Abstract
Background:
Opioid abuse is a public health epidemic in the United States. Much literature has focused on the prescribing practices of physicians and opioid misuse by adults. However, there are limited data on the effect of opioid prescriptions on adolescent recreational ingestion of these medications.
Objectives:
The objective of this study was to assess for a relationship between opioid prescribing practices across the United States and adolescent opioid ingestion calls to poison centers.
Methods:
This was an observational study using the National Poison Data System. The study population consisted of poison center calls regarding adolescents between 2005 and 2010 in the database with a coding of “intentional abuse” and an opioid ingestion. National opioid prescription estimates were generated using nationally representative outpatient and inpatient databases.
Results:
There were 4186 adolescent opioid ingestion calls during the study period. There was a general increase between 2005 and 2010 in both teen opioid abuse calls (617 in 2005 to 782 in 2010) and national opioid prescriptions (approximately 78 million in 2005 to 108 million in 2010). For each opioid prescription increase per 100 persons per year, the annual teen opioid abuse calls increased by 1.8% (95% confidence interval 0.9–2.8%), equivalent to an absolute increase of about 0.04 to 0.05 calls per 100,000 teens annually.
Conclusions:
There appears to be an association between opioid prescriptions nationally and poison center calls for adolescent opioid ingestions. This is particularly important in this patient population because of impulsivity and early exposure to substance abuse. Providers should be aware of the nonmedical use of opioids by adolescents and educate patients accordingly.
Keywords: adolescent, child, ingestion, opioid pain, medicine
INTRODUCTION
Opioid prescribing practices have been studied in multiple settings within multiple specialties in the United States (1–4). An increase in opioid prescriptions has been seen in the United States, Canada and the United Kingdom (4,5). The greatest concern about increased opioid prescribing is the potential for abuse through increased availability of opioids at home. This has been well documented in the adult literature, with recent studies showing a decline in various street drugs in conjunction with an increase in prescription medication abuse, resulting in increased opioid-related deaths (6,7).
In response to concerning opioid prescribing practices, various approaches to limit nonmedical use have been instituted, including increased surveillance, alternative therapies for chronic pain, and abuse-deterrent formulations of pain medications, with varying degrees of success (8–10). While much past and ongoing research has focused on adults, there is limited research on the effect of opioid prescribing on the pediatric population. One study showed a correlation among adult prescriptions and pediatric ingestions primarily in children <5 years of age, which presumably are accidental ingestions (11). However, further data are needed on the effects of prescribing practices and adolescent recreational ingestions to further direct anticipatory guidance and preventative efforts. The American Academy of Pediatrics has released numerous statements and positions that encourage pediatricians and primary care providers to both counsel on adolescent substance abuse and raise the suspicion to diagnose it (12–14). The objective of this study was to investigate the association between opioid prescriptions and adolescent opioid ingestions using nationally representative data in the United States.
METHODS
This was a retrospective observational study using three nationally representative databases. Teen opioid abuse calls were obtained from the National Poison Data System for the years 2004 through 2013. All calls during this time period with patients 13 to 19 years of ager were included. Only calls coded as “intentional abuse” and involving a single agent opioid or an opioid in combination with acetaminophen were used in this analysis. The estimated number of opioid prescriptions per year by geographic region (i.e., Northeast, South, Midwest, and West) was determined using the National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS), which are national probability surveys of outpatient and emergency department visits at nationally representative facilities. All visits were included, and for emergency department visits, only opioid prescriptions given at discharge (rather than administration in the hospital setting) were included to reflect opioid prescribing. NAMCS and NHAMCS data were available for the years 2005 to 2010; all analyses were therefore restricted to 2005 to 2010. Estimates of population size by region were obtained from the Surveillance, Epidemiology, and End Results (SEER) Program Populations database (15). Estimates were provided by state and were combined into geographic region. For estimates of the teen population, ages 13 through 19 were included. For estimates of the total population, all ages were included. The institutional review board at our institution determined to exempt this study from review.
Statistical Analysis
To calculate the annual rate of opioid prescriptions per person, the estimated total number of opioid prescriptions per region was calculated as the numerator. The denominator was the total regional population per year provided by SEER data. The number was calculated per 100 persons to provide more easily interpretable numbers. To calculate the annual number of opioid abuse ingestion calls per teen, the numerator was the total number of opioid abuse calls within each region, and the denominator was the total region population of persons 13 to 19 years of age provided by SEER data. The annual number was calculated per 100,000 teens to provide a more interpretable number.
We performed Poisson regression models to assess for a change over time and regional differences in both opioid prescriptions and teen opioid abuse poison center calls. For our primary objective, we performed a Poisson regression model to determine if there was a relationship between opioid prescriptions and teen opioid abuse poison center calls. To assess for a relationship between opioid prescriptions and teen opioid abuse poison center calls, the outcome was the number of teen opioid abuse poison center calls within each region and the predictor was opioid prescriptions per 100 persons within each region. Within all Poisson models, to account for the variation in the population of teens within each region, the log transformed number of teens in each region for each year was included as the offset. For all models, we used generalized estimating equations with robust standard errors to control for correlation between outcomes and overdispersion (in which the observed variance is greater than the estimated variance).
RESULTS
There were 4186 total teen opioid abuse calls to poison centers across the United States between 2005 and 2010. There was an annual increase of 5.1% (95% confidence interval [CI] 1.2–9.2) in teen opioid abuse calls per 10,000 teens (p = 0.01) with 617 calls in 2005 and 782 calls in 2010, corresponding to an increase of 2.05 calls per 100,000 teens in 2005 to 2.59 calls per 100,000 teens in 2010 (Table 1). There were regional differences, with the West having the lowest and the Midwest having the highest yearly rate of teen opioid abuse calls per 100,000 teens (p < 0.01; Table 2, Figure 1).
Table 1.
Teen Opioid Abuse Calls and Opioid Prescriptions per Person by Year
| Year | Opioid Prescriptions per 100 Persons per Year (SD) | Teen Opioid Abuse Calls per 100,000 Teens per Year (SD) |
|---|---|---|
| 2005 | 26.37 (3.70) | 2.05 (0.50) |
| 2006 | 27.86 (3.69) | 2.11 (0.53) |
| 2007 | 32.49 (7.11) | 2.21 (0.44) |
| 2008 | 32.19 (3.81) | 2.30 (0.42) |
| 2009 | 38.33 (5.42) | 2.51 (0.50) |
| 2010 | 34.83 (4.32) | 2.59 (0.37) |
SD = standard deviation.
Table 2.
Teen Opioid Abuse Calls and Opioid Prescriptions per Person by Region
| Geographic Region | Opioid Prescriptions per 100 Persons per Year (SD) | Teen Opioid Abuse Calls per 100,000 Teens per Year (SD) |
|---|---|---|
| Northeast | 25.62 (3.01) | 1.93 (0.18) |
| Midwest | 31.10 (4.11) | 2.77 (0.39) |
| South | 37.04 (5.06) | 2.56 (0.16) |
| West | 30.13 (5.53) | 1.71 (0.32) |
SD = standard deviation.
Figure 1.
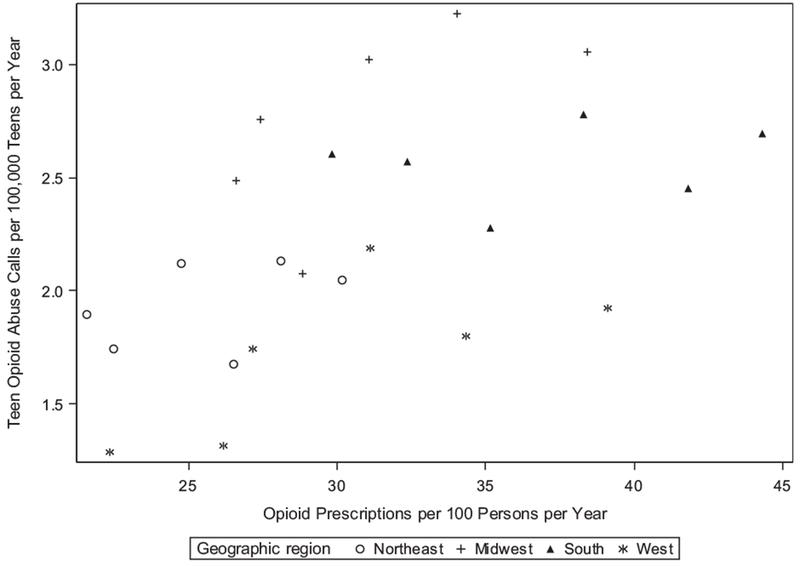
Regional teen opioid abuse calls by opioid prescriptions.
During the same study period, the total number of opioid prescriptions was estimated to be 582,133,766 based on NAMCS and NHAMCS data, with a similar annual increase of 6.9% (95% CI 5.5–8.2) in total opioid prescriptions (p < 0.01). In particular, there were estimated to be 77,932,057 opioid prescriptions in 2005 and 107,736,938 in 2010, corresponding to an increase of 26.37 opioid prescriptions per 100 persons in 2005 to 34.83 opioid prescriptions per 100 persons in 2010 (Table 1, Figure 2). There was also regional variation (p < 0.01), with the Northeast having the lowest rate of prescriptions per 100 persons and the South having the highest rates (Table 2).
Figure 2.
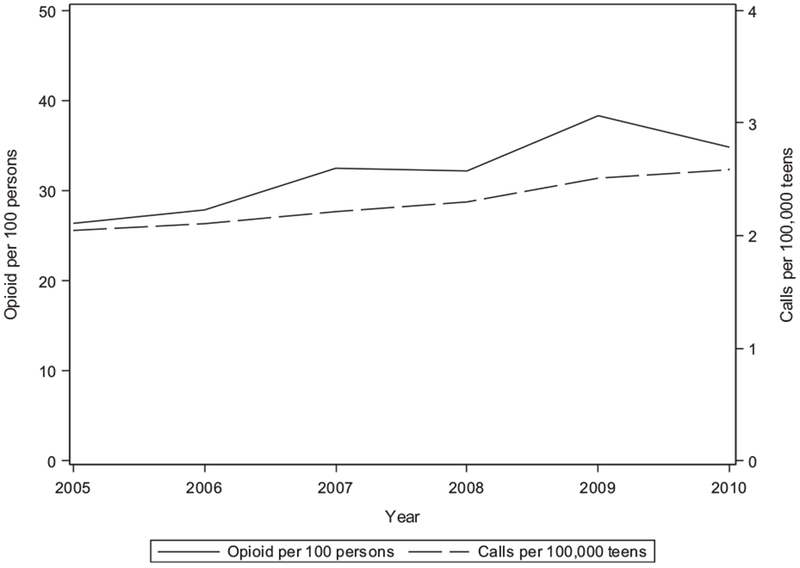
Teen opioid abuse calls and opioid prescriptions over time.
In addition, there was a positive relationship between teen opioid abuse calls and national opioid prescriptions. For each opioid prescription increase per 100 persons per year, the annual rate of teen opioid abuse calls increases by 1.8% (95% CI 0.9–2.8). The estimated annual mean teen opioid abuse calls per 100,000 teens with varying levels of annual opioid prescriptions per 100 persons is provided in Table 3 to further illustrate how an increase in teen opioid abuse calls is associated with an increase in opioid prescriptions. For example, when opioid prescriptions increased from 25 to 30 per 100 persons per year, the estimated annual teen opioid abuse calls would increase from 2.00 to 2.20 calls per 100,000 teens. Overall, each opioid prescription increase per 100 persons per year was associated with an absolute increase of approximately 0.04 to 0.05 calls per 100,000 teens annually.
Table 3.
Estimated Annual Teen Opioid Abuse Calls by Varying Opioid Prescriptions per Person
| Opioid Prescriptions per 100 Persons per Year | Estimated Yearly Mean Teen Opioid Abuse Calls per 100,000 Teens (95% CI) |
|---|---|
| 25 | 2.00 (1.63–2.46) |
| 30 | 2.20 (1.86–2.59) |
| 35 | 2.41 (2.12–2.73) |
| 40 | 2.64 (2.39–2.92) |
CI = confidence interval.
DISCUSSION
While many studies have focused on an increase in opioid prescribing across the country, this study examined the relationship between opioid prescribing and adolescent opioid abuse. This has broad clinical implications to impact provider prescribing with the knowledge of this association and to direct preventative efforts in this specific population.
The unanswered question that arises from these data is where adolescents are obtaining opioids involved in a reported ingestion. While it was not obtained from the National Poison Data System (NPDS) data whether the ingestion call resulted from a personal medication, it is often believed that adolescents are ingesting what is available to them. Based on the knowledge of opioid prescribing practices, it is possible that many of these ingestions are occurring with opioids that are not prescribed to the adolescent for which the call was made. One study that surveyed adolescents in the emergency department for previous nonmedical opioid and sedative use found that approximately 10% of the adolescents surveyed said that they had used these agents for a nonmedical use before (16). In addition, 12% to 14% of the adolescents interviewed had a home prescription for these agents. A longitudinal study that evaluated almost 13,000 high school students asked a similar question, and 12% of the respondents had used opioids for nonmedical purposes in the preceding year (17). The motivations they gave for nonmedical opioid use ranged from sleep to anxiety, and having multiple reasons to ingest opioids correlated with ingestions of multiple drugs. That same longitudinal study found that 4.4% of adolescents surveyed coingested opioids with multiple agents and that nonmedical opioid use was a growing issue in the adolescent age group (18,19). Our data showed that adolescent opioid abuse calls steadily increased during the study period, while there was a brief decrease in opioid prescriptions nationally (Table 1). It is difficult to explain this, but raises the importance of future prospective studies to investigate where adolescents are obtaining opioids for recreational purposes. It is out of the scope of this study to attempt to hypothesize regarding these sources.
Adolescents have been shown to have increasing availability to opioid medications by having prescriptions for themselves. While professional societies—including the American Academy of Pediatrics and American Academy of Neurology—recommend against opioid medications for adolescent headaches, this has not been applied widely in practice. A study that evaluated medical claims of almost 8500 adolescents with headaches found that 46% had ≥1 prescription for an opioid, and it was not uncommon to have multiple prescriptions (20). The longitudinal study of high school students found that 37% of the students with opioid prescriptions had abused pills leftover from a previous prescription. These prescriptions were written by multiple providers, including emergency physicians (45%), other physicians (38%) and dentists (27%) (21). This provides evidence that adolescents may be obtaining opioids from both people with whom they are in close contact and from their own personal prescriptions.
In addition to recreational abuse, with the rising issue of pediatric mental health, adolescents may be self-medicating. One study found that adolescents that abused prescription drugs were 30% to 35% more likely to have depression compared to individuals who did not abuse prescription medications (22). It has been shown in other studies that patients without a history of substance abuse can be drawn to using these agents if they have depression (23,24). This further supports the American Academy of Pediatrics statement that primary care providers not only need to be able to provide anticipatory guidance, but diagnose substance abuse and mental health in the medical home for adolescent patients.
LIMITATION
There are limitations to this study inherent to its design. Data from the NPDS, NHAMCS, and NAMCS are limited by what is coded and entered to represent national estimates. In particular, calls to poison centers represented in the NPDS are a passive surveillance system and no blood or urine toxicology testing is performed after a call. These data are limited to the use of preexisting records that are not explicitly designed for this particular study. Data obtained from the NPDS are dependent on a provider, family member, or patient making a call to the poison center; therefore, if a call is not made, there is no record of the ingestion. Exposures to substances reported to the NPDS therefore cannot be constructed to represent the complete incidence of national exposure of adolescents to opioid medications for recreational purposes. This does suggest that our analysis likely underestimates the occurrence of adolescent teen opioid abuse ingestions and that the true problem is most likely higher. There were differences in poison center calls and opioid prescriptions by region, but because of limited data in the NPDS, we are unable to apply it to our dataset and make inferences of regional abuse or reporting patterns. Information regarding clinical outcome and interventions received for a patient with an ingestion are dependent on the coding of the poison center and may not be reliably accurate and therefore were not evaluated in this study. There are a number of factors that can affect reporting to a system such as the NPDS, and therefore these data may not in fact represent firm trends in opioid abuse, but rather increased reporting. The goal of this study was to identify the problem and assess for a potential association between the rising volume of opioid prescriptions and teenager opioid abuse.
CONCLUSION
Our findings show that both opioid prescriptions and teen opioid abuse have increased across the United States over the past decade, and there is a positive association between the number of prescriptions and number of abuse calls. Because of the inherent limitations in the databases used that rely on reports to poison centers, the problem of opioid abuse in the adolescent population is most likely higher than the data presented. Additional preventative efforts need to be instituted from a multidisciplinary approach, including poison centers, primary care physicians, policies on prescription on appropriate indications and amounts of opioids prescribed, and oversight committees. In addition, further education should be given to providers about the potential impact of opioid prescribing on the adolescent population.
ARTICLE SUMMARY
1. Why is this topic important?
Opioid abuse is a national epidemic and assessing the use by adolescents is important for future health outcomes.
2. What does this study attempt to show?
This study attempts to identify a relationship between national opioid prescriptions and recreational adolescent opioid use.
3. What are the key findings?
There was an increase in overall national opioid prescriptions and annual poison center calls for recreational adolescent opioid use. For each opioid prescription increase per 100 persons per year, the annual teen opioid abuse calls increased by approximately 2%.
4. How is patient care impacted?
This study identifies a relationship that providers should be aware of spanning multiple specialties. Providers should educate patients on this when prescribing opioids for adults and when discussing overall adolescent health with pediatric patients.
Footnotes
Reprints are not available from the authors.
REFERENCES
- 1.Mazer-Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001–2010. Acad Emerg Med 2014;21:236–43. [DOI] [PubMed] [Google Scholar]
- 2.Mazer-Amirshahi M, Mullins PM, Rasooly IR, van den Anker J, Pines JM. Trends in prescription opioid use in pediatric emergency department patients. Pediatr Emerg Care 2014;30:230–5. [DOI] [PubMed] [Google Scholar]
- 3.Kea B, Fu R, Deyo RA, Sun BC. Are discharge prescriptions of opioids from the emergency department truly rising? Acad Emerg Med 2014;21:946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zin CS, Chen LC, Knaggs RD. Changes in trends and pattern of strong opioid prescribing in primary care. Eur J Pain Lond Engl 2014;18:1343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes T, Mamdani MM, Paterson JM, Dhalla IA, Juurlink DN. Trends in high-dose opioid prescribing in Canada. Can Fam Physician 2014;60:826–32. [PMC free article] [PubMed] [Google Scholar]
- 6.Sharp MJ, Melnik TA, Centers for Disease Control and Prevention. Poisoning deaths involving opioid analgesics - New York State, 2003–2012. MMWR Morb Mortal Wkly Rep 2015;64:377–80. [PMC free article] [PubMed] [Google Scholar]
- 7.Kuehn BM. Opioid prescriptions soar: increase in legitimate use as well as abuse. JAMA 2007;297:249–51. [DOI] [PubMed] [Google Scholar]
- 8.Green TC, Bowman S, Davis C, Los C, McHugh K, Friedmann PD. Discrepancies in addressing overdose prevention through prescription monitoring programs. Drug Alcohol Depend 2015;153:355–8. [DOI] [PubMed] [Google Scholar]
- 9.Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med 2015;372:241–8. [DOI] [PubMed] [Google Scholar]
- 10.Compton WM, Boyle M,Wargo E. Prescription opioid abuse: problems and responses. Prev Med 2015;80:5–9. [DOI] [PubMed] [Google Scholar]
- 11.Burghardt LC, Ayers JW, Brownstein JS, Bronstein AC, Ewald MB, Bourgeois FT. Adult prescription drug use and pediatric medication exposures and poisonings. Pediatrics 2013;132:18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics. Committee on Substance Abuse. American Academy of Pediatrics. Committee on Substance Abuse. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention and management of substance abuse. Pediatrics 1998; 101(1 pt 1):125–8. [PubMed] [Google Scholar]
- 13.Kulig JW, American Academy of Pediatrics Committee on Substance Abuse. Tobacco, alcohol, and other drugs: the role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics 2005;115:816–21. [DOI] [PubMed] [Google Scholar]
- 14.Alderman EM, Schonberg SK, Cohen MI. The pediatrician’s role in the diagnosis and treatment of substance abuse. Pediatr Rev Am Acad Pediatr 1992;13:314–8. [DOI] [PubMed] [Google Scholar]
- 15.US Population Data 1969–2012 with Other Software. Surveillance, Epidemiology, and End Results (SEER) Program Populations (1969–2012), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released March 2014. Available at: www.seer.cancer.gov/popdata Accessed April 2, 2015.
- 16.Whiteside LK, Walton MA, Bohnert ASB, Blow FC, Bonar EE, Ehrlich P, et al. Nonmedical prescription opioid and sedative use among adolescents in the emergency department. Pediatrics 2013; 132:825–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyd CJ, McCabe SE, Cranford JA, Young A. Adolescents’ motivations to abuse prescription medications. Pediatrics 2006; 118:2472–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCabe SE,West BT, Teter CJ, Boyd CJ. Co-ingestion of prescription opioids and other drugs among high school seniors: results from a national study. Drug Alcohol Depend 2012;126:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCabe SE, Boyd CJ, Teter CJ. Illicit use of opioid analgesics by high school seniors. J Subst Abuse Treat 2005;28:225–30. [DOI] [PubMed] [Google Scholar]
- 20.DeVries A, Koch T, Wall E, Getchius T, Chi W, Rosenberg A. Opioid use among adolescent patients treated for headache. J Adolesc Health 2014;55:128–33. [DOI] [PubMed] [Google Scholar]
- 21.McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. J Adolesc Health 2013;52:480–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ali MM, Dean D, Lipari R, Dowd WN, Aldridge AP, Novak SP.The mental health consequences of nonmedical prescription drug use among adolescents. J Ment Health Policy Econ 2015; 18:3–15. [PubMed] [Google Scholar]
- 23.Murphy SM, McPherson S, Robinson K. Non-medical prescription opioid use and violent behaviour among adolescents. J Child Adolesc Ment Health 2014;26:35–47. [DOI] [PubMed] [Google Scholar]
- 24.Grattan A, Sullivan MD, Saunders KW, Campbell CI, Von Korff MR. Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substance abuse. Ann Fam Med 2012;10:304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]


