Abstract
Objective:
To evaluate low-tube-voltage 90-kVp CT pulmonary angiography (CTPA) with advanced modeled iterative reconstruction algorithm (Admire) compared to 120-kVp equivalent dual-energy (DE) acquisition with regards to radiation exposure, image quality and diagnostic accuracy for pulmonary embolism (PE) assessment.
Methods:
CTPA studies of 40 patients with suspected PE (56.7 ± 16.3 years) performed on a third-generation 192-slice dual-source CT scanner were retrospectively included. 120-kVp equivalent linearly-blended (60% 90-kVp, 40% 150-kVp) and 90-kVp images were reconstructed. Attenuation and noise of the pulmonary trunk were measured to calculate contrast-to-noise ratios (CNR). Three radiologists assessed the presence of central and segmental PE and diagnostic confidence. Interobserver agreement was calculated using intraclass correlation coefficient (ICC). Radiation exposure was assessed as effective dose (ED).
Results:
Pulmonary trunk CNR values were significantly increased in 90-kVp compared to linearly-blended series (15.4 ± 6.3 vs 11.3 ± 4.6, p < 0.001). Diagnostic accuracy for PE assessment was similar in both series with excellent interobserver agreement (p = 0.48; ICC, 0.83; p = 0.48). Overall confidence for PE assessment was rated excellent for both series with a significant advantage for linearly-blended series (p < 0.001; 4.1 vs 3.8). ED was reduced by 37.2% with 90-kVp compared to 120-kVp equivalent image series (1.1 ± 0.6 vs 1.7 ± 0.7 mSv, p < 0.001).
Conclusion:
90-kVp CTPA with Admire provided increased quantitative image quality with similar diagnostic accuracy and confidence for PE assessment compared to 120-kVp equivalent acquisition, while radiation dose was reduced by 37.2%.
Advances in knowledge:
90-kVp CTPA with an advanced iterative reconstruction algorithm results in excellent image quality and reduction of radiation exposure without limiting diagnostic performance.
Introduction
CT pulmonary angiography (CTPA) is a fast, accurate and widely available imaging technique and, as such, the modality of choice for assessment of acute pulmonary embolism (PE), a major cause of morbidity, mortality and hospitalization.1 Diagnostic accuracy of CTPA for PE detection is constantly increasing with values greater than 90%, while at the same time, there is concern over the cumulative radiation exposure of patients.2 With the introduction of new scanner generations, which allow a more precise setting of tube voltage with an increment of 10 kV and an increased tube current capacity, acquisition at lower tube voltages has become available. Low-tube-voltage acquisition results in greater attenuation of iodinated contrast medium, but also increased noise compared to standard 120-kVp acquisition, while radiation dose is reduced substantially, when tube current is kept constant.3–5 Iterative reconstruction (IR) techniques reduce image noise independently of tube current and voltage settings without radiation penalty. Thus, IR allow for increased contrast combined with low-tube-voltage scans, which has been shown to improve image quality at lower radiation doses than standard 120-kVp scans.6–9 A new IR algorithm, advanced modeled iterative reconstruction algorithm (Admire), has shown beneficial results in several body regions, including CT angiography (CTA) of the thorax in congenital heart disease patients, and coronary CTA.10, 11 To our knowledge, the impact of Admire on low-tube-voltage CTPA for the evaluation of PE has not been investigated so far.
Hence, the aim of our study was to evaluate the impact of low-tube-voltage 90-kVp CTPA in combination with Admire compared to 120-kVp equivalent linearly-blended image series with regards to image quality, diagnostic accuracy and confidence for PE assessment.
Methods and Materials
Patients
This retrospective study was approved by the local institutional review board with a waiver for written consent. All studies were performed during clinical routine in patients with suspected acute PE between March and July 2016. “Triple-rule-out” studies for acute chest pain, examinations with inaccurate region of interest (ROI) placement during bolus-tracking, severe motion artifacts, a flow-rate below 5 ml s−1, or extravasation during contrast injection were excluded. Thus, a total of 40 patients (19 female; mean age, 56.7 ± 16.3 years) were enrolled in this study. Mean body mass index was 25.4 ± 3.2 kg m−2.
CT protocol
All CTPA studies were performed on a 192-slice third-generation dual-source CT scanner (Somatom Force, Siemens Healthcare, Forchheim, Germany). The scanner operated in dual-energy (DE) mode providing 90-kVp (95 ref. mAs) and 150-kVp (59 ref. mAs). The second X-ray tube was equipped with a tin filter (Selective Photon Shield II, Siemens Healthcare). Patients received commands for slight inspiratory breath-hold, before acquisition started in craniocaudal direction with a pitch of 0.7 and collimation of 192 × 0.6. Automatic tube current modulation (Caredose 4D, Siemens Healthcare) was activated in all scans.
A total of 0.9 ml kg−1 body weight with a maximum of 90 ml of non-ionic contrast agent (Ultravist, Iopromide 300 mg iodine/ml, Bayer Healthcare, Berlin, Germany) was i.v. injected at a flow-rate of 5 ml s−1 via an antecubital vein, followed by a 50 ml saline chaser. Bolus-tracking technique triggered the scan, with a ROI in the pulmonary trunk, threshold of 120 HU and delay of 7 s.
Data reconstruction
CTPA data were reconstructed as 120-kVp equivalent linearly-blended M_0.6 image series, combining 60% of the 90-kVp and 40% of the 150-kVp spectrum, and as 90-kVp series. All data were reconstructed as axial and coronal images with a section thickness and increment of 2 mm using Admire (Siemens Healthcare) at a strength level of 3 of 5.
Radiation dose
Cumulative radiation doses expressed as dose-length-product (DLP) and CT dose index (CTDIvol) were recorded from the patient’s protocol saved in the patient achieving and communication system. Radiation doses of the 90-kVp acquisition were extracted by a validated software. To calculate effective dose (ED), DLP was multiplied with the International Commission on Radiological Protection conversion factor for thorax CT (0.014 mSv mGy*cm–1). Radiation doses of the 90-kVp acquisition were extracted from the dataset by previously used and validated software which has been developed inhouse in cooperation with Fraunhofer Institute Darmstadt, Germany.12
Quantitative image analysis
Quantitative analysis was performed by a radiologist with three years of experience in chest imaging using a commercially available PACS (picture archiving and communication system) workstation (Centricity 4.2, General Electric Healthcare, Milwaukee, WI). Circular ROIs were placed in the pulmonary trunk and erector spinae muscle to measure attenuation and standard deviation in HU). ROIs were drawn as large as possible, but avoiding surrounding anatomical structures. Standard deviation of subcutaneous pectoral fat was recorded to quantify image noise. To ensure data consistency, all measurements were performed three times and results were averaged. The following formulas for calculating quantitative image quality based on contrast-to-noise ratio (CNR) and signal-to-noise ratio (SNR) were used: CNR = (HUartery−HUmuscle)/noise, and SNR = HUartery/noise.
Qualitative image analysis
To provide a reference standard for the diagnosis of PE, a consensus reading was performed by two board-certified radiologists with more than 8 years of experience using all available image series and follow-up examinations. The reference standard for our study was based on the same CTPA acquisition.
Four blinded radiologists with 3–6 years of experience in CTPA (two residents, two consultants) independently assessed linearly-blended 120-kVp and 90-kVp image series for the presence of central and segmental PE with 1 = PE certainly absent, 2 = PE possibly absent, 3 = indeterminate, 4 = PE possibly present and 5 = PE definitely present. Central PE was defined as endoluminal clots in the pulmonary trunk or main pulmonary arteries. Additionally, radiologists rated their overall diagnostic confidence in the assessment of PE, as well as for the evaluation of central and segmental pulmonary arteries, ranging from 1 = poor to 5 = excellent diagnostic confidence. Preset window settings (width, 800 HU; level, 300 HU) could be freely modified. To reduce the risk of recall bias, only a single imaging protocol was evaluated during each session, with a minimum of 2 weeks between readings.
Statistical analysis
Statistical analysis was performed using dedicated software (Medcalc 12.7.2; Medcalc Software bvba, Ostend, Belgium). The Kolmogorov-Smirnov test was applied to evaluate normality of data distribution. Normally distributed data was analyzed using the paired Student t-test, while unequal variances were analyzed using the Wilcoxon signed-rank test. The non-parametric Friedman test with post-hoc test was used to evaluate qualitative image quality.
Ratings were dichotomized, and scores of 1 and 2 were regarded as negative, while 3 to 5 were considered positive for PE to calculate sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV), diagnostic accuracy and 95% confidence intervals. Additionally, Receiver operating characteristic (ROC) analysis was performed to compare area under the curve (AUC) values.
Inter and intrareader agreement was assessed using Intraclass Correlation Coefficient (ICC) in a two-way mixed-effects model and interpreted as follows: ICC 0–0.20, slight; 0.21–0.40, fair; ICC 0.41–0.60, moderate; ICC 0.61–0.80, substantial; and ICC 0.81–1, almost perfect agreement.
A p-value ≤ 0.05 was considered a significant result.
Results
Radiation dose
Mean ED for extracted 90-kVp and linearly-blended 120-kVp image series were 1.1 ± 0.6 mSv and 1.7 ± 0.7 mSv, respectively (DLP, 77.5 ± 44 mGy*cm and 123.4 ± 51.1 mGy*cm; CTDIvol, 2.6 ± 1.7 mGy and 4.1 ± 2.0 mGy). Thus, 90-kVp CTPA acquisition resulted in a significant radiation dose reduction of 37% (all p < 0.001).
Quantitative image analysis
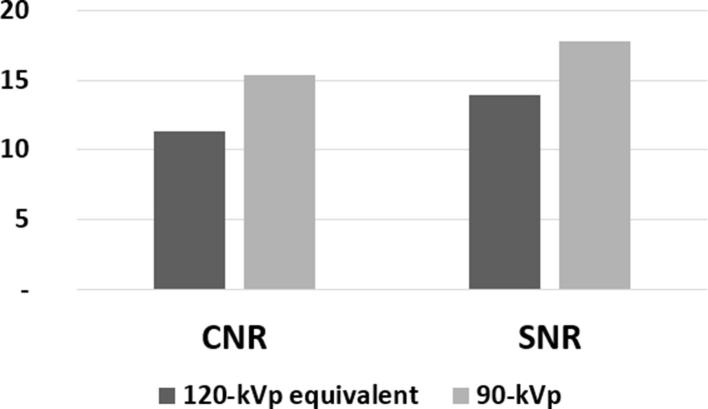
90-kVp image series showed significantly higher attenuation in the pulmonary trunk compared to linearly-blended M_0.6 series (mean attenuation, 373 ± 103.22 vs 285.47 ± 76.6 HU, p < 0.001) with simultaneously increased image noise (mean noise, 21.03 ± 3.3 vs 20.31 ± 2.89 HU, p < 0.001), resulting in significantly higher CNR and SNR values (mean CNR, 15.38 ± 6.26 vs 11.3 ± 4.6; mean SNR, 17.85 ± 6.41 vs 13.93 ± 4.75, all p < 0.001). Results of quantitative image analysis are displayed in Figure 1.
Figure 1.
Mean CNR and SNR of the pulmonary trunk for linearly-blended and 90-kVp image series. CNR, contrast-to-noise ratio; SNR, signal-to-noise ratio.
Diagnostic accuracy
According to the initial consensus reading, 9 of 40 patients (22.5%) were positive for central and segmental PE, while another 9 patients showed segmental PE only.
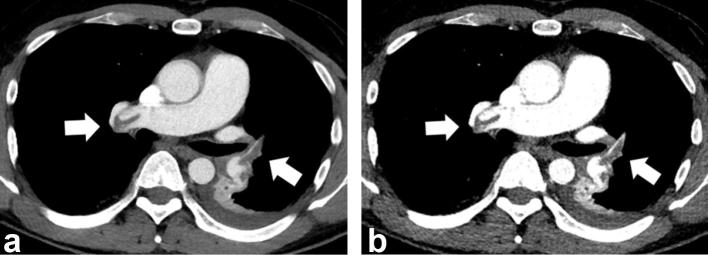
Results were comparable regarding diagnostic accuracy for central PE between both image series, with a diagnostic accuracy of 0.98 and AUC of 0.996 for 90 kVp images, while linearly-blended 120-kVp series showed a diagnostic accuracy of 0.98 and AUC of 0.995 (p = 0.48) (Figure 2). Diagnostic accuracy of 1.0 (AUC, 1.0) for the detection of segmental PE were similar excellent for both image series. Sensitivity, specificity, NPV and PPV are displayed in Table 1.
Figure 2.
Axial reformatted, 120-kVp equivalent linearly-blended M_0.6 (a) and 90-kVp (b) CTPA images of a 45-year-old male patient with bilateral central and segmental PE (arrows). 90-kVp provided higher vessel contrast and slightly increased noise compared to 120-kVp equivalent (M_0.6) series. While the suitability for artery assessment of both images is similar, radiation dose was reduced by 37.2% using 90-kVp acquisition (ED, 1.1 ± 0.6vs 1.7±0.7 mSv, p < 0.001). Window settings in both reconstructions were: level, 100 HU; width, 400 HU. CTPA, CT pulmonary angiography; HU, Hounsfield units; PE, pulmonary embolism.
Table 1.
Diagnostic accuracy for the evaluation of PE
| Parameter | Central PE | Segmental PE |
| Sensitivity | 1.0 | 1.0 |
| Specificity | 0.98 | 1.0 |
| PPV | 0.98 | 1.0 |
| NPV | 1.0 | 1.0 |
NPV, negative predictive value; PE, pulmonary embolism; PPV, positive predictive value.
Qualitative image analysis
Diagnostic confidence scores for overall PE assessment were good for both image series, but showed significantly higher confidence for linearly-blended images compared to 90-kVp images (4.1 ± 0.5 vs 3.8 ± 0.6, p < 0.001). Results for diagnostic confidence for central and segmental PE assessment comparing linearly-blended and 90-kVp series did not reach significance (central, 4.0 ± 0.4 vs 4.2 ± 0.4, p = 0.308; segmental, 3.8 ± 0.6 vs 3.5 ± 0.6, p = 0.063). Detailed results for qualitative image analysis are summarized in Table 2.
Table 2.
Diagnostic confidence in the assessment of PE
| Parameter | 120-kVp equivalent | 90-kVp | p-value |
| Overall confidence | 4.1 ± 0.5 | 3.8 ± 0.6 | <0.001 |
| Confidence central PE | 4.0 ± 0.4 | 4.2 ± 0.4 | 0.308 |
| Confidence segmental PE | 3.8 ± 0.6 | 3.5 ± 0.6 | 0.063 |
PE, pulmonary embolism.
Discussion
Our study showed that low-tube-voltage 90-kVp CTPA in combination with a recently introduced IR algorithm provides increased objective image quality resulting in similar excellent diagnostic accuracy and confidence for PE assessment compared to 120-kVp equivalent linearly-blended image series at significant lower radiation doses.
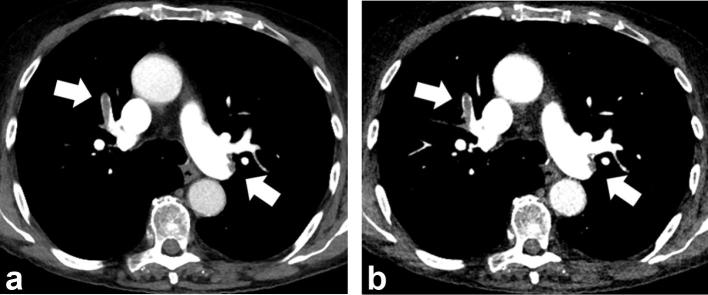
Dual-source CT scanners allow simultaneous acquisition of two image series at different tube voltage settings (DE mode). These datasets are mainly used for post-processing.13–15 One of these post-processing techniques is virtual monoenergetic imaging, which provides image series at virtual, low energy levels that have shown incremental image quality in CTA scans due to increased contrast with improved diagnostic accuracy of vascular pathologies.16, 17 A similar effect of increased contrast of iodinated structures can be reached by reducing tube voltage. Two technical developments overcame the limitation of increased image noise when scanning at lower tube voltages: increased tube capacity and further improvement of IR algorithms. When using IR techniques, low-tube-voltage CTA have shown similar good subjective image quality than standard 120-kVp images.18–21 A single vendor’s equipment was used for this study, however, CT scanners from other vendors provide similar IR software. In comparison to DE acquisitions which are usually performed with similar radiation doses as 120-kVp scans,22 reduced tube voltage lowers radiation exposure, while contrast is beneficially increased (Figure 3). The main drawback of scanning at lower tube voltages is the missing option for further post-processing provided by DE datasets. Thus, accurate contrast bolus is crucial with respect to varying factors such as CT scanner, contrast bolus and patient.
Figure 3.
Axial reformatted, 120-kVp equivalent M_0.6 (a) and 90-kVp (b) CTPA images of a 59-year-old male patient with bilateral central and segmental PE (arrows). 90-kVp images show greater attenuation of iodinated vessels and slightly increased noise, while the visualization of pulmonary arteries and, as such, diagnostic value of both image series remains similar. Window settings in both reconstructions were: level, 100 HU; width, 400 HU. CTPA, CT pulmonary angiography; HU, Hounsfield units.
In contrast to cancer staging and follow-up scans, CT-based assessment of PE is mostly performed in an acute setting, and often no follow-up CT study is available to perform a direct comparison between those images. For the present study, an intra-individual comparison of single-source 90-kVp and DE-based 120-kVp equivalent CTPA seemed to be a justified approach, as several confounders to image quality, such as different timing of contrast bolus, could be excluded. Bauer et al showed that linearly-blended DE image series based on merging 80-kVp and Sn-140-kVp acquisition of a second-generation dual-source CT scanner have similar image quality than 64-slice single-source 120-kVp image series.23
Viteri-Ramirez et al compared two low-kVp CTPA protocols in patients with up to 80 kg (176 lbs) body weight with reported ED values of 0.9 ± 0.6 mSv for the 80-kVp protocol and 2.3 ± 1 mSv for the 100-kVp protocol.24 Tube voltage selection in steps of 10 kV allows 90-kVp acquisition, which may be beneficial to body-weight depending selection between 80-kVp and 100-kVp protocols in clinical routine. However, further tube voltage reduction is possible with CTPA scans as low as 70-kVp in high-pitch mode with a radiation exposure as low as 0.92 mSv and a contrast bolus of only 15 ml.25 High-pitch mode uses both X-ray tubes simultaneously with similar tube voltage settings. This technique is favorable in patients unable to follow breathing instructions. However, high-pitch mode requires dual-source technique which is, so far, not widely available due to high cost. As most available CT scanners use single-source CT technique, research of low-tube-voltage techniques benefits a broader number of sites. Thus, CT settings for this study were set more conservative to provide a safe protocol for emergent CT imaging. Our results could show that 90-kVp CTPA scans in a non-selective patient cohort showed improved objective image quality compared to 120-kVp equivalent image series.
This study has some limitations apart from its vendor-specific nature and retrospective study design which need to be addressed. First, to allow an intra-individual comparison we did not use true 120-kVp datasets, but 120-kVp equivalent linearly-blended DE image series. This allowed us to reconstruct low-tube-voltage image series from the same acquisition for an intra-individual comparison independent from potential interfering factors such as variability in contrast medium bolus, body habitus, patient position, or scan settings. Second, our results were based on a small cohort of only 40 patients, which is acceptable for preliminary results, while further research in a larger patient cohort is necessary. Third, the reference standard of the study was not independent, as it was based on the same CTPA study.
In conclusion, 90-kVp CTPA in combination with Admire provides excellent suitability and similarly good diagnostic accuracy for the assessment of PE than 120-kVp equivalent linearly-blended image series, while lowering radiation dose by 37%.
Footnotes
The authors Doris Leithner and Tatjana Gruber-Rouh contributed equally to the work.
Contributor Information
Doris Leithner, Email: doris.leithner@gmail.com.
Tatjana Gruber-Rouh, Email: tgruberrouh@googlemail.com.
Martin Beeres, Email: beeres@gmx.net.
Julian L Wichmann, Email: docwichmann@gmail.com.
Scherwin Mahmoudi, Email: scherwin.mahmoudi@gmail.com.
Simon S Martin, Email: simartin@outlook.com.
Lukas Lenga, Email: l.lenga@gmx.de.
Moritz H Albrecht, Email: moritzalbrecht@gmx.net.
Christian Booz, Email: boozchristian@gmail.com.
Thomas J Vogl, Email: T.Vogl@em.uni-frankfurt.de.
Jan-Erik Scholtz, Email: janerikscholtz@gmail.com.
REFERENCES
- 1.Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galie N. ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014; 2014: 3033–69. [DOI] [PubMed] [Google Scholar]
- 2.Zhang LJ, Lu GM, Meinel FG, McQuiston AD, Ravenel JG, Schoepf UJ. Computed tomography of acute pulmonary embolism: state-of-the-art. Eur Radiol 2015; 25: 2547–57. doi: 10.1007/s00330-015-3679-2 [DOI] [PubMed] [Google Scholar]
- 3.Fanous R, Kashani H, Jimenez L, Murphy G, Paul NS. Image quality and radiation dose of pulmonary CT angiography performed using 100 and 120 kVp. AJR Am J Roentgenol 2012; 199: 990–6. doi: 10.2214/AJR.11.8208 [DOI] [PubMed] [Google Scholar]
- 4.Szucs-Farkas Z, Schibler F, Cullmann J, Torrente JC, Patak MA, Raible S, et al. Diagnostic accuracy of pulmonary CT angiography at low tube voltage: intraindividual comparison of a normal-dose protocol at 120 kVp and a low-dose protocol at 80 kVp using reduced amount of contrast medium in a simulation study. AJR Am J Roentgenol 2011; 197: W852–W859. doi: 10.2214/AJR.11.6750 [DOI] [PubMed] [Google Scholar]
- 5.Schueller-Weidekamm C, Schaefer-Prokop CM, Weber M, Herold CJ, Prokop M. CT angiography of pulmonary arteries to detect pulmonary embolism: improvement of vascular enhancement with low kilovoltage settings. Radiology 2006; 241: 899–907. doi: 10.1148/radiol.2413040128 [DOI] [PubMed] [Google Scholar]
- 6.Laqmani A, Kurfürst M, Butscheidt S, Sehner S, Schmidt-Holtz J, Behzadi C, et al. CT pulmonary angiography at reduced radiation exposure and contrast material volume using iterative model reconstruction and iDose4 technique in comparison to FBP. PLoS One 2016; 11: e0162429. doi: 10.1371/journal.pone.0162429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pontana F, Henry S, Duhamel A, Faivre JB, Tacelli N, Pagniez J, et al. Impact of iterative reconstruction on the diagnosis of acute pulmonary embolism (PE) on reduced-dose chest CT angiograms. Eur Radiol 2015; 25: 1182–9. doi: 10.1007/s00330-014-3393-5 [DOI] [PubMed] [Google Scholar]
- 8.Sauter A, Koehler T, Fingerle AA, Brendel B, Richter V, Rasper M, et al. Ultra low dose CT pulmonary angiography with lterative reconstruction. PLoS One 2016; 11: e0162716. doi: 10.1371/journal.pone.0162716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JW, Lee G, Lee NK, Moon JI, Ju YH, Suh YJ, et al. Effectiveness of adaptive statistical iterative reconstruction for 64-slice dual-energy computed tomography pulmonary angiography in patients With a reduced Iodine load: comparison with standard computed tomography pulmonary angiography. J Comput Assist Tomogr 2016; 40: 777–83. doi: 10.1097/RCT.0000000000000443 [DOI] [PubMed] [Google Scholar]
- 10.Nam SB, Jeong DW, Choo KS, Nam KJ, Hwang JY, Lee JW, et al. Image quality of CT angiography in young children with congenital heart disease: a comparison between the sinogram-affirmed iterative reconstruction (SAFIRE) and advanced modelled iterative reconstruction (ADMIRE) algorithms. Clin Radiol 2017; 72: 1060–5. doi: 10.1016/j.crad.2017.07.006 [DOI] [PubMed] [Google Scholar]
- 11.Gassenmaier T, Distelmaier I, Weng AM, Bley TA, Klink T. Impact of advanced modeled iterative reconstruction on interreader agreement in coronary artery measurements. Eur J Radiol 2017; 94: 201–8. doi: 10.1016/j.ejrad.2017.06.029 [DOI] [PubMed] [Google Scholar]
- 12.Wichmann JL, Kraft J, Nöske EM, Bodelle B, Burck I, Scholtz JE, et al. Low-tube-voltage 80-kVp neck CT: evaluation of diagnostic accuracy and interobserver agreement. AJNR Am J Neuroradiol 2014; 35: 2376–81. doi: 10.3174/ajnr.A4052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leithner D, Wichmann JL, Vogl TJ, Trommer J, Martin SS, Scholtz JE, et al. Virtual monoenergetic imaging and Iodine perfusion maps improve diagnostic accuracy of dual-energy computed tomography pulmonary angiography with suboptimal contrast attenuation. Invest Radiol 2017; 52: 659–65. doi: 10.1097/RLI.0000000000000387 [DOI] [PubMed] [Google Scholar]
- 14.Nute JL, Le Roux L, Chandler AG, Baladandayuthapani V, Schellingerhout D, Cody DD. Differentiation of low-attenuation intracranial hemorrhage and calcification using dual-energy computed tomography in a phantom system. Invest Radiol 2015; 50: 9–16. doi: 10.1097/RLI.0000000000000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Albrecht MH, Trommer J, Wichmann JL, Scholtz JE, Martin SS, Lehnert T, et al. Comprehensive comparison of virtual monoenergetic and linearly blended reconstruction techniques in third-generation dual-source dual-energy computed tomography angiography of the thorax and abdomen. Invest Radiol 2016; 51: 582–90. doi: 10.1097/RLI.0000000000000272 [DOI] [PubMed] [Google Scholar]
- 16.Martin SS, Wichmann JL, Weyer H, Scholtz JE, Leithner D, Spandorfer A, et al. Endoleaks after endovascular aortic aneurysm repair: Improved detection with noise-optimized virtual monoenergetic dual-energy CT. Eur J Radiol 2017; 94: 125–32. doi: 10.1016/j.ejrad.2017.06.017 [DOI] [PubMed] [Google Scholar]
- 17.Weiss J, Notohamiprodjo M, Bongers M, Schabel C, Mangold S, Nikolaou K, et al. Noise-optimized monoenergetic post-processing improves visualization of incidental pulmonary embolism in cancer patients undergoing single-pass dual-energy computed tomography. Radiol Med 2017; 122: 280–7. doi: 10.1007/s11547-016-0717-3 [DOI] [PubMed] [Google Scholar]
- 18.Sun J, Zhang Q, Hu D, Duan X, Peng Y. Improving pulmonary vessel image quality with a full model-based iterative reconstruction algorithm in 80kVp low-dose chest CT for pediatric patients aged 0-6 years. Acta Radiol 2015; 56: 761–8. doi: 10.1177/0284185114540884 [DOI] [PubMed] [Google Scholar]
- 19.Husarik DB, Schindera ST, Morsbach F, Chuck N, Seifert B, Szucs-Farkas Z, et al. Combining automated attenuation-based tube voltage selection and iterative reconstruction: a liver phantom study. Eur Radiol 2014; 24: 657–67. doi: 10.1007/s00330-013-3049-x [DOI] [PubMed] [Google Scholar]
- 20.Scholtz JE, Wichmann JL, Hüsers K, Beeres M, Nour-Eldin NE, Frellesen C, et al. Automated tube voltage adaptation in combination with advanced modeled iterative reconstruction in thoracoabdominal third-generation 192-slice dual-source computed tomography: effects on image quality and radiation dose. Acad Radiol 2015; 22: 1081–7. doi: 10.1016/j.acra.2015.05.010 [DOI] [PubMed] [Google Scholar]
- 21.May MS, Wüst W, Brand M, Stahl C, Allmendinger T, Schmidt B, et al. Dose reduction in abdominal computed tomography: intraindividual comparison of image quality of full-dose standard and half-dose iterative reconstructions with dual-source computed tomography. Invest Radiol 2011; 46: 465–70. doi: 10.1097/RLI.0b013e31821690a1 [DOI] [PubMed] [Google Scholar]
- 22.Tawfik AM, Kerl JM, Razek AA, Bauer RW, Nour-Eldin NE, Vogl TJ, et al. Image quality and radiation dose of dual-energy CT of the head and neck compared with a standard 120-kVp acquisition. AJNR Am J Neuroradiol 2011; 32: 1994–9. doi: 10.3174/ajnr.A2654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bauer RW, Kramer S, Renker M, Schell B, Larson MC, Beeres M, et al. Dose and image quality at CT pulmonary angiography-comparison of first and second generation dual-energy CT and 64-slice CT. Eur Radiol 2011; 21: 2139–47. doi: 10.1007/s00330-011-2162-y [DOI] [PubMed] [Google Scholar]
- 24.Viteri-Ramírez G, García-Lallana A, Simón-Yarza I, Broncano J, Ferreira M, Pueyo JC, et al. Low radiation and low-contrast dose pulmonary CT angiography: comparison of 80 kVp/60 ml and 100 kVp/80 ml protocols. Clin Radiol 2012; 67: 833–9. doi: 10.1016/j.crad.2011.11.016 [DOI] [PubMed] [Google Scholar]
- 25.Du Q, Sui X, Song W, Song L, Xu X. Application of high-pitch CT pulmonary angiography at 70 kV tube voltage with 15 ml contrast medium using third-generation dual-source CT. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2017; 39: 28–33. doi: 10.3881/j.issn.1000-503X.2017.01.006 [DOI] [PubMed] [Google Scholar]