Abstract
For women enrolled in prevention of mother-to-child transmission (PMTCT) programs, non-disclosure of their HIV status can be a significant barrier to sustained HIV care engagement. To explore decision-making surrounding HIV disclosure among HIV-infected pregnant women, we conducted repeated in-depth interviews during pregnancy and postpartum with 20 women recruited from a PMTCT clinic in Cape Town, South Africa. Three domains were examined using thematic analysis: (1) disclosure experiences, (2) challenges associated with partner disclosure, and (3) implications of nondisclosure. All women had disclosed to someone by the time of the baby’s birth, typically limiting their disclosure to trusted individuals. Only half of participants disclosed to the father of the child. Nondisclosure, particularly to partners, was a significant source of worry and stress. Women used pregnancy as an explanation for using medication and attending frequent clinic appointments, and recognized impending challenges in the postpartum period when this excuse would no longer apply. Results suggest that PMTCT programs have a key role to play in helping individuals to make decisions about HIV disclosure, and assisting patients to navigate the disclosure process, especially with partners.
Keywords: South Africa, HIV, disclosure, pregnancy, PMTCT, Option B+
INTRODUCTION
Pregnancy is a time when many women first learn about their HIV status and initiate antiretroviral therapy (ART) for lifetime use (1). Early and consistent engagement in ART is essential during pregnancy and the postpartum period to prevent HIV transmission to the child and to protect the health of the mother. However, data from multiple countries suggest that care engagement during this period is sub-optimal (2), which raises concerns about forward transmission to children and partners, as well as deleterious impacts on the mother’s health and well-being. Across multiple studies, HIV non-disclosure has been identified as a key barrier to HIV care engagement (3,4). HIV disclosure, defined as telling another person either directly or indirectly about one’s HIV status, is challenging at any period, but presents particular complexities during the vulnerable period of pregnancy and the postpartum period (5,6).
A systematic review of HIV serostatus disclosure among pregnant and postpartum women found that across studies in South Africa, prevalence of HIV disclosure to any person ranged from 53–89% (7), and prevalence of HIV disclosure to a sexual partner was similar (8, 9). Evidence suggests that women who test positive for HIV in the context of antenatal care (ANC) are less likely to disclose than women testing in other settings, such as those attending voluntary HIV testing and counseling clinics (10). In qualitative studies, the rationale for non-disclosure of HIV during pregnancy has included concerns of abandonment or rejection, in particular the loss of emotional and financial support for both the mother and the child, and a fear of blame and/or anticipated violence from a partner (11–14). In situations where pregnancies are unintended or unplanned, HIV-infected pregnant women face what has been called a “double disclosure bind” of navigating disclosure of both the pregnancy and the HIV status (15). In the postpartum period, barriers to HIV disclosure and HIV care engagement can also be exacerbated in the postpartum period, as women experience a number of physical, social, and economic changes as new mothers that may affect their health behaviors (20).
Decisions about HIV disclosure are informed by a woman’s perceptions of HIV stigma and anticipated responses from individuals in her family and broader social circle. A woman’s decision to not disclose is often prompted by personal experiences of witnessing mistreatment, social exclusion, or gossip about others with HIV (14,16–19). While disclosure of a stigmatized condition like HIV has the potential to elicit negative reactions, positive experiences of disclosure can give individuals access to social support, which facilitates care-seeking behavior both emotionally (through encouragement and advice) and practically (through reminders and financial assistance) (16,21–24). Improved care engagement contributes to a lower viral load, which can virtually eliminate the possibility of vertical transmission to children during pregnancy and breastfeeding or horizontal transmission to sexual partners.
It is estimated that 30.8% of pregnant women receiving antenatal care in South Africa are infected with HIV, a rate among the highest in the world (25). Supporting women in HIV disclosure during pregnancy and the early postpartum period is an essential component of comprehensive, effective prevention of mother-to-child transmission (PMTCT) programs. It is therefore critical to understand the circumstances of women’s lives, their relationships with others, and their disclosure decision-making processes, in order to respond in a patient-centered manner. To address this need, we conducted a qualitative study to explore HIV disclosure decision-making and processes among women during the pregnancy and postpartum periods in Cape Town, South Africa. We examined emerging themes in three domains: (1) the disclosure experience, (2) challenges associated with partner disclosure, and (3) implications of non-disclosure. These findings can shed light on the context in which disclosure decisions occur, in order to develop interventions that support women in making decisions about HIV disclosure during a vulnerable period of their lives.
METHODS
Setting
The study was situated in the township of Phillipi, approximately 15 miles from the Cape Town Central Business District. Community resources and local infrastructure are limited in Phillipi, and socioeconomic indicators point to high rates of poverty and hardship. According to the most recent available census data (29), only 32% of residents had completed a high school education, 38% were unemployed, and 78% reported an annual household income below 3,200 South African Rand (US $278, based on exchange rates during the study period).
Recruitment and study procedures were conducted in a single government clinic in Phillipi. The facility has an antenatal care (ANC) clinic that provides routine HIV testing for all pregnant women. Patients who are identified as HIV-infected are followed in a separate PMTCT clinic within the same facility, where they receive clinical care and counseling specific to their HIV status. Services for labor and delivery are provided at a separate maternity hospital, and women return to the clinic for postpartum care. At the time of the study, the clinic followed national PMTCT guidelines of Option B+, whereby all pregnant women who are HIV-infected initiate lifelong ART (26). ART and all health care services are provided free of charge.
Sample and Recruitment
Clinic patients were eligible to participate in the study if they were over the age of 18, pregnant, diagnosed with HIV, and initiating ART during the current pregnancy or re-initiating ART after having defaulted treatment. Women who had already initiated lifetime ART and were continuing their use during the current pregnancy were excluded from participation. Eligible patients were identified by the nurse in the PMTCT clinic. The nurse told the patient about the study, either in person at a clinic appointment or via telephone, and those interested in learning more were introduced to a member of the research team. The research coordinator provided additional information about the study and answered questions, and then proceeded to schedule a visit to complete the first in-depth interview. Twenty study participants were enrolled between June 2015 and June 2017, and nineteen participants (95%) completed repeat interviews.
Procedures
Enrolled participants took part in two semi-structured interviews: the first interview was conducted in the third trimester of pregnancy and the second interview was conducted approximately three months postpartum. All interviews were conducted by a South African researcher who had previous experience with qualitative research. Interviews were conducted in Xhosa in a private room in the study clinic, and lasted 90 minutes on average. Interviews followed a semi-structured guide that included broad opening questions and more specific follow-up probes. Interviews focused broadly on care engagement in the context of PMTCT, with disclosure as one of several specific areas of inquiry.
In the pregnancy interview, participants were given the opportunity to talk about their pregnancy, HIV diagnosis, feelings about living with HIV, relationships, and their social support system. Once these issues were explored more broadly, participants were asked specifically about HIV disclosure. This tiered approach first provided the broader context of the participant, which then allowed the interviewer to probe more deeply about the rationale for disclosure decisions, how disclosure decisions impacted relationships, and how participants navigated disclosure or non-disclosure in the context of PMTCT care.
In the postpartum interviews, the interviewer began with a discussion about childbirth and the early postpartum period, and then revisited topics from the first interview, including decision-making around new disclosures, changing rationale for non-disclosure, and the impact of disclosure or non-disclosure on current HIV care engagement and anticipated future care. The interviewer was trained prior to data collection on how to follow the open-ended guide and probe on salient themes throughout the interviews, and received ongoing supervision.
All participants provided written informed consent to participate in the study and interviews were audio recorded with participant consent. Participants were compensated 100 Rand ($8.70, based on exchange rates during the study period) for their time and related travel costs. Study procedures were approved by the institutional review boards at Duke University and the University of Cape Town.
Analysis
Audio recordings of the interviews were transcribed and simultaneously translated into English, with key identifying information (e.g., names and places) deleted from the transcripts. The textual data were then analyzed in four steps, using a thematic analysis approach (27) that draws upon the inductive nature of grounded theory (28). We opted not to use a qualitative software program and instead to follow a process that kept us deeply connected to the data via multiple readings of the transcript, writing activities to explore and organize emerging findings, and consensus-oriented discussions to deepen and challenge our understanding of the data. First, individual narrative memos (approximately six single-spaced pages each) were written to summarize and organize the content of each transcript and to highlight emerging inductive themes (29). Each transcript and memo pair was read by at least one other investigator, who provided input to ensure that the memo accurately captured key details from the original transcript. Relevant quotations were incorporated into the memos to closely reflect participants’ own words. Preparing the memos enabled the authors to begin exploring the relationships and themes in the data and proceed to the next step of analysis. Second, the memos were reviewed to identify key areas of inquiry related to HIV disclosure. Consensus building discussion identified three domains: (1) disclosure patterns and reactions, (2) challenges of partner disclosure, and (3) implications of non-disclosure. Third, a data display matrix (30) was created to capture details and themes related to each of these domains across the transcripts and at the two time points. The transcript-memo pairs were examined, with relevant information added to the matrix and discussed as a team. Fourth, data reduction involved a synthesis of data within each domain, with data visualization and representative quotes used to lend evidence to the identified themes and to contextualize the findings.
RESULTS
Description of the sample
The twenty women in the sample ranged in age from 18 to 37, with an average age of 27 (Table 1). Fifteen (75%) had been diagnosed with HIV during the current pregnancy. Of the five women with established HIV diagnoses, four women had never taken ART and one woman had previously taken ART and was re-initiating treatment after defaulting one year prior. The majority of women were unemployed, had low levels of education, and reported that their pregnancy was unplanned.
Table 1.
Description of the sample at pregnancy interview (n=20)
| n | |
|---|---|
| Age, Mean (range) | 26.9 (18–37) |
| Relationship status | |
| Single | 7 |
| In a relationship | 9 |
| Married | 3 |
| Separated | 1 |
| Education | |
| Some high school | 14 |
| Completed high school | 5 |
| Some university or more | 1 |
| Any employment | 9 |
| First pregnancy | 8 |
| Diagnosed with HIV during current pregnancy |
15 |
Experiences of HIV disclosure during pregnancy and postpartum
Participants described whether they had disclosed their status, when and to whom they had disclosed, and their decision-making processes surrounding disclosure. The interviews covered motivations to disclose, or to withhold disclosure, to various people in their lives, and the reactions they had received when disclosing their status to date.
Patterns of disclosure
HIV disclosure in the sample was common but selective (Table 2). We examined disclosures to people in three categories: father of the child, family, and others. At the time of the pregnancy interview, all but one woman had disclosed to at least one person. Half (10/20) had disclosed to the father of the child.
Table 2.
Prevalence of disclosure at time of pregnancy and postpartum interviews (n=20)
| Disclosure at pregnancy interview |
Disclosure at Postpartum interview |
|
|---|---|---|
| n (%) | n (%) | |
| Any disclosure | 19 (95) | 20 (100) |
| Father of child | 10 (50) | 11 (55) |
| Family | 12 (60) | 18 (90) |
| Other | 14 (70) | 14 (70) |
Among the 19 women who completed postpartum interviews, 12 had new disclosures since their initial interview, three of which occurred before the birth of the child. One woman disclosed to the father of the child soon after the pregnancy IDI, stating she was motivated by the interview. In the case of the one woman with no disclosures at baseline, she reported that her sister-in-law discovered her ART before the baby’s birth, resulting in an unintended disclosure. Therefore, by the time of the baby’s birth, all participants had at least one person who knew her HIV status, and 11/20 (55%) women had disclosed to the father of the child. In the postpartum period, all new disclosures were to family members.
Decision to disclose: right person, right time
In discussing their decision-making surrounding disclosure, women frequently spoke about the difficulty of disclosing their HIV status, their deliberation regarding the individuals to whom they wanted to disclose, and rumination surrounding the appropriate circumstances of the disclosure. Participants also commonly described identifying someone they could trust to provide support and to keep their HIV status a secret from others, determining the level of trust by evaluating their existing relationship, and anticipating the person’s reaction. One woman explained her decision to disclose to two trusted friends who would support and motivate her rather than an “aunt who might have gossiped and judged me and spread it till home in Eastern Cape (Participant 17)”. Several participants noted that successful disclosure to one trusted individual helped to facilitate further disclosure, as friends and family provided encouragement to disclose, or in some cases even performed the disclosure with the woman’s permission.
Almost all women spoke about someone else they knew who was infected with HIV, indicating that HIV was common in the communities where the participants lived. For some, this normalization of infection, and the knowledge that they and their baby could lead healthy lives with treatment, helped them view their status as “not something bad,” and made it easier for them to share the news. Others drew upon the experiences of family members who were infected, which they witnessed secondhand and used to inform their own decisions about disclosure. Two women who had known a family member with HIV recounted being motivated by previous incidents where non-disclosure led to negative outcomes or hurt feelings.
“The reason why I told [my mother] is because of the way she felt when my big sister was sick also from HIV. She ended up blaming my sister for not telling her that she had HIV and ending up very sickly, with my mom unable to help.” –Participant 11, new HIV diagnosis, pregnancy interview
Many women, seeking solidarity and advice, chose to disclose to someone they knew who was infected with HIV or who had personal experience supporting someone with HIV. This woman explained how she felt she could trust someone with HIV to keep her status confidential:
“The reason why I chose to tell her was because she is also infected and it would have been difficult for her to go around and talk about something that she is also a victim of” – Participant 14, new HIV diagnosis, postpartum interview
At the same time that women sought support from others who had been impacted by HIV, they were also nervous about being recognized at the HIV clinic by other patients. For some, this made them reluctant to join a support group with other HIV-infected individuals, out of fear that their status would become more widely known. Therefore, even though HIV was perceived as common and normal, women also had a heightened anticipation of stigma should their status be known broadly in the community.
Women were highly motivated to stay engaged in HIV care during pregnancy and in the postpartum period, often speaking of a desire to protect their babies from infection and to stay healthy themselves so they would be around to take care of their children. This commitment to HIV care was closely tied to motivations for disclosure; participants frequently shared that disclosure would allow them to be open about their need to take medication and attend clinic appointments, as well as enable them to seek practical and emotional support in seeking care. Several women disclosed to others living in their households, including relatives and partners, who might see them taking their pills, and one participant disclosed to a coworker and her neighbor, so if something should happen, there would be “someone close by who will know what to do (Participant 9)”.
Timing of disclosure was strategic. Even when a woman had identified someone to whom she wished to disclose, she sometimes waited for the optimal time when circumstances were right or when she was “ready.” In many cases, ideal timing for disclosure revolved around the birth of the child. Visits from mothers or aunts to help care for the baby provided the opportunity for many to disclose to someone they wanted to tell in person rather than over the phone. One woman, who became emotional when discussing disclosure to her mother, described her desire to wait until she was sure the baby was healthy before telling her mother, to prevent undue stress and concern: “I know my mom hurts easily. I don’t want to tell her right now, but I want to tell her after giving birth when I know that I’m fine and the baby is also fine (Participant 7).” Women also described motivations to disclose preemptively, before someone found out by discovering pills or hearing it from someone else:
“[I] did not want to tell [my sister] because I feared she was going to do the same as she did to our late sister and that I will be the talk of the town. I took time to tell her, but eventually I told her myself because I did not want her to learn about it from outside.” – Participant 14, new HIV diagnosis, pregnancy interview
Reactions to disclosure
When women made a decision to disclose their HIV status to someone, the reactions were almost always positive, even when participants were initially concerned about how the person might respond. Women reported that their family members and friends reassured them they could have a healthy child and that they could also live a healthy life with appropriate treatment, noting that HIV is a controllable disease and therefore “much better than diseases like diabetes and high blood pressure (Participant 14).” Upon disclosure, many friends and family members pointed to examples of “beautiful” people they knew with HIV who were consistently taking treatment and living a healthy life; others offered cautionary tales of those who died after defaulting on their ART.
The majority of women who disclosed to others reported that they had received advice and encouragement to adhere to their treatment, for the benefit of themselves and for the health of the baby. Many friends and family members went on to actively support their HIV care, providing reminders about medication or accompanying them to appointments. Disclosure also presented the opportunity for participants to support and encourage others, as several women noted that their disclosure motivated others to share their HIV status: “More people in my family after I disclosed got courage to disclose their status too! More people came out and started talking about taking their ARVs (Participant 18).”
Disclosure frequently brought a sense of relief and freedom to women who no longer had to hide their status. Participants described feeling as though a burden had been lifted, in contrast to keeping a secret, which “kills you inside (Participant 5)”. For some, disclosing to a trusted individual helped them on the pathway to self-acceptance:
“I couldn’t stand the thought that I was HIV positive. I lost hope. But when I got home my mother motivated me…and now I am feeling strong. It took me a very long time because sometimes I would think about it, but eventually I decided to accept my situation.” – Participant 12, new HIV diagnosis, pregnancy interview
In the postpartum interviews, almost all women expressed satisfaction with their decisions to disclose; they felt that disclosure led others to provide more support, and few could recall instances of feeling stigmatized. Although most participants felt that their trusted friends and family had “kept the secret to themselves (Participant 18),” one woman questioned how dependable her sister-in-law and sister were. After hearing from her brother that they were gossiping about her, she explained: “I started feeling discrimination and I started feeling that I have actually disclosed to the wrong people.” However, she maintained that disclosure was the right decision for her to “get this off my chest,” and the way they treated her “is not my problem but theirs” (Participant 20).
Reasons for non-disclosure
Just as women expressed being deliberate about their disclosure, they also spoke about being deliberate about their non-disclosure. Reasons for non-disclosure often included a fear of stigma or “judgement” and the possibility that the person would gossip about them: “The cousins are the ones I want to keep this knowledge from. They tend to look down on people. Even when we are chatting at home: ‘so-and-so is like this.’ So I fear that they will degrade me too (Participant 4).”
Pregnancy contributed to the complexity of the decision-making process. Women often faced the dual burden of disclosing both their HIV status and their pregnancies. One woman who felt ashamed by her pregnancy feared that sharing her HIV would further disappoint and distress her parents, saying “it would kill them!” She anticipated that challenges of disclosure would likely persist even after the baby’s birth, explaining “then it’ll be even worse because their concern will be, ‘she’s going to die and leave us with the small child’ (Participant 2).”
Many women acknowledged that they simply did not feel brave enough to disclose to someone or were not yet “ready” to do so. Some associated their readiness to disclose with self-acceptance of their HIV status:
“I’m not ready now. I only want [my mother] to know when I have accepted everything and I’m fine. I don’t want her when she looks at me to see someone who’s weak and sickly. I want her to see a strong and healthy person. I want her to accept the situation and she will do that if she sees that I have also accepted it!” –Participant 7, new HIV diagnosis, pregnancy interview
Women also noted the difficult lives that they and their families faced, with frequent mentions of interpersonal violence and other forms of trauma, poverty, and other health issues. Participants commonly chose not to disclose their status for fear of adding strain to others’ already difficult lives. For example, in the pregnancy interviews, five women had deliberately not disclosed to their mothers, with a rationale that they were protecting them from an additional burden of stress and hardship.
Challenges unique to partner disclosure in the context of pregnancy
Only half of the participants (n=10) had disclosed to the father of the baby at the time of the pregnancy interview, and only one additional woman had disclosed by the time of the postpartum interview (reporting that she was motivated to disclose by the interview). When discussing decision-making related to partner disclosure, some themes were consistent with disclosures to other individuals (e.g., assessing level of trust, anticipating reactions, considering best timing of disclosure), and other themes were unique to disclosure to a partner. The unique considerations that went into disclosure to a partner included feeling added responsibility to share the information with the partner (related to the partner needing to know his own HIV status and protect himself from HIV exposure), fear of being blamed and held responsible for the infection, and fear of violence or abandonment, often related to the preexisting uncertainty and instability of the relationship with the baby’s father.
Participants described the complexity of their relationships, often fraught with conflict and abuse, infidelity, financial stress, and a lack of trust. Pregnancy further complicated these tenuous relationships. Half of the participants reported they were not in a relationship at the time of the pregnancy interview, although several of these women still described the father of the baby as their “boyfriend,” reported that they planned to reunite with the father, or reported having initiated a relationship with a new partner. Several women directly pointed to the pregnancy as the reason that their relationship with the baby’s father ended, while others cited their partner’s infidelity, abuse, or financial stress as causes for their breakup. When women were asked about disclosure to the father of the child or to other sexual partners, they commonly reflected on the level of stability in those relationships as influencing their decision to disclose. Of those describing themselves as single at the time of the pregnancy interview, only 3 out of 10 had disclosed to the father of the child, and one additional woman had disclosed to a new boyfriend; of those describing themselves as married or in a relationship, 8 out of 10 had disclosed to the father of the child.
Motivations for disclosure to partners
The eleven women who disclosed to the father of the child before the baby’s birth described various motivations. Similar to the themes that emerged in decisions about disclosing to others, disclosure to the partner was a way to gain freedom to take ART without hiding and relieve the stress and anxiety of keeping a secret. Women were also motivated (and encouraged by others) to disclose to a partner in order to protect him from HIV infection or progression of an existing infection. Women reported that in disclosing, they hoped their partner would then get tested for HIV and begin treatment if necessary.
Several women disclosed to the father of their child as an act of confrontation, especially when he had been unfaithful or the woman had previously tested negative for HIV. As one woman explains:
“I got very upset, sister, because I had been faithful to this man and yet this man was sleeping around. I was very upset and I told him about how upset I was and I told him that he’s the one who infected me, no one else! He did not deny it because he knew that he’s the one who sleeps around.” –Participant 13, new HIV diagnosis, pregnancy interview
Partners responded to confrontation in different ways. One boyfriend did not deny the accusation, but asked the woman to “give him a break” because she was causing him stress. After some time they “became right” and he now supports her by reminding her of her clinic appointments. Another confrontation led to ongoing quarrels in the marriage over who was to blame for bringing the infection into the relationship, and their fights led the husband to move in with a new girlfriend by the time of the postpartum interview. One participant ended the relationship with her boyfriend, feeling that he had deliberately infected her and she could no longer trust him.
With the exception of the confrontational disclosures, when women chose to disclose, their partners’ reactions were generally supportive. Several women noted that after disclosure, their partners began reminding them to take their pills and motivated them to attend clinic appointments to protect the baby. At the same time, one woman explained that she became a source of support to her boyfriend, who was distressed upon learning of her status and refused to be tested himself until he was ready, which was a common theme:
“His response on that was, if he can find out that he’s HIV positive, he will kill himself. I asked him not to do that for the sake of our child… He calmed down and I think he got back to his senses and the he said, he’s hearing me and will try to (get tested).” – Participant 5, new HIV diagnosis, pregnancy interview.
Of the eleven women who had disclosed to the father of their child, two women reported that their partner had disclosed his HIV positive status prior to the pregnancy, and one woman had learned about the partner’s HIV positive status when she discovered his pills. Six women reported that the father of the child had not yet tested by the time of the baby’s birth. Only two men had gone to test and both discovered they were also positive. By the postpartum interview, one additional woman had convinced her boyfriend to test and start ART, and another asked a male nurse to help schedule an appointment for her husband to confirm an HIV diagnosis and begin treatment.
Rationale for non-disclosure to partners
Almost half of the women (n=9) had not disclosed to the father of the child by the time of the follow-up interview. Three women had ended their relationships with the father of the child and were no longer in communication with the men. Of the six women still in contact with the father of the baby, five women described not feeling ready or “not being brave enough yet” to disclose. Several of these women identified disclosure to a partner as something they wished to do and an area where they could benefit from support, as they struggled to put their intentions into action.
In the context of describing disclosure to the father of their child or another romantic partner, women’s reluctance to disclose was often related to broader challenges in their relationships with the partners, which were particularly tenuous during pregnancy. Women were afraid that after disclosing, they would be blamed for bringing the infection into the relationship, as this participant explained: “I suspect there is a chance that he might say, ‘No, you brought this thing to us! (Participant 1)’”. Women were also concerned about their partners’ ability to keep a secret, especially when alcohol was involved: “With some of them, their husbands or baby daddy when they are drunk may go around telling people about their wives’ or girlfriends’ status, and people make fun of that (Participant 2).”
Women were also worried that the father of the baby would leave upon learning their status: “Some of us, we hide it because we don’t want to be dumped by these boyfriends (Participant 18)”. Pregnancy appeared to increase women’s vulnerability and raise the stakes of abandonment. Financial difficulties and unemployment were often-noted stressors, and many felt those stressors would increase after the baby was born. As one woman explained: “I’m not ready to tell him either because I’m uncertain of what could happen should I tell him. And even worse now, there’s a baby coming (Participant 19).”
Implications of non-disclosure during pregnancy and postpartum
Four themes emerged in the data as implications for non-disclosure: 1) stress and wellbeing, 2) desire for passive disclosure, 3) strategies to maintain care engagement, and 4) risk for defaulting.
Stress and wellbeing
Most of the women in this sample were dealing with two life-changing circumstances simultaneously: an HIV status and a pregnancy. One woman said that she considered terminating the pregnancy to lessen the burden: “After finding out, I thought, how will I deal with these two things at the same time? I thought that I should just get rid of one of the two (Participant 7).” Non-disclosure, particularly to the father of the child and family members, added further stress and anxiety to women’s already difficult lives. One woman noted her internal conflict about disclosing to her partner and its impact on her wellbeing: “I do think about it sometimes, and that sometimes keeps me awake at night. Sometimes I want to tell, but there’s this other thought that comes immediately that says, ‘Shut up, don’t say it.’ I am scared (Participant 4)”. Women felt guilty for keeping secrets, even questioning “perhaps this baby is a mistake if I’m going to keep quiet and not tell [the baby’s father about my status] (Participant 2).” With partners, non-disclosure added further anxiety around sexual activity:
“We are okay but one thing I’m still scared of doing is sleeping with him because I’ve been told, if I sleep with someone without a condom, I’m re-infecting myself. Whenever he wants to have sex with me I shy away and pretend as if I’ll come and avail myself some other time.” –Participant 6, new HIV diagnosis, pregnancy interview
Desire for passive disclosure
To ease the burden of disclosure, many women expressed a desire for their loved ones to learn about their status without needing to actively disclose. One woman, worried about disclosing to her mother, often left her pills out in places where her mother could find them.When asked if she thought her mother knew about her status, she replied:
“I don’t know but maybe by her suspecting and finding out may mean less work for me than to lie in front of her eyes! I mean if she can confront me I can just tell the truth! I can just tell her that I did not have the guts to tell her.” -Participant 2, new HIV diagnosis, pregnancy interview
Another woman, who had not disclosed to anyone in the five years since her HIV diagnosis, was relieved when her sister-in-law discovered her medication, and felt thankful that someone now knew about her status and could support her without her needing to actively disclose.
Women often wanted their partner to know his own status, and saw HIV testing as a way for the partner to get treatment and initiate conversations around HIV. One woman discussed her desire to be re-tested together with her partner, so they would appear to learn their statuses for the first time together. This desire was driven by the common belief that the first person in the relationship to disclose a positive status would be blamed for being the first person infected: “I may want us to go get tested. I may want to come alone at the clinic and get a nurse I know and tip her to pretend as if it’s my first diagnosis (Participant 4)”. Another woman, who was fearful that her boyfriend would blame her for the infection if she told him herself, explained: “Sometimes I really feel like disclosing but it’s just so difficult. I can’t tell him because men are so impossible. I have been advising him, however, that he go to the clinic (Participant 6).”
Strategies to maintain care engagement
All participants expressed a commitment to lifetime treatment, largely motivated by a desire to stay healthy and to protect and support their children. However, in the face of non-disclosure, women often had to adopt strategies to maintain HIV care engagement. Such strategies included repackaging their medication and attributing their pill-taking and clinic attendance to pregnancy or other health issues like diabetes or high blood pressure. Pregnancy made it easier for women to justify frequent clinic visits and taking medication, but many acknowledged that maintaining non-disclosure would become more difficult in the postpartum period. One woman described how her boyfriend believed her HIV medications were prenatal vitamins, and how difficult it was for her to maintain that lie:
“He reminds me… ‘It’s eight o’clock now. Come and take the baby’s pills… the ones for making the baby grow, dear.’ But I know… like, ‘My God, if you only knew what these pills are for.’ I don’t know. It’s really difficult.” -Participant 8, new HIV diagnosis, pregnancy interview
In the postpartum interview, one woman explained how taking her pills on time had become challenging, given that her partner would often be in the room where her pills are, putting her in “an awkward position” where “I can’t do anything.”
Women often anticipated challenging situations for medication adherence and planned ahead so they would not be caught off guard. One woman explained her plan to go next door and borrow a pill from her HIV-positive neighbor’s house if she had visitors and could not access her own pills without being seen. Another woman moved the “hiding position” for her pills so she could take them more easily when she had visitors. In the postpartum interviews, women often said that they tried to schedule appointments for themselves and the baby together in order to avoid frequent, and potentially suspicious, visits to the clinic. Others talked about coming up with new excuses for attending the clinic: “maybe I will just tell them I fetch high blood pressure pills (Participant 4).”
Risk for defaulting
Despite participants’ efforts to maintain care engagement in the face of non-disclosure, women noted that fear of disclosure increased the risk of missing appointments or defaulting on treatment. Several women criticized the layout of the clinic as compromising privacy, fearing that other clinic attendees might know they have HIV based on where they sit. One woman’s clinic experience validated this fear, as a neighbor spotted her friend picking up HIV medication and later gossiped about her at home. Another woman was considering transferring clinics because of her fear of unwanted disclosures, sharing that this same fear may lead others to “turn away from the clinics” entirely (Participant 2).
Because of the challenges of hiding their medication and clinics visits, some women felt they would have to choose between disclosure and long-term retention in care. Women frequently weighed the merits of each course of action in the interviews. Looking to the future, one woman considered:
“Maybe I may end up not taking ARVs if I get married to someone and perhaps I don’t want him to know that I’m taking ARVs, even though I know that by doing that I would be putting my life at risk” – Participant 2, new HIV diagnosis, postpartum interview.
Another woman, who had stopped taking her pills and attending her clinic appointments while in a previous relationship, drew upon firsthand experience to explain the dilemma that might lead women to discontinue their medication because of a relationship. On the one hand, she said, “the minute the partner doesn’t know, it gets quite difficult to take the treatment,” but “on the other hand, when one tells the boyfriend, who knows, the boyfriend might break up (Participant 18).”
DISCUSSION
HIV disclosure is a complex decision at any point, and even more so during the vulnerable pregnancy and postpartum periods. HIV disclosure carries the risk of social exclusion and material loss, but it also opens up the possibility to garner social support, alleviate mental health distress, and receive assistance in HIV care engagement. In this qualitative study with HIV-infected pregnant and postpartum women, we found that decisions about HIV disclosure were weighed carefully to consider the best person and best timing for HIV disclosures. No one in our sample had disclosed universally; rather, disclosure was selective and strategic. Only half of participants had disclosed to the father of their child, and non-disclosure to a partner was often a significant source of distress. Navigating HIV care engagement in the face of non-disclosure required specific strategies of concealment; these strategies may become more challenging in the later postpartum period, as women no longer have pregnancy for an excuse to attend frequent medical appointments. Taken together, these findings point to the importance of programs that aid women in making healthy decisions related to disclosure and facilitating disclosures when appropriate, which can relieve feelings of shame and anxiety and improve long-term HIV care engagement (11,31).
As has been noted widely in the literature, HIV stigma and HIV disclosure go hand in hand (3,16,32). HIV stigma includes enacted, anticipated and internalized forms of stigma (33). In this sample, reports of enacted stigma were rare, likely due to the very limited and selective nature of disclosure. Anticipated stigma, which refers to the expectation that one would be stigmatized when disclosing an HIV stigma, was common, and was a primary reason for non-disclosure. Anticipated stigma was based on observations of how other people living with HIV had been treated, whether in one’s family or in the broader community. As a result, women often sought out individuals who were living with HIV or had personal experiences with someone living with HIV, because they could feel confident that these individuals would not stigmatize them upon disclosure. Internalized stigma, including feeling of shame, were also ubiquitous and manifested in feeling “not brave enough” to tell others about an HIV status that they had not accepted themselves. For some, shame about the HIV status was compounded by shame about an unintended pregnancy and the burden of initiating and remaining adherent to HIV care, highlighting the “triple burden” faced by many women diagnosed with HIV during pregnancy (15,34).
Decisions about disclosure to a sexual partner, typically the father of the child, were influenced less directly by stigma, and more by a balance between a sense of responsibility and a perception of consequences. On the one hand, women noted feelings of obligation to tell a partner about potential HIV exposure, but on the other hand they worried about abandonment and the threat of violence. In this situation, women feared that disclosure would lead to being blamed for introducing HIV into the relationship (31,35). During pregnancy, it may be more likely that the balance between responsibility and fear of consequences tips toward the latter, given social and financial vulnerability around the pregnancy period. Few women in our sample had stable incomes, and there was significant stress around the ability to meet the economic needs of a child after birth. The fact that a large proportion of women had experienced dissolution of their relationships prior to or during their pregnancy speaks to the instability of partnerships in this setting, which makes HIV disclosure decisions particularly challenging (3,36).
Partner HIV testing in PMTCT may alleviate the burden placed on women of being the first person to know their HIV status (37–39). However, the data from this study suggests a resistance to HIV testing among men. Of the 11 women who disclosed to their partners, only five had then sought an HIV test themselves. Other studies from South Africa suggest that men face gender-specific barriers in HIV testing and treatment (40). Efforts to broaden HIV partner testing must be accompanied with community-based campaigns to encourage men to seek HIV testing and treatment, and presenting male role models living with HIV. By contrast, mandatory or coercive partner testing in PMTCT may undermine women’s autonomy, put them at risk of violence, and ultimately create barriers to entry in PMTCT (41).
Women who disclosed their HIV status noted important positive consequences in the form of added emotional support, instrumental support for care engagement, and improved self-acceptance. Women found particular comfort in disclosing to others who were either HIV-infected themselves or had been personally touched by HIV. In many cases, a woman’s HIV disclosure revealed that the person to whom she had disclosed was also HIV infected. This speaks to the added value of appropriate HIV disclosures, which build a supportive environment for others to disclose and may help to move a community towards a reduction in HIV stigma. These findings also underscore the importance of having available and visible networks of HIV-infected individuals who can provide peer support for people living with HIV (42,43). Peer support programs were instrumental in reducing stigma during the early stages of the HIV epidemic, and remain important today, as they help to sustain HIV care engagement across the continuum and improve coping behaviors among people living with HIV. During pregnancy and the early postpartum period, peer support related to HIV disclosure may be combined with education and support around pregnancy and parenting, in order to bolster the overall functioning and well-being of pregnant women and mothers living with HIV (44).
Non-disclosure of HIV may have impacts that undermine the potential of PMTCT programs, particularly in the test-and-treat era. Concealment of one’s HIV status may lead to loss to follow up, inconsistent clinic attendance, or poor medication adherence (2). Data from South Africa suggests that about a quarter of HIV-infected pregnant women fail to achieve full viral suppression at time of delivery, which drastically increases the potential for vertical transmission to the child (45). After childbirth, sustained care engagement may become even more challenging in the face of non-disclosure, once pregnancy is no longer an excuse for clinic attendance and taking medication. Postpartum non-adherence creates the opportunity for viral rebound, which may lead to the forward transmission to children via breastmilk as well as to sexual partners.
Our results suggest that PMTCT programs have a key role to play in helping individuals to make decisions about HIV disclosure, and assisting patients to navigate the disclosure process, particularly with partners. Training for health care providers on patient-centered care, with application to counseling on HIV disclosure, can help providers to develop skills in active listening, compassionate patient communication, and collaborative problem solving (46–48). There was evidence from our data that patients looked to providers to guide their decisions about HIV disclosure, and some participants offered suggestions for how providers could help to bring their partners in for HIV testing. Nurse-facilitated disclosures may be feasible in PMTCT settings (49); however, providers should also be attuned to the challenges patients face in disclosure, remain respectful of decisions not to disclose, and be equipped with creative strategies for supporting patients regardless of HIV disclosure decisions.
Future research on HIV disclosure in the pregnancy and postpartum periods should also include women who have established HIV diagnoses and are continuing HIV care during pregnancy. With a generalized epidemic and expansion of universal test-and-treat protocols for HIV, the majority of HIV-infected pregnant women in South Africa will likely enter ANC already knowing their HIV diagnosis and having previously initiated ART. The PMTCT setting creates an opportunity to support women in reassessing decisions about HIV disclosures, navigating new HIV disclosures, and setting a trajectory for sustained HIV care engagement that is not hampered by non-disclosures.
This study was unique in its repeated in-depth interviews during the pregnancy and postpartum periods, which allowed for a longitudinal perspective of HIV disclosure over the PMTCT continuum. The findings, however, must be interpreted in the light of the study’s limitations. Eligible participants were identified by the PMTCT nurses, and may reflect women who were more engaged, either in the quantity or quality of their contact with the clinic. Nurses were not asked to track the women who were not approached, or who were approached and refused participation, so we cannot evaluate the representativeness of the sample. The study missed women who did not attend antenatal care, or who presented late in pregnancy and were immediately transferred to the maternity hospital for their ANC services. It is possible that social desirability bias and discomfort talking about personal issues may have impeded the depth of some discussions. Finally, several women mentioned the impact of the pregnancy interview on their subsequent disclosure decisions, which changed the course of the naturalistic disclosure trajectory.
This study sheds light on the challenges of HIV disclosure in the context of PMTCT services in South Africa. Despite the generalized epidemic and universal availability of HIV treatment, HIV disclosure, particularly to male partners, remains a significant source of stress. The results of this study speak to the importance of integrating disclosure support and decision making into PMTCT programs in order to bolster and sustain the impact of PMTCT services.
Figure 1.
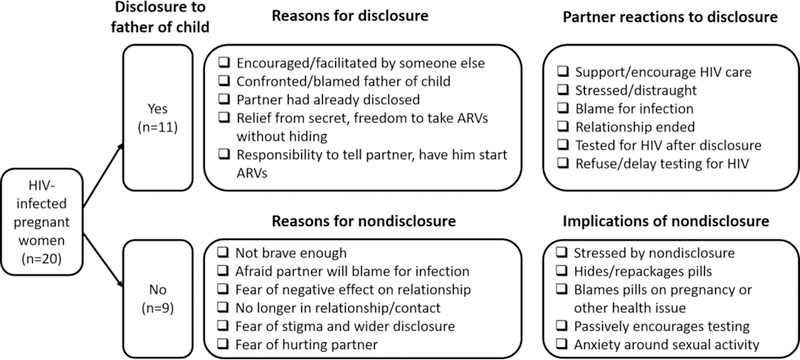
Disclosure to the father of the child
Acknowledgments:
This study was funded by a grant from the Duke University Center for AIDS Research (P30 AI064518) and supported by a grant from the National Institute of Mental Health (R34 MH102001). The first author was a scholar in the UCLA HIV/AIDS, Substance Abuse and Trauma Training Program (R25 DA035692). The research team is grateful for the support of the Western Cape Provincial Department of Health, the clinic administrators and health care providers, and the patients who contributed to this research.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: All authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. (Duke C0784, UCT 032/2015)
Informed consent: Informed consent was obtained from all individual participants included in the study.
REFERENCES
- 1.World Health Organization. Programmatic update: Use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants [Internet]. World Health Organization; 2012. Available from: http://www.who.int/hiv/PMTCT_update.pdf [Google Scholar]
- 2.Knettel BA, Cichowitz C, Ngocho JS, Knippler ET, Chumba LN, Mmbaga BT, et al. Retention in HIV Care During Pregnancy and the Postpartum Period in the Option B+ Era: A Systematic Review and Meta-Analysis of Studies in Africa. J Acquir Immune Defic Syndr 2018;77(5):427–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evangeli M, Wroe AL. HIV Disclosure Anxiety: A Systematic Review and Theoretical Synthesis. AIDS Behav 2017;21(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinkerton SD, Galletly CL. Reducing HIV Transmission Risk by Increasing Serostatus Disclosure: A Mathematical Modeling Analysis. AIDS Behav 2007. September;11(5):698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ekama SO, Herbertson EC, Addeh EJ, Gab-Okafor CV, Onwujekwe DI, Tayo F, et al. Pattern and Determinants of Antiretroviral Drug Adherence among Nigerian Pregnant Women. J Pregnancy 2012. [DOI] [PMC free article] [PubMed]
- 6.Spangler SA, Onono M, Bukusi EA, Cohen CR, Turan JM. HIV-Positive Status Disclosure and Use of Essential PMTCT and Maternal Health Services in Rural Kenya. J Acquir Immune Defic Syndr 2014. December 1;67(Suppl 4):S235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care 2015;27(4):436–50. [DOI] [PubMed] [Google Scholar]
- 8.Mnyani CN, McIntyre J. Challenges to delivering quality care in a prevention of mother-to-child transmission of HIV programme in Soweto, South Africa. Southern Afr J HIV Med 2013. May 21;14(2):64. [Google Scholar]
- 9.Peltzer K, Chao L- W, Dana P. Family Planning Among HIV Positive and Negative Prevention of Mother to Child Transmission (PMTCT) Clients in a Resource Poor Setting in South Africa. AIDS Behav 2009. October 1;13(5):973–9. [DOI] [PubMed] [Google Scholar]
- 10.Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ 2004. April;82(4):299–307. [PMC free article] [PubMed] [Google Scholar]
- 11.Naigino R, Makumbi F, Mukose A, Buregyeya E, Arinaitwe J, Musinguzi J, et al. HIV status disclosure and associated outcomes among pregnant women enrolled in antiretroviral therapy in Uganda: a mixed methods study. Reprod Health 2017. August 30;14(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adeniyi OV, Ajayi AI, Selanto-Chairman N, Goon DT, Boon G, Fuentes YO, et al. Demographic, clinical and behavioural determinants of HIV serostatus non-disclosure to sex partners among HIV-infected pregnant women in the Eastern Cape, South Africa. Xu J, editor. PLOS ONE 2017. August 24;12(8):e0181730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Madiba S, Letsoalo R. HIV Disclosure to Partners and Family among Women Enrolled in Prevention of Mother to Child Transmission of HIV Program: Implications for Infant Feeding in Poor Resourced Communities in South Africa. Glob J Health Sci 2013. July;5(4):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Visser MJ, Neufeld S, de Villiers A, Makin JD, Forsyth BWC. To tell or not to tell: South African women’s disclosure of HIV status during pregnancy. AIDS Care 2008. October;20(9):1138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crankshaw TL, Voce A, King RL, Giddy J, Sheon NM, Butler LM. Double disclosure bind: complexities of communicating an HIV diagnosis in the context of unintended pregnancy in Durban, South Africa. AIDS Behav 2014. January;18 Suppl 1:S53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one’s HIV-positive status, stigma and social support. AIDS Care 2008. November;20(10):1266–75. [DOI] [PubMed] [Google Scholar]
- 17.Olley BO, Ogunde MJ, Oso PO, Ishola A. HIV-related stigma and self-disclosure: the mediating and moderating role of anticipated discrimination among people living with HIV/AIDS in Akure Nigeria. AIDS Care 2016. June 2;28(6):726–30. [DOI] [PubMed] [Google Scholar]
- 18.Kimberly JA, Serovich JM, Greene K. Disclosure of HIV-Positive Status: Five Women’s Stories. Family Relations 1995. July;44(3):316. [Google Scholar]
- 19.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. Am J Public Health 2017. June;107(6):863–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Myer L, Phillips TK. Beyond “Option B+”: Understanding Antiretroviral Therapy (ART) Adherence, Retention in Care and Engagement in ART Services Among Pregnant and Postpartum Women Initiating Therapy in Sub-Saharan Africa. J Acquir Immune Defic Syndr 2017. June 1;75 Suppl 2:S115–22. [DOI] [PubMed] [Google Scholar]
- 21.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol 2000. March;19(2):124–33. [PubMed] [Google Scholar]
- 22.Klitzman RL, Kirshenbaum SB, Dodge B, Remien RH, Ehrhardt AA, Johnson MO, et al. Intricacies and inter-relationships between HIV disclosure and HAART: A qualitative study. AIDS Care 2004. July;16(5):628–40. [DOI] [PubMed] [Google Scholar]
- 23.Kelly JD, Hartman C, Graham J, Kallen MA, Giordano TP. Social Support as a Predictor of Early Diagnosis, Linkage, Retention, and Adherence to HIV Care: Results From The Steps Study. J Assoc Nurses AIDS Care 2014. September;25(5):405–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzalez JS, Penedo FJ, Antoni MH, Durán RE, McPherson-Baker S, Ironson G, et al. Social Support, Positive States of Mind, and HIV Treatment Adherence in Men and Women Living With HIV/AIDS. Health Psychol 2004. July;23(4):413–8. [DOI] [PubMed] [Google Scholar]
- 25.South Africa, National Department of Health. The 2015 National Antenatal Sentinel HIV and Syphilis Survey 2017.
- 26.Department of Health. National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults Pretoria, South Africa: National Department of Health, Republic of South Africa; 2015. [Google Scholar]
- 27.Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis Thousand Oaks, CA: SAGE; 2012. [Google Scholar]
- 28.Charmaz K Constructing grounded theory 2nd edition. Thousand Oaks, CA: SAGE; 2014. [Google Scholar]
- 29.Birks M, Chapman Y, Francis K. Memoing in qualitative research: Probing data and processes. J Res Nurs 2008. January 1;13(1):68–75. [Google Scholar]
- 30.Miles MB. Qualitative data analysis : an expanded sourcebook Thousand Oaks, CA: SAGE; 1994. [Google Scholar]
- 31.King R, Katuntu D, Lifshay J, Packel L, Batamwita R, Nakayiwa S, et al. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS Behav 2008. March;12(2):232–43. [DOI] [PubMed] [Google Scholar]
- 32.Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV Disclosure Across Diverse Settings: A Review. Am Journal Public Health 2011. June;101(6):1011–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV Stigma Mechanisms and Well-Being among PLWH: A Test of the HIV Stigma Framework. AIDS Behav 2013. June;17(5):1785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stinson K, Myer L. Barriers to initiating antiretroviral therapy during pregnancy: a qualitative study of women attending services in Cape Town, South Africa. Afr J AIDS Res 2012;11(1):65–73. [DOI] [PubMed] [Google Scholar]
- 35.Shamu S, Zarowsky C, Shefer T, Temmerman M, Abrahams N. Intimate Partner Violence after Disclosure of HIV Test Results among Pregnant Women in Harare, Zimbabwe. PLOS ONE 2014. October 28;9(10):e109447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vu L, Andrinopoulos K, Mathews C, Chopra M, Kendall C, Eisele TP. Disclosure of HIV Status to Sex Partners Among HIV-Infected Men and Women in Cape Town, South Africa. AIDS Behav 2012. January;16(1):132–8. [DOI] [PubMed] [Google Scholar]
- 37.Masters SH, Agot K, Obonyo B, Napierala Mavedzenge S, Maman S, Thirumurthy H. Promoting Partner Testing and Couples Testing through Secondary Distribution of HIV Self-Tests: A Randomized Clinical Trial. Tsai AC, editor. PLOS Medicine 2016. November 8;13(11):e1002166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aluisio A, Richardson BA, Bosire R, John-Stewart G, Mbori-Ngacha D, Farquhar C. Male Antenatal Attendance and HIV Testing Are Associated With Decreased Infant HIV Infection and Increased HIV-Free Survival. J of Acquir Immune Defic Syndr 2011. January;56(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Medley A, Baggaley R, Bachanas P, Cohen M, Shaffer N, Lo Y-R. Maximizing the impact of HIV prevention efforts: Interventions for couples. AIDS Care 2013. May 7;25(12):1569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Musheke M, Ntalasha H, Gari S, Mckenzie O, Bond V, Martin-Hilber A, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health 2013;13:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hardon A, Vernooij E, Bongololo-Mbera G, Cherutich P, Desclaux A, Kyaddondo D, et al. Women’s views on consent, counseling and confidentiality in PMTCT: a mixed-methods study in four African countries. BMC Public Health 2012;12:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paudel V, Baral KP. Women living with HIV/AIDS (WLHA), battling stigma, discrimination and denial and the role of support groups as a coping strategy: a review of literature. Reprod Health 2015;12:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simoni JM, Nelson KM, Franks JC, Yard SS, Lehavot K. Are Peer Interventions for HIV Efficacious? A Systematic Review. AIDS Behav 2011. November;15(8):1589–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Richter L, Rotheram-Borus MJ, Van Heerden A, Stein A, Tomlinson M, Harwood JM, et al. Pregnant women living with HIV (WLH) supported at clinics by peer WLH: a cluster randomized controlled trial. AIDS Behav 2014. April;18(4):706–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Myer L, Phillips T, McIntyre J, Hsiao N-Y, Petro G, Zerbe A, et al. HIV viraemia and mother-to-child transmission risk after antiretroviral therapy initiation in pregnancy in Cape Town, South Africa. HIV Med 2017. February;18(2):80–8. [DOI] [PubMed] [Google Scholar]
- 46.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns 2002. September;48(1):51–61. [DOI] [PubMed] [Google Scholar]
- 47.Epstein RM, Street RL. The Values and Value of Patient-Centered Care. Ann Fam Med 2011. March 1;9(2):100–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Consumers and Communication Group, editor. Cochrane Database Syst Rev 2012. December 12;12:CD003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Geubbels E, Williams A, Ramaiya A, Tancredi D, Young S, Chantry C. HIV status disclosure among postpartum women in rural Tanzania: predictors, experiences and uptake of a nurse-facilitated disclosure intervention. AIDS Care 2018. January 24;1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


