Abstract
Introduction:
Differentiation between pancreatic ductal adenocarcinoma (PDAC) from benign mimickers is a well-known problem in cytological materials. Recent studies incorporated biological markers into this question and some studies showed that expression of S100P, IMP3, and maspin as well as nonexpression of von Hippel-Lindau gene product (pVHL) were significantly correlated with PDAC. In this study, we aimed to investigate diagnostic value of maspin, IMP3, S100P, and pVHL immunostaining in fine needle aspiration biopsies (FNABs) of pancreatic lesions.
Materials and Method:
In all, 33 cases of FNAB cell blocks of PDAC and 34 cases of surgical non-neoplastic pancreas specimens which were retrieved from the archives slides from 2007 to 2011 were included in this study. All the cases were stained with maspin, IMP3, S100P, and pVHL. Expression patterns of markers were scored and compared with benign mimickers. Test performance of each antibody and possible antibody combinations were also evaluated.
Results:
The study was composed of 33 PDAC and 34 control cases (8 chronic pancreatitis, 3 mucinous cystic neoplasm, and 23 nontumoral pancreatic tissue of PDAC). Diagnostic sensitivity for malignancy in S100P, IMP3, and maspin was 84.8%, 81.8%, and 87.5%, respectively. Specificity of these three markers was 100%. Sensitivity and specificity of pVHL for detecting nontumoral pancreatic tissue were 100% and 81.8%, respectively. When maspin, IMP3, and S100P expression were used together as triple test, sensitivity was 62.5% and specificity 100%. However, when any two of each three markers were evaluated (triple test/dual response), sensitivity reached 93.8% and specificity 100%.
Conclusion:
We observed that dual response in triple test (positive staining with two of these three markers) of maspin, IMP3, and S100P immunocytochemistry is very sensitive and specific in differential diagnosis of PDA and non-neoplastic pancreatic lesions. pVHL may have an additional role, when triple assessment is not satisfactory.
Keywords: IMP3, maspin, pancreatic adenocarcinoma, pVHL, S100P
INTRODUCTION
Pancreatic ductal adenocarcinoma (PDAC) is one of the most common fatal cancers whose incidence nearly equals the mortality rate.[1] PDAC accounts for 85%–90% of pancreatic neoplasms. As the initial symptoms are nonspecific, the diagnosis of the PDAC is usually delayed,[1] and most of the tumors are inoperable at the time of diagnosis. When a pancreatic mass is found in a patient, PDAC is usually a major concern, and diagnosis mostly is made by fine needle aspiration biopsy (FNAB) or and small tissue core biopsy, rather than a pancreatic surgical resection specimen.[2]
Differential diagnosis of a well-differentiated PDAC from non-neoplastic pancreatic tissue may be very challenging, even in surgical material. This differential diagnosis may be more complicated in FNAB and small tissue core biopsies.[3] Therefore, specific tumor-associated markers that could be useful in differential diagnosis of PDAC are being sought. Of recent markers for potential benefit, prostate stem cell antigen, mesothelin, MUC-1, and claudin-4 are conspicuous for differentiating PDAC from benign pancreatic epithelial lesions.[3,4,5,6]
There are some reports that evaluate usefulness of IMP3, S100P, maspin, and von Hippel-Lindau gene product (pVHL) in differentiating benign/reactive bile duct epithelium including gallbladder adenocarcinoma and ampullary adenocarcinoma.[3,7,8,9,10,11,12,13] These antibodies were also evaluated in PDAC. However, reports that use diagnostic value of these antibodies in the differential diagnosis of PDAC in FNAB material from normal/reactive pancreatic tissue are limited to few.[3,7,8,9] The goal of this study was to investigate the diagnostic use of pVHL, maspin, IMP3, and S100P immunostains on differential diagnosis of PDAC and benign/reactive pancreatic epithelium.
MATERIALS AND METHOD
The study was approved by the institutional review board at Ankara University Faculty of Medicine. In all, 33 cases of FNAB cell blocks of ductal carcinoma of the pancreas were retrieved from the archives of the Division of Cytopathology and 34 cases of surgical (pancreatico-duodenectomy specimen) non-neoplastic pancreas specimens were retrieved from the Department of Pathology at Ankara University Faculty of Medicine from 2007 to 2011. Cell blocks and smear were obtained by ultrasound-guided percutaneous aspiration performed by a modified Menghini-type semi-automated aspiration biopsy needle with 21- to 22-gauge. Menghini is an aspiration or suction-type needle which allows cytological material and fragmented biopsy samples in one shut. All the aspiration was performed in Radiology Department by ultrasound guidance. When the biopsy was performed, rapid on-side cytopathological evaluation was made by a cytopathologist. After smears were prepared, the remaining materials were immediately placed in formalin for cell block.
Adenocarcinoma cases which had malignant cytology with an adequate cellularity in the cell block preparations were included in this study. Adequate cellularity in the cell block was defined as at least five groups of atypical epithelial cells (more than 10 cells in each group) [Figure 1]. All of the cases were confirmed by either histologically or radiological correlation. (Tumor extending into the stomach, colon, or adjacent great vessels with/without lymph node metastases or distant metastases were used for radiologic confirmation in nine cases).
Figure 1.
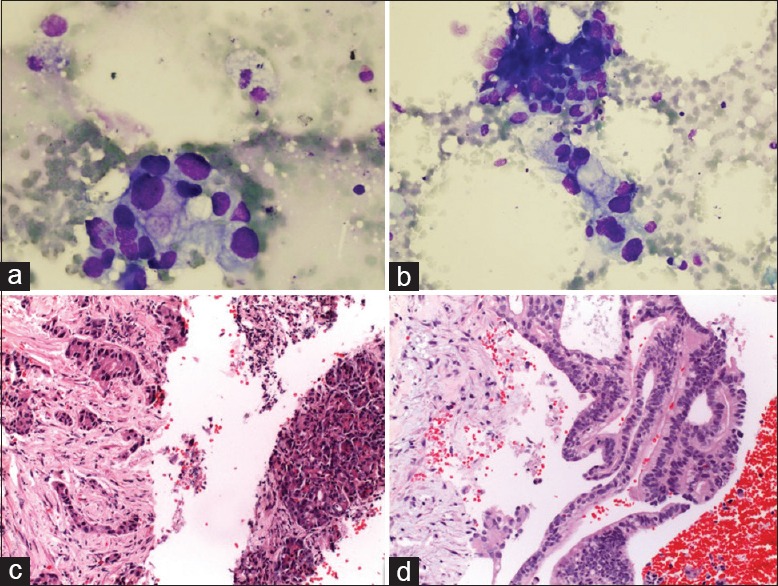
(a and b) Cytologic feature of PDAC: loosely arranged epithelial cells showing marked nuclear enlargement, nuclear membrane irregularity, anisonucleosis (MGG ×400). (c and d) Cell block sections of a PDAC. (c)Irregular, angulated small tubules are embedded in a sclerotic stroma; in the right part, there is a nontumoral pancreatic tissue. (d) Pseudostratified tumor cells that form fused glands and cribriform structure (H&E ×400)
For control group, paraffin blocks of benign/reactive pancreatic tissue that was obtained from the surgical material of pancreatic resection specimens (8 chronic pancreatitis, 3 mucinous cystic neoplasm, 23 PDACs) were included.
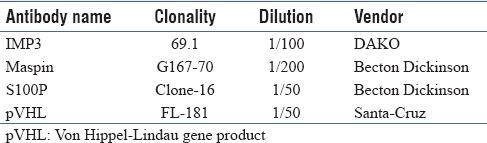
Immunocytochemical study was performed from cell blocks of PDAC and paraffin blocks of the control group. Antibodies used in this study are S100P, IMP3, maspin, and pVHL. Staining was done on Ventana staining system in the immunohistochemistry laboratory of the Department of Pathology at the University of Ankara. Detailed information about the antibodies is summarized in Table 1.
Table 1.
Summary of antibody information
Scoring
For S100P and maspin, nuclear and/or cytoplasmic staining; for pVHL, membranous and cytoplasmic expression; and for IMP3, cytoplasmic staining were regarded as definite positivity. The staining intensity for both tumor cell blocks and control group was graded as weak or strong. The distribution (number of tumor cells stained) was recorded as negative (<5% of tumor cells stained), 1+ (5%–25%), 2+ (26%–50%), 3+ (51%–75%), and 4+ (>75%).[3] All immunostained slides were blindly reviewed by two cytopathologists (A.A.-A. and K.C.). Test performance of each antibody and possible antibody combinations were also evaluated.
Statistical analysis
Chi-square analysis was performed with SPSS 11.5 for Windows software to evaluate statistical significance of the immunostaining profile between PDAC and control group.
RESULTS
Positive immunoreactivity for IMP3 was observed in 28 of the 33 (84.8%) PDAC cases, with 26 cases (92.9%) showing strong staining [Figure 2a]. Reactivity was diffuse as +3 or more in 25 cases (89.3%) and as +2 or more in 27 cases (96.4) among these positive stained cases [Table 2].
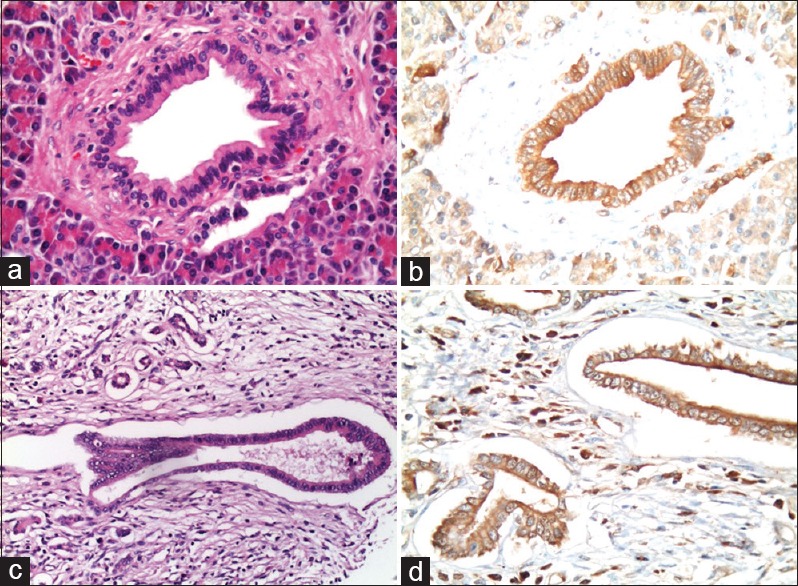
Figure 2.
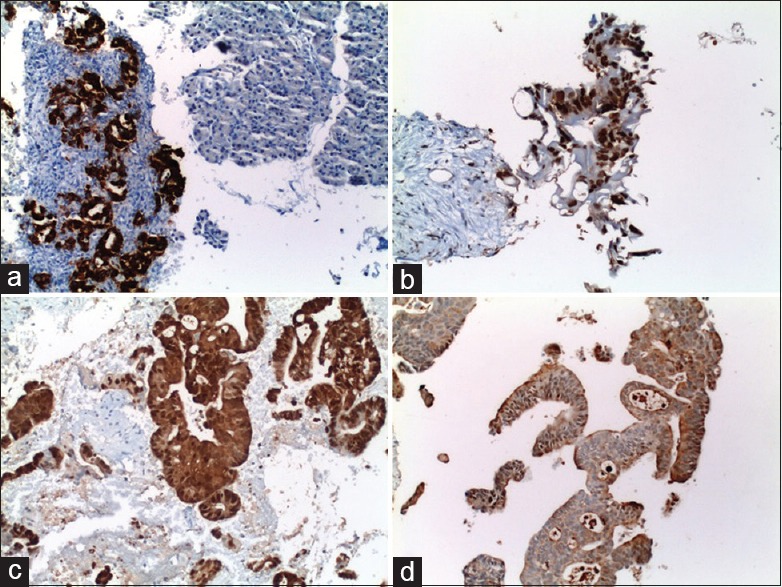
(a) H and E section of normal pancreatic tissue, (b) strong pVHL staining in normal pancreatic tissue, (c) H and E section of chronic pancreatitis, and (d) strong pVHL staining in chronic pancreatitis (a-c: H&E ×400, b-d: pVHL ×400)
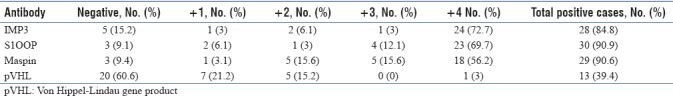
Table 2.
Summary of immunostaining results for IMP3, S100P, maspin, and pVHL in pancreatic ductal adenocarcinoma
Thirty cases (90.9%) of the PDAC showed positive staining with S100P, which were strong in 28 (93.3%) cases [Figure 2b]. Twenty-seven (90%) of these positive stained cases were diffuse as +3 or more, and 28 (93.3%) of these positive stained cases were diffuse as +2 or more [Table 2].
Maspin staining was observed in 29 of the 33 (90.6%) PDAC cases [Figure 2c]. All the staining were strong, and between these positive labeling cases, 23 (79.3%) cases were diffuse as +3 or more and 28 (96.6%) cases were diffuse as +2 or more [Table 2]. In contrast to PDAC cases, all the non-neoplastic pancreatic ducts were negative for IMP3, S100P, and maspin [Figure 2c, Table 3].
Table 3.
Summary of immunostaining results for IMP3, S100P, maspin, and pVHL in benign/reactive pancreatic epithelium
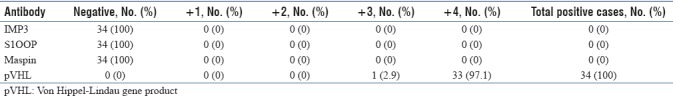
All the non-neoplastic pancreatic tissues were strongly and diffusely (+3 or more) positive with pVHL antibody [Figure 3]. pVHL was positive in 13 (39.4%) of the 33 PDAC cases [Figure 2d]. Most of these positive staining were focal (92.4%) and weak (76.9%) [Tables 2 and 3].
Figure 3.
(a) IMP3 (×400), (b) S100P (×400), (c) maspin (×400)staining of PDAC cases, and (d) focal and strong staining of pVHL in PDAC (×400)
Statistical analysis
IMP3, S100P, and maspin staining in PDAC cases were significantly different from non-neoplastic pancreatic tissue (P < 0.01). When 2+, 3+, and 4+ staining were considered as positive staining, sensitivity and specificity of IMP3, S100P, and maspin were high enough to detect PDAC (sensitivity 81.8%, 84.8%, 87.5% and specificity was 100% for all three markers). pVHL was observed to be very sensitive (100%) for detecting non-neoplastic pancreatic tissue. Some of the PDAC cases (13/39) were stained with pVHL (mostly focal and weak). Specificity of this marker for non-neoplastic pancreatic tissue was 81.8% [Table 4].
Table 4.
Sensitivity, specificity, accuracy, and positive and negative predictive values for IMP3, S100P, maspin, and pVHL
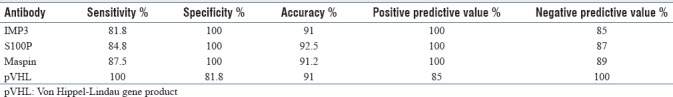
Test performance of possible antibody combinations was also evaluated. When maspin, IMP3, and S100P expression were used together as triple test, sensitivity was 62.5% and specificity 100%. However, when any two of each three markers were evaluated (triple test/dual response), sensitivity reached 93.8% and specificity 100%.
DISCUSSION
Recently, many biomarkers were investigated to decrease interobserver variability of interpretation of morphological assessment of pancreatic lesions. In this study, we arbitrarily categorized maspin, IMP3, and S100P as triple test. The results of this study demonstrate that dual response in triple test of maspin, IMP3, and S100P immunocytochemistry is sufficient to differentiate PDAC from benign mimickers. However, when triple assessment is not satisfactory, use of pVHL might be valuable.
PDAC is the fourth leading cause of cancer-related death worldwide.[14] In majority of the cases, PDAC is not curable by surgery and diagnosis has been made with FNAB or core needle biopsies.[2] Differentiation of PDAC from non-neoplastic pancreatic tissue in cytopathological assessment is not always straightforward. There are several reports that evaluate diagnostic value of cytological criteria in PDAC.[15,16] Despite these well-defined cytological criteria, false-negative rates, atypical, and suspicious diagnosis remain still high, especially when a PDAC was evaluated by a less experienced pathologists. To overcome this problem, several antibodies have been evaluated. There are several reports that interpret diagnostic value of S100P, maspin, pVHL, and IMP3 in the differential diagnosis of PDAC from normal/reactive pancreatic tissue. Studies that evaluate these antibodies in FNAB smears or cell blocks are limited to few.[3,7,8,9]
IMP3 is an oncofetal protein that belongs to insulin-like growth factor II mRNA binding protein (IMP). In adult tissues, IMP3 is expressed at low or undetectable levels[17,18] but in malignant tumors is over-expressed in stomach, colon, pancreas, lung, renal cell, and liver cancers.[18,19,20,21,22] Zhao et al. applied KOC (IMP3) to 48 alcohol-fixed, PAP-stained EUS-FNAB smears (40 PDAC and 8 benign cases) and reported KOC expression as 88% in PDAC and none of the benign cases.[7] Even though the size of their study is limited, it gives very important information that IMP3 can be evaluated on alcohol-fixed FNA smears.
S100P belongs to S100 family of calcium-binding protein and has been found to demonstrate increased level of expression during progression from pancreatic intraepithelial neoplasia to invasive adenocarcinoma.[23] To our best knowledge, the first study that evaluated diagnostic value of S100P in FNAB specimens of the pancreas was published in 2008.[8] They found positive staining with S100P antibody in all cases of PDAC and atypical or suspicious cases. Cases that were diagnosed as atypical or suspicious proved to be PDAC in surgical material.
Dim et al. studied five markers including S100P, prostate stem cell antigen, fascin, 14-3-3 sigma, and mesothelin in endoscopic ultrasound-guided FNAB of the pancreas to evaluate usefulness of these antibodies in differential diagnosis of PDAC and normal pancreatic tissue.[9] They reported S100P as the best diagnostic marker among five others, which represented 90% of sensitivity and 67% of specificity.[9]
In this study, when maspin, IMP3, and S100P expression were present, it was strongly evident in most of the cases (>90%). Sensitivity of S100P, IMP3, and maspin was 84.8%, 81.8%, and 87.5%, respectively. Specificity of these three markers was 100%. None of the non-neoplastic pancreatic tissue was stained with these antibodies. When any two of each three markers were evaluated (triple test/dual response), sensitivity reached 93.8% and specificity 100%. Whereas pVHL was positive in all non-neoplastic pancreatic tissue (100%), only 39.4% of PDAC cases (13 cases) have weak and focal expression. Nine of the 13 (69.2%) pVHL-positive PDAC cases were stained with all the other three markers. None of the pVHL-positive PDAC cases indicated negative staining with any of other three antibodies.
Liu et al. evaluated usefulness of 26 antibodies in the differential diagnosis of PDAC from non-neoplastic pancreatic tissue.[3] They also used maspin, S100P, IMP-3, and pVHL in 44 cases of PDAC from FNAB specimens on cell blocks. They reported high expression rate of maspin, S100P, and IMP-3 (100%, 100%, and 93% of cases). They did not find any staining in PDAC cases with pVHL. They claimed that pVHL, maspin, S100P, and IMP-3 were the best immunohistochemical markers for confirming the diagnosis of PDAC in both surgical and FNAB cell blocks. Maspin, IMP3, and S100P staining rates of this study are similar to our results. However, pVHL expression in PDAC is different than this study. In our study, we found pVHL to be positive in 39.4% of PDAC cases. To the best of our knowledge, Liu et al.'s study and our study are the only ones that evaluated these four antibodies together in FNAB material of PDAC.
There are some reports that evaluate S100P and pVHL in pancreatic intraepithelial neoplasia (PanIN) beside PDAC.[10] Lin et al. reported loss of pVHL and gain of S100P expression in PanINs and PDAC.[10] This finding should be a clue to early role of these markers in development of PanINs and progression from PanIN to PDAC.[10] One study that evaluated maspin in PDAC cases found maspin expression predominantly in low histological grade and this should be a clue to role of maspin in development and differentiation of PDAC.[11]
Some of these antibodies were also evaluated in other biliary tract carcinomas, such as hilar [hepatocellular carcinoma (HCC)] and intrahepatic cholangiocarcinomas (ICCs). S100P expression was found to have higher expression in PDAC than ICC. HCC and ICC did not show any significant difference for S100P expression.[12] Levy et al. evaluated S100P, pVHL, and IMP3 in adenocarcinomas of endoscopic bile duct biopsies. They reported that S100P and IMP3 positivity and pVHL-negative staining are useful to distinguish adenocarcinoma from reactive epithelium in challenging cases.[13]
In summary, S100P, maspin, pVHL, and IMP3 were surrogate biomarkers in the differential diagnosis of PDAC and from mimickers. Whereas S100P, IMP3, and maspin positivity support PDAC diagnosis, pVHL positivity supports benign lesions such as normal/chronic pancreatitis. For positive immunostaining profile of two or three of these markers, dual response in triple test (IMP3, S100P, maspin) is the most useful in distinction of PDAC from benign mimickers (sensitivity 93.8% and specificity 100%). Finally, after evaluating cytological criteria on a pancreatic FNAC, using IMP3, maspin, S100P, and pVHL to cell bock sections may reduce false-negative rates.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Campbell F, Verbeke CS. Pathology of the Pancreas: A Practical Approach. London: Springer; 2013. [Google Scholar]
- 2.Demay RM. Chapter 19 Pancreas. In: Demay RM, editor. The Art and Science of Cytopathology. 2nd ed. Chicago: ASCP Press; 2012. pp. 1297–343. [Google Scholar]
- 3.Liu H, Shi J, Anandan V, Wang HL, Diehl D, Blansfield J, et al. Reevaluation and identification of the best immunohistochemical panel (pVHL, maspin, S100P, IMP3) for ductal adenocarcinoma of the pancreas. Arch Pathol Lab Med. 2012;136:601–9. doi: 10.5858/arpa.2011-0326-OA. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy DM, Maitra A, Argani P, Rader AE, Faigel DO, Van Heek NT, et al. Novel markers of pancreatic adenocarcinoma in fine-needle aspiration: Mesothelin and prostate stem cell antigen labeling increases accuracy in cytologically borderline cases. Appl Immunohistoc Mol Morphol. 2003;11:238–43. doi: 10.1097/00129039-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Chhieng DC, Benson E, Eltoum I, Eloubeidi MA, Jhala N, Jhala D, et al. MUC1 and MUC2 expression in pancreatic ductal carcinoma obtained by fine-needle aspiration. Cancer. 2003;99:365–71. doi: 10.1002/cncr.11857. [DOI] [PubMed] [Google Scholar]
- 6.Yantiss RK, Woda BA, Fanger GR, Kalos M, Whalen GF, Tada H, et al. KOC (K homology domain containing protein overexpressed in cancer): A novel molecular marker that distinguishes between benign and malignant lesions of the pancreas. Am J Surg Pathol. 2005;29:188–95. doi: 10.1097/01.pas.0000149688.98333.54. [DOI] [PubMed] [Google Scholar]
- 7.Zhao H, Mandich D, Cartun RW, Ligato S. Expression of K homology domain containing protein overexpressed in cancer in pancreatic FNA for diagnosing adenocarcinoma of pancreas. Diagn Cytopathol. 2007;35:700–4. doi: 10.1002/dc.20739. [DOI] [PubMed] [Google Scholar]
- 8.Deng H, Shi J, Wilkerson M, Meschter S, Dupree W, Lin F. Usefulness of S100P in diagnosis of adenocacinoma of pancreas on fine-needle aspiration biopsy specimens. Am J Clin Pathol. 2008;129:81–8. doi: 10.1309/5D76NDE81LE8G545. [DOI] [PubMed] [Google Scholar]
- 9.Dim DC, Jiang F, Qiu Q, Li T, Darwin P, Rodgers WH, et al. The usefulness of S100P, mesothelin, fascin, prostate stem cell antigen, and 14-3-3 sigma in diagnosing pancreatic adenocarcinoma in cytological specimens obtained by endoscopic ultrasound guided fine-needle aspiration. Diagn Cytopathol. 2014;42:193–9. doi: 10.1002/dc.21684. [DOI] [PubMed] [Google Scholar]
- 10.Lin F, Shi J, Liu H, Hull ME, Dupree W, Prichard JW, et al. Diagnostic utility of S100P and von Hippel-Lindau gene product (pVHL) in pancreatic adenocarcinoma-with implication of their roles in early tumorigenesis. Am J Surg Pathol. 2008;32:78–91. doi: 10.1097/PAS.0b013e31815701d1. [DOI] [PubMed] [Google Scholar]
- 11.Ohike N, Maass N, Mundhenke C, Biallek M, Zhang M, Jonat W, et al. Clinicopathological significance and molecular regulation of maspin expression in ductal adenocarcinoma of the pancreas. Cancer Lett. 2003;199:193–200. doi: 10.1016/s0304-3835(03)00390-2. [DOI] [PubMed] [Google Scholar]
- 12.Gandou C, Harada K, Sato Y, Igarashi S, Sasaki M, Ikeda H, et al. Hilar cholangiocarcinoma and pancreatic ductal adenocarcinoma share similar histopathologies, immunophenotypes, and development-related molecules. Hum Pathol. 2013;44:811–21. doi: 10.1016/j.humpath.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Levy M, Lin F, Xu H, Dhall D, Spaulding BO, Wang HL. S100P, von Hippel-Lindau gene product, and IMP3 serve as a useful immunohistochemical panel in the diagnosis of adenocarcinoma on endoscopic bile duct biopsy. Hum Pathol. 2010;41:1210–9. doi: 10.1016/j.humpath.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 14.Yadav D, Lowenfels A. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–61. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen MB, Egerter DP, Holly EA, Ahn DK, Miller TR. Pancreatic adenocarcinoma: Regression analysis to identify improved cytologic criteria. Diagn Cytopathol. 1991;7:341–5. doi: 10.1002/dc.2840070404. [DOI] [PubMed] [Google Scholar]
- 16.Robins DB, Katz RL, Evans DB, Atkinson EN, Green L. Fine needle aspiration of the pancreas. In quest of accuracy. Acta Cytol. 1995;39:1–10. [PubMed] [Google Scholar]
- 17.Mueller-Pillasch F, Pohl B, Wilda M, Lacher U, Beil M, Wallrapp C, et al. Expression of the highly conserved RNA binding protein KOC in embryogenesis. Mech Dev. 1999;88:95–9. doi: 10.1016/s0925-4773(99)00160-4. [DOI] [PubMed] [Google Scholar]
- 18.Mueller-Pillasch F, Lacher U, Wallrapp C, Micha A, Zimmerhackl F, Hameister H, et al. Cloning of a gene highly overexpressed in cancer coding for a novel KH-domain containing protein. Oncogene. 1997;14:2729–33. doi: 10.1038/sj.onc.1201110. [DOI] [PubMed] [Google Scholar]
- 19.Nielson J, Christiansen J, Lykke-Andersen J, Johnsen AH, Wewer UM, Nielson FC. A family of insulin-like growth factor II mRNA-binding proteins represses translation in late development. Mol Cell Biol. 1999;19:1262–70. doi: 10.1128/mcb.19.2.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yantiss RK, Woda BA, Fanger GR, Kalos M, Whalen GF, Tada H, et al. KOC (K homology domain containing protein overexpressed in cancer): A novel marker that distinguishes between benign ad malignant lesions of the pancreas. Am J Surg Pathol. 2005;29:188–95. doi: 10.1097/01.pas.0000149688.98333.54. [DOI] [PubMed] [Google Scholar]
- 21.Jiang Z, Lohse CM, Chu PG, Wu CL, Woda BA, Rock KL, et al. Oncofetal protein IMP3: A novel molecular marker that predicts metastases of papillary and chromophobe renal cell carcinomas. Cancer. 2008;112:2676–82. doi: 10.1002/cncr.23484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeng YM, Chang CC, Hu FC, Chou HY, Kao HL, Wang TH, et al. RNA-binding protein insulin like growth factor II mRNA-binding protein 3 expression promotes tumor invasion and predicts early recurrence and poor prognosis in hepatocellular carcinoma. Hepatology. 2008;48:1118–27. doi: 10.1002/hep.22459. [DOI] [PubMed] [Google Scholar]
- 23.Dowen SE, Crnogorac-Jurcevic T, Gangeswaran R, Hansen M, Eloranta JJ, Bhakta V, et al. Expression of S100P and its novel binding partner S100PBPR in early pancreatic cancer. Am J Pathol. 2005;166:81–92. doi: 10.1016/S0002-9440(10)62234-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


