Abstract
Background
Maintaining optimal intracuff pressure of the endotracheal tube is important during airway management. Rotation of the head can affect the cuff pressure of the endotracheal tube. We investigated the change in cuff pressure and the degree of tube displacement according to the direction of head rotation (toward the same side vs opposite side of tube fixation) using a TaperGuard endotracheal tube.
Methods
We conducted a prospective study in 58 patients, aged 18 to 70 years, who underwent tympanomastoidectomy under general anesthesia. TaperGuard endotracheal tube was secured at the corner of the mouth, either on the same side as that of the head rotation (Group S, n = 29) or on the opposite side (Group O, n = 29). After endotracheal intubation, the endotracheal tube cuff pressure was set at 22 cmH2O in the neutral position of the head. The cuff pressure was measured again after lateral rotation of the head and readjusted to 22 cmH2O. In addition, the change in distance from the carina to the tip of the endotracheal tube was measured before and after the change in position. The incidences of cough, sore throat, and hoarseness were assessed at 30 minutes, 6 hours, and 24 hours after surgery.
Results
There were no differences between groups in terms of patient characteristics and duration of anesthesia. The change in cuff pressure after head rotation in Group S (8.07 ± 1.07 cmH2O) was greater than that in Group O (2.24 ± 0.95 cmH2O) (P < .001). In addition, 21 (72.4%) patients in Group S and no patient in Group O had pressures above 30 cmH2O (P < .001). Furthermore, the tube tip moved away from the carina by 8.55 ± 7.01 mm in Group S and by 2.83 ± 4.72 mm in Group O (P < .001).
Conclusion
Fixation of the TaperGuard endotracheal tube on the side contralateral to head rotation was associated with a smaller intracuff pressure increase and lesser tube displacement compared to fixation of the tube on the ipsilateral side.
Keywords: cuff, endotracheal tube, intubation, lateral rotation, pressure
1. Introduction
Maintaining optimal intracuff pressure of the endotracheal tube is important. Cuff pressures above the optimal range (20–30 cmH2O) can cause adverse events such as sore throat, cough, and nerve palsy. In extreme cases, tracheal fistula or rupture may occur, which are serious complications as they can decrease the blood supply to the tracheal mucosa.[1,2] In contrast, cuff pressures under the optimal range can cause inadequate ventilation, microaspiration, ventilator-associated pneumonia, and contamination of the operating room by anesthetic gases.[3,4]
It has been suggested that the newly developed TaperGuard endotracheal tube (Covidien, Athlone, Ireland) can achieve adequate ventilation as it has better sealing characteristics and reduced cuff pressures compared to the conventional cylindrical endotracheal tube.[5,6] However, in 1 study, the cuff pressure was higher in the TaperGuard endotracheal tube than in the cylindrical endotracheal tube after head rotation.[7] The same study showed that head rotation toward the side of tube fixation increased the cuff pressure and resulted in withdrawal of the tip of the TaperGuard tube.[7] Moreover, in a study by Kim et al, where a cylindrical endotracheal tube was used, the tube tip was displaced away from the carina when the head was rotated toward the side of tube fixation; when the head was rotated toward the opposite side, the tube was displaced in an inconsistent manner, showing no movement, withdrawal, or advancement of the tube tip.[8] In the study by Kim et al, only the tube position was assessed in relation to head rotation, whereas changes in cuff pressure were not observed; moreover, they used a conventional cylindrical endotracheal tube.[8] Therefore, we decided to assess the change in cuff pressure and tube displacement based on the direction of head rotation using a TaperGuard endotracheal tube.
In this study, we investigated the pressure change of the cuff and the degree of tube displacement of a TaperGuard endotracheal tube based on the direction of head rotation (toward the same side vs opposite side of tube fixation).
2. Methods
After approval by the Ethics Committee of Kyungpook National University Hospital (KNUH 2017-12-001-002), this study was registered at Clinical Trials.gov (NCT03524586). We obtained written informed consent from all patients.
Fifty-eight patients with American Society of Anesthesiologists physical status classification I to III and aged 18 to 80 years undergoing tympanomastoidectomy under general anesthesia were enrolled in this study. Exclusion criteria included a history of difficult intubation, limited neck movement, neck pain, and body mass index more than 35 kg/m2.
A physician who was not involved in perioperative care divided the patients into 2 groups by computer-generated randomization as follows: Group S (n = 29), wherein the endotracheal tube was secured at the corner of the mouth on the same side as that of the head rotation, and Group O (n = 29), wherein the endotracheal tube was secured on the opposite side of head rotation. The attending anesthesiologist was informed about the group allocation prior to anesthesia. Endotracheal intubation was performed using a TaperGuard endotracheal tube with an inner diameter of 7 mm in female patients and 7.5 mm in male patients by the same anesthesiologist. The anesthesiologist also measured the cuff pressure and the distance between the tube tip and the carina during the study period.
Using standard monitoring protocols in the operating room, anesthesia was induced with propofol (2 mg/kg), rocuronium (0.8 mg/kg), and a continuous infusion of remifentanil (0.05–0.1 μg/kg/min). Endotracheal intubation was performed by direct laryngoscopy. The tip of the tube was placed 4 cm above the carina using a fiberoptic bronchoscope (FOB), and the tube was fixed at the corner of the mouth either on the same side as that of head rotation or on the opposite side. The cuff of the endotracheal tube was inflated with air and the patients received mechanical ventilation in volume-controlled mode (tidal volume of 8 mL/kg and respiratory rate of 10 to 12 cycles/min to maintain the end-tidal carbon dioxide tension between 30 and 35 mm Hg). Anesthesia was maintained with sevoflurane with 50% oxygen in air and remifentanil. The cuff pressure was set at 22 cmH2O using a manometer (Mallinckrodt Medical, Hennef, Germany) in the neutral position of the head, and it was checked again after rotating the patient's head laterally. If there was a significant change in cuff pressure after positioning the head (below 20 cmH2O or above 30 cm H2O), then the cuff pressure was readjusted to 22 cmH2O by regulating the cuff volume. The distance between the tube tip and the carina was obtained using an FOB and the difference in distance based on the direction of the head rotation was recorded. Symptoms such as sore throat, hoarseness, and cough were assessed at 30 minutes, 6 hours, 12 hours, and 24 hours postoperatively. The primary outcome was the change in cuff pressure after head rotation. Secondary outcomes were the distance between the tube tip and the carina, and the incidence of postoperative complications.
The sample size was calculated based on a preliminary study that revealed that the change of cuff pressure of the TaperGuard endotracheal tube was 9 ± 2.3 cmH2O (mean ± standard deviation) with the tube fixed on the same side as that of head rotation. We presumed a 30% difference in the mean cuff pressure between the groups to be significant. Therefore, at least 23 patients per group would be required to achieve a power of 0.9 and α of 0.01. Considering a 20% dropout rate, 29 patients in each group would be required.
The SPSS software (SPSS, Chicago, IL) was used for statistical analysis. Student t test, Chi-squared test, and Fisher exact test were used as appropriate. P < .05 was considered statistically significant.
3. Results
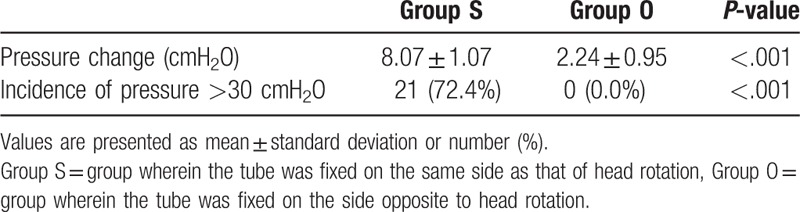
Fifty-eight patients were randomly divided into 2 groups (Fig. 1). There were no differences in terms of patient characteristics and duration of anesthesia (Table 1). The change in cuff pressure after head rotation in Group S (8.07 ± 1.07 cmH2O) was greater than that in Group O (2.24 ± 0.95 cmH2O) (P < .001) (Table 2). In addition, 21 (72.4%) patients in Group S had cuff pressures above 30 cmH2O, whereas no patient in Group O had cuff pressure over 30 cmH2O (P < .001) (Table 2).
Figure 1.
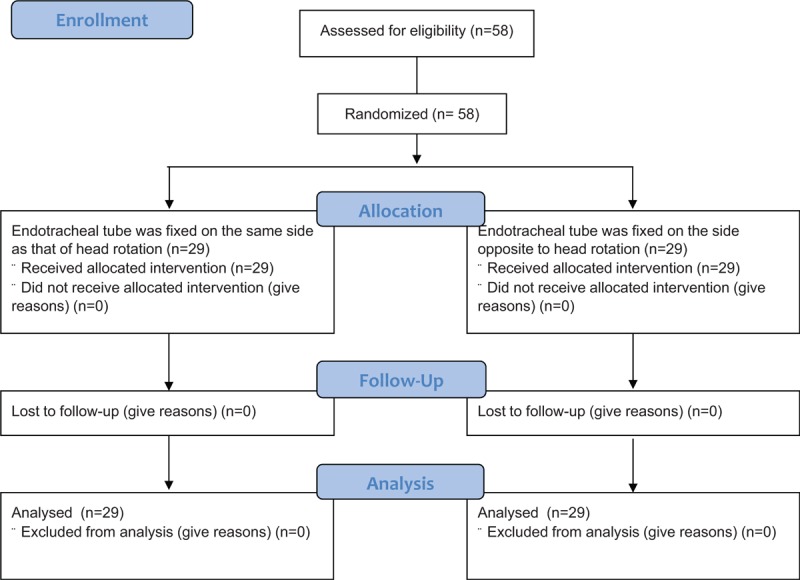
Flow diagram of the study design.
Table 1.
Demographics of the study patients (N = 58).
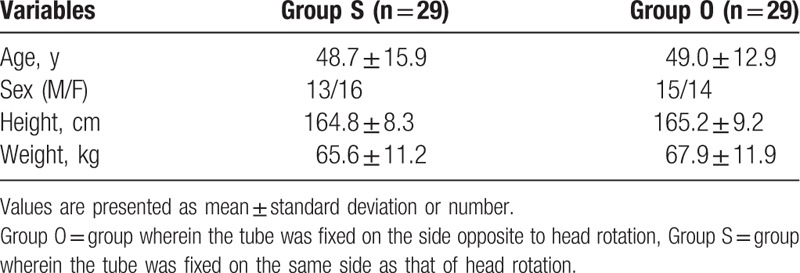
Table 2.
The change in cuff pressure after head rotation.
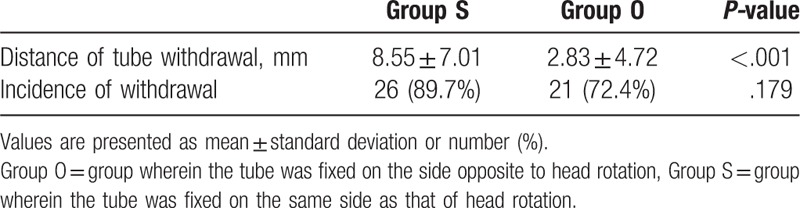
The tube tip moved away from the carina by 8.55 ± 7.01 mm with head rotation toward the same side of tube fixation (Group S) and by 2.83 ± 4.72 mm with head rotation to the opposite side (Group O) (P < .001) (Table 3). Withdrawal of the tube tip was seen in 26 (89.7%) patients in Group S and in 21 (72.4%) patients in Group O (Table 3).
Table 3.
Withdrawal of the tube tip after head rotation.
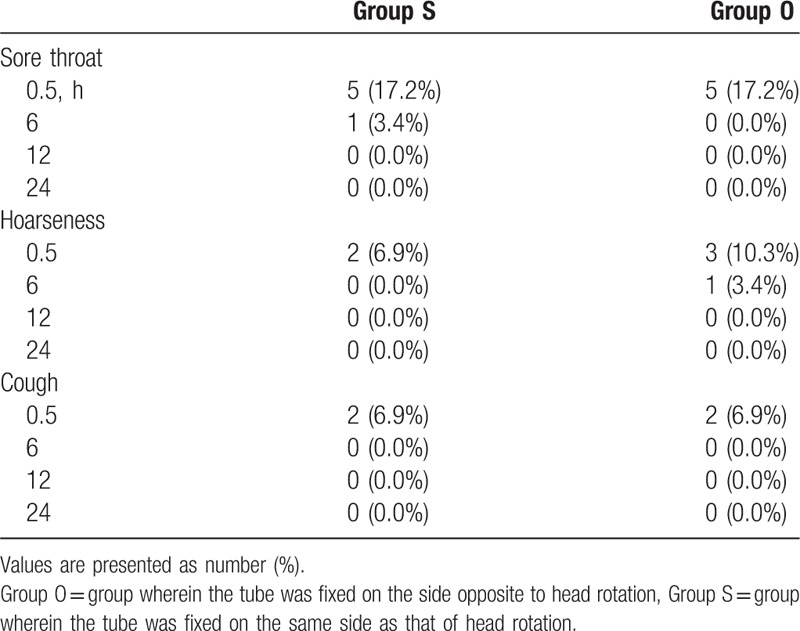
The incidence of sore throat, hoarseness, and cough was not significantly different between the 2 groups at each time point (30 minutes, 6 hours, 12 hours, and 24 hours postoperatively) (Table 4).
Table 4.
Incidence of sore throat, hoarseness, and cough.
4. Discussion
In this study, we investigated the pressure change of the cuff and the degree of tube displacement of a TaperGuard endotracheal tube based on the direction of head rotation. We found that the intracuff pressure of the TaperGuard endotracheal tube increased more with head rotation toward the same side of tube fixation than with head rotation to the opposite side. We also observed that the extent of withdrawal of the tube tip from the carina was greater with head rotation toward the same side of tube fixation than with head rotation to the opposite side.
The function of a tube cuff is to provide proper sealing between the trachea and the endotracheal tube, which prevents aspiration of oral contents into the lung and air leakage during positive pressure ventilation.[1] Maintaining adequate intracuff pressures in tracheally intubated patients is of great concern since both over and under inflation of the cuff can lead to several complications.[9,10] For example, excessive cuff pressure can cause various complications, such as ischemia of the tracheal mucosa and postoperative discomfort due to sore throat and hoarseness.[9,11,12] In contrast, low cuff pressures can cause air leakage and aspiration, which can lead to ventilator-associated pneumonia, with its associated increased morbidity and mortality.[3,4] Thus, in intubated patients, it is important to maintain the lowest possible tube cuff pressure while maintaining an adequate seal. Usually, the cuff pressure is recommended to be maintained between 20 and 30 cmH2O.[9,10]
Various factors can affect intracuff pressure. For example, time after cuff inflation is a factor that can decrease the cuff pressure. Alzahrani et al[13] reported that 53% of 1060 measurements of cuff pressures were found to be under 20 cmH2O 3 hours after adjusting cuff pressure. According to Valencia et al's study,[14] cuff pressure was decreased inadvertently to under 20 cmH2O in 45.3% of intubated patients at 8 hours after previous measurements of cuff pressure in an intensive care unit. In addition, the use of neuromuscular blocking agents can lead to a reduction in cuff pressure because of lower laryngeal muscle tone.[15,16] On the contrary, nitrous oxide may increase the cuff pressure during general anesthesia because it fills the cuff through diffusion.[17] Several studies have suggested that positional changes of patients may also affect cuff pressure in various ways.[18–20] Finally, physical characteristics of tube and cuff including size, thickness, compliance, diameter, and shape also result in wide variations of cuff pressure.[21,22]
In the present study, the abovementioned factors that could alter the cuff pressure were taken into consideration. Rocuronium (0.8 mg/kg) was used for muscle relaxation. Endotracheal intubation was conducted using a TaperGuard endotracheal tube with an inner diameter of 7 mm in female patients and 7.5 mm in male patients. Anesthesia was maintained without nitrous oxide. Head rotation and measurement of cuff pressure and tube tip position were performed immediately after induction. In addition, there were no differences in the demographic characteristics of the patients.
The shape of a conventional endotracheal tube is generally cylindrical, whereas the TaperGuard endotracheal tube is cone-shaped, tapering distally. Previous studies have reported that the TaperGuard endotracheal tube has a better sealing effect compared to the cylindrical-shaped cuff of the conventional high-volume low-pressure endotracheal tube.[23–25] In addition, Madjdpour et al[5] showed that the TaperGuard endotracheal tube has better air-sealing characteristics than those of the conventional cylindrical endotracheal tube using a tracheal model attached to a test lung. They suggested that the conventional cylindrical-shaped cuff is larger in diameter than the trachea, which tends to create longitudinal folds, resulting in air leakage through those channels. In contrast, the taper-shaped cuff has a larger proximal end diameter than the trachea and it becomes narrower as toward distal end of cuff. Cuff diameter matches the trachea at some point along the cuff, which is the adequate sealing zone without folds. The location of the sealing zone is different among patients because of variations in trachea diameters.[5,25] Due to the improved tracheal sealing properties, TaperGuard endotracheal tubes are widely used in many clinical settings, including our institution.
In some operations, including neurosurgery, otorhinolaryngeal surgery, neck surgery, and facial surgery, the change of head position that is required for adequate operative field exposure affects the cuff pressure in intubated patients. Brimacombe et al[20] reported that head movement caused increases in cuff pressure with conventional cylindrical endotracheal tubes. The mean differences of the cuff pressure after extension, flexion, and lateral rotation from the neutral position were 2, 8, and 5 mm Hg, respectively. Lizy et al[18] reported a result based on the use of conventional endotracheal tubes showing that cuff pressure was increased by head movement, and that 25 of 72 (34.7%) of the measurements were greater than 30 cmH2O. Another previous study showed that head rotation toward the side of tube fixation increased the cuff pressure in TaperGuard tubes.[7] In the present study, we found that the increase in cuff pressure with head rotation was significantly lower on the side opposite to tube fixation than on the same side of tube fixation. There was no cuff pressure greater than 30 cmH2O on the side opposite to tube fixation, whereas 21 (72.4%) measurements were over 30 cmH2O on the same side of tube fixation.
Movement of the head and neck can also cause displacement of the tube.[8] Generally, head flexion can advance the tube, which could cause endobronchial intubation, whereas head extension can withdraw the tube, which could lead to unintentional extubation.[26,27] Kim et al observed results with a cylindrical tube; the tube was displaced away from the carina with head rotation toward the same side of endotracheal tube fixation. However, fixing the tube on the side opposite to that of head rotation caused an unpredictable displacement of the tube (advance or withdrawal).[8] In the present study, we also found that the extent of withdrawal of the tube tip from the carina was greater with head rotation toward the same side of tube fixation than with head rotation to the opposite side.
The side where the tube is fixed is partly dependent on convenience for surgical access or on the surgeon's request. However, maintenance of adequate intracuff pressure after head rotation is also clinically important. Excessive cuff pressure (>30 cmH2O) should be avoided because it diminishes mucosal capillary perfusion and may cause tracheal injury. Thus, we recommend securing the endotracheal tube at the corner of the mouth on the opposite side of the head rotation if intubation is performed using TaperGuard tube. It also reduces the extent of tube displacement, which helps prevent inadvertent extubation. If the endotracheal tube needs to be secured on the same side as the head rotation for surgical reasons, the anesthesiologist should check the cuff pressure after the head is rotated and readjust it if necessary.
This study has some limitations. First, data could not be collected by blinded observers. It was difficult to hide the position of head rotation from the observer; this could have acted as a probable source of bias. Second, the incidence of postoperative complications such as sore throat, hoarseness, and cough was not different in the two groups, which might be because we adjusted the cuff pressure to 22 cmH2O after head rotation. Third, our sample size was relatively small, although we calculated the minimal sample size based on a preliminary study to achieve an adequate power. Finally, the study was conducted at a single center, and the patients were all from an Asian population. Thus, the results may not be generalizable. Multicenter studies in various populations are needed to verify our findings.
5. Conclusion
In the present study, we demonstrated that fixation of the TaperGuard endotracheal tube to the side contralateral to head rotation was associated with a smaller intracuff pressure increase and less tube tip displacement compared to fixation of the tube on the ipsilateral side. We recommend securing the endotracheal tube at the corner of the mouth on the opposite side of the head rotation if intubation is performed using a TaperGuard tube. If the endotracheal tube needs to be secured on the same side as the head rotation for surgical reasons, the anesthesiologist should check the cuff pressure after head rotation and make any necessary adjustments. Further studies with larger sample sizes are needed to validate our conclusions.
Author contributions
Writing – review & editing: Saeyoung Kim.
Footnotes
Abbreviations: FOB = fiberoptic bronchoscope, Group O = group wherein the tube was fixed on the side opposite to head rotation, Group S = group wherein the tube was fixed on the same side as that of head rotation.
This work was supported by the Biomedical Research Institute grant, Kyungpook National University Hospital (2017).
The authors have no conflicts of interest to disclose.
References
- [1].King K, Mandava B, Kamen JM. Tracheal tube cuffs and tracheal dilatation. Chest 1975;67:458–62. [DOI] [PubMed] [Google Scholar]
- [2].Carden KA, Boiselle PM, Waltz DA, et al. Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest 2005;127:984–1005. [DOI] [PubMed] [Google Scholar]
- [3].Main E, Castle R, Stocks J, et al. The influence of endotracheal tube leak on the assessment of respiratory function in ventilated children. Intensive Care Med 2001;27:1788–97. [DOI] [PubMed] [Google Scholar]
- [4].Wood C, Ewen A, Goresky G, et al. Exposure of operating room personnel to nitrous oxide during paediatric anaesthesia. Can J Anaesth 1992;39:682–6. [DOI] [PubMed] [Google Scholar]
- [5].Madjdpour C, Mauch J, Dave M, et al. Comparison of air-sealing characteristics of tapered-vs. cylindrical-shaped high-volume, low-pressure tube cuffs. Acta Anaesthesiol Scand 2012;56:230–5. [DOI] [PubMed] [Google Scholar]
- [6].D’haese J, De Keukeleire T, Remory I, et al. Assessment of intraoperative microaspiration: does a modified cuff shape improve sealing? Acta Anaesthesiol Scand 2013;57:873–80. [DOI] [PubMed] [Google Scholar]
- [7].Choi E, Park Y, Jeon Y. Comparison of the cuff pressure of a TaperGuard endotracheal tube and a cylindrical endotracheal tube after lateral rotation of head during middle ear surgery: a single-blind, randomized clinical consort study. Medicine 2017;96:e6257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kim J-T, Kim H-J, Ahn W, et al. Head rotation, flexion, and extension alter endotracheal tube position in adults and children. Can J Anesth 2009;56:751–6. [DOI] [PubMed] [Google Scholar]
- [9].Seegobin R, Van Hasselt G. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed) 1984;288:965–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lorente L, Blot S, Rello J. Evidence on measures for the prevention of ventilator-associated pneumonia. Eur Resp J 2007;30:1193–207. [DOI] [PubMed] [Google Scholar]
- [11].Liu J, Zhang X, Gong W, et al. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg 2010;111:1133–7. [DOI] [PubMed] [Google Scholar]
- [12].Geng G, Hu J, Huang S. The effect of endotracheal tube cuff pressure change during gynecological laparoscopic surgery on postoperative sore throat: a control study. J Clin Monit Comput 2015;29:141–4. [DOI] [PubMed] [Google Scholar]
- [13].Alzahrani AR, Al Abbasi S, Abahoussin OK, et al. Prevalence and predictors of out-of-range cuff pressure of endotracheal and tracheostomy tubes: a prospective cohort study in mechanically ventilated patients. BMC Anesthesiol 2015;15:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Valencia M, Ferrer M, Farre R, et al. Automatic control of tracheal tube cuff pressure in ventilated patients in semirecumbent position: a randomized trial. Crit Care Med 2007;35:1543–9. [DOI] [PubMed] [Google Scholar]
- [15].Sivarajan M, Joy JV. Effects of general anesthesia and paralysis on upper airway changes due to head position in humans. Anesthesiology 1996;85:787–93. [DOI] [PubMed] [Google Scholar]
- [16].Girling KJ, Bedforth NM, Spendlove JL, et al. Assessing neuromuscular block at the larynx: the effect of change in resting cuff pressure and a comparison with video imaging in anesthetized humans. Anesth Analg 1999;88:426–31. [DOI] [PubMed] [Google Scholar]
- [17].Combes X, Schauvliege F, Peyrouset O, et al. Intracuff pressure and tracheal morbidity: influence of filling with saline during nitrous oxide anesthesia. Anesthesiology 2001;95:1120–4. [DOI] [PubMed] [Google Scholar]
- [18].Lizy C, Swinnen W, Labeau S, et al. Cuff pressure of endotracheal tubes after changes in body position in critically ill patients treated with mechanical ventilation. Am J Crit Care 2014;23:e1–8. [DOI] [PubMed] [Google Scholar]
- [19].Godoy ACFd, Vieira RJ, Capitani EMD. Endotracheal tube cuff pressure alteration after changes in position in patients under mechanical ventilation. J Bras Pneumol 2008;34:294–7. [DOI] [PubMed] [Google Scholar]
- [20].Brimacombe J, Keller C, Giampalmo M, et al. Direct measurement of mucosal pressures exerted by cuff and non-cuff portions of tracheal tubes with different cuff volumes and head and neck positions. Br J Anaesth 1999;82:708–11. [DOI] [PubMed] [Google Scholar]
- [21].Bernhard WN, Yost L, Joynes D, et al. Intracuff pressures in endotracheal and tracheostomy tubes. Related cuff physical characteristics. Chest 1985;87:720–5. [DOI] [PubMed] [Google Scholar]
- [22].Lichtenthal P, Borg U. Endotracheal cuff pressure: role of tracheal size and cuff volume. Crit Care 2011;15:147.21489326 [Google Scholar]
- [23].Dave M, Frotzler A, Spielmann N, et al. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Br J Anaesth 2010;105:538–43. [DOI] [PubMed] [Google Scholar]
- [24].Zanella A, Scaravilli V, Isgro S, et al. Fluid leakage across tracheal tube cuff, effect of different cuff material, shape, and positive expiratory pressure: a bench-top study. Intensive Care Med 2011;37:343–7. [DOI] [PubMed] [Google Scholar]
- [25].Gaszyńska E, Ratajczyk P, Wieczorek A, et al. Comparison of microaspiration around TaperGuard tube cuffs and standard tracheal tubes in obese patients subjected to surgery under general anesthesia. Pol J Surg 2014;86:107–10. [DOI] [PubMed] [Google Scholar]
- [26].Yap S, Morris R, Pybus D. Alterations in endotracheal tube position during general anaesthesia. Anaesth Intensive Care 1994;22:586–8. [DOI] [PubMed] [Google Scholar]
- [27].Hartrey R, Kestin I. Movement of oral and nasal tracheal tubes as a result of changes in head and neck position. Anaesthesia 1995;50:682–7. [DOI] [PubMed] [Google Scholar]


