Abstract
Background: The purpose of this study was to profile the bacterium in the ascites and blood of patients with acute surgical abdomen by metagenome analysis. Methods: A total of 97 patients with acute surgical abdomen were included in this study. Accompanied with the standard culture procedures, ascites and blood samples were collected for metagenome analysis to measure the relative abundance of bacteria among groups of patients and between blood and ascites. Results: Metagenomic analysis identified 107 bacterial taxa from the ascites of patients. A principal component analysis (PCA) could separate the bacteria of ascites into roughly three groups: peptic ulcer, perforated or non-perforated appendicitis, and a group which included cholecystitis, small bowel lesion, and colon perforation. Significant correlation between the bacteria of blood and ascites was found in nine bacterial taxa both in blood and ascites with more than 500 sequence reads. However, the PCA failed to separate the variation in the bacteria of blood into different groups of patients, and the bacteria of metagenomic analysis is only partly in accordance with those isolated from a conventional culture method. Conclusion: This study indicated that the metagenome analysis can provide limited information regarding the bacteria in the ascites and blood of patients with acute surgical abdomen.
Keywords: metagenome analysis, acute surgical abdomen, infection, ascites, blood
1. Introduction
Acute abdomen is a condition that demands immediate attention and treatment. Acute abdomen may be caused by a heterogeneous group of conditions ranging from relatively benign conditions such as acute appendicitis to conditions such as diffuse peritonitis and intestinal infarction and is indicative of a surgical problem [1]. The identification of pathogenic microorganisms contaminated in the peritoneal cavity of patients with acute abdomen is important to prevent its progression into sepsis. However, the human gastrointestinal tract harbors a complex indigenous microbial flora [2,3]. Normal gut microbiota contains an estimated 1014 microbes [4], representing over 1000 different species of bacteria belonging to 190 different genera [5]. As the gastrointestinal tract proceeds distally, both the density and diversity of the flora increase within the colon, the majority of which reside in the host colon [6]. Although 500–600 distinct microbial species can be cultured from normal stool, conventional culture methods cultivate only 10–30% of gut microbiota [7,8]. Even in critically ill patients with sepsis, cultures were positive only in 60% of the cases [9]. In addition, the conventional culture method takes several days before the results are available and is labor intensive. Furthermore, empirical treatment with antibiotics prior to sample collection hampers bacterial growth in culture, thus compromising the sensitivity of the test.
In recent years, metagenome analysis by next-generation sequencing has emerged as a new method to identify the etiological agents of an infectious disease [10]. This method is based on the amplification and analysis of bacterial 16S rRNA genes with massively parallel processing [11]. Millions of DNA/RNA molecules in a specimen are sequenced in parallel and pathogens can be identified by matching the sequences to a reference database without bacterial cultivation [12,13]. This technology has allowed researchers to identify previously uncharacterized bacteria or viruses that cause infectious diseases [10,14,15] and also to investigate organisms previously thought to be inaccessible, including obligate anaerobes and other microorganisms that cannot survive outside their hosts without symbionts [11]. Furthermore, the metagenome analysis is not only useful for rapid bacterial diagnostics but also helps in assessing potential antimicrobial susceptibility [13]. It carries the potential to assist in using antibiotics based on an increased understanding of antibiotic-resistant genes in the gut microbiome [16,17,18].
The metagenome analysis has been performed to investigate the etiological agents of inflammatory diseases [19,20] in patients with sepsis [21], in neutropenic patients [22] and in children with central nervous system infection [23]. In a study of six patients with acute cholecystitis, the results of metagenome analysis from subjects with bacteria in bile were consistent with the results from conventional culture examination and antimicrobial susceptibility testing [13]. In a study of bacterial bloodstream infection in critically ill patients, the metagenome analysis showed significantly better diagnosis compared to the blood culture of patients who had received antibiotic pretreatment [24].
With the rapid development of applications in a clinical setting, the 16S metagenomic analysis provides an assumption-free approach to identify bacteria and has the potential to provide early diagnosis and novel treatments [16]. For example, in a clinical setting, the evaluation of cytological and biochemical components from abdominal fluid via abdominal paracentesis or diagnostic peritoneal lavage from a patient with acute abdominal disease is essential for the rapid determination of the disease etiology [25,26,27]. These results often assist the surgeon to make a decision regarding the necessity for surgery and initiate appropriate therapy [25,26,27]. Whether the additional metagenomic information from ascites could aid such decision-making merits further investigation. Using metagenome analysis, it would be interesting to answer the following questions: (1) Does the identified bacterial profile in ascites or blood reflect different etiologies of acute surgical abdomen? (2) Could bacteria in blood be indicative of those that could present in ascites? (3) Are the results of metagenome analysis in accordance with those obtained from conventional culture methods? Therefore, this study was designed to profile and compare the bacteria of ascites and blood in those patients with acute surgical abdomen using metagenome analysis.
2. Materials and Methods
2.1. Enrollment of Patients
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in an approval by the Institutional Review Board of Chang Gung Memorial Hospital (Ref: 201601132B0). One hundred patients who had acute surgical abdomen consecutively since 1 September 2016 were enrolled in this study. All patients read and signed the consent form before sample collection. Only those patients who were aged 18 years and above and those who had received laparotomy or laparoscopy were included. Exclusion criteria included patients with cancer, with an immunocompromised disease or those who had received cardiopulmonary resuscitation and those who has been intubated.
2.2. Clinical Data and Specimen Collection
Detailed patient information was recorded including age, sex, white blood cell count (WBC) and the percentage of segmented neutrophils which were detected at the emergency department before the operation. The operation generally started within 3 h once the diagnosis of surgical acute abdomen was established. During the laparotomy, 3 mL ascitic fluid from the abdominal cavity and 6 mL venous blood was collected from patients using EDTA tubes. The ascites were collected in the most dependent part of the abdomen or around the gall bladder. The ascites collected in the day-time were sent for DNA extraction immediately and the ascites collected in the night-time were stored at −80 °C until the next day’s morning for DNA extraction. Serum was obtained from 1 mL blood, aliquoted into 300 μL microtubes, and stored at −80 °C for cytokine analysis. All other samples were incubated with 400 μg of lysozyme (Sigma Aldrich, St. Louis, MO, USA) for 1 h at 37 °C to maximize bacterial DNA extraction. Samples of venous blood and ascitic fluid were also sent for culturing, and the isolated microorganisms were identified according to the standard microbiological procedures of the hospital [28].
2.3. Cytokine Analysis
The concentrations of C-reactive protein CRP (mg/L) and procalcitonin (ng/dL) in the serum were determined using the Bio-Plex® system (Bio-Rad, Hercules, CA, USA) according to the manufacturer’s instructions. The serum was diluted in the ratio of 1:4 with the sample diluent and incubated at room temperature for 30 min with 300 rpm agitation to capture antibody-coupled magnetic beads. Following three washes, samples were incubated at room temperature for 30 min in the dark, centrifuged at 300 rpm and a biotinylated detection antibody, streptavidin–phycoerythrin, was added in each captured analyte and quantified using a Bio-Plex array reader.
2.4. Metagenome Analysis
2.4.1. DNA Extraction
All DNA extractions were performed with 1 mL of ascitic fluid and blood using the QIAamp DNA Blood Mini Kit (No. 51104, Qiagen, Hilden, Germany) following the manufacturer’s protocol. The extracted DNA was eluted with recommended volume (400 μL) of elution buffer. DNA was isolated as per the manufacturer’s instructions. DNA concentration was measured by a Qubit® 2.0 Fluorometer (Life Technologies, Invitrogen, Carlsbad, CA, USA).
2.4.2. Amplification and Sequencing of 16S rRNA
The V3–V4 region of the bacterial 16S rRNA gene was amplified by PCR using barcoded primers reported by Klindworth et al. [29] and fused with Illumina adapter overhang nucleotide sequences. Primer sequences were 5′-TCGTCGGCAGCGTCAGATGTGTATAAGAGACAGCCTACGGGNGGCWGCAG-3′ and 5′ GTCTCGTGGGCTCGGAGATGTGTATAAGAGACAGGACTACHVGGGTATCTAATCC-3′. Two independent PCR reactions were performed for each sample. The products were pooled and indexed using Illumina’s 16S Metagenomic Sequencing Library Preparation protocol (Illumina, San Diego, CA, USA). The raw next generation sequencing (NGS) reads were first subject to quality trimming from the 3′ end, optimized for merged paired reads and fixed length trimming, followed by operational taxonomic unit (OTU) clustering before assigning a taxonomy [30]. The relative abundance based on the OTU number or taxa was used for downstream comparison of richness among groups of patients and between blood and ascites [31]. Due to possible spurious taxonomical labeling [24], those having an OTU number less than ten in both ascites and blood in all bacterial species were arbitrarily neglected in future analysis.
2.5. Statistical Analysis
Data were analyzed using the R statistical package version 3.3.0. The Kolmogorov–Smirnov test was used to ascertain the normality of the data. Non-normally distributed numeric variables were described by the median and interquartile range (IQR). Numeric variables were compared using the Kruskal–Wallis test to identify significantly different bacterial taxa among different groups, while categorical variables were compared by χ2 test. Statistical significance was indicated by two-sided p-values of <0.05. Hierarchical clustering of the isolates was performed using Ward’s method using Euclidean distances. The Kaiser–Meyer–Olkin (KMO) index of sampling adequacy and Bartlett’s test of sphericity were used to determine suitability of the data for dimension reduction analysis [32]. Principal components analysis (PCA) was conducted based on scree plot patterns [33] to reduce the data to a minimum number of components that could facilitate more precise data interpretation.
3. Results
3.1. Patient Characteristics
Among the enrolled patients, one patient who had a minimal amount of 16S rRNA gene in the ascites and two patients who were diagnosed as ileus were excluded from this study. Finally, a total of 97 patients with acute surgical abdomen were included and grouped into patients with peptic ulcer (n = 25, which included seven gastric ulcers and 18 duodenal ulcers), cholecystitis (n = 10), small bowel lesion (n = 9, which included five ischemic small bowels and four small bowel perforations), colon perforation (n = 4), perforated appendicitis (n = 30, including those with gangrene), and non-perforated appendicitis (n = 19, which thereafter was indicated as appendicitis) (Table 1). Those patients who had perforated or non-perforated appendicitis were significantly younger than the other groups of patients; in contrast, those patients who had peptic ulcer or colon perforation were significantly older than the other groups of patients. No significant difference was found among groups of patients regarding sex, WBC count, percentage of the segmented neutrophils and level of CRP and procalcitonin. General inflammation markers such as WBC count, levels of CRP and procalcitonin failed to distinguish specific etiology of acute surgical abdomen ranging from relatively benign conditions, such as acute appendicitis, to more sever ailments, such as colon perforation.
Table 1.
Characteristics and inflammation profile of the patients. WBC: white blood cells.
| Variables | Peptic Ulcer | Cholecystitis | Small Bowel Lesion | Colon Perforation | Perforated Appendicitis | Non-Perforated Appendicitis | p-Value |
|---|---|---|---|---|---|---|---|
| (n = 25) | (n = 10) | (n = 9) | (n = 4) | (n = 30) | (n = 19) | ||
| Female, n (%) | 9 (36%) | 6 (60%) | 2 (18%) | 4 (100%) | 12 (40%) | 10 (53%) | 0.09 |
| Age (years) | 70.0 (55.0–84.0) | 52.5 (45.5–57.3) | 58.0 (49.0–72.0) | 74.5 (63.0–80.0) | 37.0 (27.5–57.8) | 35.0 (31.0–42.0) | 0.002 |
| WBC (103/uL) | 9.4 (5.7–14.7) | 12.4 (10.8–14.2) | 11.6 (8.6–15.9) | 10.9 (9.7–12.3) | 12.4 (11.3–16.1) | 13.3 (12.2–14.9) | 0.20 |
| Segment (%) | 83.0 (78.0–88.4) | 85.8 (82.2–87.9) | 84.8 (75.6–88.0) | 85.9 (78.9–91.2) | 82.6 (76.5–88.2) | 79.8 (76.6–84.2) | 0.51 |
| C-reactive protein (mg/L) | 36.8 (2.9–99.1) | 9.1 (3.9–167.3) | 127.2 (47.5–240.5) | 113.0 (42.2–221.3) | 25.8 (18.3–55.2) | 14.0 (3.8–23.0) | 0.97 |
| Procalcitonin (ng/dL) | 1847.0 (11.0–3601.0) | 11.3 (10.3–1895.0) | 13.5 (11.0–3176.0) | 12.8 (11.4–14.4) | 12.0 (10.5–2743.0) | 11.5 (9.5–2960.0) | 0.16 |
3.2. Hierarchical Clustering of the Bacteria
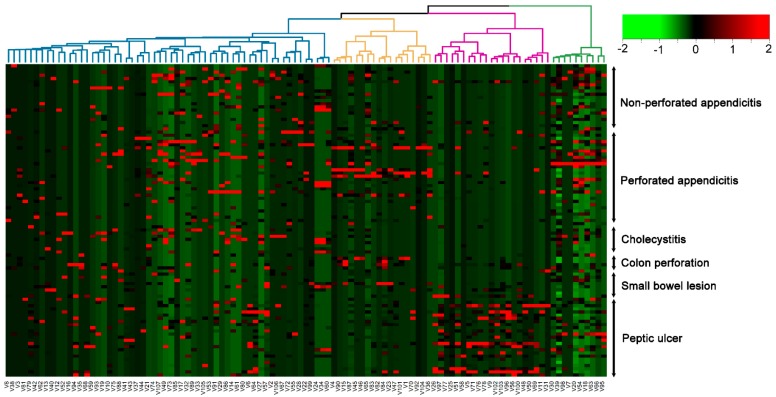
An overview of 107 bacterial taxa identified from the ascites of patients by metagenome analysis is shown in Supplementary Table S1. At the phylum level, bacteria were dominated by members of Proteobacteria and Firmicutes, followed by Actinobacteria and Bacteriodetes, with Spirochaetes and Verrucomicrobia in much lower numbers. Hierarchical cluster analysis (Figure 1) of bacterial communities by Ward’s method using Euclidean distances showed that patients of the peptic ulcer group had a different bacterial community.
Figure 1.
Hierarchical clustering of the 107 bacterial taxa identified from the ascites of these patients from metagenome analysis.
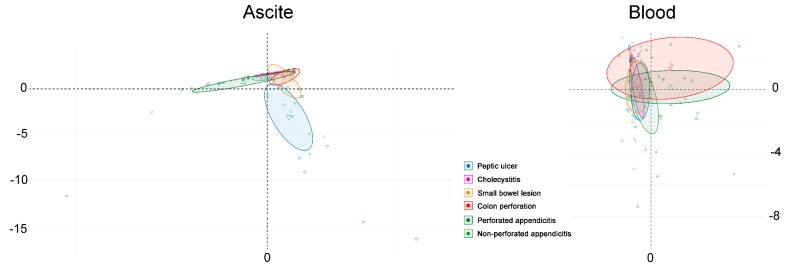
3.3. Principal Component Analysis
Principal component analysis (PCA) was performed on the bacteria of ascites and blood to separate patients with different etiologies of acute surgical abdomen (Figure 2). The Kaiser–Meyer–Olkin test (KMO = 0.61) and Bartlett’s test of sphericity (χ2 = 3642, p < 0.0001) [34] were used to validate that the chosen variables are able to obtain reliable and distinct factors. The resulting five-factor structure with 22 bacteria explains 77% of the total variance (Figure 1). Factor loadings of variables are shown in Figure 2. The PCA could separate the bacteria of ascites into roughly three groups: peptic ulcer, perforated or non-perforated appendicitis, and a group which included cholecystitis, small bowel lesion and colon perforation. However, the PCA could not separate the variation in bacteria of blood into different groups of patients according to their etiologies of acute surgical abdomen.
Figure 2.
A principal component analysis conducted on the bacteria of ascites and blood to separate patients with different etiologies of acute surgical abdomen (PC1 explaining 34.1% of the variance; PC2 explaining 22.6% of the variance).
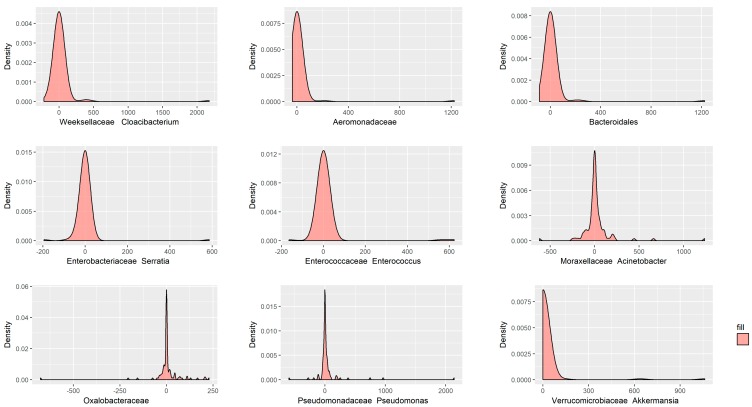
3.4. Correlation of Bacteria of Blood and Ascites
To assess whether the bacteria in the blood could indicate the bacteria that were contaminated in the ascites, the abundance of bacteria detected in blood were compared to those detected in ascites. The bacteria of blood and ascites were comparable in 48 of 107 bacterial taxa (see Supplementary Table S1) and belonged to different species. At the phylum level, the similar bacteria were dominated by members of Proteobacteria (16 taxa), Firmicutes (15 taxa), Bacteriodetes (11 taxa) and Actinobacteria (5 taxa), with Spirochaetes (1 taxa) in much lower frequency. Depending on the criteria of identifying at least more than 500 sequence reads in both blood and ascites, there were nine taxa showing significant correlation, including Weeksellaceae Cloacibacterium, Aeromonadaceae, Bacteroidales, Enterobacteriaceae Serratia, Enterococcaceae Enterococcus, Moraxellaceae Acinetobacter, Oxalobacteraceae, Pseudomonadaceae Pseudomonas, Verrucomicrobiaceae Akkermansia (Figure 3).
Figure 3.
Nine bacterial taxa present a significant correlation both in the blood and ascites, with more than 500 sequence reads.
3.5. Correlation of Bacteria from Metagenome Analysis and Conventional Culture Methods
Conventional cultures of 19 ascites and three blood samples showed positive results (Table 2). These cultures of ascites and blood of patients with acute surgical abdomen showed mixed infection with Gram-positive, Gram-negative and anaerobic bacteria and did not correlate well with those identified from metagenome analysis. In the ascites, the correlation between metagenomic bacteria and conventional cultures were found as Enterobacteriaceae for Escherichia coli in nine patients or Enterobacter cloacae in one patient, Klebsiella for Klebsiella pneumoniae in two patients, Neisseria subflava for Neisseria flavescens in one patient, Streptococcus for Streptococcus oralis in two patients or for Streptococcus mitis in one patient, and Bacteroides fragilis for Bacteroides fragilis in two patients. In the blood, the correlation between metagenomic bacteria and conventional cultures could be only found as Enterobacteriaceae for Escherichia coli in one patient.
Table 2.
Comparison of metagenomic bacterium and conventional culture in the ascites and blood.
| Ascites Culture vs. Bacterium of 16S Metagenomics | |||
| No. | Diagnosis | Ascites Culture | Bacterium |
| 1 | Gastric ulcer | Klebsiella pneumoniae |
Enterobacteriaceae
Streptococcus |
| 2 | Duodenal ulcer | Escherichia coli |
Enterobacteriaceae
Prevotella sp Streptococcus |
| 3 | Duodenal ulcer |
Neisseria flavescens
Streptococcus mitis Streptococcus oralis |
Actinobacillus parahaemolyticus
Neisseria subflava Streptococcus |
| 4 | Duodenal ulcer | Escherichia coli |
Enterobacteriaceae
Haemophilus parainfluenzae |
| 5 | Duodenal ulcer |
Viridans streprococcus
Veillonella parvula |
Enterobacteriaceae
Actinobacillus parahaemolyticus |
| 6 | Duodenal ulcer |
Viridans streptococcus
Streptococcus salicarius |
Enterobacteriaceae |
| 7 | Duodenal ulcer |
Klebsiella pneumoniae
Streptococcus salivarius Staphylococcus aureus |
Enterobacteriaceae
Klebsiella |
| 8 | Duodenal ulcer | Streptococcus oralis |
Enterobacteriaceae
Streptococcus |
| 9 | Duodenal ulcer |
Streptococcus salivarius
Escherichia coli Acinetobacter |
Enterobacteriaceae |
| 10 | Small bowel perforation |
Escherichia coli
Enterobacter cloacae Pseudomonas aeruginosa |
Enterobacteriaceae |
| 11 | Small bowel ischemia | Klebsiella pneumoniae | Klebsiella |
| 12 | Small bowel ischemia |
Escherichia coli
Lactobacilus Bacteroides ovatus |
Enterobacteriaceae
Prevotella copri |
| 13 | Colon perforation |
Escherichia coli
Streptococcus anginosus Bacteroides thetaiotaomicron |
Enterobacteriaceae
Prevotella copri |
| 14 | Colon perforation |
Escherichia coli
Streptococcus asalivarius Klebsiella pneumoniae |
Prevotella copri |
| 15 | Colon perforation |
Enterococcus faecium
Pseudomonas aeruginosa |
Enterobacteriaceae
Lactobacillus Prevotella |
| 16 | Perforated appendicitis |
Escherichia coli
Enterococcus avium Pseudomonas aeruginosa |
Odoribacter
Rikenellaceae |
| 17 | Perforated appendicitis |
Escherichia coli
Bacteroides fragilis Bacteroides thetaiotaomicron |
Enterobacteriaceae
Porphyromonas Bacteroides fragilis |
| 18 | Perforated appendicitis |
Escherichia coli
Pseudomonas aeruginosa Bacteroides vulgatus |
Porphyromonas endodontalis
Enterobacteriaceae Bacteroides fragilis |
| 19 | Perforated appendicitis |
Escherichia coli
Streptococcus anginosus Bacteroides fragilis |
Enterobacteriaceae
Porphyromonas Bacteroides fragilis |
| Blood Culture vs. Bacterium of 16S Metagenomics | |||
| No. | Diagnosis | Blood Culture | Bacterium |
| 20 | Gastric ulcer | Roseomonas mucosa | Enterobacteriaceae |
| 2 | Duodenal ulcer | Escherichia coli | Enterobacteriaceae |
| 10 | Small bowel perforation | Staphylococcus | Enterobacteriaceae |
4. Discussion
In this study, the bacteria of ascites from metagenome analysis can be separated into three groups: peptic ulcer, perforated or non-perforated appendicitis, and a group which includes cholecystitis, small bowel lesion and colon perforation. The human appendix has been reported to harbor a robust and varied microbiota distinct from the microbiotas in other niches within the human microbiome [35]. The bacterial growth in inflamed appendices consists of a mix of aerobic and anaerobic bacteria, most often dominated by Escherichia coli and Bacteroides [36]. The metagenome analysis of microbial composition of the human appendix identified Firmicutes as the dominant phylum, with additional varied levels of Proteobacteria, Bacteroidetes, Actinobacteria and Fusobacteria [35]. Unsurprisingly, in those patients with peptic ulcer, the bacteria from acidic environment of the stomach may be different from those that grow in the gastrointestinal tract. It was not until the discovery of H. pylori in 1982 by Marshall and Warren that the acidic environment of the stomach was considered sterile [37]. However, many bacterial strains including Streptococcus, Neisseria, Lactobacillus and others have been repeatedly identified from the gastric fluid [38]. Most common bacteria of the stomach mucosa belong to the following five phyla: Actinobacteria, Bacteroidetes, Firmicutes, Proteobacteria (includes H. pylori), and Fusobacteria [39]. In contrast, acute cholecystitis is strongly associated with retrograde bacterial infection [13], and the bacteria are similar to those that reside in the intestine.
The results of this study revealed that the use of a bacterial profile from the ascites to reflect on different etiologies of acute surgical abdomen is still in its infancy and rather relies on PCA, which consists of varied information from specific groups of bacteria. In addition, the PCA failed to separate the variation in bacteria of blood into different groups of patients according to the different etiologies of acute surgical abdomen. This study indicates that metagenomic diagnosis may encounter some problems. First, the broad range of bacteria that can be detected limits the specificity of the assay. It is also unclear whether the detected bacteria are truly clinically significant or are environmental contaminants picked up during sample preparation. The lack of appropriate controls makes it difficult to distinguish such environmental contaminants from clinically relevant bacteria. Second, the patients are generally treated with antimicrobial agents before operation. Although the metagenome analysis is based on the sequences acquired and is regardless of dead or live bacteria, the probable impact of antibiotic use on the metagenome analysis is therefore unknown, as some information acquired from metagenome analysis may even be related to those dead bacteria and therefore be less informative. Third, the elapsed time from the occurrence of the disease to the harvesting of ascites or blood specimen for metagenome analysis may vary among some etiologies of acute surgical abdomen, especially for an illness that may have presented in an acute or subacute phase (for example, non-perforated appendicitis and cholecystitis). In such sample, the diversity of gut microbiota is significantly decreased and pathogenic bacteria would comprise the majority of gut microbiota [40]. At last, it has been reported that the intestinal microbiota from adulthood through old age changes [41], and the broad range in patient ages sustaining a varied etiology of acute surgical abdomen may lead to some bias in the analysis of the metagenomic profile. This study indicated that there still remains a space for improvement regarding the metagenomics analysis. Moreover, additional clinical manifestation or additional biochemistry biomarkers may be helpful to differentiate the various etiologies of acute surgical abdomen, such as making a difference between the cholecystitis from the perforation in the bowel.
It has been reported that 16S metagenome analysis detects more clinically significant bacteria than blood culture in children with severe febrile illness [24]. In a study of metagenomics analysis of brain abscesses, all 30 culture-positive specimens are also positive for PCR experiments [42]. In a comparative study of the bacterial pathogens from clinical specimens, it was found that metagenomics results have a concordance rate/positive predictive value of 91.8% (56/61) when compared with culture positive specimens [43]. The concordance rate would decrease to 77.3% (n = 75/97) when using stringent comparison criteria for metagenomics vs. culture comparison [43]. However, in this study, the results of metagenome analysis are only partly in accordance with those carried out from conventional cultures. Among the 107 bacterial taxa in the ascites, 48 taxa can be found in blood and nine taxa correlated both in the blood and ascites. We think this discordance may be partly attributed to a comparison made under relatively stringent conditions; that is, we arbitrarily neglected an OTU number less than ten in both ascites and blood in all bacterial species. Without some selection criteria, the metagenomics analysis can give a wide range of organism and microbial profiles which are difficult to interpret [43] and associated with high false-positive results [24]. Of note is the fact that the clinical features of peritonitis are dependent more on the response of the host than on the intrinsic virulence of the infecting flora [1]. For example, experimental studies suggest that the anaerobes play an important role in the induction of abscess formation, whereas the aerobic Gram-negative microbes are largely responsible for the lethality of peritonitis [44]. Some studies reported that in patients with inflammatory bowel disease, the gut microbiota show an increase in the number of species belonging to Proteobacteria, including E. coli [45], while the proportion of Proteobacteria in healthy human intestinal microbiota was only 1% [46]. Therefore, of concern is not only the issue of correlation of the bacterial taxa between blood and ascites, but the clinical meaning of the metagenome analysis also remains to be explored.
So far, it is too early to say whether this technique would or would not replace conventional bacterial culture. In particular, metagenomics allows the detection of full-length antibiotic resistance genes from the Antibiotic Resistance Database [47] or from the environmental samples of unknown composition [48], making metagenomics analysis advantageous to provide timely and valuable information in prescribing antibiotics or modifying antibiotic therapy in secondary peritonitis. It is expected that, with a profound understanding of the role of the human microbiome in diseases and their interactions, as well as inter-individual differences, the metagenome analysis will progress immensely [49].
5. Conclusions
This study reveals that, at the current stage, metagenome analysis can only provide limited information regarding the bacteria of ascites and blood of patients with acute surgical abdomen and, although many questions still remain unanswered, there is plenty of scope for improvement of the metagenome approach to profile bacteria in surgical patients with infectious diseases.
Supplementary Materials
The supplementary material is available online at http://www.mdpi.com/2077-0383/7/10/346/s1.
Author Contributions
S.-C.W. wrote the manuscript; C.-S.R. drafted the manuscript and was involved in the literature review; H.-T.L. designed the study; P.-J.K. helped with the revision of the manuscript; P.-C.C. performed the statistical analyses; T.-M.H., C.-H.T., J.F.C. and C.-Y.H. were responsible for the acquisition of the contributing cases; H.-Y.H. proofread the manuscript; and C.-H.H. designed the study, analyzed the data, and edited the tables.
Funding
The work was supported by Chang Gung Memorial Hospital (CMRPG8F1861 to Hang-Tsung Liu and CMRPG8E0711 to Ching-Hua Hsieh).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Marshall J.C. Intra-abdominal infections. Microbes Infect. 2004;6:1015–1025. doi: 10.1016/j.micinf.2004.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Weinstock G.M. Genomic approaches to studying the human microbiota. Nature. 2012;489:250–256. doi: 10.1038/nature11553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savage D.C. Microbial ecology of the gastrointestinal tract. Annu. Rev. Microbiol. 1977;31:107–133. doi: 10.1146/annurev.mi.31.100177.000543. [DOI] [PubMed] [Google Scholar]
- 4.Ley R.E., Peterson D.A., Gordon J.I. Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell. 2006;124:837–848. doi: 10.1016/j.cell.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 5.Qin J., Li R., Raes J., Arumugam M., Burgdorf K.S., Manichanh C., Nielsen T., Pons N., Levenez F., Yamada T., et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quigley E.M. Gut bacteria in health and disease. Gastroenterol. Hepatol. 2013;9:560–569. [PMC free article] [PubMed] [Google Scholar]
- 7.Sokol H., Seksik P. The intestinal microbiota in inflammatory bowel diseases: Time to connect with the host. Curr. Opin. Gastroenterol. 2010;26:327–331. doi: 10.1097/MOG.0b013e328339536b. [DOI] [PubMed] [Google Scholar]
- 8.Tannock G.W. Molecular assessment of intestinal microflora. Am. J. Clin. Nutr. 2001;73(Suppl. 2):410s–414s. doi: 10.1093/ajcn/73.2.410s. [DOI] [PubMed] [Google Scholar]
- 9.Vincent J.L., Sakr Y., Sprung C.L., Ranieri V.M., Reinhart K., Gerlach H., Moreno R., Carlet J., Le Gall J.R., Payen D. Sepsis in European intensive care units: Results of the SOAP study. Crit. Care Med. 2006;34:344–353. doi: 10.1097/01.CCM.0000194725.48928.3A. [DOI] [PubMed] [Google Scholar]
- 10.Chan J.Z., Pallen M.J., Oppenheim B., Constantinidou C. Genome sequencing in clinical microbiology. Nat. Biotechnol. 2012;30:1068–1071. doi: 10.1038/nbt.2410. [DOI] [PubMed] [Google Scholar]
- 11.Tringe S.G., Rubin E.M. Metagenomics: DNA sequencing of environmental samples. Nat. Rev. Genet. 2005;6:805–814. doi: 10.1038/nrg1709. [DOI] [PubMed] [Google Scholar]
- 12.Takeuchi F., Sekizuka T., Yamashita A., Ogasawara Y., Mizuta K., Kuroda M. MePIC, metagenomic pathogen identification for clinical specimens. Jpn. J. Infect. Dis. 2014;67:62–65. doi: 10.7883/yoken.67.62. [DOI] [PubMed] [Google Scholar]
- 13.Kujiraoka M., Kuroda M., Asai K., Sekizuka T., Kato K., Watanabe M., Matsukiyo H., Saito T., Ishii T., Katada N., et al. Comprehensive Diagnosis of Bacterial Infection Associated with Acute Cholecystitis Using Metagenomic Approach. Front. Microb. 2017;8:685. doi: 10.3389/fmicb.2017.00685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lavezzo E., Toppo S., Franchin E., Di Camillo B., Finotello F., Falda M., Manganelli R., Palu G., Barzon L. Genomic comparative analysis and gene function prediction in infectious diseases: Application to the investigation of a meningitis outbreak. BMC Infect. Dis. 2013;13:554. doi: 10.1186/1471-2334-13-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faria N.R., Azevedo R., Kraemer M.U.G., Souza R., Cunha M.S., Hill S.C., Theze J., Bonsall M.B., Bowden T.A., Rissanen I., et al. Zika virus in the Americas: Early epidemiological and genetic findings. Science. 2016;352:345–349. doi: 10.1126/science.aaf5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang W.L., Xu S.Y., Ren Z.G., Tao L., Jiang J.W., Zheng S.S. Application of metagenomics in the human gut microbiome. World J. Gastroenterol. 2015;21:803–814. doi: 10.3748/wjg.v21.i3.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bengtsson-Palme J., Angelin M., Huss M., Kjellqvist S., Kristiansson E., Palmgren H., Larsson D.G., Johansson A. The Human Gut Microbiome as a Transporter of Antibiotic Resistance Genes between Continents. Antimicrob. Agents Chemother. 2015;59:6551–6560. doi: 10.1128/AAC.00933-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fitzpatrick D., Walsh F. Antibiotic resistance genes across a wide variety of metagenomes. FEMS Microbiol. Ecol. 2016;92:2. doi: 10.1093/femsec/fiv168. [DOI] [PubMed] [Google Scholar]
- 19.Coit P., Sawalha A.H. The human microbiome in rheumatic autoimmune diseases: A comprehensive review. Clin. Immunol. 2016;170:70–79. doi: 10.1016/j.clim.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 20.Ferreira C.M., Vieira A.T., Vinolo M.A., Oliveira F.A., Curi R., Martins Fdos S. The central role of the gut microbiota in chronic inflammatory diseases. J. Immunol. Res. 2014;2014:689492. doi: 10.1155/2014/689492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faria M.M., Conly J.M., Surette M.G. The development and application of a molecular community profiling strategy to identify polymicrobial bacterial DNA in the whole blood of septic patients. BMC Microbiol. 2015;15:215. doi: 10.1186/s12866-015-0557-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gyarmati P., Kjellander C., Aust C., Kalin M., Ohrmalm L., Giske C.G. Bacterial Landscape of Bloodstream Infections in Neutropenic Patients via High Throughput Sequencing. PLoS ONE. 2015;10:e0135756. doi: 10.1371/journal.pone.0135756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turner P., Suy K., Tan L.V., Sar P., Miliya T., Hong N.T.T., Hang V.T.T., Ny N.T.H., Soeng S., Day N.P.J., et al. The aetiologies of central nervous system infections in hospitalised Cambodian children. BMC Infect. Dis. 2017;17:806. doi: 10.1186/s12879-017-2915-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Decuypere S., Meehan C.J., Van Puyvelde S., De Block T., Maltha J., Palpouguini L., Tahita M., Tinto H., Jacobs J., Deborggraeve S. Diagnosis of Bacterial Bloodstream Infections: A 16S Metagenomics Approach. PLoS Negl. Trop. Dis. 2016;10:e0004470. doi: 10.1371/journal.pntd.0004470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Connally H.E. Cytology and fluid analysis of the acute abdomen. Clin. Tech. Small Anim. Pract. 2003;18:39–44. doi: 10.1016/1096-2867(03)90024-7. [DOI] [PubMed] [Google Scholar]
- 26.Dye T. The acute abdomen: A surgeon’s approach to diagnosis and treatment. Clin. Tech. Small Anim. Pract. 2003;18:53–65. doi: 10.1016/1096-2867(03)90026-0. [DOI] [PubMed] [Google Scholar]
- 27.Walters J.M. Abdominal paracentesis and diagnostic peritoneal lavage. Clin. Tech. Small Anim. Pract. 2003;18:32–38. doi: 10.1016/1096-2867(03)90023-5. [DOI] [PubMed] [Google Scholar]
- 28.Kawecki D., Chmura A., Pacholczyk M., Lagiewska B., Adadynski L., Wasiak D., Czerwinski J., Malkowski P., Sawicka-Grzelak A., Kot K., et al. Bacterial infections in the early period after liver transplantation: Etiological agents and their susceptibility. Med. Sci. Monit. 2009;15:Cr628–Cr637. doi: 10.1016/S1201-9712(08)60021-1. [DOI] [PubMed] [Google Scholar]
- 29.Klindworth A., Pruesse E., Schweer T., Peplies J., Quast C., Horn M., Glockner F.O. Evaluation of general 16S ribosomal RNA gene PCR primers for classical and next-generation sequencing-based diversity studies. Nucleic Acids Res. 2013;41:e1. doi: 10.1093/nar/gks808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lluch J., Servant F., Paisse S., Valle C., Valiere S., Kuchly C., Vilchez G., Donnadieu C., Courtney M., Burcelin R., et al. The Characterization of Novel Tissue Microbiota Using an Optimized 16S Metagenomic Sequencing Pipeline. PLoS ONE. 2015;10:e0142334. doi: 10.1371/journal.pone.0142334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCann J.C., Wickersham T.A., Loor J.J. High-throughput Methods Redefine the Rumen Microbiome and Its Relationship with Nutrition and Metabolism. Bioinf. Boil. Insights. 2014;8:109–125. doi: 10.4137/BBI.S15389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guadagnoli E., Velicer W.F. Relation of sample size to the stability of component patterns. Psychol. Bull. 1988;103:265–275. doi: 10.1037/0033-2909.103.2.265. [DOI] [PubMed] [Google Scholar]
- 33.Liu Y.J., Tran T., Postma G., Buydens L.M.C., Jansen J. Estimating the number of components and detecting outliers using Angle Distribution of Loading Subspaces (ADLS) in PCA analysis. Anal. Chim. Acta. 2018;1020:17–29. doi: 10.1016/j.aca.2018.03.044. [DOI] [PubMed] [Google Scholar]
- 34.Kang H. A guide on the use of factor analysis in the assessment of construct validity. J. Korean Acad. Nurs. 2013;43:587–594. doi: 10.4040/jkan.2013.43.5.587. [DOI] [PubMed] [Google Scholar]
- 35.Guinane C.M., Tadrous A., Fouhy F., Ryan C.A., Dempsey E.M., Murphy B., Andrews E., Cotter P.D., Stanton C., Ross R.P. Microbial composition of human appendices from patients following appendectomy. mBio. 2013;4:e00366-12. doi: 10.1128/mBio.00366-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhangu A., Soreide K., Di Saverio S., Assarsson J.H., Drake F.T. Acute appendicitis: Modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 37.Marshall B.J., Warren J.R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311–1315. doi: 10.1016/S0140-6736(84)91816-6. [DOI] [PubMed] [Google Scholar]
- 38.Minalyan A., Gabrielyan L., Scott D., Jacobs J., Pisegna J.R. The Gastric and Intestinal Microbiome: Role of Proton Pump Inhibitors. Curr. Gastroenterol. Rep. 2017;19:42. doi: 10.1007/s11894-017-0577-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bik E.M., Eckburg P.B., Gill S.R., Nelson K.E., Purdom E.A., Francois F., Perez-Perez G., Blaser M.J., Relman D.A. Molecular analysis of the bacterial microbiota in the human stomach. Proc. Natl. Acad. Sci. USA. 2006;103:732–737. doi: 10.1073/pnas.0506655103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zaborin A., Smith D., Garfield K., Quensen J., Shakhsheer B., Kade M., Tirrell M., Tiedje J., Gilbert J.A., Zaborina O., et al. Membership and behavior of ultra-low-diversity pathogen communities present in the gut of humans during prolonged critical illness. mBio. 2014;5:e01361-14. doi: 10.1128/mBio.01361-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O’Toole P.W. Changes in the intestinal microbiota from adulthood through to old age. Clin. Microbiol. Infect. 2012;18(Suppl. 4):44–46. doi: 10.1111/j.1469-0691.2012.03867.x. [DOI] [PubMed] [Google Scholar]
- 42.Al Masalma M., Lonjon M., Richet H., Dufour H., Roche P.H., Drancourt M., Raoult D., Fournier P.E. Metagenomic analysis of brain abscesses identifies specific bacterial associations. Clin. Infect. Dis. 2012;54:202–210. doi: 10.1093/cid/cir797. [DOI] [PubMed] [Google Scholar]
- 43.Abayasekara L.M., Perera J., Chandrasekharan V., Gnanam V.S., Udunuwara N.A., Liyanage D.S., Bulathsinhala N.E., Adikary S., Aluthmuhandiram J.V.S., Thanaseelan C.S., et al. Detection of bacterial pathogens from clinical specimens using conventional microbial culture and 16S metagenomics: A comparative study. BMC Infect. Dis. 2017;17:631. doi: 10.1186/s12879-017-2727-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tzianabos A.O., Onderdonk A.B., Smith R.S., Kasper D.L. Structure-function relationships for polysaccharide-induced intra-abdominal abscesses. Infect. Immun. 1994;62:3590–3593. doi: 10.1128/iai.62.8.3590-3593.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morgan X.C., Tickle T.L., Sokol H., Gevers D., Devaney K.L., Ward D.V., Reyes J.A., Shah S.A., LeLeiko N., Snapper S.B., et al. Dysfunction of the intestinal microbiome in inflammatory bowel disease and treatment. Genome Biol. 2012;13:R79. doi: 10.1186/gb-2012-13-9-r79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tap J., Mondot S., Levenez F., Pelletier E., Caron C., Furet J.P., Ugarte E., Munoz-Tamayo R., Paslier D.L., Nalin R., et al. Towards the human intestinal microbiota phylogenetic core. Environ. Microbiol. 2009;11:2574–2584. doi: 10.1111/j.1462-2920.2009.01982.x. [DOI] [PubMed] [Google Scholar]
- 47.Liu B., Pop M. ARDB—Antibiotic Resistance Genes Database. Nucleic Acids Res. 2009;37:D443–D447. doi: 10.1093/nar/gkn656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rowe W., Baker K.S., Verner-Jeffreys D., Baker-Austin C., Ryan J.J., Maskell D., Pearce G. Search Engine for Antimicrobial Resistance: A Cloud Compatible Pipeline and Web Interface for Rapidly Detecting Antimicrobial Resistance Genes Directly from Sequence Data. PLoS ONE. 2015;10:e0133492. doi: 10.1371/journal.pone.0133492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heintz-Buschart A., Wilmes P. Human Gut Microbiome: Function Matters. Trends Microbiol. 2018;26:563–574. doi: 10.1016/j.tim.2017.11.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.