Evidence-Based Outcomes Article.
Abstract
Background:
The effectiveness of gender-confirming surgery is best evaluated on the basis of patient-reported outcomes. This is the first explorative study using the BODY-Q chest module, administered in trans men before and after mastectomy.
Methods:
Between October of 2016 and May of 2017, trans men were recruited to participate in a cross-sectional study. Data collection included standardized anamnesis and examination, screening questions on depression/anxiety, and seven BODY-Q scales, including new scales measuring satisfaction of the chest and nipples. Mean scores for preoperative and postoperative participants were compared, and regression analyses were conducted to identify factors associated with BODY-Q scores.
Results:
In total, 101 persons participated (89 percent; 50 preoperatively and 51 postoperatively). Postoperative participants reported significantly higher (better) scores on the chest (67), nipple (58), body (58) (t tests, all p < 0.001), and psychological (60) (t test, p = 0.05) scales compared with preoperative patients. Postoperative chest and nipple mean scores did not differ significantly from a gynecomastia comparison, whereas scores were less favorable on the psychosocial domains. Preoperatively, chest scores were not associated with objective breast size. Lower postoperative chest scores were associated with planned revision surgery (β = −0.52) and depressive symptoms (β = −0.59).
Conclusions:
The present findings indicate that chest and nipple satisfaction differences in trans men undergoing mastectomy can be detected using the BODY-Q chest module. Future prospective studies are needed to measure clinical change in satisfaction and how this relates to changes in other aspects of health-related quality of life.
Gender dysphoria refers to distress caused by an incongruence between one`s experienced gender and gender assigned at birth.1 This distress results in some individuals applying for medical interventions that aim to make bodily characteristics more gender-congruent. In trans men (those assigned female at birth who identify as male/masculine), gender-confirming intervention generally encompasses testosterone therapy and/or gender-confirming surgery that targets primary and secondary sex characteristics.
Before undergoing treatment, gender dysphoria in trans men is frequently accompanied by body dissatisfaction,2 impaired sexual well-being,3 and unfavorable quality of life.4 Given the nature of the treatment, scholars and clinicians emphasize that gender-confirming medical interventions is best evaluated using subjective data reported by the person receiving it.5 Concepts that are used to operationalize subjective evaluation (also called patient-reported outcomes, although transgender individuals are generally not referred to as “patients”) include treatment satisfaction, body image, self-esteem, life evaluations, happiness, and sexual function.6
For trans men, testosterone therapy, usually the first received gender-confirming medical intervention, was shown to improve mental health and quality of life.7 Masculinizing chest surgery is considered the most important surgical intervention for many trans men.8 Past studies of the effectiveness of mastectomy found that body image improved after surgery,8,9 as did psychological well-being and experienced gender dysphoria.10 Factors associated with treatment satisfaction and quality of life included treatment expectations,11 physical appearance,9 health care experiences and complications,11,12 psychological distress,9 and social support and discrimination.13
To facilitate future outcome assessments in gender-confirming interventions, carefully designed patient-reported outcomes instruments specific to the transgender population are needed. In a recent review of patient-reported outcomes instruments used to assess outcomes following gender-confirming surgery, Barone et al. identified a need for new transgender-specific assessment tools that cover functional, psychorelational, and cosmetic components.6 Although 17 (mostly generic) patient-reported outcomes instruments were identified by this team, all were considered limited by their development, validation, or content. After the publication of this review, patient-reported outcomes scales measuring the appearance of the chest and nipples were published as a supplement to the BODY-Q, specifically for use in trans men.14,15 The BODY-Q is a questionnaire designed to measure outcomes in weight loss and/or body contouring surgery, and measures appearance, health-related quality of life, and health care experiences. The new BODY-Q chest module was subsequently developed and tested in an international heterogeneous sample of men and trans men who were undergoing weight loss, gynecomastia, or gender-confirming chest surgery.
Aims
The primary aim of this explorative study is to present the findings on the BODY-Q chest module for a Dutch sample of 101 preoperative and postoperative trans men. To identify factors associated with the BODY-Q scores, participants’ scores were correlated with clinical variables for the preoperative and postoperative groups separately. To determine the effect of surgery, preoperative and postoperative scores were compared. Finally, to interpret the postoperative scores, trans men’s outcomes were compared with a sample of men who underwent surgery for gynecomastia. Based on the available literature, a positive effect of surgery on patient-reported outcomes pertaining to body satisfaction and psychosocial well-being is expected. However, other factors such as mental health problems are expected to also interfere with these outcomes.
PARTICIPANTS AND METHODS
Procedure
The present cross-sectional study was conducted at the Department of Plastic, Reconstructive and Hand Surgery and the Center of Expertise on Gender Dysphoria of the VU University Medical Center, Amsterdam, The Netherlands. Data collection was part of the BODY-Q chest module field test.15 Multidisciplinary care was conducted according to the World Professional Association for Transgender Health Standards of Care.16 Participants were recruited between October of 2016 and May of 2017 when applying for mastectomy (preoperative participants), or when attending follow-up visits at a psychologist or physician (postoperative participants). Preoperative and postoperative participants therefore concerned different groups. All persons eligible for mastectomy (18 years or older, gender dysphoria diagnosis confirmed,1 with a body mass index between 18 and 35 kg/m2) and with sufficient knowledge of the Dutch language were considered eligible to participate. Postoperative participants had to be at least 6 months after their last chest surgery, which also includes revision surgery. After obtaining informed consent, a paper questionnaire was filled out at the clinic. The study was approved by the local medical ethics committee.
Chest wall surgery was performed by specialized surgeons by means of either a periareolar mastectomy (semicircular incision with liposuction, in case of small breasts with good elasticity without nipple reduction required), by means of a concentric circular mastectomy (periareolar skin resection; in case of medium-size breasts with good skin quality or small breasts with poor skin quality), or by means of lower pole skin resection with free nipple grafting (inframammary incision and nipple graft; in case of large breasts or medium-size breasts with poor skin elasticity). Postoperative chest compression was applied for 6 weeks. Secondary chest corrections were performed no earlier than 6 months after initial surgery.
Measures
Sample Characteristics
Standardized clinical data were collected during anamnesis (i.e., relationship status, education level, gender identity, highest weight, and chest-binding habits) and physical examination (i.e., body mass index, breast size, and elasticity). Information on testosterone prescription, chest surgery technique, and secondary chest corrections were obtained from medical records.
BODY-Q Chest Module
The BODY-Q is a patient-reported outcomes instrument developed to evaluate appearance (of the body and specific areas of the body), health-related quality of life, and health care experiences for patients who undergo weight loss and/or body contouring surgery.14 The chest module was subsequently developed to provide a means of measuring satisfaction with the appearance of the chest and nipples.15 Each BODY-Q scale (including the chest module scales) is scored on a scale from 0 (worst) to 100 (best). For this study, the following scales were administered:
Chest: A 10-item scale, in which satisfaction with different aspects of the chest (e.g., appearance in a snug T-shirt) is rated on a four-point scale (very dissatisfied to very satisfied).
Nipples: A five-item scale, in which satisfaction with different aspects of the nipples (e.g., size) is rated on a four -point scale (very dissatisfied to very satisfied).
Body: A 10-item scale, in which satisfaction with different aspects of the body in general is rated on a four-point scale (very dissatisfied to very satisfied).
Psychological: A 10-item scale, in which agreement with different statements regarding psychological function is rated on a four-point scale (definitely disagree to definitely agree).
Social: A 10-item scale, in which agreement with different statements regarding social function is rated on a four-point scale (definitely disagree to definitely agree).
Expectations: An eight-item scale that measures how people seeking plastic surgery expect their appearance and quality of life might improve (e.g., “I will look fantastic”), rated on a four-point scale (definitely disagree to definitely agree). Higher scores indicate more unrealistic expectations.
Appearance-related distress: An eight-item scale that measures distress related to appearance (e.g., “I feel anxious when people look at me”), rated on a four-point scale (definitely disagree to definitely agree). Higher scores indicate more distress.
Single-Item Questions
Participants were asked questions to report on factors that are (possibly) associated with the BODY-Q scale scores. Postoperative participants were asked “Do you plan to apply for a secondary correction of your chest?” (yes/unsure/no), and two single-item screening questions on mental health issues: “Do you experience feelings of anxiety/depression?” (five-point Likert scale from not at all to a lot).
Statistical Analyses
BODY-Q scale raw scores were transformed from 0 to 100 values according to the BODY-Q instructions.14,15 Sample characteristics were calculated as means and frequencies for the preoperative and postoperative groups. Parametric statistics were used, because BODY-Q scores were distributed normally for both before and after surgery participant groups. Differences in mean scores were tested between the preoperative and postoperative groups (independent sample t tests) and within the postoperative group (per surgical technique; one-way analysis of variance). Postoperative scores were compared with data from men operated on for gynecomastia from the field-test sample15 through independent sample t tests. A linear regression with forced entry was performed on the preoperative BODY-Q domain scores including breast size, body mass index, anxiety, and depressive symptoms as predictors. Similarly, a linear regression with forced entry was performed on the postoperative BODY-Q scale scores, including planned corrections, body mass index, anxiety, and depressive symptoms as predictors. Bonferroni correction was applied to correct for multiple linear regressions (p = 0.05/5 = 0.01 were considered statistically significant). All statistical analyses were performed using IBM SPSS Version 22.0 (IBM Corp., Armonk, N.Y.).
RESULTS
Sample Characteristics
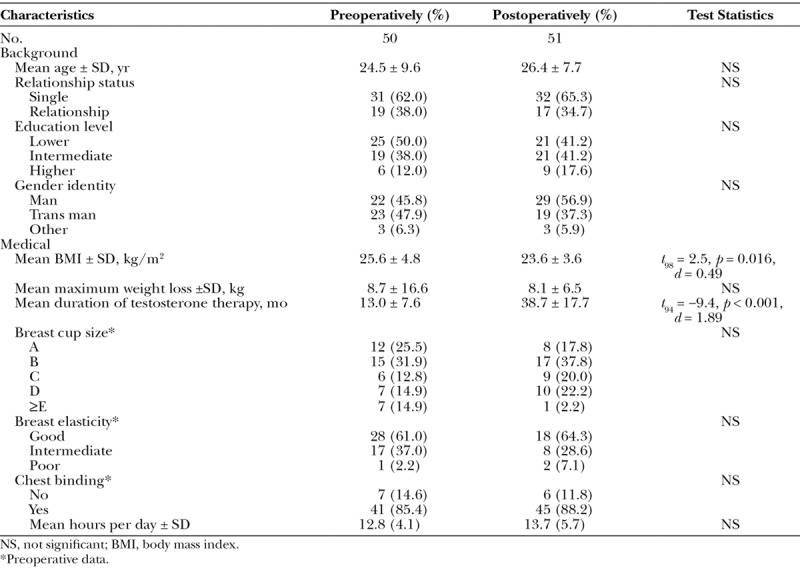
Sixty-two preoperative trans men were recruited, of whom 50 participated (81 percent), and 51 of the 52 recruited postoperative trans men participated (98 percent). Seven persons refused participation because of lack of interest, whereas no reason was given in six other cases. Table 1 displays information on the participating sample. No significant differences between the preoperative and postoperative groups were observed on most background and breast characteristics (measured before surgery). On average, preoperative participants did have a significantly higher body mass index and had understandably been on testosterone therapy for a shorter period. None of the participants had undergone genital gender-confirming surgery. Mean follow-up time for the postoperative participants was 26 months after initial/revision surgery (range, 6 to 68 months).
Table 1.
Sample Characteristics (n = 101)
Among the postoperative group, six had undergone periareolar mastectomy (12 percent), 27 had undergone concentric circular skin resection (55 percent), and 16 had undergone an inframammary skin resection (33 percent), whereas this information was irretrievable for two participants. Secondary corrections were more prevalent after inframammary skin resections (69 percent) and concentric circular mastectomy (62 percent), than for the periareolar group (17 percent). The most frequent corrections included liposuction, removal of dog-ears, and nipple and scar corrections. Eleven participants (23 percent) stated they planned to undergo a secondary correction, without differences among the surgical techniques. In mental health screening, approximately 20 percent of the postoperative participants experienced a substantial level of anxiety (somewhat to a lot), whereas 35 percent experienced depressive symptoms. No significant differences between surgical techniques were observed.
Patient-Reported Outcomes (BODY-Q Chest Module)
Figure 1 displays the BODY-Q scale scores for the preoperative and postoperative groups. The mean score ± SD for preoperative participants was 45 ± 19 for appearance-related distress and 65 ± 17 for expectations. The preoperative group scored significantly lower on the chest (23 ± 17 versus 67 ± 21; p < 0.001), nipples (35 ± 21 versus 58 ± 24; p < 0.001), and body (40 ± 14 versus 58 ± 21; p < 0.001) scales compared with postoperative participants, and somewhat more positive on the psychological (60 ± 17; p = 0.05) and social (64 ± 18; p > 0.05) scales. No such differences were found between groups on the psychological or social scales. No statistically significant differences on the mean chest and nipple scales were observed between the participants who underwent periareolar mastectomy (chest, 74 ± 19; nipple, 58 ± 22), concentric circular mastectomy (chest, 69 ± 20; nipple, 62 ± 23), and inframammary skin resection mastectomy with free nipple grafts (chest, 67 ± 22; nipple, 58 ± 24).
Fig. 1.
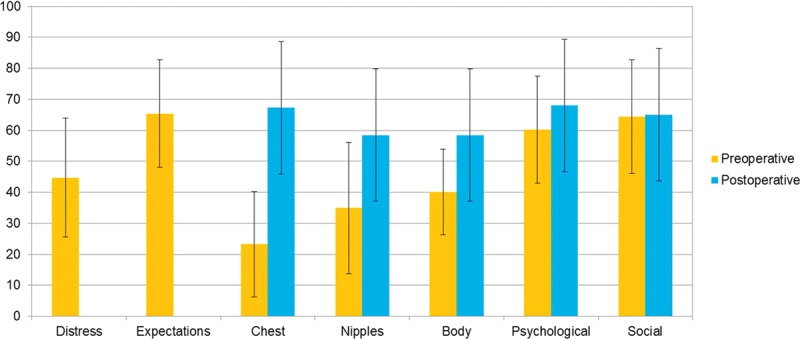
BODY-Q Chest Module scores and the effect of mastectomy. Distress and expectations scales were administered only to preoperative participants. Preoperative-to-postoperative differences are as follows: chest, t98 = −11.4, p < 0.001, d = 2.3; nipples, t97 = −5.2, p < 0.001, d = 1.0; body, t97 = −5.2, p < 0.001, d = 1.0; psychological, t97 = −2.0, p = 0.05, d = 0.40; and social, t97 = −0.17, p > 0.05, d = 0.03. For the distress scale, 0 = lowest and 100 = highest. For the expectations scale, 0 = lowest and 100 = highest. For all BODY-Q scales, 0 = worst and 100 = best scores.
In the field-test sample, 91 men underwent chest surgery for gynecomastia. When the mean scores for trans men were compared with men with gynecomastia, no significant differences were found on the chest (gynecomastia, 64 ± 25) and nipple satisfaction (gynecomastia, 63 ± 26) scales. Trans men reported significantly lower scores than the gynecomastia group on the body (gynecomastia, 69 ± 22; t117 = 2.7, p = 0.007), psychological (gynecomastia, 78 ± 20; t114 = 2.4, p = 0.02), and social (gynecomastia, 73 ± 21; t114 = 2.0, p = 0.05) scales.
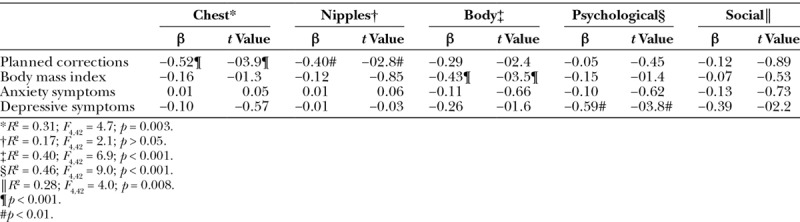
Associated Factors
In the preoperative group, chest and nipple scores were not associated with objectified breast size (Table 2). Also, no associations between chest, psychological, and social domains and the items measuring anxiety/depression symptoms were observed. The scores for the body scale were negatively associated with body mass index (higher body mass index associated with lower satisfaction with the body). Postoperatively, planned corrections were negatively associated (less positive scores) with the chest and nipple scales and the body scale was negatively associated with body mass index. Lower scores on the psychological scale were associated with a confirming answer on the item measuring depressive symptoms (Table 3).
Table 2.
Factors Associated with Preoperative BODY-Q Chest Module Scores (n = 50)
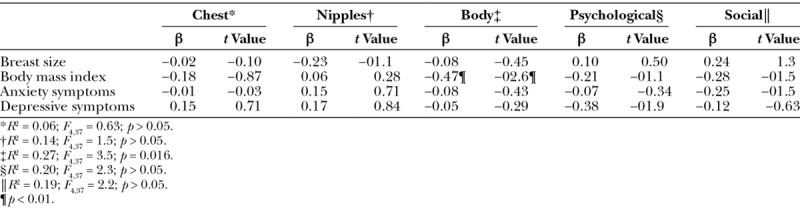
Table 3.
Factors Associated with Postoperative BODY-Q Chest Module Scores (n = 51)
DISCUSSION
The growing field of gender-confirming surgery lacks transgender-specific validated patient-reported outcomes instruments. The present explorative study is the first to report findings of the newly developed chest module that forms part of the BODY-Q instrument. These scales were developed for different chest conditions, including trans men undergoing mastectomy. This study shows that mastectomy is associated with more than chest satisfaction only: postoperative levels of satisfaction with body and psychological function were higher as well (albeit studied in a cross-sectional, and not a prospective design). Preoperative quality-of-life impairments were not related to breast size, whereas persistent postoperative levels were mostly related to co-occurring depressive symptoms as observed from a screening question.
Our preoperative findings confirm earlier studies reporting on the impaired body image2,8,9 and psychosocial well-being in trans men.4 Gender-incongruent physical characteristics often cause mental distress and the avoidance of gendered activities such as sports or sexual activity. Preoperatively, the lowest scores were observed on the female breasts and nipples, but the overall body satisfaction was lower as well.
With regard to the effect of surgery, our findings suggest that mastectomy improves patient-reported satisfaction with appearance and health-related quality of life. The largest preoperative-to-postoperative differences were observed on the chest and nipple scales, although postoperative scores for satisfaction with body and psychological function were more positive as well. These findings confirm earlier findings on the effectiveness of gender-confirming surgery on patient-reported outcomes, albeit mostly studied using nonvalidated measures.8–10 An interesting finding is that satisfaction with overall body appearance was higher in the postoperative group, although not all gender-incongruent body parts were operated on (yet). Earlier studies hypothesized that this improvement may be the result of a more positive self-evaluation, and easier social participation and subsequent positive experiences (and a lower body mass index in case of sports).8,9 In addition, the male chest reduces experienced gender dysphoria and possibly also subsequent psychiatric symptoms.10 The social domain showed no significant differences after surgery. One explanation may be that improvements in social function (e.g., social confidence) may take longer after surgery, or may change only after one has undergone genital gender-confirming surgery. Also, social discomfort may be related to body characteristics that are not subject to medical treatments (e.g., body height).9
When comparing the postoperative findings with clinical control values, values for body satisfaction and for psychological and social well-being were lower than for men operated on for gynecomastia.15 Although gynecomastia is known to be associated with impaired body image and psychosocial issues,17 the origin of gender dysphoria–related distress is likely to be more profound. Also, the gender-confirming mastectomies are often more extensive operations, possibly leading to poorer aesthetic outcomes. In trans men, body evaluation may be less positive because they may “pass” less as men,2 and as a result individuals can be confronted with discrimination.13 Also, a substantial share of the postoperative participants opt for additional genital gender-confirming surgery, possibly contributing to a lower satisfaction with body in the present.9 In addition, co-occurring mental health problems in trans men may also account for some of the difference in psychosocial functioning.
Several factors were found to be associated with the BODY-Q outcomes, including body mass index, secondary corrections, and psychological function. Preoperatively and postoperatively, a higher body mass index was associated with lower body satisfaction. Body mass index was higher in trans men who were not operated on, compared with those who were. Earlier studies found that sports participation and health awareness are fairly low in trans men who applied for mastectomy.8 Therefore, it is important for clinicians to support a healthy lifestyle in this population, and to know how mastectomy may contribute. The association between body mass index and patient-reported outcomes after surgery was observed in patients operated on for massive weight loss as well.18 Interestingly, preoperative breast size did not correspond with the degree of chest/nipple dissatisfaction. Possible explanations may include (1) all preoperative participants applied for mastectomy and were (very) dissatisfied, and (2) chest dissatisfaction originating from gender dysphoria may relate primarily to the presence of female breasts, rather than the size of these breasts. Postoperative chest and nipple scores were associated with planned secondary corrections. This could imply that BODY-Q scores may further improve after chest corrections have been performed. Also, previous studies observed the importance of preoperative expectations of surgery and experienced complications on quality of life after gender-confirming operations.11,12 As mastectomies are frequently followed by secondary corrections, surgeons should prepare trans men to anticipate possible disappointing outcomes after initial surgery and the possible need for revision surgery. Patient-reported outcomes after mastectomy were related to co-occurring depressive symptoms, assessed by the screening question. The relationship between patient-reported outcomes and mental health problems was observed earlier in transgender populations9,10 and in patients undergoing post–weight loss surgery.18 Mental health symptoms may indicate negative personality traits or lower self-esteem, or may even increase the risk of poorer objective outcomes. Therefore, it is of importance for surgeons in this field to understand the interplay between patient-reported outcomes and mental health and to refer to mental health professionals when necessary.
The study was limited by the cross-sectional design, making it impossible to make conclusive statements on predictive factors of postoperative patient-reported outcomes. Also, although the sample size was sufficient to detect the major differences, small yet clinically significant associations may not have been detected. Moreover, the sample size and multiple testing may have influenced our findings. Another limitation relates to the use of BODY-Q scales; although the chest and nipple scales were developed and validated for trans men, the other BODY-Q scales did not include trans men and trans women in their development. Similarly, our screening questions for anxiety and depression were single items rather than validated measuring scales. Lastly, no objective outcome measures have been collected to compare with the BODY-Q data. A future study can systematically follow-up on the same group and include multiple associated variables, including validated and objective outcomes. This might help gaining insight about how patient-reported outcomes evolve over time within the same population.
CONCLUSIONS
The present findings indicate that the BODY-Q chest module is a clinically useful measure of outcomes important to trans men undergoing mastectomy. Preoperative breast dissatisfaction seemed mostly related to gender dysphoria and less related to breast size. Although postoperative values were higher, trans men scored lower than the control group operated on for gynecomastia. Postoperative values were mostly related to planned secondary corrections and depressive symptoms. Therefore, surgeons should be advised to counsel trans men on the possibility of corrections and to be attentive to psychological issues, and collaborate with mental health professionals. Finally, research to measure clinical changes using the BODY-Q chest module in this group is recommended. There is also a need for the development of patient-reported outcomes scales that could be used to evaluate other gender-confirming treatments.
ACKNOWLEDGMENTS
The authors would like to thank the study participants, the BODY-Q developers, and Müjde Özer and Marlon Buncamper for assistance in data collection; and Floyd Timmermans for editing the final manuscript.
Footnotes
Disclosure: Anne Klassen is a co-developer of the BODY-Q and may receive a share of the license revenues. The remaining authors have no financial disclosures.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 20135th ed Arlington, Va: American Psychiatric Publishing; [Google Scholar]
- 2.van de Grift TC, Cohen-Kettenis PT, Steensma TD, et al. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav. 2016;45:575–585.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cerwenka S, Nieder TO, Briken P, et al. Intimate partnerships and sexual health in gender-dysphoric individuals before the start of medical treatment. Int J Sex Health 2014;26:52–65.. [Google Scholar]
- 4.Bockting W, Coleman E, Deutsch MB, et al. Adult development and quality of life of transgender and gender nonconforming people. Curr Opin Endocrinol Diabetes Obes. 2016;23:188–197.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuiper B, Cohen-Kettenis P. Sex reassignment surgery: A study of 141 Dutch transsexuals. Arch Sex Behav. 1988;17:439–457.. [DOI] [PubMed] [Google Scholar]
- 6.Barone M, Cogliandro A, Di Stefano N, Tambone V, Persichetti P. A systematic review of patient-reported outcome measures following transsexual surgery. Aesthetic Plast Surg. 2017;41:700–713.. [DOI] [PubMed] [Google Scholar]
- 7.White Hughto JM, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health 2016;1:21–31.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van de Grift TC, Kreukels BP, Elfering L, et al. Body image in trans men: Multidimensional measurement and the effects of mastectomy. J Sex Med. 2016;13:1778–1786.. [DOI] [PubMed] [Google Scholar]
- 9.van de Grift TC, Elaut E, Cerwenka SC, et al. Effects of medical interventions on gender dysphoria and body image: A follow-up study. Psychosom Med. 2017;79:815–823.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith YL, Van Goozen SH, Kuiper AJ, Cohen-Kettenis PT. Sex reassignment: Outcomes and predictors of treatment for adolescent and adult transsexuals. Psychol Med. 2005;35:89–99.. [DOI] [PubMed] [Google Scholar]
- 11.van de Grift TC, Elaut E, Cerwenka SC, et al. Surgical satisfaction, quality of life and their association after gender affirming surgery: A follow-up study. J Sex Marit Ther. 2018;44:138–148.. [DOI] [PubMed] [Google Scholar]
- 12.Zeluf G, Dhejne C, Orre C, et al. Health, disability and quality of life among trans people in Sweden: A web-based survey. BMC Public Health 2016;16:903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Başar K, Öz G, Karakaya J. Perceived discrimination, social support, and quality of life in gender dysphoria. J Sex Med. 2016;13:1133–1141.. [DOI] [PubMed] [Google Scholar]
- 14.Klassen AF, Cano SJ, Alderman A, et al. The BODY-Q: A patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open 2016;4:e679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klassen AF, Kaur M, Poulsen L, et al. The BODY-Q chest module for use in gynecomastia, post-weight loss, body contouring and gender confirming surgery. Plast Reconstr Surg. (accepted for publication). [Google Scholar]
- 16.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Intl J Transgend. 2012;13:165–232.. [Google Scholar]
- 17.Kinsella C, Jr, Landfair A, Rottgers SA, et al. The psychological burden of idiopathic adolescent gynecomastia. Plast Reconstr Surg. 2012;129:1–7.. [DOI] [PubMed] [Google Scholar]
- 18.Suijker J, Troncoso E, Pizarro F, et al. Long-term quality-of-life outcomes after body contouring surgery: Phase IV results for the Body-QoL cohort. Aesthet Surg J. 2018;38:279–288.. [DOI] [PubMed] [Google Scholar]


