Abstract
Weight bias (negative attitudes towards individuals with obesity) has been widely observed, but not examined in parents. In this study, we measured parents’ (N=658; 74.2% female) explicit and implicit weight bias against children with obesity. Many parents (n=612; 93%) endorsed some moderate explicit weight bias. Fathers had greater explicit bias than mothers and parents with overweight/obesity had less bias than those with healthy-weight. Other parent/child variables (i.e., parent age, child sex, child weight, child age) were not significantly associated with explicit bias. Parents also demonstrated implicit weight bias. No parent or child variables were significantly associated with implicit bias. Parents may contribute, among many others, to the stigmatizing environment experienced by youth with overweight/obesity, which has been associated with negative child psychosocial functioning and health. Clinical research into strategies to reduce parental weight bias against children with obesity or increase children’s resilience to weight discrimination is needed to improve children’s health and well-being.
Keywords: implicit bias, weight stigma, body image, parents
Parents Have Both Implicit and Explicit Biases Against Children with Obesity
Weight bias—negative attitudes and stereotypes about individuals solely based on excess weight—has been documented across many groups, including adults across the weight spectrum (Carels et al., 2009), and children (even children as young as 3 years old) (Pont et al., 2017; Skinner et al., 2017). Perhaps most surprisingly, health care providers specializing in obesity demonstrate implicit and explicit weight bias (Tomiyama et al., 2015). The extent of weight bias found in these studies is comparable to biases against other groups associated with negative stereotypes, including racial minorities.
Obesity has increased over the past few decades, and so has bias against individuals with obesity (Puhl & Heuer, 2009). Weight discrimination—the behavioral expression of weight bias—has been documented across many life domains, including work, health care, mass media, and relationships (Puhl & Heuer, 2009) and is associated with medical problems such as diabetes, cardiac problems, and gastrointestinal problems (Udo, Purcell, & Grilo, 2016), even when adjusting for other forms of discrimination (Udo & Grilo, 2017). Among children, relational discrimination is particularly relevant and manifests at school and at home; much attention has been paid to weight-related teasing and bullying (Pont et al., 2017). Children with obesity who experience weight bias have severely impaired quality of life, indeed, even greater deficits than impairments in quality of life experienced by children with cancer (Schwimmer, Burwinkle, & Varni, 2003). Children who experience weight bias feel worse about themselves and their bodies, and have greater risk for depression, eating disorders, worsening obesity, and health problems.
It is important to distinguish between explicit and implicit weight bias, both conceptually and methodologically. Explicit attitudes are conscious and stated, for example, a belief that individuals with obesity are to blame for their weight. Implicit attitudes, on the other hand, are automatic initial reactions. Individuals may not recognize or report implicit attitudes, but express them in tasks that assess associations of a characteristic with positive and negative attributes.
The implicit association test (IAT) is well-established and measures implicit associations by comparing reaction times for congruent pairings with reaction times for incongruent pairings (Greenwald, McGhee, & Schwartz, 1998; Greenwald, Poehlman, Uhlmann, & Banaji, 2009; Hofmann, Gawronski, Gschwendner, Le, & Schmitt, 2005; Nosek, Greenwald, & Banaji, 2005). Weight-related IATs have shown evidence of implicit associations of excess weight with negative words (Carels et al., 2009; Phelan et al., 2015; Tomiyama et al., 2015). Much of this work has focused on adult obesity or obesity more generally (i.e., unspecified age group); however, two studies used the IAT and found that undergraduate students in training to become physical education teachers had implicit weight bias against children with obesity (Lynagh, Cliff, & Morgan, 2015; O’Brien, Hunter, & Banks, 2007).
Importantly, there is some evidence that implicit bias can lead to discrimination. For example, one study looked at hiring discrimination among candidates matched on credentials but differing in weight status, and found that implicit (but not explicit) attitudes about people with obesity were associated with the likelihood that the candidate would be invited for an interview (Agerstrom & Rooth, 2011). Implicit weight bias also affects outcomes among individuals seeking weight loss treatment; for example, weight bias has been associated with less self-monitoring, greater caloric intake and treatment drop out (Carels et al., 2009). In a review of the effects of implicit biases, Greenwald and colleagues (2015) provide empirical evidence for the extent to which implicit biases can have an impact on society through discrimination. They conceptualized the influence of implicit bias on society as accumulations of many small effects, or repeated effects on a minority of individuals, noting the “four-fifths” rule established by courts (U.S. Equal Employment Opportunity Commission, 1978, § 1607.4.D) as a means of quantifying discrimination. The “four-fifths” rule states that when a marginalized group receives favorable treatment at a rate less than eighty percent as often as the majority group, this is evidence that the marginalized group is experiencing an adverse impact. Children with obesity are a marginalized group in the sense that they experience weight bias and weight-related discrimination, accumulations of which severely impair children’s health and quality of life (Pont et al., 2017).
The present study aimed to extend the literature on weight bias by asking whether parents had implicit negative attitudes towards children with obesity, and whether parents reported explicit negative attitudes towards children with obesity. Based on the emerging weight bias literature, we hypothesized that parents would show implicit bias but would deny explicit bias towards children with obesity (O’Brien et al., 2007; Puhl & Latner, 2007). We also hypothesized that parents with obesity themselves or who have children with obesity would show less implicit and explicit bias against children with obesity because they would have empathy and positive contact with people with obesity, which is known to reduce bias (e.g., Phelan et al., 2015; Teachman, Gapinski, Brownell, Rawlins, & Jeyaram, 2003).
Method
Participants
Participants (N=658) were recruited from the Mechanical Turk recruitment platform to complete an online “cognitive task” and an online survey about parents’ opinions about weight and eating. Parents were eligible if they were a primary caregiver for a child 5-15 years old. Mechanical Turk provides high-quality and convenient data and yields samples with greater diversity in geography and demographic characteristics than undergraduate samples. Recent comparisons indicate psychometric properties of measures completed by Mechanical Turk participants do not differ in reliability or validity from participants recruited using traditional sources, and Mechanical Turk has growing popularity for both survey-based and experimental social science research (Buhrmester, Kwang, & Gosling, 2011). This study was reviewed and approved by our university’s institutional review board; all participants provided informed consent.
Parents in this study included both fathers (n=169, 25.7%) and mothers (n=488, 74.2%), not recruited as dyads. Most were biological parents (n=608). Average parent age was 36.81 years (SD=7.96). Parents had an average BMI of 28.14 kg/m2 (SD=7.33); categorically, 39.5% of parents (n=260) had a BMI in the overweight or obesity range. Most parents were non-Hispanic White (n=536; 81.5%) and well-educated (college degree or higher, n=333, 50.6%, or some college, n=264, 38.6%). Parents were instructed to answer questions about one child. Children were sons (n=320, 48.9%) and daughters (n=334, 51.1%), and were, on average, 9.44 years old (SD=2.90). The average BMI z-score for children, based on CDC growth charts accounting for age and sex, was 0.64 (SD=1.30), or the 65.93rd percentile (SD=32.82); categorically, 42.2% of children (n=278) had a BMI percentile in the overweight or obesity range.
Measures
Demographic and Health Characteristics
Parents reported the age, height and weight of their child, which were used to calculate child body mass index (BMI) z-score and child BMI percentile. Parents reported their own height and weight, which were used to calculate BMI. Parents also reported their age and sex. Parents were classified as having a history of obesity using the parent weight history questions from the Child Feeding Questionnaire (Birch et al., 2001).
Implicit Association Test (IAT) for Child Obesity
Implicit attitudes were measured by the IAT for child obesity, from UConn Rudd Center materials (www.uconnruddcenter.org). Participants began with two learning tasks. The first learning task used congruent pairs: participants categorized “good” words and “flower” words in the same column and “bad” words and “insect” words in the other column. The second learning task used incongruent pairs: participants categorized “bad” and “flower” words in the same column and “good” and “insect” words in the other column. Next, pairings were made with two weight-related tasks: “good” and “bad” with “thin children” and “fat children” words, and “smart” and “stupid” with “thin children” and “fat children” words. The bad/good and stupid/smart tasks were counterbalanced, but participants viewed congruent pairings followed by incongruent pairings for each, consistent with the design of the original IAT (Greenwald et al., 1998). Participants were instructed to classify as many words as possible as quickly as they could without making mistakes. They were given 20 seconds for each task. As with earlier work (e.g., Teachman & Brownell, 2001), we excluded participants with fewer than 4 correct answers because this suggested inattention or difficulty understanding the task.
When participants categorize words faster (and thus have a higher score), that association is thought to be more automatic; when participants categorize words slower (and thus score lower), that association is thought to be less strong in the individuals’ mind, and the difference between the congruent and incongruent tasks demonstrates the extent of the bias. Bias scores were calculated by dividing the difference between the “incongruent” score (total correct in fat/good or fat/smart pairing) and the “congruent” score (total correct in fat/bad or fat/stupid pairing) by the “congruent” score to produce a percent bias. For example, if a participant got 10 correct in the congruent task and 8 correct in the incongruent task, this would be a −20% bias. Therefore, negative values indicate weight bias and positive values indicate a positive attitude towards children with obesity.
Explicit Attitudes Towards Children with Obesity
The “Attitudes Towards Obese Persons” scale (Allison, Basile, & Yuker, 1991) was adapted for the current study to assess attitudes towards children with obesity by changing “people” to “children.” Items are listed in Table 1. Possible mean scores range from −3 to +3; lower, more negative scores indicate more explicit bias against children with obesity. The measure yielded internally consistent scores in the current study, α=.83, which is consistent with the original scale (Allison et al., 1991).
Table 1.
Percentages of parents (N = 658) endorsing negative attitudes toward children with obesity.
| Items | % Endorsing Bias |
|---|---|
| 1. Obese children are as happy as nonobese children | 22.8% |
| 2. Most obese children feel that they are not as good as other children. | 40.6% |
| 3. Most obese children are more self-conscious than other children. | 63.2% |
| 4. Obese students cannot be as successful as other students. | 9.0% |
| 5. Most nonobese children would not want to date or marry anyone who is obese. | 24.6% |
| 6. Severely obese children are usually untidy. | 15.6% |
| 7. Obese children are usually sociable. | 12.0% |
| 8. Most obese children are not dissatisfied with themselves. | 29.9% |
| 9. Obese children are just as self-confident as other children. | 29.2% |
| 10. Most people feel uncomfortable when they associate with obese children. | 18.5% |
| 11. Obese children are often less aggressive than nonobese children. | 13.7% |
| 12. Most obese children have different personalities than nonobese children. | 16.3% |
| 13. Very few obese children are ashamed of their weight. | 41.6% |
| 14. Most obese children resent normal weight children. | 15.9% |
| 15. Obese children are more emotional than nonobese children. | 16.3% |
| 16. Obese children should not expect to lead normal lives. | 6.3% |
| 17. Obese children are just as healthy as nonobese children. | 52.0% |
| 18. Obese children are just as attractive as nonobese children. | 23.5% |
| 19. Obese children tend to have family problems. | 12.2% |
| 20. One of the worse things that could happen to a child would be for him to become obese. | 16.8% |
Note. Percentages indicate how many parents endorsed “moderately” or “strongly” agree for each item. Reverse-scored items are italicized and the associated percentages indicate how many parents endorsed “moderately” or “strongly” disagree.
Results
Implicit Weight Bias
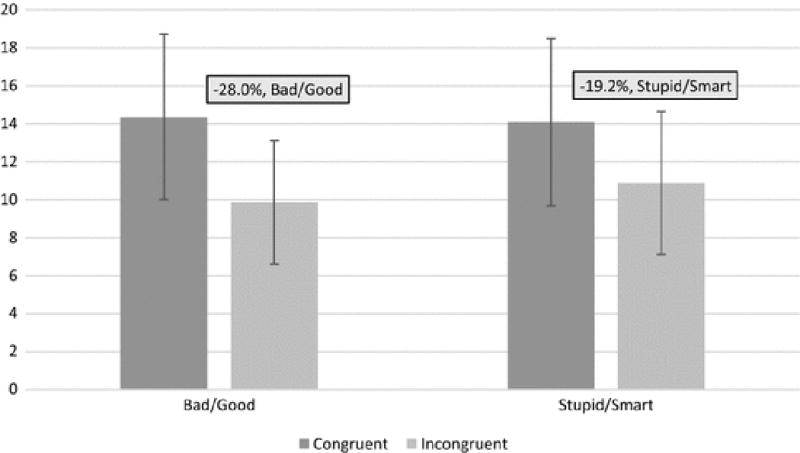
Figure 1 depicts the mean correct classifications in congruent and incongruent tasks. There was a bias consistent with our hypothesis: parents correctly paired more words in the congruent condition (M=14.36, SD=4.34) than the incongruent condition (M=9.84, SD=3.26, p<.001) for the bad/good tasks, and for the stupid/smart tasks (congruent: M=14.09, SD=4.42; incongruent: M=10.88, SD=3.76, p<.001). The mean percent bias was −28.2% for the bad/good tasks, which was significantly different from zero, t657=29.16, p<.001, d=1.14, and −19.2% for the stupid/smart tasks, t657=18.67, p<.001, d=0.73. The bad/good and stupid/smart tasks were correlated with each other, r=.266, p<.001.
Fig. 1.
Explicit Weight Bias
The mean of parents’ explicit attitudes towards children with obesity was neutral (M=0.10, SD=0.88), but inspection of the responses revealed that parents endorsed responses along the full range of possible scores and that nearly all (93.0%) parents “moderately” or “strongly” agreed with at least one explicit weight bias item, see Table 1. The most frequently endorsed items were “Most obese children are more self-conscious than other children” (63.2% moderately or strongly agreed), “Obese children are just as healthy as non-obese children” (52.0% moderately or strongly disagreed), and “Most obese children feel that they are not as good as other children” (40.6% moderately or strongly agreed). Although less frequently endorsed, we note that a few of the items (summarized in Table 1) were nonetheless endorsed at perhaps surprising frequencies given their strongly negative wording, for example: “Severely obese children are usually untidy” (15.6% moderately or strongly agreed), and “Obese children are usually sociable” (12.0% moderately or strongly disagreed).
Explicit attitudes were not significantly correlated with implicit attitudes in the bad/good tasks (r=.003, p=.93) or the stupid/smart tasks (r=.021, p=.59).
Associations with Implicit and Explicit Attitudes
Table 2 summarizes the lack of associations between implicit attitudes and parent/child characteristics, and the minority of significant associations with explicit attitudes.
Table 2.
Differences in implicit and explicit biases by demographic and weight characteristics. Bad/Good Implicit Bias
| Bad/Good Implicit Bias | Stupid/Smart Implicit Bias | Explicit Bias | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | t | p | d | n | M | SD | t | p | d | n | M | SD | t | p | d | |
| Parent current overweight/obesity | 0.89 | 0.37 | 0.07 | 0.26 | 0.79 | 0.02 | −2.10 | 0.04 | 0.17 | |||||||||
| No | 397 | −27.5% | 26.0 | 397 | −18.9% | 27.2 | 397 | 0.16 | 0.88 | |||||||||
| Yes | 260 | −29.2% | 22.8 | 260 | −19.5% | 25.2 | 260 | 0.01 | 0.87 | |||||||||
| Parent history of childhood overweight/obesity | 1.64 | 0.10 | 0.14 | 1.24 | 0.22 | 0.11 | 1.83 | 0.07 | 0.16 | |||||||||
| No | 392 | −29.0% | 24.6 | 392 | −20.6% | 24.4 | 392 | 0.15 | 0.86 | |||||||||
| Yes | 203 | −25.4% | 26.2 | 203 | −17.8% | 28.7 | 203 | 0.02 | 0.90 | |||||||||
| Child current overweight/obesity | 1.03 | 0.30 | 0.08 | 1.11 | 0.27 | 0.09 | −0.53 | 0.60 | 0.04 | |||||||||
| No | 366 | −28.8% | 24.7 | 366 | −20.2% | 25.6 | 366 | 0.08 | 0.84 | |||||||||
| Yes | 278 | −26.8% | 25.0 | 278 | −17.9% | 27.2 | 278 | 0.12 | 0.93 | |||||||||
| Parent Sex | −0.89 | 0.38 | 0.08 | 0.95 | 0.34 | 0.09 | −3.00 | 0.003 | 0.27 | |||||||||
| Father | 169 | −26.7% | 24.1 | 169 | −20.9% | 27.4 | 169 | −0.07 | 0.91 | |||||||||
| Mother | 488 | −28.7% | 25.0 | 488 | −18.6% | 26.1 | 488 | 0.16 | 0.86 | |||||||||
| Child Sex | −0.33 | 0.74 | 0.03 | 0.88 | 0.38 | 0.07 | 0.57 | 0.57 | 0.04 | |||||||||
| Son | 320 | −27.7% | 22.8 | 320 | −20.1% | 26.7 | 320 | 0.12 | 0.86 | |||||||||
| Daughter | 334 | −28.4% | 26.6 | 334 | −18.3% | 26.1 | 334 | 0.08 | 0.90 | |||||||||
| Child Age | 1.45 | 0.15 | 0.13 | 1.90 | 0.06 | 0.16 | 1.53 | 0.13 | 0.13 | |||||||||
| Child (5-11) | 431 | −29.4% | 23.6 | 431 | −20.3% | 24.6 | 431 | 0.14 | 0.91 | |||||||||
| Adolescent (12-15) | 198 | −26.1% | 27.3 | 198 | −16.0% | 30.5 | 198 | 0.03 | 0.83 | |||||||||
Note. Implicit bias scores are presented as the mean percent loss between congruent and incongruent trials. Explicit bias mean scores range from −3 to +3; lower, more negative scores indicate more explicit bias against children with obesity.
Implicit attitudes were not significantly associated with parent demographic/health characteristics (sex, current overweight/obesity, history of childhood overweight/obesity) or parent-reported child characteristics (sex, current overweight/obesity, age).
Explicit attitudes significantly differed by parent sex (mothers M=0.16, SD=0.86; fathers M=−0.07, SD=0.91, p=.003), and parent current weight status (current overweight/obesity M=0.16, SD=0.88; current healthy-weight M=0.01, SD=0.87, p=.036); there was no interaction of sex by weight status, p=.638. Explicit attitudes were not significantly associated with other parent demographic/health characteristics (history of childhood overweight/obesity) or parent-reported child characteristics (sex, current overweight/obesity, age).
Discussion
The results of our study suggest that parents have weight bias against children with obesity—both explicit and implicit. Awareness of such negative weight biases among parents is important for parents and for clinicians who work with families, as it offers insight into the experiences of children with obesity who suffer from overtly stated pity and judgment because of their weight, as well as the subtle societal impediments to their well-being because of their weight. In our study, nearly all (93%) parents endorsed moderate or even strong agreement with individual items reflecting weight bias. Moreover, parents showed an implicit association in both IAT tasks toward pairing “fat children” with negative words (“bad” and “stupid”) and “thin children” with positive words (“good” and “smart”). Employing the conceptual “four-fifths” rule that small and repeated biases may have a meaningful influence at the societal level (e.g., Greenwald et al., 2015), this suggests that implicit weight bias towards children with obesity may be problematic, particularly as some parents also endorse explicit bias against children with obesity. Demographic and health characteristics of parents and children were not significantly associated with either implicit or explicit weight bias, with the exceptions of parent sex and parent overweight/obesity with explicit weight bias. This is notable because it shows the pervasiveness of parental weight bias against children with obesity, rather than the adoption of weight bias by a subset of parents.
Although parents expressed both implicit and explicit biases, these two forms of bias were not significantly correlated. This interesting finding is actually consistent with previous research (Hofmann et al., 2005). A small or nonsignificant correlation might be due to the social undesirability of endorsing negative stereotypes (such as negative attitudes about children with obesity), or due to unawareness of these biases (Hofmann et al., 2005). Alternatively, discrepancies may reflect a potentially true difference between implicit attitudes (that are akin to “gut” reactions) and explicit attitudes (that may also account for responses using an individual’s more complex schema) (Hahn, Judd, Hirsh, & Blair, 2014). Evidence for this potentially true difference is demonstrated by earlier work where participants accurately predicted their implicit attitudes even though their prediction of their implicit attitudes was discrepant from their explicit attitudes (Hahn et al., 2014). On the one hand, it is not surprising that social desirability might create a hesitation to endorse negative attitudes about children with obesity, because the targets were children; however, importantly, we did see responses along the full range of possible scores on the explicit measure. The nonsignificant correlation between explicit and implicit attitudes underscores that it is important to avoid relying on explicit measures of weight bias, because this may miss underlying implicit attitudes.
The inclusion of both task-based and self-report data, as well as the assessment of both implicit and explicit weight bias, are strengths of the current study, which extends earlier work on adults by focusing on children with obesity and assessing potential bias in parents (including both mothers and fathers). However, the study has several limitations that are important to note. First, these were cross-sectional data. Although we counterbalanced tasks, we did not include any intervention or manipulation that could have influenced biases. This makes it impossible to make conclusions about the cause of weight bias. Yet, there are other ways to assess both implicit and explicit attitudes, and examining these may yield additional nuanced information that could help to reduce bias against children with obesity. Questionnaires are also susceptible to inattention; however, the online platform used for recruitment in the current study, Mechanical Turk, provides high-quality data from diverse, internally-motivated participants and allows for the inclusion of items designed to evaluate participants’ attention (Buhrmester et al., 2011). Additionally, height and weight data were reported by parents about themselves and about their children. Earlier work has shown that self-reported and measured weights are highly correlated and unrelated to psychological factors (Gay, Monsma, & Torres-McGehee, 2009; White, Masheb, & Grilo, 2010), but associations of discrepancies between parent-reported and measured child weights have not been studied. Future research could clarify these potential areas of inaccurate reporting. In addition, our sample was limited to parents of children between 5 and 15 years old, and participants had limited racial/ethnic diversity, with the majority mothers, well-educated and biological parents. Future research should examine whether our results generalize to the important groups of parents not well-represented in our sample, including non-traditional primary caregivers such as guardians or grandparents.
The next step in this line of research should investigate how to reduce parental weight bias against children with obesity. Some work, focused on adult patients with obesity, has been done with medical students, with some success (Alberga et al., 2016; Kushner, Zeiss, Feinglass, & Yelen, 2014; Phelan et al., 2015; Pont et al., 2017). Psychoeducation appears to influence explicit, but not implicit, weight bias (Swift et al., 2013). Empathy-training, role modeling, and positive contact with individuals with obesity appear to improve implicit weight bias (Phelan et al., 2015; Teachman et al., 2003). Consistent with these efforts to train the next generation of medical providers, the American Academy of Pediatrics recently published clinical and advocacy recommendations for pediatric providers to reduce weight bias against children with obesity, including modeling supportive and nonbiased attitudes, and using respectful language (Pont et al., 2017). Providing psychoeducation to parents about weight bias and its effects, paired with parent training and modeling positive weight-related communication, could empower parents to improve the home environment for children, particularly children with obesity. Controlled trials with follow-up assessments are needed to determine whether interventions to prevent or reduce parental weight bias against children with obesity produce meaningful change and improve health outcomes for individuals with obesity (Alberga et al., 2016). Moreover, given the pervasiveness of weight bias, including parental weight bias against children with obesity, it will be important to have simultaneous efforts directed at reducing bias and increasing children’s resilience when they experience bias and discrimination.
Our study provides the first evidence that parents have explicit and implicit negative attitudes towards children with obesity. It is striking that even parents, including those who themselves have obesity and whose children have obesity, have implicit weight bias. This provides further evidence that weight bias appears to be pervasive and near-universal. Also striking is that parents—as with other groups (Ambwani, Thomas, Hopwood, Moss, & Grilo, 2014)—endorsed explicit weight bias, including statements that appear very socially undesirable to endorse (e.g., “One of the worst things that could happen to a child would be for him to become obese”). Importantly, weight bias is associated with health problems such as diabetes and cardiac problems (Udo et al., 2016) and expressions of explicit weight bias are associated with excess weight and disordered eating (Lydecker, Riley, & Grilo, 2018). Universal and targeted prevention programs that reduce both forms of weight bias may have a large impact on children’s health, particularly as the effects of weight bias on youth can impair mental and physical health.
Acknowledgments
This research was funded, in part, by National Institutes of Health (K24 DK070052). An earlier version of this research was presented at the Society for Adolescent Health and Medicine annual conference in 2017. For the past 12-months, Dr. Grilo reports receiving honoraria for lectures delivered for CME-related activities and plenaries and lectures at professional academic conferences and reports royalties from academic books published by Guilford Press and Taylor & Francis Publishers. Beyond 12-months, Dr. Grilo reports having received consultant fees from Shire and Sunovion, and honoraria for CME-related lectures and for lectures delivered at grand rounds and professional academic conferences nationally and internationally.
Footnotes
Compliance with Ethical Standards:
All authors declare no conflicts of interest. Dr. Grilo reports no relevant direct or indirect conflicts of interest with respect to this study, but reports the following recent and previous broader interests.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Agerstrom J, Rooth DO. The role of automatic obesity stereotypes in real hiring discrimination. Journal of Applied Psychology. 2011;96:790–805. doi: 10.1037/a0021594. [DOI] [PubMed] [Google Scholar]
- Alberga AS, Pickering BJ, Alix Hayden K, Ball GD, Edwards A, Jelinski S, Russell-Mayhew S. Weight bias reduction in health professionals: A systematic review. Clin Obes. 2016;6:175–188. doi: 10.1111/cob.12147. [DOI] [PubMed] [Google Scholar]
- Allison DB, Basile VC, Yuker HE. The measurement of attitudes toward and beliefs about obese persons. International Journal of Eating Disorders. 1991;10:599–607. [Google Scholar]
- Ambwani S, Thomas KM, Hopwood CJ, Moss SA, Grilo CM. Obesity stigmatization as the status quo: Structural considerations and prevalence among young adults in the U.S. Eating Behaviors. 2014;15:366–370. doi: 10.1016/j.eatbeh.2014.04.005. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Carels RA, Young KM, Wott CB, Harper J, Gumble A, Oehlof MW, Clayton AM. Weight bias and weight loss treatment outcomes in treatment-seeking adults. Annals of Behavioral Medicine. 2009;37:350–355. doi: 10.1007/s12160-009-9109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay J, Monsma EV, Torres-McGehee T. Give or take a few? Comparing measured and self-reported height and weight as correlates of social physique anxiety. Research Quarterly for Exercise and Sport. 2009;80:656–662. doi: 10.1080/02701367.2009.10599605. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the Implicit Association Test can have societally large effects. Journal of Personality and Social Psychology. 2015;108:553–561. doi: 10.1037/pspa0000016. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. Journal of Personality and Social Psychology. 1998;74:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology. 2009;97:17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- Hahn A, Judd CM, Hirsh HK, Blair IV. Awareness of implicit attitudes. Journal of Experimental Psychology: General. 2014;143:1369–1392. doi: 10.1037/a0035028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann W, Gawronski B, Gschwendner T, Le H, Schmitt M. A meta-analysis on the correlation between the implicit association test and explicit self-report measures. Personality and Social Psychology Bulletin. 2005;31:1369–1385. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- Kushner RF, Zeiss DM, Feinglass JM, Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Medical Education. 2014;14:53. doi: 10.1186/1472-6920-14-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker JA, Riley KE, Grilo CM. Associations of parents’ self, child, and other “fat talk” with child eating behaviors and weight. 2018 doi: 10.1002/eat.22858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynagh M, Cliff K, Morgan PJ. Attitudes and beliefs of nonspecialist and specialist trainee health and physical education teachers toward obese children: Evidence for “anti-fat” bias. Journal of School Health. 2015;85:595–603. doi: 10.1111/josh.12287. [DOI] [PubMed] [Google Scholar]
- Nosek BA, Greenwald AG, Banaji MR. Understanding and using the Implicit Association Test: II. Method variables and construct validity. 2005;31:166–180. doi: 10.1177/0146167204271418. [DOI] [PubMed] [Google Scholar]
- O’Brien KS, Hunter JA, Banks M. Implicit anti-fat bias in physical educators: physical attributes, ideology and socialization. 2007;31:308–314. doi: 10.1038/sj.ijo.0803398. [DOI] [PubMed] [Google Scholar]
- Phelan SM, Puhl RM, Burke SE, Hardeman R, Dovidio JF, Nelson DB, van Ryn M. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Medical Education. 2015;49:983–992. doi: 10.1111/medu.12770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pont SJ, Puhl R, Cook SR, Slusser W, Section On, O., & Obesity, S. Stigma Experienced by Children and Adolescents With Obesity. 2017;140 doi: 10.1542/peds.2017-3034. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychological Bulletin. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. 2003;289:1813–1819. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- Skinner AC, Payne K, Perrin AJ, Panter AT, Howard JB, Bardone-Cone A, Perrin EM. Implicit Weight Bias in Children Age 9 to 11 Years. Pediatrics. 2017;140:e20163936. doi: 10.1542/peds.2016-3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift JA, Tischler V, Markham S, Gunning I, Glazebrook C, Beer C, Puhl R. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obesity Facts. 2013;6:91–102. doi: 10.1159/000348714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? International Journal of Obesity and Related Metabolic Disorders. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Gapinski KD, Brownell KD, Rawlins M, Jeyaram S. Demonstrations of implicit anti-fat bias: The impact of providing causal information and evoking empathy. Health Psychology. 2003;22:68–78. doi: 10.1037//0278-6133.22.1.68. [DOI] [PubMed] [Google Scholar]
- Tomiyama AJ, Finch LE, Belsky AC, Buss J, Finley C, Schwartz MB, Daubenmier J. Weight bias in 2001 versus 2013: Contradictory attitudes among obesity researchers and health professionals. Obesity. 2015;23:46–53. doi: 10.1002/oby.20910. [DOI] [PubMed] [Google Scholar]
- Udo T, Grilo CM. Cardiovascular disease and perceived weight, racial, and gender discrimination in US adults. 2017;100:83–88. doi: 10.1016/j.jpsychores.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, Purcell K, Grilo CM. Perceived weight discrimination and chronic medical conditions in adults with overweight and obesity. International Journal of Clinical Practice. 2016;70:1003–1011. doi: 10.1111/ijcp.12902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Equal Employment Opportunity Commission. Uniform Guidelines on Employee Selection Procedures. 1978 § 1607.4.D. Retrieved from: https://www.gpo.gov/fdsys/pkg/CFR-2013-title29-vol4/xml/CFR-2013-title29-vol4-part1607.xml.
- White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height in binge eating disorder: Misreport is not related to psychological factors. Obesity. 2010;18:1266–1269. doi: 10.1038/oby.2009.347. [DOI] [PMC free article] [PubMed] [Google Scholar]


