Abstract
Background
Hypertension contributes substantially to chronic disease and mortality. Mineral intakes can modify blood pressure.
Objective
Individual minerals and their intake ratios in US adults and their association with blood pressure were examined.
Methods
Regression models were used to examine the associations of sodium, potassium, and calcium intakes and their ratios from food and supplements with blood pressure in 8777 US adults without impaired renal function from the 2011–2014 NHANES. We evaluated men (n = 4395) and women (n = 4382) separately. Models for predicting blood pressure were developed using age, blood pressure medication, race, body mass index (BMI), and smoking as explanatory variables.
Results
Few adults met the recommended intake ratios for sodium:potassium (1.2% and 1.5%), sodium:calcium (12.8% and 17.67%), and sodium:magnesium (13.7% and 7.3%) for men and women, respectively. Approximately half of adults (55.2% of men and 54.8% of women) met calcium:magnesium intake ratio recommendations. In our regression models, the factors that explained the largest amount of variability in blood pressure were age, blood pressure medication, race/ethnicity, BMI, and smoking status. Together, these factors explained 31% and 15% of the variability in systolic blood pressure in women and men, respectively. The sodium:potassium (men and women), sodium:magnesium (women), and sodium:calcium (men) intake ratios were positively associated with systolic blood pressure, whereas calcium intake was inversely associated with systolic blood pressure in men only. When mineral intake ratios were added individually to our regression models, they improved the percentage of variability in blood pressure explained by the model by 0.13–0.21%.
Conclusions
Strategies to lower blood pressure are needed. Lower sodium:potassium intake ratios provide a small benefit for protection against hypertension in US adults.
Keywords: blood pressure, sodium, potassium, calcium, magnesium
Introduction
Cardiovascular disease was the most common underlying cause of death worldwide in 2013, accounting for nearly one-third of all deaths (1). According to the most recent report from the American Heart Association, >1 in 3 American adults have ≥1 type of cardiovascular disease and 34% of American adults have hypertension (1). This same report emphasizes nutrition and diet quality as one of the health behaviors to focus on for improving cardiovascular health.
Higher intakes of potassium, calcium, and magnesium and lower intakes of sodium have been associated with a lower risk of hypertension and cardiovascular disease (2–4). The ratio of sodium to potassium intake was more strongly and consistently associated with cardiovascular disease and all-cause mortality than either single nutrient in a prospective analysis of a representative sample of US adults from NHANES III (4). Dietary patterns emphasizing fruits, vegetables, and dairy are rich in minerals, tend to be lower in sodium, and are known to reduce blood pressure (BP) (5). However, to our knowledge, a rigorous evaluation of other minerals and mineral ratios and their respective roles in BP has not been conducted.
Previously, we reported sodium and potassium intakes and their ratio in US adults from the 2011–2012 NHANES (6). Only ∼10% of US adults met the sodium:potassium intake ratio associated with a reduced risk of cardiovascular mortality (1.0) (4). Most adults (90% ± 0.8%) consumed >2300 mg Na/d, primarily from mixed dishes, protein foods, and grains, and <3% had potassium intakes >4700 mg/d, primarily from vegetables and dairy. Furthermore, a recent analysis of the 2009–2012 NHANES showed that a substantial portion of US adults consumed less than the Estimated Average Requirement for calcium (19.6% ± 1.3%) and magnesium (22.3% ± 1.6%) from food and supplements combined (7). Thus, most Americans have mineral intakes that are not aligned with dietary guidelines. Given the relation between intakes of each of these minerals and cardiovascular disease, the combined effect of high sodium intake and inadequate intake of potassium, calcium, and magnesium is of particular concern.
Examining the effects of multiple mineral intakes and their ratios on the risk of cardiovascular disease is important for developing dietary guidelines beyond a simplistic focus on sodium reduction. Our aim was to examine the associations of sodium, potassium, calcium, and magnesium intakes from food and dietary supplements, as well as their intake ratios, with BP.
Methods
The NHANES is a nationally representative, cross-sectional health examination survey that samples noninstitutionalized, civilian US residents using a complex, stratified, multistage probability cluster sampling design. The NHANES is planned and conducted by the US CDC, National Center for Health Statistics. Written informed consent for all participants was obtained (8). The NHANES protocol was approved by the National Center for Health Statistics research ethics review board. Data were collected through an in-home interview and a visit to a mobile examination center.
This analysis was completed with the use of 2 data cycles from NHANES 2011–2012 and 2013–2014 because the National Center for Health Statistics recommends that analysts combine ≥4 y of data to improve the reliability and stability of statistical estimates (9). The inclusion criteria for this analysis were men and women aged ≥20 y, who were not pregnant or lactating, and with complete and plausible data. We excluded participants with an estimated glomerular filtration rate <30 mL/min because impaired kidney function is related to BP independently of diet. The final analytical sample size was 8777. Demographic data in NHANES are collected with a computer-assisted personal interview in the participants’ home, including sex, age, and race/ethnicity. The self-identified race/ethnic groups are classified by NHANES as non-Hispanic white, non-Hispanic black, Hispanic and Mexican American, non-Hispanic Asian, and “other” (referred to hereafter as white, black, Hispanic, and Asian). Estimates of the “other” race category are not presented separately in this analysis per the National Center for Health Statistics analytical guidelines. Self-reported tobacco smoking was categorized as “yes” or “no” based on current usage obtained from questionnaire data.
Brachial systolic and diastolic BP (SBP and DBP, respectively) readings were measured by a trained and certified physician in the mobile examination center after the participant had rested quietly in a seated position for 5 min (10). Three consecutive blood pressure readings were obtained. If a BP measurement was interrupted or incomplete, a fourth attempt may be made. Hypertension was classified as an SBP of >130 mm Hg or a DBP of >80 mm Hg (11). Because the distributions of SBP and DBP were strongly skewed, all of the analyses were performed by using logs of these variables. Extreme values beyond the 1st and 99th percentiles were Winsorized (replaced by the 1st and 99th percentile, respectively). Measured height and weight, collected in the mobile examination center, were used to calculate BMI (in kg/m2), which was treated as a continuous variable.
Dietary data in NHANES are collected as part of the What We Eat in America survey (12) through two 24-h dietary recalls using the USDA’s Automated Multiple-Pass Method (13, 14). The dietary recall captures all foods, beverages, and dietary supplements consumed within the previous 24 h. We used only day-1 data because this was collected in the mobile examination center at the same time concurrent BP readings were recorded, and our primary aim was to assess recent mineral intakes relative to BP. The usual intake of the same population showed a similar prevalence of mineral intakes as in our previous study, which used 2 time points of intake (6), giving us confidence in our use of a single time point for diet assessment. We prioritized a close temporal diet assessment to BP because steady state to a shift in sodium intake occurs rapidly within 2–4 d (15). The second diet recall assessment in NHANES can occur 3–10 d after BP is measured. Comprehensive information on the use of all types of prescription and nonprescription dietary supplements was first collected during the household interview; detailed collection procedures have been described elsewhere (16–18). Briefly, trained interviewers asked participants to provide supplement product containers if they were available; containers were seen for >80% of the reported supplements. Information about product type, name, frequency and duration of use, and dosage was recorded for each supplement reported during the interview. During the 24-h recall, trained interviewers asked participants if they used the products reported in the home and collect detailed information on any new products added since the home interview.
The USDA Food and Nutrient Database for Dietary Studies was used to convert foods and beverages as reported into gram amounts and to determine their respective energy and nutrient contents (12). The National Center for Health Statistics provided the average daily intake of nutrients from all dietary supplements as calculated for individuals by using the number of days supplement use was reported, the reported amount taken per day, and the serving size unit from the product label. Nutrient contents from foods, beverages, and dietary supplements were combined and estimated for sodium, potassium, magnesium, and calcium, as well as the mineral ratios of sodium:potassium, sodium:calcium, sodium:magnesium, and calcium:magnesium.
The targeted values for those ratios were based on DRIs outlined by the Food and Nutrition Board of the National Academies of Sciences, Engineering, and Medicine (i.e., 2300 mg Na/d, 4700 mg K/d, 1000 mg Ca/d for women aged 19–50 y and men aged 19–70 y, 310 mg Mg/d for women aged 19–30 y and 400 mg/d for men aged 19–30 y) (19–21). The Automated Multiple-Pass Method methodology used for the 24-h dietary recall has been validated for sodium. Reporting accuracy, calculated as the ratio of reported sodium intake to that estimated from the urinary biomarker, was 0.93 (95% CI: 0.89, 0.97) for men and 0.90 (95% CI: 0.87, 0.94) for women, on average (22). Recovery biomarkers do not exist to estimate the magnitude of misreporting for calcium and magnesium.
All statistical analyses were performed using Statistical Analysis Software (version 9.4; SAS Institute, Inc.) and Statistical Analysis Software-callable Sudan software (version 11.0; RTI International). NHANES sample weights were used to account for differential nonresponse or noncoverage to adjust for planned oversampling of some groups and to adjust the dietary data for uneven representation of days of the week. Because intakes of sodium, potassium, calcium, and magnesium were strongly skewed to the right, all of the analyses were performed using logs of these variables and their ratios.
Extreme outliers of mineral intake of dietary supplement users were Winsorized to reduce their influence. Regression models were used to examine the association of individual minerals and their ratios with SBP, DBP, and hypertension controlled for known covariates. Significance was set at P ≤ 0.05, except for the race comparison, which was set at P < 0.005 to adjust for the 10 comparisons.
Parallel analyses were performed for SBP and DBP. A model for assessing BP was developed using the following explanatory variables: age, expressed as linear and quadratic terms; a binary indicator of BP medication usage; interactions of age variables with BP medication usage; race; BMI; and a binary indicator of current smoking. Effects of individual mineral intakes and their ratios were assessed by adding each of these terms to the basic model. Subsets of these mineral variables were also examined.
Results
Mineral intakes
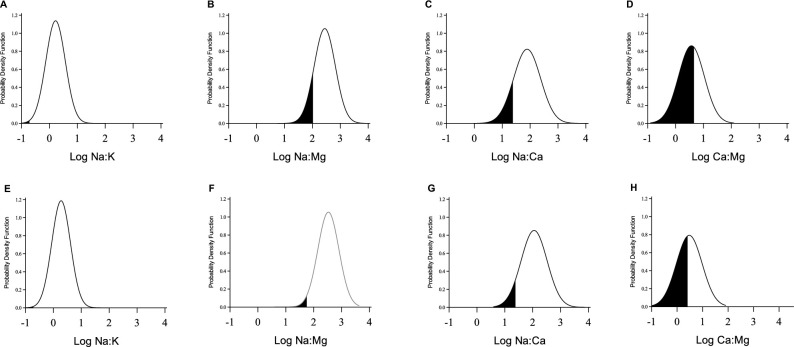
Subject characteristics for the analytical sample of 4395 men and 4382 women meeting our eligibility criteria are given in Table 1. Usual intakes of sodium, potassium, calcium, and magnesium by sex and selected characteristics are shown in Table 2. Sodium intakes were >2300 mg/d for most Americans. Usual intakes were below recommendations for potassium, calcium, and magnesium. Although intake represents the total intake from all foods, beverages, and supplements for all 4 minerals, dietary supplements do not contribute substantially to sodium or potassium intakes, so intake of these minerals will mainly come from foods and beverages. Mineral intake ratio distributions relative to calculated ratios from DRIs for individual minerals for men and women are shown in Figure 1. Less than 2% of Americans achieved recommended intake ratios for sodium:potassium, and <16% consumed recommended intakes for sodium:calcium. Sex differences were observed with other mineral intake ratios. For women, ∼7% achieved recommended intake ratios compared with men, at 14%, for sodium:magnesium. For women, approximately one-third compared with more than half of men met recommended intakes for calcium:magnesium.
TABLE 1.
Participant characteristics in US adults by sex: NHANES 2011–20141
| Men | Women | |
|---|---|---|
| Characteristic | (n = 4395) | (n = 4382) |
| Age, y | 45.9 ± 0.5 | 47.7 ± 0.5 |
| BMI, kg/m2 | 28.7 ± 0.1 | 29.2 ± 0.2 |
| Race/ethnicity, % | ||
| Non-Hispanic white | 68 | 68 |
| Non-Hispanic black | 10 | 11 |
| Hispanic | 15 | 14 |
| Non-Hispanic Asian | 4 | 5 |
| Current smoker, % | ||
| Yes | 21 | 17 |
| No | 79 | 83 |
| Taking blood pressure medication, % | ||
| Yes | 25 | 27 |
| No | 75 | 73 |
| Blood pressure, mm Hg | ||
| Systolic | 123 ± 0.4 | 120 ± 0.4 |
| Diastolic | 72 ± 0.3 | 70 ± 0.3 |
| Hypertension (systolic blood pressure >130 mm Hg or diastolic blood pressure >80 mm Hg), % | 35 | 29 |
1Values are means ± SEs unless otherwise stated.
TABLE 2.
Estimated intakes of sodium, potassium, calcium, and magnesium in US adults by sex: NHANES 2011–20141
| Intakes, mg/d | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample | Sodium | Potassium | Calcium | Magnesium | ||||||
| Characteristic | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women |
| Total sample, n | 4395 | 4382 | 4194 ± 34 | 3018 ± 23 | 3105 ± 32 | 2371 ± 27 | 1186 ± 16 | 1070 ± 14 | 370 ± 4 | 296 ± 3 |
| Race/ethnicity, % | ||||||||||
| Non-Hispanic white | 68 | 68 | 4189 ± 40 | 2967 ± 30 | 3116 ± 42 | 2403 ± 39 | 1234 ± 19 | 1135 ± 18 | 377 ± 6 | 303 ± 5 |
| Non-Hispanic black | 10 | 11 | 4077 ± 85 | 3112 ± 58 | 2792 ± 48 | 2176 ± 36 | 981 ± 25 | 857 ± 19 | 329 ± 8 | 263 ± 4 |
| Hispanic | 15 | 14 | 4325 ± 78 | 3092 ± 54 | 3144 ± 48 | 2391 ± 41 | 1186 ± 29 | 1013 ± 17 | 373 ± 7 | 288 ± 5 |
| Non-Hispanic Asian | 4 | 5 | 4212 ± 126 | 3366 ± 92 | 2949 ± 61 | 2361 ± 37 | 914 ± 27 | 875 ± 26 | 372 ± 9 | 301 ± 7 |
| Racial differences2 | No differences | A > W | H,W > A,B | W,H,A > B | W,H > B,A | W > H > A,B | W,H,A > B | W,A,H > B | ||
| Hypertension (130/80 mm Hg), % | 35 | 29 | 4058 ± 46 | 2928 ± 52 | 3030 ± 41 | 2337 ± 42 | 1126 ± 19 | 1104 ± 28 | 360 ± 6 | 263 ± 6 |
| No hypertension, % | 65 | 71 | 4267 ± 37 | 3055 ± 27 | 3145 ± 33 | 2385 ± 25 | 1218 ± 18 | 1056 ± 16 | 375 ± 5 | 297 ± 3 |
| Hypertension difference3 | No HTN > HTN | No HTN > HTN | nd | nd | No HTN > HTN | nd | No HTN > HTN | nd | ||
1Values are means ± SEs and population percentages presented by sex of estimated usual intakes of sodium, potassium, calcium, and magnesium. A, Asian; B, black; H, Hispanic; HTN, hypertension; nd, no difference; W, white.
2There were 10 comparisons. The adjusted P-value requirement for each comparison is 0.005.
cHypertension is defined as systolic blood pressure >130 mm Hg or diastolic blood pressure >80 mm Hg. “No HTN > HTN” indicates that individuals who did not have hypertension had significantly higher intakes than individuals who did have hypertension.
FIGURE 1.
Sodium:potassium (A, E), sodium:magnesium (B,F), sodium:calcium (C, G), and calcium:magnesium (D, H) intake ratios in US women (A-D) and men (E-H). Shaded areas indicate those achieving recommended intake ratios.
The variability in mineral intakes and mineral intake ratios that was explained after adjusting for sex, age, BP medication, interaction of age and BP medication, race/ethnicity, BMI, and current smoking status ranged from 5% for calcium, sodium:calcium, and calcium:magnesium to 14% for sodium. Men had higher intakes of all minerals and higher intake ratios of sodium:potassium, sodium:magnesium, and sodium:calcium, but not of calcium:magnesium, compared with women (P < 0.0001). Age was a significant factor (P < 0.0001) of sodium, potassium, and magnesium intakes as well as the intake ratios of sodium:potassium, sodium:magnesium, and calcium:magnesium. Among both sexes, blacks consumed less sodium, potassium, and magnesium than other racial/ethnic groups. The sodium:potassium intake ratio was greater for blacks and Asians than Hispanics or whites. The order of calcium intake by race was white > Hispanic > Asian and black.
BP
Many factors beyond diet were strongly associated with BP (Table 3). Age explained 26% of the variation in SBP for women and only 10% for men. The addition of BP medication and its interaction term with age, race/ethnicity, BMI, and smoking status explained an additional 5% for women (R2 = 0.31) and men (R2 = 0.16). For DBP, age explained 8% of the variation for women and 12% for men. The addition of BP medication and its interaction with age, race/ethnicity, BMI, and smoking status explained a total of 11% of the variation in women (R2 = 0.11) compared with 14% in men (R2 = 0.14). Figure 2 shows how BP varies with age and BP medication usage. BP was higher for those who use BP medication and the difference decreases with age.
TABLE 3.
Predictors of SBP in the US NHANES 2011–20141
| log(SBP) | log(DBP) | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | β estimate | SE | P | Racial difference | β estimate | SE | P | Racial difference |
| Women (n = 4382) | ||||||||
| Intercept | 4.64 | 4.35 | ||||||
| Age, y | 0.003 | 0.000223 | <0.0001 | 0.0026 | 0.000273 | <0.0001 | ||
| Age-squared | 0.00004 | 0.000012 | 0.0023 | −0.00011 | 0.000012 | <0.0001 | ||
| BP medication | ||||||||
| No | −0.11 | 0.029628 | 0.0010 | −0.25 | 0.042142 | <0.0001 | ||
| Yes | 0 | 0 | 0 | 0 | ||||
| Age by BP medication | −0.0016 | 0.000634 | 0.0154 | −0.0048 | 0.000907 | <0.0001 | ||
| Age-square by BP medication | 0.000031 | 0.000019 | 0.1045 | 0.000058 | 0.000022 | 0.0147 | ||
| Race/ethnicity2 | <0.0001 | B > A,H,W | <0.0001 | A,B,W > H | ||||
| Asian | 0.0083 | 0.007010 | 0.0051 | 0.008509 | ||||
| Black | 0.033 | 0.005772 | −0.0039 | 0.008644 | ||||
| Hispanic | −0.00015 | 0.005343 | −0.031 | 0.008321 | ||||
| Other | 0.012 | 0.013597 | −0.029 | 0.018877 | ||||
| White | 0 | 0 | 0 | 0 | ||||
| BMI | 0.0027 | 0.000368 | <0.0001 | 0.0018 | 0.000318 | <0.0001 | ||
| Smoker | ||||||||
| No | −0.0074 | 0.004666 | 0.1218 | 0.017 | 0.006426 | 0.0114 | ||
| Yes | 0 | 0 | 0 | 0 | ||||
| Men (n = 4395) | ||||||||
| Intercept | 4.72 | 4.20 | ||||||
| Age, y | 0.0018 | 0.000193 | <0.0001 | 0.0032 | 0.000224 | <0.0001 | ||
| Age-squared | 0.000044 | 0.000009 | <0.0001 | −0.00015 | 0.000011 | <0.0001 | ||
| BP medication | ||||||||
| No | −0.10 | 0.033611 | 0.0048 | −0.13 | 0.060934 | 0.0347 | ||
| Yes | 0 | 0 | 0 | 0 | ||||
| Age by BP medication | −0.0019 | 0.000716 | 0.0112 | −0.0029 | 0.001254 | 0.0262 | ||
| Age-squared by BP medication | 0.000012 | 0.000020 | 0.5424 | 0.000027 | 0.000030 | 0.3852 | ||
| Race/ethnicity2 | <0.0001 | B > A,H,W | 0.0001 | A > H,W | ||||
| Asian | 0.015 | 0.005660 | 0.027 | 0.007614 | ||||
| Black | 0.042 | 0.005344 | 0.0046 | 0.009244 | ||||
| Hispanic | 0.0027 | 0.004171 | −0.022 | 0.009696 | ||||
| Other | 0.025 | 0.012920 | −0.0062 | 0.017611 | ||||
| White | 0 | 0 | 0 | 0 | ||||
| BMI | 0.0035 | 0.000403 | <0.0001 | 0.0036 | 0.000462 | <0.0001 | ||
| Smoker | ||||||||
| No | −0.015 | 0.005271 | 0.0095 | 0.012 | 0.006155 | 0.0693 | ||
| Yes | 0 | 0 | 0 | 0 | ||||
1A, Asian; B, black; BP, blood pressure; DBP, diastolic blood pressure; H, Hispanic; SBP, systolic blood pressure; W, white.
2There were 10 comparisons. The adjusted P-value requirement for each comparison was 0.005.
FIGURE 2.
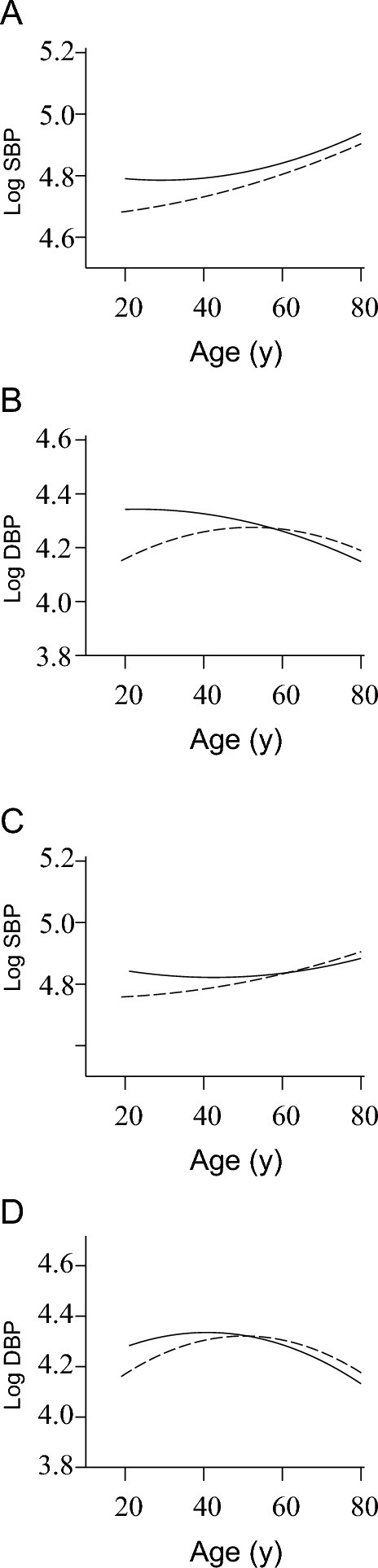
Variations in SBP (A, C) and DBP (B, D) in US women (A, B) and men (C, D) with age, blood pressure medication usage, and their interaction. The solid lines indicate those taking blood pressure medication, and the dashed lines indicate those who are not taking blood pressure medication. DBP, diastolic blood pressure; SBP, systolic blood pressure.
When added to these models, intakes of minerals or their ratios entered individually explained <1% of the variation for SBP. Final models for SBP resulted in R2 of 0.31 for women and 0.15 for men (Table 4). Significant positive relations were found for SBP with sodium:potassium (P < 0.01) and sodium:magnesium (P < 0.02) in women and with sodium:potassium (P < 0.02), sodium:calcium (P = 0.001), and calcium alone (P = 0.001, inverse) in men. Models that included combinations of single minerals or their ratios slightly improved the amount of variability in SBP accounted for in women (R2 = 0.31). For men, adding all single mineral intakes to the model resulted in a slightly better model of SBP (R2 = 0.16) than by including minerals or mineral ratios one at a time in the model. Final models for DBP resulted in an R2 of 0.11 for women and 0.14 for men (Table 4). Models that included combinations of single minerals or their ratios made little difference in the model for DBP for women (R2 = 0.11) and men (R2 = 0.15).
TABLE 4.
Dietary-mineral predictors of SBP and DBP in the US NHANES 2011–20141
| Women log(SBP) | Women log(DBP) | Men log(SBP) | Men log(DBP) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β estimate | P | R 2 | β estimate | P | R 2 | β estimate | P | R 2 | β estimate | P | R 2 | |
| Model from Table 3 | 0.31 | 0.11 | 0.15 | 0.14 | ||||||||
| Mineral intake (log) | ||||||||||||
| Sodium | 0.0054 | 0.13 | 0.31 | 0.00052 | 0.92 | 0.11 | 0.00043 | 0.90 | 0.15 | 0.0075 | 0.29 | 0.14 |
| Potassium | −0.0063 | 0.14 | 0.31 | −0.0048 | 0.33 | 0.11 | −0.0063 | 0.08 | 0.15 | 0.0062 | 0.41 | 0.14 |
| Calcium | −0.00099 | 0.80 | 0.31 | 0.004 | 0.30 | 0.11 | −0.0082 | 0.001 | 0.15 | −0.0016 | 0.71 | 0.14 |
| Magnesium | −0.0061 | 0.16 | 0.31 | −0.0051 | 0.27 | 0.11 | −0.003 | 0.29 | 0.15 | −0.002 | 0.80 | 0.14 |
| Mineral intake ratios (log) | ||||||||||||
| Sodium:potassium | 0.014 | 0.01 | 0.31 | 0.006 | 0.30 | 0.11 | 0.011 | 0.01 | 0.15 | 0.0041 | 0.57 | 0.14 |
| Sodium:calcium | 0.0045 | 0.28 | 0.31 | 0.00079 | 0.89 | 0.11 | 0.01 | 0.001 | 0.15 | 0.004 | 0.45 | 0.14 |
| Sodium:magnesium | 0.011 | 0.02 | 0.31 | 0.0063 | 0.27 | 0.11 | 0.0065 | 0.09 | 0.15 | 0.0081 | 0.30 | 0.14 |
| Calcium:magnesium | 0.0043 | 0.35 | 0.31 | 0.0046 | 0.36 | 0.11 | −0.0064 | 0.08 | 0.15 | 0.0023 | 0.70 | 0.14 |
1Values were adjusted for age, age-squared, blood pressure medication, interactions of age and age-squared with blood pressure medication, race, BMI, and smoking. DBP, diastolic blood pressure; SBP, systolic blood pressure.
With the use of logistic regression models to predict the incidence of hypertension (SBP >130 or DBP >80 mm Hg), calcium intake was inversely associated with hypertension in men only after adjusting for age, BP medication, race/ethnicity, BMI, and smoking status (estimate of β = −0.1337, P = 0.03).
Discussion
In this cohort of a nationally representative sample of US adults, we observed that age and race/ethnicity explained most of the variation in BP. The intake ratios of sodium:potassium, but not sodium and potassium added individually, contributed weakly but significantly to models for SBP but not DBP. If potassium is increased from the average intake of 2371 mg/d to the recommended intake of 4700 mg/d, and sodium intake is decreased from the average of 3018 mg/d to 1500 mg/d, SBP is predicted to decrease from the averages of 119 mm Hg to 117 mm Hg. In addition, calcium intake alone was inversely associated and the intake ratio of sodium:calcium was positively associated with SBP in men. Although the variation explained appears to be quite small, on the population level this may have meaningful implications. Even small reductions in BP have large health benefits (23).
Meta-analyses of randomized controlled trials have consistently identified a positive relation between sodium reduction and BP (24, 25). The evidence for a relation between adequate potassium and BP reduction was considered moderate by the 2010 Dietary Guidelines for Americans Advisory Committee on the basis of 36 clinical trials and 17 cohort studies evaluated from the 2005 committee plus an additional 10 new studies (26). In a Cochrane review of 13 randomized controlled trials, the relation between calcium supplementation and BP was considered weak due to poor quality of the evidence (27).
Dietary pattern interventions, notably the Dietary Approaches to Stop Hypertension (DASH) trials, have considered that reduction in BP may be due to foods rich in potassium, calcium, and magnesium, with further reductions in BP with reduction in sodium intakes (5, 28). However, effects of intakes of these combined nutrients have been less rigorously studied. Considering multiple nutrients (i.e., potassium, calcium, and magnesium) is important for understanding the effect of diet quality on BP because they may modify the response to dietary sodium. High dietary sodium intakes can alter mineral excretion by increasing intravascular volume. An increase in urinary calcium was associated with increased SBP in 2 large cohorts: the International Study of Macro- and Micronutrients in Blood Pressure (INTERMAP) and the International Cooperative Study on Salt, Other Factors, and Blood Pressure (29). An older Cochrane review of randomized controlled trials did evaluate the effect of mineral ratios on BP and reported no significant effects, but the randomized controlled trials were few and not of high quality (30). In the Nurses’ Health Study II, potassium supplementation, but not calcium or magnesium supplementation, was effective at lowering BP after 16 wk and combined supplements were not better than potassium alone (31). Several epidemiologic studies have considered the combined effects of sodium and potassium intakes only on BP. Consistent with our findings, using urinary excretion rates as a biomarker for sodium intakes, a lower sodium to potassium intake ratio showed a stronger relation with lower BP than either nutrient alone (32, 33). More recently in Shandong and Jiangsu, China, in adults, increased sodium intakes, sodium-to-potassium intake ratio, and reduced potassium intakes were associated with higher BP (34). Considering additional minerals or their ratios together had minor contributions for explaining the variance in BP by sodium:potassium alone in our study. In the INTERMAP Study in 17 populations, a recent evaluation of contributing nutrients to BP showed that 24-h sodium and sodium:potassium excretions in multiple-variant analysis significantly predicted BP, but 80 other dietary variables did not attenuate the relation (35). Because mineral intakes tend to be highly correlated, their separate effects are not easily distinguished.
Strengths of this study include the use of a nationally representative cohort of adults. The sampling period of 2011–2014 from NHANES included a large sample of Asians for the first time. We examined 4 key minerals important to reducing the risk of high BP and their intake ratios, including from food and dietary supplements.
This study also has limitations. We chose to use a single 24-h dietary recall taken at the time of outcome measure assessment, which does not allow determination of individual variation. Self-reported sodium intake is much less reliable than 24-h urinary sodium and reporting accuracy is less for women than for men (22). This cross-sectional analysis precludes effects that may occur over time. When compared with 24-h urinary sodium excretion, USDA's Automated Multiple-Pass Method is accurate for assessing sodium intake in normal-weight individuals but is less accurate in obese individuals. The Automated Multiple-Pass Method recall underestimated intake by >20% in obese individuals (22). The finding that few adults met the recommended intake ratios reduced the range of mineral intake ratios, potentially limiting the true strength of a relation between mineral intake ratios and BP. We cannot rule out the possibility of reverse causality for the contribution of BP medications in our models.
In summary, we found very small benefits of lower intake ratios of sodium:potassium, sodium:magnesium, and sodium:calcium for protection against hypertension. Considering intakes of multiple nutrients as a predictor of diet quality will likely inform risks of chronic disease more than single-nutrient evaluations. More controlled feeding studies are needed to better help us understand how minerals modulate BP.
Acknowledgments
The authors’ responsibilities were as follows—CMW and GPM: had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis; CMW, RLB, and GPM: conceived and designed the study; CMW and RLB: drafted the manuscript; LDM and GPM: performed the statistical analysis; CMW, RLB, LDM, AJM, DGR, JDG, AJL, and GPM: acquired, analyzed, or interpreted the data and critically revised the manuscript for important intellectual content; and all authors: read and approved the final manuscript.
Notes
Preliminary findings were previously presented at the International Union of Nutritional Sciences 21st International Congress of Nutrition, 15–20 October 2017, in Buenos Aires.
Supported by International Life Sciences Institute–North America and National Heart, Lung, and Blood Institute U01HL128834.
The funders had no role in the conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Author disclosures: RLB, LDM, AJM, DGR, JDG, AJL, and GPM, no conflicts of interest. CMW is on the Board of the International Life Sciences Institute.
Abbreviations used: BP, blood pressure: DBP, diastolic blood pressure; SBP, systolic blood pressure.
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C et al. Heart disease and stroke status—2017 update: a report from the American Heart Association. Circulation 2017; 135:e146–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kass L, Weekes J, Carpenter L. Effect of magnesium supplementation on blood pressure: a meta-analysis. Eur J Clin Nutr 2012;66:412–8. [DOI] [PubMed] [Google Scholar]
- 3. Zhang X, Li Y, Del Gobbo LC, Rosanoff A, Wang J, Zhang W, Song Y. Effects of magnesium supplementation on blood pressure: a meta-analysis of randomized double-blind placebo-controlled trials. Hypertension 2016;68:324–33. [DOI] [PubMed] [Google Scholar]
- 4. Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang M-H, Gwinn M, Dowling N, Khoury MJ, Hu FB. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2011;171:1183–91. [DOI] [PubMed] [Google Scholar]
- 5. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 6. Bailey RL, Parker EA, Rhodes DG, Goldman JD, Clemens JC, Moshfegh AJ, Thuppal SV, Weaver CM. Estimating sodium and potassium intakes and their ratio in the American diet: data from the 2011–2012 NHANES. J Nutr 2016;146:745–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blumberg JB, Frei BB, Fulgoni VL, Weaver CM, Zeisel SH. Impact of frequency of multi-vitamin/multi-mineral supplement intake on nutritional adequacy and nutrient deficiencies in U.S. adults. Nutrients 2017;9:849–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Center for Health Statistics. About the National Health and Nutrition Examination Survey [Internet]. Hyattsville (MD): CDC; 2009[cited 2008 Aug 17]. Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm. [Google Scholar]
- 9. Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital Health Stat 2 2013;161:1–24. [PubMed] [Google Scholar]
- 10. National Center for Health Statistics National Health and Nutrition Examination Survey 2011–2012 data documentation, codebook, and frequencies: blood pressure. Hyattsville (MD): National Center for Health Statistics; 2012. [cited 2017 Nov 20]. Available from: https://wwwn.cdc.gov/nchs/nhanes/2011-2012/BPX_G.htm. [Google Scholar]
- 11. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71(6):e13–e115. [DOI] [PubMed] [Google Scholar]
- 12.USDA, Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies 2011–2012. Food Surveys Research Group Home Page; 2014[Internet]. [cited 2015 Jun 1]. Available from: http://www.ars.usda.gov/nea/bhnrc/fsrg. [Google Scholar]
- 13. Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr 2006;136(10):2594–9. [DOI] [PubMed] [Google Scholar]
- 14. Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA et al. The USDA automated multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008; 88:324–32. [DOI] [PubMed] [Google Scholar]
- 15. Palacios C, Wigertz K, Martin BR, Jackman L, Pratt JH, Peacock M, McCabe G, Weaver CM. Sodium retention in black and white female adolescents in response to salt intake. J Clin Endocrin Metab 2004; 89(4):1858–63. [DOI] [PubMed] [Google Scholar]
- 16. Bailey RL, Gahche JJ, Miller PE, Thomas PR, Dwyer JT. Why US adults use dietary supplements. JAMA Intern Med 2013;173(5):355–61. [DOI] [PubMed] [Google Scholar]
- 17. National Center for Health Statistics , National Health and Nutrition Examination Survey 2011-2012. Data documentation, codebook, and frequencies dietary supplement use 30-day. Hyattsville (MD): National Center for Health Statistics; 2014. [Google Scholar]
- 18. National Center for Health Statistics National Health and Nutrition Examination Survey 2013–2014. Data documentation, codebook, and frequencies dietary supplement use 30-day. Hyattsville (MD): National Center for Health Statistics; 2016. [Google Scholar]
- 19. Food and Nutrition Board , Dietary reference intakes for calcium and vitamin D 2011, Washington, DC: National Academy Press. [Google Scholar]
- 20. Food and Nutrition Board, Dietary Reference Intakes for water, potassium, sodium, chloride, and sulfate. Washington (DC): Institute of Medicine; 2004. [Google Scholar]
- 21. Food and Nutrition Board , Dietary Reference Intakes for calcium, phosphorus, magnesium, vitamin D and fluoride. Washington (DC): National Academies Press; 1997. [PubMed] [Google Scholar]
- 22. Rhodes DG, Murayi T, Clemens JC, Baer DJ, Sebastian RS, Moshfegh AJ. The USDA automated multiple-pass method accurately assesses population sodium intakes. Am J Clin Nutr 2013;97:958–64. [DOI] [PubMed] [Google Scholar]
- 23. Stamler R. Implications of the INTERSALT study. Hypertension 1991;47:I-16–20. [DOI] [PubMed] [Google Scholar]
- 24. Cobb LK, Andersson CAM, Elliott P, Hu FB, Liu K, Neaton JD, Whelton PK, Woodward M, Apple LJ. Methodological issues in cohort studies that relate sodium intake to cardiovasc ular disease outcome: a science advisory from the American Heart Association. Circulation 2014;129:1173–86. [DOI] [PubMed] [Google Scholar]
- 25. Graudal NA, Galloe Am, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglycerides: a meta-analysis. JAMA 1998;279:1383–91. [DOI] [PubMed] [Google Scholar]
- 26. Dietary Guidelines Advisory Committee Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010. Washington (DC): USDA, Agricultural Research Service; 2011. [Google Scholar]
- 27. Dickenson HO, Nicolson D, Cook JV, Campbell F, Beyer FR, Ford DA, Mason J. Calcium supplementation for the management of primary hypertension in adults. Cochrane Database Systematic Rev 2006;2:CD004639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 29. Kestleloot H, Tzoulaki I, Brown IJ, Chan Q, Wijeyesekera A, Ueshima H, Zhao L, Dyer AR, Unwin RJ, Stamler J et al. Relation of urinary calcium and magnesium excretion to blood pressure: the International Study of Macro- and Micronutrients and Blood Pressure and the International Cooperative Study on Salt, Other Factors and Blood Pressure. Am J Epidemiol 2001;174:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Beyer FR, Dickinson HO, Nicolson D, Ford GA, Mason J. Combined calcium, magnesium and potassium supplementation for the management of primary hypertension in adults. Cochrane Database Syst Rev 2006;(3):CD004805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sacks FM, Willett WC, Smith A, Brown LE, Rosner B, Moore TJ. Effect on blood pressure of potassium, calcium, and magnesium in women with low habitual intake. Hypertension 1998;31:131–8. [DOI] [PubMed] [Google Scholar]
- 32. Cook NR, Obarzanek E, Cutler JA, Buring JE, Rexrod KM, Kumanyika SK, Appel LJ, Whelton PK; Trials of Hypertension Prevention Collaborative Research Group Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention Follow-up Study. Arch Intern Med 2009;169:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hedayati SS, Minhajuddin AT, Ijaz A, Moe OW, Elsayed EF, Reilly RF, Huang CL. Association of urinary sodium/potassium ratio with blood pressure: sex and racial differences. Clin J Am Soc Nephrol 2012; 7:315–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Xu J, Chen X, Ge Z, Liang H, Yan L, Guo X, Zhang Y, Wang L, Ma J. Associations of usual 24-hour sodium and potassium intakes with blood pressure and risk of hypertension among adults in China's Shandong and Jiangsu Provinces. Kidney Blood Pres Res 2017;42:188–200. [DOI] [PubMed] [Google Scholar]
- 35. Stamler J, Chan Q, Daviglus ML, Dyer AR, Van Horn L, Garside DB, Miura K, Wu Y, Ueshima H, Zhao L et al. Relationship of dietary sodium (salt) to blood pressure and its possible modulation by other dietary factors—the INTERMAP study. Hypertension 2018;71:631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]