Abstract
Background and Aims
Manual bag mask ventilation is a life saving skill. An investigation was made to compare two different facemasks used in bag mask ventilation, the standard and the novel Tao face mask, and evaluate the ability of novices to achieve adequate tidal volume.
Methods
The study design was a crossover trial, which randomized forty medical students with no previous airway experience to learn bag mask ventilation with the standard mask and the Tao face mask. Primary outcome measures were mean and median tidal volume per mask, and secondary measures were hand area, age, gender, and order of mask usage.
Results
Medical students who used the Tao mask first achieved significantly more tidal volume than those who used the standard mask first (p = 0.002). However, when comparing face masks that were used second, the tidal volume did not differ significantly between the two masks (p = 1.000). Greater tidal volume was achieved on the second attempt relative to the first attempt with each mask. There was significantly more tidal volume achieved with greater hand size with the standard mask, whether it was used first or second (p < 0.001 and p = 0.012 respectively). Greater hand size was associated with greater tidal volume in the Tao mask also, but only when used first (p < 0.001). When first attempting bag mask ventilation, inexperienced students achieved greater tidal volume with the Tao Mask. The results also suggest that hand size matters less when using the Tao Mask.
Conclusion
When first attempting bag mask ventilation inexperienced students achieved greater tidal volume with the Tao Mask. The results also suggest that hand size matters less when using the Tao mask.
Keywords: upper airway anatomy, failed intubation: treatment, airway assessment: co-existing disease
Introduction
Manual positive pressure ventilation by facemask can be life-saving for patients who are hypoxic, hypercapnic, apneic, or in situations of failed intubation. This mask ventilation skill is routinely required for emergency medical technicians, respiratory therapists, nurses, and physicians in a variety of clinical settings. Although mask ventilation skills are routinely taught to patient care providers, even the most skilled airway specialists such as physician anesthesiologists still struggle to effectively mask-ventilate approximately 5% of patients [1].
The effective use of a standard mask without a pharyngeal airway in place (Figure 1) requires the simultaneous establishment of a seal between the mask and face and lifting of the jaw. The traditional preferred grip is referred to as the C&E technique. This requires the index finger and thumb to form a “C” and push down on the mask to establish a seal between the mask and face. The remaining three fingers (middle, ring, and little) form the “E” and wrap under the jaw to provide lift. The grip required to establish the seal and jaw lift simultaneously is awkward and difficult to teach. The basic design of the standard facemask has not changed in approximately 100 years. The Tao mask design is novel. The airway connector of this mask is located towards the nasal bridge, which provides additional space to hold the mask and seal to the face effectively. The Tao mask allows for the avoidance of the difficult C&E technique and instead encourages a more natural handgrip. With the Tao mask, downward pressure with the palm of the hand centered on the mask provides the seal between the face and the mask. Jaw lift is provided with all four fingers aligned under the jaw. It can be used for one handed bag mask ventilation by individuals with either a right or left handed grip. Two handed bag mask ventilation creates a better seal and is more effective; however, one handed bag mask ventilation is used frequently today in clinical practice. Smaller hand size was associated with the need to use two handed bag mask ventilation and an oral airway in a previous study [2].
Fig. 1.
Standard Mask (Vital Signs® Adult Face Mask with Adjustable Air Cushion Size 5, Manufactured by CareFusion)
The Tao face mask has been compared to the standard face mask both before and after neuromuscular blockade with experienced airway management providers [3]. The Tao face mask was equivalent in safety and superior in effectiveness compared to the standard face mask, despite a study design which favored the standard mask due to provider experience. The incidence of difficult bag mask ventilation is higher with novice providers [4]; therefore, the Tao mask could have even more effectiveness with novices. No study has been performed previously with the Tao face mask using novice airway providers.
We hypothesized that mask ventilation by novice operators would be superior with the Tao mask compared to the standard mask (see Figure 2). The aim of this study was to compare the efficacy of this novel mask to the standard mask when used by medical students with no airway experience for manual positive pressure ventilation. A secondary aim of the study was to evaluate the effect of hand size on the efficacy of mask ventilation with the standard and Tao mask.
Fig. 2.
Tao Face Mask
Methods
Study subjects
This study was conducted at the Medical University of South Carolina from January to April of 2017. Eligible subjects were second year medical students, and voluntary enrollment was used. Informed written consent was obtained from each medical student. Medical students were excluded if they had current or past Advanced Cardiac Life Support (ACLS) certification or if they had significant experience in bag mask ventilation, such as formal bag mask training in the past. The Institutional Review Board at MUSC approved this study. De-identified study data was collected and entered into an MUSC affiliated Redcap database.
Study design
The primary goal of this study was to compare the efficacy of the novel mask (Tao mask) to that of a commonly used, standard facemask (Vital Signs #082510) using medical students on a simulator. Bag mask ventilation (BMV) was assessed on a Laerdal ALS simulator (Laerdal Medical), and breath-to-breath tidal volume data was measured with a Boehringer Wright Respirometer (Boehringer Laboratories Inc., Phoenixville, PA). We referred to the standard mask as Mask 1 and the Tao mask as Mask 2. The masks were identified as Mask 1 and Mask 2 to each participant, and the words “standard” or “Tao” mask were never used.
The study was conducted as a crossover study in which each participant received training in the use of each type of mask and was then asked to perform BMV using each mask. Simple randomization using a pseudo-random number generator was made by the study statistician to obtain the randomization scheme, and this was put into an excel spreadsheet. After randomisation to use Mask 1 or Mask 2 first, each participant watched a brief instructional video on the use of the mask they were assigned to use first. The video presented an anesthesiologist demonstrating and verbalizing how to perform BMV on a Laerdal ALS simulator (Laerdal Medical) using that particular mask. Following ventilation with the first mask, the participant watched a second similar video explaining the proper way to perform BMV with the next mask. Therefore, there were two separate instructional videos, and the participants were randomized to the video they would watch first. No additional information or instruction was provided. No practice was allowed on either mask. After the video, the participants performed BMV, and the achieved tidal volumes were recorded. The simulator operator then played a recording which prompted the students to attempt BMV every ten seconds for two minutes, for a total of 12 breaths. Tidal volumes were measured with a respirometer and announced verbally with each inspiration so that participants could gauge their success with each breath, and tidal volumes of each breath were recorded by a separate study member.
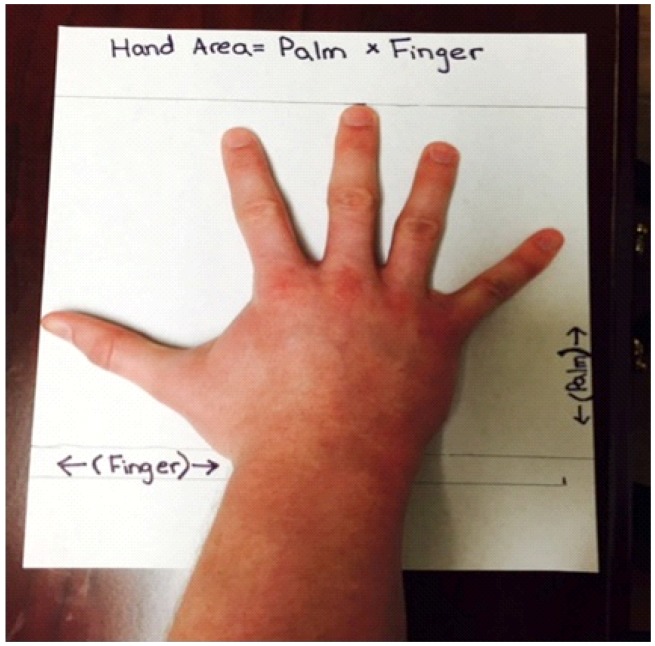
Additional data collected on each participant included their age, gender, hand size, and mask use sequence. Hand size was measured for each participant from the base of palm to tip of middle finger (Palm) and from thumb to the 5th finger (Finger). Hand area was then calculated by Palm (cm) × Finger (cm) and recorded in cm2 (Figure 3).
Fig. 3.
Hand Size, Showing Hand Area = Palm × Finger measurements
Statistical analysis
This study was a crossover trial in which all participants were asked to ventilate patients with both the Tao and standard masks. Descriptive statistics were calculated across all study participants and by randomization group. Associations between randomization groups with categorical variables were compared using chi-square or Fisher’s exact tests where appropriate and with continuous variables using 2-sample t-tests or Wilcoxon ranks sum tests where appropriate to evaluate whether randomization was effective. The primary outcome of interest was an average tidal volume over the 2 minute time period. The association between tidal volume over time with mask type and order of use was evaluated using a linear mixed model approach. The model included fixed effects for mask type, order of use, and the interaction between mask type and order of use and a random subject effect to account for repeated measures for each participant. Prior to examining differences between the two masks, we conducted tests for the carryover effect using linear contrasts from a linear mixed model [5]. The difference in scores between mask types on each patient, mask order, and the interaction between mask type and order were then compared using linear contrast statements from the linear mixed model.
A sample size of 40 participants provides > 80% power to detect and effect size of 0.65 under a 2 × 2 crossover design using a two-sided t-test and significance level α = 0.05. We developed a linear regression model with difference in area under the curve (AUC) for the tidal volume as the dependent variable to evaluate other potential covariates such as gender, age, hand area, and order of the training. Given a sample size of 40 participants, we fitted a linear model with up to 4 covariates. Harrell’s rule of thumb suggests that 10 observations per covariate are necessary to reliably estimate parameters in a linear model, thus 40 participants allowed us to determine if the mask type is significantly associated with AUC while controlling for up to 3 other variables [6].
A secondary analysis was conducted to examine the impact of the participant hand size on tidal volume achieved during BMV. The association between tidal volume with hand size was also evaluated using a linear mixed model approach. We also evaluated the impact of the hand size by the mask type and order of use; thus the mixed model included fixed effects for hand area, mask type, order of use, and the interactions between mask type, order of use, and hand size as well as a random subject effect. Differences in the impact of hand size by mask type and order of use were evaluated using linear contrasts from the mixed model. A Bonferroni approach was used to adjust for multiple comparisons between mask types, order of use, and the impact of hand size within group. All analyses were conducted in SAS v. 9.4 (SAS Institute, Cary, NC).
Results
There were a total of forty medical students, twenty in each arm of the study. The mean age of the study participants was 25.4 ± 2.4 years of age. There was not a significant difference by randomization group in age, gender, or hand measurements. Of the forty medical students, 21 were male. The average Finger measurement was 20.9 cm. The average Palm measurement was 19.1 cm, and the average Hand Area was 402.7 cm2.
Comparison of mask type and order of use
Prior to examining differences between the Tao and standard masks, we evaluated carryover, and a significant carryover effect was noted (p = 0.011); therefore, we limited comparisons between the mask types within the time period (e.g. comparison of the standard mask and the Tao mask at first use) and between time periods for the same mask type (e.g. comparison of the standard mask used first or standard mask used second). There were significant associations between the average tidal volume with mask type, order in which the masks were used, and the interaction between mask type and the order of use. Specifically, participants achieved significantly greater average tidal volume using the Tao mask compared to the regular mask if they were conducting their first trial (p = 0.002). However, the average tidal volume did not differ significantly between mask types when participants were conducting their second trial (p = 1.000). The second use of both masks produced significantly greater tidal volumes (Table 1) than the first use. Average tidal volume achieved by each mask type and order of use and the mean difference between tidal volume by mask type within period and between periods within mask type is shown in Table 1.
Table 1.
Average tidal volume by mask type and order of use, and differences by mask type or order. All values are estimated from a linear mixed model
| Mask Type or Comparison | Mean (95% CI) | p |
|---|---|---|
| Standard (Used 1st) | 137.4 (126.8, 148.0) | |
| Standard (Used 2nd) | 190.7 (180.1, 201.3) | |
| Tao (Used 1st) | 167.9 (157.3, 178.5) | |
| Tao (Used 2nd) | 192.0 (181.4, 202.6) | |
| Tao 1st vs. Standard 1st | 30.5 (15.4, 45.6) | 0.002 |
| Tao 2nd vs. Standard 2nd | 1.28 (−13.8, 16.3) | 1.000 |
| Standard 2nd vs. Standard 1st | 53.3 (38.2, 68.4) | < 0.001 |
| Tao 2nd vs. Tao 1st | 24.1 (9.05, 39.2) | 0.020 |
Impact of Hand Size
The average hand size (as noted by area) was 402.7 ± 58.9 cm2 and ranged between 309.4 to 510.6 cm2. We examined the impact of hand size (area in cm2) on tidal volume achieved by mask type and order of use. The linear mixed model included significant effects for mask type, order of used, hand area, the interaction between mask type and order of use, between mask type and hand area, between order of use and hand area, and the three way interaction between mask type, order of use, and hand area. Regression coefficients with 95% confidence intervals and associated p-values for the final model are reported in Table 2.
Table 2.
Linear mixed model of tidal volume by mask type, order of use, and hand area. Values reported are the estimated regression coefficients (95% CI) and p-values from a linear mixed model including fixed effects for mask type, order of use, hand area, and the interactions between these variables
| Model parameter | Regression coefficient (95% CI) | p |
|---|---|---|
| Intercept | −146.4 (−217.2, −75.6) | < 0.001 |
| Mask Type (Standard) | 243.3 (143.1, 343.5) | < 0.001 |
| Order of Use (Standard 1st) | 382.6 (280.5, 484.6) | < 0.001 |
| Hand Area (cm2) | 0.78 (0.61, 0.96) | < 0.001 |
| Mask Type (Standard) × Order (Standard 1st) | −495.0 (−639.3, 350.7) | < 0.001 |
| Mask Type (Standard) × Hand Area (cm2) | −0.55 (−0.84, −0.30) | < 0.001 |
| Order (Standard 1st) × Hand Area (cm2) | −0.89 (−1.14, −0.64) | < 0.001 |
| Mask Type (Standard) × Order (Standard 1st) × Hand Area (cm2) | 1.03 (0.68, 1.39) | < 0.001 |
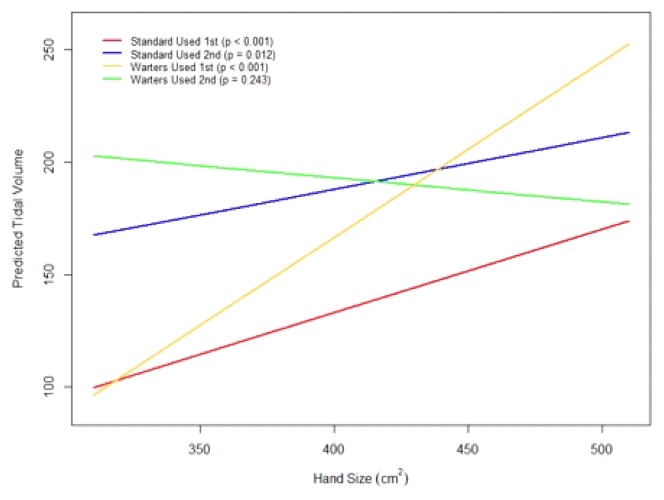
The linear mixed model found a significant increase in average tidal volume with increasing hand size for the standard mask when used first (p < 0.001), for the standard mask when used second (p = 0.012), and for the Tao mask when used first (p < 0.001). Specifically, for participants using the standard mask first, tidal volume increased on average by 3.7 mL for a 10 cm2 increase in hand size. Participants using the standard mask second showed a 2.3 unit increase for a 10 cm2 increase in hand size. Participants using the Tao mask first showed the greatest increase in average tidal volume with increasing hand size with a 7.8 mL increase in tidal volume for a 10 cm2 increase in hand size. There was a downward trend in tidal volume with increasing hand size for the Tao mask when it was used secondly, although this association was not statistically significant (p = 0.234). Figure 4 shows the regression lines for predicted tidal volume by hand size for the 4 groups.
Fig. 4.
Estimated Tidal Volume by Hand Area from the linear mixed model for the following groups: (1) Standard mask when used 1st (red), (2) Standard mask when used 2nd (blue), (3) Tao mask when used 1st (gold), and (4) Tao mask when used 2nd (green)
Discussion
Our study demonstrated that airway novices were able to generate significantly higher mean tidal volumes with the novel Tao mask compared to a standard facemask on first use, thus suggesting an improved ease of use compared to the standard mask. There was also a significant increase in mean tidal volumes achieved for both mask types when each mask type was used second compared to the same mask type when used first. This likely reflects a learning effect that occurs as students become more comfortable with mask ventilation techniques. Studies have shown that video instruction prior to standard mask ventilation in novice operators improves performance. Diendl et al. demonstrated that a self-instructional video significantly improved BMV performance in inexperienced providers using a neonatal airway simulator [7]. While video instruction on proper mask techniques for both the standard and Tao face masks may be an effective way to improve initial performance, there is likely also a component of self adjustment that occurs during the second mask attempt that explains improved performance during the second mask trial.
We believe that the improved performance of the Tao mask on first use is explained by the ergonomic grip. Studies have shown that the “C&E” grip may cause problematic compression of the submandibular tissue along with reduced jaw lift [8]. The Tao mask design allows the palm to be placed in the center of the mask, providing a superior seal between the mask and face compared to the “C&E” grip. The Tao mask design also allows four fingers to align under the center of the chin to provide lift. This provides and actually encourages a superior jaw lift compared to three fingers centered on the angle of the jaw as occurs with the C&E technique. A prior study also showed that when experienced personnel used the Tao mask in an anesthetic setting, ventilation was significantly better than with a standard mask [3].
The improved tidal volumes achieved with each mask type in the present study when used second compared to the same mask type when used first is likely explained by intrinsic features of the Laerdal ALS simulator as it applies to the airway in terms of “mask seal” and lung resistance [9, 10]. The Laerdal ALS airway & lungs are similar to the Laerdal SimMan as it applies to airway anatomy, lung resistance, and compliance when in the “normal ventilation” mode. Hesselfeldt et al. formally evaluated this specific airway. When compared to an equivalent normal male, the simulator’s “mask seal” is more difficult than a human airway but is not a “difficult mask seal.” Lung resistance on the simulator is decreased, allowing easier ventilation compared to the average human, and the compliance of the simulator airway, including chest wall and skin, is similar to that of a human [11]. These findings are consistent with the hypothesis and results in this study. When novices were initially exposed to a moderately difficult mask seal on the simulator, the Tao mask allowed for an easier mask seal. However, it is relatively simple to learn how to seal the mask on this simulator, and it is easier than a normal human to ventilate. After two minutes of practice on the simulator with the first trial, both groups had likely learned how to achieve a mask seal. Pastis et al. modified the simulator’s airway specifically to increase the lung resistance to create a “difficult BMV” scenario in order to expose differences in levels of ability to seal the face mask in BMV. Experienced anesthesia providers could achieve ventilation, but BMV novices could not until trained [9]. The idea of a standardized, simulated “difficult BMV” airway may be a better experimental model for discerning safely the differences in different physical masks or training methods for future studies.
Our study also found improved tidal volumes with increasing hand size with the standard mask when used first or second but for the Tao mask only when used first. This indicates practitioners with small hands are potentially more likely to achieve larger tidal volumes when using the Tao mask compared to the standard mask. Hand size and how it relates to ability to mask ventilate with standard masks is controversial. A previous study showed a positive correlation between smaller hand size and smaller tidal volumes and larger hand size achieving larger tidal volumes with a silicone standard facemask [12, 13]. Another study found a smaller hand size was marginally associated with the placement of an oral airway while performing BMV [2]. Several other studies have shown no difference in manual ventilation performance based on hand size [11, 14]. Our data indicate that increased hand size is correlated with improved ventilation with a standard mask but not the Tao mask when used second. The Tao mask would therefore potentially have an advantage over the standard mask for practitioners with small hands. Further studies with experienced practitioners will need to confirm this potential advantage of the Tao mask for practitioners with small hands.
The biggest limitation of this study was the use of a simulator rather than real patients. The previous study on the Tao face mask involved actual patients [3]. Because the airway providers in our study had no prior bag mask experience, we opted to use a simulator for possible patient safety concerns. Future studies utilizing actual patients are required since the use of a simulator may have confounded our results.
Despite tremendous advances in simulation, mask ventilation on a mannequin may not realistically simulate all of the challenges and variety associated with patients. Specifically, adequate jaw lift is essential to adequately ventilate patients, whereas the mannequin used in this study requires little jaw lift to generate tidal volumes. The simulation mannequin may not be ideally designed to reproduce real patients, and a new airway mannequin would be welcomed.
Our study shows improved tidal volumes with the Tao mask compared to the standard mask with airway novices on a mannequin, as well as a potential advantage of the Tao mask for practitioners with small hands. Future studies should compare the efficacy and ease of use of the Tao mask compared to the standard mask on actual patients, as well as the effect of the hand size using both masks in a clinical setting.
Conclusions
The Tao face mask is novel and beneficial. Airway novices were able to generate significantly higher mean tidal volumes with the novel Tao mask compared to a standard facemask on first use. This suggests that the Tao mask is inherently more “user friendly” than a standard facemask. There was also a significant increase in mean tidal volumes achieved for both mask types when each mask type was used second compared to the same mask type when used first. This reflects the learning curve of novice mask users. Gaining experience with the first mask attempt resulted in improvements in subsequent mask ventilation performance. This study demonstrated that hand size may matter less when using the Tao face mask, thus reflecting a potential advantage compared to the standard mask. Lastly, a training mannequin that better replicates human airway mechanics is required, and similar studies on actual patients would be helpful to support our conclusions.
Footnotes
Competing interests
Dr. Warters is the inventor of the Tao Mask. He did not participate in the data collection or analysis of data.
References
- 1.Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, Riou B. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236. doi: 10.1097/00000542-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Pastis NJ, Tobin CD, Scott JB, Schaefer JJ. Hand size variation and success in simulated difficult bag mask ventilation. Am J Respir Crit Care Med. 2015;191:A4546. [Google Scholar]
- 3.Brown TA, Szabo TA, Bridges KH, Sabbagh MJ, Hand WR, Wolf BJ, et al. Safety and effectiveness of a novel facemask for positive pressure ventilation. Anesth Analg. 2018;127:151–156. doi: 10.1213/ANE.0000000000002621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Orbany M, Woehlck HJ. Difficult mask ventilation. Anesth Analg. 2009;109:1870–1880. doi: 10.1213/ANE.0b013e3181b5881c. [DOI] [PubMed] [Google Scholar]
- 5.Wellek S, Blettner M. On the proper use of the crossover design in clinical trials: part 18 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2012;109:276–281. doi: 10.3238/arztebl.2012.0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 7.Deindl P, Schwindt J, Berger A, Schmölzer GM. An instructional video enhanced bag-mask ventilation quality during simulated newborn resuscitation. Acta Paediatr. 2015;104:e20–26. doi: 10.1111/apa.12826. [DOI] [PubMed] [Google Scholar]
- 8.Fei M, Blair JL, Rice MJ, Edwards DA, Liang Y, Pilla MA, et al. Comparison of effectiveness of two commonly used two-handed mask ventilation techniques on unconscious apnoeic obese adults. Br J Anaesth. 2017;118:618–624. doi: 10.1093/bja/aex035. [DOI] [PubMed] [Google Scholar]
- 9.Pastis NJ, Doelken P, Vanderbilt AA, Walker J, Schaefer JJ. Validation of simulated difficult bag-mask ventilation as a training and evaluation method for first-year internal medicine house staff. Simul Healthc. 2013;8:20–24. doi: 10.1097/SIH.0b013e318263341f. [DOI] [PubMed] [Google Scholar]
- 10.Hesselfeldt R, Kristensen MS, Rasmussen LS. Evaluation of the airway of the SimMan™ full-scale patient simulator. Acta Anaesthesiol Scand. 2005;49:1339–1345. doi: 10.1111/j.1399-6576.2005.00856.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee HM, Cho KH, Choi YH, Yoon SY, Choi YH. Can you deliver accurate tidal volume by manual resuscitator? Emerg Med J. 2008;25:632–634. doi: 10.1136/emj.2007.053678. [DOI] [PubMed] [Google Scholar]
- 12.Na JU, Han SK, Choi PC, Cho JH, Shin DH. Influence of face mask design on bag-valve-mask ventilation performance: a randomized simulation study. Acta Anaesthesiol Scand. 2013;57:1186–1192. doi: 10.1111/aas.12169. [DOI] [PubMed] [Google Scholar]
- 13.Hess D, Spahr C. An evaluation of volumes delivered by selected adult disposable resuscitators: the effects of hand size, number of hands used, and use of disposable medical gloves. Respir Care. 1990;35:800–805. [PubMed] [Google Scholar]
- 14.Khoury A, Sall FS, De Luca A, Pugin A, Pili-Floury S, Pazart L, et al. Evaluation of Bag-Valve-Mask Ventilation in Manikin Studies: What Are the Current Limitations? Biomed Res Int. 2016;2016 doi: 10.1155/2016/4521767. 4521767. [DOI] [PMC free article] [PubMed] [Google Scholar]