Abstract
Context:
After anterior cruciate ligament reconstruction (ACLR), women have a greater risk of incurring a second anterior cruciate ligament injury and they display different landing movement patterns than men. It remains unclear if clinical movement-assessment tools, such as the Landing Error Scoring System (LESS), can detect sex differences in movement patterns after ACLR.
Objective:
To compare total LESS scores and individual LESS errors between men and women with a history of ACLR.
Design:
Cross-sectional study.
Setting:
Laboratory.
Patients or Other Participants:
A total of 168 individuals (41 men and 127 women; mean age: men = 20 years [range, 19–25 years], women = 19 years [range, 18–20 years]; mean time since surgery: men = 21 months [range, 12–36 months], women = 27.5 months [range, 17–39 months]) with a history of primary, unilateral ACLR.
Main Outcome Measure(s):
Participants completed a minimum of 3 trials of a drop vertical-jump task scored using the LESS. The between-sexes difference in LESS score was assessed using analysis of covariance, whereas the associations between participant sex and errors on each LESS item were assessed using logistic or multinomial regression.
Results:
Women displayed a greater number of total landing errors (men = 4.6 ± 2.3, women = 6.1 ± 2.3; P < .001) and were more likely to commit errors in trunk flexion at initial contact (men = 4.9%, women = 23.6%; odds ratio [OR] = 4.94), medial knee position at initial contact (men = 17.1%, women = 42.5%; OR = 6.01), medial knee displacement (men = 24.4%, women = 73.2%; OR = 7.88), total joint displacement (1 error: men = 58.5%, women = 71.7%, OR = 2.10; 2 errors: men = 7.3%, women = 14.2%, OR = 3.71), and overall impression (1 error: men = 75.6%, women = 84.3%, OR = 3.24; 2 errors: men = 2.4%, women = 10.2%, OR = 12.89) compared with men.
Conclusions:
Women with ACLR displayed worse LESS scores and were more likely to commit errors related to medial knee displacement and overall landing quality than men with ACLR.
Key Words: movement quality, drop-jump landing, return to sport
Anterior cruciate ligament (ACL) injury is becoming increasingly common among young, physically active individuals who participate in sport-related activity.1 Individuals who opt to undergo ACL reconstruction (ACLR) experience a substantially increased risk for contralateral and ipsilateral ACL injury compared with their healthy counterparts during the first 2 years after surgery.2,3 Although a number of potential risk factors for injury after primary ACLR, including fear of reinjury,4 reduced thigh muscle strength,5 and altered lower extremity functional performance,5 have been highlighted in the literature, it has become increasingly clear that persistent alterations in lower extremity movement quality play a significant role in this subsequent increase in the ACL injury risk.6,7 As a result, recommendations for standardized, multifactorial clinical assessment of individuals who are attempting a return to physical activity or sport have been made with the goal of identifying those at elevated risk of subsequent ACL injury during this critical transition.5,8 Movement quality has been included as a key factor in several of these recommendations, and the Landing Error Scoring System (LESS) is among the most commonly described assessment tools.8,9
Laboratory-based measures, such as 3-dimensional (3-D) motion capture, have been used to identify movement patterns linked with a risk of reinjury or contralateral injury among individuals with ACLR.10 However, use of these assessments in the clinical environment is challenging due to the equipment costs, time associated with data collection and processing, and required technical training. The LESS has been adopted as a screening tool to assess an individual's ACL injury risk based on a 17-item video evaluation of movement quality during a standardized drop-jump task.11 The LESS composite score has been concurrently validated against 3-D motion capture11 and prospectively validated as a predictor of primary ACL injury risk in young athletes (error cutpoint = 5.17 errors, sensitivity = 86%, specificity = 71%, area under the curve = 0.78).12 The LESS has also been shown to have acceptable interrater (intraclass correlation coefficient; ICC [2,k] = 0.84) and intrarater (ICC [2,1] = 0.91) reliability, providing further support for its use in the clinical environment.11 Consequently, the LESS has been highlighted as a useful tool for improving clinical accessibility to and standardizing biomechanical screening of movement quality to assess the subsequent ipsilateral and contralateral ACL injury risks among individuals with ACLR.8 Due to the substantial risk of reinjury after an initial ACL tear2,3 and persistent kinematic alterations,13 clinicians must be able to identify high-risk movements in order to prevent ACL reinjury.14
Sex differences in lower extremity kinematics assessed during functional-movement patterns, such as a jump landing, have been identified as a primary risk factor for ACL injury, which occurs with a 4 to 6 times greater incidence among physically active women compared with men.15,16 Unfortunately, despite surgical reconstruction and rehabilitation, as many as 32.2% of physically active women with ACLR will experience a subsequent ACL injury to the involved or contralateral limb within 2 years of primary ACLR versus 21.0% of men with comparable age and activity characteristics.2 Similar to the evaluation of primary ACL injury risk, sex differences in frontal- and sagittal-plane landing kinematics, identified using 3-D motion analysis, persisted after ACLR.7 However, despite evidence that LESS scores were greater among individuals after ACLR compared with healthy individuals,17,18 it remains unclear if the LESS can detect kinematic differences between men and women. The ability of a clinically feasible assessment tool, such as the LESS, to detect sex differences in specific kinematic variables and overall movement quality may have significant clinical implications for identifying individuals at greatest risk for ipsilateral or contralateral ACL injury after ACLR. Therefore, the primary objective of our investigation was to compare LESS scores and individual LESS item errors between men and women with a history of ACLR. We hypothesized that women with ACLR would commit more total errors and be more likely to commit frontal-plane knee-joint errors on the LESS than men with ACLR.
METHODS
This investigation was part of ongoing cross-sectional studies at 2 data-collection sites. All reported measures were collected during a single testing session. This research was approved by the Michigan State University (Approval # 15-1182) and University of Wisconsin-Madison (Approval # 2013-1429) Institutional Review Boards for Human Subjects Research, and all participants provided informed written consent before testing, after which the rights of the participants were protected. This project includes data used in a prior investigation from the University of Wisconsin-Madison (N = 27).17
Participants
A total of 168 individuals with primary unilateral ACLR were enrolled (Table 1). Participants were included in the study if they were between the ages of 18 and 35 years, had a history of primary unilateral ACLR, and had been cleared for unrestricted physical activity. Participants were excluded if they had a history of lower extremity injury within the previous 6 weeks, a neurologic condition that might affect jump-landing biomechanics, or any lower extremity surgery other than unilateral ACLR. Participants in the ACLR group were not excluded if they underwent a meniscal procedure at the time of ACLR. However, individuals with either multiligament injuries that required reconstruction or articular cartilage injuries that required surgical intervention were excluded.
Table 1.
Participant Demographics
| Total |
Men (n = 41) |
Women (n = 127) |
P Value |
|
| Age, ya | 19 (18–20) | 20 (19–25) | 19 (18–20) | .002b |
| Height, cma | 170.0 (159.3–180.7) | 180.0 (171.6–188.4) | 168.0 (160.0–176.0) | <.001b |
| Body mass, kg | 68.2 (53.3–83.1) | 83.2 (64.4–102.0) | 65.7 (55.5–75.9) | <.001b |
| International Knee Documentation Committee score (0–100 scale)a | 88.5 (74.7–100.0) | 90.8 (74.7–100.0) | 87.4 (65.4–100.0) | .22 |
| Tegner Activity Score (0–10 scale)a | 7 (6–7) | 7 (6–8) | 7 (6–7) | .48 |
| Landing Error Scoring System score (mean ± SD) | 5.7 ± 2.4 | 4.6 ± 2.3 | 6.1 ± 2.3 | <.001b |
| Time since surgery, moa | 25 (15–38) | 21 (12–36) | 27.5 (17–39) | .11 |
| Graft source | .71 | |||
| Bone-patellar tendon-bone autograft | 92 | 22 | 70 | |
| Hamstring autograft | 59 | 16 | 43 | |
| Allograft | 17 | 3 | 14 |
Median (interquartile range).
Indicates a significant between-sexes difference.
Procedures
Before drop vertical-jump (DVJ) testing, participants completed patient-reported measures of knee-related function and peak physical activity. The International Knee Documentation Committee (IKDC) Subjective Knee Form is a self-reported questionnaire that evaluates an individual's perception of knee function during activities ranging from daily life to sport-specific tasks. The IKDC consists of 10 items graded on a 5-point or 10-point Likert scale and is scored from 0 (poor knee function) to 100 (good knee function).19 In addition, participants reported their current peak physical activity level on a scale of 0 (sedentary physical activity level) to 10 (elite physical activity level) using the Tegner Activity Scale.20 The Tegner Activity Scale (ICC = 0.82, 95% confidence interval [CI] = 0.66, 0.89) and the IKDC Subjective Knee Form (ICC = 0.94, 95% CI = 0.88, 0.97) scores demonstrated acceptable test-retest reliability in populations with knee injuries and have been validated for the assessment of current peak physical activity level and knee-related function, respectively.19
Participants at Michigan State University were asked to perform 3 trials, whereas participants at the University of Wisconsin-Madison were asked to perform 5 trials of a DVJ from a 30-cm box to a clearly defined landing area at a distance of one-half the participant's height.11 Participants were instructed to jump off the box onto the landing area and upon landing, immediately complete a maximal vertical jump.11 They were given the opportunity to practice in order to become familiar with the task before beginning the data-collection trials and were able to ask for clarification of the instructions at any point during the test session.
Key Points
Sex differences in movement quality have been observed between healthy men and women using the Landing Error Scoring System, but it is unclear if a similar pattern is present after anterior cruciate ligament reconstruction (ACLR).
Women with ACLR committed a greater number of landing errors than men with ACLR, even though physical activity levels and self-reported knee function did not differ between the sexes.
Compared with men after ACLR, women after ACLR were more likely to land with too little trunk flexion and a more medial knee position at initial contact, greater overall medial knee displacement, and less total joint displacement during a jump landing.
Movement-quality assessment using the Landing Error Scoring System after ACLR may enable clinicians to identify individuals at elevated risk for a second anterior cruciate ligament injury; however, prospective research is needed.
Two commercially available digital video camera recorders (University of Wisconsin-Madison: model HDC-SD80; Panasonic Corp of North America, Newark, NJ; Michigan State University: model HDR-AS200V; Sony Corp, Tokyo, Japan) were used to record each DVJ at 30 Hz in 720-pixel resolution. Cameras were placed no more than 3.5 m from the center of the landing area to ensure an unobstructed view of the landing area from all cameras. A single camera was placed anteriorly to the landing area to record frontal-plane movement, while the second camera was placed laterally to the participant's involved limb.11 Both cameras recorded each DVJ concurrently to allow for identification of landing errors in the frontal and sagittal planes. Video files were saved digitally for processing and analysis at a later time by experienced raters.
Data Analysis
All trials (Michigan State University = 3 trials per participant, University of Wisconsin-Madison = 5 trials per participant) of the DVJ were evaluated using the LESS. The LESS is a valid and reliable tool for assessing individuals with high-risk landing mechanics associated with noncontact ACL injury when used by both novice and expert raters.11 A single rater at Michigan State University and multiple raters at the University of Wisconsin-Madison were required to complete standardized training and achieve clinically acceptable (ICC > 0.80) levels of interrater reliability before evaluating the videos. Training involved reviewing standardized item definitions and scoring criteria, as described by Padua et al,11 and scoring several video trials that had been previously scored by an expert rater with more than 10 years of experience. Interrater reliability was then assessed among the total sample of raters (ICC [2,k] = 0.91, 95% CI = 0.68, 0.99) based on their evaluation of a standardized set of trials not used in our final analysis.
Videos were assessed using commercially available video-processing software (Michigan State University: version 0.8.15; Kinovea Open Source Project, University of Wisconsin-Madison: QuickTime version v7.7.9; Apple Inc, Cupertino, CA). The LESS scoring was limited to subjective evaluation of the video files, but the rater was allowed to use slow-motion playback to help identify key movement patterns associated with LESS scoring items. The LESS was scored on the previously defined 17-item system.11 Raters evaluated all trials of DVJs in both the sagittal and frontal planes. All conditions were assessed during the descending phase of a DVJ, which was defined as the time from initial contact to maximal lower extremity joint displacement. The mode of each scoring item was calculated across all trials, and these modes were then summed to provide a total LESS score. This procedure was limited to the participant's involved limb.
Statistical Analysis
Participant demographics, time since surgery, peak physical activity level, and knee-related function were assessed for distributional normality using Shapiro-Wilk tests before analysis. Participant age (P < .001), height (P = .004), body mass (P < .001), time since surgery (P < .001), and IKDC score (P < .001) were non-normally distributed. Sex differences in these variables were assessed using Mann-Whitney U tests. Based on a preliminary simple linear regression analysis, time since surgery was not significantly associated with total LESS score (adjusted R2 = 0.01, P = .22) and was not included as a covariate in our analyses. We also compared data-collection sites for all dependent variables to assess potential differences in sample characteristics and data-collection methods that may have influenced the results. Based on our findings, data-collection site was included as a covariate in all subsequent analyses.
Total LESS score was compared between sexes using analysis of covariance with data-collection site as a covariate. The frequency of each score for each item (represented as a total percentage of scores) was calculated for the total sample, men, and women. The associations of participant sex with errors reported for each LESS item were investigated using logistic regression in the case of binary LESS items or multinomial regression in the case of ternary LESS items. Before completing our analysis, we evaluated time since surgery as a potential covariate. For binary LESS items, odds ratios (ORs) and 95% CIs were used to assess the odds that women who had undergone ACLR would commit an error on a specific item compared with men who had undergone ACLR. For ternary LESS items, which are limited to the overall impression and joint displacement, separate ORs and 95% CIs were used to assess the odds that women with ACLR would commit a specific level of error (score = 1 or 2) versus men with ACLR. In all multinomial regression analyses, no error (score = 0) was used as the reference category when generating the appropriate ORs. An OR >1 with a CI that did not cross zero indicated items for which the odds were significantly greater that women would commit an error. All statistical analyses were performed using SPSS (version 23.0; IBM Corp, Armonk, NY).
RESULTS
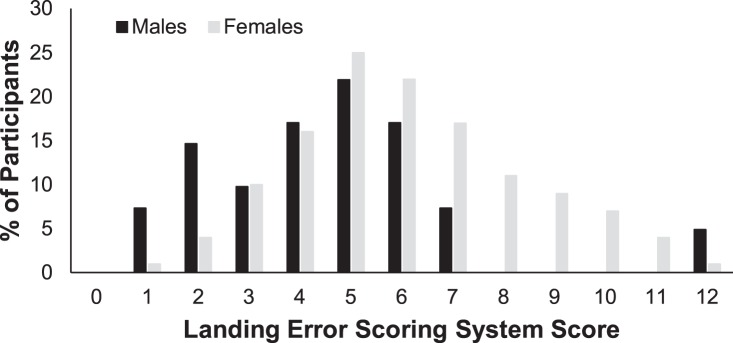
Overall, women displayed higher total LESS scores (mean difference = 1.6 errors, 95% CI = 0.8, 2.6 errors; P < .001) than men (Figure). The covariate, data-collection site, did not have a significant effect on the LESS score in this analysis (P = .27). Individual item frequencies among all participants as well as the men (n = 41) and women (n = 127) are shown in Table 2. In brief, women were more likely to display errors for trunk flexion at initial contact (men = 4.9%, women = 23.6%; OR = 4.94), medial knee position at initial contact (men = 17.1%, women = 42.5%; OR = 6.01), medial knee displacement (men = 24.4%, women = 73.2%; OR = 7.88), total joint displacement (1 error: men = 58.5%, women = 71.7%, OR = 2.10; 2 errors: men = 7.3%, women = 14.2%; OR = 3.71), and overall impression (1 error: men = 75.6%, women = 84.3%, OR = 3.24; 2 errors: men = 2.4%, women = 10.2%, OR = 12.89) compared with men (Table 2).
Figure.
A comparison of the distributions of Landing Error Scoring System scores between men and women with anterior cruciate ligament reconstruction.
Table 2.
Percentage Distribution of Landing Error Scoring System Item Scores by Sexa
| Item Description |
Scoring |
Overall Frequency |
Men |
Women |
Odds Ratio (95% Confidence Interval)b |
| Knee flexion: initial contact | 0 = Absent | 62.5 | 58.5 | 63.8 | 0.98 (0.46, 2.08) |
| 1 = Present | 37.5 | 41.5 | 36.2 | ||
| Hip flexion: initial contact | 0 = Absent | 87.5 | 85.4 | 88.2 | 1.23 (0.40, 3.72) |
| 1 = Present | 12.5 | 14.6 | 11.8 | ||
| Trunk flexion: initial contact | 0 = Absent | 81.0 | 95.1 | 76.4 | 4.94 (1.11, 22.06) |
| 1 = Present | 19.0 | 4.9 | 23.6 | ||
| Ankle plantar flexion: initial contact | 0 = Absent | 76.2 | 80.5 | 74.8 | 1.61 (0.65, 3.95) |
| 1 = Present | 23.8 | 19.5 | 25.2 | ||
| Medial knee position: initial contact | 0 = Absent | 63.7 | 82.9 | 57.5 | 6.01 (2.18, 16.60) |
| 1 = Present | 36.3 | 17.1 | 42.5 | ||
| Lateral trunk position: initial contact | 0 = Absent | 70.8 | 63.4 | 73.2 | 0.71 (0.33, 1.53) |
| 1 = Present | 29.2 | 36.6 | 26.8 | ||
| Stance width: wide | 0 = Absent | 95.8 | 95.1 | 96.1 | 1.18 (0.21, 6.80) |
| 1 = Present | 4.2 | 4.9 | 3.9 | ||
| Stance width: narrow | 0 = Absent | 62.5 | 61.0 | 63.0 | 0.73 (0.34, 1.57) |
| 1 = Present | 37.5 | 39.0 | 37.0 | ||
| Foot position: external rotation | 0 = Absent | 83.9 | 87.8 | 82.7 | 2.21 (0.72, 6.73) |
| 1 = Present | 16.1 | 12.2 | 17.3 | ||
| Foot position: internal rotation | 0 = Absent | 98.2 | 95.1 | 99.2 | 0.22 (0.02, 2.71) |
| 1 = Present | 1.8 | 4.9 | 0.8 | ||
| Symmetric foot contact: initial contact | 0 = Absent | 70.2 | 73.2 | 69.3 | 1.26 (0.56, 2.82) |
| 1 = Present | 29.8 | 26.8 | 30.7 | ||
| Knee-flexion displacement | 0 = Absent | 78.0 | 85.4 | 75.6 | 1.84 (0.70, 4.96) |
| 1 = Present | 22.0 | 14.6 | 24.4 | ||
| Hip-flexion displacement | 0 = Absent | 86.9 | 95.1 | 84.3 | 4.48 (0.96, 20.81) |
| 1 = Present | 13.1 | 4.9 | 15.7 | ||
| Trunk-flexion displacement | 0 = Absent | 70.8 | 75.6 | 69.3 | 1.51 (0.66, 3.45) |
| 1 = Present | 29.2 | 24.4 | 30.7 | ||
| Medial knee displacement | 0 = Absent | 38.7 | 75.6 | 26.8 | 7.88 (3.46, 17.92) |
| 1 = Present | 61.3 | 24.4 | 73.2 | ||
| Joint displacement | 0 = Soft | 9.5 | 34.1 | 14.2 | |
| 1 = Average | 82.1 | 58.5 | 71.7 | 2.10 (0.82, 5.38) | |
| 2 = Stiff | 8.3 | 7.3 | 14.2 | 3.71 (0.88, 15.72) | |
| Overall impression | 0 = Excellent | 19.0 | 22.0 | 5.5 | |
| 1 = Average | 68.5 | 75.6 | 84.3 | 3.24 (1.05, 10.03) | |
| 2 = Poor | 12.5 | 2.4 | 10.2 | 12.89 (1.31, 127.05) |
All analyses included data-collection site as a covariate to take into account potential differences in evaluation technique.
Odds ratio describes the odds that a female participant displayed an error relative to a male participant for a given item.
In our sample, men were older (P = .002) and taller (P < .001) and had greater body mass (P < .001) than women (Table 1). When we compared data-collection sites, a greater proportion of participants was female (P = .02) and younger (P < .001) at the University of Wisconsin-Madison than at Michigan State University (Table 3). The LESS score was not different between data-collection sites (mean difference = 0.2 errors, 95% CI = –0.7, 1.0 errors; P = .74).
Table 3.
Comparison of Data-Collection Sites
| Variable |
University of Wisconsin-Madison |
Michigan State University |
P Value |
| Participants, men/women | 26/105 | 15/22 | .02b |
| Age, ya | 19 (18–20) | 21 (19–22) | <.001b |
| Height, cma | 170.0 (159.3–180.7) | 171.5 (159.7–183.3) | .54 |
| Body mass, kga | 68.1 (54.5–81.7) | 68.3 (48.2–88.4) | .52 |
| International Knee Documentation score (0–100)a | 91.5 (73.6–100.0) | 92.0 (77.0–100.0) | .05 |
| Tegner Activity Score (0–10)a | 7 (6–7) | 7 (6–8) | .08 |
| Landing Error Scoring System score (mean ± SD) | 5.7 ± 2.2 | 5.8 ± 3.1 | .74 |
| Time since surgery, moa | 24 (15–37) | 31 (16–50) | .15 |
| Graft source | .12 | ||
| Bone-patellar tendon-bone autograft | 73 | 19 | |
| Hamstring autograft | 42 | 17 | |
| Allograft | 16 | 1 |
Median (interquartile range).
Indicates a significant between-sexes difference.
DISCUSSION
The LESS has been recommended as a clinical screening tool that can be used to assess the risk of ACL injury.12,14 More recently, clinical recommendations8,9 have begun to include the LESS as a component of comprehensive criteria that may be used to identify individuals who are prepared for unrestricted physical activity or sport after ACLR. Previous authors have highlighted the disparity in second ACL injury rates among the sexes2 while emphasizing the potential role that sex differences in overall movement quality may play in this finding.10 Based on our findings, the LESS was able to detect differences in overall movement quality (Table 1) and the likelihood of committing specific movement errors (Table 2) between men and women that are consistent with kinematic patterns previously observed during functional tasks in this population.21,22 These findings suggest that the LESS may be a useful clinical tool for assessing movement quality among men and women with ACLR; however, subsequent investigators must address the predictive ability of the LESS for identifying individuals who will go on to experience a second ACL injury.
Valid, reliable, and efficient clinical assessments of movement quality are essential components for systematically evaluating the risk of subsequent knee injury after return to unrestricted physical activity or sport participation post-ACLR.8,23 The results of this study (ACLR = 5.7 ± 2.4 errors) are consistent with those of previous reports (Bell et al17 = 6.7 ± 2.1 errors, Kuenze et al18 = 6.0 ± 3.6 errors) regarding the number of landing errors displayed by individuals with ACLR. This finding would broadly classify those with ACLR as being at high risk of subsequent ACLR based on the previously established cutoff value (≥5 errors = high risk).12 It is important to note that this cutoff was established in a youth population and may not be directly applicable to our sample. However, Bell et al17 and Kuenze et al18 also reported that individuals with ACLR displayed a greater number of landing errors than healthy individuals. This is a concern based on a recent report24 that as many as 29.5% of young individuals with ACLR will experience a subsequent contralateral or ipsilateral ACL injury, which is a significantly elevated risk compared with the general population of age- and sex-matched individuals without a history of ACL injury. The ability of the LESS to consistently measure movement quality during a landing task in a clinically feasible manner among individuals with ACLR strengthens the evidence supporting the use of this assessment tool in the ACLR population.
From studies2,3 that have assessed the risk of contralateral or ipsilateral ACL injury among individuals with ACLR, it is clear that young, physically active women (32.2%) are at an elevated risk of injury compared with men (21.0%) of similar activity profiles. We found that women with ACLR displayed a significantly greater number of landing errors (LESS = 6.1 ± 2.3 errors) than men (LESS = 4.6 ± 2.3 errors) with ACLR (Figure), which is consistent with a greater risk of ACL injury. Among our sample, 75.6% of women were categorized as having high-risk movements (5 or greater errors) versus 51.2% of men. Although men constituted a smaller sample (n = 41) than women (n = 127) in our study, it is notable that the total LESS scores among women ranged from 1 error to 12 errors with a relatively normal distribution; LESS scores among men ranged from 1 error to 12 errors, with 95% of men scoring 7 errors or fewer. These findings highlight a sex-based discrepancy in overall movement quality similar to that observed using the LESS in healthy, physically active populations (men = 4.2 ± 2.1 errors, women = 5.7 ± 1.9 errors).25 The clear sex-based difference in total LESS scores indicates that overall lower extremity movement patterns may be contributing factors to the similar sex difference that is observed for the risk of ipsilateral and contralateral ACL injury among individuals with previous ACLR. However, prospective evaluation of the association between LESS score and ACL injury among men and women must be completed before these important clinical outcomes can be directly linked.
The LESS has been most commonly used to assess overall movement quality while taking into account multiplanar lower extremity kinematics at multiple points during a jump landing and overall joint displacement and landing quality.11,12,17 However, this approach limits the direct comparison of specific errors with known kinematic risk factors for ACL injury that have been established using laboratory techniques such as 3-D motion analysis. Individuals with ACLR displayed reduced involved-limb knee-flexion26–28 and hip-flexion angles,29 coupled with increased trunk-flexion angles,30 compared with healthy individuals during a double-limb landing task. This pattern is categorized on the LESS as a stiff landing. In our sample, women were 4.94 (95% CI = 1.11, 22.06) times more likely to commit a trunk-flexion error than men. Women were also 3.71 (95% CI = 0.88, 15.72) times more likely to have their landing rated as stiff than men. Yet this finding should be interpreted with caution as the CI for the OR crosses 1.00, which indicates a meaningful chance that a sex difference was not present. Additionally, individuals with ACLR who experienced greater frontal-plane knee range of motion during a landing task were at greater risk of second ACL injury.10 In this investigation, women were 6.01 (95% CI = 2.18, 16.60) times more likely to commit an error in medial knee positioning at initial contact, 7.88 (95% CI = 3.46, 17.92) times more likely to commit an error in medial knee displacement, and 12.89 (95% CI = 1.31, 127.05) times more likely to have their overall landing quality rated as poor compared with men (Table 2). These findings are consistent with those of previous authors who assessed kinematic indicators of primary ACL injury risk among physically active women16 as well as kinematic movement profiles among women with ACLR.27 Consequently, our results strengthen the case for the application of the LESS in the ACLR population, especially when attempting to assess sex differences in kinematic patterns that may be associated with the risk of second ACL injury. However, subsequent prospective reevaluation of the LESS as a tool for predicting ipsilateral or contralateral ACL injury among individuals with ACLR would provide stronger evidence for its use in determining the injury risk among individuals transitioning from the rehabilitation setting to unrestricted physical activity or sport.
Several key limitations should be considered when evaluating our findings. The data presented are descriptive in nature, which significantly limits our ability to establish a relationship between the LESS score and the subsequent risk of ACL injury in this cohort of participants. Although high-risk categorization has been predictive of an increased primary ACL injury risk, it remains unclear if the same system of risk categorization can be applied to individuals with ACLR and if the errors observed in this analysis would be confirmed by more objective measurement techniques, such as 3-D motion analysis. Researchers should attempt to prospectively assess the risk of ACL injury among those with ACLR to establish whether a relationship is present between these assessments and the subsequent risk of injury. In addition, the risk of a second ACL injury is greatest among women younger than 20 years.2 However, our investigation was limited to men and women over the age of 18 years, which hindered our ability to consider age and maturation stage. A larger sample of participants, specifically a balanced sample of men and women and participants under the age of 18 years, would enable more thorough, age-group–specific assessments using the LESS among individuals with ACLR. Lastly, it is possible that our participants may have experienced injuries more than 6 weeks before enrollment that negatively affected their performance on the LESS. Although we did not record these data, subsequent investigators should consider including a more comprehensive assessment of acute and chronic conditions that may confound participant performance on the LESS.
CONCLUSIONS
Women experience an elevated risk of second ACL injury after ACLR that may be related to lower extremity patterns that are more likely to occur among women than men. In this study, the LESS was able to detect differences in overall movement quality and specific movement errors between men and women that were consistent with kinematic patterns that have been linked to the risk of a second ACL injury in this population. The LESS may be a clinically feasible tool for assessing high-risk movement patterns among individuals with ACLR; however, prospective work is needed to evaluate the association between LESS score and second ACL injury incidence before evidence-based recommendations can be made.
REFERENCES
- 1.Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr. 2017;171(8):808–810. doi: 10.1001/jamapediatrics.2017.0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22(2):116–121. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2011;41(8):553–559. doi: 10.2519/jospt.2011.3591. [DOI] [PubMed] [Google Scholar]
- 8.Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192–199. doi: 10.1007/s00167-016-4246-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc. 2018. In press. [DOI] [PMC free article] [PubMed]
- 10.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Jr, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009;37(10):1996–2002. doi: 10.1177/0363546509343200. [DOI] [PubMed] [Google Scholar]
- 12.Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The Landing Error Scoring System as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50(6):589–595. doi: 10.4085/1062-6050-50.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43(11):2727–2737. doi: 10.1177/0363546515602016. [DOI] [PubMed] [Google Scholar]
- 14.DiStefano LJ, Blackburn JT, Marshall SW, Guskiewicz KM, Garrett WE, Padua DA. Effects of an age-specific anterior cruciate ligament injury prevention program on lower extremity biomechanics in children. Am J Sports Med. 2011;39(5):949–957. doi: 10.1177/0363546510392015. [DOI] [PubMed] [Google Scholar]
- 15.Stanley LE, Kerr ZY, Dompier TP, Padua DA. Sex differences in the incidence of anterior cruciate ligament, medial collateral ligament, and meniscal injuries in collegiate and high school sports: 2009–2010 through 2013–2014. Am J Sports Med. 2016;44(6):1565–1572. doi: 10.1177/0363546516630927. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 17.Bell DR, Smith MD, Pennuto AP, Stiffler MR, Olson ME. Jump-landing mechanics after anterior cruciate ligament reconstruction: a landing error scoring system study. J Athl Train. 2014;49(4):435–441. doi: 10.4085/1062-6050-49.3.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuenze CM, Foot N, Saliba SA, Hart JM. Drop-landing performance and knee-extension strength after anterior cruciate ligament reconstruction. J Athl Train. 2015;50(6):596–602. doi: 10.4085/1062-6050-50.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 20.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 21.Miranda DL, Fadale PD, Hulstyn MJ, Shalvoy RM, Machan JT, Fleming BC. Knee biomechanics during a jump-cut maneuver: effects of sex and ACL surgery. Med Sci Sports Exerc. 2013;45(5):942–951. doi: 10.1249/MSS.0b013e31827bf0e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nyland J, Klein S, Caborn DN. Lower extremity compensatory neuromuscular and biomechanical adaptations 2 to 11 years after anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(9):1212–1225. doi: 10.1016/j.arthro.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Hewett TE. Prediction of future injury in sport: primary and secondary anterior cruciate ligament injury risk and return to sport as a model. J Orthop Sports Phys Ther. 2017;47(4):228–231. doi: 10.2519/jospt.2017.0603. [DOI] [PubMed] [Google Scholar]
- 24.Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44(2):384–392. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- 25.Wesley CA, Aronson PA, Docherty CL. Lower extremity landing biomechanics in both sexes after a functional exercise protocol. J Athl Train. 2015;50(9):914–920. doi: 10.4085/1062-6050-50.8.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Delahunt E, Prendiville A, Sweeney L, et al. Hip and knee joint kinematics during a diagonal jump landing in anterior cruciate ligament reconstructed females. J Electromyogr Kinesiol. 2012;22(4):598–606. doi: 10.1016/j.jelekin.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30(1):72–78. doi: 10.1002/jor.21504. [DOI] [PubMed] [Google Scholar]
- 28.Tsai LC, McLean S, Colletti PM, Powers CM. Greater muscle co-contraction results in increased tibiofemoral compressive forces in females who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30(12):2007–2014. doi: 10.1002/jor.22176. [DOI] [PubMed] [Google Scholar]
- 29.Decker MJ, Torry MR, Noonan TJ, Riviere A, Sterett WI. Landing adaptations after ACL reconstruction. Med Sci Sports Exerc. 2002;34(9):1408–1413. doi: 10.1097/00005768-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Oberländer KD, Brüggemann GP, Höher J, Karamanidis K. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45(3):506–513. doi: 10.1249/MSS.0b013e3182752ae3. [DOI] [PubMed] [Google Scholar]