemoral joint forces. Force redistribution may be achieved by realigning the forces acting on the joint, increasing the contact area, or both. This relationship has led to procedures that involve anteromedialization (AMZ) of the tibial tuberosity, also known as the Becker or Fulkerson osteotomy. Beck et al143 used a cadaveric model to measure changes in patellar contact pressure after AMZ. They found that AMZ of the tibial tubercle effectively shifted patellofemoral joint loading to a more proximal and medial aspect of the trochlea. They concluded that this change would reduce overall lateral patellofemoral joint stress and may benefit individuals with PFP.
Long-term investigations after AMZ have supported its use in a cohort of individuals with PFP. Dantas et al62 reported improvements in average Lysholm scores from 63.3 to 98 at 52 months after AMZ. They also noted that patients with patellar instability but no significant articular cartilage changes were more likely to benefit from AMZ. Karamehmetoglu et al63 reported similar favorable outcomes. They followed 18 patients (21 knees) an average of 28 months after AMZ and observed that 85.7% of patients reported good to excellent results.
CONCLUSIONS
Although PFP is one of the most common lower extremity diagnoses experienced by active individuals, it continues to be among the most challenging to manage. A multifactorial problem, PFP has numerous causes resulting from irritation of innervated patellofemoral joint structures.70,144 However, a common theme is that excessive patellofemoral joint loading not only leads to PFP but must be minimized during rehabilitation.
From a biomechanical standpoint, repetitive out-of-plane motions from the hip (adduction and internal rotation) and knee (abduction) lead to increased patellofemoral joint loading.17,78 From a neuromuscular standpoint, quadriceps weakness and tightness are other sources of abnormal joint loading.5,24 Identifying these risk factors can provide a framework for advancing the development and implementation of prevention programs.
To date, the only recommendation for a PFP prevention program is to include lower extremity stretching and weight-bearing quadriceps-strengthening exercises.145 This finding is limited in scope but corroborates well with the information in this position statement describing quadriceps weakness and tightness as risk factors. However, addressing mechanical risk factors involving the hip and knee during running and landing activities may benefit a prevention program. Future studies are needed to make this determination.
Regarding rehabilitation, a multimodal approach with a particular emphasis on active interventions is recommended.29 Early hip-strengthening exercise appears to be an important component and should be combined with pain-free quadriceps exercises and movement retraining.48,71,127 The key consideration is that exercise should not cause further patellofemoral joint irritation. Although not indicated for all patients, a certain cohort may benefit from passive interventions such as patellar taping and foot orthoses.29,101,139 These recommendations highlight the ongoing need to identify patient subgroups who may benefit from targeted interventions and further advance our knowledge for managing this common, yet complex knee problem.97,146
ACKNOWLEDGMENTS
We gratefully acknowledge the efforts of Michael J. Callaghan, PhD, MPhil, MCSP; Natalie Collins, PhD; Stephen D. Halverson, MA, LAT, ATC, CSCS; Karrie Hamstra-Wright, PhD, ATC; Brian Noehren, PhD, PT, FACSM; and the Pronouncements Committee in the preparation of this document.
FINANCIAL DISCLOSURES
Lori A. Bolgla, PhD, PT, MAcc, ATC; Michelle C. Boling, PhD, LAT, ATC; Kimberly L. Mace, DAT, ATC; and Michael J. DiStefano, MA, ATC, PES, CSCS have no disclosures to report.
Donald C. Fithian, MD is a consultant for Breg, Inc (Carlsbad, CA).
Christopher M. Powers, PhD, PT, FACSM, FAPTA, has a license agreement with DJ Orthopedics (DJO Global, Vista, CA) and is on the Scientific Advisory Board for Alter G, Inc (Fremont, CA).
DISCLAIMER
The NATA and NATA Foundation publish position statements as a service to promote the awareness of certain issues to their members. The information contained in the position statement is neither exhaustive nor exclusive to all circumstances or individuals. Variables such as institutional human resource guidelines, state or federal statutes, rules, or regulations, as well as regional environmental conditions, may impact the relevance and implementation of those recommendations. The NATA and NATA Foundation advise members and others to carefully and independently consider each of the recommendations (including the applicability of same to any particular circumstance or individual). The position statement should not be relied upon as an independent basis for care but rather as a resource available to NATA members or others. Moreover, no opinion is expressed herein regarding the quality of care that adheres to or differs from the NATA and NATA Foundation position statements. The NATA and NATA Foundation reserve the right to rescind or modify its position statements at any time.
REFERENCES
- 1.Rathleff MS, Skuldbol SK, Rasch MN, Roos EM, Rasmussen S, Olesen JL. Care-seeking behaviour of adolescents with knee pain: a population-based study among 504 adolescents. BMC Musculoskelet Disord. 2013. 14:225. (Level of evidence [LOE]: 2) [DOI] [PMC free article] [PubMed]
- 2.Wood L, Muller S, Peat G. The epidemiology of patellofemoral disorders in adulthood: a review of routine general practice morbidity recording. Prim Health Care Res Dev. 2011;12(2):157–164. doi: 10.1017/S1463423610000460. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 3.Nimon G, Murray D, Sandow M, Goodfellow J. Natural history of anterior knee pain: a 14- to 20-year follow-up of nonoperative management. J Pediatr Orthop. 1998;18(1):118–122. (LOE: 2) [PubMed] [Google Scholar]
- 4.Molgaard C, Rathleff MS, Simonsen O. Patellofemoral pain syndrome and its association with hip, ankle, and foot function in 16- to 18-year-old high school students: a single-blind case-control study. J Am Podiatr Med Assoc. 2011;101(3):215–222. doi: 10.7547/1010215. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 5.Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108–2116. doi: 10.1177/0363546509337934. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barber Foss KD, Myer GD, Chen SS, Hewett TE. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train. 2012;47(5):519–524. doi: 10.4085/1062-6050-47.5.01. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boling MC, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725–730. doi: 10.1111/j.1600-0838.2009.00996.x. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins NJ, Bierma-Zeinstra SM, Crossley KM, van Linschoten RL, Vicenzino B, van Middelkoop M. Prognostic factors for patellofemoral pain: a multicentre observational analysis. Br J Sports Med. 2013;47(4):227–233. doi: 10.1136/bjsports-2012-091696. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 10.Stathopulu E, Baildam E. Anterior knee pain: a long-term follow-up. Rheumatology (Oxford) 2003;42(2):380–382. doi: 10.1093/rheumatology/keg093. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 11.Lankhorst NE, van Middelkoop M, Crossley KM, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med. 2016;50(14):881–886. doi: 10.1136/bjsports-2015-094664. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 12.Blond L, Hansen L. Patellofemoral pain syndrome in athletes: a 5.7-year retrospective follow-up study of 250 athletes. Acta Orthop Belg. 1998;64(4):393–400. (LOE: 2) [PubMed] [Google Scholar]
- 13.Witvrouw E, Callaghan MJ, Stefanik JJ, et al. Patellofemoral pain: consensus statement from the 3rd International Patellofemoral Pain Research Retreat held in Vancouver, September 2013. Br J Sports Med. 2014;48(6):411–414. doi: 10.1136/bjsports-2014-093450. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 14.Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69(3):548–556. (LOE: 3) [PubMed] [Google Scholar]
- 15.Noehren B, Hamill J, Davis I. Prospective evidence for a hip etiology in patellofemoral pain. Med Sci Sports Exerc. 2013;45(6):1120–1124. doi: 10.1249/MSS.0b013e31828249d2. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 16.Stefanyshyn DJ, Stergiou P, Lun VM, Meeuwisse WH, Worobets JT. Knee angular impulse as a predictor of patellofemoral pain in runners. Am J Sports Med. 2006;34(11):1844–1851. doi: 10.1177/0363546506288753. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Di Stasi SL, Foss KD, Micheli LJ, Hewett TE. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015;49(2):118–122. doi: 10.1136/bjsports-2013-092536. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowling GJ, Murley GS, Munteanu SE, et al. Dynamic foot function as a risk factor for lower limb overuse injury: a systematic review. J Foot Ankle Res. 2014. 7(1):53. (LOE: 2) [DOI] [PMC free article] [PubMed]
- 19.Rathleff MS, Rathleff CR, Crossley KM, Barton CJ. Is hip strength a risk factor for patellofemoral pain? A systematic review and meta-analysis. Br J Sports Med. 2014. 48(14):1088. (LOE: 1) [DOI] [PubMed]
- 20.Herbst KA, KD Barber Foss, Fader L, et al. Hip strength is greater in athletes who subsequently develop patellofemoral pain. Am J Sports Med. 2015;43(11):2747–2752. doi: 10.1177/0363546515599628. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pappas E, Wong-Tom WM. Prospective predictors of patellofemoral pain syndrome: a systematic review with meta-analysis. Sports Health. 2012;4(2):115–120. doi: 10.1177/1941738111432097. (LOE: 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2012;42(2):81–94. doi: 10.2519/jospt.2012.3803. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 23.Van Tiggelen D, Cowan S, Coorevits P, Duvigneaud N, Witvrouw E. Delayed vastus medialis obliquus to vastus lateralis onset timing contributes to the development of patellofemoral pain in previously healthy men: a prospective study. Am J Sports Med. 2009;37(6):1099–1105. doi: 10.1177/0363546508331135. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 24.Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28(4):480–489. doi: 10.1177/03635465000280040701. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 25.Thijs Y, De Clercq D, Roosen P, Witvrouw E. Gait-related intrinsic risk factors for patellofemoral pain in novice recreational runners. Br J Sports Med. 2008;42(6):466–471. doi: 10.1136/bjsm.2008.046649. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 26.Neal BS, Griffiths IB, Dowling GJ, et al. Foot posture as a risk factor for lower limb overuse injury: a systematic review and meta-analysis. J Foot Ankle Res. 2014. 7(1):55. (LOE: 1) [DOI] [PMC free article] [PubMed]
- 27.Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85(5):815–822. doi: 10.1016/s0003-9993(03)00613-0. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 28.Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther. 2005;35(3):136–146. doi: 10.2519/jospt.2005.35.3.136. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 29.Barton CJ, Lack S, Hemmings S, Tufail S, Morrissey D. The ‘Best Practice Guide to Conservative Management of Patellofemoral Pain': incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med. 2015;49(14):923–934. doi: 10.1136/bjsports-2014-093637. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 30.Peters JS, Tyson NL. Proximal exercises are effective in treating patellofemoral pain syndrome: a systematic review. Int J Sports Phys Ther. 2013;8(5):689–700. (LOE: 2) [PMC free article] [PubMed] [Google Scholar]
- 31.Khayambashi K, Fallah A, Movahedi A, Bagwell J, Powers C. Posterolateral hip muscle strengthening versus quadriceps strengthening for patellofemoral pain: a comparative control trial. Arch Phys Med Rehabil. 2014;95(5):900–907. doi: 10.1016/j.apmr.2013.12.022. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 32.Ferber R, Bolgla LA, Earl-Boehm JE, Emery CA, Hamstra-Wright KL. Strengthening of the hip and core versus knee-muscles for the treatment of patellofemoral pain: a multicentre randomized controlled trial. J Athl Train. 2015;50(4):366–377. doi: 10.4085/1062-6050-49.3.70. (LOE: 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakagawa TH, Muniz TB, de Marche Baldon R, Dias Maciel C, de Menezes Reiff RB, Serrao FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22(12):1051–1060. doi: 10.1177/0269215508095357. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 34.Dolak KL, Silkman C, Medina McKeon J, Hosey RG, Latterman C, Uhl TL. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41(8):560–570. doi: 10.2519/jospt.2011.3499. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 35.Ismail MM, Gamaleldein MH, Hassa KA. Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. Eur J Phys Rehabil Med. 2013;49(5):687–698. (LOE: 2) [PubMed] [Google Scholar]
- 36.Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39(1):154–163. doi: 10.1177/0363546510379967. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 37.Ferber R, Kendall KD, Farr L. Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train. 2011;46(2):142–149. doi: 10.4085/1062-6050-46.2.142. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fukuda TY, Rossetto FM, Magalhães E, Bryk FF, Lucareli PR, de Almeida Aparecida Carvalho N. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40(11):736–742. doi: 10.2519/jospt.2010.3246. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 39.Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42(1):22–29. doi: 10.2519/jospt.2012.3704. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 40.Fukuda TY, Melo WP, Zaffalon BM, et al. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. J Orthop Sports Phys Ther. 2012;42(10):823–830. doi: 10.2519/jospt.2012.4184. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 41.Baldon Rde M, Serrao FV, Scattone Silva R, Piva SR. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(4):240–A8. doi: 10.2519/jospt.2014.4940. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 42.Steinkamp LA, Dillingham MF, Markel MD, Hill JA, Kaufmen KR. Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med. 1993;21(3):438–444. doi: 10.1177/036354659302100319. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 43.Powers CM, Ho KY, Chen YJ, Souza RB, Farrokhi S. Patellofemoral joint stress during weight-bearing and non-weight-bearing quadriceps exercises. J Orthop Sports Phys Ther. 2014;44(5):320–327. doi: 10.2519/jospt.2014.4936. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 44.Bolgla LA, Malone TR. Exercise prescription and patellofemoral pain: evidence for rehabilitation. J Sport Rehabil. 2005;14(1):72–88. doi: 10.1123/jsr.17.1.1. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 45.Collins NJ, Bisset LM, Crossley KM, Vicenzino B. Efficacy of nonsurgical interventions for anterior knee pain: systematic review and meta-analysis of randomized trials. Sports Med. 2012;42(1):31–49. doi: 10.2165/11594460-000000000-00000. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 46.Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther. 2011;6(2):112–125. (LOE: 2) [PMC free article] [PubMed] [Google Scholar]
- 47.Napier C, Cochrane CK, Taunton JE, Hunt MA. Gait modifications to change lower extremity gait biomechanics in runners: a systematic review. Br J Sports Med. 2015;49(21):1382–1388. doi: 10.1136/bjsports-2014-094393. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 48.Agresta C, Brown A. Gait retraining for injured and healthy runners using augmented feedback: a systematic literature review. J Orthop Sports Phys Ther. 2015;45(8):576–584. doi: 10.2519/jospt.2015.5823. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 49.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):691–696. doi: 10.1136/bjsm.2009.069112. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 50.Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech (Bristol, Avon) 2012;27(10):1045–1051. doi: 10.1016/j.clinbiomech.2012.07.011. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rogvi-Hansen B, Ellitsgaard N, Funch M, Dall-Jensen M, Prieske J. Low level laser treatment of chondromalacia patellae. Int Orthop. 1991;15(4):359–361. doi: 10.1007/BF00186879. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 52.Callaghan MJ, Oldham JA. Electrical muscle stimulation of the quadriceps in the treatment of patellofemoral pain. Arch Phys Med Rehabil. 2004;85(6):956–962. doi: 10.1016/j.apmr.2003.07.021. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 53.Callaghan MJ, Oldham JA, Winstanley J. A comparison of two types of electrical stimulation of the quadriceps in the treatment of patellofemoral pain syndrome. A pilot study. Clin Rehabil. 2001;15(6):637–646. doi: 10.1191/0269215501cr457oa. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 54.Bily W, Trimmel L, Modlin M, Kaider A, Kern H. Training program and additional electric muscle stimulation for patellofemoral pain syndrome: a pilot study. Arch Phys Med Rehabil. 2008;89(7):1230–1236. doi: 10.1016/j.apmr.2007.10.048. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 55.Yip SL, Ng GY. Biofeedback supplementation to physiotherapy exercise programme for rehabilitation of patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2006;20(12):1050–1057. doi: 10.1177/0269215506071259. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 56.Harrison EI, Sheppard MS, McQuarrie AM. A randomized controlled trial of physical therapy treatment programs in patellofemoral pain syndrome. Physiother Can. 1999;51(2):93–100. (LOE: 1) [Google Scholar]
- 57.Dursun N, Dursun E, Kilic Z. Electromyographic biofeedback-controlled exercise versus conservative care for patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82(12):1692–1695. doi: 10.1053/apmr.2001.26253. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 58.Lake DA, Wofford NH. Effect of therapeutic modalities on patients with patellofemoral pain syndrome: a systematic review. Sports Health. 2011;3(2):182–189. doi: 10.1177/1941738111398583. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Clifton R, Ng CY, Nutton RW. What is the role of lateral retinacular release? J Bone Joint Surg Br. 2010;92(1):1–6. doi: 10.1302/0301-620X.92B1.22909. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 60.Panni AS, Tartarone M, Patricola A, Paxton EW, Fithian DC. Long-term results of lateral retinacular release. Arthroscopy. 2005;21(5):526–531. doi: 10.1016/j.arthro.2005.01.007. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 61.Pagenstert G, Wolf N, Bachmann M, et al. Open lateral patellar retinacular lengthening versus open retinacular release in lateral patellar hypercompression syndrome: a prospective double-blinded comparative study on complications and outcome. Arthroscopy. 2012;28(6):788–797. doi: 10.1016/j.arthro.2011.11.004. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 62.Dantas P, Nunes C, Moreira J, Amaral LB. Antero-medialisation of the tibial tubercle for patellar instability. Int Orthop. 2005;29(6):390–391. doi: 10.1007/s00264-005-0015-5. (LOE: 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Karamehmetoglu M, Ozturkmen Y, Azboy I, Caniklioglu M. Fulkerson osteotomy for the treatment of chronic patellofemoral malalignment. Acta Orthop Traumatol Turc. 2007;41(1):21–30. (LOE: 3) [PubMed] [Google Scholar]
- 64.Iliadis AD, Jaiswal PK, Khan W, Johnstone D. The operative management of patella malalignment. Open Orthop J. 2012;6:327–339. doi: 10.2174/1874325001206010327. (LOE: 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gerbino PG, Zurakowski D, Soto R, Griffin E, Reig TS, Micheli LJ. Long-term functional outcome after lateral patellar retinacular release in adolescents: an observational cohort study with minimum 5-year follow-up. J Pediatr Orthop. 2008;28(1):118–123. doi: 10.1097/bpo.0b013e31815b4dcf. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 66.Dannawi Z, Khanduja V, Palmer CR, El-Zebdeh M. Evaluation of the modified Elmslie-Trillat procedure for patellofemoral dysfunction. Orthopedics. 2010. 33(1):13. (LOE: 3) [DOI] [PubMed]
- 67.Kumar A, Jones S, Bickerstaff DR, Smith TW. Functional evaluation of the modified Elmslie-Trillat procedure for patello-femoral dysfunction. Knee. 2001;8(4):287–292. doi: 10.1016/s0968-0160(01)00105-3. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 68.Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H. Deterioration of long-term clinical results after the Elmslie-Trillat procedure for dislocation of the patella. J Bone Joint Surg Br. 2002;84(6):861–864. doi: 10.1302/0301-620x.84b6.12804. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 69.Dye SF, Staubli HU, Biedert RM, Vaupel GL. The mosaic of pathophysiology causing patellofemoral pain: therapeutic implications. Oper Techniq Sports Med. 1999;7(2):46–54. (LOE: 3) [Google Scholar]
- 70.Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;436:100–110. doi: 10.1097/01.blo.0000172303.74414.7d. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 71.Lack S, Barton C, Sohan O, Crossley K, Morrissey D. Proximal muscle rehabilitation is effective for patellofemoral pain: a systematic review with meta-analysis. Br J Sports Med. 2015;49(21):1365–1376. doi: 10.1136/bjsports-2015-094723. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 72.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 73.Lee TQ, Morris G, Csintalan RP. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33(11):686–693. doi: 10.2519/jospt.2003.33.11.686. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 74.Mizuno Y, Kumagai M, Mattessich SM, et al. Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res. 2001;19(5):834–840. doi: 10.1016/S0736-0266(01)00008-0. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 75.Elias JJ, Cech JA, Weinstein DM, Cosgrea AJ. Reducing the lateral force acting on the patella does not consistently decrease patellofemoral pressures. Am J Sports Med. 2004;32(5):1202–1208. doi: 10.1177/0363546503262167. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 76.Myer GD, Ford KR, Barber-Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010;25(7):700–707. doi: 10.1016/j.clinbiomech.2010.04.001. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rathleff MS, Vicenzino B, Middelkoop M, et al. Patellofemoral pain in adolescence and adulthood: same same, but different? Sports Med. 2015;45(11):1489–1495. doi: 10.1007/s40279-015-0364-1. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 78.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51. doi: 10.2519/jospt.2010.3337. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 79.Souza RB, Draper CE, Fredericson M, Powers CM. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40(5):277–285. doi: 10.2519/jospt.2010.3215. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 80.Crossley KM, van Middelkoop M, Callaghan MJ, Collins NJ, Rathleff MS, Barton CJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester: part 2. Recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions) Br J Sports Med. 2016;50(14):844–852. doi: 10.1136/bjsports-2016-096268. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Farrokhi S, Keyak JH, Powers CM. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: a finite element analysis study. Osteoarthritis Cartilage. 2011;19(3):287–294. doi: 10.1016/j.joca.2010.12.001. (LOE: 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Goodfellow J, Hungerford DS, Zindel M. Patello-femoral joint mechanics and pathology. 1. Functional anatomy of the patello-femoral joint. J Bone Joint Surg Br. 1976;58(3):287–290. doi: 10.1302/0301-620X.58B3.956243. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 83.Neumann DA. Knee. In: Neumann DA, editor. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation 2nd ed. St. Louis, MO: Mosby;; 2010. 520–572. (LOE: 3) [Google Scholar]
- 84.Thijs Y, Van Tiggelen D, Roosen P, De Clercq D, Witvrouw E. A prospective study on gait-related intrinsic risk factors for patellofemoral pain. Clin J Sport Med. 2007;17(6):437–445. doi: 10.1097/JSM.0b013e31815ac44f. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 85.Prins MR, van der Wurff P. Females with patellofemoral pain syndrome have weak hip muscles. A systematic review. Aust J Physiother. 2009;55(1):9–15. doi: 10.1016/s0004-9514(09)70055-8. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 86.McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc Rev. 2007;15(2):95–104. doi: 10.1097/JSA.0b013e318054e35c. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 87.Souza RB, Powers CM. Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009;37(3):579–587. doi: 10.1177/0363546508326711. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 88.Van Cant J, Pineux C, Pitance L, Feipel V. Hip muscle strength and endurance in females with patellofemoral pain: a systematic review with meta-analysis. Int J Sports Phys Ther. 2014;9(5):564–582. (LOE: 1) [PMC free article] [PubMed] [Google Scholar]
- 89.Milgrom C, Finestone A, Eldad A, Shlamkovitch N. Patellofemoral pain caused by overactivity: a prospective study of risk factors in infantry recruits. J Bone Joint Surg Am. 1991;73(7):1041–1043. (LOE: 2) [PubMed] [Google Scholar]
- 90.Duvigneaud N, Bernard E, Stevens V, Witvrouw E, Van Tiggelen D. Isokinetic assessment of patellofemoral pain syndrome: a prospective study in female recruits. Isokin Exerc Sci. 2008;16(4):213–219. (LOE: 2) [Google Scholar]
- 91.Van Tiggelen D, Witvrouw E, Coorevits P, Croisier JL, Roget P. Analysis of isokinetic parameters in the development of anterior knee pain syndrome: a prospective study in a military setting. Isokin Exerc Sci. 2004;12(4):223–228. (LOE: 2) [Google Scholar]
- 92.Witvrouw E, Werner S, Mikkelsen C, Van Tiggelen D, Vanden Berghe L, Cerulli G. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):122–130. doi: 10.1007/s00167-004-0577-6. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 93.Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801. doi: 10.2519/jospt.2005.35.12.793. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 94.Hamstra-Wright KL, Earl-Boehm J, Bolgla L, Emery C, Ferber R. Individuals with patellofemoral pain have less hip flexibility than controls regardless of treatment outcome. Clin J Sport Med. 2017;27(2):97–103. doi: 10.1097/JSM.0000000000000307. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 95.Piva SR, Fitzgerald GK, Irrgang JJ, et al. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90(2):285–295. doi: 10.1016/j.apmr.2008.08.214. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–415. doi: 10.1016/0197-2456(89)90005-6. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 97.Watari R, Kobsar D, Phinyomark A, Osis S, Ferber R. Determination of patellofemoral pain sub-groups and development of a method for predicting treatment outcome using running gait kinematics. Clin Biomech (Bristol, Avon) 2016;38:13–21. doi: 10.1016/j.clinbiomech.2016.08.003. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 98.Selfe J, Callaghan M, Witvrouw E, et al. Targeted interventions for patellofemoral pain syndrome (TIPPS): classification of clinical subgroups. BMJ Open. 2013. 3(9):e003795. (LOE: 3) [DOI] [PMC free article] [PubMed]
- 99.Crossley K, Bennell K, Green S, Cowan S, McConnell J. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30(6):857–865. doi: 10.1177/03635465020300061701. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 100.Collins N, Crossley K, Beller E, Darnell R, McPoil T, Vicenzino B. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Br J Sports Med. 2009;43(3):169–171. doi: 10.1136/bmj.a1735. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 101.Vicenzino B, Collins N, Cleland J, McPoil T. A clinical prediction rule for identifying patients with patellofemoral pain who are likely to benefit from foot orthoses: a preliminary determination. Br J Sports Med. 2010;44(12):862–866. doi: 10.1136/bjsm.2008.052613. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 102.Rathleff MS, Roos EM, Olesen JL, Rasmussen S. Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med. 2015;49(6):406–412. doi: 10.1136/bjsports-2014-093929. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 103.van Linschoten R, van Middelkoop M, Berger MY, et al. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. BMJ. 2009. 339:b4074. (LOE: 1) [DOI] [PMC free article] [PubMed]
- 104.Natri A, Kannus P, Jarvinen M. Which factors predict the long-term outcome in chronic patellofemoral pain syndrome? A 7-yr prospective follow-up study. Med Sci Sports Exerc. 1998;30(11):1572–1577. doi: 10.1097/00005768-199811000-00003. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 105.Powers CM, Perry J, Hsu A, Hislop HJ. Are patellofemoral pain and quadriceps strength associated with locomotor function? Phys Ther. 1997;77(10):1063–1075. doi: 10.1093/ptj/77.10.1063. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 106.Bennell K, Duncan M, Cowan S, McConnell J, Hodges P, Crossley K. Effects of vastus medialis oblique retraining versus general quadriceps strengthening on vasti onset. Med Sci Sports Exerc. 2010;42(5):856–864. doi: 10.1249/MSS.0b013e3181c12771. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 107.Cowan SM, Bennell KL, Hodges PW, Crossley KM, McConnell J. Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82(2):183–189. doi: 10.1053/apmr.2001.19022. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 108.Witvrouw E, Danneels L, van Tiggelen D, Willems TM, Cambier D. Open versus closed kinetic chain exercises in patellofemoral pain: a 5-year prospective randomized study. Am J Sports Med. 2004;32(5):1122–1130. doi: 10.1177/0363546503262187. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 109.Clijsen R, Fuchs J, Taeymans J. Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis. Phys Ther. 2014;94(12):1697–1708. doi: 10.2522/ptj.20130310. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 110.Chiu JK, Wong YM, Yung PS, Ng GY. The effects of quadriceps strengthening on pain, function, and patellofemoral joint contact area in persons with patellofemoral pain. Am J Phys Med Rehabil. 2012;91(2):98–106. doi: 10.1097/PHM.0b013e318228c505. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 111.Bolgla LA, Shaffer SW, Malone TR. Vastus medialis activation during knee extension exercises: evidence for exercise prescription. J Sport Rehabil. 2008;17(1):1–10. doi: 10.1123/jsr.17.1.1. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 112.Roush MB, Sevier TL, Wilson JK, et al. Anterior knee pain: a clinical comparison of rehabilitation methods. Clin J Sport Med. 2000;10(1):22–28. doi: 10.1097/00042752-200001000-00005. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 113.Eburne J, Bannister G. The McConnell regimen versus isometric quadriceps exercises in the management of anterior knee pain. A randomised prospective controlled trial. Knee. 1996;3(3):151–153. (LOE: 2) [Google Scholar]
- 114.Thomee R. A comprehensive treatment approach for patellofemoral pain syndrome in young women. Phys Ther. 1997;77(12):1690–1703. doi: 10.1093/ptj/77.12.1690. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 115.McMullen W, Roncarati A, Koval P. Static and isokinetic treatments of chondromalacia patella: a comparative investigation. J Orthop Sports Phys Ther. 1990;12(6):256–266. doi: 10.2519/jospt.1990.12.6.256. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 116.Hazneci B, Yildiz Y, Sekir U, Atdin T, Kalyon TA. Efficacy of isokinetic exercise on joint position sense and muscle strength in patellofemoral pain syndrome. Am J Phys Med Rehabil. 2005;84(7):521–527. doi: 10.1097/01.phm.0000167682.58210.a7. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 117.Alaca R, Yilmaz B, Goktepe AS, Mohur H, Kalyon TA. Efficacy of isokinetic exercise on functional capacity and pain in patellofemoral pain syndrome. Am J Phys Med Rehabil. 2002;81(11):807–813. doi: 10.1097/00002060-200211000-00002. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 118.Boling MC, Bolgla LA, Mattacola CG, Uhl TL, Hosey RG. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2006;87(11):1428–1435. doi: 10.1016/j.apmr.2006.07.264. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 119.Loudon JK, Gajewski B, Goist-Foley HL, Loudon KL. The effectiveness of exercise in treating patellofemoral-pain syndrome. J Sport Rehabil. 2004;13(4):323–342. (LOE: 2) [Google Scholar]
- 120.Osteras B, Osteras H, Torstensen TA. Long-term effects of medical exercise therapy in patients with patellofemoral pain syndrome: results from a single-blinded randomized controlled trial with 12 months follow-up. Physiotherapy. 2013;99(4):311–316. doi: 10.1016/j.physio.2013.04.001. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 121.Song C, Lin Y, Wei T, Lin D, Yen T, Jan M. Surplus value of hip adduction in leg-press exercise in patients with patellofemoral pain syndrome: a randomized controlled trial. Phys Ther. 2009;89(5):409–418. doi: 10.2522/ptj.20080195. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 122.Syme G, Rowe P, Martin D, Daly G. Disability in patients with chronic patellofemoral pain syndrome: a randomised controlled trial of VMO selective training versus general quadriceps strengthening. Man Ther. 2009;14(3):252–263. doi: 10.1016/j.math.2008.02.007. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 123.Davies GJ, Manske RC, Cooley K, Fletcher-Klos D, Johnson-Stuhr P. Selective activation of the vastus medialis oblique: what does the literature really tell us? Physiother Can. 2001;53(2):136–151. (LOE: 3) [Google Scholar]
- 124.Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007;37(4):155–160. doi: 10.2519/jospt.2007.2433. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 125.Mascal CL, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33(11):647–660. doi: 10.2519/jospt.2003.33.11.647. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 126.Tyler TF, Nicholas SJ, Mullaney MJ, McHugh MP. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34(4):630–636. doi: 10.1177/0363546505281808. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 127.Kooiker L, Van De Port IG, Weir A, Moen MH. Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2014;44(6):391–B1. doi: 10.2519/jospt.2014.4127. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 128.Baldon Rde M, Piva SR, Scattone Silva R, Serrao FV. Evaluating eccentric hip torque and trunk endurance as mediators of changes in lower limb and trunk kinematics in response to functional stabilization training in women with patellofemoral pain. Am J Sports Med. 2015;43(6):1485–1493. doi: 10.1177/0363546515574690. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 129.Salsich GB, Graci V, Maxam DE. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther. 2012;42(12):1017–1024. doi: 10.2519/jospt.2012.4231. (LOE: 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pfeiffer RP, DeBeliso M, Shea KG, Kelley L, Irmischer B, Harris C. Kinematic MRI assessment of McConnell taping before and after exercise. Am J Sports Med. 2004;32(3):621–628. doi: 10.1177/0363546503261693. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 131.Bennell K, Duncan M, Cowan S. Effect of patellar taping on vasti onset timing, knee kinematics, and kinetics in asymptomatic individuals with a delayed onset of vastus medialis oblique. J Orthop Res. 2006;24(9):1854–1860. doi: 10.1002/jor.20226. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 132.Cowan SM, Hodges PW, Crossley KM, Bennell KL. Patellar taping does not change the amplitude of electromyographic activity of the vasti in a stair stepping task. Br J Sports Med. 2006;40(1):30–34. doi: 10.1136/bjsm.2005.018499. (LOE: 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Callaghan MJ, Selfe J. Patellar taping for patellofemoral pain syndrome in adults. Cochrane Database Syst Rev. 2012. (4):CD006717. (LOE: 1) [DOI] [PMC free article] [PubMed]
- 134.Lun VM, Wiley JP, Meeuwisse WH, Yanagawa TL. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sport Med. 2005;15(4):235–240. doi: 10.1097/01.jsm.0000171258.16941.13. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 135.Denton J, Willson JD, Ballantyne BT, Davis IS. The addition of the Protonics brace system to a rehabilitation protocol to address patellofemoral joint syndrome. J Orthop Sports Phys Ther. 2005;35(4):210–219. doi: 10.2519/jospt.2005.35.4.210. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 136.Hossain M, Alexander P, Burls A, Jobanputra P. Foot orthoses for patellofemoral pain in adults. Cochrane Database Syst Rev. 2011. (1):CD008402. (LOE: 1) [DOI] [PubMed]
- 137.Barton CJ, Munteanu SE, Menz HB, Crossley KM. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: a systematic review. Sports Med. 2010;40(5):377–395. doi: 10.2165/11530780-000000000-00000. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 138.Barton CJ, Menz HB, Crossley KM. Effects of prefabricated foot orthoses on pain and function in individuals with patellofemoral pain syndrome: a cohort study. Phys Ther Sport. 2011;12(2):70–75. doi: 10.1016/j.ptsp.2010.09.002. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 139.Mills K, Blanch P, Dev P, Martin M, Vicenzino B. A randomised control trial of short term efficacy of in-shoe foot orthoses compared with a wait and see policy for anterior knee pain and the role of foot mobility. Br J Sports Med. 2012;46(4):247–252. doi: 10.1136/bjsports-2011-090204. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 140.Kettunen JA, Harilainen A, Sandelin J, et al. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: a randomized controlled trial. BMC Med. 2007. 5:38. (LOE: 2) [DOI] [PMC free article] [PubMed]
- 141.Kettunen JA, Harilainen A, Sandelin J, et al. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: 5-year follow-up. Br J Sports Med. 2012;46(4):243–246. doi: 10.1136/bjsm.2010.079020. (LOE: 1) [DOI] [PubMed] [Google Scholar]
- 142.Ferguson AB, Jr, Brown TD, Fu FH, Rutkowski R. Relief of patellofemoral contact stress by anterior displacement of the tibial tubercle. J Bone Joint Surg Am. 1979;61(2):159–166. (LOE: 3) [PubMed] [Google Scholar]
- 143.Beck PR, Thomas AL, Farr J, Lewis PB, Cole BJ. Trochlear contact pressures after anteromedialization of the tibial tubercle. Am J Sports Med. 2005;33(11):1710–1715. doi: 10.1177/0363546505278300. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 144.Grelsamer R, Moss G, Ee G, Donell S. The patellofemoral syndrome; the same problem as the Loch Ness Monster? Knee. 2009;16(5):301–302. doi: 10.1016/j.knee.2009.05.005. (LOE: 3) [DOI] [PubMed] [Google Scholar]
- 145.Coppack RJ, Etherington J, Wills AK. The effects of exercise for the prevention of overuse anterior knee pain: a randomized controlled trial. Am J Sports Med. 2011;39(5):940–948. doi: 10.1177/0363546510393269. (LOE: 2) [DOI] [PubMed] [Google Scholar]
- 146.Selfe J, Janssen J, Callaghan M, et al. Are there three main subgroups within the patellofemoral pain population? A detailed characterisation study of 127 patients to help develop targeted intervention (TIPPs) Br J Sports Med. 2016;50(14):873–880. doi: 10.1136/bjsports-2015-094792. (LOE: 2) [DOI] [PMC free article] [PubMed] [Google Scholar]