Abstract
Background:
Prevention of PTSD requires identification of subpopulations contributing most to the population burden of PTSD. This study examined the relative contribution of subthreshold PTSD and probable PTSD on future PTSD in a representative military cohort.
Methods:
We analyzed data on 3,457 US National Guard members from the state of Ohio, assessed by telephone annually from 2008–2014. At each wave, participants were classified into one of three groups based on the PTSD Checklist: probable PTSD (DSM-IV-TR criteria), subthreshold PTSD (Criterion A1, at least one symptom in each cluster, symptom lasting longer than 30 days, and functional impairment), and no PTSD. We calculated the exposure rate, risk ratio (RR), and population attributable fraction (PAF) to determine the burden of future probable PTSD attributable to subthreshold PTSD compared to probable PTSD.
Results:
The annualized prevalence of subthreshold PTSD and probable PTSD was respectively 11.9% and 5.0%. The RR for probable PTSD was twice as great among respondents with probable PTSD the prior interview than that of those with subthreshold PTSD (7.0 vs. 3.4); however, the PAF was considerably greater in participants with subthreshold PTSD the prior interview (PAF=35%; 95% CI=26.0–42.9%) than in those with probable PTSD (PAF=28.0%; 95% CI=21.8–33.8%). Results were robust to changes in subthreshold PTSD definition.
Conclusions:
Subthreshold PTSD accounted for a substantial proportion of this population’s future PTSD burden. Population-based preventive interventions, compared to an approach focused exclusively on cases of diagnosable PTSD, is likely to affect the greatest reduction in this population’s future PTSD burden.
Keywords: Anxiety/Anxiety disorder, PTSD/posttraumatic stress disorder, Life Events/Stress, Trauma, Epidemiology
INTRODUCTION
Exposure to potentially traumatic events can elicit a range of psychological symptoms (Fink & Galea, 2015). While symptoms will be mild to moderate for the majority of people, followed by a return to pre-trauma health shortly thereafter, an estimated 1.3% to 8.8% of trauma exposed persons will experience severe distress and impairment that is consistent with posttraumatic stress disorder (PTSD) (Atwoli, Stein, Koenen, & McLaughlin, 2015). Further, another 3.6% to 25.6% of persons experience clinically significant posttraumatic stress symptoms that, despite failure to meet full diagnostic criteria for PTSD, might cause distress and impairment and warrant treatment (Jakupcak et al., 2011; Mota et al., 2016; Pietrzak, Goldstein, Malley, Johnson, & Southwick, 2009). The dominant lens through which we consider psychiatric disorders is binary, i.e., we consider whether individuals have a diagnosis or not. A consequence of this binary model of psychiatric disorders has been a tendency to neglect the people with subsyndromal manifestations of disorder. Thus, persons with symptoms falling below the threshold might not be recognized in clinical care settings or reported in community surveys. Better data on both the course of subthreshold PTSD and the proportion of future PTSD attributable to subthreshold PTSD within a population would inform decisions about the value of their inclusion or their exclusion in intervention dissemination efforts and clinical care.
PTSD first appeared as a diagnosis in the DSM-III. Although the exact diagnostic criteria for PTSD has varied over time, four features of PTSD have remained stable: 1) experiencing or witnessing a traumatic event; 2) re-experiencing symptoms of the event, including nightmares and/or flashbacks; 3) avoidance of people, situations, or places that are reminders of the event; and 4) hyperarousal symptoms, including irritability and concentration issue (Wilson, 1994). Although a 1-month duration of symptoms is a criterion for PTSD, symptoms can endure anywhere from a few months to several decades (Kessler et al., 2017). During this time, people with PTSD experience a reduced quality of life and increased use of health services (Brunello et al., 2001; Kessler, 2000; Pacella, Hruska, & Delahanty, 2013). Beginning in the 1990s (Stein, Walker, Hazen, & Forde, 1997; Weiss et al., 1992), researchers began to notice that people who do not meet the full diagnostic criteria for PTSD can experience significant impairment, including diminished social and family functioning (Stein et al., 1997), elevated rates of depression and suicidal ideation (Cukor, Wyka, Jayasinghe, & Difede, 2010; Marshall et al., 2001), and increase health care use (Breslau, Lucia, & Davis, 2004). And, while a complex diagnostic algorithm is necessary to provide reliability, consistency, and communication about a specific disorder, the use of syndrome-based, binary classifications, such as those found in the DSM-III, its successors, and ICD-10, produce artificial boundaries between health and disorder (Kendler & Paranas, 2015; Zachar & Kendler, 2017), which can obfuscate a substantial proportion of trauma exposed persons who experience subthreshold posttraumatic stress symptoms.
The prevalence of subthreshold PTSD has varied substantially across different studies. A recent meta-analysis by Brancu et al. (2016) found 81 papers reporting the prevalence of subthreshold PTSD published between 1997 and 2014, and among these papers, the prevalence varied from less than 1% to nearly 50%. Brancu et al. (2016) attributed the variability in prevalence estimates to differences in sample composition and population across studies, rather than differences in how studies defined subthreshold PTSD. In particular, Brancu et al. (2016) found that community-based studies (vs. epidemiological) and studies comprised of persons with varying Criterion A events (vs. a single trauma type, such as military combat, natural disaster, or sexual assault) tended to report lower prevalence estimates. Despite the large number of papers that have documented the prevalence of subthreshold PTSD, to the best of our knowledge only a single study has examined the longitudinal course of subthreshold PTSD (Cukor et al., 2010) and no longitudinal studies have been conducted in a military setting.
In this study, we explore the public health burden of subthreshold PTSD using prospective data from a longitudinal study of U.S. Army National Guard soldiers from the state of Ohio. The aim of this study was three-fold: (1) to document the prevalence of subthreshold PTSD relative to threshold PTSD; (2) to identify the risk for future PTSD among persons with subthreshold PTSD and PTSD at baseline; and (3) to identify the burden of future PTSD that could be reduced by screening for, and mitigating, subthreshold PTSD.
MATERIALS AND METHODS
STUDY SAMPLE
We utilized data from the Ohio Army National Guard Mental Health Initiative (OHARNG MHI) (Calabrese et al., 2011). The OHARNG MHI is a longitudinal cohort survey that has annually collected population-based data of Ohio Army National Guard soldiers from November 2008 to present. Addresses were selected from the Guard’s complete registry in June 2008 (N = 12,225). After an alert letter was sent to all Guard members, 1,013 (8.3%) opted not to participate in the study. After eliminating members without a valid telephone number listed, who did not wish to participate, or who were deemed ineligible due to age, retirement status or language, the official enrollment at baseline was 2,616, representing a cooperation rate and response rate of 68% and 43%, respectively. Retention of Wave 1 participants was 81%, 69%, 61%, and 52% at Waves 2 to 5. In order to replenish the sample after loss to follow up, a second and third round of baseline interviews for new participants was also initiated in 2010 (n = 578) and 2011 (n = 263).
Participants were interviewed from 2008 to 2014, approximately 12 months apart for five total waves. Participant in the initial cohort of 2,616 participants contributed a maximum of 4 person-years, whereas participants in 2010 and 2011 supplemental cohorts contributed a maximum of 2 person-years and 1-person-year, respectively. Each person-year began with a completed wave of data collection and ended with the following wave of data collection. Of the 8,053 potential person-years, 5,219 completed the following wave of data collection and 2,834 missed the following wave of data collection. To compensate for non-completed person-years (n=2,834 person-years), response propensity (based on measures available in the prior survey) weighting factors were developed and applied in all analyses of this data. Table 1 shows the distribution of several demographic and psychiatric factors among the 8,053 potential person-years, the 5,219 completed person-years, the 2,834 incomplete person-years (censored), and the censoring-weighted analytic sample.
TABLE 1.
Comparison of Potential Person-Years, Complete Person-Years, and Incomplete Person-Years, and All Person-Years Censoring-Weighted Sample
| Characteristic | Potential Person-Years (n = 8053) | Complete Person-Years (n = 5219) | Incomplete Person-Years (n = 2834) | Censoring-Weight Person-Years |
|---|---|---|---|---|
| % | % | % | % | |
| Age (years) | ||||
| 18–24 | 36.5 | 32.9 | 43.3 | 36.5 |
| 25–34 | 31.7 | 32.8 | 29.7 | 31.7 |
| 35–44 | 22.3 | 23.3 | 20.2 | 22.3 |
| ≥45 | 9.5 | 11.0 | 6.8 | 9.5 |
| Male | 85.4 | 85.8 | 84.6 | 85.4 |
| Marital status: Never married | 42.1 | 38.9 | 48.0 | 42.0 |
| Marital status: Married | 48.2 | 51.8 | 41.7 | 48.3 |
| Marital status: Previously married | 9.7 | 9.4 | 10.3 | 9.7 |
| Education: Some college + | 77.4 | 80.8 | 71.2 | 77.5 |
| Currently employed | 81.4 | 82.7 | 78.9 | 81.5 |
| Baseline probable PTSD | 5.8 | 5.2 | 7.0 | 5.1 |
| Baseline probable depression | 2.9 | 2.8 | 3.1 | 3.0 |
| Baseline probable alcohol use disorder | 5.3 | 5.3 | 5.4 | 5.5 |
Note: Survey attrition was accounted for using response propensity weights using standardized inverse probability-of-censoring weights to account for baseline covariates associated with censoring: age, sex, marital status, education, income, employment, PTSD, depression, current alcohol use disorder. Baseline posttraumatic stress disorder was determined using the posttraumatic stress disorder checklist (PCL), with responses anchored to a Criterion A1 event identified using three screeners of potentially traumatic events, and DSM-IV-TR criterion. Probable major depression was assessed using the patient health questionnaire (PHQ-9) and required respondents to endorse 5 or more of the 9 depressive symptom criteria have been present at least “more than half the days” in the past 2 weeks, and 1 of the symptoms is either depressed mood or anhedonia. Probable alcohol use disorder required respondents to answer either 1 or more alcohol abuse symptoms or 3 or more alcohol dependence symptoms on the Mini International Neuropsychiatric Interview questionnaire (MINI). PTSD, posttraumatic stress disorder.
Study-trained interviewers explained the study and received informed consent before the baseline interview. Ethical approval was granted by the Ohio National Guard and the Institutional Review Boards of University Hospital Case Medical Center (UHCMC), University of Toledo (UT), University of Michigan, Ann Arbor Veterans Administration Medical Center, Columbia University, Boston University, and the Office of Humans Research Protections of the U.S. Army Medical Research and Materiel Command.
DEFINITION OF SUBTHRESHOLD PTSD
A battery of psychiatric screeners was administered via a 60-minute computer assisted interview at each wave of data collection. Respondent PTSD status was assessed in three phases. First, traumatic events were assessed with the Life Events Checklist (LEC)-Civilian Version (Gray, Litz, Hsu, & Lombardo, 2004), the Deployment Risk and Resilience Inventory (DRRI) items (King, King, Vogt, Knight, & Samper, 2006), and events used by Breslau et al. (Breslau et al., 1998). Events could have occurred either during or outside of their most recent deployment. These were all events that met Criterion A1 for the definition of a traumatic event according to the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000). Second, respondents were asked to review the traumatic events they endorsed and identify their “worst event”. Finally, PTSD symptoms were assessed using the PTSD Checklist-Civilian Version (PCL). To better map the screener to the DSM-IV definition of PTSD, respondents were asked to answer each item in relation to their self-selected “worst” Criterion A1 event. In addition to the17 DSM-IV PTSD symptoms asked during the PCL, respondents were asked three additional questions to assess Criterion E and F. Criterion E was assessed by asking respondents the following question: “What was the longest period of time during which you were having these problems?” – experiencing symptoms for one month or longer was required to meet Criterion E. Criterion F was assessed using the following two questions: “How difficult did these problems make it for you to do your work, take care of things at home, or get along with other people? Would you say – not difficult at all, somewhat difficult, very difficult, or extremely difficult” and “When you had several of these bad moods, feelings, and memories, how distressing was it for you? Was it – not at all distressing, mildly distressing, moderately distressing, or severely distressing?” To meet Criterion F, respondents had to endorse either very or extremely difficult in response to the former question or moderate to severe distress in response to the latter question.
Respondents were categorized as positive for probable DSM-IV PTSD if they reported a Criterion A1 event, being bothered “moderately” or more on at least one intrusion (Criterion B), three avoidance/numbing (Criterion C), and two hyperarousal (Criterion D) symptoms, with symptoms lasting one month or more (Criterion E) and causing significant distress or impairment (Criterion F). In a clinical reappraisal on a sub-sample of the telephone survey participants (Prescott et al., 2014), we found past-year telephone diagnosis of PTSD using the PCL had moderate sensitivity (0.54) and high specificity (0.92) and negative predictive value (0.97) compared to the Clinician-Administered PTSD Scale (CAPS).
Because no single definition of subthreshold PTSD exists, we used the three most common subthreshold PTSD definitions according to the recent meta-analysis by Brancu et al. (Brancu et al., 2016): 1) Criterion B and Criterion C or Criterion D (Definition 1); 2) two of three Criterion (e.g., Criterion B and Criterion D) (Definition 2); and 3) at least one symptom in each cluster (Definition 3). In addition to the above criteria, symptoms could not meet DSM-IV PTSD criterion and respondents had to endorse a DSM-IV Criterion A1 event, Criterion E, and Criterion F. Using the Cohen’s kappa coefficient, we found agreement among the three definitions of probable subthreshold PTSD was substantial, ranging from .78 (95%CI: .76-.80) between Definition 2 and Definition 3 to .97 (95%CI: .97-.98) between Definition 2 and Definition 1 (Table 2). To provide the most conservative estimates of exposure rate, risk ratio, and population attributable fraction, we prioritized the most stringent definition of probable subthreshold PTSD (i.e., Definition 1) (Brancu et al., 2016), using Definition 2 and Definition 3 to check robustness of estimates to different definitions of probable subthreshold PTSD.
TABLE 2.
Agreement among the three definitions of subthreshold posttraumatic stress disorder (PTSD) in Ohio Army National Guard Mental Health Initiative sample, 2009–2014
| Subthreshold PTSD | Kappa (95% CI) |
||||
|---|---|---|---|---|---|
| Definition 1a | Definition 2b | Definition 3c | |||
| Definition 1a | - | .97 (.97, .98) | .80 (.78, .82) | ||
| Definition 2b | - | - | .78 (.76, .80) | ||
| Definition 3c | - | - | - | ||
Notes. Definition 1 require respondents screen positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C or Criterion D, plus Criterion E and Criterion F. Definition 2 require respondents screen positive for a DSM-IV-TR Criterion A event, two of the three Criterion B, Criterion C, or Criterion D, plus Criterion E and Criterion F. Definition 3 require respondents screen positive for a DSM-IV-TR Criterion A event, a response of 3–5 (Moderately or above) on at least 1 Criterion B item, 1 Criterion C item, and 1 Criterion D item, plus Criterion E and Criterion F. CI, confidence interval.
STATISTICAL ANALYSES
Our analysis was completed in two steps. First, we conducted a series of generalized linear models where lagged variables for probable PTSD and subthreshold PTSD were the predictors of primary interest and next-year probable PTSD was the outcome. To estimate the risk ratio, we specified the model fit with a binomial distribution with a logistic link function (Zou, 2004). All models were adjusted for study year, used robust standard errors to account for repeated observations, and were weighted to account for survey attrition. To account for survey attrition, response propensity weights were estimated in two steps (Rizzo, Kalton, & Brick, 1996; Sommers, Riesz, & Kashihara, 2004; Wun, Ezzati-Rice, Diaz-Tena, & Greenblatt, 2007): 1) fitting a multivariable logit regression of the panel response status at follow-up (i.e., response versus nonresponse) on a set of baseline variables associated with nonresponse (age, sex, marital status, education, income, employment, PTSD, depression, current alcohol use disorder) and 2) setting the weighting adjustments for the follow-up respondents to the inverse of the response propensity. Results are expressed as adjusted relative risks (RR) with 95% confidence intervals (CIs). Second, we estimated the population attributable fraction (PAF) for probable PTSD and subthreshold PTSD and next-year probable PTSD. The PAF estimates the potential public health impact that would be associated with hypothetically removing the exposure from the population. It was calculated according to the following formula (Rockhill, Newman, & Weinberg, 1998): Adjusted PAF (regression analysis)
Where pdi = proportion of cases falling into ith exposure level and RRi = relative risk comparing ith exposure level with unexposed group (i = 0). All statistical analyses were conducted using SAS v9.3 (Cary, NC).
RESULTS
Among the total survey group, 5.1% screened positive for probable PTSD at baseline and 12.0%, 12.5%, and 11.9% screened positive for subthreshold PTSD Definition 1 through Definition 3, respectively. The proportion of respondents with subthreshold PTSD at baseline that progressed to probable PTSD the subsequent year ranged from 15.9% (definition 1) to 17.3% (definition 2). Figure 1 shows that the mean symptom cluster score was similar among the three definitions of subthreshold PTSD, and mean symptom cluster scores for subthreshold PTSD fell about half-way between respondents who screened positive for probable PTSD and respondents who did not screen positive for subthreshold PTSD.
Figure 1.
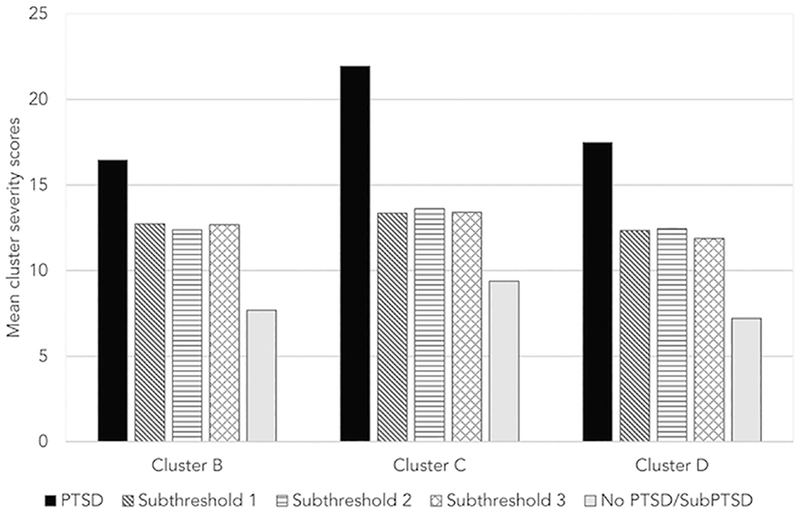
. Mean symptom cluster severity scores among those meeting criteria for probable DSM-IV PTSD, subthreshold PTSD definition 1, subthreshold PTSD definition 2, and subthreshold PTSD definition 3 compared to persons not meeting criteria for probable PTSD nor any subthreshold definition. Symptom cluster severity score is obtained by summing the scores for the items within the given cluster. Persons with PTSD screened positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C, Criterion D, Criterion E, and Criterion F. Subthreshold Definition 1 persons screened positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C or Criterion D, plus Criterion E and Criterion F. Subthreshold Definition 2 Persons screened positive for a DSM-IV-TR Criterion A event, two of the three Criterion B, Criterion C, or Criterion D, plus Criterion E and Criterion F. Subthreshold Definition 3 persons screened positive for a DSM-IV-TR Criterion A event, a response of 3–5 (Moderately or above) on at least 1 Criterion B item, 1 Criterion C item, and 1 Criterion D item, plus Criterion E and Criterion F.
The relative risk for diagnosable PTSD at follow up was twice as high for respondents with probable PTSD at baseline than for respondents with subthreshold PTSD at baseline (Figure 2 and Web Table 3). The relative risk for respondents with subthreshold PTSD at baseline to screen positive for probable PTSD at follow up ranged from 3.2 (95% CI=2.5–4.1) for Definition 1 to 3.7 (95% CI=2.9–4.7) for Definition 2, whereas respondents with probable PTSD at baseline had 7.0 times (95% CI=5.9–8.3) the risk of probable PTSD at follow up compared to respondents without PTSD at baseline. The PAF for probable PTSD at follow up was uniformly higher for the various baseline measures of subthreshold PTSD than probable PTSD. For example, 28.0% (95% CI=21.8%−33.8%) of all probable PTSD cases at follow-up were attributable to persons with probable PTSD at baseline, compared to about 35% of probable PTSD cases at follow-up which were attributable to subthreshold PTSD, with the excess fraction ranging from 35.0% (95% CI=26.0%−42.9%) for Definition 3 to 36.4% (95% CI=27.4%−44.3%) for Definition 1.
Figure 2.
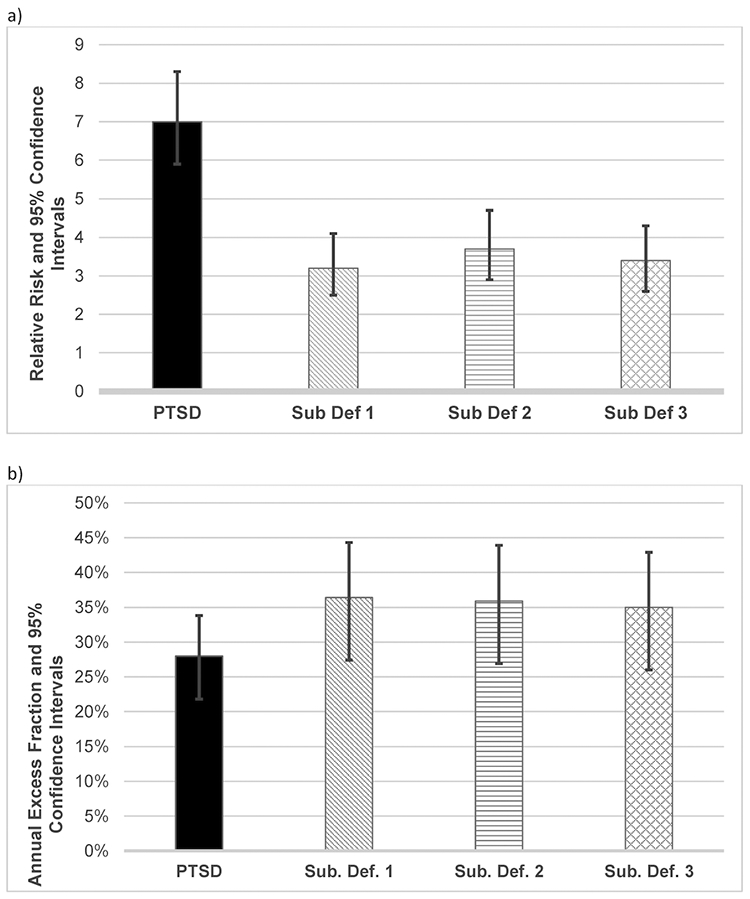
. Risk ratio associated with posttraumatic stress disorder and each subthreshold definition Graph A) shows that the risk ratio for future PTSD was twice as great among persons with subthreshold PTSD compared to PTSD. Graph B) shows the population attributable fraction of PTSD related to persons with subthreshold PTSD the prior year was substantial, suggesting that in the absence of subthreshold PTSD the future population burden of PTSD would fall by about 35% to 36%, relative to 28% for PTSD. Persons with PTSD screened positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C, Criterion D, Criterion E, and Criterion F. Sub Def 1 persons screened positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C or Criterion D, plus Criterion E and Criterion F. Sub Def 2 Persons screened positive for a DSM-IV-TR Criterion A event, two of the three Criterion B, Criterion C, or Criterion D, plus Criterion E and Criterion F. Sub Def 3 persons screened positive for a DSM-IV-TR Criterion A event, a response of 3–5 (Moderately or above) on at least 1 Criterion B item, 1 Criterion C item, and 1 Criterion D item, plus Criterion E and Criterion F.
TABLE 3.
Baseline posttraumatic stress disorder (PTSD) status predicting probable PTSD a year later over five waves (6 years) and annual excess fraction of probable PTSD attributable to baseline PTSD and subthreshold PTSD
| PTSD status | PTSD |
|
|---|---|---|
| Relative Risk (95% CI) | Annual Excess Fraction (95% CI) | |
| PTSD | 7.16 (5.97, 8.59) | 28.0% (21.8%, 33.8%) |
| Subthreshold PTSD Definition 1 | 3.19 (2.47, 4.13) | 36.4% (27.4%, 44.3%) |
| Subthreshold PTSD Definition 2 | 3.68 (2.88, 4.71) | 35.9% (26.9%, 43.9%) |
| Subthreshold PTSD Definition 3 | 3.39 (2.62, 4.39) | 35.0% (26.0%, 42.9%) |
Notes. Persons with PTSD screened positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C, Criterion D, Criterion E, and Criterion F. Sub Def 1 persons screened positive for a DSM-IV-TR Criterion A event, Criterion B, Criterion C or Criterion D, plus Criterion E and Criterion F. Sub Def 2 Persons screened positive for a DSM-IV-TR Criterion A event, two of the three Criterion B, Criterion C, or Criterion D, plus Criterion E and Criterion F. Sub Def 3 persons screened positive for a DSM-IV-TR Criterion A event, a response of 3–5 (Moderately or above) on at least 1 Criterion B item, 1 Criterion C item, and 1 Criterion D item, plus Criterion E and Criterion F. CI, confidence interval; PTSD, posttraumatic stress disorder
DISCUSSION
In a cohort of U.S. National Guard soldiers from the state of Ohio, subthreshold PTSD was common, with 12% screening positive for subthreshold PTSD compared to 5% screening positive for probable PTSD. Moreover, even though respondents with probable PTSD had twice the risk of future PTSD than those with subthreshold PTSD, the larger proportion of the population with subthreshold PTSD contributed more to the population’s future PTSD burden than those with diagnosable PTSD at prior interviews. Specifically, assuming a causal relationship between subthreshold PTSD and future diagnosable PTSD, the population burden of diagnosable PTSD would have been reduced by about 35% to 36%, if, hypothetically, the symptoms of those with subthreshold PTSD had been reduced to the level of those without subthreshold PTSD, relative to a 28% reduction if those with probable PTSD had been reduced to the level of those without subthreshold PTSD. Results were robust to changes in definition of subthreshold PTSD.
The prevalence of subthreshold PTSD was similar to those found in previous studies. Indeed, the prevalence of probable subthreshold PTSD in our National Guard sample (12.0%) approached the lower bound of the 95% CI from a random-effects model-based prevalence estimate of subthreshold PTSD from Brancu et al (2016) (14.7%; 95% CI=12.3%−17.2%); however, our estimate was similar to the estimate from the group of studies that employed the most rigorous methodology (12.6%).
In our study, persons with probable PTSD had a 7-fold increase in their risk of probable PTSD the subsequent year relative to persons without PTSD, compared to about a 3-fold increase in risk among persons with subthreshold PTSD. The fact that subthreshold PTSD symptoms predicted developing probable PTSD in the future is consistent with studies showing that subthreshold symptoms are at risk factor for developing future psychiatric disorders (Angst & Merikangas, 1997; Fergusson, Horwood, Ridder, & Beautrais, 2005). To the best of our knowledge, however, only a single study has examined the longitudinal course of subthreshold PTSD (Cukor et al., 2010), finding that 14.1% of subthreshold cases progressed to PTSD. Although the previous study was among workers dispatched to the World Trade Center site following the 9/11 terrorist attacks, we observed a similar proportion of persons advancing from subthreshold PTSD to probable PTSD per year (15.9% to 17.3%).
We found that a greater proportion of future probable PTSD cases could be prevented by reducing PTSD symptoms among the greater proportion of the population with subthreshold PTSD (12.0%) than the smaller, high-risk, group with chronic probable PTSD (5.0%). This finding—that over one in three probable PTSD cases arose from persons with subthreshold PTSD the prior year—is of substantial public health relevance. A clinical focus on the highest risk minority within the population with PTSD is likely to miss an opportunity to affect the greatest reduction of the future PTSD burden within the population. However, it is difficult to know the best strategy to reduce future PTSD risk among persons with subthreshold PTSD.
One strategy is to apply a broad population prevention strategy focused on the factors that can modify PTSD risk within the population, such as social support (Hobfoll et al., 2007; Ozbay et al., 2007) and alcohol use (Cohen, Fink, Sampson, & Galea, 2015). Through lowering the average risk of PTSD across the entire population, it is likely to follow that persons with subthreshold PTSD will experience a similar shift in PTSD risk. Alternatively, a targeted prevention strategy might focus on identifying, engaging, and linking to care persons exhibiting either subthreshold PTSD or probable PTSD symptoms. While limited guidance is available to clinicians for the best approach to treating persons with subthreshold PTSD symptoms, a growing body of evidence suggests that the same trauma-focused treatments, originally developed for the treatment of PTSD, can be effectively used to treat patients with subthreshold PTSD (Dickstein, Walter, Schumm, & Chard, 2013; Hobfoll, Blais, Stevens, Walt, & Gengler, 2016). Nonetheless, critical questions remain about the urgency with which persons with subthreshold PTSD should be treated and the types of treatment modalities that should be applied to this population.
There are six limitations important for interpretation of this study. First, we used DSM-IV-TR diagnostic criteria to determine probable PTSD, instead of the updated DSM-5 criteria. This decision to use criteria from the DSM-IV instead of the DSM-5 aimed to preserve data from Waves 1 through Waves 3, collected prior to the publication of the DSM-5 and PCL5 in 2013 (American Psychiatric Association, 2013; Weathers et al., 2013). Changes in diagnostic criteria for PTSD from the DSM-IV and DSM-5 included: removal of the subjective component of the index event, clarifying and tightening the definition of a traumatic event, increase the number of symptoms from 17 to 20, and splitting the avoidance and numbing cluster (Criterion C) in DSM-IV into the avoidance cluster (Criterion C) and the cognition and mood group (Criterion D) (Pai, Suris, & North, 2017). While these changes to the diagnostic criteria may affect the proportion of respondents screening positive for PTSD, it remains true that future research needs to focus on the spectrum of PTSD symptomology, over an arbitrary cutoff of a binary diagnosis. Second, although we used three well validated measures to assess respondents’ exposure to DSM-IV Criterion A-qualifying traumas, a “gold standard” clinician-interview such as the CAPS was not administered to evaluate whether or not the respondents “worst” event involved actual or threatened death, serious injury, or threat to physical integrity to themselves or others. Further, given that a telephone administered PCL was used to assess both the presence and the severity of PTSD symptoms, over an independent clinical interview-based diagnoses of PTSD, these results more appropriately reflect the probable presence of PTSD symptoms than DSM-IV algorithm-derived diagnostic classification of PTSD. Although a prior study on the diagnostic utility of the PCL found comparable estimates of symptomatology between the PCL and CAPS in this sample (Fine et al., 2013; Prescott et al., 2014), we used the terms probable PTSD to make clear this limitation—comparison between the results of this study and other work that uses clinical assessments of PTSD should be made cautiously. Third, respondents with subthreshold PTSD might be comprised of multiple subgroups of people, including: a) people with symptoms advancing in a linear manner from no PTSD to subthreshold PTSD to diagnosable PTSD; b) people whose PTSD has remitted to a subthreshold level; and c) people in a chronic state of subthreshold PTSD. While our dataset is insufficiently powered to examine each of these three subgroups independently, future studies should consider heterogeneous symptom trajectories among persons with subthreshold PTSD. Fourth, there was loss to follow-up across the years of our study, requiring additional recruitment. To address this concern, we used an analytic approach to account for the potential influence of missingness, and we show that the distribution of baseline characteristics was similar in our censoring weighted analytic sample compared to our full baseline sample. Fifth, our findings may not generalize to other populations, including non-military populations and active-duty military populations. Finally, the method of population-attributable fraction assumes causality. It must be noted that elimination of a risk marker may not necessarily improve outcomes. However, our focus on reducing subthreshold PTSD to affect the population burden of PTSD increases the likelihood that reductions of this risk will improve outcomes.
CONCLUSION
In conclusion, our findings that respondents with subthreshold PTSD had an increased risk of future PTSD as compared to persons without PTSD, suggests a need to move beyond a binary PTSD diagnosis. The elevated risk for future PTSD among those with subthreshold PTSD—combined with our finding that persons with subthreshold PTSD contribute more to the future population burden of probable PTSD than persons with chronic PTSD—suggest that it is important to include persons with subthreshold PTSD into intervention dissemination efforts and clinical care. Treatment for persons who go on to develop PTSD can receive current evidence-based PTSD care; however, research is need to identify when and how to best treat those with subthreshold PTSD.
Acknowledgements.
This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Joint Warfighter Medical Research Program (Grants W81XWH-15–1-0080, W81XWH-07–1-0409, and W81XWH-10–1-0579 to J.R.C., I.L., M.T.B., S.G.) and National Institute on Drug Abuse at the National Institutes of Health (Grant T32DA031099 to D.S.F.). The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702–5014 is the awarding and administering acquisition office. Opinions, interpretations, conclusions, and recommendations are those of the author and are not necessarily endorsed by the Department of Defense.
Footnotes
The Authors have no conflicts to report.
REFERENCES
- American Psychiatric Association. (2000). DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision.
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. Washington, DC: Author. [Google Scholar]
- Angst J, & Merikangas K (1997). The depressive spectrum: diagnostic classification and course. Journal of Affective Disorders, 45(1–2), 31–39; discussion 39–40. [DOI] [PubMed] [Google Scholar]
- Atwoli L, Stein DJ, Koenen KC, & McLaughlin KA (2015). Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr Opin Psychiatry, 28(4), 307–311. doi: 10.1097/YCO.0000000000000167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brancu M, Mann-Wrobel M, Beckham JC, Wagner HR, Elliott A, Robbins AT, … Runnals JJ (2016). Subthreshold posttraumatic stress disorder: A meta-analytic review of DSM-IV prevalence and a proposed DSM-5 approach to measurement. Psychological Trauma: Theory, Research, Practice and Policy, 8(2), 222–232. doi: 10.1037/tra0000078 [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P (1998). Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry, 55(7), 626–632. [DOI] [PubMed] [Google Scholar]
- Breslau N, Lucia VC, & Davis GC (2004). Partial PTSD versus full PTSD: an empirical examination of associated impairment. Psychological Medicine, 34(7), 1205–1214. [DOI] [PubMed] [Google Scholar]
- Brunello N, Davidson JR, Deahl M, Kessler RC, Mendlewicz J, Racagni G, … Zohar J (2001). Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology, 43(3), 150–162. doi: 10.1159/000054884 [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Prescott M, Tamburrino M, Liberzon I, Slembarski R, Goldmann E, … Galea S (2011). PTSD comorbidity and suicidal ideation associated with PTSD within the Ohio Army National Guard. Journal of Clinical Psychiatry, 72(8), 1072–1078. doi: 10.4088/JCP.11m06956 [DOI] [PubMed] [Google Scholar]
- Cohen GH, Fink DS, Sampson L, & Galea S (2015). Mental Health Among Reserve Component Military Service Members and Veterans. Epidemiologic Reviews, 37(1). doi: 10.1093/epirev/mxu007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukor J, Wyka K, Jayasinghe N, & Difede J (2010). The nature and course of subthreshold PTSD. Journal of Anxiety Disorders, 24(8), 918–923. [DOI] [PubMed] [Google Scholar]
- Dickstein BD, Walter KH, Schumm JA, & Chard KM (2013). Comparing response to cognitive processing therapy in military veterans with subthreshold and threshold posttraumatic stress disorder. Journal of Traumatic Stress, 26(6), 703–709. doi: 10.1002/jts.21869 [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, & Beautrais AL (2005). Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry, 62(1), 66–72. doi: 10.1001/archpsyc.62.1.66 [DOI] [PubMed] [Google Scholar]
- Fine TH, Contractor AA, Tamburrino M, Elhai JD, Prescott MR, Cohen GH, … Calabrese JR (2013). Validation of the telephone-administered PHQ-9 against the in-person administered SCID-I major depression module. Journal of Affective Disorders, 150(3), 1001–1007. doi: 10.1016/j.jad.2013.05.029 [DOI] [PubMed] [Google Scholar]
- Fink DS, & Galea S (2015). Life Course Epidemiology of Trauma and Related Psychopathology in Civilian Populations. Curr Psychiatry Rep, 17(5), 566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the life events checklist. Assessment, 11(4), 330–341. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Blais RK, Stevens NR, Walt L, & Gengler R (2016). Vets prevail online intervention reduces PTSD and depression in veterans with mild-to-moderate symptoms. Journal of Consulting and Clinical Psychology, 84(1), 31–42. doi: 10.1037/ccp0000041 [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, … Ursano RJ (2007). Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry, 70(4), 283–315; discussion 316–269. doi: 10.1521/psyc.2007.70.4.283 [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Hoerster KD, Varra A, Vannoy S, Felker B, & Hunt S (2011). Hopelessness and suicidal ideation in Iraq and Afghanistan war veterans reporting subthreshold and threshold posttraumatic stress disorder. The Journal of nervous and mental disease, 199(4), 272–275. [DOI] [PubMed] [Google Scholar]
- Kendler KS, & Paranas J (2015). Philosophical issues in psychiatry: Explanation, phenomenology, and nosology. Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Kessler RC (2000). Posttraumatic stress disorder: the burden to the individual and to society. Journal of Clinical Psychiatry, 61 Suppl 5, 4–12; discussion 13–14. [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, … Koenen KC (2017). Trauma and PTSD in the WHO World Mental Health Surveys. Eur J Psychotraumatol, 8(sup5), 1353383. doi: 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, & Samper RE (2006). Deployment Risk and Resilience Inventory: a collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology, 18(2), 89. [Google Scholar]
- Marshall RD, Olfson M, Hellman F, Blanco C, Guardino M, & Struening EL (2001). Comorbidity, impairment, and suicidality in subthreshold PTSD. American Journal of Psychiatry, 158(9), 1467–1473. [DOI] [PubMed] [Google Scholar]
- Mota NP, Tsai J, Sareen J, Marx BP, Wisco BE, Harpaz-Rotem I, … Pietrzak RH (2016). High burden of subthreshold DSM-5 post-traumatic stress disorder in U.S. military veterans. World Psychiatry, 15(2), 185–186. doi: 10.1002/wps.20313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, & Southwick S (2007). Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont), 4(5), 35–40. [PMC free article] [PubMed] [Google Scholar]
- Pacella ML, Hruska B, & Delahanty DL (2013). The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. Journal of Anxiety Disorders, 27(1), 33–46. doi: 10.1016/j.janxdis.2012.08.004 [DOI] [PubMed] [Google Scholar]
- Pai A, Suris AM, & North CS (2017). Posttraumatic Stress Disorder in the DSM-5: Controversy, Change, and Conceptual Considerations. Behav Sci (Basel), 7(1). doi: 10.3390/bs7010007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Johnson DC, & Southwick SM (2009). Subsyndromal posttraumatic stress disorder is associated with health and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety, 26(8), 739–744. doi: 10.1002/da.20574 [DOI] [PubMed] [Google Scholar]
- Prescott MR, Tamburrino M, Calabrese JR, Liberzon I, Slembarski R, Shirley E, … Galea S (2014). Validation of lay-administered mental health assessments in a large Army National Guard cohort. International Journal of Methods in Psychiatric Research, 23(1), 109–119. doi: 10.1002/mpr.1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzo L, Kalton G, & Brick JM (1996). A comparison of some weighting adjustment methods for panel nonresponse. Survey methodology, 22(1), 43–53. [Google Scholar]
- Rockhill B, Newman B, & Weinberg C (1998). Use and Misuse of Population Attributable Fractions. American Journal of Public Health, 88(1), 15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers J, Riesz S, & Kashihara D (2004). Response propensity weighting for the Medical Expen- diture Panel Survey - Insurance Component (MEPS-IC). Retrieved from http://ww2.amstat.org/sections/srms/Proceedings/y2004/files/Jsm2004-000365.pdf
- Stein MB, Walker JR, Hazen AL, & Forde DR (1997). Full and partial posttraumatic stress disorder: findings from a community survey. American Journal of Psychiatry, 154(8), 1114–1119. doi: 10.1176/ajp.154.8.1114 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). . Scale available from the National Center for PTSD at www.ptsd.va.gov.
- Weiss DS, Marmar C, Schlenger W, Fairbank J, Jordan B, Hough R, & Kulka RA (1992). The prevalence of lifetime and partial post-traumatic stress disorder in Vietnam theater veterans. Journal of Traumatic Stress, 5, 365–376. [Google Scholar]
- Wilson JP (1994). The historical evolution of PTSD diagnostic criteria: from Freud to DSM-IV. Journal of Traumatic Stress, 7(4), 681–698. [DOI] [PubMed] [Google Scholar]
- Wun LM, Ezzati-Rice TM, Diaz-Tena N, & Greenblatt J (2007). On modelling response propensity for dwelling unit (DU) level non-response adjustment in the Medical Expenditure Panel Survey (MEPS). Statistics in Medicine, 26(8), 1875–1884. doi: 10.1002/sim.2809 [DOI] [PubMed] [Google Scholar]
- Zachar P, & Kendler KS (2017). The Philosophy of Nosology. Annual Review of Clinical Psychology, 13(1), 49–71. doi: 10.1146/annurev-clinpsy-032816-045020 [DOI] [PubMed] [Google Scholar]
- Zou G (2004). A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology, 159(7), 702–706. [DOI] [PubMed] [Google Scholar]


