Abstract
This retrospective study investigated the effect of nursing intervention (NIV) in Chinese patients under preoperative cataract (PC). A total of 70 eligible patients with PC were included. Thirty-five patients in an intervention group received regular clinical treatment and NIV before the surgery, while the other 35 patients received regular clinical treatment only. The NIV was applied 4 sessions, 1 week before the surgery. The primary outcome of satisfaction was measured by 11-points visual analog scale. The secondary outcomes were measured by the functional impairment caused by cataract (the VF-14), cooperativeness during the surgery period, and sleep quality. All the outcome measurements were assessed before and after the surgery. After NIV, patients in the intervention group exerted better outcomes in decreasing anxiety (P < .01), increasing current experience with satisfaction (P < .01), and enhancing the cooperativeness during the surgery period (P < .01), compared to those outcomes in the control group. The results of this study showed that NIV may help increase satisfaction in experience and cooperation, and decrease anxiety in Chinese patients with PC.
Keywords: effect, nursing intervention, preoperative cataract
1. Introduction
Cataract surgery is one of the most widely used interventions for patients with cataract.[1–3] Currently, little research has been explored the preoperative nervous in cataract patients before the surgery, although several studies have reported that patients with preoperative cataract (PC) often suffer from anxiety and fear before the surgery.[4,5] The other studies also reported that patients experienced anxiety and fear throughout the whole operation process.[6,7] Moreover, such condition also results in more adverse events, such as high blood pressure and heart rate.[8,9]
Several interventions are reported to reduce perioperative distress and to overcome its adverse effects from patients with PC.[10–13] However, these treatments still have limited effectiveness for the treatment of patients with PC. Alternative treatment is still needed for patients with PC to prevent and to treat their anxiety and fear before the surgery. Nursing intervention (NIV) is a potential intriguing candidate to treat such condition.[14] Unfortunately, a few clinical studies investigated the effect of NIV for treating patients with PC with anxiety and fear before the surgery. In this retrospective study, we assessed the effect of NIV for the treatment of Chinese patients with PC with anxiety.
2. Methods
2.1. Design
This retrospective study was approved by the Ethical Committee of First Affiliated Hongqi Hospital of Mudanjiang Medical University. It was performed from the March 2016 to December 2017 at the First Affiliated Hongqi Hospital of Mudanjiang Medical University. All patients provided the assigned informed consent.
This study included 70 Chinese patients with PC. Of these, 35 patients underwent NIV plus routine treatment and were assigned to an intervention group. The other 35 subjects received routine treatment alone before the surgery and were assigned to a control group. All outcomes in both groups were evaluated before and after surgery.
2.2. Participants
Patients were included if they were at waiting list of cataract surgery, more than 18 years old, no surgery history of cataract surgery, and healthy hearing ability. However, patients were excluded if they had severe diseases, such as cancers, psychiatric or neurologic conditions, or medications to reduce anxiety before the study. In addition, patients were also excluded if they previously received NIV or had insufficient outcome and characteristic information.
2.3. Intervention
Patients in both groups received regular clinical treatment. Additionally, patients in the intervention group also received NIV by an experienced nurse. The nurse instructed the patients about the anatomy of an eye and its adjacent functional structures, cooperation during the surgery period, as well as the pain management and rehabilitation care after the surgery by the power point and videotapes. Furthermore, the patients were also instructed how to make psychologic preparation and relieve anxiety. Such program was instructed 4 sessions, and 1 week before the surgery.
2.4. Outcome measurements
The primary outcome was measured by 11-points visual analog scale (VAS) to evaluate the satisfaction.[15] The satisfaction consisted of 4 items of anxiety, discomfort, risk, and current satisfaction with experience. Each item was measured by VAS scale independently. The validity and reliability of VAS scales have been established.
The secondary outcomes included visual function, cooperation during the surgery period, and sleep quality. Visual function was measured by the functional impairment caused by cataract (VF-14).[16] It was also validated. The cooperation during the surgery period was measured by a 7-point Likert scale, with 1, totally uncooperativeness; 7, totally cooperativeness. This scale was also validated by the previous study.[17] Additionally, sleep quality was measured before the surgery. All patients were asked “Did you sleep well on the night before the surgery?” with the answer of “YES” or “NO.” VAS and VF-14 were assessed, at baseline, 1 week before and after the surgery. Cooperativeness during the surgery period was measured after the surgery; and sleep quality was evaluated 1-week before and after the surgery.
2.5. Statistical analysis
All characteristics of included patients, and outcome data were analyzed by an experienced statistician using SPSS Statistics 19.0 (IBM Corp, Armonk, NY). Mann–Whitney U test was employed to analyze the count data. Fisher exact test was employed to analyze dichotomous data. P < .05 was defined as a statistical significance.
3. Results
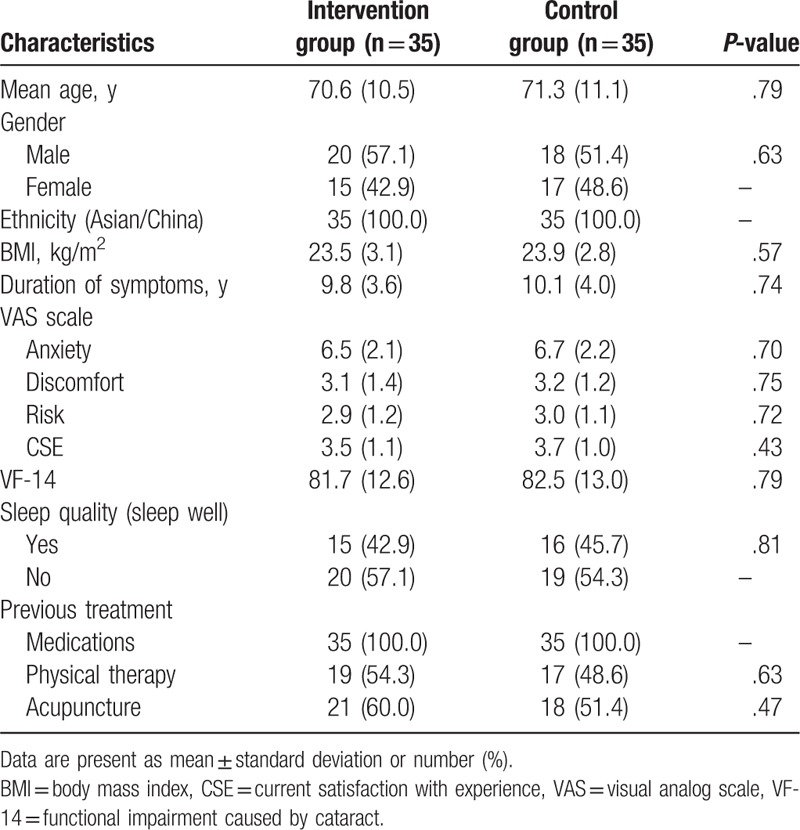
The comparisons of all characteristic values of all included patients are showed in Table 1. There were no significant differences regarding all these characteristics between 2 groups.
Table 1.
Characteristics of included patients.
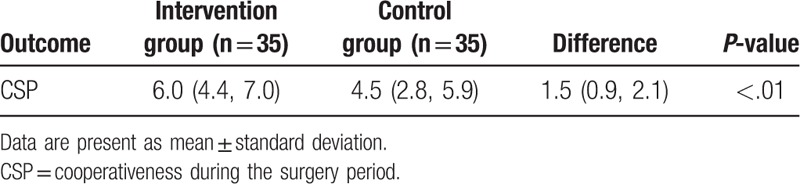
Before and after the surgery, patients in the intervention group exerted better outcomes in anxiety (P < .01, Tables 2 and 3) and current satisfaction with experience (P < .01, Tables 2 and 3), both measured by VAS scale, as well as the cooperativeness during the surgery period, measured by 7-point Likert scale (P < .01, Table 4), compared with patients in the control group.
Table 2.
Change of VAS scale at 1 week presurgery (change from baseline).
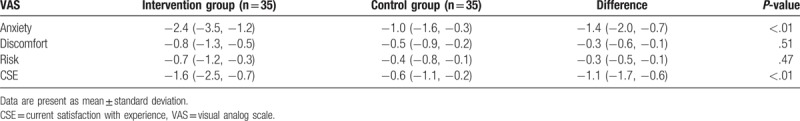
Table 3.
Change of VAS scale after surgery (change from baseline).
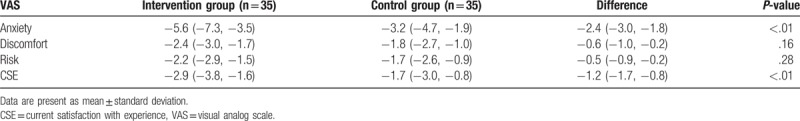
Table 4.
Comparison of cooperativeness during the surgery period between 2 groups.
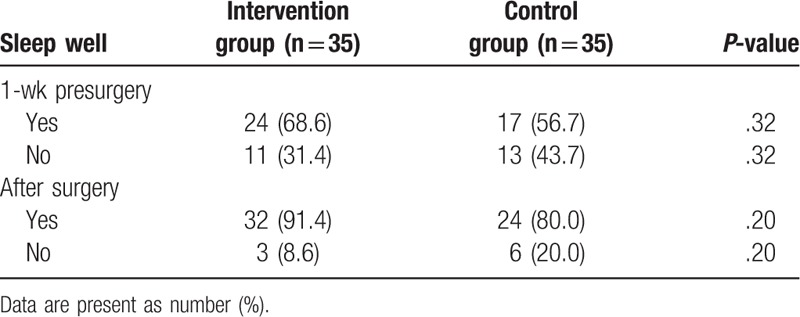
On the contrary, patients in the intervention group did not experience more promising outcomes in discomfort (before, P = .51, Table 2; after, P = .16, Table 3) and risk (before, P = .47, Table 2; after, P = .28, Table 3), measured by VAS scale, and visual function, measure by VF-14 scale before (P = .78, Table 5) and after (P = .51, Table 5) the surgery, respectively; and sleep quality before (P = .32, Table 6) and after (P = .20, Table 6) the surgery, compared with patients in the control group.
Table 5.
Change of VF-14 at 1 week presurgery and after surgery (change from baseline).
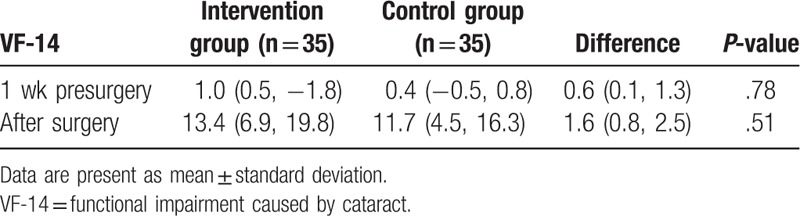
Table 6.
Sleep quality 1 week presurgery and after surgery.
4. Discussion
Presently, no study specifically focuses on the exploration in effect of NIV for patients with PC among Chinese population. Thus, to our best knowledge, this retrospective study firstly investigated the effect of NIV in Chinese patients with PC. We found that NIV may help to increase satisfaction, and improve the cooperativeness of patients with PC.
Previous related studies explored the effect of education in patients with cataract surgery. One study investigated the effects of patient education and therapeutic suggestions in patients with PC.[17] Its results found that patient education intervention benefit for patients prior to cataract surgery.[17] The other study investigated the effect of video for patients with day-stay cataract surgery to evaluate the patient expectations and satisfaction.[13] The results found that video can significantly increase satisfaction with the cataract surgery, and also can reduce anxiety.[13]
The results of this study are partly consistent with the previous study.[13] This study found that patients in the intervention group showed more cooperativeness than patients in the control group. Additionally, patients in the intervention group also exerted better outcomes in anxiety, and satisfaction with experience during the operation period, compared with patients in the control group, although there were no significant differences in discomfort, risk, visual function, and sleep quality between 2 groups.
This retrospective study has several strengths and limitations. This is the first study to explore the effect of NIV in patients with PC among Chinese population, which can provide potential evidence for the clinical practice. As for limitations, the effect of this study is the combination of the NIV and regular clinical treatment, not the NIV alone, although patients in both group received same clinical treatment, which was used to treat PC. Moreover, the sample size is quite small, which may also affect the results of this study. Furthermore, this study is a nonrandomized controlled trial, which may increase the risk of the selection bias. Therefore, all these limitations should be avoided in the future study.
5. Conclusion
The results of this study demonstrated that NIV may benefit to increase satisfaction in experience, and cooperativeness, and also decrease anxiety in Chinese patients with PC. Further studies are still needed to warrant the results of this study.
Author contributions
Conceptualization: Li Zhang, Dan-hui Gong, Jia-feng Liu, Xin Zhao.
Data curation: Xin Zhao.
Formal analysis: Dan-hui Gong.
Investigation: Jia-feng Liu, Xin Zhao.
Methodology: Dan-hui Gong.
Project administration: Li Zhang, Xin Zhao.
Resources: Li Zhang, Xin Zhao.
Software: Dan-hui Gong, Xin Zhao.
Supervision: Li Zhang, Jia-feng Liu, Xin Zhao.
Validation: Jia-feng Liu.
Visualization: Jia-feng Liu.
Writing – original draft: Li Zhang, Dan-hui Gong, Jia-feng Liu, Xin Zhao.
Writing – review & editing: Li Zhang, Dan-hui Gong, Jia-feng Liu, Xin Zhao.
Footnotes
Abbreviations: NIV = nursing intervention, PC = preoperative cataract, VAS = visual analog scale, VF-14 = functional impairment caused by cataract.
The authors report no conflicts of interest
References
- [1].Moraru A, Pînzaru G, Moţoc A, et al. Functional results of cataract surgery in the treatment of phacomorphic glaucoma. Rom J Ophthalmol 2017;61:202–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rewri P, Sharma M, Vats DP, et al. Seroprevalence, risk associations, and cost analysis of screening for viral infections among patients of cataract surgery. Indian J Ophthalmol 2018;66:394–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Chen CL, Clay TH, McLeod S, et al. A revised estimate of costs associated with routine preoperative testing in medicare cataract patients with a procedure-specific indicator. JAMA Ophthalmol 2018;136:231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Foggitt PS. Anxiety in cataract surgery: pilot study. J Cataract Refract Surg 2001;27:1651–5. [DOI] [PubMed] [Google Scholar]
- [5].Marback R, Temporini E, Júnior NK. Emotional factors prior to cataract surgery. Clinics 2007;62:433–8. [DOI] [PubMed] [Google Scholar]
- [6].Nijkamp MD, Kenens CA, Dijker AJM, et al. Determinants of surgery related anxiety in cataract patients. Br J Ophthalmol 2004;88:1310–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nijkamp MD, Ruiter RAC, Roeling M, et al. Factors related to fear in patients undergoing cataract surgery: a qualitative study focusing on factors associated with fear and reassurance among patients who need to undergo cataract surgery. Patient Educ Couns 2002;47:265–72. [DOI] [PubMed] [Google Scholar]
- [8].Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg 1999;89:1346–51. [DOI] [PubMed] [Google Scholar]
- [9].Brody S, Erb C, Veit R, et al. Intraocular pressure changes: the influence of psychological stress and the Valsalva maneuver. Biol Psychol 1999;51:43–57. [DOI] [PubMed] [Google Scholar]
- [10].Tan JF, Tay LK, Ng LH. Video compact discs for patient education: reducing anxiety prior to cataract surgery. Insight 2005;30:16–21. [PubMed] [Google Scholar]
- [11].Cheung D, Sandramouli S. The consent and counselling of patients for cataract surgery: a prospective audit. Eye (Lond) 2005;19:963–71. [DOI] [PubMed] [Google Scholar]
- [12].Gioia L, Cabrini L, Gemma M, et al. Sedative effect of acupuncture during cataract surgery: prospective randomized double-blind study. J Cataract Refract Surg 2006;32:1951–4. [DOI] [PubMed] [Google Scholar]
- [13].Pager CK. Randomised controlled trial of preoperative information to improve satisfaction with cataract surgery. Br J Ophthalmol 2005;89:10–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lara-Smalling A, Cakiner-Egilmez T. Diabetes and cataract surgery: preoperative risk factors and positive nursing interventions. Insight 2014;39:18–20. [PubMed] [Google Scholar]
- [15].Scrimshaw SV, Maher C. Responsiveness of visual analogue and McGill pain scale measures. J Manip Physiol Ther 2001;24:501–4. [DOI] [PubMed] [Google Scholar]
- [16].Steinberg EP, Tielsch JM, Schein OD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol 1994;112:630–8. [DOI] [PubMed] [Google Scholar]
- [17].Kekecs Z, Jakubovits E, Varga K, et al. Effects of patient education and therapeutic suggestions on cataract surgery patients: a randomized controlled clinical trial. Patient Educ Couns 2014;94:116–22. [DOI] [PubMed] [Google Scholar]


