Abstract
Objectives
ENT surgeons and anesthesiologists work closely together in managing challenging airway cases. Sharing knowledge, experiences, and expectations interdisciplinary is essential in order to facilitate decision‐making and adequate management in emergency front‐of‐neck airway cases.
Methods
A survey was performed, to analyze level of experience, technique of preference, training, knowledge of material and protocols, and self‐efficacy scores of Dutch ENT surgeons and residents in performing an urgent or emergency front‐of‐neck airway.
Results
Within one year (January 2014–2015), 25.7% of the 257 respondents had performed an urgent or emergency front‐of‐neck airway. Of all reported emergency front‐of‐neck airways (N = 30), 80% were managed by tracheotomy. In future emergency front‐of‐neck airway cases, 74% stated cricothyrotomy would be their technique of preference. The majority would choose an uncuffed large‐bore cannula technique. Post‐academic hands‐on training was attended by 42% of respondents. Self‐efficacy scores were highest for surgical tracheotomy, and higher when trained or experienced. In case of an emergency scenario, 8.6% would not perform a front‐of‐neck airway themselves. The main reasons for reluctance to start in general were lack of experience and lack of training. Reported items for improvement were mainly the development of a protocol and training.
Conclusion
The chance of encountering an airway emergency scenario requiring front‐of‐neck airway is realistic. There is inconsistency between advised technique, technique of preference and technique actually performed by ENT surgeons. This study shows that there is both a need and desire for improvement in training and organization of care. Interdisciplinary guidelines and education is needed and could eventually safe lives.
Level of evidence
5
Keywords: Cricothyrotomy, tracheotomy, invasive airway management, survey, front‐of‐neck airway
INTRODUCTION
A challenging airway case can eventually lead to a situation in which tracheal intubation has failed and ventilation or oxygenation by noninvasive means is impossible. This is referred to as a cannot intubate, cannot oxygenate (CICO) situation.1, 2 Difficult airways are more likely to occur in the ear, nose, and throat (ENT) surgery population.3, 4
There is no gold standard for a difficult airway algorithm.5 Most guidelines are anesthesia orientated and all lead to a final step of invasive or front‐of‐neck airway (FONA). FONA can also be the primary technique of choice when tracheal access is considered unlikely to be successful, time consuming, and/or patients’ vitals are at risk. Depending on the circumstances, a case requiring FONA can be referred to as urgent (loss of patent airway is imminent but patients’ vitals are acceptable) or emergent (ie, CICO situation, no time to waste). We believe it is important to make a clear difference between these two scenarios, since the performer and approach in techniques used will vary.
In the Netherlands, ENT surgeons and anesthesiologists often work together in both urgent and emergency cases. It is important to understand how colleagues from other specialties feel about difficult airway management in general and in cases requiring FONA specifically. Anesthesiologists might have certain expectations concerning the role of ENT surgeons in such cases and vice versa. In the past, anesthesiologists have been surveyed about preparedness for difficult airway and or CICO scenarios.6, 7 To the best of our knowledge, no survey had been done regarding preparedness for FONA in an ENT surgeon and resident population. The objective of this survey is to investigate the organization of care in managing emergency airway scenarios by Dutch ENT surgeons and residents, in order to determine which aspects need improvement.
MATERIALS AND METHODS
A national survey was conducted using an online questionnaire, powered by Castor. The medical ethical committee (CCMO Arnhem‐Nijmegen) concluded that formal ethical approval was not required for this study (2015‐1660).
Questionnaire
The questionnaire was developed based on the literature and expert opinion. The survey contained personal questions subdivided into demographic data, materials, experience, the performance of FONA between January 2014 and 2015, training and self‐efficacy scores and general questions regarding available devices, protocols and airway management training available in the hospital the respondent was working at (see Appendix). Self‐efficacy is a way to describe the level of confidence a person has in performing a specific skill adequately. An emergency scenario was defined as a scenario in which IMMEDIATE action is required. Example: a cannot intubate, cannot oxygenate scenario. An urgent scenario was defined as (imminent) respiratory insufficiency based on an upper airway obstruction.
Participants
The questionnaire was sent to 599 registered members of the Dutch Society for Otorhinolaryngology and Head and Neck Surgery. Specialists involved in the construction of the questionnaire were excluded. The emails were sent in February 2015. All participants were informed that filling in the questionnaire was considered consent to use the collected data for research. Participation was voluntary.
Statistical Analysis
Data were analyzed using SPSS Statistics 20.0, statistical software for Windows (SPSS, Chicago, Illinois, USA), and Microsoft Office Excel 2010 (Microsoft Corporation, Redmond, Washington, USA). Data are presented as frequencies and percentages, unless otherwise indicated. Data are presented as numbers or percentages; self‐efficacy scores are presented on a 0–10 numeric rating scale (0 no confidence through 10 maximum confidence).
To compare categorical variables a Chi square test was used. Fisher's exact test was used in the case the expected frequency was less than 5 in one or more cells. To analyze the SE score, an independent samples t‐test was used. All statistical tests were two‐sided.
Personal comments were categorized by the first author and reassessed by the second author.
RESULTS
Returned surveys from 257 participants yielded a 43% response rate (257/599). The demographics are shown in Table 1.
Table 1.
Demographics.
| n | % | |
|---|---|---|
| Practise status | ||
| ENT specialist | 212 | 82.5% |
| Resident | 45 | 17.5% |
| 1st year* | 9 | 20% |
| 2nd year* | 8 | 17.8% |
| 3rd year* | 9 | 20% |
| 4th year* | 7 | 15.6% |
| 5th year* | 12 | 26.7% |
| Sex | ||
| Male | 166 | 64.6% |
| Female | 91 | 35.4% |
| Type of practice | ||
| University hospital | 95 | 37% |
| Community hospital with residents | 86 | 33.5% |
| Community hospital | 74 | 28.8% |
| Private clinic | 2 | 0.8% |
Percentage of all residents
ENT = ear, nose, throat.
Experience
Between January 2014 and 2015, a total of 117 FONAs were reported by 25.7% of all respondents (N = 66, 5 residents and 61 surgeons).
Of all procedures, 84 were labeled urgent and 30 were labeled emergent. Three procedures were not labeled as either one of them. Of all performed urgent and emergency FONAs, one patient did not survive. This was a reported performed tracheotomy in an emergency scenario. In seven cases, complications occurred.
Thirty emergency FONAs were reported. These were performed by 23 surgeons and 1 resident. A tracheotomy was performed in 80% of these emergency FONAs. One tracheotomy was a Percutaneous Dilatational Tracheostomy (PDT) and all other procedures were classical tracheotomies. In 20% (N = 6) of cases, a cricothyrotomy was performed. Of these six cases, one was a rapid four‐step technique, one was a Seldinger technique and four were uncuffed Quicktrach procedures. Fifty‐eight respondents reported a total of another 90 urgent or emergency FONAs in the past year where someone else performed the procedure. A total of 94 respondents (36.5%) encountered a scenario in which urgent or emergency FONA had to be performed. Sixty‐six respondents performed and 28 observed, but did not perform, FONA.
Materials, Protocols, and Technique of Preference
Of those respondents who could name available sets (N=238), 59.2% (N=141) stated that their hospital worked with a uniform device or technique, 15.1% (N =36) stated that there was no uniform technique and 25.6% (N = 61) did not know. Of all respondents who could name a uniform set, the majority named a large‐bore catheter percutaneous set. In this group, 88.7% named “Quicktrach” (60.3% uncuffed, 28.4% cuffed).
On the question: “Does your hospital work with an algorithm?”, 33.9% (N = 87) stated “yes”, 17.5% (N = 45) stated “no” and 38.5% (N = 99) answered “I don't know.’’ The remaining 10.1% (N = 26) of respondents stated that an algorithm was being developed in their hospital.
In the case of a future emergency scenario, 73.5% (N = 189) stated a cricothyrotomy would be their technique of preference. Forty‐nine respondents (19.1%) would perform a tracheotomy. The rest of the respondents would either wait for a colleague (4.3%) or use other less invasive treatment options first (3.1%), like a rigid or fiberoptic scope. The vast majority of the 189 respondents, (80.4%, N = 152) would perform a percutaneous large‐bore cricothyrotomy technique. In this group, 57.2% (N = 87) would choose an uncuffed large‐bore catheter technique. Surgical cricothyrotomy would be the technique of preference in 15% of the 189 respondents (N = 28) (the scalpel bougie technique was chosen by 5 of these 28). A small‐bore technique was chosen by 1.6% (N = 3). Six respondents would do a cricothyrotomy but could not say which technique.
Of the 19.1% (N = 49) who would choose a tracheotomy technique, 95.9% would choose the classical surgical technique.
When analyzing the subgroup (N = 24) who performed emergency FONA in the past year, 46% stated a cricothyrotomy would be their technique of preference. In this group (N = 24), 80% had actually performed a tracheotomy.
Training, Competency, and Self‐Efficacy
Post‐academic hands‐on training performing FONA had been attended by 42% (N = 108). More than half of the respondents did not have facilities to train in at their own hospital (51.6%, N = 133), or were not aware of it (20.7%, N = 53). Local training facilities were available to 27.7% (N = 71).
Respondents were mostly trained in surgical tracheotomy and large‐bore cannula cricothyrotomy techniques. Except for one, all ENT surgeons had learned to perform a classical tracheotomy during their residency. Twenty‐one ENT surgeons (9.9%) and one ENT resident (2.2%) felt they do not have to be competent in performing FONA. Other professionals who should be competent in performing urgent or emergency FONA are shown in Figure 1.
Figure 1.
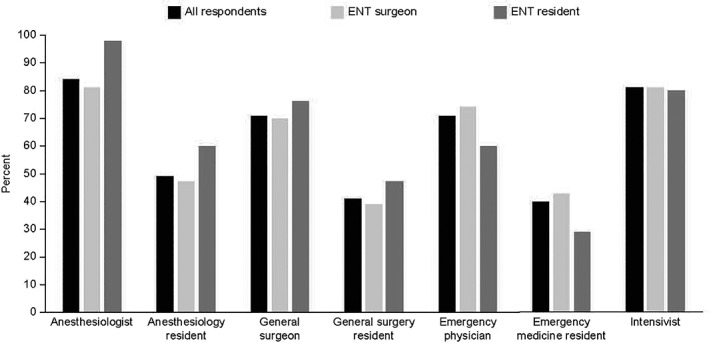
Other physicians who should be competent in performing urgent or emergency FONA according to all respondents and subgroups.
The highest scores in both the surgeon and resident groups were for surgical tracheotomy (7.6 vs. 5.9). The highest scores in the cricothyrotomy group were for the large‐bore technique. Self‐efficacy scores per technique are shown in Table 2.
Table 2.
Self‐Efficacy Scores per Physician per Technique.
| ENT surgeon | ENT resident | |
|---|---|---|
| Tracheotomy | ||
| PDT | 5.18 (3,013) | 2.58 (2,580) |
| Surgical | 7.63 (2,213) | 5.87 (2,989) |
| Cricothyrotomy | ||
| Small bore catheter | 5.11 (2,837) | 3.36 (2,765) |
| Large bore catheter | 6.74 (2,071) | 5.67 (2,266) |
| Surgical | 5.74 (2,743) | 3.58 (2,633) |
Self‐efficacy scores (0 no confidence–10 maximal confidence) are given as mean (SD)
ENT = ear, nose throat; PDT = Percutaneous Dilatational Tracheostomy; SD = standard deviation
The respondents who had clinical experience in performing urgent or emergency FONA, or had had post‐academic hands‐on training in emergency invasive airway management had higher self‐efficacy scores (Table 3).
Table 3.
Self‐Efficacy Scores per Technique per Subgroup
| Clinical experience past year | Post‐academic training | |||||||
|---|---|---|---|---|---|---|---|---|
| Yes (n = 66) | No (n = 191) | 95% CI | P‐value | Yes (n = 108) | No (n = 140) | 95% CI | P‐value | |
| Tracheotomy | ||||||||
| PDT | 6.41 (3.631) | 4.14 (3.046) | 1.50; 3.04 | <.001 | 5.06 (3.035) | 4.60 (3.153) | −0.33; 1.24 | .253 |
| Classic surgical | 8.97 (1.457) | 6.75 (2.473) | 1.72; 2.72 | <.001 | 7.52 (2.581) | 7.14 (2.397) | −0.24; 1.01 | .229 |
| Cricothyrotomy | ||||||||
| Small‐bore catheter | 6.15 (2.609) | 4.34 (2.581) | 1.06; 2,57 | <.001 | 5.19 (3.018) | 4.52 (2.804) | −0.07; 1.40 | .075 |
| Large‐bore catheter | 7.62 (1.708) | 6.18 (2.155) | 0.86; 2.02 | <.001 | 7.02 (1.986) | 6.23 (2.226) | 0.25; 1.33 | .004 |
| Surgical | 6.74 (2.825) | 4.88 (2.691) | 1.10; 2.63 | <.001 | 5.42 (2.955) | 5.39 (2.776) | −0.69; 0.75 | .933 |
(N) number of respondents trained or not trained or with or without clinical experience in urgent or emergency FONA in one year
Self‐efficacy scores (0 no confidence–10 maximal confidence) are given as mean (SD)
95% CI gives the 95% confidence interval for the difference in mean self‐efficacy scores (“yes” minus “no”)
PDT = Percutaneous Dilatational Tracheostomy
Reluctance, Improvement, and Personal Comments
In total, 8.6% (N = 22, 10 residents and 12 surgeons) of all respondents would not perform emergency FONA.
Some argued that in their hospital other specialists were in charge. The most important reason in general not to commence was lack of experience (44.7%, N = 115). Sixty‐five respondents (25.3%) stated they felt no reluctance to start. Other limiting factors according to all respondents were lack of training (12.8%, N = 33), low self‐efficacy (5.1%, N = 13) and poor knowledge of procedure (1.2%, N = 3), or other (8.9%, N = 23, see Table 4). Figure 2 shows results per subgroup.
Table 4.
Personal Comments Regarding Improvement and Reluctance to Start.
| Comments concerning reluctance to start * were related to: | Free comments regarding improvement † were related to: |
| Protocol/local agreements | Protocol |
| • Purchase of material • Distribution of tasks, especially when more specialties are involved • Response time • Checklist/protocol • Multidisciplinary agreements |
• Local agreements between specialties • Uniformity • Available material, location • Distribution of tasks |
| Experience | Training |
| • Either no experience or last tracheotomy many years ago • Theatre nurses and team members not well prepared to assist |
• Annual • Mandatory • Multidisciplinary • All aspects of difficult airway management |
| Material | Knowledge |
| Location of material | • Anatomy |
| No uniform technique | • Skills |
| Changing techniques Other • Communication, decision making, overruling a colleague • Unknown long term complications • Time pressure • Dealing with previous encountered complications Training • Both surgeon and team |
• Strongly dependent on available person • More general awareness needed amongst all team members • Available material location and protocol Material • Uniformity • Check‐up • location |
| Suggestions/questions | |
| • Need for recommendations | |
| • How should one handle a pediatric emergency airway case? | |
| • Multidisciplinary approach in PDT? | |
| Other | |
| • Positive statements on organization at this moment; Respondents stating things are well organized in their hospital or work is in progress at the moment, often following recent complications in airway management cases | |
| • Nontechnical skills like communication |
Items named by 8.9% of respondents
Items named by 36.2% of respondents
PDT = Percutaneous Dilatational Tracheostomy
Figure 2.
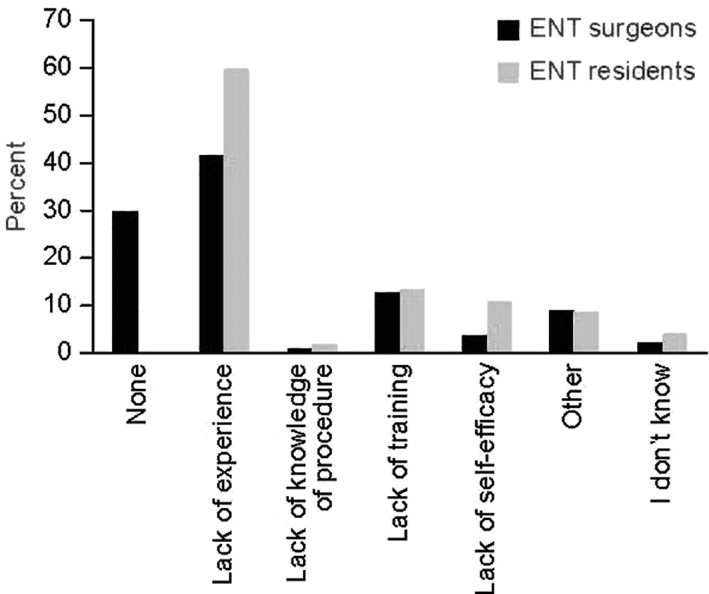
Most limiting factors in decision making regarding starting a FONA for subgroups ENT surgeons and residents.
Points of improvement, suggested by all respondents, were training in technical and nontechnical skills (64.2%), protocol and organization (57.2%), application of available material (37.4%), knowledge of anatomy (14%), and “I don't know’”(12%). Figure 4 shows results per subgroup. Table 4 summarizes mentioned personal free comments regarding improvement. All respondents who had performed urgent or emergency FONA in the previous year (N = 66), including those who had experienced complications or a failed procedure, would perform emergency FONA in the future. Having observed FONA was not associated with a higher percentage of respondents commencing future emergency FONA, compared with not having observed nor performed (Table 5).
Figure 4.
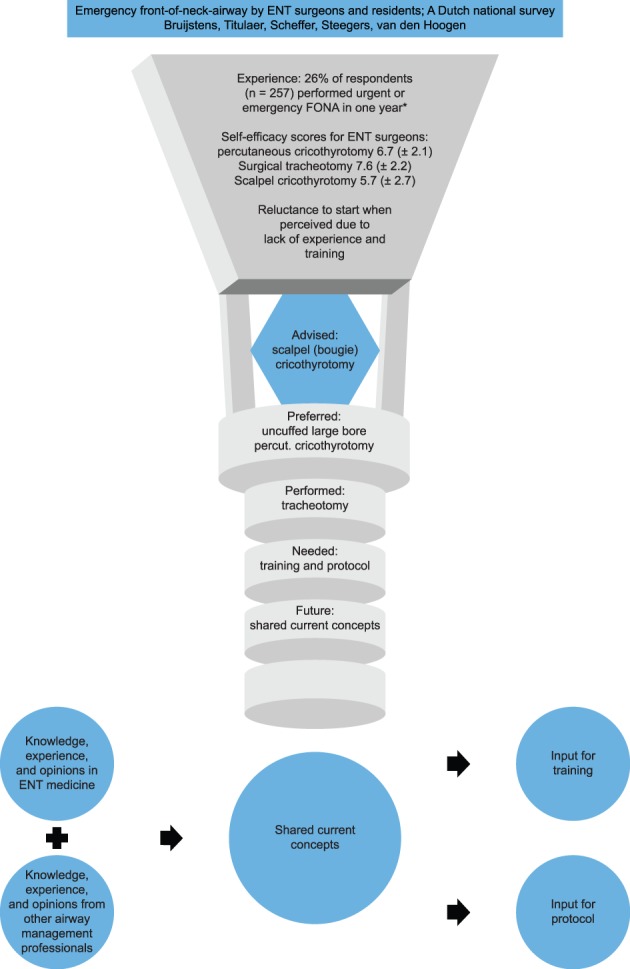
Graphical summary of content
Table 5.
Number of Respondents Who Would Perform Emergency FONA in the Future
| Would you create an invasive airway yourself? | |||
|---|---|---|---|
| Yes | No | P‐value | |
| Performed the procedure | 66 | 0 | .002 |
| Did not perform the procedure | 169 | 22 | |
| Observed, but did not perform | 25 | 3 | 1 |
| Did not observe, did not perform | 144 | 19 | |
FONA = front‐of‐neck airway
Figure 3.
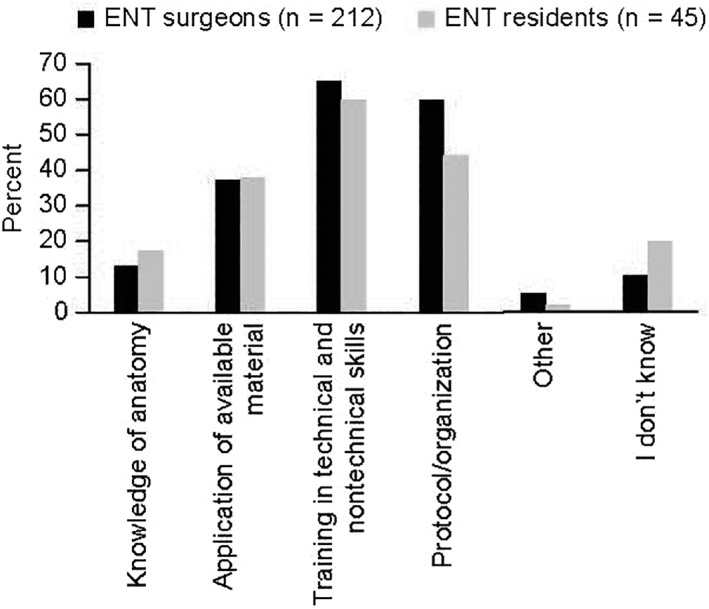
Items respondents would like to see improved in their hospital/organization (multiple answers possible), in percentages for subgroups
DISCUSSION
Experience
This survey was retrospective and not intended to determine incidence. However, it was not the number of reported emergency scenarios (30) that is most striking in these results, but the relatively large percentage of ENT surgeons and residents (36.5%, N = 94) who reported having encountered a case in which an urgent or emergency FONA was needed. Moreover, in personal comments some respondents stated they encounter these scenarios in a setting where more than one professional is present. In such cases, besides deciding what technical skill to perform and when to start, another important question arises: who is going to perform a FONA? Urgent scenarios can deteriorate. Therefore, the chance of encountering an emergency scenario as an ENT surgeon requiring FONA is realistic.
Materials and Protocols
For cricothyrotomy, most respondents work with uncuffed large‐bore techniques. Uncuffed large‐bore cannulas create an unsecured airway with less minute volume and suboptimal ventilation abilities.1 Expert opinion,1 NAP4,3 and difficult airway society (DAS) guidelines2 do not recommend small‐bore catheters or uncuffed cannulas in inexperienced hands because of possible serious complications. At the time of the survey there was no gold standard for a cricothyrotomy technique,1, 8 but surgical FONA was associated with better success rates than percutaneous techniques.3, 9, 10 The scalpel bougie method11, 12 might be an interesting alternative to a percutaneous technique for ENT surgeons, since it is based on skills that they are already familiar with. Moreover, this technique uses materials readily available (scalpel, introducing catheter, cuffed tube 6). The latest DAS guidelines2 suggested the scalpel (bougie) surgical cricothyrotomy technique as technique of choice in adults. The level of evidence is growing but is not yet conclusive for naming the scalpel bougie the gold standard cricothyrotomy technique.
Interestingly, discussion in anesthesiology journals mainly concern small bore (needle) cricothyrotomy versus scalpel (bougie) cricothyrotomy when choosing a FONA technique.13, 14 Our results show a different perspective in ENT surgeons and residents; these different perspectives should at the very least be shared interdisciplinary.
This study points out that many respondents are not aware of hospital protocols. This suggests that already existing guidelines, developed agreements and work in progress need to be brought to the attention of ENT surgeons and residents.
Recently an editorial15 written for United Kingdom airway professionals was published in both an otolaryngology and anesthesiology journal, underlining the importance of disseminating new guidelines on difficult airway management amongst all relevant specialties.
Training and Self‐Efficacy
Besides lack of clinical experience, this survey indicates that lack of training may have an influence on confidence in performing FONA and deciding to perform FONA in the future. Our results were consistent with those of Makowski et al.16 and suggest that one needs to perform the procedure oneself to raise the level of confidence, instead of just observing.
Residents are often first on call in emergency situations. Mean self‐efficacy scores were fairly low in all techniques in this group. Lack of self‐efficacy contributed more to reluctance to start in residents than in surgeons.
Due to the low number of cricothyrotomies performed, it is impossible to achieve and maintain competency during regular practice. Ideally, a well‐constructed program of training and maintaining skills in models would result in all ENT specialists and residents feeling (more) confident to handle an airway emergency and actually commence a procedure when needed.
Inconsistencies
Guidelines focus on cricothyrotomy for true emergency scenarios.2, 17, 18 Obtaining access to the trachea is quicker; identification of anatomic landmarks and access to the airway is easier, fewer structures can possibly be harmed.
The majority of respondents stated they would choose an uncuffed large‐bore cricothyrotomy technique in future emergency scenarios, most of the respondents had actually performed a tracheotomy in an emergency scenario, and the advised technique is a surgical scalpel (bougie) technique. At the time of the survey, the most recent DAS guidelines2 had not been published yet, but current concepts were not in favor of uncuffed large bore cannulas.1, 3
Studies have shown that the majority of anesthesiologists were ill‐prepared for a CICO‐situation and many have chosen techniques not recommended by international guidelines.6, 7, 19 The literature focusing on these skills in ENT departments is scarce20, 21 and does not concern primarily ENT surgeons or residents.
It seems ENT surgeons and residents fall back on skills in which they feel most confident, namely surgical tracheotomy and uncuffed large‐bore cannulas. These are also techniques respondents were mainly trained in or had clinical experience with.
In determining the technique of preference, self‐efficacy scores, training and available materials seem to play a role.
Regardless of the chosen technique, ENT surgeons should choose and train their technique of preference in advance. They should not only perform the technique they feel most confident in, but should also take note of recent developments and respect circumstances that may favor one technique over the other.
In our institution, at this moment, we train our ENT and anesthesiology residents to choose a tracheotomy in an urgent scenario, and a cricothyrotomy in an emergency scenario. We train together and we train both a cuffed percutaneous technique and scalpel bougie cricothyrotomy.
A limitation of this study is the response rate of 43%. Potential bias is a concern. On the other hand, two surveys amongst anesthesiologists often referred to in FONA literature had response rates of 47% and 39%.6, 7 The distribution of residents and consultants analyzed was representative for the total study population invited to participate (17.5% and 82.5% vs. 20% and 80%). Many respondents wrote personal remarks to illustrate their involvement with this subject.
Questions were partly retrospective. Recall bias is another concern. We cannot exclude that all reported emergency cases were in fact urgent cases or vice versa or that they actually happened in a different year. Respondents may have filled out socially desirable answers. Unfortunately, we do not have an (interdisciplinary) complication registration.
Future studies should try to combine both more objective data and outcome. We felt a survey would provide us with information we can use to start a more solid prospective interdisciplinary way of collecting data, complications, and points of improvement.
In the absence of an internationally uniform applied classification on context of FONA, but to facilitate understanding of different type of scenarios, we defined two nonelective scenarios; an urgent scenario in which there is time, and an emergency scenario in which there is no time left. These definitions need to be further optimized and other professionals should continue contextualizing FONA for every reported case. This definition of context is important because context will also determine who will be the designated performer of the FONA procedure. An initiative has recently been started to address critical language (referring to standardized communication) in airway management.22
We cannot explain the discrepancy between preferred and performed technique. We did not ask this question. Possibly attending a Dutch ENT meeting where this subject was a topic, or reading literature could have changed opinion on technique of preference. Possibly some, now we have illustrated the different contexts of elective, urgent and emergent, have a different opinion on what technique is best suited for what context. Future surveys should address how professionals decide on their technique of preference. It would be interesting to know whether techniques are chosen mainly based on whatever material is available, based on trained technique, based on performed technique in real life or based on what literature suggests. It would also be interesting to determine whether training scalpel bougie technique will change the technique of preference of ENT surgeons in a true emergency case.
We believe that our data are clinically relevant for both ENT surgeons and other airway professionals like anesthesiologists. In other surveys, some anesthesiologists have also responded to wait for other professionals in case of a true emergency airway scenario. Anesthesiologists and other airway professionals might expect ENT surgeons are willing and capable in performing FONA in urgent and emergency scenarios. This could, however, be a dangerous assumption, as 10% of ENT surgeons in this survey stated they feel they do not have to be competent in performing this procedure and 8.6% of respondents would not start FONA themselves. According to 81.1% of ENT surgeons, an anesthesiologist should be competent in performing urgent or emergency FONA. There seems to be a gap in expectations on who should be competent. To facilitate decision making and prevent a delay in actually starting FONA in time, local agreements need to be made on who will perform what procedure under which circumstances.
Clinical Applicability of the Survey
Based on the results of the survey, it seems there is a clear need and desire for reorganizing care regarding emergency invasive airway management in most hospitals.
Translating named items for improvement by respondents into recommendations, we find overlap with the NAP4 recommendations made in 2011.3
Many of the named items can be addressed in advance by:
-
Appointing a local multidisciplinary team responsible for all aspects of advanced airway management and in particular invasive airway management. This team should:
– Take note of current concepts, techniques and existing guidelines from relevant specialties;
– Make conscious decisions on what cricothyrotomy technique to use;
– Decide who should be competent in cricothyrotomy and tracheotomy;
– Train and assess these people on a regular base; and
– Create local work plans.
-
Training and assessments should:
– Consist of technical skills and non‐technical skills, human factors such as communication, teamwork, leadership, situation awareness and decision making;
– Ideally be organized with all team members;
– Focus on starting FONA in time;
– Explicate the difference between an expected and unexpected challenging airway, and urgent and emergency airway scenarios; and
– Be aimed at competency rather than familiarization.
CONCLUSION
The vast majority of ENT surgeons feel they should be competent; Dutch ENT residence training state that at the end of their training, residents should be competent in performing a cricothyrotomy and tracheotomy. These arguments should favor a clear effort to train to competence, maintain these skills in post‐academic professional careers, and organize logistics to create a standard of knowledge and care in emergency invasive airway management by ENT residents and surgeons. Interdisciplinary guidelines or protocols and education can be of value.
Editor's Note: This Manuscript was accepted for publication 25 May 2018.
Conflict of Interest: No external funding is declared. LB organizes an emergency invasive airway course in the Netherlands. FvdH is a faculty member of this course. Nonsterile samples have been provided by third parties for these courses.
BIBLIOGRAPHY
- 1. Hamaekers AE, Henderson JJ. Equipment and strategies for emergency tracheal access in the adult patient. Anaesthesia 2011;66(Suppl 2):65–80. [DOI] [PubMed] [Google Scholar]
- 2. Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015;115:827–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cook TM, Woodall N, Frerk C, Fourth National Audit P. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011;106:617–631. [DOI] [PubMed] [Google Scholar]
- 4. Arne J, Descoins P, Fusciardi J, et al. Preoperative assessment for difficult intubation in general and ENT surgery: predictive value of a clinical multivariate risk index. Br J Anaesth 1998;80:140–146. [DOI] [PubMed] [Google Scholar]
- 5. Artime CA, Hagberg CA. Is there a gold standard for management of the difficult airway? Anesthesiol Clin 2015;33:233–240. [DOI] [PubMed] [Google Scholar]
- 6. Wong DT, Lai K, Chung FF, Ho RY. Cannot intubate‐cannot ventilate and difficult intubation strategies: results of a Canadian national survey. Anesth Analg 2005;100:1439–1446. [DOI] [PubMed] [Google Scholar]
- 7. Wong DT, Mehta A, Tam AD, Yau B, Wong J. A survey of Canadian anesthesiologists' preferences in difficult intubation and “cannot intubate, cannot ventilate” situations. Can J Anaesth 2014;61:717–726. [DOI] [PubMed] [Google Scholar]
- 8. Langvad S, Hyldmo PK, Nakstad AR, Vist GE, Sandberg M. Emergency cricothyrotomy–a systematic review. Scand J Trauma Resusc Emerg Med 2013;21:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hubble MW, Wilfong DA, Brown LH, Hertelendy A, Benner RW. A meta‐analysis of prehospital airway control techniques part II: alternative airway devices and cricothyrotomy success rates. Prehosp Emerg Care 2010;14:515–530. [DOI] [PubMed] [Google Scholar]
- 10. Nakstad AR, Bredmose PP, Sandberg M. Comparison of a percutaneous device and the bougie‐assisted surgical technique for emergency cricothyrotomy: an experimental study on a porcine model performed by air ambulance anaesthesiologists. Scand J Trauma Resusc Emerg Med 2013;21:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heard AM, Green RJ, Eakins P. The formulation and introduction of a 'can't intubate, can't ventilate' algorithm into clinical practice. Anaesthesia 2009;64:601–608. [DOI] [PubMed] [Google Scholar]
- 12. Hill C, Reardon R, Joing S, Falvey D, Miner J. Cricothyrotomy technique using gum elastic bougie is faster than standard technique: a study of emergency medicine residents and medical students in an animal lab. Acad Emerg Med 2010;17:666–669. [DOI] [PubMed] [Google Scholar]
- 13. Timmermann A, Chrimes N, Hagberg CA. Need to consider human factors when determining first‐line technique for emergency front‐of‐neck access. Br J Anaesth 2016;117:5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baker PA, O'Sullivan EP, Kristensen MS, Lockey D. The great airway debate: is the scalpel mightier than the cannula? Br J Anaesth 2016;117(Suppl 1):i17–i9. [DOI] [PubMed] [Google Scholar]
- 15. Pracy JP, Brennan L, Cook TM, et al. Surgical intervention during a Can't Intubate Can't Oxygenate (CICO) event: Emergency Front‐of‐neck Airway (FONA)? Clin Otolaryngol 2016;41:624–626. [DOI] [PubMed] [Google Scholar]
- 16. Makowski AL. A survey of graduating emergency medicine residents' experience with cricothyrotomy. West J Emerg Med 2013;14:654–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management–part 2–the anticipated difficult airway. Can J Anaesth 2013;60:1119–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management–part 1–difficult tracheal intubation encountered in an unconscious/induced patient. Can J Anaesth 2013;60:1089–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Green L. Can't intubate, can't ventilate! A survey of knowledge and skills in a large teaching hospital. Eur J Anaesthesiol 2009;26:480–433. [DOI] [PubMed] [Google Scholar]
- 20. Whitcroft KL, Moss B, McRae A. ENT and airways in the emergency department: national survey of junior doctors' knowledge and skills. J Laryngol Otol 2016;130:183–189. [DOI] [PubMed] [Google Scholar]
- 21. Awad Z, Pothier DD. Management of surgical airway emergencies by junior ENT staff: a telephone survey. J Laryngol Otol 2007;121:57–60. [DOI] [PubMed] [Google Scholar]
- 22. Chrimes N, Cook TM. Critical airways, critical language. Br J Anaesth 2017;118:649–654. [DOI] [PubMed] [Google Scholar]


