Abstract
Purpose
The purpose of this study was to compare the clinical efficacy and safety of percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP) in the treatment of the elderly with very severe osteoporotic vertebral compression fractures (vsOVCFs).
Methods
From September 2012 to September 2015, 57 patients with vsOVCFs who had undergone PVP and PKP surgeries at our medical center were reviewed retrospectively, at least 2 years follow-up. All patients were divided into PVP group (n=31) and PKP group (n=26). Clinical data including clinical and radiological evaluation results were performed pre- and postoperatively.
Results
The operation time of PVP group (29.6±3.3 minutes) was less than that of PKP group (37.4±4.2 minutes), with significant differences (P<0.05). Compared with preoperative data, the VAS scores, Oswestry disability index (ODI) scores, and local kyphotic angle were improved with significant differences at 1 day after surgery and the last follow-up in two groups (P<0.05). However, there were no differences in VAS and ODI scores between the two groups (P>0.05). The local kyphotic angle of PVP group was more than that of PKP group after surgery, with significant differences (P<0.05). At 1 day after surgery and the last follow-up, the anterior height of vertebrae fractured was significantly improved compared with preoperative in PKP group (P<0.05), and there was no statistical difference compared with preoperative in PVP group (P>0.05). However, there were no significant differences between the two groups in the leakage rate of bone cement (P>0.05) and incidence of adjacent-level vertebra fracture (P>0.05).
Conclusion
Both PVP and PKP can significantly relieve the pain of the patients with vsOVCFs. Restoring the vertebral height and local kyphotic angle corrections of PKP are comparatively better than those of PVP. However, the operation time of PKP is significantly longer than that of PVP and PKP is not superior in the leakage rate of bone cement and incidence of adjacent-level vertebra fracture compared to PVP.
Keywords: percutaneous vertebroplasty, percutaneous kyphoplasty, osteoporosis, vertebral compression fractures, cement leakage
Introduction
Osteoporotic vertebral compression fractures (OVCFs) are one of the most common complications of osteoporosis in the elderly population, which cause severe back pain, restrict activity, and lower the quality of life.1–3 The minimally invasive techniques such as percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP) were introduced to reduce these clinical problems other than traditional methods such as conservative treatment or open surgery.4–6 PVP, which has been recognized as an effective procedure in the treatment of OVCFs, does not have the advantage of reduction of the sagittal alignment of the spine compared to PKP. Previous studies have demonstrated that both PVP and PKP can immediately relieve the back pain and improve the quality of life.5,7,8
The very severe OVCFs (vsOVCFs), which refer to part of the vertebral body collapsed to less than one-third of its original height, have been cited as an absolute or relative contraindication by many authors for PVP/PKP and instead recommend conservative treatment.9–12 This contraindication was justified by the technical difficulties to perform and the resultant high risk of cement leakage. However, classical open surgery with decompression and stabilization of the fractured vertebra with different kinds of metal implants often fails because of the poor quality of osteoporotic bone. Additionally, because of the risk of open surgery in elderly patients, these procedures have generally been limited to cases where there is concurrent spinal instability or neurological deficit.13,14
In recent years, with the continuous improvement of minimally invasive technique, PVP and PKP are gradually applied for the treatment of vsOVCFs.15–17 However, studies reporting on the outcomes of PVP or PKP in the treatment of vsOVCFs are limited. So far, it is unknown which one of PVP and PKP is more effective for the treatment of vsOVCFs, because few comparative studies have been carried out. The patients in the current study who underwent PVP and PKP for the treatment of vsOVCFs from September 2012 to September 2015 were retrospectively analyzed. The goal of this long-term study was tantamount to compare the clinical effects of the two methods and determine the optimal operation procedure for vsOVCFs.
Materials and methods
Study population selection
This was a retrospective clinical study. A total of 57 patients (23 men, 34 women; age ranged from 64 to 85 years, mean 75.0 years) were identified who had minimally invasive surgery for vsOVCFs in the authors’ institution between September 2012 and September 2015, and were divided into two groups: 31 patients received PVP (PVP group) and 26 patients received PKP (PKP group). Table 1 summarizes the detailed characteristics of the two groups of patients which are comparable. Patients older than 60 years of age, bone mineral density T scores <–2.5, and with one level of thoracolumbar vsOVCFs (assessed by MRI, from thoracic 8 to lumbar 2 vertebral bodies) due to osteoporosis were included in this study. vsOVCFs were diagnosed in patients who complained of back pain or lower back pain, had a history of low-energy trauma and tenderness in the thoracolumbar region according to the physical examination, and manifested compression of the vertebral body on plain radiograph (part of the vertebral body collapsed to less than one-third of their original height). All patients enrolled in this study had relatively severe pain despite undergoing conservative management for 2 weeks. However, the patients who met the following criteria were excluded from this study: 1) spinal cord compression or stenosis of the vertebral canal >30% of the local canal diameter; 2) neurologic deficits; 3) tumor or metastatic tumor that was confirmed by preoperative examination and postoperative pathology; 4) uncorrectable bleeding disorders; 5) systemic or local spine infections; 6) severe comorbidity in the heart, liver, kidney, and lung intolerance to surgery; 7) follow-up <2 year or lost. This study was conducted in accordance with the Declaration of Helsinki and approved by ethics committee of The Third Hospital of Hebei Medical University. There is no need to obtain informed consent from patients because this is a retrospective study, and all data were collected and analyzed anonymously.
Table 1.
Patient demographics (PVP and PKP groups)
| Variables | Total (57 cases) | PVP (31 cases) | PKP (26 cases) | t/c2 value | P-value |
|---|---|---|---|---|---|
|
| |||||
| Age (years)a | 75.0±6.4 | 74.8±5.6 | 75.3±7.3 | 0.292 | 0.771 |
| Sexb | |||||
| Men | 23 (40.4%) | 12 | 11 | 0.076 | 0.783 |
| Women | 34 (59.6%) | 19 | 15 | ||
| BMI (kg/m2)a | 24.7±4.1 | 24.9±4.5 | 24.4±3.7 | 0.452 | 0.653 |
| BMD (T-score)a | –3.5±0.6 | –3.6±0.5 | –3.4±0.6 | 1.373 | 0.175 |
| Duration of disease (months)a | 2.6±1.7 | 2.8±1.8 | 2.4±1.6 | 0.879 | 0.383 |
| Vertebral compression (%)a | 73.3±4.3 | 73.4±4.1 | 73.1+4.5 | 0.263 | 0.793 |
| Operative levelsb | |||||
| T8–T9 | 10 (17.5%) | 5 | 5 | 0.179 | 0.914 |
| T10–T12 | 28 (49.1%) | 15 | 13 | ||
| L1–L2 | 19 (33.3%) | 11 | 8 | ||
| Operation time (minutes)a | 33.2±3.7 | 29.6±3.3 | 37.4±4.2 | 7.851 | 0.000∗ |
| Cement volume (mL)a | 3.2±1.0 | 2.8±0.8 | 3.6±1.1 | 3.173 | 0.002∗ |
| Adjacent-level fractureb | 5 (8.8%) | 3/31 | 2/26 | 0.070 | 0.792 |
| Cement leakageb | 15 (26.3%) | 7/31 | 8/26 | 0.489 | 0.484 |
| Average length of stay (days)a | 2.1±1.0 | 2.1±1.0 | 2.2±0.9 | 0.393 | 0.695 |
| Follow-up (years)a | 2.7±0.6 | 2.6±0.5 | 2.8±0.7 | 1.255 | 0.215 |
Note:
Independent two-sample t-test;
chi-square test;
P<0.05.
Abbreviations: BMD, bone mineral density; BMI, body mass index; PKP, percutaneous kyphoplasty; PVP, percutaneous vertebroplasty.
Surgical management
Before the operation, all the patients took X-ray (anteroposterior), computed tomography (CT, including sagittal reconstruction), and magnetic resonance imaging (MRI) scans. The same senior surgeon performed the surgery in all the patients. The surgery was performed under local infiltration anesthesia under electrocardiographic monitoring with the patient in the prone position with the spine extended by chest and pelvic bolsters on a radiolucent operating table. G-arm fluoroscopy was used for simultaneous viewing of anteroposterior and lateral projections of the spine to identify an extrapedicular or transpedicular entry point into the vertebral body. A puncture needle was placed percutaneously into the posterior vertebral body through unilateral transpedicular approach, and the PVP (Figure 1) and PKP (Figure 2) procedures were performed in the standard fashion reported in previous studies.18,19 The procedure of PVP was much the same as PKP, but without insertion and inflation of the balloon. The injection and leakage of bone cement were monitored using G-arm fluoroscopy during the surgery. With any doubt of cement leakage into the spinal canal on the fluoroscopy, cement injection was stopped. Bone cement used was polymethyl methacrylate. After the operation, the patients began to walk by themselves after 4–6 hours. All the patients had conservative treatment of bisphosphonates, calcitonin, and vitamin D supplementation pre- and postoperation.
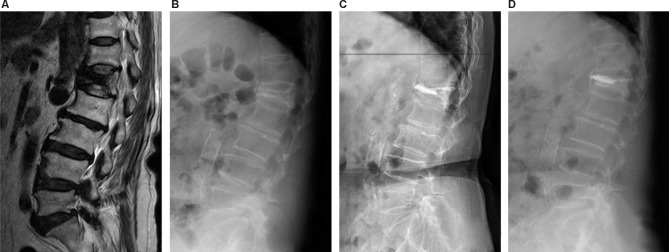
Figure 1.
A 74-year-old female patient was admitted to our hospital after she slipped down. (A) Preoperative T1 sagittal MRI showed acute recent fracture of L1 vertebra. (B) Plain lateral radiograph showed OVCF of L1 vertebra with 72.6% severe collapse, 7.4 mm anterior height of vertebrae fractured, and 28.2° local kyphosis. (C) Plain lateral radiograph showed 7.5 mm anterior height of vertebrae fractured and 23.5° local kyphosis 1 day after PVP surgery. (D) The anterior height of vertebrae fractured and local kyphotic angle improved and maintained at the last follow-up.
Abbreviations: OVCF, osteoporotic vertebral compression fracture; PVP, percutaneous vertebroplasty.
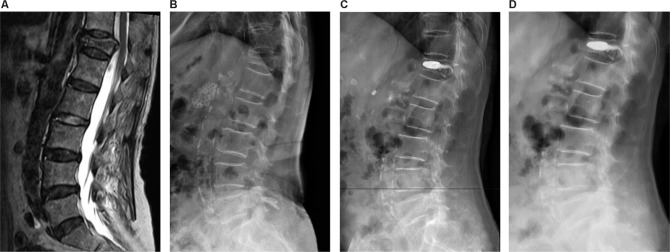
Figure 2.
A 68-year-old female patient was admitted to our hospital after she slipped down. (A) Preoperative T1 sagittal MRI showed acute recent fracture of T12 vertebra. (B) Plain lateral radiograph showed OVCF of T12 vertebra with 70.4% severe collapse, 8.0 mm anterior height of vertebrae fractured, and 27.4° local kyphosis. (C) Plain lateral radiograph showed 14.3 mm anterior height of vertebrae fractured and 19.6° local kyphosis 1 day after PKP surgery. (D) The anterior height of vertebrae fractured and local kyphotic angle improved and maintained at the last follow-up.
Abbreviations: OVCF, osteoporotic vertebral compression fracture; PVP, percutaneous vertebroplasty.
Evaluation criteria
Clinical data including clinical and radiological evaluation results were collected by two independent authors preoperatively and at 1 days, 3, 6, and 12 months and final follow-up after surgery. All the patients were followed up at least 2 years after surgery. Clinical evaluation incorporated the visual analog scale (VAS) score (ranged from 0 to 10; 0: no pain, 10: worst pain) for pain evaluation and the Oswestry disability index (ODI) score for functional assessment. Local kyphotic angle and anterior height of the fractured vertebrae body were measured preoperatively, postoperatively, and at last follow-up, as were cement leakage, recollapse of the cemented vertebral body, and any adjacent segment fracture. In patients who complained of new onset of back pain, additional radiograph or MRI was performed. New OVCFs were diagnosed if plain radiograph revealed a definite decrease in the vertebral body height or MRI showed bone marrow edema at the corresponding anatomic level.
Statistical analysis
All data were collected, and SPSS Version 17.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical evaluation. The results were presented as mean ± SD. A Student’s t-test was used to identify a significant difference between pre- and postoperative measurements of VAS score, ODI score, local kyphotic angle, and anterior height of vertebrae fractured for each group. The independent two-sample t-test was used to identify a significant difference between the groups. Categorical data were compared via the chi-squared test (Fisher’s exact test for small samples). In all analyses, P-value <0.05 was considered statistically significant.
Results
This retrospective study included 57 patients comprising 23 men and 34 women with a mean age at operation of 75.0 (range from 64 to 85) years. The average compressive rate of fractured vertebral bodies was 73.3% (ranged from 66.7% to 80.4%). After the PVP/PKP surgery, the patients were followed up with an average of 2.7 years and all adjacent-level fractures occurred within one year.
Of these 57 patients, there were 31 patients in the PVP group and 26 patients in the PKP group. There were no significant differences in age, sex, BMI, BMD, duration of disease, vertebral compression, operative levels, average length of stay, and follow-up between PVP and PKP groups (P>0.05, Table 1). The operation time of PVP group (29.6±3.3 minutes) was less than that of PKP group (37.4±4.2 minutes), with significant differences (P<0.05, Table 1). Compared with preoperative data, the VAS scores, ODI scores, and local kyphotic angle were improved with significant differences at 1 day after surgery and the last follow-up in the two groups (P<0.05, Table 2). However, there were no differences in VAS and ODI scores between the two groups (P>0.05, Table 2). The local kyphotic angle of PVP group was more than that of PKP group after surgery, with significant differences (P<0.05, Table 2). At 1 day after surgery and the last follow-up, the anterior height of vertebrae fractured was significantly improved compared with preoperative in PKP group (P<0.05, Table 2), and there was no statistical difference compared with preoperative in PVP group (P>0.05, Table 2). Therefore, PKP was significantly better than PVP in restoring the vertebral height and correction of local kyphotic angle.
Table 2.
Comparison of surgical results between PVP vs PKP groups in patients with severe OVCF
| Outcomes | PVP
|
PKP
|
||||||
|---|---|---|---|---|---|---|---|---|
| Preoperative | 1 day after surgery | 1 year after surgery | Last follow-up | Preoperative | 1 day after surgery | 1 year after surgery | Last follow-up | |
|
| ||||||||
| VAS score | 7.3±1.1 | 2.1±1.1a | 1.5±1.1a,b | 1.7±1.0a,b | 6.9±1.2 | 2.3±1.2a | 1.6±1.0a,b | 1.6±1.1a,b |
| ODI score | 75.5±10.2 | 28.5±10.4a | 22.4±8.4a,b | 23.5±8.5a,b | 71.7±9.2 | 29.8±10.1a | 23.7±8.3a,b | 24.2±8.6a,b |
| Local kyphotic angle (°) | 30.4±3.6 | 25.7±3.1a | 26.0±2.9a | 26.5±3.0a | 29.6±3.3 | 19.1±3.3a,c | 19.4±3.4a,c | 20.1±3.5a,c |
| Anterior height of vertebrae fractured (mm) | 8.5±1.1 | 8.7±1.1 | 8.6±1.1 | 8.6±1.0 | 8.6±1.1 | 12.5±2.9a,c | 12.4±2.8a,c | 12.2±2.7a,c |
Notes:
Significant difference between preoperative and postoperative using paired t-test; P<0.05.
Significant difference between 1 day after surgery and last follow-up using paired t-test; P<0.05.
Significant difference between two groups using independent two-sample t-test; P<0.05.
Abbreviations: OVCF, osteoporotic vertebral compression fracture; ODI, Oswestry disability index; PKP, percutaneous kyphoplasty; PVP, percutaneous vertebroplasty; VAS, visual analog scale.
Cement leakage occurred in 15 cases (26.3%, seven cases in PVP and eight cases in PKP), without pulmonary embolism and spinal cord injury. A total of five patients (8.8%, three cases in PVP and two cases in PKP) had adjacent-level fracture during the follow-up period and all adjacent-level fractures occurred within one year. These patients underwent additional PVP/PKP surgery. And immediate relief of typical back pain was reported in all patients after reoperation. There were no significant differences between the two groups in the leakage rate of bone cement (χ2=0.489, P>0.05, Table 1) and the incidence of adjacent vertebra fracture (χ2=0.070, P>0.05, Table 1). During the follow-up period, there were no adverse events such as infection, bone cement displacement, or abscission in the two groups.
Discussion
The OVCFs, which are mainly caused by osteoporosis, have become a major health problem worldwide nowadays. Most OVCFs can be healed within a few months by conservative therapy, but when the symptoms persist after conservative therapy, surgical treatment such as PVP or PKP should be regarded as a better choice. Hulme et al20 found that about 95% pain and dysfunction caused by fracture can be relieved successfully by these two methods. According to the examination of preoperative anteroposterior and lateral X-radiographs, OVCFs are graded on the basis of the extent of vertebral body collapse: mild (20%–25%); moderate (26%–40%); severe (>40%); very severe (>67%). Despite these good results, vsOVCFs have always been considered as an absolute or relative contraindication due to the technical difficulty and the more important theoretical risk of cement leakage.9–12
With the improvement of imaging and surgical techniques, PVP and PKP have been investigated in the treatment of vsOVCFs. Sigaux et al16 observed that 12 vsOVCFs in ten patients have been treated by PVP and found that all the patients had immediately relieved the back pain. Lee et al17 reported 31 patients with vsOVCFs who underwent PKP surgery with a follow-up time of 1 year and showed that all the patients had significant improvements in pain relief, vertebral body height variation, and kyphotic angle. However, studies assessing PVP and PKP in vsOVCFs are scarce and mainly limited to case reports or small patient cohorts. Until now, it is unknown which one of PVP and PKP is more effective for the treatment of vsOVCFs. In this comparative study, all patients underwent PKP or PVP with unilateral approach successfully. And the VAS and ODI scores were used to measure the pain relief after operation, through the short-term (1 day after surgery) and long-term (at least 2 years) follow-up; the pooled results showed that there was no statistical difference between PVP and PKP groups. However, a sustained, statistically significant decrease in VAS and ODI scores was noted in both the groups, which means that both PVP and PKP can reduce the symptoms of back pain and improve the quality of life. In addition, our radiological findings showed that PKP had an effect on restoring vertebral body height and reducing local kyphotic angle, and the correction had only a slightly loss at the last follow-up. The mean anterior height of vertebrae fractured and local kyphotic angle in PKP group were significantly better than those in PVP group at 1 day after surgery and the last follow-up, which means that PKP could result in the magnitude of local correction. However, kyphosis deformity was also improved to some extent in the PVP group. Nevertheless, needing more complex operational steps, such as establishing expander channel on the pedicle repeatedly, the PKP surgery calls for more surgical time.21,22 That is consistent with our statistic findings. Therefore, PVP is more suitable for vsOVCF patients with older age, more internal medical diseases, and difficulty persisting in prone position under local anesthesia for a long time. In addition, unilateral approach was safe and effective for patients with vsOVCFs, and it was also recommended.
The major complications arising from PVP or PKP are related to leakage of bone cement. Although cement leakage is rarely symptomatic, the reported incidence of cement leakage varies from 5% to >80%.23–25 vsOVCFs often have some cleft in the vertebral wall and endplate, which increase the risk of cement leakage. Nieuwenhuijse et al11 performed PVP operation in 34 patients with vsOVCFs. And the leakage rate of bone cement was up to 91.9%, more than one time higher than that of non-vsOVCF patients. As we all know, the high injection pressure with low viscosity of the cement would lead to higher frequency leakage of cement during PVP than in PKP. On the contrary, with the help of a balloon, the PKP procedure created a cavity that could be utilized to package the cement. It is the methodological difference in PKP which leads to a lower rate of cement leakage. However, due to the poor vertebral strength in patients with vsOVCFs, balloon distraction during PKP may lead to damage to the vertebral wall and upper and lower endplates, increasing the risk of cement leakage. In the present study, the incidence of cement leakage was detected in 26.3% (15/57) of treated vertebrae in single-level vsOVCF patients. The incidence was lower than the results from previous studies. Moreover, there was no significant difference between PVP (22.6%, 7/31) and PKP (30.8%, 8/26) groups in this study. We believed that this may be due to small average amount of cement in the operation, as well as the absence of an excessive reduction of the vertebral body and correction of local kyphosis for vsOVCFs patients.
Several studies have reported an increase in the incidence of new symptomatic adjacent vertebral compression fractures after bone cement augmentation, compared with conservative treatment.26,27 The possible risk factors include the amount of injected bone cement, intradiscal leakage, compact and solid cement pattern, and greater kyphosis correction.28–31 However, it is still unclear that what the exact relevant element is and whether such fractures are part of the natural course of osteoporosis. In the current study, we found a similar incidence of adjacent-level fractures (8.8%, 5/57) during the follow-up period comparing with previous studies.31–34 All adjacent-level fractures occurred within one year. Furthermore, there was no significant difference between PVP (9.7%, 3/31) and PKP (7.7%, 2/26) groups. Therefore, our research indicated that the incidence of adjacent-level vertebral fractures is not related to the choice of surgical methods.
Conclusion
In this study, both PVP and PKP can significantly relieve the pain of the patients with vsOVCFs. Moreover, restoring the vertebral height and local kyphotic angle corrections of PKP is comparatively better than those of PVP. But the operation time of PKP is significantly longer than that of PVP. And PKP is not superior in the leakage rate of bone cement and incidence of adjacent-level vertebra fracture compared to PVP. However, this study was merely a retrospective study with a small sample size to explore the best surgical methods for vsOVCFs. There is still a need for a large sample multicenter study to further confirm this result.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Footnotes
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Landham PR, Baker-Rand HL, Gilbert SJ, et al. Is kyphoplasty better than vertebroplasty at restoring form and function after severe vertebral wedge fractures? Spine J. 2015;15(4):721–732. doi: 10.1016/j.spinee.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 2.Edidin AA, Ong KL, Lau E, Kurtz SM. Morbidity and mortality after vertebral fractures: comparison of vertebral augmentation and nonoperative management in the medicare population. Spine. 2015;40(15):1228–1241. doi: 10.1097/BRS.0000000000000992. [DOI] [PubMed] [Google Scholar]
- 3.Kado DM, Browner WS, Palermo LM, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med. 1999;159(11):1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 4.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26(14):1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 5.Wardlaw D, Cummings SR, van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373(9668):1016–1024. doi: 10.1016/S0140-6736(09)60010-6. [DOI] [PubMed] [Google Scholar]
- 6.Komemushi A, Tanigawa N, Kariya S, et al. Percutaneous vertebroplasty for osteoporotic compression fracture: multivariate study of predictors of new vertebral body fracture. Cardiovasc Intervent Radiol. 2006;29(4):580–585. doi: 10.1007/s00270-005-0138-5. [DOI] [PubMed] [Google Scholar]
- 7.Papanastassiou ID, Phillips FM, van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J. 2012;21(9):1826–1843. doi: 10.1007/s00586-012-2314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Folman Y, Shabat S, Yoram F, Shay S. A comparison of two new technologies for percutaneous vertebral augmentation: confidence vertebroplasty vs. sky kyphoplasty. Isr Med Assoc J. 2011;13(7):394–397. [PubMed] [Google Scholar]
- 9.Peh WC, Gilula LA, Peck DD. Percutaneous vertebroplasty for severe osteoporotic vertebral body compression fractures. Radiology. 2002;223(1):121–126. doi: 10.1148/radiol.2231010234. [DOI] [PubMed] [Google Scholar]
- 10.Nieuwenhuijse MJ, van Erkel AR, Dijkstra PD. Percutaneous vertebroplasty in very severe osteoporotic vertebral compression fractures: feasible and beneficial. J Vasc Interv Radiol. 2011;22(7):1017–1023. doi: 10.1016/j.jvir.2011.02.036. [DOI] [PubMed] [Google Scholar]
- 11.Cotten A, Boutry N, Cortet B, et al. Percutaneous vertebroplasty: state of the art. Radiographics. 1998;18(2):311–320. doi: 10.1148/radiographics.18.2.9536480. [DOI] [PubMed] [Google Scholar]
- 12.Manson NA, Phillips FM. Minimally invasive techniques for the treatment of osteoporotic vertebral fractures. J Bone Joint Surg Am. 2006;88(8):1862–1872. doi: 10.2106/00004623-200608000-00026. [DOI] [PubMed] [Google Scholar]
- 13.Chen D, An ZQ, Song S, Tang JF, Qin H. Percutaneous vertebroplasty compared with conservative treatment in patients with chronic painful osteoporotic spinal fractures. J Clin Neurosci. 2014;21(3):473–477. doi: 10.1016/j.jocn.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 14.Lange A, Kasperk C, Alvares L, Sauermann S, Braun S. Survival and cost comparison of kyphoplasty and percutaneous vertebroplasty using German claims data. Spine. 2014;39(4):318–326. doi: 10.1097/BRS.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 15.Muijs SP, Nieuwenhuijse MJ, van Erkel AR, Dijkstra PD. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: evaluation after 36 months. J Bone Joint Surg Br. 2009;91(3):379–384. doi: 10.1302/0301-620X.91B3.20970. [DOI] [PubMed] [Google Scholar]
- 16.Sigaux J, Guignard S, Tuilier T, Eymard C, Gaston A, Chevalier X. Efficacity and feasibility of vertebroplasty for severe vertebral fracture: a retrospective study of 12 vertebroplasties. Joint Bone Spine. 2013;80(3):328–331. doi: 10.1016/j.jbspin.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 17.Lee JK, Jeong HW, Joo IH, Ko YI, Kang CN. Percutaneous balloon kyphoplasty for the treatment of very severe osteoporotic vertebral compression fractures: a case-control study. Spine J. 2018;18(6):962–969. doi: 10.1016/j.spinee.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 18.Atalay B, Caner H, Gokce C, Altinors N. Kyphoplasty: 2 years of experience in a neurosurgery department. Surg Neurol. 2005;64(Suppl 2):S72–S76. doi: 10.1016/j.surneu.2005.07.039. [DOI] [PubMed] [Google Scholar]
- 19.Bach HG, Lim RD. Minimally invasive spine surgery for low back pain. Dis Mon. 2005;51(1):34–57. doi: 10.1016/j.disamonth.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31(17):1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 21.Chang X, Lv YF, Chen B, et al. Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop. 2015;39(3):491–500. doi: 10.1007/s00264-014-2525-5. [DOI] [PubMed] [Google Scholar]
- 22.Wang H, Sribastav SS, Ye F, et al. Comparison of Percutaneous Vertebroplasty and Balloon Kyphoplasty for the Treatment of Single Level Vertebral Compression Fractures: A Meta-analysis of the Literature. Pain Physician. 2015;18(3):209–222. [PubMed] [Google Scholar]
- 23.Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31(17):1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 24.Muijs SP, Akkermans PA, van Erkel AR, Dijkstra SD. The value of routinely performing a bone biopsy during percutaneous vertebroplasty in treatment of osteoporotic vertebral compression fractures. Spine. 2009;34(22):2395–2399. doi: 10.1097/BRS.0b013e3181b8707e. [DOI] [PubMed] [Google Scholar]
- 25.Schmidt R, Cakir B, Mattes T, Wegener M, Puhl W, Richter M. Cement leakage during vertebroplasty: an underestimated problem? Eur Spine J. 2005;14(5):466–473. doi: 10.1007/s00586-004-0839-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Legroux-Gérot I, Lormeau C, Boutry N, Cotten A, Duquesnoy B, Cortet B. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol. 2004;23(4):310–317. doi: 10.1007/s10067-004-0914-7. [DOI] [PubMed] [Google Scholar]
- 27.Voormolen MH, Lohle PN, Juttmann JR, van der Graaf Y, Fransen H, Lampmann LE. The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol. 2006;17(1):71–76. doi: 10.1097/01.RVI.0000190910.43602.3C. [DOI] [PubMed] [Google Scholar]
- 28.Lin WC, Cheng TT, Lee YC, et al. New vertebral osteoporotic compression fractures after percutaneous vertebroplasty: retrospective analysis of risk factors. J Vasc Interv Radiol. 2008;19(2 Pt 1):225–231. doi: 10.1016/j.jvir.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 29.Moon ES, Kim HS, Park JO, et al. The incidence of new vertebral compression fractures in women after kyphoplasty and factors involved. Yonsei Med J. 2007;48(4):645–652. doi: 10.3349/ymj.2007.48.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96(1 Suppl):56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 31.Rho YJ, Choe WJ, Chun YI. Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J. 2012;21(5):905–911. doi: 10.1007/s00586-011-2099-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yi X, Lu H, Tian F, et al. Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg. 2014;134(1):21–30. doi: 10.1007/s00402-013-1886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim SH, Kang HS, Choi JA, Ahn JM. Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol. 2004;45(4):440–445. doi: 10.1080/02841850410005615. [DOI] [PubMed] [Google Scholar]
- 34.Lee WS, Sung KH, Jeong HT, et al. Risk factors of developing new symptomatic vertebral compression fractures after percutaneous vertebroplasty in osteoporotic patients. Eur Spine J. 2006;15(12):1777–1783. doi: 10.1007/s00586-006-0151-7. [DOI] [PubMed] [Google Scholar]