Abstract
Background
Breast milk is the most important nutrition for premature babies, but mothers of premature infants have difficulty in initiating and sustaining lactation. Breastfeeding infants who are separated with mothers have decreased morbidity. Nevertheless, such decrease is limited due to insufficient milk supply resulting from mother–baby separation during lac.
Objective
To evaluate the effect of intervention methods based on the health belief model on promoting the secretion of milk among mothers who were separated with their babies.
Methods
In this prospective, randomized controlled clinical trial, we enrolled 260 separation mothers between September 26, 2016 and March 7, 2017, in a 3rd-grade women and children hospital of Chengdu. The mothers all had cesarean delivery and were randomized into 2 groups: the intervention group (educated by investigators based on the health belief) and the control group (routinely educated by obstetric nurses). Data on the onset of lactation and the milk volume during 3 days postpartum were collected. The breast swelling rate within 3 days postpartum and the exclusive breastfeeding rate at 42 days postpartum were compared. The psychologic scores of separation maternal in both groups were assessed with State-Trait Anxiety Inventory at the 3rd day postpartum.
Results
Compared with the control group, the intervention group had significantly earlier lactation time (P < .01), significantly larger milk volume (P < .01) during 24, 24 to 48, and 48 to 72 hours, and significantly lower psychologic scores (P < .01) at the 3rd-day postpartum.
The onset of lactation among mothers who initiated milk expression within 1 hour after childbirth were earlier than those who initiated milk expression between 1 and 6 hours (P < .01); the milk volume within 24-hour postpartum did not differ significantly between the 2 groups (P > .05). However, the milk volume of the early-expression group (<1 hour) was significantly higher than that of the late-expression group (1–6 hours) during 24 to 48 and 48 to72 hours (P < .05).
The breast swelling rate of separation mothers within 3 days postpartum in the intervention group was lower than that in the control group (P < .05). The exclusive breastfeeding rate of mothers in the intervention group was significantly higher than that in the control group (59% vs 35%; P < .01) at 42 days postpartum.
Conclusion
Nursing intervention based on the health belief model can stimulate milk secretion in mothers who were separated with their babies.
Keywords: lactation, maternal, milk expression, mother–baby separation, nursing intervention
1. Introduction
Newborns are sent to Neonatal Intensive Care Unit (NICU) and separated with mothers due to various reasons, such as premature birth, low birth weight, infection, asphyxia, hypoglycemia, jaundice, and other high risk factors.[1–4] Establishing milk supply among mothers who were separated with baby early after childbirth is challenging and crucial,[5] and the provision of human milk is an important component of the premature infant care plan.[6] Because the infants’ gastrointestinal and immunologic systems are immature, breast milk is vital to them in that it contains immunoglobulins, nucleotides, hormones, and bioactive peptides and can thus provide numerous nutrients and vast benefits to the infants.[7] Such benefits include a decreased incidence of necrotizing enterocolitis (NEC), feeding intolerance, and late-onset sepsis,[7–9] as well as improved neurodevelopmental outcomes and decreased length of hospital stay.[10] For mothers, the absence of breastfeeding is associated with increased risks of breast cancer, ovarian cancer, diabetes, hypertension, and myocardial infarction.[11,12] However, the separation mothers are more likely to struggle with the initiation and maintenance of a sufficient breast milk secretion than those mothers whose babies stay with them,[9] with a high risk of breastfeeding failure.[13] An insufficient breast milk secretion is one of the major barriers that compromise breastfeeding in infants who were separated with mothers. It is recommended that breast milk expression should be initiated within 6 hours after childbirth, 8 to 12 times per day.[14]
As a matter of fact, however, numerous separation mothers are struggling with delayed lactogenesis II and inadequate milk volumes; but previous studies were mainly focused on maternal health education, breast care and psychologic intervention during mother–baby separation with small sample size and inadequate theoretical basis. To address these issues, we conducted a randomized controlled trial (RCT) study to determine the effects of education and support intervention on lactation outcomes among mothers who were separated with their babies. Intervention study was based on the health belief model (HBM).
The HBM was proposed by Hochbaum firstly in 1958. It emphasized that health cognition plays a key role in behavior change of individuals, by helping individuals aware of the current factors that affect health could enhance their health beliefs, and take the appropriate health behavior ultimately.[15]
2. Patients and methods
A RCT was carried out in a third-grade women and children hospital of Chengdu between September 26, 2016 and March 7, 2017. Ethical approval was granted by the Institutional Review Board of West China Second University Hospital, Sichuan University, and written informed consent was obtained before enrollment of the participants into the study.
2.1. Sample size estimation
Using the formula of group comparison, the sample size was estimated according to the milk volume of separation mothers in the study performed by Luo et al.[16] Given an α-error of 5% and power of 80%, a sample size of 130 was required in each group. Given the attrition rate of 10%, 286 mothers had to be included in the study, who were divided into 2 equal groups of 143 patients each. Finally, a total of 260 separation mothers completed follow-up, 130 cases in each group (Flow Diagram).
2.2. Participants
About 260 mothers who had gone through cesarean delivery and aged 18 years or above were eligible and were randomized into the intervention group and the control group. The mothers with following situations would be excluded: infants were dead; had sexually transmitted diseases such as human immunodeficiency virus and syphilis; had a history of breast surgery, breast disease, seriously sunken nipple; were too ill to express milk (such as severe postpartum hemorrhage, etc.) or suffering from mental illness which made it difficult for them to cooperate with the researchers; and used drugs that affect lactation (such as some specific antibiotics, sedatives, diuretics) during pregnancy or puerperium.
2.3. Randomization
Randomization was conducted using the computer-generated random sequence number. Each separation mother was assigned to one of the 2 groups. Allocation conducted with opaque sealed envelopes, and we used parallel study design with allocation ratio 1:1. The nurses, the separation mothers and family members were blinded to the group assignment but the investigators were not. Our RCT was registered in the Chinese Cochrane Centre.
2.4. Intervention
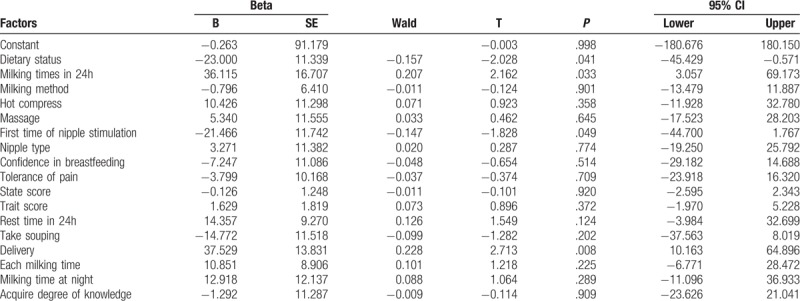
The control group was routinely educated by obstetric nurses while the intervention group was educated by the investigators based on the results of investigation and HBM. In our previous investigation study, multiple linear regression results suggested that the mode of delivery, 1st time nipple stimulation, milking times during 24 hours and mother's daily diet were the independent influencing factors of milk secretion during mother–baby separation. Therefore, in the intervention group, all participants were given a health education handbook developed according to the HBM. The mothers were encouraged to begin the 1st expression within 1 hour after cesarean delivery; however, the initiation of milk expression depended on mothers’ condition, which means that the milk expression could only be done when the mothers felt comfortable with doing it. Before the onset of lactation, all participants in both groups expressed breast milk exclusively by hand, and their milking times are fewer than 3 per day. Then, the participants were asked to switch to double pumping with a hospital-grade electric breast pump (Medela, Inc, McHenry, IL). Participants were instructed to use the breast pump and advised to express milk for 20 to 30 minutes every 2 to 3 hours and to maintain 8 to 12 times per day. Data were documented with regard to the frequency, time, and method of milk expression. Milk volume from each expression was measured by using digital containers (±1 mL), and when the milk amount was less than 1 mL, a sterile syringe was used to measure the volume accurately. Milk amount was measured daily for the first 3 days, the 24-hour milk volume was measured by adding up the volumes of each expression (Table 1)
Table 1.
Multivariate analysis of factors associated with milk volume in separation mother.
Finally, the psychologic scores of separation maternal in both groups were assessed with State-Trait Anxiety Inventory. STAI is a self-assessment scale, which is suitable for group investigation. The reliability structural validity test of the scale showed that the correlation coefficient S-AI of the test–retest score is 0.88 and the T-Al is 0.90. The correlation coefficient between S-AI and T-AI score is 0.84 in the initial test and 0.77 in the retest.[17] It was implemented by hand out the State-Trait Anxiety questionnaire to mothers in both groups on the third day after childbirth.
2.5. Statistical analysis
All obtained data were entered into the Epidata software by double entry. Descriptive analyses were performed using SPSS version 21.0 software (IBM, Armonk, NY). Univariate comparisons of independent data were performed with Student t or the Mann–Whitney U test for continuous variables and the Chi-squared or Fisher exact test for categorical variables. P < .05 was considered statistically significant.
3. Results
3.1. Sample characteristics
Characteristics of mothers are summarized (Table 2). The 2 groups did not differ in maternal age, education, occupation, family per monthly income, maternal history, gestational age, or pregnancy complications (P > .05). The HBM is showed in Figure 1.
Table 2.
Comparison of social demographic data of 2 groups.
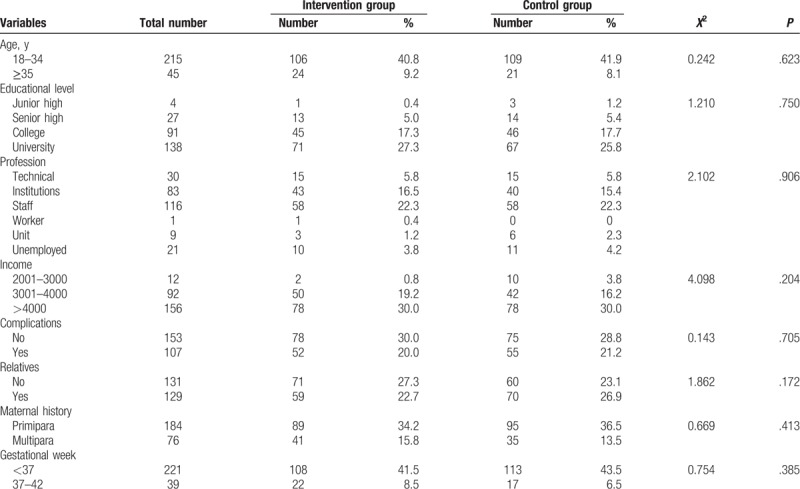
Figure 1.
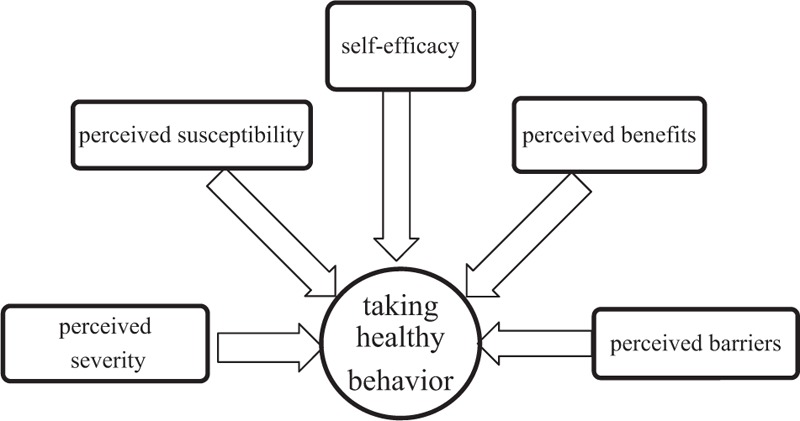
The health belief model emphasized that health cognition plays a key role in behavior change of individual, by helping individuals aware of the current factors that affect health could enhance their health beliefs, and take the appropriate health behavior ultimately.
3.2. Comparison of lactation time within 3 days postpartum, milk volume, and psychologic state between 2 groups
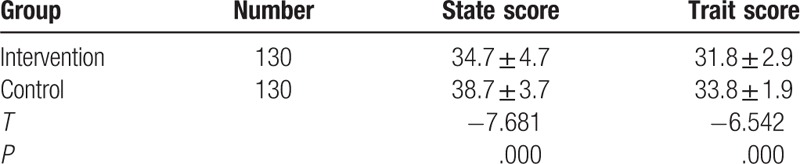
Compared with the control group, the intervention group had significantly earlier lactation time (P < .01) and significantly higher milk volume during 24, 24 to 48, and 48 to 72 hours (P < .01). The psychologic scores of the intervention group were significantly lower than that of the control group (P < .01) in 3 days postpartum (Tables 3 and 4).
Table 3.
Comparison of lactation time (onset) and milk volume between 2 groups.
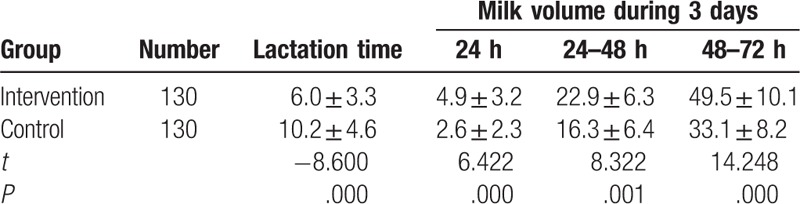
Table 4.
Comparison of psychologic state between 2 groups.
3.3. Comparison of lactation time, milk volume within 3 days postpartum between the early milk expression group (<1 hour) and late milk expression group (1–6 hours) in intervention group
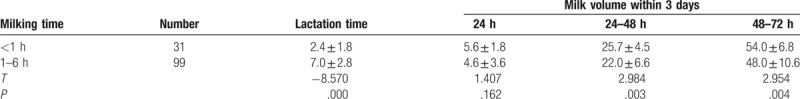
The onset of lactation among mothers who initiated milk expression within 1 hour after birth was earlier than the mothers who did it between 1 and 6 hours (P < .01); the milk volume in 24 hours of postpartum did not differ significantly between these 2 groups (P > .05). However, the milk volume of the early milk expression group (<1 hour) was higher than that of the late milk expression group (1–6 hours) during 24 to 48 and 48 to 72 hours (P < .05) (Table 5).
Table 5.
Comparison of lactation time and milk volume within 3 days postpartum between the early milking mothers (<1 hour) and the late milking mothers (1–6 hours) in the intervention group.
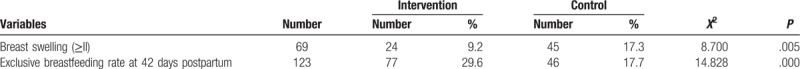
3.4. Comparison of breast swelling rate in 3 days postpartum and exclusive breastfeeding rate in 42 days postpartum between 2 groups
Compared to the control group, the intervention group had a significantly lower breast swelling rate within 3 days postpartum (P < .05) but a significantly higher exclusive breastfeeding rate (59% vs 35%; P < .01).
4. Discussion
In this prospective, randomized, controlled study, the HBM was used to promote the breastfeeding behavior of separated mothers for the 1st time. The HBM holds that whether the individual adopts healthy behaviors mainly depends on the following factors: perceived susceptibility; perceived severity, perceived benefits, and perceived barriers and self-efficacy. It emphasizes that health cognition plays a key role in behavior change of the individual. Following this philosophy, our intervention measures focused on helping individuals become aware of the current factors that affect lactation and breastfeeding. In the intervention group, we have strengthened the theory of breastfeeding for separation mothers, and provided operational guidance at the same time. These efforts ultimately improved the behavioral compliance of maternal behavior greatly.
4.1. Nursing intervention based on the HBM can promote milk secretion
4.1.1. Nursing intervention based on HBM can advance the initiation time of lactation and increase milk volume
In the present study, the initiation time of milk expression was much earlier than the control group (2.0 ± 1.2 hours vs 7.1 ± 3.5 hours) and larger milk volume throughout the first 3 days postpartum. A previous study has shown that initiating milk expression within 6 hours after delivery is associated with higher milk production later on.[18] Luo found in 2012 that initiating milk expression within 2 hours after birth can significantly increase the amount of lactation.[19] Also in 2012, 1 pilot study demonstrated that initiating milk expression within 1 hour after delivery was more effective than between 2 and 6 hours,[20] and could produce more milk at 1 to 3 weeks after delivery among mothers of infants having very low birth weight.[7] But there were no study in previous focused on the mothers of cesarean delivery, which were associated with the delay of lactogenesis stage II,[21] low pumping frequency, and lower milk volume.[6] So, our study focused on the cesarean delivery mothers. In the study, stratification analysis was performed in intervention group for exploring the effect of early milk expression (within 1 hour), and the early milk expressing group with high milk volume. Our results are consistent with results of previous studies, We concluded from the study that beginning milk expression within 1 hour would lead to the early secretion of prolactin, which resulted from the early initiation. In addition, the number of milking sessions in the intervention group was larger than that in the control group at each period of time. It was found that increasing the number of milking could promote the prolactin secrete persistently and help keep it at a high level, thus facilitating the maintenance of lactation. Early initiation of milk expression and frequent milk removal are important factors on the development of adequate milk supply among mothers separated with infants,[5] which are associated with higher milk production later on.[18] This indicates that we should encourage separation mothers to express milk as soon as possible.
4.1.2. Nursing interventions based on HBM can improve the diet of separation mothers after childbirth, and increase milk volume
Studies have confirmed that providing dietary guidance to mothers who were separated with their babies can meet the nutritional needs of the mothers and maintain and promote lactation.[22] It is generally recommended for mothers to fast before and after cesarean section and began to eat a small amount of food after the intestine movement restores and anal exhaust is done, liquid first, semi-liquid next, and general food in the end.[23] This means that the intake of mothers after cesarean section cannot guarantee nutritional needs, which inhibit the secretion of milk. In this study, we provided diet and exercise guidance to separation mothers based on the HBM and instructed the mothers to exercise on bed after assessing their postpartum physical conditions for promoting intestinal peristalsis, increasing appetite, and promoting the secretion of milk indirectly (Table 6).
Table 6.
Comparison of breast swelling rate within 3 days postpartum and exclusive breastfeeding rate within 42 days postpartum between 2 groups.
4.1.3. Nursing interventions based on HBM can relieve anxiety
In the state of mother–baby separation, the inability to perform the mother's role caused anxiety and depression, which leads to a series of changes in the mother's endocrine glandular regulation and central nervous system, and finally inhibits milk secretion.[22] In the present study, the psychologic status and traits scores in the intervention group were lower than those of the control group. We found that psychologic intervention could reduce the negative emotions of the mother and indirectly promote milk secretion. Effective communication can enhance mothers’ confidence of breastfeeding.[24] In the study, we actively talked with separation mothers in the intervention group to learn about their psychologic needs and then provided them with psychologic support accordingly. At the same time, we encouraged family members to help the new mother express and store milk. A study has found that the husband's company and coordination could help the mother to go through this particular period in a more positive way.[25] In addition, mother–baby separation will lead to decrease of breastfeeding compliance.[26] In this study, we provided information support for mothers in the intervention group, informing them of the health condition and treatment progress of the newborns to meet their psychologic needs, which further alleviated the maternal anxiety.
4.2. Nursing interventions based on HBM can promote breastfeeding
4.2.1. Nursing interventions based on HBM can reduce the incidence of breast swelling and pain
In this study, the incidence of breast swelling in the intervention group was lower than that in the control group within 3 days postpartum, suggesting that breast nursing such as breast massage and heat treatment can help clear the obstruction of the breast tubes and thus prevent or alleviate breast swelling and pain, and ultimately promote breastfeeding.
4.2.2. Intervention based on HBM can improve exclusive breastfeeding rate at 42 days postpartum
The results showed that the measures based on the HBM in the intervention group can improve the exclusive breastfeeding rate at 42 days postpartum. Studies performed by Sullivan et al suggested that exclusive breastfeeding can reduce the incidence of NEC by 77% among premature infants,[27] and enhance the feeding tolerance of newborns.[28] It can be concluded that exclusive breastfeeding is essential for the infants who are separated with their mothers. In 2013, He et al intervened to the separation mothers based on the clinical nursing pathway. The results showed that exclusive breastfeeding rates at 42 days postpartum were 57% in the intervention group and 38% in the control group. In our study, exclusive breastfeeding rates at 42 days postpartum were 59% in the intervention group, significantly higher than that in the control group (35%). Compared with the study of He et al, our study excluded the separation mothers of natural delivery, which confirmed the fact that health education based on the HBM could promote the breastfeeding behavior of separation mothers that had cesarean section better.
4.3. Limitations
Our study has several limitations. First, although the 2 groups of mothers were assigned to different rooms randomly by the investigator, the outcomes may have been contaminated by the communication between family members of these mothers because they could move freely around the ward. Second, it remains controversial over the effect of simultaneous or sequential milk expression on improving milk volume. This study was intended to compare the differences between the 2 models of milk expression, but the participants did not adopt a fixed method of expression, which resulted in incomparable data. Third, we did not collect the separation time of each case, which is likely to affect the rate of exclusive breastfeeding within 42 days postpartum.
5. Conclusion
In this prospective, randomized, controlled study, we measured the impact of initiation of milk expression within 1 hour on milk volume and breastfeeding behavior. Nursing intervention based on the HBM is an effective intervention model for separation mothers who choose cesarean section, and it is essential for promoting milk secretion and breastfeeding. Although the medical professionals at the Obstetric Department are aware of mothers’ difficulties and the importance of the volume of milk obtained, little has been studied regarding the conditions most conducive to milk expression. So, future research should pay more attention to this aspect.
Acknowledgments
The authors thank Liu and Li of West China Second University Hospital, Sichuan University for the clinical support and Dong-tao Lin from College of Foreign Languages and Cultures of Sichuan University for editing the manuscript. They are grateful to all mothers who participated in this study.
Author contributions
BRL assisted YL and JRY on formulating the research questions, designing the study and supervising the quality of this manuscript. This intervention was performed by YL, data were collected by YL and JRY, manuscripts was written by YL, and was revised by JRY and BRL.
Conceptualization: Yi Liu, Xinghui Liu, Xiufang Zhao.
Data curation: Yi Liu.
Formal analysis: Yi Liu.
Funding acquisition: Yi Liu.
Investigation: Yi Liu.
Methodology: Yi Liu.
Project administration: biru Luo, Xinghui Liu.
Resources: Jianrong Yao.
Software: Yi Liu.
Supervision: Biru Luo, Jianrong Yao.
Validation: Yi Liu.
Writing – original draft: Yi Liu.
Writing – review & editing: Yi Liu.
Footnotes
Abbreviations: 95% CI = 95% confidence interval, HBM = health belief model, NEC = necrotizing enterocolitis, NICU = neonatal intensive care unit, RCT = randomized controlled trial.
YL and BL contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Thakkar P, Arora K, Goyal K, et al. To evaluate and compare the efficacy of combined sucrose and non-nutritive sucking for analgesia in newborns undergoing minor painful procedure: a randomized controlled trial. J Perinatol 2016;36:67–70. [DOI] [PubMed] [Google Scholar]
- [2].Parkash A, Haider N, Khoso ZA, et al. Frequency, causes and outcome of neonates with respiratory distress admitted to Neonatal Intensive Care Unit, National Institute of Child Health, Karachi. J Pak Med Assoc 2015;65:771–5. [PubMed] [Google Scholar]
- [3].Dean E. Neonatal jaundice. Nurs Stand 2016;30:15. [DOI] [PubMed] [Google Scholar]
- [4].Taryn MDL. An innovative model for achieving breast-feeding success in infants with complex surgical anomalies. J Perinat Neonat Nurs 2010;24:246–53. [DOI] [PubMed] [Google Scholar]
- [5].Lussier MM, Brownell EA, Proulx TA, et al. Daily breastmilk volume in mothers of very low birth weight neonates: a repeated-measures randomized trial of hand expression versus electric breast pump expression. Breastfeed Med 2015;10:312–7. [DOI] [PubMed] [Google Scholar]
- [6].Murase M, Nommsen-Rivers L, Morrow AL, et al. Predictors of low milk volume among mothers who delivered preterm. J Hum Lact 2014;30:425–35. [DOI] [PubMed] [Google Scholar]
- [7].Parker LA, Sullivan S, Krueger C, et al. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med 2015;10:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sisk PM, Lovelady CA, Gruber KJ, et al. Human milk consumption and full enteral feeding among infants who weigh </= 1250 grams. Pediatrics 2008;121:e1528–33. [DOI] [PubMed] [Google Scholar]
- [9].Heon M, Goulet C, Garofalo C, et al. An intervention to promote breast milk production in mothers of preterm infants. West J Nurs Res 2016;38:529–52. [DOI] [PubMed] [Google Scholar]
- [10].Lee TY, Lee TT, Kuo SC. The experiences of mothers in breastfeeding their very low birth weight infants. J Adv Nurs 2009;65:2523–31. [DOI] [PubMed] [Google Scholar]
- [11].Stuebe AM. Enabling women to achieve their breastfeeding goals. Obstet Gynecol 2014;123:643–52. [DOI] [PubMed] [Google Scholar]
- [12].Unar-Munguia M, Torres-Mejía G, Colchero MA, et al. Breastfeeding mode and risk of breast cancer: a dose-response meta-analysis. J Hum Lact 2017;33:422–34. [DOI] [PubMed] [Google Scholar]
- [13].Maastrup R, Hansen BM, Kronborg H, et al. Factors associated with exclusive breastfeeding of preterm infants. Results from a prospective national cohort study. PLoS One 2014;9:e89077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wang Lixin. Breastfeeding Guidance Manual. Beijing: Science and Technology Press; 2012. [Google Scholar]
- [15].Ma X. Health Education. Beijing: People's Medical; 2012. [Google Scholar]
- [16].Luo Wanying, Luo Biru, Guo Xiujing, et al. Study on effect of early nursing intervention on breast milk secretion of mothers separating from their infant. Nur Res 2009;23:1635–6. [Google Scholar]
- [17].Wang Xiangdong, Wang Xilin, Ma Hong. Handbook of Mental Health Rating Scale (updated version). 1999;Beijing: China Mental Health Journal, 238–241. [Google Scholar]
- [18].Nyqvist KH, Häggkvist AP, Hansen MN, et al. Expansion of the baby-friendly hospital initiative ten steps to successful breastfeeding into neonatal intensive care: expert group recommendations. J Hum Lact 2013;29:300–9. [DOI] [PubMed] [Google Scholar]
- [19].Luo Linxue, Wei Guiyuan, Fang Wenzhu, et al. The effects of early regular breast care in maternal lactation with maternal separation. Chongqing Yixue 2012;41:3599–600. [Google Scholar]
- [20].Parker LA, Sullivan S, Krueger C, et al. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol 2012;32:205–9. [DOI] [PubMed] [Google Scholar]
- [21].Nommsen-Rivers LA, Chantry CJ, Peerson JM, et al. Delayed onset of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. Am J Clin Nutr 2010;92:574–84. [DOI] [PubMed] [Google Scholar]
- [22].Zeng Liying. Effect of early breast nursing intervention on lactation of separation maternal. Yixuemeixuemeirong 2015;3:214. [Google Scholar]
- [23].Zhang Jin, Liu Chunyan. The research status of the effect of postpartum mother's separation from their newborns and its nursing intervention. Int J Nurs 2007;26:1121–3. [Google Scholar]
- [24].Meng Weiqing. Experience of promoting successful breastfeeding in clinical nursing. Chin Commun Phys 2013;13:286–7. [Google Scholar]
- [25].He Yumin, Lu Xizhi, Xu Ruoqiao. Maternal separation of clinical nursing path for success rates of maternal breastfeeding and observation. Chin J Trauma Disability Med 2013;21:52. [Google Scholar]
- [26].Hao Minying, Zhang Xueju, Li Mei, et al. Effect of comprehensive nursing intervention on successful breastfeeding of separation maternal from cesarean section. Int J Nurs 2015;34:2943–5. [Google Scholar]
- [27].Sullivan S, Schanler RJ, Kim JH, et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr 2010;156:562–7. [DOI] [PubMed] [Google Scholar]
- [28].Vohr BR, Schanler RJ, Kim JH, et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics 2007;120:e953–9. [DOI] [PubMed] [Google Scholar]


