Abstract
Rationale:
Liposarcoma is a cancerous mesenchymal tumor and the most common soft-tissue sarcoma that starts in the adipose tissue. Liposarcoma is commonly found in lower extremities and retroperitoneum, but rarely occurs in the mediastinum.
Patient concerns:
A 63-year-old male was referred to our clinic with a 6-month history of chronic cough and dyspnea.
Diagnose:
Chest x-rays demonstrated a large mass occupying the left hemithorax. Contrast-enhanced computed tomography (CT) revealed a large mass in the anterior mediastinum, which caused the extrinsic compression of the main and left pulmonary artery and the right shift of mediastinum. Diagnosis of liposarcoma was confirmed by microscopic examination and immunohistochemistry analysis.
Interventions:
The patient underwent a thoracotomy for resection of the mediastinal lesion via left thoracic approach.
Outcomes:
The patient discharged without any complications and has been continuing to follow up in clinic without any complaints.
Lessons:
The primary mediastinal liposarcoma is rare, and we recommend that the liposarcoma should be considered in the differential diagnosis of a patient presenting with a mediastinal mass.
Keywords: liposarcoma, mediastinum
1. Introduction
Liposarcomas are malignant tumors with a mesenchymal origin and represent the most common type of soft tissue sarcoma.[1] Its most frequent location is the lower extremities (75%), followed by retroperitoneum (20%).[2–4] Mediastinum maybe one of the rarest primary site, accounting for <1% liposarcomas. Among these few reported cases, mediastinal liposarcoma has been described in all mediastinal compartments, but it seems to preferentially locate in the posterior space.[5] In this study, we reported the clinical presentation and radiological imaging of a rare case of primary mediastinal liposarcoma.
2. Case report
A 63-year-old male presented with a 6-month history of chronic cough and progressive dyspnea. He denied smoking and alcoholism. No other abnormal symptoms or medical history were recorded, such as chest pain, hemoptysis, or infection history. His cough and shortness of breath were aggravated by exertion. Physical examination found no abnormalities. Chest x-rays demonstrated a large mass occupying the left hemithorax (Fig. 1A). Contrast-enhanced CT revealed a large mass in the anterior mediastinum measuring 20 × 13 × 18 cm (Fig. 1B). This giant space-occupying lesion caused the extrinsic compression of the main and left pulmonary artery and the right shift of mediastinum. The mass was heterogeneous in density (−100–13 HU), with variable proportions of fat (50%), soft tissue (40%), and myxoid (10%). There was no calcification or postcontrast enhancement within this lesion. No percutaneous needle biopsy was performed.
Figure 1.
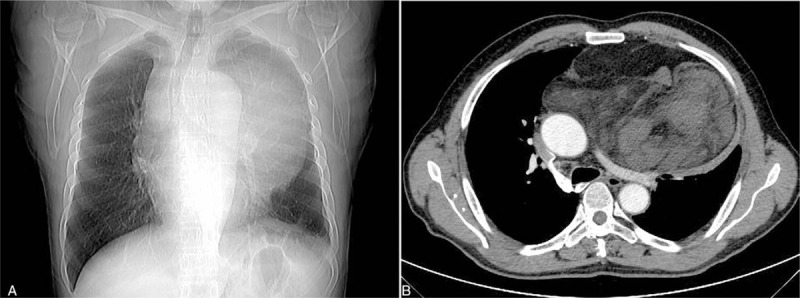
(A) Chest radiograph demonstrated a large mass occupying the left hemithorax; (B) contrast-enhanced computed tomography (CT) revealed a large mass in the anterior mediastinum. CT = computed tomography.
The patient underwent a thoracotomy for resection of the mediastinal lesion via left thoracic approach. The mass was successfully resected from the anterior mediastinum with an intact capsule (Fig. 2A). The smooth lobulated yellow-red mass weighed 1575 g and measured 22.0 × 16.0 × 11.0 cm. Microscopically, the tumor was composed of spindle cells organized in a fascicular pattern and fat cells (Fig. 2B). Immunohistochemically, the spindle cells were positive for vimentin, CD 34, and negative for desmin, SMA, WT-1, S-100, SY, and WT-1. Thus, the tumor was diagnosed as a well-differentiated liposarcoma with regional dedifferentiated area. The patient was discharged without any complications and has been continuing to follow up in clinic without any complaints for 2 years.
Figure 2.
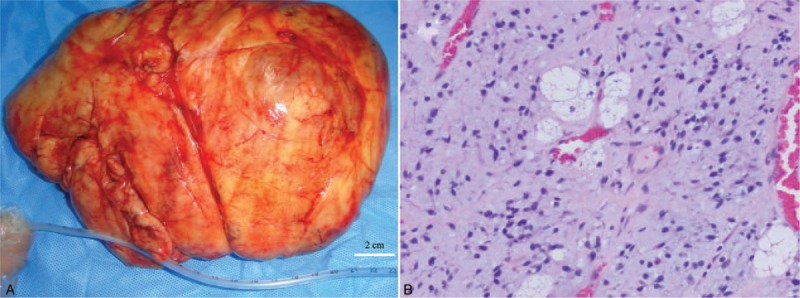
(A) Macroscopic view of the large mediastinal tumor after resection; (B) microscopic pathological examination confirmed the diagnosis of liposarcoma (magnification ×200).
3. Discussion
Liposarcoma originates from primitive mesenchymal cells.[6] Histologically, liposarcoma is classified into 4 subtypes: myxoid/round cell, pleomorphic, atypical lipomatous tumor/well-differentiated liposarcoma and dedifferentiated liposarcoma.[7–9] These tumors are characterized by amplification of MDM2 and CDK4 genes on chromosome 12.[10] Most of these mass are identified incidentally or worked up secondary to complications by compression or irritation of adjacent structures. The possible symptoms of mediastinal liposarcoma are dyspnea, wheezing, chest pain, cough, SVC (superior vena cava) compression and voice hoarseness.[11] Typically, our case presented to our clinic with the complaint of chronic cough and dyspnea.
Imaging manifestations of liposarcoma on CT depend on the degree of differentiation of these subtypes. Septated fatty mass, consisting of at least 75% adipose tissue, typically appears in the low-grade atypical lipomatous tumor/ well-differentiated liposarcoma. Proportion of adipose tissue is usually <25% in the intermediate-grade myxoid and high-grade pleomorphic liposarcoma. Imaging without fat attenuation is shown in approximately 20% of liposarcoma. Cyst-like appearance may be found in 20% of myxoid liposarcoma. The hemorrhage and necrosis area is commonly observed in the pleomorphic liposarcoma.[11,12] Diagnosis maybe confirmed by fine needle aspiration biopsy. Since fine needle aspiration biopsy was not available at the time, it limited us to achieve the pathological diagnosis preoperatively.
Complete surgical resection is still the mainstay of therapy for liposarcoma.[13] No convincing improvement of the prognosis by use of radiation or chemotherapy has been demonstrated.[14] The prognosis of liposarcoma is not influenced by the factors of tumor size, gender or age, while the histopathologic type maybe the most important factor determining survival in patients with liposarcoma.[15] Thus, atypical lipomatous tumor/well-differentiated liposarcoma is associated with a better survival, while the dedifferentiated and pleomorphic type carry the worst prognosis.[14,16] Given the high risk of recurrence, periodical re-examining is recommended, especially for patients who had received incomplete resection.
Author contributions
Data curation: Yu-Shang Yang, Cheng-Yun Bai, Wen-Jun Li, Yong Li.
Writing – original draft: Yu-Shang Yang, Cheng-Yun Bai, Yong Li.
Writing – review & editing: Zhong-Cheng Li.
Footnotes
Abbreviations: CT = computed tomography.
YSY and CYB equally contributed to this work and should both be regarded as the first authors.
Disclosure
The study was approved by the Ethical Committee of Affiliated Hospital of Qinghai University.
Informed written consent was obtained from the patient for publication of this case report and accompanying images.
The authors have no conflicts of interest to disclose.
References
- [1].Dei Tos AP. Liposarcomas: diagnostic pitfalls and new insights. Histopathology 2014;64:38–52. [DOI] [PubMed] [Google Scholar]
- [2].Wang Q, Juan YH, Li Y, et al. Multidetector computed tomography features in differentiating exophytic renal angiomyolipoma from retroperitoneal liposarcoma: a STROBE-Compliant Observational Study. Medicine (Baltimore) 2015;94:e1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rhu J, Cho CW, Lee KW, et al. Single-center experience with intra-abdominal liposarcoma: optimal minimum duration for postoperative remnant tumor screening. Medicine (Baltimore) 2017;96:e7537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bagaria SP, Gabriel E, Mann GN. Multiply recurrent retroperitoneal liposarcoma. J Surg Oncol 2018;117:62–8. [DOI] [PubMed] [Google Scholar]
- [5].Hirai S, Hamanaka Y, Mitsui N, et al. Surgical resection of primary liposarcoma of the anterior mediastinum. Ann Thorac Cardiovasc Surg 2008;14:38–41. [PubMed] [Google Scholar]
- [6].Moreau LC, Turcotte R, Ferguson P, et al. Myxoid\round cell liposarcoma (MRCLS) revisited: an analysis of 418 primarily managed cases. Ann Surg Oncol 2012;19:1081–8. [DOI] [PubMed] [Google Scholar]
- [7].Mansfield SA, Pollock RE, Grignol VP. Surgery for abdominal well-differentiated liposarcoma. Curr Treat Options Oncol 2018;19:1. [DOI] [PubMed] [Google Scholar]
- [8].Hoshi M, Matsumoto S, Manabe J, et al. Surgery for dedifferentiated liposarcoma, presenting two radiologically and pathologically distinctive patterns. Jpn J Clin Oncol 2006;36:462–7. [DOI] [PubMed] [Google Scholar]
- [9].Tuna M, Ju Z, Amos CI, et al. Soft tissue sarcoma subtypes exhibit distinct patterns of acquired uniparental disomy. BMC Med Genomics 2012;5:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ma J, Zhang HM, Zhang LW, et al. Primary mediastinal giant liposarcoma with smooth muscle and neural differentiation: A case report. Oncol Lett 2015;9:2667–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Harth S, Litzlbauer HD, Behrens CB, et al. Dedifferentiated liposarcoma of the anterior mediastinum: a rare case. Rofo 2016;188:95–7. [DOI] [PubMed] [Google Scholar]
- [12].Downes KA, Goldblum JR, Montgomery EA, et al. Pleomorphic liposarcoma: a clinicopathologic analysis of 19 cases. Mod Pathol 2001;14:179–84. [DOI] [PubMed] [Google Scholar]
- [13].Nassif NA, Tseng W, Borges C, et al. Recent advances in the management of liposarcoma. F1000Res 2016;5:2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chen M, Yang J, Zhu L, et al. Primary intrathoracic liposarcoma: a clinicopathologic study and prognostic analysis of 23 cases. J Cardiothorac Surg 2014;9:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Oh YJ, Yi SY, Kim KH, et al. Prognostic model to predict survival outcome for curatively resected liposarcoma: a multi-institutional experience. J Cancer 2016;7:1174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kim ES, Jang SH, Park HC, et al. Dedifferentiated liposarcoma of the retroperitoneum. Cancer Res Treat 2010;42:57–60. [DOI] [PMC free article] [PubMed] [Google Scholar]


