Abstract
Background:
Vascular dementia (VD) is a commonly-seen disease in the elderly. What is more, “Acupuncture at 3-points for intelligence” is one of the most important components of “Jin's three-needle therapy” created by Rui Jin, a professor of Guangzhou University of Chinese Medicine, which can be used in the VD patients. In this article, researchers will assess the clinical efficacy and safety of acupuncture at 3-points for intelligence in the treatment of VD.
Methods:
A systematic literature search for articles up to September 2018 will be conducted using 9 databases: PubMed, Cochrane Library, Embase, CNKI, CBM, VIP, Wanfang database, OASIS, and CiNii. Inclusion criteria are randomized controlled trials (RCTs) of acupuncture at 3-points for intelligence on treating VD. The primary outcome measures will be scores reflecting the neurological function of participants based on common medical scales. Hemorheology indexes, homocysteine (Hcy), acetylcholine (Ach), nitric oxide (NO), and adverse events will also be assessed. Stata V.13.0 software will be used for data synthesis, sensitivity analysis, meta-regression, subgroup analysis, and risk of bias assessment. A funnel plot will be developed to evaluate reporting bias. Egger and Begg tests will be further performed to conduct quantitative evaluation of publication bias and to evaluate the symmetry of funnel plot. We will use the Grading of Recommendations Assessment, Development, and Evaluation system to assess the quality of evidence.
Results:
The results of this systematic review and meta-analysis will be published in a peer-reviewed journal.
Conclusion:
Our study will provide the evidence for the clinical efficacy and safety of acupuncture at 3-points for intelligence in the treatment of VD.
Keywords: acupuncture, meta-analysis, protocol, systematic review, vascular dementia
Key Points
This study will assess the clinical efficacy and safety of acupuncture at 3-points for intelligence in the treatment of Vascular Dementia.
Two reviewers will independently conduct the data extraction and risk of bias assessment.
The Grading of Recommendations Assessment, Development, and Evaluation system will be applied to further evaluate study findings.
There may be a language bias, as both English and Chinese studies will be included.
There may be clinical heterogeneity due to variations in treatment frequency and duration and the use of additional therapies.
1. Introduction
1.1. Description of the condition
With a high incidence in the elderly, vascular dementia (VD) is characterized by chronic brain ischemia and progressive memory decline.[1] Some findings have shown that obesity, underweight, diabetes, hyperlipidemia, smoking, atrial fibrillation, hyperhomocystinemia as well as hypertension are possible vascular risks for VD.[2,3] Besides, the metabolic syndromes, including insulin resistance, hypertension, and dyslipidemia, are connected to lower cognitive performance which increases the odds of dementia onset.[4] And one of the most important pathological factors of VD is poststroke, for the reason that transient ischemic attack does huge harm to cerebral vessels.[5] VD not only shorten human life, but also lower patients and their family's quality of life, even impose economic burden.[5,6] Current evidence represented that antihypertensives and statins might cut down the incidence of dementia.[7] However, there are only few effective therapies for VD which the underlying mechanism of its pathology remains unclear.[1] Fortunately, the ancient Chinese healing technique, acupuncture therapy—acupuncture at 3-points for intelligence, which is a kind of JIN's 3-needle therapy, are widely used in treating VD patients in China.[8] What's more, acupuncture is generally considered safe when performed correctly.[9]
1.2. Description of the intervention
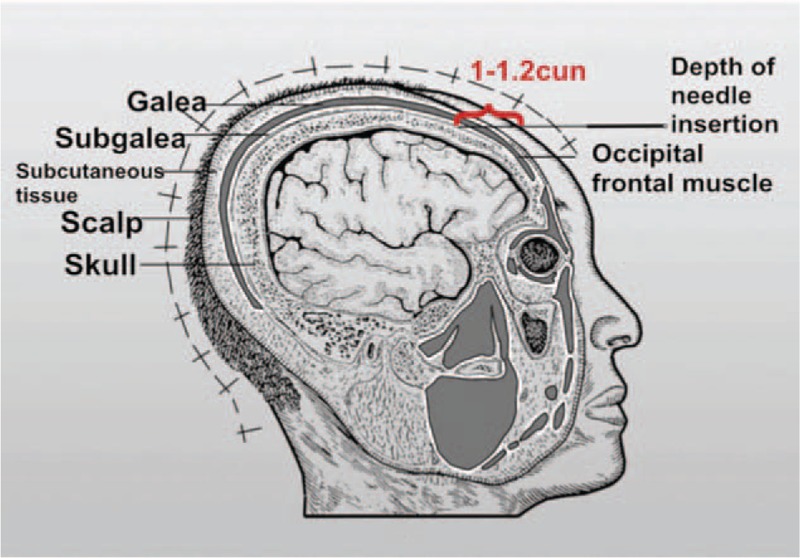
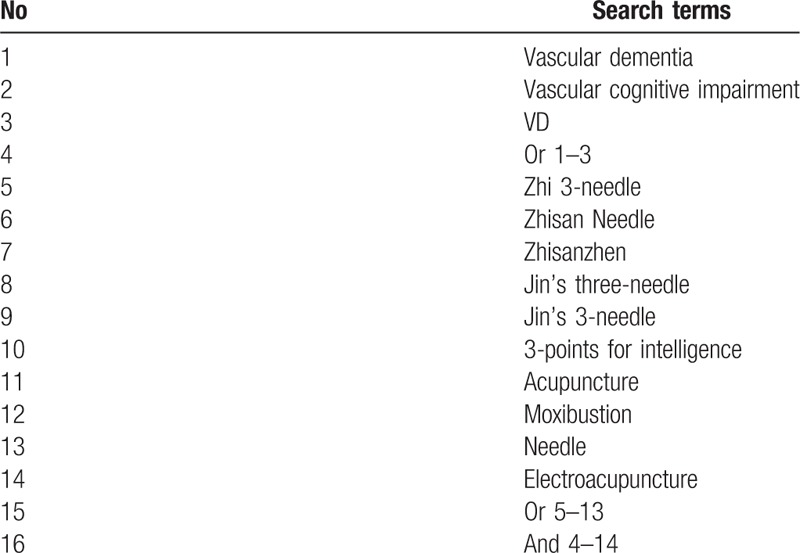
“Acupuncture at 3-points for intelligence” is one of the most important components of “Jin's 3-needle therapy” created by Rui Jin, a professor of Guangzhou University of Chinese Medicine. Acupuncture at 3-points for intelligence is composed of 3 acupoints: Shenting (GV24) and Benshen (GB13,bilateral).[10] GV24 is located on the head, 0.5 cun directly above the midpoint of the anterior hairline. GB13 is located on the head, 0.5 cun above the anterior or hairline, 3 cun lateral to GV24, at the junction of medial two-thirds and lateral third of the line connecting GV24 and ST8, which is shown in Figs. 1 and 2. Cun is defined based on the rules of traditional acupuncture as the width of the interphalangeal joint of the patient's thumb.[11] As it is shown in Fig. 3, needling is done subcutaneously from the front toward the back of the cranium parallel to the midsagittal plane to a depth of 1 to 1.2 cun to the subgalea for adult. The needle will be manipulated by lifting and twirling until the participant feels a sensation (denominated de-qi). Pay attention to avoid any visible subcutaneous cranial veins. When removing the needles one must apply pressure to the needle hold for a while so as to avoid subcutaneous bleeding. The quality of acupuncture depends on the patient's specific condition. Jin's 3-needle therapy has been used to cure children's mental retardation. It is beneficial in improving the children patients’ verbal comprehension, expression ability, hand-eye coordination ability, attention, logical reasoning ability, and visual perception.[12] Furthermore, acupuncture at 3-points for intelligence has been proven to have a definite clinical effect on the treatment of primary insomnia[13] and poststroke depression.[14] Many clinical trials have shown that acupuncture treatment can improve the cognition by removing oxidized biochemical substances and promoting the release of neurotransmitters, which revealed that the mechanism of promoting angiogenesis in acupuncture and moxibustion is the core of VD treatment.[15,16] There have been no relevant systematic reviews and meta-analyses on the effects of acupuncture at 3-points for intelligence on the treatment of VD. In addition, there is insufficient evidence to support the widespread application of acupuncture at 3-points for intelligence on the treatment of VD. Consequently, an exploration of this therapy's effect on VD is needed. In this study, researchers plan to conduct a systematic review and meta-analysis to evaluate current evidence on the effects of acupuncture at 3-points for intelligence on VD.
Figure 1.
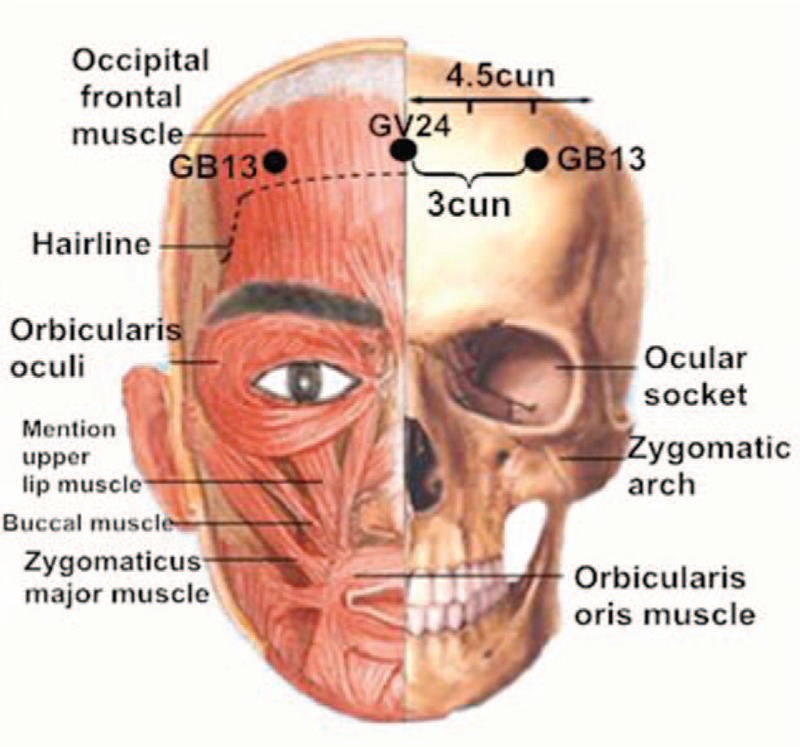
The anatomical location of GV24 and GB13.
Figure 2.

The location of GV24 and GB13.
Figure 3.
Depth of needle insertion of GV24 and GB13.
Researchers will include randomized controlled trials (RCTs) with no language restrictions that compare the effects of acupuncture or electroacupuncture with usual care or placebo acupuncture.
2. Methods and analysis
2.1. Eligibility criteria
2.1.1. Study type
We will include all RCTs to assess the safety and efficacy of acupuncture at 3-points for intelligence therapy in the treatment of vascular dementia, regardless of the course of treatment, the age, course of disease, gender, and ethnicity of the patients. There is no restriction on language or publication status.
2.1.2. Participants
We will select patients with both cerebrovascular disease and dementia, in which cerebrovascular disease is the prominent but not the only absolute cause of dementia. All patients should be diagnosed as VD according to at least one of the current or past definitions or guidelines of VD, such as:
-
1.
Diagnostic and Statistical Manual of Mental Disorder 4th, DSM-IV.
-
2.
National Institute of Neurological Disease and Stroke—Association Internationale pour la Rechercheer l’Enseignement et Neurosciences, NINDS-AIREN.
-
3.
International Classification of Disease, ICD-10-R.
-
4.
Alzheimer disease diagnosis and treatment center, ADDTC.
There will be no limitation on age, sex, and ethnicity of participants.
2.1.3. Types of interventions
2.1.3.1. Experimental interventions
We will include RCTs using only acupuncture at 3-points for intelligence (including ordinary acupuncture and electroacupuncture) or acupuncture at 3-points for intelligence with routine treatment of the control group. The difference between acupuncture at 3-points for intelligence and traditional acupuncture is that the traditional acupuncture involves inserting needles into classic acupoints of traditional meridian, while acupuncture at 3-points for intelligence only select 3 acupoints at a time, Shenting (GV24) and Benshen (GB13, bilateral). Some RCTs will be excluded (for example, fine needle, electrical stimulation, or hand). There is no restriction on the length and frequency of treatment.
2.1.3.2. Comparator interventions
The control intervention will include sham acupuncture, placebo acupuncture, no treatment, medication (such as acetylcholinesterase inhibitors, excitatory amino acid antagonists, butylphthalide), or other active treatments (such as, lifestyle, dietary modification).
We will analyze the following comparisons:
-
1.
Acupuncture at 3-points for intelligence monotherapy compared with sham or placebo treatment.
-
2.
Acupuncture at 3-points for intelligence monotherapy compared with black control group.
-
3.
Acupuncture at 3-points for intelligence plus another medication or active treatment compared with another medication or active treatment.
-
4.
Acupuncture at 3-points for intelligence plus another medication or active treatment compared with sham or placebo treatment plus another medication or active treatment.
2.1.4. Outcome measures
The primary outcome measurement will be scores reflecting the neurological function of participants based on certain common scales: minimental state examination (MMSE), Activity of Daily Living Scale (ADL), Montreal Cognitive Assessment (MoCA), Hachinski Ischemic Scale (HIS), Hastgawa Dementia Scale (HDS), Blessed dementia scale (BDS), National Institutes of Health Stroke Scale (NIHSS), Hamilton depression scale (HAMD) and so on.
The secondary outcome measurement will be hemorheology indexes, Hcy, Ach, NO, and adverse events.
2.2. Information sources
2.2.1. Search strategy and identification of studies
We will retrieve literature in the following databases from their respective inception to September 2018: PubMed, Cochrane Library, Embase, 4 Chinese databases (CNKI, CBM, VIP, and Wanfang database), 1 Korean medical database (OASIS), and 1 Japanese medical database (CiNii). The search terms will be “vascular dementia” OR “vascular cognitive impairment” OR “VD” AND “Zhi 3-needle” OR “Zhisan Needle” OR “Zhisanzhen” OR “Jin's 3-needle” OR “Jin's 3-needle” OR “3-points for intelligence” OR “acupuncture” OR “moxibustion” OR “needle” OR “electroacupuncture.” The Chinese, Japanese and Korean translations of these terms will be used for databases search of corresponding countries. The search strategy for PubMed is given in Table 1.
Table 1.
Search strategy utilized for the PubMed database.
Two reviewers (TL and ZS) will independently scan the full texts of potential eligible studies. A third reviewer will discuss and settle the discrepancies about inclusion in the meta-analysis. And we will produce Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart to set out the number of articles identified, screened, included, and excluded. Reasons for exclusion and ascertaining eligible studies will also be shown. The study selection process will completely be stated in a PRISMA flow chart (http://www.prisma-statement.org) (Fig. 4).
Figure 4.
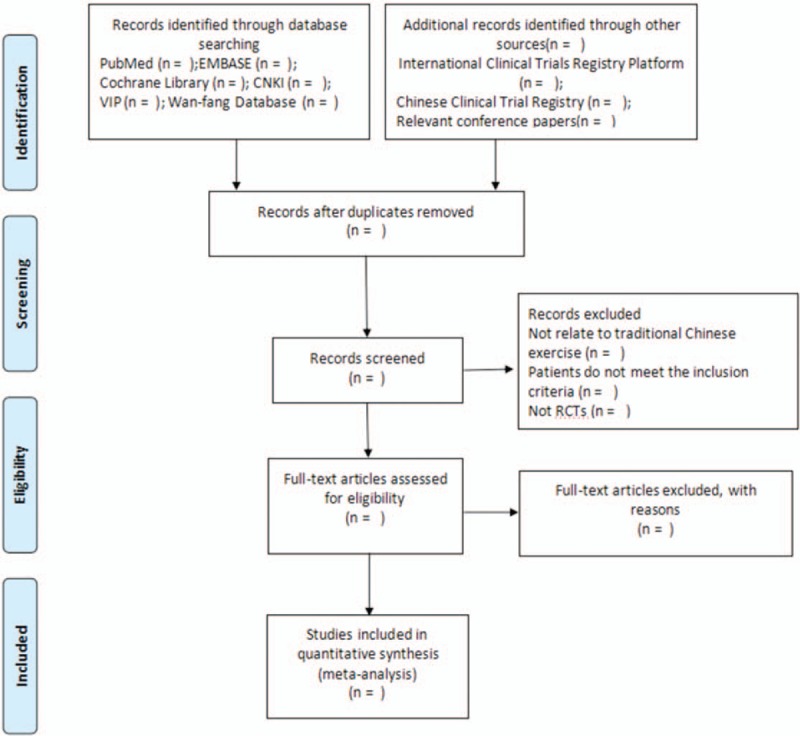
Flow diagram of the study selection process.
2.2.2. Study selection
We will exclude articles of which no data on scales outcomes are presented, results are reused, or related information are not available. Two reviewers (TL and ZS) will independently screen titles and abstracts to select potential references according to the criteria mentioned above. If necessary, reviewers will examine full texts to identify eligible studies. Endnote V.X7 software will be utilized to manage literature and remove duplicate literature.
2.3. Data extraction
The reviewers will extract the characteristics of the included studies (about the subjects, interventions, results) by using a self-developed data extraction table. The following items will be included in the data extraction form: title, first author, funding year of publication, country of study, design, inclusion and exclusion criteria, methods of randomization, allocation concealment, age, sex, sample size, dose, follow-up time points, compliance, primary and secondary outcomes, method of outcome assessments, blinding of outcome assessment, adverse events. Any disagreement will be resolved by consensus or consultation with the third reviewer.
2.3.1. Addressing missing data or unclear measurement scales
If necessary, we will attempt to contact authors of studies by email or telephone for missing data or clarification about evaluation scales. If we could not obtain sufficient information in this way, we will analyze the available data. We will try to evaluate the potential influence of missing data on the review results (in the Discussion section).
2.4. Risk of bias in included studies
Risk of bias for each included RCTs will be assessed by 2 authors (ML and SJ) according to the Cochrane Handbook for Systematic Reviews of Interventions. This recommends the assessment of several sources of bias, including selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. We will try to describe the risk of bias reported in each study. Thus, we will be able to judge the risks as low, high, or unclear (unclear or unknown risk of bias). If necessary, we will contact authors of included articles for further information.
2.5. Statistical analysis
2.5.1. Data synthesis and analysis
Stata V.13.0 software will be applied for data analysis. 95% CIs and weighted mean differences will be calculated. Risk ratio with 95% CIs will be used to express the estimate of the effect for dichotomous outcomes. For continuous outcomes, we will express the estimate of the effect as mean difference with 95% CIs. The Q and I2 test statistics will be performed to evaluate the heterogeneity of the included studies. For the Q statistic, P < .05 will be considered as indicating significant differences. For the I2 statistic, I2 < 25% indicates no significant heterogeneity, I2 = 25% to 50% is considered moderate heterogeneity and I2 > 50% indicates strong heterogeneity. If there is heterogeneity, data will be analyzed with the random effects models, otherwise, the fixed effects models will be adopted.
2.5.2. Additional analyses
We will explore the possible sources of heterogeneity by conducting sensitivity analysis, partial sequence analysis, and subgroup stratification analysis. The process needs to be implemented according to the different research features, such as research types, locations, racial difference, sample size, gender differences, quality of research, adjustable or unadjustable confounding factors, treatment, and other related parameters. If the extracted data is insufficient for quantitative analysis, qualitative analysis will be carried out.
2.5.3. Assessment of reporting biases
A funnel plot will be developed using software to qualitatively assess the reporting bias of the included studies. We will further use Egger and Begg tests to conduct quantitative evaluation of publication bias and to evaluate the symmetry of funnel plot. We interpret the value of P < .1 as having statistical significance (i.e., publication bias).
2.6. Quality of evidence
The quality of the evidence of the included studies will be evaluated according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach. Due to the possible limitations of the study, inconsistencies, inaccuracies, indirect evidence and reporting bias, the quality of evidence for each study will be graded as 4 levels: high, moderate, low, or very low.
3. Ethics and dissemination
Our expected goal is to publish this systematic review and meta-analysis in a peer-reviewed journal. Our article will provide information on the safety and efficacy of acupuncture at 3-points for intelligence in treating VD patients compared with other conventional treatments. This study will not involve participants’ privacy, therefore ethical approval is not required.
4. Discussion
Acupuncture at 3-points for intelligence is a form of acupuncture that has been used in clinical practice for more than 30 years in China.[17] Acupuncture at 3-points for intelligence is effective and safe which is suitable for patients with VD.[18,19] In particular, the effect of electroacupuncture at 3-points for intelligence on VD is extremely significant.[20] Previous studies have indicated that acupuncture at 3-points for intelligence can obviously improve the intelligence level and cognitive function of patients with VD. The incubation stage of cognitive evoked potential P300 and the amplitude of N2 and –P8b are significantly improved, indicating that the cognitive functions of patients are significantly ameliorated.[16] One study has reported that acupuncture is considered a preferable alternative pharmacotherapy for treating relevant outcomes in dementia such as behavioral disturbances.[21] Research has also reflected a beneficial effect of additional acupuncture on cognitive status and activities of daily living for VD patients.[22]
Acupuncture at 3-points for intelligence has been developed to treat VD, but the efficacy of the therapy compared with medications for VD is unknown. From a medical perspective, treatments, and/or management of dementia and its prevention require a long-term care rather than short-term intensive treatment. Therefore, compliance, economic costs, safety, and efficacy of the interventions are quite important. The purpose of this review is to systematically assess the effect of acupuncture at 3-points for intelligence on treating VD. We aim to collect enough studies to ensure the meta-analysis more convincing. We expect to find that acupuncture at 3-points for intelligence therapy has a positive effect on the treatment of VD. In summary, this review will be the first to evaluate the impact of acupuncture at 3-points for intelligence on the treatment of VD. The results of this review may help to establish a better approach to treat VD and provide reliable evidence for its extensive application.
Author contributions
WS, ML, and DX conceived the study and drafted the protocol. JL, CJ, LZ, and WW revised it. TL, ZS, YX, SJ, and LW developed the search strategies, conducted data collection, and analyzed independently. All authors have approved the final manuscript.
Conceptualization: Tong Lin, Danghan Xu.
Formal analysis: Zhizhong Sun, Liang Zheng.
Investigation: Shuliang Ji.
Methodology: Yizi Xie, Lin Wang.
Resources: Tong Lin.
Software: Jietao Lin.
Writing – original draft: Weipeng Sun, Minying Li.
Writing – review & editing: Chao Jia, Wei Wu.
Footnotes
Abbreviations: Ach = acetylcholine, ADL = activity of daily living scale, BDS = blessed dementia scale, GB = the gall bladder channel of foot-shaoyang, GRADE = grading of recommendations assessment, development, and evaluation, GV = governor vessel, HAMD = Hamilton depression scale, Hcy = homocysteine, HDS = Hastgawa Dementia Scale, HIS = Hachinski Ischemic Scale, MMSE = mini-mental state examination, MoCA = Montreal cognitive assessment, NIHSS = National Institutes of Health Stroke Scale, NO = nitric oxide, PRISMA = preferred reporting items for systematic reviews and meta-analysis, RCTs = randomized controlled trials, VD = vascular dementia.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
Ethics and dissemination: Ethical approval and informed consent are not required, as the study will be a literature review and will not involve direct contact with patients or alterations to patient care.
Trial registration: The protocol for this review has been registered in the PROSPERO network (registration number: CRD42018107152).
WS, ML, and TL contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].O’Brien JT, Thomas A. Vascular dementia. Lancet 2015;386:1698–706. [DOI] [PubMed] [Google Scholar]
- [2].Hasnain M, Vieweg WV. Possible role of vascular risk factors in Alzheimer's disease and vascular dementia. Curr Pharm Des 2014;20:6007–13. [DOI] [PubMed] [Google Scholar]
- [3].Sahathevan R, Brodtmann A, Donnan GA. Dementia, stroke, and vascular risk factors; a review. Int J Stroke 2012;7:61–73. [DOI] [PubMed] [Google Scholar]
- [4].Yates KF, Sweat V, Yau PL, et al. Impact of metabolic syndrome on cognition and brain: a selected review of the literature. Arterioscler Thromb Vasc Biol 2012;32:2060–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kalaria RN, Akinyemi R, Ihara M. Stroke injury, cognitive impairment and vascular dementia. Biochim Biophys Acta 2016;1862:915–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Van De Vorst IE, Vaartjes I, Geerlings MI, et al. Prognosis of patients with dementia: results from a prospective nationwide registry linkage study in the Netherlands. BMJ Open 2015;5:e008897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Barca ML, Engedal K, Laks J, et al. Quality of life among elderly patients with dementia in institutions. Dement Geriatr Cogn Disord 2011;31:435–42. [DOI] [PubMed] [Google Scholar]
- [8].Larsson SC, Markus HS. Does treating vascular risk factors prevent dementia and Alzheimer's Disease? A systematic review and meta-analysis. J Alzheimers Dis 2018;64:657–68. [DOI] [PubMed] [Google Scholar]
- [9].Li J, Zhang X, Han J. Treatment for vascular dementia by acupuncture and moxibustion. J Clin Acupuncture Moxibustion 2012;3:72–4. [Google Scholar]
- [10].Chan M, Wu X, Wu J, et al. Safety of acupuncture: overview of systematic reviews. Sci Rep 2017;7:3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Melchart D, Streng A, Hoppe A, et al. Acupuncture in patients with tension-type headache: randomized controlled trial. BMJ 2005;331:376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zeng X, Li Q, Xu Q, et al. Acupuncture mechanism and redox equilibrium. Evid Based Complement Alternat Med 2014;2014:483294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Huang X, Yuan Q, Luo Q, et al. Clinical efficacy on mental retardation in the children treated with JIN's three scalp needling therapy and the training for cognitive and perceptual disturbance. Zhongguo Zhen Jiu 2015;35:651–6. [PubMed] [Google Scholar]
- [14].Yang H, Huang F, Kuang W, et al. Efficacy of acupuncture at Zhisanzhen in treatment of primary insomnia: a report of 35 cases. J Anhui Univ Chin Med 2014;3:74–6. [Google Scholar]
- [15].Tian X, Zhang Q, Xu S. A study of clinical efficacy evaluation of Zhisanzhen as primary acupuncture in treating patients with post-stroke depression. Chin J Integr Traditional Western Med Intensive Crit Care 2011;4:219–21. [Google Scholar]
- [16].Xie F, Xu Z, Xiong X. Effect of mental tri-needle electro-acupuncture on postoperative cognitive function in elderly patients after hip joint replacement surgery. J Guangzhou Univ Traditional Chin Med 2016;6:813–7. [Google Scholar]
- [17].Li Q, Li L, Xu Q, et al. Effect of electroacupuncture at Zhisanzhen on cognitive function and ability of life activity in patients with vascular dementia. Chinese J Pract Nervous Dis 2015;8:1–2. [Google Scholar]
- [18].Jin R, Lai X, Wang S. Clinical observation on 558 cases of mentally retarded children treated with Sishen needle and Zhi three-needle. Zhong Guo Zhen Jiu 1992;2:3–5. [Google Scholar]
- [19].Zhou F, Zeng K. Clinical study of Zhi three-needle combined with hyperbaric oxygen in the treatment of vascular dementia. Hunan J Traditional Chin Med 2015;8:82–3. [Google Scholar]
- [20].Tang Z, Lu Y, Song H, et al. Effects of electroacupuncture at Zhi three- needle on learning and memory ability and β-Amyloid expression in VD rats. Chinese J Gerontol 2012;13:2794–6. [Google Scholar]
- [21].Abraha I, Rimland JM, Trotta FM, et al. Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. BMJ Open 2017;7:e012759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shi G, Li Q, Yang B, et al. Acupuncture for vascular dementia: a pragmatic randomized clinical trial. Scientific World J 2015;2015:161439. [DOI] [PMC free article] [PubMed] [Google Scholar]


