Summary
Background
As countries embark on public health-oriented drug law reform, health impact evaluations are needed. In 2012, Mexico mandated the narcomenudeo reform, which depenalised the possession of small amounts of drugs and instituted drug treatment instead of incarceration. We investigated the past and future effect of this drug law reform on HIV incidence in people who inject drugs in Tijuana, Mexico.
Methods
In this epidemic modelling study, we used data from the El Cuete IV cohort study to develop a deterministic model of injecting and sexual HIV transmission in people who inject drugs in Tijuana between 2012 and 2030. The population was stratified by sex, incarceration status, syringe confiscation by the police, HIV stage, and exposure to drug treatment or rehabilitation (either opioid agonist treatment or compulsory drug abstinence programmes). We modelled the effect of these exposures on HIV risk in people who inject drugs, estimating the effect of observed and potential future reform enforcement levels.
Findings
In 2011, prior to the narcomenudeo reform, 547 (75%) of 733 people who inject drugs in the El Cuete cohort reported having ever been incarcerated, on average five times since starting injecting. Modelling estimated the limited reform implementation averted 2% (95% CI 0·2–3·0) of new HIV infections in people who inject drugs between 2012 and 2017. If implementation reduced incarceration in people who inject drugs by 80% from 2018 onward, 9% (95% CI 4–16) of new HIV infections between 2018 and 2030 could be averted, with 21% (10–33) averted if people who inject drugs were referred to opioid agonist treatment instead of being incarcerated. Referral to compulsory drug abstinence programmes instead of prison could have a lower or potentially negative impact with −2% (95% CI −23 to 9) infections averted.
Interpretation
Mexican drug law reform has had a negligible effect on the HIV epidemic among people who inject drugs in Tijuana. However, appropriate implementation could markedly reduce HIV incidence if linked to opioid agonist treatment. Unfortunately, compulsory drug abstinence programmes are the main type of drug rehabilitation available and their expansion could potentially increase HIV transmission.
Introduction
Public health-oriented drug law reforms were implemented in the late 1990s and early 2000s in the Netherlands, Portugal, and Switzerland, and are currently being implemented in several countries including Mexico, Brazil, Paraguay, Uruguay, Colombia, Malaysia, Canada, and some US states.1 This move follows mounting evidence that criminalisation fails to reduce drug use, while fuelling crime, violence, and negative health outcomes at substantial economic cost.2 The harms of punitive drug policies disproportionately affect people who inject drugs. Incarceration and the period post-release have been associated with HIV, tuberculosis, hepatitis B and C, overdose, and mental health disorders in people who inject drugs.3 Additionally, policing practices including arrest, extortion, and syringe confiscation have been associated with increased risk of blood-borne infection transmission in people who inject drugs.4,5
Studies of the effect of drug law reforms on the health of people who inject drugs are needed, but very few assessments have been done in Latin America and other low-income and middle-income settings, despite growing momentum for such reforms.5 However, druglaw reforms are complex structural interventions for which evaluation through community randomised controlled trials might be legally, ethically, or logistically difficult or unfeasible.6 Epidemic modelling is a useful method to address this limitation because it allows simulating control scenarios accounting for demographic and epidemic dynamics through time.7 Three modelling studies have assessed the contribution of incarceration to HIV, hepatitis C, and tuberculosis epidemics in people who inject drugs, but none have evaluated the effect of drug law reform on disease incidence.2,8,9
In 2009, Mexico enacted drug and health law reforms (referred to as the narcomenudeo reform hereafter), which depenalised possession of small amounts of selected drugs for personal consumption (appendix p 1) and mandated drug treatment on the third apprehension under drug possession thresholds instead of incarceration.10 The northwest state of Baja California became subject to the full enforcement of the narcomenudeo reform in 2012. The state has the highest prevalence of past-year illicit drug use (4·4% vs 2·7% at the national level)11 and its largest city, Tijuana, on the Mexico–US border has an estimated 10 000 people who inject drugs.12 HIV prevalence in people who inject drugs was 3·5% in 2011, and incidence was 1·1 per 100 personyears between 2011 and 2017.13 As recorded in other settings, people who inject drugs in Tijuana are often incarcerated or harassed by the police (eg, via syringe confiscation),13 exposures associated with receptive needle sharing.4,14 The narcomenudeo reform has the potential to reduce incarceration in people who inject drugs, and therefore prevent HIV transmission.
However, findings of early studies indicated little knowledge about the reform among the Tijuana police.15 Affordable and quality evidence-based drug treatment services were scarce, and in 2014, government funds were allocated to compulsory drug abstinence programmes.16 In Tijuana, these entail physically restraining individuals, brought involuntarily by family, friends or the police, in non-medically supervised centres over 3–6 months and subjecting them to non-evidence based interventions, often involving punishment, to achieve detoxification and abstinence.17 Given these contextual circumstances, the effect of the narcomenudeo reform implementation on the HIV epidemic in Tijuana is unclear.
In 2011, the El Cuete IV cohort study18 recruited 734 people who inject drugs through convenience sampling and has since provided biannual quantitative and periodic qualitative information about HIV, risk behaviours, and exposures to policing, incarceration, and harm reduction services in people who inject drugs (appendix p 1). It was designed to monitor and assess the effect of the drug law reform on these structural exposures in people who inject drugs, and provides a unique opportunity to inform an epidemic model to estimate its effect on HIV incidence.
This epidemic modelling study, in which we used data from the El Cuete IV study to assess the past and future effect of the narcomenudeo reform on HIV incidence in people who inject drugs in Tijuana, should serve as a case study to guide effective reform implementation in Mexico and other settings.
Methods
Epidemic model structure
We developed a dynamic deterministic compartmental model of injecting and sexual HIV transmission in people who inject drugs, including incarceration and police harassment (via syringe confiscation; figure 1). The population was stratified by sex, incarceration stage, exposure to syringe confiscation in the past 6 months, and HIV stage (figure 1). We neglected ART because coverage was less than 1% in HIV-infected people who inject drugs in Tijuana. The model was additionally stratified by exposure to drug treatment or rehabilitation (either opioid agonist treatment or compulsory drug abstinence programmes). Injecting and sexual transmission were represented through a system of coupled ordinary differential equations as functions of the number of syringe sharing events or sex acts, the probability of transmission through syringe sharing or by sex act and the HIV prevalence and HIV stage in partners. Syringe sharing contacts were assumed to follow random mixing. Sexual contacts were assumed to be exclusively heterosexual and shared between people who inject drugs and non-injecting partners. Differences in number of sex acts and condom use with stable, casual, and commercial partners were represented. A relative risk of HIV infection through injecting in people who inject drugs exposed to recent syringe confiscation, compulsory drug abstinence programmes, opioid agonist treatment and recent incarceration was applied to reflect their effect on the frequency of receptive sharing events, based on data described in the next section (appendix p 5).
Figure 1: Disaggregation of the people who inject drugs population.
By (A) sex, (B) incarceration, (C) syringe confiscation, and (D) HIV status, and the flows and corresponding rates between states within each model dimension, and (E) OAT or CAP to which people who inject drugs are diverted to instead of incarceration under different enforcement scenarios of the Narcomenudeo reform as indicated by the red shading. OAT=opioid agonist treatment. CAP=compulsory abstinence programme. *In prison, no syringe confiscation by the police occurs because there is no interaction with the police and there is no access to either OAT or CAPs.
HIV co-infection models (in which the co-infection was transmitted only via sexual or injecting routes) have been successfully used to distinguish the relative contribution of sexual versus injecting risk on HIV in people who injected drugs. Therefore, to more accurately estimate the potential effect of interventions addressing injecting transmission, we also estimated the contribution of sexual transmission to HIV incidence using a simplified model of HIV and syphilis co-infection (appendix pp 16–19).
Epidemic model parameterisation and calibration
The model was parameterised using demographic and HIV risk behaviour data from El Cuete IV and calibrated to HIV incidence and prevalence data by sex and incarceration history in people who inject drugs in Tijuana from 2005–15 (table 1). We used data from El Cuete IV to parameterise temporal trends in exposure to incarceration and police (recent [<6 months] incarceration, recent [<6 months] syringe confiscation by the police). Additional prison demography parameters were estimated using a simplified cohort model calibrated to incarceration data from El Cuete IV (appendix pp 10, 11). The relative risk of receptive syringe sharing associated with these exposures was also estimated from El Cuete IV baseline (appendix p 5). Because we found no association between exposure to recent syringe confiscation and incarceration, or effect on receptive syringe sharing, we assumed these mechanisms operated independently. We also assessed temporal trends in current opioid agonist treatment use (yes or no) and recent (<6 months) exposure to compulsory drug abstinence programmes, as these are potentially related to the narcomenudeo reform provision for drug treatment. Because the proportion exposed to recent compulsory drug abstinence programmes was very low at baseline (<2%), we examined the potential association between ever exposure to compulsory drug abstinence programmes and receptive syringe sharing at baseline. Similarly, because the proportion on opioid agonist treatment was very low at baseline (3%), we used data from an international meta-analysis19 to parameterise the effect of this treatment on HIV risk. To account for parameter uncertainty, we sampled parameters from assigned prior distributions using Latin Hypercube Sampling (table 2). 120 000 parameter sets were sampled and 204 selected runs producing a log likelihood above the 99th percentile were used for the final analyses. Most of these runs lay between the 95% confidence Intervals (95% CI) of the data (appendix pp 14, 15).
Table 1:
Key model parameters associated with incarceration and police harassment
| Point estimate (sampled range) |
Sampling distribution |
Source | ||
|---|---|---|---|---|
| Men | Women | |||
| Demographic | ||||
| Rate of exposure to syringe confiscation in past 6 months at baseline (per year) | 0·26 (0·16–0·36) | 0·23 (0·13–0·33) | Beta | El Cuete IV13 |
| Rate of exiting prison among people who inject drugs incarcerated in the past 6 months at baseline (per year) | 3·1 (0–7) | 2·9 (0–7) | Truncated normal | El Cuete IV13 |
| Proportion of people who inject drugs incarcerated before starting injecting | 82% (79–92) | 33% (19–61) | Fitted values | Fitted to El Cuete data using cohort model (appendix) |
| Primary incarceration rate (per year) | 0·018(0–0·047) | 0·034 (0·001–0·055) | Fitted values | Fitted to El Cuete data using cohort model (appendix) |
| Reincarceration rate (per year) | 0·27 (0·80–0·46) | 0·20 (0·03–0·40) | Truncated normal | El Cuete IV13 |
| Behavioural | ||||
| Relative change in proportion reporting recent receptive syringe sharing among recently released from prison vs never or not recently incarcerated | 1·30 (1·15–1·46)* | 1·30 (1·15–1·46)* | Log-normal | El Cuete IV13 |
| Relative change in proportion reporting recent receptive syringe sharing among recently exposed vs not recently exposed to syringe confiscation by the police | 1·16 (1·03–1·29)* | 1·16 (1·03–1·29)* | Log-normal | El Cuete IV13 |
| Relative change in proportion reporting recent receptive syringe sharing among people who inject drugs ever vs never exposed to CAP | 1·14 (1·00–1·30)* | 1·14 (1·00–1·30)* | Log-normal | El Cuete IV13 |
| Relative risk of injecting HIV acquisition among people who inject drugs on OAT compared to no OAT | 0·46 (0·32–0·67) | 0·46 (0·32–0·67) | Log-normal | MacArthur et al19 |
| Rate of OAT cessation (per year) | 1 | 1 | Fixed | Bukten et al,20 Martin et al21 |
Data are mean (95% CI). Parameters were allowed to vary within the 95% CI shown in brackets. Additional detail on El Cuete IV data is provided in the appendix.
LLK=log-likelihood. CAP=compulsory abstinence programme. OAT=opioid agonist treatment.
Adjusted for duration of injection.
Table 2:
Data used to calibrate the model
| Point estimate (95%CI) |
Distribution used for LLK calculation |
Source | ||
|---|---|---|---|---|
| Men | Women | |||
| HIV prevalence among people who inject drugs in 2005 | 2·3% (1–5·3) | 2·3% (1–5·3) | Beta | Frost et al22 |
| HIV prevalence among people who inject drugs in 2006 | 2·4% (1·3–3.6) | 5·4% (1·5–7·8) | Beta | Strathdee et al23 |
| HIV prevalence among ever incarcerated people who inject drugs in 2011 | 3·5% (1·7–5·4) | 5·2% (1·7–8·8) | Beta | El Cuete IV13 |
| Relative HIV prevalence among ever versus never incarcerated people who inject drugs in 2011 | 1·1 (0·3–4·7) | 3·2 (0·7–15) | Normal | El Cuete IV13 |
| HIV incidence among people who inject drugs in 2015 (per 100 person-years) | 0·5 (0·06–0·9) | 1·1 (0·3–1·8) | Poisson | El Cuete IV13 |
| Proportion of new infections attributable to sexual transmission in 2006 | 0·45 (0·30–0·60) | 0·45 (0·30–0·60) | Normal | HIV/syphilis model (appendix) |
Data are mean (95% CI). Parameters were allowed to vary within the 95% CI shown in brackets. Additional detail on El Cuete IV data is provided in the appendix. LLK=log-likelihood.
Adjusted for duration of injection.
The UCSD and Colegio de la Frontera Norte boards approved El Cuete IV, and all participants provided written informed consent.
Epidemic modelling analyses
To assess the contribution of incarceration and syringe confiscation to the HIV epidemic in people who inject drugs with no drug law reform (2012–30), we modelled a baseline scenario with no change in incarceration or syringe confiscation from 2012 (mandated start of the reform). In view of the low proportion on ART (<1%), opioid agonist treatment (3%) and recent compulsory drug abstinence programmes (<2%) at baseline, we assumed no coverage of these for the baseline scenario.
To estimate the population attributable fraction of potential modifiable variables associated with the narcomenudeo reform, we assessed the population attributable fraction of incarceration and syringe confiscation from 2012 until 2030. This was implemented by setting incarceration rates to zero and eliminating the increased risk in people who inject drugs recently incarcerated and recently exposed to syringe confiscation. We calculated the relative reduction in the number of new infections between 2012 and 2030 in this scenario compared to the baseline scenario. Additionally, we investigated the population attributable fraction of recent incarceration and syringe confiscation in isolation.
To estimate the potential interim effect of the limited enforcement of the narcomenudeo reform up to now (2012–17), we modelled observed changes in policing (ie, syringe confiscation) and recent incarceration since the mandated narcomenudeo reform enforcement in 2012 in people who inject drugs in the El Cuete cohort. We estimated the number of new infections prevented between 2012 and 2017 compared with the baseline scenario.
It is uncertain how full implementation of the narcomenudeo reform could affect the incarceration of people who inject drugs, but in 2011, 80% of incarcerations in the past 6 months were due to possessing drugs or minor infractions associated with drug use.13 To estimate the potential future effect of the narcomenudeo reform on the HIV epidemic in people who inject drugs under different degrees of implementation from 2018 to 2030, we modelled four scenarios that incorporated observed changes in recent incarceration and syringe confiscation over 2012 to 2017, assuming these remained stable thereafter. The scenarios explored assumed: first, no additional changes; second, 80% reduction in incarceration rates in people who inject drugs in a limited enforcement scenario; third, opioid agonist treatment instead of incarceration for drug-related crimes (80% of incarcerations), assuming a 53% (95% CI 33–68) reduction in injecting-related HIV acquisition risk on opioid agonist treatment for 1 year on average; and finally, compulsory drug abstinence programmes instead of incarceration for drug-related crimes (80% of incarcerations; table 1, appendix).
Sensitivity analyses exploring a lower reduction in incarceration (and associated diversion to opioid agonist treatment or compulsory drug abstinence programmes) and longer or shorter duration on opioid agonist treatment were implemented.
For statistical and epidemic modelling analyses, we used SAS (version 9.4) and Matlab R2015b, respectively.
Results
In 2011, before the narcomenudeo reform, 547 (75%) of 733 people who inject drugs in the El Cuete cohort in Tijuana reported having ever been incarcerated, on average five times since starting injecting drugs. People who inject drugs recently incarcerated (past 6 months) had a relative risk of 1·30 (95% CI 1·15–1·46) of receptive syringe sharing compared with those never or not recently incarcerated, adjusting for duration of injection (table 1). Although the proportion of people who inject drugs reporting recent incarceration fluctuated around an average of 5·8% between 2013 and 2016, no trend was observed over time (appendix pp 2–5). In 2011, nearly 11% of people who inject drugs reported having syringes confiscated by police in the past 6 months, an experience associated with a 1·16 (95% CI 1·03–1·29) relative risk of receptive syringe sharing, compared with those not recently exposed, adjusting for duration of injection (table 1). A decrease in exposure to recent syringe confiscation was recorded between 2012 and 2013 and continued to reach 0% by 2015 (appendix pp 2, 3).
Levels of drug treatment were low and remained negligible between 2011 and 2016. The proportion of people who inject drugs on opioid agonist treatment was 3·1% in 2011, and remained low over time (2·2% in 2016). Only 1·4% of people who inject drugs reported exposure to compulsory drug abstinence programmes in the past 6 months in 2011. Although there were spikes (up to 5%) in the proportion of people who inject drugs reporting recent exposure in 2015 and 2016, no trend could be confirmed so it is unclear whether the reform led to a consistent rise in exposure. In 2011, 10·3% of people who inject drugs reported ever exposure to compulsory drug abstinence programmes, which was associated with a 1·14 (95% CI 1·00–1·30) relative risk of receptive syringe sharing compared with those never exposed, adjusting for duration of injection.
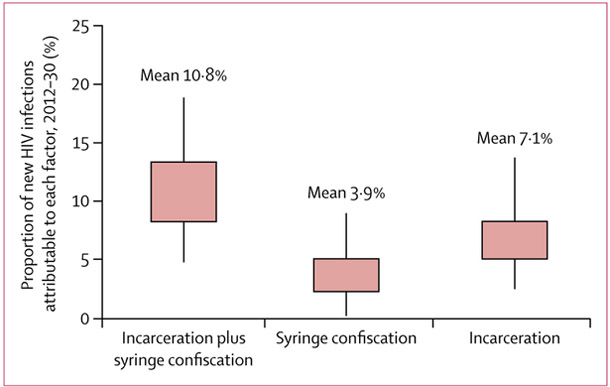
Using these findings, modelling suggested that in the absence of the narcomenudeo reform from 2012 to 2030, 10·8% (95% CI 4·8–18·9) of the estimated 1715 (699–3108) new HIV infections in people who inject drugs could be attributed to incarceration and syringe confiscation, corres-ponding to 192 (95% CI 42–464) new infections (figure 2). Incarceration alone could contribute 7·1% (95% CI 2·5–13·8) of new infections, whereas syringe confiscation alone could contribute 3·9% (0·2–9·0) of new infections.
Figure 2: Model projections of HIV infections attributable to incarceration and syringe confiscation in people who inject drugs in Tijuana from 2012–30.
Boxes represent the 25–75% range, whiskers represent the 2·5–97·5% CI of model projections.
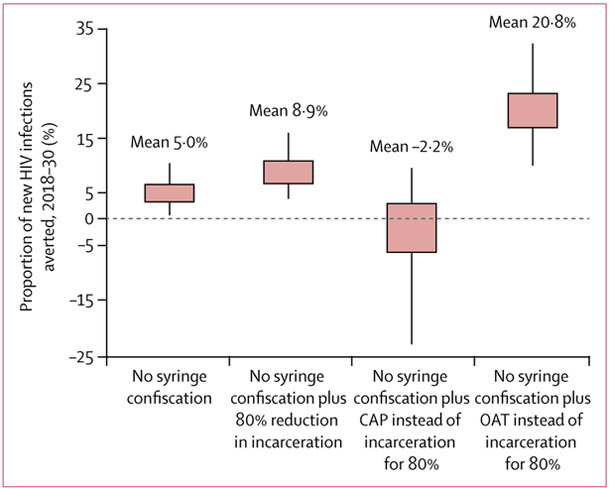
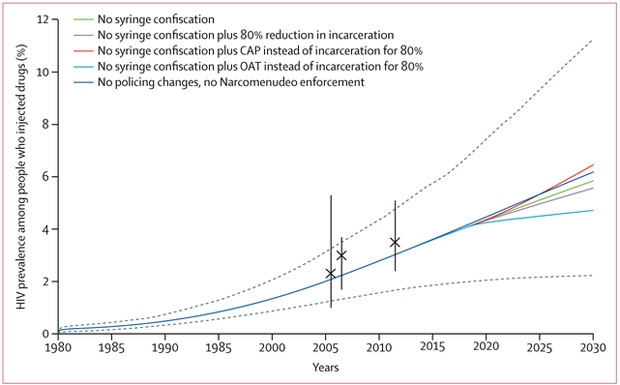
The small observed changes in policing experienced by people who inject drugs since the narcomenudeo reform in 2012 (no incarceration changes, but decrease in exposure to recent syringe confiscation by police) has probably resulted in a small decrease in HIV incidence, averting 1·6% (95% CI 0·2–3·3) of new HIV infections in people who inject drugs over this period (2012–17). If syringe confiscation is kept at zero but no additional changes in narcomenudeo reform implementation occur, 5·0% (95% CI 0·7–10·4) of the estimated 1253 (481–2358) new HIV infections could be averted from 2018 to 2030 compared with no reform (figures 3, 4).
Figure 3: Model projections of the proportion of new HIV infections averted among people who inject drugs in Tijuana from 2018–30 assuming different enforcement of the Narcomenudeo reform.
Boxes represent the 25–75% range, whiskers represent the 2·5–97·5% CI of model projections. CAP=compulsory abstinence programme. OAT=opioid abstinence treatment.
Figure 4: HIV prevalence among people who inject drugs in Tijuana at baseline (assuming no changes in policing or implementation of the Narcomenudeo reform) and different degrees of implementation of the Narcomenudeo reform from 2018 onwards.
Black crosses and whiskers are mean and 95% CI from El Cuete II, III, and IV. Solid lines show the mean model trajectory for each scenario. The solid blue line shows the model projection with no policing changes, dashed grey lines show the 95% CI trajectories for this scenario. CAP=compulsory abstinence programme. OAT=opioid abstinence treatment.
If the incarceration rate of people who inject drugs is reduced by 80% from 2018 in addition to continued elimination of syringe confiscation by police as recorded so far, then 8·9% (95% CI 3·8–16·0) of new infections could be averted from 2018 to 2030 compared with no reform (figures 2, 3). Additionally, if people who inject drugs who would have been incarcerated were referred to evidence-based opioid agonist treatment services, 20·8% (95% CI 9·9–32·5) of new infections could be averted (figure 3, 4).
Improper reform implementation could limit effect or perhaps even cause harm. Modelling predicts that if people who inject drugs were sent to compulsory drug abstinence programmes instead of prison, this could potentially result in more HIV infections compared with no reform (−2·2% infections averted from 2018 to 2030 [95% CI −23·2 to 9·5]) and be accompanied by a rise in HIV prevalence (figure 4).
Findings of sensitivity analyses showed that while the magnitude of the association varies with lower reductions in incarceration and lower or higher opioid agonist treatment duration, results do not change qualitatively (appendix p 22).
Discussion
As drug policy reform gathers momentum, rigorous scientific studies are necessary to assess the public health impact of these structural interventions and to improve implementation. Our epidemic modelling study is unique in that it quantifies the effect of drug-law reform on HIV transmission in people who inject drugs. We show that syringe confiscation and incarceration could contribute to more than 10% of new infections in people who inject drugs in Tijuana between 2012 and 2030 and that observed reductions in syringe confiscation between 2012 and 2017 have only prevented a small proportion of new infections. Substantial reductions in incarceration (80%) could prevent nearly one in ten new infections over the next 12 years (2018–30) and this would increase to one in five new infections if opioid agonist treatment was provided to people who inject drugs who would otherwise be incarcerated. Appropriately enforced reform could therefore have a substantial effect on the epidemic. These findings, while unique in terms of assessing drug law reform impact, support previous modelling studies indicating that reductions in incarceration could reduce HIV and hepatitis C transmission in people who inject drugs.2,8,9 The narcomenudeo reform in Mexico carries the potential to address structural factors in people who inject drugs that increase their HIV risk. Unfortunately, stark discrepancies between written laws and policing practices in Tijuana have translated into minimal benefits, and potential harms.
Our findings show that if people who inject drugs were instead referred to compulsory drug-abstinence programmes, the main drug-rehabilitation programme available in Tijuana, the effect would be smaller and the number of new HIV infections could rise. The main concern with compulsory treatment is the potential effect of coercion on patients’ wellbeing and treatment success. In Tijuana, this is compounded by the lack of legal specification regarding the type of mandated drug treatment. Indeed, interviews in people who inject drugs in Tijuana found that none of the compulsory drug abstinence programme referrals were legal, and they often involved police abuse and were associated with traumatic experiences (appendix pp 22, 23).24 Increases in syringe sharing in those exposed to compulsory drug-abstinence programmes could be the result of poor mental health and low self-care after psychological or physical abuses in these centres. Compulsory drug-abstinence programmes exposure in people who inject drugs in Tijuana was also associated with non-fatal overdoses.17 Similarly, studies in China and Thailand found positive associations between exposure to compulsory drug abstinence programmes and drug paraphernalia sharing25 and avoidance of health care,26 respectively. By contrast, in settings such as Portugal, referral to treatment is recommended but only imposed on a case-by-case basis.27
Poor knowledge of the reform and drug laws in Tijuana police posed a substantial barrier to reform enforcement. In 2015, less than one in ten police officers correctly identified the possession threshold for heroin,28 just over half correctly recognised syringes to be legal, and twothirds reported making at least one arrest for syringe possession in the past 6 months. During interviews with high-level police, public health, and drug treatment sector officials, participants expressed confusion about the reform,29 and typically identified mass-media as their source of information. No action was taken to develop, disseminate or implement reform operating procedures (appendix pp 22, 23).29 Between 2015 and 2016, Proyecto Escudo, a novel police education programme framed as occupational health training, was implemented to assist the enforcement of the narcomenudeo reform by shifting police knowledge, attitudes, and practices targeting people who inject drugs thereby promoting police-public health collaboration.15 Preliminary findings suggest improved understanding of the legal status of syringe, heroin, and marijuana possession, along with better attitudes about public health-driven drug law reform.28,30 Future work should assess the effect of this police education programme on HIV transmission in people who inject drugs.
Although the promise of police education is encouraging, numerous barriers to reform implementation exist, including conflict between the narcomenudeo’s provisions on drugs and the local ordinance prohibiting their public consumption or, ambiguously, any deviant behaviour. A spectrum of minor infractions, such as sleeping in public, loitering, or failure to produce identification are punishable. In addition, while the narcomenudeo reform depenalises drug possession under a threshold, it allows detention (up to 48 h) until determination that the amount was below thresholds. These thresholds are very low compared with those established in other settings such as Portugal, which allow for the possession of quantities corresponding to 10 days of personal consumption. Given police incentives are based on metrics such as numbers of arrests made, these are unlikely to decrease.
Another barrier is the lack of affordable and quality drug treatment in Tijuana. Only three evidence-based outpatient opioid agonist treatment providers (total capacity 800 patients, only 150 subsidised) and one public inpatient centre (30 patients capacity) currently operate.31 These providers charge USD$75–250 per month for opioid agonist treatment, unaffordable for most people who inject drugs, 75% of whom earn below $200 per month.13 While expansion of opioid agonist treatment could have synergistic effects on HIV treatment, such as improving ART retention and adherence, access to HIV services is virtually missing for people who inject drugs in Tijuana. Hence, integration of drug treatment and HIV services is unfortunately unlikely to be achieved at present.
As with other modelling studies, our analysis is limited by uncertainty in the underlying data. First, the model parameterisation relies partly on self-reported behaviours in people who inject drugs subject to social desirability bias and recall imprecision. However, the El Cuete IV team is highly experienced at interviewing people who inject drugs and has developed a trusting relationship with the community, so we expect these to be minimised. Second, we relied on the model’s capacity to capture HIV transmission and incarceration dynamics in this population. We modelled multiple epidemic trajectories that fit to these data and represented uncertainty in our findings. We note that we sampled from a wide range of parameter values, and despite obtaining a relatively low number of fits (n=204), diverse epidemic trajectories were simulated propagating underlying parameter uncertainty. Third, our analysis focused on two exposures (incarceration and syringe confiscation) associated with receptive syringe sharing and potentially associated with the narcomenudeo reform. As such, the contribution of police or criminal justice exposures was potentially underestimated as people who inject drugs report multiple forms of police harassment, including bribery, beatings and sexual coercion,32 which might be associated with HIV risk. Similarly, people who inject drugs reported short-term detention, which remains legal under the narcomenudeo reform, and which could increase HIV risk. Future work should quantify the effect of these exposures on HIV, and potential for additional reforms to reduce them. Fourth, despite observed associations between incarceration and policing and syringe sharing, causality still needs to be established. Longitudinal analyses examining changes in individual risk before, during, and after incarceration and before and after police harassment will clarify the mechanisms through which these exposures directly or indirectly affect risk behaviour. Fifth, we did not study the effect of the reform on other health outcomes in people who inject drugs or the broader population. Future studies could incorporate the potential effect on sexual partners of people who inject drugs (not injecting themselves) or other outcomes such as transmission of hepatitis C and tuberculosis. We also did not examine the cost-effectiveness of the narcomenudeo reform. The costs and benefits will be multisectoral, affecting security and health expenditure, economic productivity and criminal victimisation. While estimating these costs was outside the scope of this paper, we discuss key elements and data required for an analysis in Tijuana (appendix pp 24–28).
In conclusion, our findings show that in the absence of a clear implementation strategy at the law enforcement (police reform) and health system (evidence-based drug treatment programmes) levels, inadequately or improperly implemented drug law reform will have minimal or negative public health effects. Our study therefore serves as a call to action to countries reforming their drug policies to implement monitoring, evaluation, and alignment of drug treatment with international standards. Indeed, modelling studies such as ours provide a useful tool to assess the effect of drug law reform on disease epidemics in Mexico and other countries. Further, our study supports the need to explore partnerships between the objectives of the security sector and the imperatives of public health.
Supplementary Material
Research in context
Evidence before this study
We reviewed the published literature on epidemic modelling of drug policy impact on health by searching PubMed on Jan 10, 2018, using the following search terms: (“drug* policy” OR “drug* policies” OR “drug* law*” OR “criminalization” OR “decriminalization” OR “incarceration” OR “prison”) AND (“health” OR “HIV” OR “HCV” OR “hepatitis” OR “tuberculosis” OR “Tuberculosis” OR “disease”) AND (“Model*”). We also searched for related articles in the references of selected articles. We did not apply restrictions by language or date of publication. Numerous studies modelled disease transmission (such as HIV, hepatitis B and C, or tuberculosis) within prison or in people who inject drugs. Three modelling studies explored the hypothetical effect of reduced incarceration on HIV and HCV epidemics in people who inject drugs, but were focused on settings without drug law reform (Altice, 2016; Csete, 2016; and Stone, 2017).
Added value of this study
To our knowledge, our epidemic modelling study is the first to assess the effect of a documented drug law reform on HIV incidence in people who inject drugs. It capitalises on data from a cohort study designed to investigate the effect of the Mexican drug law reform on HIV risk in people who inject drugs in Tijuana, the city with the highest estimated number of people who inject drugs in Mexico. The reform allows for the possession of selected drugs for personal consumption and mandates drug treatment at the third apprehension. Our findings suggest that, so far, the reform has only had a minor effect on HIV incidence because of its limited implementation. However, if properly implemented—such that 80% of people who inject drugs who would have been incarcerated received opioid agonist treatment instead—HIV incidence could be reduced by 21% (95% CI 10–33) between 2018 and 2030. Furthermore, less impact, or even harm, could occur if people who inject drugs were instead referred to compulsory drug abstinence programmes, the main type of drug rehabilitation available in Tijuana.
Implications of all the available evidence
Epidemic modelling, informed by longitudinal studies monitoring policing and incarceration exposures among people who inject drugs and associated risk, supports rigorous evaluations of the effect of drug law reforms on disease epidemics. Appropriately implemented drug law reform leading to reduced incarceration and referral to opioid agonist treatment could prevent HIV and related epidemics among people who inject drugs in Tijuana. This study is highly relevant to other cities in Mexico and Latin America that have HIV epidemics among people who inject drugs, as the rule of law is often weak across the region, hampering reform enforcement, and compulsory abstinence programmes are the main type of drug rehabilitation available and can cause harm.
Acknowledgments
This study was supported by grants from the National Institute on Drug Abuse (R01DA037773, R37DA019829, K01DA04342102 and R01DA039073) and by the University of California, San Diego, Center for AIDS Research (CFAR), an NIH-funded programme (P30 AI036214), which is supported by the following NIH Institutes and Centers: NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, and NIDDK. AB was funded by NIDA US–Mexico drug abuse prevention research fellowship, the UC MEXUS CONACyT postdoctoral fellowship and the UCSD CFAR grant NIAID P30 AI036214. BN was funded by the NIH grant R01-DA-041747. CR was supported by UC-MEXUS/CONACyT scholarship 209407/313533, UC MEXUS Dissertation Grant DI 15–42, Fogarty International Center D43TW008633. PV was also funded by the UK NIHR funded Health Protection Research Unit in the Evaluation of Interventions. Support was also provided by the Global Fund to Fight HIV, Tuberculosis and Malaria. We are grateful to the El Cuete IV participants and team for their time and effort to generate these data. We also thank Cassandra Cyr for her help with the literature review.
Funding National Institute on Drug Abuse, UC San Diego Center for AIDS Research.
Footnotes
Declaration of interests
PV and NKM have received unrestricted research grants awarded to their universities from Gilead. All other authors declare no competing interests.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Contributor Information
Annick Borquez, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA.
Leo Beletsky, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA; School of Law and Bouvé College of Health Sciences, Northeastern University, Boston, MA, USA.
Bohdan Nosyk, BC Centre for Excellence in HIV/AIDS, Vancouver, BC, Canada; Faculty of Health Sciences, Simon Fraser University, Burnaby, BC, Canada.
Prof Steffanie A Strathdee, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA.
Prof Alejandro Madrazo, Drug Policy Program, Centro de Investigación y Docencia Económicas, Sede Región Centro, Aguascalientes, Mexico.
Daniela Abramovitz, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA.
Claudia Rafful, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA; Centre for Urban Health Solutions, St Michael’s Hospital, Toronto, ON, Canada.
Mario Morales, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA; School of Social Work, San Diego State University, CA, USA.
Javier Cepeda, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA.
Dimitra Panagiotoglou, BC Centre for Excellence in HIV/AIDS, Vancouver, BC, Canada.
Emanuel Krebs, BC Centre for Excellence in HIV/AIDS, Vancouver, BC, Canada.
Prof Peter Vickerman, Population Health Sciences, University of Bristol, Bristol, UK.
Prof Marie Claude Boily, Department of Infectious Disease Epidemiology, Imperial College London, London, UK.
Nicholas Thomson, Johns Hopkins Bloomberg School of Public Health, Baltimore, MA, USA; Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC, Australia.
Natasha K Martin, Division of Infectious Diseases and Global Public Health, University of California San Diego, San Diego, CA, USA; Population Health Sciences, University of Bristol, Bristol, UK.
References
- 1.Mackey TK, Werb D, Beletsky L, Rangel G, Arredondo J, Strathdee SA. Mexico’s “ley de narcomenudeo” drug policy reform and the international drug control regime. Harm Reduct J 2014; 11: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Csete J, Kamarulzaman A, Kazatchkine M, et al. Public health and international drug policy. Lancet 2016; 387: 1427–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dolan K, Wirtz AL, Moazen B, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet 2016; 388: 1089–1102. [DOI] [PubMed] [Google Scholar]
- 4.Pollini RA, Brouwer KC, Lozada RM, et al. Syringe possession arrests are associated with receptive syringe sharing in two Mexico-US border cities. Addiction 2008; 103: 101–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strathdee SA, Beletsky L, Kerr T. HIV, drugs and the legal environment. Int J Drug Policy 2015; 26 (suppl 1): S27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Habicht JP, Victora CG, Vaughan JP. Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. Int J Epidemiol 1999; 28: 10–18. [DOI] [PubMed] [Google Scholar]
- 7.Garnett GP, Cousens S, Hallett TB, Steketee R, Walker N. Mathematical models in the evaluation of health programmes. Lancet 2011; 378: 515–25. [DOI] [PubMed] [Google Scholar]
- 8.Stone J, Martin NK, Hickman M, et al. Modelling the impact of incarceration and prison-based hepatitis C virus (HCV) treatment on HCV transmission among people who inject drugs in Scotland. Addiction 2017; 112: 1302–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altice FL, Azbel L, Stone J, et al. The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. Lancet 2016; 388: 1228–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pérez Correa C, Silva K. El Estado frente al consumo y los consumidores de sustancias ilícitas en México. CIDE Drug Policy Program. http://www.politicadedrogas.org/PPD/index.php/site/documento/id/18.html (accessed July 18, 2018).
- 11.National Commission Against Addictions (CONADIC). National Survey on Drugs, Alcohol and Tobacco Use (ENCODAT) 2016. https://www.gob.mx/cms/uploads/attachment/file/234856/CONSUMO_DE_DROGAS.pdf (accessed April 5, 2018).
- 12.Magis-Rodriguez C, Brouwer KC, Morales S, et al. HIV prevalence and correlates of receptive needle sharing among injection drug users in the Mexican-US border city of Tijuana. J Psychoactive Drugs 2005; 37: 333–39. [DOI] [PubMed] [Google Scholar]
- 13.Strathdee S Proyecto el Cuete phase IV. NIDA grant R01 DA0 19829; 2010–2020. https://gph.ucsd.edu/research/active-projects/Pages/el-cuete.aspx (accessed July 15, 2018).
- 14.Pollini RA, Alvelais J, Gallardo M, et al. The harm inside: injection during incarceration among male injection drug users in Tijuana, Mexico. Drug Alcohol Depend 2009; 103: 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strathdee SA, Arredondo J, Rocha T, et al. A police education programme to integrate occupational safety and HIV prevention: protocol for a modified stepped-wedge study design with parallel prospective cohorts to assess behavioural outcomes. BMJ Open 2015; 5: e008958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanitaria Juridicción. Report of the total of people censed at treatment centers in Tijuana during the operativo. Tijuana, Mexico, 2016. [Google Scholar]
- 17.Rafful C, Orozco R, Rangel G, et al. Increased non-fatal overdose risk associated with involuntary drug treatment in a longitudinal study with people who inject drugs. Addiction 2018; 113: 1056–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robertson AM, Garfein RS, Wagner KD, et al. Evaluating the impact of Mexico’s drug policy reforms on people who inject drugs in Tijuana, B.C., Mexico, and San Diego, CA, United States: a binational mixed methods research agenda. Harm Reduct J 2014; 11: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacArthur GJ, Minozzi S, Martin N, et al. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ 2012; 345: e5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bukten A, Skurtveit S, Gossop M, et al. Engagement with opioid maintenance treatment and reductions in crime: a longitudinal national cohort study. Addiction 2012; 107: 393–99. [DOI] [PubMed] [Google Scholar]
- 21.Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission in people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clin Infect Dis 2013; 57 (suppl 2): S39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frost SD, Brouwer KC, Firestone Cruz MA, et al. Respondent-driven sampling of injection drug users in two U.S.–Mexico border cities: recruitment dynamics and impact on estimates of HIV and syphilis prevalence. J Urban Health 2006; 83 (suppl 1): 83–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strathdee SA, Lozada R, Pollini RA, et al. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. J Acquir Immune Defic Syndr 2008; 47: 369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rafful C, Medina-Mora ME, González-Zúñiga P, et al. Somebody is gonna get hurt: involuntary drug treatment in Mexico Medical Anthropol (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen HT, Tuner N, Chen CJ, Lin HY, Liang S, Wang S. Correlations between compulsory drug abstinence treatments and HIV risk behaviors among injection drug users in a border city of South China. AIDS Educ Prev 2013; 25: 336–48. [DOI] [PubMed] [Google Scholar]
- 26.Kerr T, Hayashi K, Ti L, Kaplan K, Suwannawong P, Wood E. The impact of compulsory drug detention exposure on the avoidance of healthcare among injection drug users in Thailand. Int J Drug Policy 2014; 25: 171–74. [DOI] [PubMed] [Google Scholar]
- 27.Hughes C, Stevens A. What can we learn from the Portuguese decriminalization of illicit drugs? Br J Criminol 2010; 50: 999–1022. [Google Scholar]
- 28.Arredondo J, Strathdee SA, Cepeda J, et al. Measuring improvement in knowledge of drug policy reforms following a police education program in Tijuana, Mexico. Harm Reduct J 2017; 14: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Werb D, Strathdee SA, Meza E, et al. Institutional stakeholder perceptions of barriers to addiction treatment under Mexico’s drug policy reform. Glob Public Health 2017; 12: 519–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cepeda JA, Strathdee SA, Arredondo J, et al. Assessing police officers’ attitudes and legal knowledge on behaviors that impact HIV transmission among people who inject drugs. Int J Drug Policy 2017; 50: 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Commission Against Addictions (CONADIC). Directory of specialized inpatient drug treatment centres recognized by the National Commission Against Addictions. Mexico, 2017. https://www.gob.mx/salud/conadic/documentos/conadic-cuenta-con-un-directorio-nacional-de-establecimientos-residenciales-de-atencion-a-las-adicciones-reconocidos (accessed July 19, 2018). [Google Scholar]
- 32.Pinedo M, Burgos JL, Zuniga ML, Perez R, Macera CA, Ojeda VD. Police victimization among persons who inject drugs along the U.S.–Mexico Border. J Stud Alcohol Drugs 2015; 76: 758–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.