Abstract
We present here an experimental approach for exploring a new class of tumor biomarkers that are overexpressed by circulating tumor cells (CTCs) and are likely targetable in immunotherapy against tumor metastasis. Using carbohydrate microarrays, anti-tumor monoclonal antibodies (mAbs) were scanned against a large panel of carbohydrate antigens to identify potential tumor glycan markers. Subsequently, flow cytometry and fiber-optic array scanning technology (FAST) were applied to determine whether the identified targets are tumor-specific cell-surface markers and are, therefore, likely suitable for targeted immunotherapy. Finally, the tumor glycan-specific antibodies identified were validated using cancer patients’ blood samples for their performance in CTC-detection and immunotyping analysis. In this article, identifying breast CTC-specific glycan markers and targeting mAbs serve as examples to illustrate this tumor biomarker discovery strategy.
Keywords: Glycan markers, Breast circulating tumor cells, Carbohydrate microarray, Breast cancer
15.1. Introduction
Breast cancer (BCa) is among the most prevalent cancers and accounts for the highest number of cancer-related deaths among women worldwide (Chatterjee and Zetter 2005). Identifying biomarkers of immunological significance is important in developing precision diagnostic and therapeutic strategies to advance current BCa healthcare. Recognition of abnormal glycosylation in virtually every cancer type has raised great interest in exploration of the tumor glycome for biomarker discovery (Hakomori 1989, 2001; Fukuda 1996; Dube and Bertozzi 2005). Potential glycan markers of BCa identified may include, but are not limited to, mucin-1 (CA 15–3) (Persson et al. 2009), carcinoembryonic antigen (Haidopoulos et al. 2000), sialyl Lewis x (Renkonen et al. 1997; Nakagoe et al. 2002), and glycoforms of a number of serum acute phase proteins, such as α1-acid glycoprotein, α1-antichymotrypsin, and haptoglobin β-chain (Abd Hamid et al. 2008). Since carbohydrate moieties are often surface-exposed and easily accessible by antibodies, some targets have been employed for antibody therapeutics (Vassilaros et al. 2013; Apostolopoulos et al. 2006; Shibata et al. 2009; Tomlinson et al. 1995).
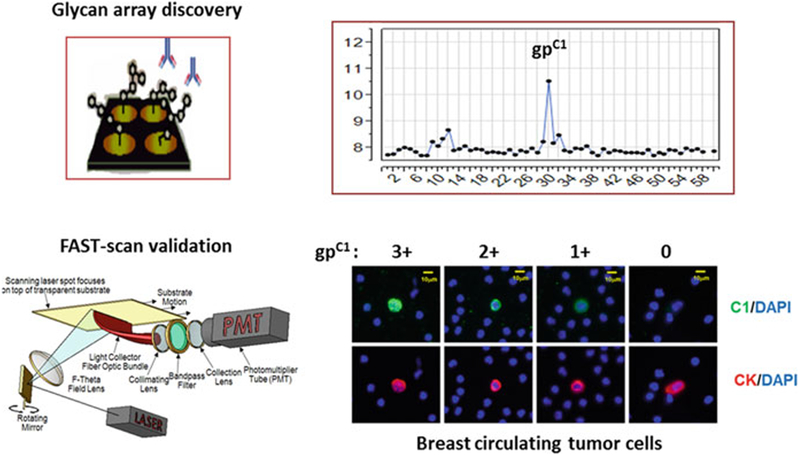
Exploring glycan markers of breast circulating tumor cells (bCTCs) represents a new development in tumor biomarker discovery. Although bCTCs are rare in blood, they play a key role in tumor metastasis (Jacob et al. 2007; Hayashi and Yamauchi 2012). Detection of CTCs has been explored as a non-invasive “liquid biopsy” for tumor diagnosis and prognosis (Somlo et al. 2011; Das et al. 2012; Liu et al. 2012). Glycan markers of bCTCs may have unique value in BCa healthcare, especially in the personalized therapy that targets specific immunotypes of BCa. Thus, our team has worked to establish a practical strategy to facilitate identification and characterization of potential glycan markers of bCTCs. Figure 15.1 highlights two core technologies explored in this investigation.
Fig. 15.1.
Glycan array discovery and FAST-scan validation of a novel glycan marker gpC1 of bCTCs (Adapted from Wang et al. 2015a)
15.2. Carbohydrate Microarray Identifies Blood Group Precursors as the Natural Ligands of Anti-tumor Antibody HAE3
Antibody responses elicited by native tumor glycoprotein antigens may target glycan-based antigenic determinants in addition to conventional protein epitopes. MAbs established by such immunization strategies are highly valuable for tumor biomarker discovery (Wang et al. 2015a; Wang et al. 2015b; Codington et al. 1972; Gao et al. 2014; Newsom-Davis et al. 2009). In this study, an anti-tumor mAb, HAE3, served as a key reagent for probing bCTC-glycan markers. This mAb was raised against epiglycanin, the major sialomucin glycoprotein (~ 500 kDa) of murine mammary adenocarcinoma TA3 cells (Codington et al. 1972). Interestingly, HAE3 was found to strongly cross react with a number of human epithelial tumors in tissues, including lung, prostate, bladder, esophagus, and ovarian cancers (Li et al. 2004; Liang et al. 2004; Somlo et al. 2011; Yao et al. 2004). This cross-species tumor binding profile suggests the possibility that HAE3 may recognize a conserved tumor glycan marker that is co-expressed by both mouse- and human-derived epithelial cancers.
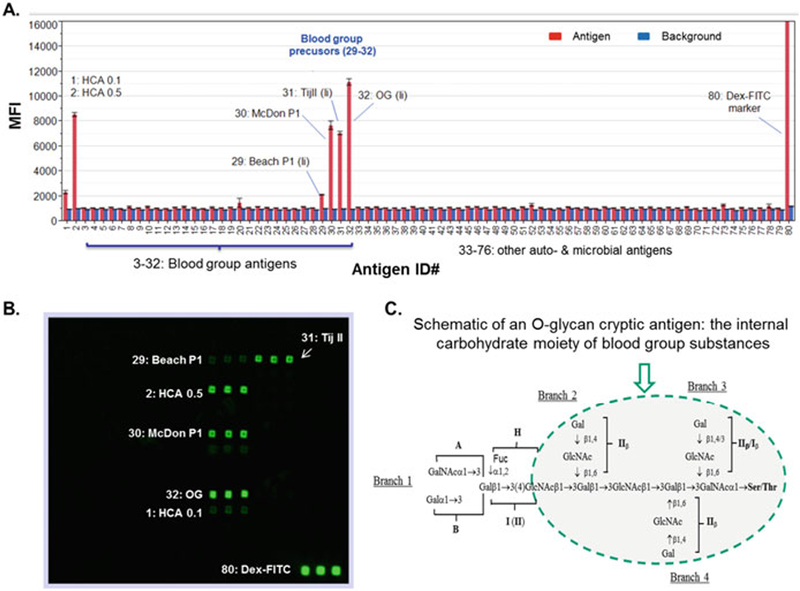
We produced, therefore, a comprehensive carbohydrate microarray to explore potential tumor glycan markers using antibody HAE3. As shown in Fig. 15.2, a large collection of purified natural carbohydrate antigens was applied for carbohydrate microarray construction. Blood group substance reference reagents (Kabat 1956) used include Cyst 9 and Cyst 14, A active; Beach phenol insoluble, B active; Hog, H active; JS phenol insoluble, H and Leb active, and N-1 20% from the second 10%, Lea active. Importantly, a number of blood group precursor references, including OG, Tij II, Beach P1, and McDon P1 (29#–32#), were spotted in this carbohydrate microarray. These precursor substances were prepared to remove most of the α-L-fucosyl end groups that are essential for blood group A, B, H, or Lewis active side chains, but possess the internal domains or core structures of blood group substances. A large panel of other autoantigens and microbial polysaccharides were also spotted in the same microarrays to critically examine the antibody binding specificity. A preparation of HAE3-reactive human carcinoma-associated antigen (HCA) served as a positive control for this assay (Li et al. 2004).
Fig. 15.2.
Carbohydrate microarray analysis of anti-epiglycanin mAb HAE3. Seventy-six glyco-proteins, glycoconjugates, and polysaccharides were spotted in triplicates in 1 to 2 dilutions to yield the customized microarrays for antibody screening. (a) Microarray detections were shown as the mean fluorescent intensities (MFIs) of each microspot with antigen-binding signal in red and background reading in blue. Each error bar is constructed using one standard deviation from the mean of triplicate detections. The labeled antigens include HCA (ID# 1 and 2), a number of blood group precursors (29#–32#), and a microarray spotting marker (80#). (b) Images of a microarray stained with HAE3 (5 μg/ml). (c) Schematic of a blood group substance structure with the conserved O-glycan core highlighted (Adapted from Wang et al. 2015b)
In Fig. 15.2a, HAE3 binding signal (red column) are plotted with corresponding local background reading (blue column) as an overlay plot. Each data point represents the mean of triplicate detections; these are shown in the Fig. 15.2b microarray image with the number of positive antigens labeled. Each error bar is constructed using one standard deviation from the mean. As illustrated, HAE3 is strongly positive with HCA (1# and 2#) as expected. Importantly, this antibody selectively binds to four blood group precursor antigens, Beach P1 (29#), McDon P1 (30#), Tij II (31#), and OG (32#). By contrast, HAE3 has no detectable cross-reactivity with blood group substances A, B. O, or Lewis antigens, or the large panel of other carbohydrate antigens spotted in the same array.
Figure 15.2c is a schematic of blood group substance structure with the common blood group precursor core structure highlighted. The four branched structure in the circle represents the internal portion of the carbohydrate moiety of blood group substances, which was proposed based on extensive immunochemical characterization of precursor OG and other P1 fractions of blood group precursors that were isolated from ovarian cancer cyst fluids (Vicari and Kabat 1970; Feizi et al. a, 1971b; Wu et al. 2007). Selective detection of these blood group precursors from a large panel of blood group substances by HAE3 illustrated that this antibody is specific for a shared cryptic glyco-epitope of these precursor substances.
15.3. Flow Cytometry Analysis to Examine Tumor Cell Surface Expression of HAE3+ Glyco-Epitopes
We further examined whether the HAE3+ glyco-epitopes were expressed as cell surface tumor markers. To ensure the observed cross-species antigenic reactivities are not owing to the unexpected presence of oligoclonal populations in the original HAE3 hybridoma cell line, we further subcloned HAE3 and produced antibody from a single clone, HAE3-C1 (C1). Antibody C1 was verified by carbohydrate microarrays and a glycan-specific ELISA to be highly specific for a conserved O-glycan cryptic glyco-epitope gpC1 in human blood group precursors (Wang et al. 2015a).
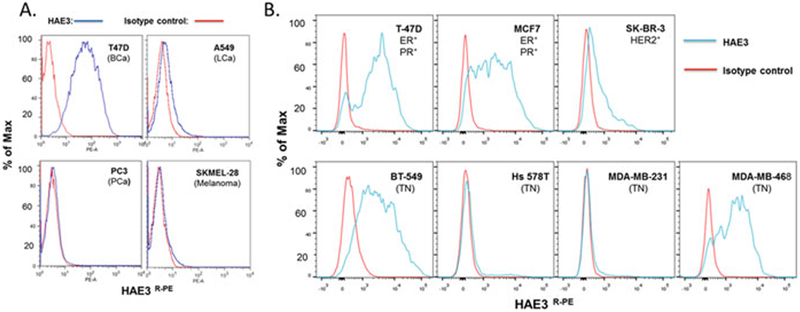
In the first set of experiments, we screened a panel of four tumor cell lines by cell surface staining in flow cytometry. These include (a) a BCa line, T-47D, which was selected owing to the fact that breast cancer patients were found to produce substances in circulation that are highly effective in inhibiting AE3-binding of epiglycanin (Codington et al. 2002; Codington et al. 1997); (b) a lung cancer (LCa) line, A549, which is known to produce an HAE3-positive substance in cell culture; (c) a prostate cancer (PCa) line, PC3, which is found to express a blood group B-related F77 glyco-epitope (Gao et al. 2014; Nonaka et al. 2014); and (d) a melanoma cell line SKMEL-28, which is derived from skin but not epithelial tissue. As shown in Fig. 15.3a, melanoma SKMEL-28 and prostate cancer PC3 were negative for HAE3. The A549 lung cancer cell line was weakly positive. By contrast, the breast cancer cell line T-47D was strongly positive in HAE3-cell surface staining.
Fig. 15.3.
HAE3 cell surface staining detected selective expression of the HAE3-cryptic glycan markers in human cancer cell lines. (a) Four tumor cell lines, T-47D, A549, PC3, and SKMEL-28, were stained with the C1 preparation of HAE3 (IgM) at 1:6 dilution or with an isotype control IgM,9.14.7 (5.0 μg/ml). (b) Seven breast cancer cell lines were stained with purified mAb HAE3(5.0 μg/ml) or 9.14.7 (5.0 μg/ml). These cell lines are T-47D, MCF-7, SK-BR-3, BT-549, Hs578T, MDA-MB-231, and MDA-MB-468. An R-PE-conjugated goat anti-mouse IgM antibody was applied to quantify the cell surface-captured IgM antibodies. Blue line: HAE3 stain; Red line:9.14.7 IgM isotype control (Adapted from Wang et al. 2015b)
Given these results, we extended the flow cytometry analysis to a panel of seven human breast cancer cell lines, including two estrogen receptor positive (ER+) and progesterone receptor positive (PR+) lines (T-47D and MCF-7), one ER+ (SK-BR-3), and four triple-negative (TN) cancers that lack the estrogen, progesterone, and Her2/neu receptors (BT-549, Hs 578 T, MDA-MB-231, and MDA-MB-468). Fig. 15.3b shows that two ER+PR+ lines, T-47D and MCF-7, and two triple-negative lines, BT-549 and MDA-MB-468, are HAE3 strongly positive. SK-BR-3 is intermediately positive. By contrast, the two remaining triple-negative cell lines, Hs578T and MDA-MB-231, were HAE3 negative.
15.4. Detection of Glycan Marker-Positive bCTCs in Stage IV Breast Cancer Patients
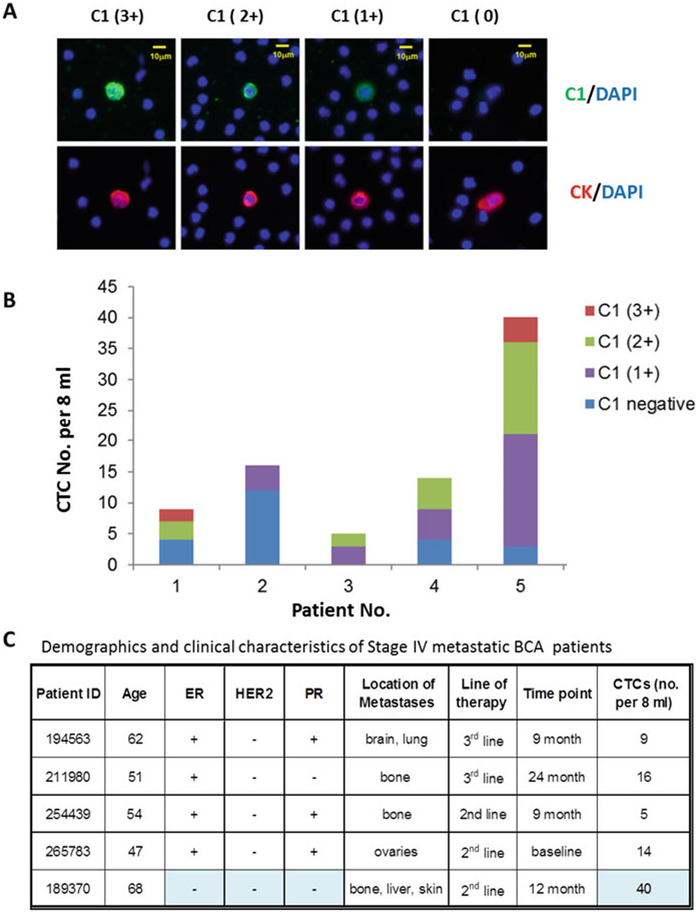
With antibody C1 as a key probe, we investigated whether gpC1 is applicable for detection and immunotyping analysis of CTCs in patients with metastatic breast cancer. In a pilot clinical case study, we characterized blood samples from five Stage IV breast cancer patients using the FAST-scan technology. Figure 15.4a illustrates how CTCs captured from the Stage IV breast cancer patients were scored as 3+, 2+, 1+, and 0, left to right. Four representative bCTCs are shown in which the epithelial-derived cells were labeled by anti-cytokeratins (CK) antibodies in red, and the gpC1 positive cells were stained in green in the background of the DAPI-blue labeling of white blood cells. Figure 15.4b and c show that all subjects characterized had gpC1-positive CTCs. Approximately 40% of CTCs captured in these patients expressed higher levels (2+ and 3+) of the gpC1 markers; gpC1-positive and -negative CTCs were found to co-exist in four subjects. Notably, a triple-negative patient (ID# 189370) produced predominantly gpC1-positive CTCs (37 of 40 CTCs) with 50% scored gpC1 2+/3+. In this patient, metastatic tumors were seen in multiple sites, including bone, liver, and skin.
Fig. 15.4.
Glycan marker gpC1 is expressed in significant numbers of CTCs in Stage IV breast cancer patients. (a) FAST-scan images of bCTCs. Upper panels: Co-staining of C1 (green) and DAPI (blue); Bottom panels: co-staining of anti-CK (red) and DAPI (blue). (b) Distribution of gpC1–positive and -negative bCTCs in five subjects. C1-staining of bCTCs was semi-quantitatively measured by the FAST scan as antibody negative (blue), 1+ (purple), 2+ (green), and 3+ (red) as described. A patient with triple-negative BCa (ID# 189370) was measured gpC1–positive in 37 of 40 CTCs with 50% scored as strong positive (2+ and 3+). (ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor 2). (c) A summary of patients’ demographics and clinical characteristics (Adapted from Wang et al. 2015a)
It is noteworthy that more than 1 million global cases of BCa are diagnosed each year and approximately 15% are triple negative. Owing to the lack of an effective therapeutic target, a younger age at onset, and early metastatic spread, patients suffering triple-negative BCa often have poor prognoses and clinical outcomes (Anders and Carey 2009; Brenton et al. 2005). If gpC1 were confirmed to be significantly associated with the triple-negative BCa in a larger cohort validation study, this O-core cryptic glycan marker could be used for immunotype-enhanced precision diagnosis and prognosis of BCa and targeted immunotherapy against BCa metastasis.
15.5. Summary
Although tumor-associated abnormal glycosylation has been recognized for years, identifying glycan markers of CTCs remains technically challenging. We describe here a practical approach to overcome this difficulty. Conceptually, we take advantage of the fact that the immune systems of many animal species are able to recognize subtle changes in sugar moieties displayed by cells or soluble antigens and produce specific antibodies for abnormally expressed tumor glycan markers. Experimentally, we first screened anti-tumor mAbs using carbohydrate microarrays to identify those that are specific for glycan markers. Subsequently, we determined whether the selected mAbs are specific for the cell-surface glycan markers using flow cytometry and FAST-scan technology. Finally, we used the new antibody probe to monitor CTC-expression of corresponding glycan markers in advanced breast cancer patients. This approach is likely to be generally useful for exploring potential glycan markers of CTCs of epithelial cancers.
Acknowledgments
The authors acknowledge the Kabat Collection of Carbohydrate Antigens at SRI International for a number of carbohydrate antigens that were applied in this study.
This work was supported in part by NIH grants U01CA128416 (DW) and R56AI118464 (DW), and by SRI International IR&D funds (DW and XL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest There are no conflicts of interest to declare for any of the authors involved in this work.
References
- Abd Hamid UM, Royle L, Saldova R et al. (2008) A strategy to reveal potential glycan markers from serum glycoproteins associated with breast cancer progression. Glycobiology 18(12):1105–1118 [DOI] [PubMed] [Google Scholar]
- Anders CK, Carey LA (2009) Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin Breast Cancer 9(Suppl 2):S73–S81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apostolopoulos V, Pietersz GA, Tsibanis A et al. (2006) Pilot phase III immunotherapy study in early-stage breast cancer patients using oxidized mannan-MUC1 [ISRCTN71711835]. Breast Cancer Ress: BCR 8(3):R27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenton JD, Carey LA, Ahmed AA et al. (2005) Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol Off J Am Soc Clin Oncol 23(29):7350–7360 [DOI] [PubMed] [Google Scholar]
- Chatterjee SK, Zetter BR (2005) Cancer biomarkers: knowing the present and predicting the future. Future Oncol 1(1):37–50 [DOI] [PubMed] [Google Scholar]
- Codington JF, Sanford BH, Jeanloz RW (1972) Glycoprotein coat of the TA3 cell. Isolation and partial characterization of a sialic acid containing glycoprotein fraction. Biochemistry 11(14):2559–2564 [DOI] [PubMed] [Google Scholar]
- Codington JF, Mass N, Haavik S et al. (1997) Antibodies to human carcinoma antigen. US Pat No5,693,763, December 2, 1997 [Google Scholar]
- Codington JF, Haavik S, Nikrui N et al. (2002) Immunologic quantitation of the carcinoma specific human carcinoma antigen in clinical samples. Cancer 94(3):803–813 [DOI] [PubMed] [Google Scholar]
- Das M, Riess JW, Frankel P et al. (2012) ERCC1 expression in circulating tumor cells (CTCs) using a novel detection platform correlates with progression-free survival (PFS) in patients with metastatic non-small-cell lung cancer (NSCLC) receiving platinum chemotherapy. Lung Cancer 77(2):421–426 [DOI] [PubMed] [Google Scholar]
- Dube DH, Bertozzi CR (2005) Glycans in cancer and inflammation – potential for therapeutics and diagnostics. Nat Rev Drug Discov 4(6):477–488 [DOI] [PubMed] [Google Scholar]
- Feizi T, Kabat EA, Vicari G et al. (1971a) Immunochemical studies on blood groups. XLVII. The I antigen complex – precursors in the A, B, H, Lea, and leb blood group system – hemagglutination-inhibition studies. J Exp Med 133(1):39–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feizi T, Kabat EA, Vicari G et al. (1971b) Immunochemical studies on blood groups.XLIX. The I antigen complex: specificity differences among anti-I sera revealed by quantitative precipitin studies; partial structure of the I determinant specific for one anti-I serum. J Immunol 106(6):1578–1592 [PubMed] [Google Scholar]
- Fukuda M (1996) Possible roles of tumor-associated carbohydrate antigens. Cancer Res 56 (10):2237–2244 [PubMed] [Google Scholar]
- Gao C, Liu Y, Zhang H et al. (2014) Carbohydrate sequence of the prostate cancer-associated antigen F77 assigned by a mucin O-glycome designer Array. J Biol Chem 289(23):16462–16477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haidopoulos D, Konstadoulakis MM, Antonakis PT et al. (2000) Circulating anti-CEA antibodies in the sera of patients with breast cancer. Eur J Surg Oncol: J Eur Soc Surg Oncol Br Assoc Surg Oncol 26(8):742–746 [DOI] [PubMed] [Google Scholar]
- Hakomori S (1989) Aberrant glycosylation in tumors and tumor-associated carbohydrate antigens. Adv Cancer Res 52:257–331 [DOI] [PubMed] [Google Scholar]
- Hakomori S (2001) Tumor-associated carbohydrate antigens defining tumor malignancy: basis for development of anti-cancer vaccines. Adv Exp Med Biol 491:369–402 [DOI] [PubMed] [Google Scholar]
- Hayashi N, Yamauchi H (2012) Role of circulating tumor cells and disseminated tumor cells in primary breast cancer. Breast Cancer 19(2):110–117 [DOI] [PubMed] [Google Scholar]
- Jacob K, Sollier C, Jabado N (2007) Circulating tumor cells: detection, molecular profiling and future prospects. Expert Rev Proteomics 4(6):741–756 [DOI] [PubMed] [Google Scholar]
- Kabat EA (1956) Blood group substances, their chemistry and immunochemistry. Academic,New York [Google Scholar]
- Li R, Yao JL, Bourne PA et al. (2004) Frequent expression of human carcinoma-associated antigen, a mucin-type glycoprotein, in cells of prostatic carcinoma. Arch Pathol Lab Med 128(12):1412–1417 [DOI] [PubMed] [Google Scholar]
- Liang S, Yao J, Bourne PA et al. (2004) Overexpression of human carcinoma-associated antigen in esophageal adenocarcinoma and its precursor lesions. Am J Clin Pathol 122(5):747–751 [DOI] [PubMed] [Google Scholar]
- Liu X, Hsieh HB, Campana D et al. (2012) A new method for high speed, sensitive detection of minimal residual disease. Cytometry Part A J Int Soc Anal Cytol 81(2):169–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagoe T, Fukushima K, Itoyanagi N et al. (2002) Expression of ABH/Lewis-related antigens as prognostic factors in patients with breast cancer. J Cancer Res Clin Oncol 128(5):257–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newsom-Davis TE, Wang D, Steinman L et al. (2009) Enhanced immune recognition of cryptic glycan markers in human tumors. Cancer Res 69(5):2018–2025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonaka M, Fukuda MN, Gao C et al. (2014) Determination of carbohydrate structure recognized by prostate-specific F77 monoclonal antibody through expression analysis of Glycosyltransferase genes. J Biol Chem 289(23):16478–16486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson J, Backstrom M, Johansson H et al. (2009) Molecular evolution of specific human antibody against MUC1 mucin results in improved recognition of the antigen on tumor cells. Tumour Biol J Int Soc Oncodev Biol Med 30(4):221–231 [DOI] [PubMed] [Google Scholar]
- Renkonen J, Paavonen T, Renkonen R (1997) Endothelial and epithelial expression of sialyl Lewisx and sialyl Lewisa in lesions of breast carcinoma. Int J Cancer 74(3):296–300 [DOI] [PubMed] [Google Scholar]
- Shibata S, Raubitschek A, Leong L et al. (2009) A phase I study of a combination of yttrium-90-labeled anti-carcinoembryonic antigen (CEA) antibody and gemcitabine in patients with CEA-producing advanced malignancies. Clin Cancer Res Off J Am Assoc Cancer Res 15(8):2935–2941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somlo G, Lau SK, Frankel P et al. (2011) Multiple biomarker expression on circulating tumor cells in comparison to tumor tissues from primary and metastatic sites in patients with locally advanced/inflammatory, and stage IV breast cancer, using a novel detection technology. Breast Cancer Res Treat 128(1):155–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson IP, Whyman A, Barrett JA et al. (1995) Tumour marker CA15–3: possible uses in the routine management of breast cancer. Eur J Cancer 31A(6):899–902 [DOI] [PubMed] [Google Scholar]
- Vassilaros S, Tsibanis A, Tsikkinis A et al. (2013) Up to 15-year clinical follow-up of a pilot phase III immunotherapy study in stage II breast cancer patients using oxidized mannan-MUC1. Immunotherapy 5(11):1177–1182 [DOI] [PubMed] [Google Scholar]
- Vicari G, Kabat EA (1970) Structures and activities of oligosaccharides produced by alkaline degradation of a blood group substance lacking A, B, H, Le b specificities. Biochemistry 9(17):3414–3421 [DOI] [PubMed] [Google Scholar]
- Wang D, Liu X, Hsieh B et al. (2015a) Exploring glycan markers for immunotyping and precision-targeting of breast circulating tumor cells. Arch Med Res 46(8):642–650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Tang J, Liu S et al. (2015b) Blood group precursor cryptic glyco-epitopes as breast cancer cell surface markers for immune recognition and targeting. J Immunol Res 9:510810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu AM, Khoo KH, Yu SY et al. (2007) Glycomic mapping of pseudomucinous human ovarian cyst glycoproteins: identification of Lewis and sialyl Lewis glycotopes. Proteomics 7(20):3699–3717 [DOI] [PubMed] [Google Scholar]
- Yao JL, Bourne PA, Yang Q et al. (2004) Overexpression of human carcinoma-associated antigen in urothelial carcinoma of the bladder. Arch Pathol Lab Med 128(7):785–787 [DOI] [PubMed] [Google Scholar]