Abstract
MRI is an excellent diagnostic tool in the imaging of sports-related musculoskeletal pathology; however, standard slice thickness acquisitions can lack the spatial resolution to accurately define and characterise osseous abnormalities. Standard MRI sequences may be supplemented with CT to reduce diagnostic uncertainty. We provide a clinical perspective, in the form of pictorial review, on the potential applications of 3D MRI sequences, specifically using volumetric interpolated breath-hold examination in the characterisation of various musculoskeletal osseous pathologies. The potential to negate the requirement for CT in a young radiation sensitive cohort is a clinically significant concept and suggests the requirement for further studies comparing the performance of volumetric MRI to CT.
Introduction
3D volumetric MRI is playing an increasingly important role in musculoskeletal diagnostic imaging.1 3D volumetric acquisitions have the advantage of improving through plane spatial resolution and generate high-quality reformats to yield multiplanar images from the original dataset. Volumetric interpolated breath-hold examination (VIBE) is a form of volumetric imaging using fast 3D gradient-echo sequences that produces T1 images and was first introduced by Rofsky in 1999.2 It has the advantage of improving Z-axis resolution, which makes it possible to obtain high-quality multiplanar and 3D reconstruction images. VIBE has been effectively used in abdominal and breast imaging,3, 4 where short “breath-hold” length acquisitions, typically less than 30 s, are required to obtain dynamic, high-resolution T1 weighted tissue imaging minimally affected by respiratory movement. VIBE sequences are characterised by lower signal characteristics of fluid compared to standard T1 weighted images, otherwise, the appearances are similar to standard T1 weighted images.
As with standard T1, VIBE images have low contrast resolution for soft tissue and chondral pathology compared to other MRI sequences. Consequently, VIBE sequences have been of limited use in musculoskeletal imaging. However, there is high intrinsic tissue contrast between cortical bone and fatty marrow, and to a lesser extent, between bone and muscle. By applying high-resolution, small field of view (FoV) imaging to a part of the musculoskeletal system that has such high intrinsic contrast resolution, VIBE sequences can be utilised to clearly define normal cortical bony anatomy when surrounded by fat and muscle. Furthermore, mineralising callus and fibrous tissue within bone have similar signal to soft tissues on VIBE sequences, and therefore a relatively high intrinsic contrast resolution that allows ready identification of intra-cortical bone pathology. When standard images are inverted and windowed, VIBE MRI can generate high-resolution volumetric imaging of bony pathology. The images can then be inverted to resemble a similar attenuation pattern to CT.
The majority of our athletic patients are young and are having MRI examinations for musculoskeletal injury. The most clinically useful application for VIBE sequences in athletes visiting our clinic has been in the identification of traumatic osseous injury. By adding in VIBE sequences to our standard protocol, we are attempting to negate the requirement for supporting CT and its accompanying radiation exposure.
VIBE sequences at our clinic have been produced on a Siemens Magnetom 1.5T Aera & Siemens Magnetom 3T Skyra. In spinal imaging looking for stress fractures, acquisitions are run as a 3D slab with 200 × 200 mm FoV, 1.5–2 mm slice thickness, 80 mm slab thickness, fat suppression, TR 6–8, TE 3–5 ms, BW 200–220 Hz/Px, 12 deg flip angle, 0.4 × 0.4 × 2 mm voxels, slab selective Volume.
For extremities that allow the use of a higher density coil (hence greater signal) we use an isotropic 3D sequence, allowing 3D reconstructions. This is run with 0.4–0.5 mm voxels, 140–150 mm FoV, variable slab thickness (depending on region being covered). The images are then inverted to resemble a similar attenuation pattern to that of a CT image.
Lumbar Osseous Stress Injury
In the investigation of lumbar osseous stress injury, MRI has demonstrated similar sensitivity and specificity to CT in the detection of complete pars fractures, with or without marrow oedema.5 However, when assessing for the presence of incomplete pars fractures CT has long been regarded as the “gold standard” especially for mature incomplete fractures that are sclerotic without marrow oedema. Incomplete pars fractures are most commonly seen to involve the infero-medial cortex of the pars. Accurately identifying the position, size and orientation of the fracture can guide patient management and imaging follow-up.6 Dunn et al6 reviewed the appearances of incomplete pars fractures in adolescent patients using CT and standard MRI sequences. They concluded that CT was the superior modality to detect size and extent of incomplete pars fractures and was the most appropriate tool for follow-up. We share this view, finding standard MRI sequences limited in their ability to detect incomplete stress fractures especially in the absence of marrow oedema.
Ang et al recently compared 3D VIBE MRI with multislice CT for the detection of pars stress fractures of the lumbar spine.7 3 T MRI and CT of 24 patients involving 70 pars interarticularis were retrospectively reviewed. The fracture morphology (complete, incomplete or normal) was assessed on MRI and CT. They concluded that 3D T1 VIBE is 100% accurate in diagnosing complete pars fractures and has comparative diagnostic ability to CT in the detection and characterisation of incomplete pars stress fractures with sensitivity and specificity of 96.7 and 92% respectively.
When included in a lumbar spine MRI protocol for lumbar stress injury, VIBE sequences can reduce the need for complementary diagnostic and follow-up CT imaging of the lumbar spine in a radiation sensitive population (Figures 1–3).
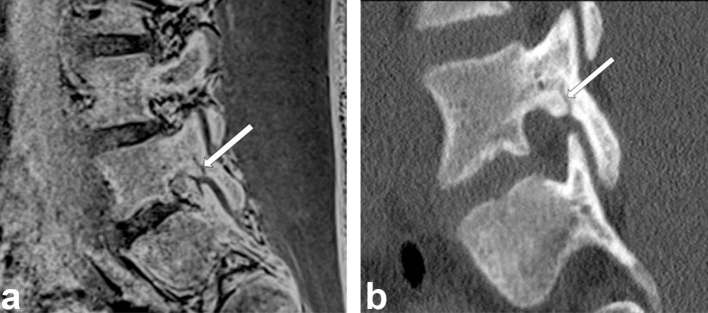
Figure 1.
A 22-year-old fast bowling cricketer with left-sided lower lumbar pain. (a) Inverted sagittal VIBE MRI (1.5 mm slice thickness, contiguous) and sagittal reconstructed (2 mm slice thickness). (b) Targeted CT of L5 performed on the same day show morphologically identical appearances of an incomplete posterior lumbar stress injury (arrows). VIBE, volumetric interpolated breath-hold examination.
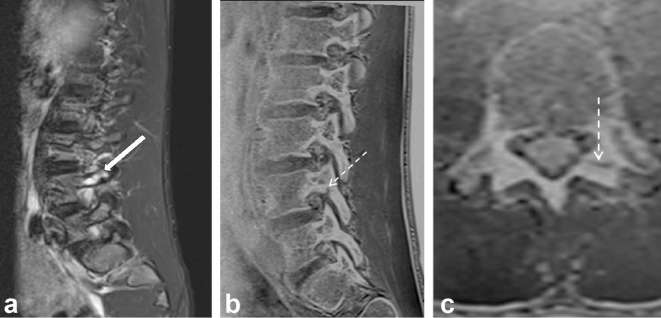
Figure 2.
A 25-year-old fast bowling cricketer with left lower lumbar pain. (a) Routine sagittal T2 FS MRI showing left L4 pedicle marrow oedema (arrow). The osseous nature of the posterior lumbar bone stress injury is not characterised. (b and c) Inverted sagittal and reconstructed axial VIBE MRI clearly resolve an incomplete posterior lumbar stress fracture (dash arrow) due to the increased spatial and contrast resolution.
Figure 3.
A 27-year-old fast bowling cricketer with lower lumbar pain. VIBE MRI is able to document healing of posterior lumbar stress injury. (a) Sagittal reconstructed CT. (b) Inverted VIBE MRI image, with hardened windows, performed on the same day shows an early incomplete posterior lumbar stress fracture (arrows). (c) Inverted sagittal VIBE MRI at 4 weeks shows a more prominent L4 pars fracture (arrow) due to resorption of cartilaginous callus in normal bone healing in a clinically quiescent injury. (d and e) Inverted sagittal VIBE MRI shows radiological correlation of progression to clinical healing at 12 and 16 weeks (arrows). The craniocaudal extent of the fracture has reduced at 12 weeks and there is increasing mineralisation at 12 and 16 weeks scan. VIBE, volumetric interpolated breath-hold examination.
Shoulder Instability
MRI is a proven useful tool in the detection of shoulder soft tissue injury, particularly when assessing the labrum with MRI arthrography.8
Vandevenne et al looked at VIBE MR arthrography to assess the rotator cuff.9 82 patients underwent direct MR arthrography of the shoulder joint using VIBE on a 1.0 T MR. T1-FS sequences were considered the gold standard and surgical correlation was only available in a small sample. Sensitivity and specificity of VIBE were greater than 92% for large articular-sided partial thickness and full thickness tears. However, the sensitivity and specificity for fraying and partial thickness tears were less. They concluded fast MR arthrography using VIBE was a valid alternative to standard T1-FS sequences for large articular-sided tears.
In the detection of accompanying osseous glenoid rim injuries, standard MRI sequences and MRI arthrography can lack the spatial resolution. CT has gained popularity by orthopaedic surgeons in pre-operative planning to more accurately identify and quantify osseous glenoid rim injuries.10
3D volumetric MRI sequences such as VIBE can also be used to more accurately characterise osseous glenoid rim injuries (Figure 4).
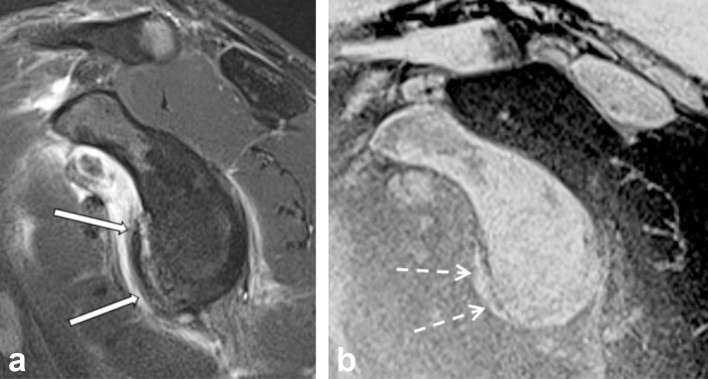
Figure 4.
A 26-year-old AFL player post anterior shoulder dislocation. (a) Sagittal oblique T2 FS MRI showing anterior Bankart lesion. Partial volume artefact due to greater slice thickness impairs characterisation of bony Bankart injury (arrows). (b) Sagittal VIBE MRI (1 mm slice thickness) more accurately defines the size and morphology of the bony Bankart lesion (dashed arrows). VIBE, volumetric interpolated breath-hold examination. AFL, australian football league.
Tian et al compared 3D VIBE sequences with CT in the detection of traumatic glenoid lesions.11 Fat-suppressed 3D VIBE MR arthrography and MSCT were performed in 56 patients. Compared with multislice CT, the sensitivity and specificity of fat-suppressed 3D VIBE images in detecting bony Bankart lesions were 95.7–100% and 93.9–97.0%, respectively, and those in predicting glenoid bone loss were 95.0 and 93.8%, respectively.
Stillwater et al recently compared the osseous reformats of 3D-MR vs 3D-CT in patients with glenohumeral instability.12 The results suggested 3D-MR performed as well as CT with no statistical significance between measured parameters of humeral height, glenoid height and glenoid width.
Loose Bodies
CT arthrography is a popular method in the detection of intraarticular loose bodies particularly in the elbow with a reported ability to detect loose bodies as small as 3 mm. There is however limited research to support the claim that CT arthrography is a sensitive and specific method. Gadolinium-enhanced MR arthrography has demonstrated a high accuracy in the detection of osseous and cartilaginous bodies combined and was significantly better than standard MR sequences (92 to 57–70%) accuracy respectively.13
Dubberly compared MRI with 3D volumetric sequences to CT arthrography in 26 consecutive patients with mechanical elbow symptoms.14 MRI studies were performed on a 1.5 T magnet. Images were produced using 3D gradient echo T2 weighted with a slice thickness of 1.5 mm reconstructed in all three planes. No gadolinium contrast was administered. Both MRI and CT arthrography had excellent sensitivity (92 to 100%) but low to moderate specificity (15 to 77%) in identifying posteriorly based loose bodies. Neither MRI nor CT arthrography was consistently sensitive (46 to 91%) or specific (13 to 73%) in predicting the presence or absence of loose bodies anteriorly.
We appreciate that MRI has limited sensitivity in the detection of loose bodies and oedematous and/or small loose bodies in complex joints, particularly when surrounded by synovitis, may be very difficult to perceive on routine MRI sequences. We anecdotally find VIBE sequences are a useful adjunct in defining loose bodies from small osteophytes (Figure 5).
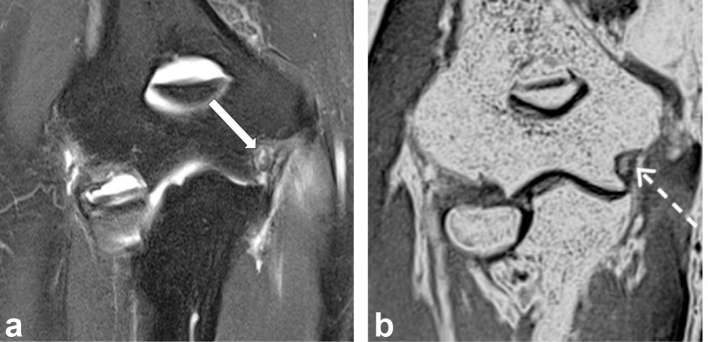
Figure 5.
A 27-year-old fast bowling cricketer with medial elbow pain, instability symptoms and clicking. (a) Coronal T2 FS MRI shows an oedematous focus (arrows) that is difficult to perceive on routine coronal T2 FS image due to surrounding medial elbow synovitis and ligament oedema. (b) Coronal VIBE MRI shows the ossified loose body more distinctly from adjacent synovitis. VIBE, volumetric interpolated breath-hold examination.
Osseous Coalition
Tarsal coalition is defined as abnormal bridging across two or more of the tarsal bones and favoured to be secondary to segmentation of the primitive mesenchyme during development.15 This can be in the form of cartilaginous (synchondrosis), fibrous (synfibrosis or syndesmosis) or osseous (synostosis). When assessing for osseous coalition, CT is considered the gold standard. Emery et al compared the performance of CT vs MRI in the diagnosis of tarsal coalition in 20 consecutive patients.16 Coalition was divided into complete (osseous) or incomplete (non-osseous). They concluded that MRI had a high rate of agreement to CT in tarsal coalition. However CT is still regarded as the “gold standard” for detecting osseous coalition. We are not aware of any studies directly comparing the accuracy of 3D MRI sequences vs CT but we have found VIBE sequences particularly informative when characterising coalition and may obviate the need for ionising radiation in this predominantly skeletally immature population (Figures 6 and 7).
Figure 6.
A 13-year-old with bilateral ankle pain and stiffness. (a) Sagittal PD MRI of the right ankle. (b) Sagittal inverted VIBE MRI demonstrates fibro-osseous talocalcaneal coalition, with bone bridging more conspicuous (arrows). (c) Coronal reconstructed VIBE MRI allows multiplanar evaluation of the fibro-osseous coalition (dashed arrow). VIBE, volumetric interpolated breath-hold examination.
Figure 7.
A 30-year-old with persistent left wrist pain following crush injury. Initial MRI diagnosed carpal fractures and capitate-hamate articular injury. (a and b) Four-month follow-up coronal T2 FS and inverted coronal VIBE MRI demonstrates the presence of ongoing marrow oedema following previous trauma to a mis-diagnosed fibro-osseous coalition between the capitate and hamate (arrows). VIBE, volumetric interpolated breath-hold examination.
Medial Tibial Stress Syndrome
Medial tibial stress syndrome (MTSS), also known as shin splints, is a common overuse injury characterised by local pain that occurs during exercise at the medial surface of the distal two thirds of the tibial shaft. Gaeta et al prospectively compared MRI, CT and bone scintigraphy in the assessment of MTSS in 42 patients experiencing pain due to early stress injuries.17 They found MRI to be the superior imaging modality with the greatest sensitivity and specificity (88 and 100%) respectively. In another study Gaeta et al concluded that CT was a particularly useful tool in detecting the early cortical osteopenic change associated with medial tibial stress response .18
The Fredericson classification has been adopted as an MRI grading system for tibial stress injuries.19 This system is graded from 1 to 4 based on MRI imaging findings and was later reviewed by Kijowski et al in a large retrospective review correlating with clinical severity and outcome. They further subdivide Grade 4 injuries into 4A and 4B, with 4B being of a significantly higher grade based on increased time to return to sports activity. 4B stress injuries are defined by a visible fracture line in the tibial cortex.20 CT has long been used as a useful adjunct in the detection of cortical fracture lines in tibial stress fractures.21
From our experience, VIBE sequences perform as well as CT in the detection of intra-cortical fracture lines in MTSS Figure 8.
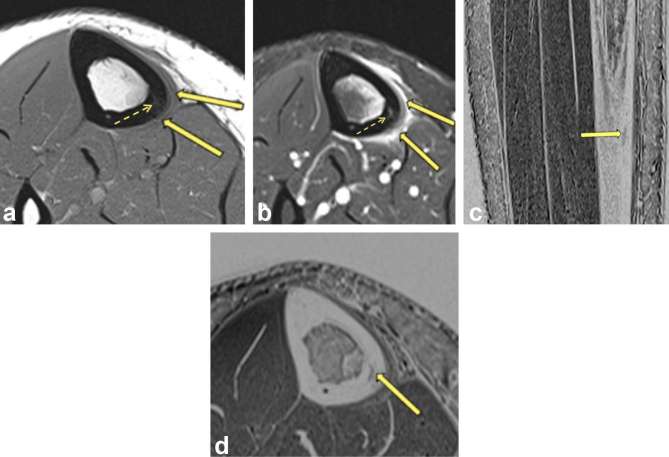
Figure 8.
A 32-year-old marathon runner with medial shin pain. (a and b) Axial PD and T2 FS MRI shows posteromedial tibial periostitis (arrows), marrow oedema and intra-cortical signal changes (dotted arrow), compatible with stress fracture. It is difficult to determine Grade 4A vs 4B (c and d). Sagittal and axial VIBE MRI confirms a well-defined intra-cortical fracture (arrows) of the posteromedial tibia compatible with Fredericson Grade 4B MTSS. VIBE, volumetric interpolated breath-hold examination.
Conclusion
3D MRI in the form of VIBE is a useful tool in the assessment of musculoskeletal osseous injury. VIBE has proven value in the assessment of lumbar stress injury and could potentially negate the requirement for supplementary CT in other musculoskeletal conditions in a young radiation sensitive cohort. This clinically significant concept suggests the requirement for further studies comparing the performance of volumetric MRI to CT.
Contributor Information
Eamon Koh, Email: eamon.koh@gmail.com.
Edward RJ Walton, Email: edwardwalton@hotmail.co.uk.
Phil Watson, Email: pwatson@envisionmi.com.au.
REFERENCES
- 1.Naraghi A, White LM. Three-dimensional MRI of the musculoskeletal system. AJR Am J Roentgenol 2012; 199: W283–W293. doi: 10.2214/AJR.12.9099 [DOI] [PubMed] [Google Scholar]
- 2.Rofsky NM, Lee VS, Laub G, Pollack MA, Krinsky GA, Thomasson D, et al. . Abdominal MR imaging with a volumetric interpolated breath-hold examination. Radiology 1999; 212: 876–84. doi: 10.1148/radiology.212.3.r99se34876 [DOI] [PubMed] [Google Scholar]
- 3.Nakayama S, Kakizaki D, Kaise H, Kusama M, Ishikawa A, Amino M, et al. . Three-dimentional volumetric interpolated breath-hold magnetic resonance imaging for the diagnosis of breast tumors. Nihon Rinsho 2004; 62: 790–8. [PubMed] [Google Scholar]
- 4.Vogt FM, Antoch G, Hunold P, Maderwald S, Ladd ME, Debatin JF, et al. . Parallel acquisition techniques for accelerated volumetric interpolated breath-hold examination magnetic resonance imaging of the upper abdomen: assessment of image quality and lesion conspicuity. J Magn Reson Imaging 2005; 21: 376–82. doi: 10.1002/jmri.20288 [DOI] [PubMed] [Google Scholar]
- 5.Ganiyusufoglu AK, Onat L, Karatoprak O, Enercan M, Hamzaoglu A. Diagnostic accuracy of magnetic resonance imaging versus computed tomography in stress fractures of the lumbar spine. Clin Radiol 2010; 65: 902–7. doi: 10.1016/j.crad.2010.06.011 [DOI] [PubMed] [Google Scholar]
- 6.Dunn AJ, Campbell RS, Mayor PE, Rees D. Radiological findings and healing patterns of incomplete stress fractures of the pars interarticularis. Skeletal Radiol 2008; 37: 443–50. doi: 10.1007/s00256-008-0449-0 [DOI] [PubMed] [Google Scholar]
- 7.Ang EC, Robertson AF, Malara FA, O'Shea T, Roebert JK, Schneider ME, et al. . Diagnostic accuracy of 3-T magnetic resonance imaging with 3D T1 VIBE versus computer tomography in pars stress fracture of the lumbar spine. Skeletal Radiol 2016; 45: 1533–40. doi: 10.1007/s00256-016-2475-7 [DOI] [PubMed] [Google Scholar]
- 8.Pavic R, Margetic P, Bensic M, Brnadic RL. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury 2013; 44(Suppl 3): S26–S32. doi: 10.1016/S0020-1383(13)70194-3 [DOI] [PubMed] [Google Scholar]
- 9.Vandevenne JE, Vanhoenacker F, Mahachie John JM, Gelin G, Parizel PM. Fast MR arthrography using VIBE sequences to evaluate the rotator cuff. Skeletal Radiol 2009; 38: 669–74. doi: 10.1007/s00256-009-0677-y [DOI] [PubMed] [Google Scholar]
- 10.Moroder P, Resch H, Schnaitmann S, Hoffelner T, Tauber M. The importance of CT for the pre-operative surgical planning in recurrent anterior shoulder instability. Arch Orthop Trauma Surg 2013; 133: 219–26. doi: 10.1007/s00402-012-1656-7 [DOI] [PubMed] [Google Scholar]
- 11.Tian CY, Shang Y, Zheng ZZ. Glenoid bone lesions: comparison between 3D VIBE images in MR arthrography and nonarthrographic MSCT. J Magn Reson Imaging 2012; 36: 231–6. doi: 10.1002/jmri.23622 [DOI] [PubMed] [Google Scholar]
- 12.Stillwater L, Koenig J, Maycher B, Davidson M. 3D-MR vs. 3D-CT of the shoulder in patients with glenohumeral instability. Skeletal Radiol 2017; 46: 325–31. doi: 10.1007/s00256-016-2559-4 [DOI] [PubMed] [Google Scholar]
- 13.Brossmann J, Preidler KW, Daenen B, Pedowitz RA, Andresen R, Clopton P, et al. . Imaging of osseous and cartilaginous intraarticular bodies in the knee: comparison of MR imaging and MR arthrography with CT and CT arthrography in cadavers. Radiology 1996; 200: 509–17. doi: 10.1148/radiology.200.2.8685349 [DOI] [PubMed] [Google Scholar]
- 14.Dubberley JH, Faber KJ, Patterson SD, Garvin G, Bennett J, Romano W, et al. . The detection of loose bodies in the elbow. J Bone Joint Surg Br 2005; 87-B: 684–6. doi: 10.1302/0301-620X.87B5.14851 [DOI] [PubMed] [Google Scholar]
- 15.Jack EA. Bone anomalies of the tarsus in relation to peroneal spastic flat foot. J Bone Joint Surg Br 1954; 36-B: 530–42. doi: 10.1302/0301-620X.36B4.530 [DOI] [PubMed] [Google Scholar]
- 16.Emery KH, Bisset GS, Johnson ND, Nunan PJ. Tarsal coalition: a blinded comparison of MRI and CT. Pediatr Radiol 1998; 28: 612–6. doi: 10.1007/s002470050430 [DOI] [PubMed] [Google Scholar]
- 17.Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, et al. . CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology 2005; 235: 553–61. doi: 10.1148/radiol.2352040406 [DOI] [PubMed] [Google Scholar]
- 18.Gaeta M, Minutoli F, Vinci S, Salamone I, D’Andrea L, Bitto L, et al. . High-resolution CT grading of tibial stress reactions in distance runners. AJR Am J Roentgenol 2006; 187: 789–93. doi: 10.2214/AJR.05.0303 [DOI] [PubMed] [Google Scholar]
- 19.Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med 1995; 23: 472–81. doi: 10.1177/036354659502300418 [DOI] [PubMed] [Google Scholar]
- 20.Kijowski R, Choi J, Shinki K, Del Rio AM, De Smet A. Validation of MRI classification system for tibial stress injuries. AJR Am J Roentgenol 2012; 198: 878–84. doi: 10.2214/AJR.11.6826 [DOI] [PubMed] [Google Scholar]
- 21.Feydy A, Drapé J, Beret E, Sarazin L, Pessis E, Minoui A, et al. . Longitudinal stress fractures of the tibia: comparative study of CT and MR imaging. Eur Radiol 1998; 8: 598–602. doi: 10.1007/s003300050442 [DOI] [PubMed] [Google Scholar]