Abstract
Ameloblastoma treatment varies based on the clinical, histopathologic, and radiographic characteristics. Aggressive surgical treatments, such as marginal or segmental resection, have traditionally been implemented, but some conservative surgical methods are also being introduced, including decompression, enucleation, or curettage. The aim of the present study was to evaluate the possibility of applying these conservative surgical treatments to ameloblastoma and to analyze the prognosis of the procedures and their healing aspects. Among all patients who visited our clinic (Department of Oral and Maxillofacial Surgery, Kyung Hee University Dental Hospital at Gangdong) from 2009 to 2017, three who had undergone conservative surgery were recruited. One of these three patients underwent both excision of the lesion and an iliac bone graft during the same procedure. In the other two patients, due to the size of the lesion, decompression was performed to reduce the size of the lesion, and then conservative surgical treatments followed. As shown in the cases of this study, patients were only treated with conservative surgical methods, such as decompression or enucleation. During the follow-up period, there were no recurrences. In conclusion, the use of conservative surgical treatment in ameloblastoma can be a reliable, safe, and successful method.
Keywords: Ameloblastoma, Enucleation, Decompression, Conservative treatment
I. Introduction
Ameloblastoma is a benign odontogenic tumor that often shows aggressive growth and has a high rate of recurrence1. It is an aggressive benign tumor of epithelial origin that may arise from the enamel, remnants of the dental lamina, the lining of odontogenic cysts, or possibly from the basal epithelial cells of the oral mucosa2. The treatment of ameloblastoma varies based on the clinical, histopathologic, and radiographic characteristics. Unicystic forms are thought to be less likely to recur; however, although a more conservative approach is recommended, it is seldom adopted in practice3. Typically, aggressive surgical treatments, such as marginal or segmental resection, have been implemented, but some conservative surgical methods are also being introduced, including decompression, enucleation, or curettage4,5. This case series show the potential for favorable healing without recurrence in ameloblastoma patients treated with conservative surgery.
II. Cases Report
1. Case 1
In 2015, a 24-year-old male was referred to our hospital for evaluation of gingival swelling in the mandibular left posterior region. The patient was a non-smoker and had no underlying disease. He had first noticed the lesion about one year prior. On extra-oral examination, facial asymmetry with swelling involving the left side of the mandible was observed at the time of admission. Intraoral examination showed a discharge of pus in the posterior region.
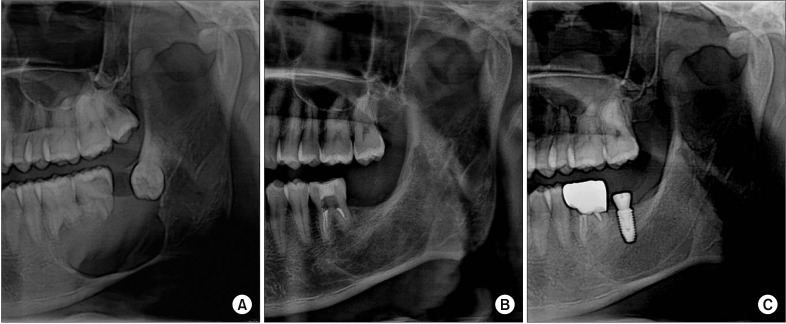
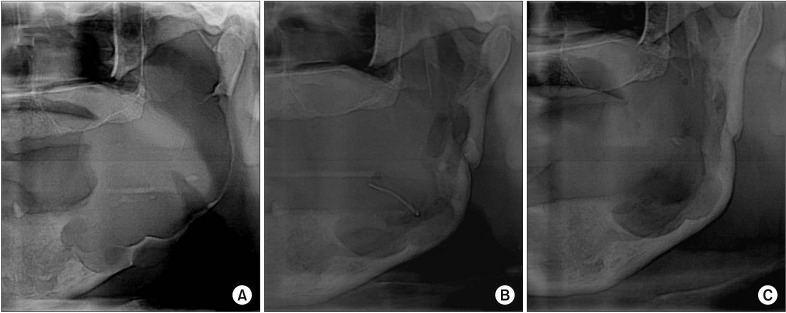
X-ray radiographs (panoramic radiograph and computed tomography [CT]) were performed.(Fig. 1. A) Axial CT showed a fairly large (27 mm×34 mm×23 mm) and well-defined rounded cystic destructive lesion involving the left mandibular body. Absorption of the roots of #36 and #37 had occurred. Incisional biopsy was performed under local anesthesia, and the tissue was sent for histopathological examination, which revealed a suggestive benign cyst. Endodontic treatment of #36 was performed.
Fig. 1. A. X-ray shows a fairly large, well-defined rounded cystic destructive lesion involving the left mandibular body. Absorption of the roots of #36 and #37 is also apparent. B. Nine months after surgery, a panoramic view reveals favorable healing of the grafted iliac bone without any inflammation. C. One year five months after surgery, an implant fixture was placed near the #37 area. A 5.0 mm×10.0 mm implant was used, and the insertion path was satisfactory.
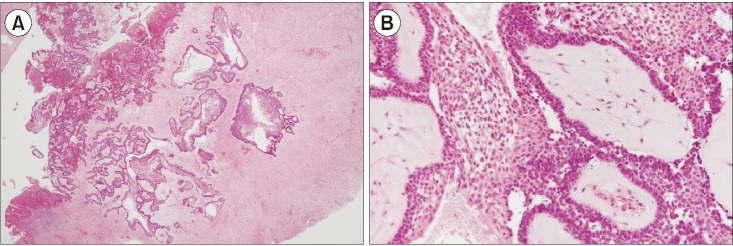
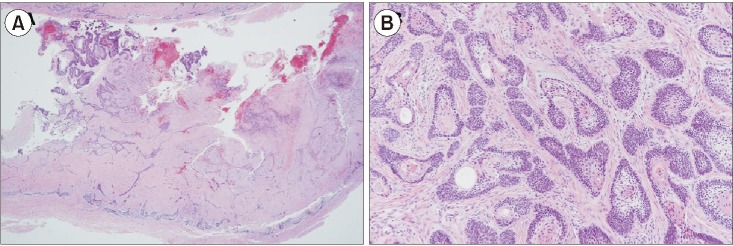
At the time of operation, extraction of #37 and #38 and enucleation of the lesion were carried out under general anesthesia. The iliac bone graft took place at the same time. After surgery, a newly excisional biopsy was performed, and the results did not show a benign cyst but instead were suggestive of unicystic ameloblastoma, mural type.(Fig. 2) A follow-up check was done at three months, six months, nine months, and one year after surgery. Nine months postoperatively, a panoramic radiograph revealed favorable healing of the iliac bone graft in the left mandibular body.(Fig. 1. B)
Fig. 2. Microscopic characteristics. A. Underlying the fibrous capsule, proliferation of neoplastic cells was noted; the cells were arranged in strands and in islands (H&E staining, ×20). B. Mural unicystic ameloblastoma shows invasive islands of the ameloblastic epithelium (H&E staining, ×100).
At one year and five months after surgery, implantation of #37 was performed. The implantation was done using a one-stage technique because the initial torque was favorable. (Fig. 1. C) Based on the results of the initial histopathological examination, cyst enucleation and an iliac bone graft were performed simultaneously in this patient. Usually in cases of ameloblastoma, a bone graft is not carried out at the same time due to the high recurrence rate. In this case, non-invasive cyst enucleation and the iliac bone graft were performed simultaneously, and the healing was satisfactory without any evidence of recurrence.
2. Case 2
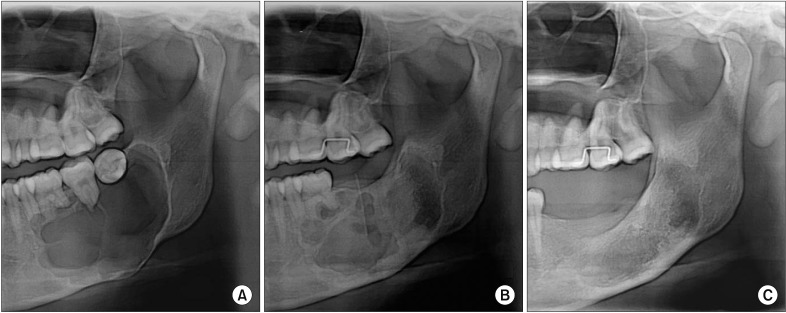
A 19-year-old female was referred to the dental hospital for further evaluation of a radiolucent lesion on the mandible. The patient was a non-smoker and had no underlying disease. A multi-ocular lesion was observed in the left mandibular body at the time of the visit. The panoramic view showed multiple root resorption near the posterior teeth and an inferiorly displaced inferior alveolar nerve canal.(Fig. 3. A) On extra-oral examination, facial asymmetry with swelling involving the left side of the mandible was noted. Bone expansion occurred at the left mandibular body and the inferior border of the mandible. An incisional biopsy was performed under local anesthesia, and the tissue was sent for histopathological examination, which resulted in a diagnosis of ameloblastoma.
Fig. 3. A. The panoramic view shows a large, round-shaped radiolucent lesion near the posterior teeth. B. Nine months later after decompression, the size of the lesion had decreased. C. One year after surgery, bone formation at the operative site was satisfactory.
Surgical enucleation or segmental mandibulectomy was regarded as inappropriate considering the patient's age and the size of the lesion. Extraction of #37 and #38 was performed under local anesthesia. Decompression was performed for nine months before surgery. A decreased size of the lesion was observed compared to the size at the initial visit.(Fig. 3. B)
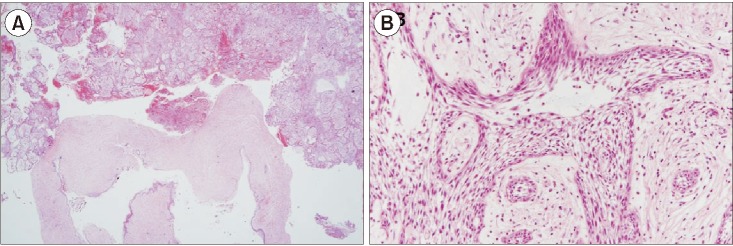
At the time of the operation, extraction of #35 and #36 and enucleation as a conservative surgery were performed, and removal of about 1 mm of bone near the lesion was also carried out. An excisional biopsy was performed, and the result revealed suggested unicystic ameloblastoma, mural type.(Fig. 4) One year after surgery, successful bone formation without any recurrence was observed.(Fig. 3. C)
Fig. 4. Microscopic characteristics. A. The tumor is composed of a partly cystic portion and a solid portion (H&E staining, ×20). B. The tumor contains anastomosing cords and strands. At the center of these anastomoses, the cells are loosely arranged and have a cystic appearance. Each cell is spindle-shaped and has hyperchromatic nuclei (H&E staining, ×100).
3. Case 3
A 63-year-old male was referred from a local dental clinic for evaluation of swelling on the left side of his face. He was currently taking hypertension medicine. At the time of the patient's visit, edema was observed on the left side of his face and was accompanied by swelling on the left anterior ramus. Panoramic x-ray showed an expansive radiolucent lesion on the left mandibular ramus.(Fig. 5. A) Aspiration produced approximately 60 mL of straw-colored clear fluid. To reduce the size of the lesion, decompression was performed. Six months after decompression, the size of the lesion had decreased, and an incisional biopsy on the left retromolar region was carried out. The tissue examination results revealed an ameloblastoma. Decompression was constantly performed for 1 year; in a panoramic x-ray to observe the patient's progress, it was confirmed that the size had been reduced.(Fig. 5. B) One year after decompression, excision for ameloblastoma was performed under general anesthesia to remove tissue around the inferior alveolar nerve and connected to the mylohyoid muscle. An excisional biopsy was also performed, and the results were suggestive of unicystic ameloblastoma, follicular type.(Fig. 6)
Fig. 5. A. The panoramic radiograph shows a fairly large, well-defined rounded destructive lesion involving the left mandibular body. B. One year after decompression, the panoramic x-ray reveals that the size of the lesion has decreased. C. Three months after surgery, bone formation has progressed well.
Fig. 6. Microscopic characteristics. A. The tumor is composed of a partly cystic portion and a solid portion (H&E staining, ×20). B. The tumor demonstrates a follicular pattern, which is composed of islands of odontogenic epithelium. The basal cells of these islands are column, hyperchromatic, and palisading. Their centers show squamous differentiation (H&E staining, ×100).
One month postoperatively, the site of surgery was healing well, and numbness was resolving.(Fig. 5. C) Four months after the operation, panoramic views indicated marked new bone formation without any sign of recurrence at the operation site.
III. Discussion
None of the three patients relapsed into ameloblastoma during the follow-up period. The incisional biopsy performed under local anesthesia for one of the patients revealed a benign cyst. Based on this result, cyst enucleation and iliac bone graft were simultaneously performed under general anesthesia. Although the final results of the biopsy indicated unicystic ameloblastoma, mural type, the grafted bone settled without complication and showed a low chance of relapse. While the treatment of ameloblastoma was not a typical one, this case showed that a conservative surgical approach was an appropriate treatment.
Radical surgery was also not required for the female patient who developed ameloblastoma on the left mandible in light of her young age. However, to reduce the size, eight months of decompression were required. A conservative approach was therefore effective. We confirmed a reduction in the lesion's size on a radiograph, and a conservative surgical approach was carried out under general anesthesia. This patient also did not relapse.
The recommended treatment for this subtype of ameloblastoma is still controversial because treatment methods are dependent on the subtype. The choice of treatment is based not only on the apparent microscopic pattern on biopsy, but also on the location, size of the lesion, and age of the patient. Solid and multicystic ameloblastoma can be treated with surgery. Due to its ability to infiltrate the bone, it is regarded as a locally aggressive tumor6,7. Conservative resection, such as curettage and enucleation, is associated with a high recurrence rate (solid and multicystic, 60%–80%; unicystic, 30%–60%)8.
In contrast, unicystic ameloblastoma is thought to be less aggressive than solid or multicystic ameloblastoma. In most unicystic ameloblastoma cases, clinical and radiographic findings suggest that the lesion is an odontogenic cyst. These tumors are usually treated as cysts by enucleation.
According to Marx and Stern9, ameloblastoma in situ that develops in and is limited to the epithelial lining of a cyst and also microinvasive ameloblastoma that arises from the epithelial lining and proliferates into the connective tissue layer of the cyst should be treated with enucleation. However, the invasive type of ameloblastoma should be treated with resection in case the tumor has penetrated through the connective tissue of the cyst.
If the ameloblastic elements are confined to the lumen of the cyst either with or without intraluminal tumor extension, then cyst enucleation may be an adequate treatment option. The patient, however, should receive long-term follow-up treatment7. In the literature, the recurrence of unicystic ameloblastoma after conservative treatment is reported to be between 10% and 25%10,11.
Because the rate of relapse is different for each treatment depending on the type of ameloblastoma, a clinical and radiological diagnosis must be made, and a biopsy is also necessary. However, as confirmed by numerous dissertations, since the relapse rate of unicystic ameloblastoma is relatively low compared to other types, conservative surgical treatment is the preferred method to avoid expansive losses that may occur with aggressive surgical treatment.
Footnotes
Authors' Contributions: S.W.K. participated in data collection and wrote the manuscript. Y.J.J., D.W.L., and H.K.K. participated in the study design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Nakamura N, Higuchi Y, Tashiro H, Ohishi M. Marsupialization of cystic ameloblastoma: a clinical and histopathologic study of the growth characteristics before and after marsupialization. J Oral Maxillofac Surg. 1995;53:748–754. doi: 10.1016/0278-2391(95)90323-2. discussion 755-6. [DOI] [PubMed] [Google Scholar]
- 2.Ghandhi D, Ayoub AF, Pogrel MA, MacDonald G, Brocklebank LM, Moos KF. Ameloblastoma: a surgeon’s dilemma. J Oral Maxillofac Surg. 2006;64:1010–1014. doi: 10.1016/j.joms.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 3.Haq J, Siddiqui S, McGurk M. Argument for the conservative management of mandibular ameloblastomas. Br J Oral Maxillofac Surg. 2016;54:1001–1005. doi: 10.1016/j.bjoms.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 4.Kumar V. Conservative surgical approach to aggressive benign odontogenic neoplasm: a report of three cases. J Korean Assoc Oral Maxillofac Surg. 2015;41:37–42. doi: 10.5125/jkaoms.2015.41.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borrello R, Bettio E, Bacci C, Valente M, Sivolella S, Mazzoleni S, et al. A conservative approach to a peripheral ameloblastoma. Case Rep Dent. 2016;2016:8254571. doi: 10.1155/2016/8254571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chae MP, Smoll NR, Hunter-Smith DJ, Rozen WM. Establishing the natural history and growth rate of ameloblastoma with implications for management: systematic review and meta-analysis. PLoS One. 2015;10:e0117241. doi: 10.1371/journal.pone.0117241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pogrel MA, Montes DM. Is there a role for enucleation in the management of ameloblastoma? Int J Oral Maxillofac Surg. 2009;38:807–812. doi: 10.1016/j.ijom.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 8.Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:660–669. doi: 10.1016/s1079-2104(96)80441-0. [DOI] [PubMed] [Google Scholar]
- 9.Marx RE, Stern D. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. Chicago: Quintessence; 2003. [Google Scholar]
- 10.Garcia NG, Oliveira DT, Rodrigues MT. Unicystic ameloblastoma with mural proliferation managed by conservative treatment. Case Rep Pathol. 2016;2016:3089540. doi: 10.1155/2016/3089540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiran KRK, George GB, Padiyath S, Rupak S. [Mural unicystic ameloblastoma crossing the midline: a rare case report] Int J Odontostomat. 2012;6:97–103. Spanish. [Google Scholar]