Abstract
Background: Acupuncture is frequently used as an efficient method to prevent and treat migraines. However, its effect on the quality of life remains controversial.
Methods: Seven databases, such as PubMed and Cochrane Library were searched to retrieve reference lists of eligible trials and related reviews. Randomized controlled trials that were published in Chinese and English were included.
Results: Acupuncture resulted in lower Visual Analog Scale scores than the medication group at 1 month after treatment (MD −1.22, 95%CI −1.57 to −0.87; low quality) and 1–3 months after treatment (MD −1.81, 95%CI −3.42 to −0.20; low quality). Compared with sham acupuncture, acupuncture resulted in lower Visual Analog Scale scores at 1 month after treatment (MD −1.56, 95%CI −2.21 to −0.92; low quality).
Conclusion: Acupuncture exhibits certain efficacy both in the treatment and prevention of migraines, which is superior to no treatment, sham acupuncture and medication. Further, acupuncture enhanced the quality of life more than did medication.
Keywords: migraine, acupuncture, systematic review, meta-analysis, efficacy and safety, adverse events, quality of life
Introduction
Migraine, a common neurological disorder, is the third most prevalent disease worldwide out of all medical conditions and the seventh highest cause of disability according to the Global Burden of Disease Study (Vos et al., 2012; Steiner et al., 2013; Diener et al., 2015; Rodriguez, 2015). In China, the prevalence of migraine is 9.3%, with annual expenses of 331.7 billion yuan (Steiner et al., 2013). Thus, migraine has broad effects and a significant social and economic burden (Yu et al., 2012). The recurrent and refractory pain, accompanied by long-term economic stress, may aggravate psychological pressure of patients and cause further tension and anxiety. Migraine is also affected by psychological factors, such as stress and emotion; therefore, a vicious circle is created, which is detrimental for treatment. In addition, migraine attacks affect daily work and life, even leaving some patients unable to work and live independently. Therefore, the quality of life in migraine patients' needs further attention.
Migraines are typically treated by various medications or nonpharmacotherapy to relieve pain or prevent attacks (Holland et al., 2012; Silberstein et al., 2012a; group CMAopchp, 2016). However, those drugs have limited efficacy in relieving headache or reducing the frequency of attacks and are often accompanied by adverse effects (Cranz, 1990; Lipton et al., 1994; Silberstein and Young, 1995; Silberstein et al., 2012b). Acupuncture has become a widely used complementary therapy in many countries (Hartel and Volger, 2004; Bodeker et al., 2005; Burke et al., 2006). Due to its stable effects, acupuncture has been increasingly used in migraine prevention. Some studies have reported that compared with medication, acupuncture had similar or even better effects in raising efficiency rates and reducing migraine attacks (Linde et al., 2009, 2016; Gao et al., 2011; Zheng and Cui, 2012; Song et al., 2016). It has also been reported that acupuncture had fewer side effects and better tolerance (Higgins and Green, 2011; Sterne et al., 2011; Gao, 2012). Therefore, due to its safety and efficacy, acupuncture is expected to be an important method for the prevention and treatment of migraine.
However, some clinical trials have found that there was little or no difference in the preventive effects between acupuncture and sham acupuncture (Linde et al., 2005; Li et al., 2012; Rodriguez, 2015). A prior study even indicated that the main effects of acupuncture may come from placebo effects (Meissner et al., 2013). Thus, the efficacy of acupuncture on migraine needs further verification. In addition, some studies have shown that acupuncture can improve depressive symptoms caused by migraine and observed post-stroke, but the efficacy in relieving psychological stress is still unclear.
Hence, the purpose of this analysis was to evaluate the efficacy and safety of acupuncture for the treatment of migraine. Further, through this research, we also aimed to confirm the effect of acupuncture for improving anxiety.
Materials and methods
Systematic review details
The systematic review was performed in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and was reported in compliance with the PRISMA statement (see Supplementary PRISMA 2009 Checklist).
Search strategy
We searched the following 7 databases from inception to Oct 19th, 2017: PubMed, the Cochrane Library, Web of Science, EMBASE, China Biology Medicine disc (CBM), China National Knowledge Infrastructure (CNKI) and the Wanfang Database. Details of the search strategies are available in the Supplementary Search Terms and Strategies. We also searched the references from the included literature and related systematic reviews to identify further studies that met the inclusion criteria for this review.
Inclusion criteria
Types of studies
Randomized control trials (RCTs) on acupuncture therapy for migraine were included. Quasi-randomized controlled trials (Quasi-RCTs) were excluded. The follow-up time was not limited. And studies meeting the criteria should be included without language and publish limits.
Types of participants
Participants were diagnosed as migraine with aura, without aura or other special types, according to the International Classification of Headache Disorders (ICHD-II) (Jes, 2004). Patients were excluded if the migraine had been caused by organic disorders (such as subarachnoid hemorrhage, cerebral hemorrhage, cerebral embolism, cerebral thrombosis, vascular malformation, arteritis, hypertension, arteriosclerosis, etc.).
Types of interventions
The intervention that we were concerned with in this review was acupuncture therapy. Any treatment that utilized filiform needles to prick acupoints, Ashi points or meridian locations was regarded as acupuncture therapy. Studies based on “microsystems” theory, such as eye-acupuncture and ear-acupuncture, were excluded. Acupoint injection was also excluded.
For included studies, the control group received no treatment, sham acupuncture or medication. No treatment meant that the patients did not receive acupuncture or any other treatment throughout the duration of the study, except when necessary to treat acute attacks. Sham acupuncture was performed without skin penetration, utilizing incorrect acupoint locations, or both. Medication refers to drugs recommended by clinical guidelines, such as calcium antagonists, antiepileptic drugs, and triptans. Traditional Chinese medicine, Chinese patent medicine and non-recommended drugs, such as Nimodipine were excluded. In addition, trials with combined therapies were not included.
Types of outcome measures
The primary outcomes that were selected consisted of the Visual Analog Scale (VAS, from 0 to 10 scores), frequency of migraine attacks (numbers/month), Migraine-Specific Quality of Life Questionnaire (MSQ), and Self-rating Depression Scale (SDS). Secondary outcomes consisted of days of migraine (days/month), adverse events (numbers of adverse event attacks), and total effective rate, which was reported as the percentage of the total participants that showed symptom improvement ≥20%.
Study selection
The reference management software Endnote X7 was used to remove the duplicate records. Two reviewers (H-QC and XL) screened the titles and abstracts of all identified studies for relevance and labeled records as included, excluded, or uncertain. Full-text articles were obtained for assessing eligibility in the case of uncertainty. If studies lacked key information, the reviewers sent emails to the author for further information. If the author did not respond, literature that lacked information was excluded. Disagreements were resolved by the third reviewer (X-YT).
Data extraction
Two reviewers (XW Wang and YH) independently extracted the data. We collected the following information using a standard form: general information (sample size, age, gender and accurate diagnosis), details of the intervention and comparison (study types, duration, treatment frequency, medication dosage, etc.), and the outcomes. Disagreements were resolved by the third reviewer.
Risk of bias assessment
Two reviewers (H-QC and YH) independently assessed the risk of bias using the tool recommended by the Cochrane Collaboration (Higgins and Green, 2011). Each trial was scored as having high, low or unclear risk for the following 7 domains: (1) random sequence generation (selection bias); (2) allocation concealment (selection bias); (3) blinding of participants and personnel (performance bias); (4) blinding of outcome assessment (detection bias); (5) incomplete outcome data (attrition bias); (6) selective reporting (reporting bias); and (7) any other bias. Disagreements were resolved in consultation with the third reviewer (GT).
Statistical analysis
Meta-analysis was performed using RevMan 5.3 software. Continuous data were presented as the mean differences (MDs) with a 95% confidence interval (CI), whereas dichotomous data were presented as relative risk (RR) with a 95% CI. Statistical heterogeneity across trials was assessed by the Cochrane Q test (P < 0.1 for statistical significance) and quantified by the I2 statistic. An I2 >50% indicated significant heterogeneity. Heterogeneous data were pooled using the random-effects model. We performed the analysis based on the time window, which we defined as (1) immediate effects (≤30 min after one treatment); (2) up to 1 month after treatment; (3) 1–3 months after treatment; (4) 3–6 months after treatment; and (5) >6 months after treatment. Subgroup analysis was performed based on adequacy of concealment (unambiguously adequate concealment vs. none or unclear adequacy); sample size (≥median sample vs. < median sample); treatment time (≥1 month vs. < 1 month); sham acupuncture methods (deep insertion at nonacupoints vs. superficial insertion at acupoints vs. superficial insertion at nonacupoints), and types of medication. In addition, to investigate potential sources of heterogeneity in our findings, we performed subgroup analyses. Further sensitivity analysis was conducted to test the impact of the quality of included trials, if needed.
Assessment of reporting biases
Publication bias was evaluated by visual inspection of a funnel plot if we included at least 10 trials in the comparison (Sterne et al., 2011; Chang et al., 2012).
Results
Study selection
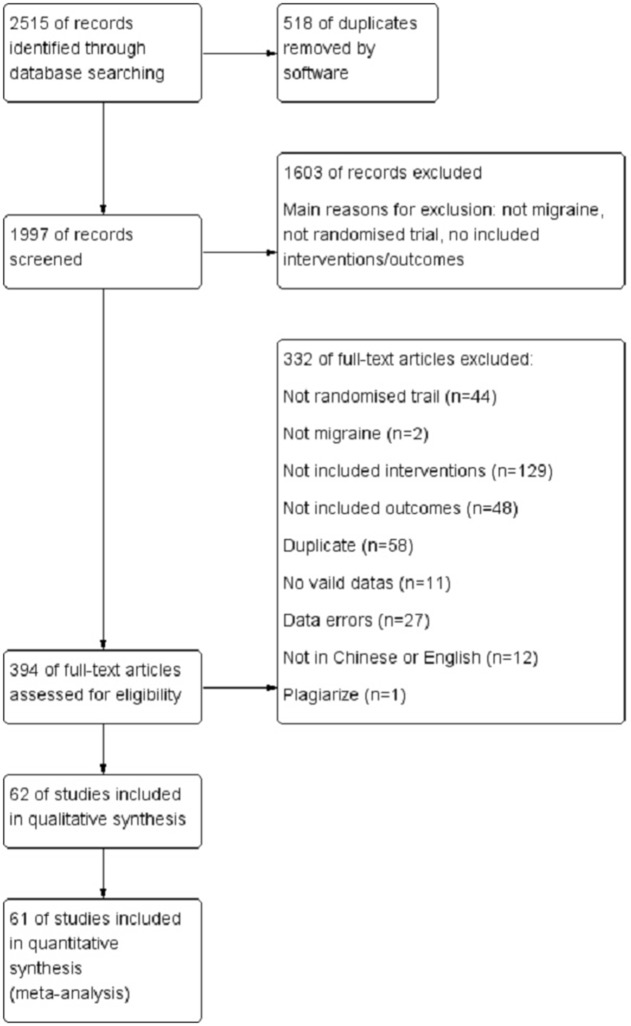
Figure 1 shows a flow chart of the study selection process according to PRISMA guideline. The initial search yielded 2,515 records, of which 518 records were removed for duplication. After screening the titles and abstracts, 394 were deemed to potentially be eligible. After reviewing the full text, 332 records were excluded (2 had patients who were not diagnosed as migraine; 129 used interventions or comparisons that did not meet the standards; 48 measured outcomes that were not included; 44 were not RCTs; 58 were repeatedly published; 11 were conference papers, protocols or other papers without valid data; 27 had data errors; 12 were not published in Chinese or English; and 1 was suspected as being plagiarized). In total, 62 trials were included for the final analysis.
Figure 1.
Flow chart.
Study characteristics
The characteristics of the included studies are summarized in Supplementary Table 1. The 62 studies included 4,947 participants (median number of participants 64.5, range 22–302); 50 trials recruited participants from China, 3 from Brazil, 3 from Germany, 2 from Italy and others from Iran, Israel, Australia and Sweden. For age distribution, 57 studies were performed on adults, 2 on adults and the elderly, 1 on adolescents, and 2 on patients without a reported age range. A total of 41 studies included medication as the control group, 22 included sham acupuncture, and 1 included no treatment. Two studies had three groups for comparison. The main acupoints selected were Shuaigu (GB8), Fengchi (GB20), Yanglingquan (GB34), Zulinqi (GB41), Baihui (GV20), Yintang (GV29), Waiguan (SJ5), Sizhukong (SJ23), and Hegu (LI4). In most studies the treatment time was 1 month (21 trials), 21 trials lasted < 1 month, 3 had a duration of 2 months, 8 had a duration of 3 months, 2 had a duration of 6 months, 6 were evaluated for immediate effects, and only 1 had an unclear treatment time. The treatment frequency was mainly once a day. The follow-up times were reported to be < 1 year, with most focused on 1 month after treatment.
Risk of bias within studies
As presented in Figure 2, most of the included studies were evaluated as having a high risk of bias based on the Cochrane risk of bias tool. There were 23 studies that were at a high risk of bias in allocation concealment, 3 at a high risk of bias in blinding toward participants, 1 at a high risk of bias in blinding of the outcome assessors, 16 at a high risk of bias in attrition bias, and 6 at a high risk of bias in selective reporting bias.
Figure 2.
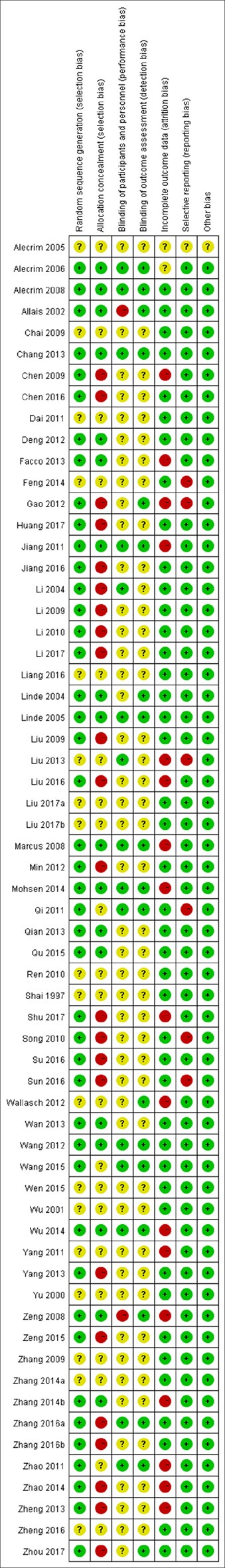
Risk of bias graph.
Effects of interventions
Primary outcomes
VAS scores
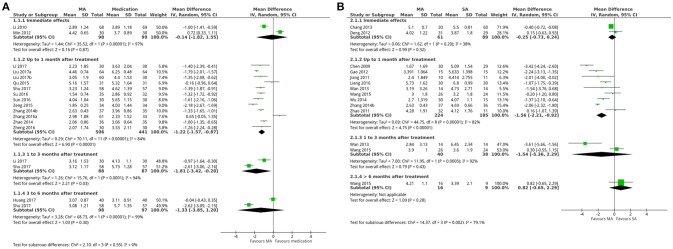
A total of 12 studies that included 947 patients reported VAS scores for acupuncture and medication (Zhang, 2014; Zhao, 2014b; Qu and Shen, 2015; Zeng and Li, 2015; Su et al., 2016; Sun et al., 2016; Zhang X., 2016; Zheng, 2016; Li, 2017; Liu, 2017; Liu et al., 2017; Shu et al., 2017). The pooled results indicated that VAS scores were lower with acupuncture than with medication at a follow-up time of up to 1 month after treatment (random-effects estimates; MD −1.22, 95%CI −1.57 to −0.87; P-value of the Chi2 test <0.00001, I2 = 84%; P-value of Z test <0.00001; low quality; Figure 3A shows the results). While 2 studies that included 175 patients reported VAS scores that were lower in acupuncture compared with medication at a follow-up time of 1–3 months after treatment (random-effects estimates; MD −1.81, 95%CI −3.42 to −0.20; P-value of the Chi2 test <0.0001, I2 = 94%; P-value of Z test = 0.03; very low quality; Figure 3A shows the results; Li, 2017; Shu et al., 2017). For acupuncture and sham acupuncture,a total of 9 trials that included 409 patients presented VAS scores were lower with acupuncture than with sham acupuncture at a follow-up time of up to 1 month after treatment (random-effects estimates; MD −1.56, 95%CI −2.21 to −0.92; P-value of the Chi2 test <0.00001, I2 = 82%; P-value of Z test <0.00001; low quality; Figure 3B shows the results; Chen, 2009; Jiang, 2011; Jiang et al., 2011; Zhao, 2011; Gao, 2012; Wan et al., 2013; Wu, 2014; Zhang, 2014; Wang et al., 2015; Liang et al., 2016).
Figure 3.
Forest plot: (A) acupuncture vs. medication- VAS Scores; (B) sham acupuncture- VAS scores. MA, manual acupuncture; SA, sham acupuncture.
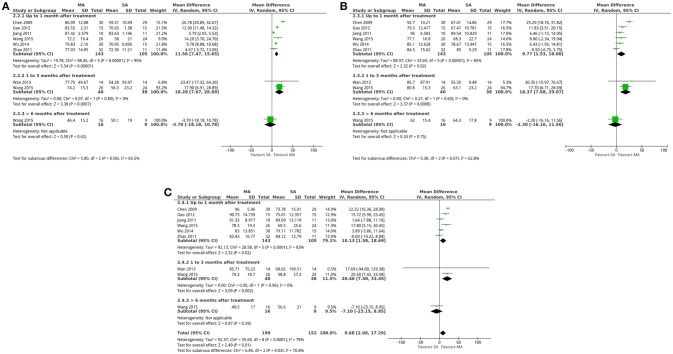
MSQ scores
The pooled results of 6 trials involving 248 patients showed MSQ scores that were greater with acupuncture than sham acupuncture at a follow-up time of up to 1 month after treatment (Chen, 2009; Jiang, 2011; Zhao, 2011; Gao, 2012; Wu, 2014; Wang et al., 2015), which included scores of role function-restrictive (random-effects estimates; MD 11.56, 95%CI 7.47–15.65; P-value of the Chi2 test <0.00001, I2 = 95%; P-value of Z test <0.00001; low quality; Figure 4A shows the results), scores of role function-preventive (random-effects estimates; MD 9.77, 95%CI 1.53–18.00; P-value of the Chi2 test <0.00001, I2 = 85%; P-value of Z test = 0.02; very low quality; Figure 4B shows the results) and scores of emotional function (random-effects estimates; MD 10.13, 95%CI 1.58–18.69; P-value of the Chi2 test <0.00001, I2 = 83%; P-value of Z test = 0.02; very low quality; Figure 4C shows the results). Further, 2 trials that included 78 patients reported MSQ scores for acupuncture and sham acupuncture at a follow-up time of 1–3 months after treatment (Wan et al., 2013; Wang et al., 2015). The pooled results indicated that the MSQ scores were greater with acupuncture than with sham acupuncture, which include scores of role function-restrictive (random-effects estimates; MD 18.28, 95%CI 7.67–28.89; P-value of the Chi2 test = 0.80, I2 = 0%; P-value of Z test = 0.0007; high quality; Figure 4A shows the results), scores of role function-preventive (random-effects estimates; MD 18.37, 95%CI 7.68–29.07; P-value of the Chi2 test = 0.60, I2 = 85%; P-value of Z test = 0.0008; high quality; Figure 4B shows the results) and scores of emotional function (random-effects estimates; MD 20.46, 95%CI 7.48–33.45; P-value of the Chi2 test = 0.96, I2 = 0%; P-value of Z test = 0.002; high quality; Figure 4C shows the results).
Figure 4.
Forest plot: (A) acupuncture vs. sham acupuncture- MSQ scores: (A) role function-restrictive; (B) role function-preventive; (C) emotional function. MA, manual acupuncture; SA, sham acupuncture.
Frequency of migraine attacks
Only 1 trial involving 221 patients, compared with no treatment group, reported attack frequency for up to 1 month after treatment (Linde et al., 2006). The results indicated that the attack frequency was less in the acupuncture group than in the no treatment group (MD −0.80, 95%CI −1.12 to −0.48; P-value of Z test <0.00001; Supplementary Table 2).
Secondary outcomes
Total effective rates
A total of 21 trials that included 1,598 patients showed total effective rates that were greater with acupuncture than medication at a follow-up time of up to 1 month after treatment (random-effects estimates; RR 1.19, 95%CI 1.13–1.27; P-value of the Chi2 test = 0.02, I2 = 43%; P-value of Z test <0.00001; low quality; Supplementary Figure A; Wu, 2001; Li and Jia, 2009; Liu, 2009; Zeng, 2009; Zhang, 2009, 2014; Song, 2010; Dai et al., 2011; Min, 2012; Qian and Wan, 2013; Zheng et al., 2013; Feng et al., 2014; Zhang and Huang, 2014; Zhao, 2014b; Wen, 2015; Chen, 2016; Jiang and Zheng, 2016; Liu and Yan, 2016; Sun et al., 2016; Zhang X., 2016; Li, 2017). The total effective rate was greater with acupuncture than medication in 6 trials that included 465 patients at a follow-up time of 3–6 months after treatment (random-effects estimates; RR 1.18, 95%CI 1.04–1.35; P-value of the Chi2 test = 0.06, I2 = 52%; P-value of Z test = 0.01; low quality; Supplementary Figure A; Song, 2010; Qi, 2011; Liu et al., 2013; Feng et al., 2014; Chen, 2016; Huang et al., 2017). One trial involving 70 patients presented total effective rates that were greater with acupuncture than medication at a follow-up time of more than 6 months (RR 1.43, 95%CI 1.11–1.85, P-value of Z test = 0.005; Supplementary Figure A; Chai, 2009).
There were three trials involving 180 patients who reported the total effective rate for acupuncture and sham acupuncture (Li, 2004; Chen, 2009; Zhang, 2014). The pooled results indicate that the total effective rate was greater with acupuncture than sham acupuncture at a follow-up time of up to 1 month after treatment (fixed-effect estimates; RR 2.43, 95%CI 1.82–3.23; P-value of the Chi2 test = 0.28, I2 = 22%; P-value of Z test <0.00001; low quality; Supplementary Figure F), while the results of 1 trial involving 48 patients presented total effective rates that were greater with acupuncture than sham acupuncture at 3–6 months after treatment (RR 5.21, 95%CI 1.75–15.49; P-value of Z test = 0.003; Supplementary Figure F; Li, 2004).
Days of migraine
One trial (Zhou, 2017) involving 64 patients reported that days of attack were 1.38 days/month less with acupuncture than with medication at a follow-up time of 1–3 months after treatment (MD −1.38, 95%CI −1.97 to −0.79; P-value of Z test <0.00001; Supplementary Figure B). 7 trials that included 488 patients reported days of attack for acupuncture and sham acupuncture at a follow-up time of up to 1 month after treatment (Alecrim-Andrade et al., 2005, 2006, 2008; Linde et al., 2006; Zhao, 2011; Wallasch et al., 2012; Wang et al., 2015). The pooled results indicated that days of attack were fewer with acupuncture compared with sham acupuncture (random-effects estimates; MD −1.30, 95%CI −2.45 to −0.16; P-value of the Chi2 test = 0.02, I2 = 61%; P-value of Z test = 0.03; low quality; Supplementary Figure G).
Adverse events
For adverse events, 14 studies (Yu et al., 2000; Allais et al., 2002; Zeng, 2009; Ren, 2010; Yang et al., 2012; Facco et al., 2013; Qian and Wan, 2013; Yang, 2013; Zheng et al., 2013; Zhao, 2014b; Qu and Shen, 2015; Zhang X., 2016; Zhang Y., 2016; Zhou, 2017) that included 1,245 participants showed that acupuncture had a lower risk than medication (random-effects estimates; RD −0.16, 95%CI −0.25 to −0.06, P-value of the Chi2 test <0.00001, I2 = 93%; P-value of Z test = 0.001; very low quality; Supplementary Figure C).
According to the meta-analysis results, the results of the VAS scores (immediate effects and 3–6 months after treatment; Figure 3A shows the results), attack frequency (up to 1 month after treatment; Supplementary Figure D), SDS scores (up to 1 month after treatment; Supplementary Figure E), total effective rates (1–3 months after treatment; Supplementary Figure A) and days of attack (up to 1 month after treatment; Supplementary Figure B) were similar for both acupuncture and medication groups. While VAS scores (immediate effects, 1–3 months after treatment and more than 6 months after treatment; Figure 3B shows the results), days of attack (more than 1 month after treatment; Supplementary Figure G), attack frequency (up to 6 months after treatment; Supplementary Figure H), MSQ (more than 6 months after treatment; Figure 4), SDS scores (up to 1 month after treatment; Supplementary Figure I), and adverse events (Supplementary Figure J) were similar for both acupuncture and sham acupuncture.
Subgroup analysis
Following the meta-analysis, the comparison between acupuncture and medication indicated significant heterogeneity in terms of VAS scores, effective rate, days of attack and adverse events. Considering the clinical heterogeneity, we designed 4 subgroups for each outcome: sample size, treatment time, adequacy of concealment and type of medication. The results of this subgroup analysis are displayed in Supplementary Table 3. The subgroup analysis compared acupuncture and sham acupuncture for VAS scores (up to 1 month after treatment), attack frequency (up to 1 month, and 1–3 months after treatment), MSQ scores (up to 1 month after treatment) and days of attack (up to 1 month, and 1–3 months after treatment). The following covariates were selected for subgroup analysis: adequacy of concealment, sample size, treatment time and acupuncture methods. Detailed results are shown in Supplementary Table 4.
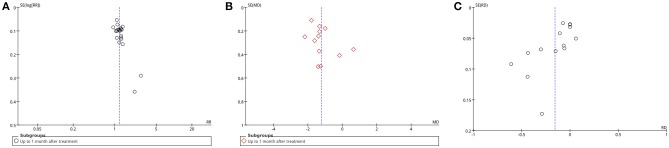
Sensitivity analysis
This analysis also assessed reporting bias in acupuncture vs. medication via funnel plots of the following outcomes: VAS scores (up to 1 month after treatment), effective rate (up to 1 month after treatment), and adverse events. These 3 funnel plots were all asymmetric, so the assessors highly suspected the possibility of reporting bias. Additionally, it was not ruled out that the low methodological quality of the trials, specifically most having a small sample size, exaggerated the effects and caused the asymmetry (Figure 5).
Figure 5.
Funnel plot: (A) manual acupuncture vs. medication-effective rate-up to 1 month after treatment; (B) manual acupuncture vs. medication-VAS scores-up to 1 month after treatment; (C) manual acupuncture vs. medication-adverse events. Note: SE, standard error; RR, risk ratio.
After removing the trials causing asymmetry, a sensitivity analysis was performed for VAS scores (up to 1 month after treatment), and effective rate (up to 1 month after treatment). The detailed results of the sensitivity analysis for effective rate and VAS scores are shown in Table 1.
Table 1.
Detailed information of trials assessed the sensitivity analysis.
| Excluded studies | Participants | MD (95% CI) | P-value | Heterogeneity: I2 | Effect model |
|---|---|---|---|---|---|
| VAS SCORES-UP TO 1 MONTH AFTER TREATMENT | |||||
| Li, 2017 | 60 | −1.21 [−1.57, −0.85] | P < 0.00001 | 86% | Random effects |
| Liu, 2017 | 128 | −1.15 [−1.53,−0.78] | P < 0.00001 | 81% | Random effects |
| Liu et al., 2017 | 90 | −1.21 [−1.58,−0.84] | P < 0.00001 | 86% | Random effects |
| Qu and Shen, 2015 | 62 | −1.30 [−1.65,−0.96] | P < 0.00001 | 83% | Random effects |
| Shu et al., 2017 | 115 | −1.20 [−1.58,−0.82] | P < 0.00001 | 86% | Random effects |
| Su et al., 2016 | 67 | −1.21 [−1.59,−0.82] | P < 0.00001 | 86% | Random effects |
| Sun et al., 2016 | 60 | −1.18 [−1.56,−0.81] | P < 0.00001 | 86% | Random effects |
| Zeng and Li, 2015 | 68 | −1.13 [−1.48,−0.78] | P < 0.00001 | 83% | Random effects |
| Zhang, 2014 | 72 | −1.20 [−1.60, −0.80] | P < 0.00001 | 86% | Random effects |
| Zhang X., 2016 | 94 | −1.39 [−1.66,−1.12] | P < 0.00001 | 72% | Random effects |
| Zhao, 2014b | 71 | −1.24 [−1.62, −0.87] | P < 0.00001 | 84% | Random effects |
| Zheng, 2016 | 60 | −1.22 [−1.58,−0.85] | P < 0.00001 | 86% | Random effects |
| VAS SCORES-UP TO 1 MONTH AFTER TREATMENT | |||||
| Chen, 2016 | 70 | 1.17 [1.12, 1.23] | P < 0.00001 | 18% | Random effects |
| Dai et al., 2011 | 40 | 1.17 [1.12, 1.23] | P < 0.00001 | 18% | Random effects |
| Feng et al., 2014 | 60 | 1.18 [1.12, 1.24] | P < 0.00001 | 17% | Random effects |
| Jiang and Zheng, 2016 | 92 | 1.17 [1.11, 1.22] | P < 0.00001 | 11% | Random effects |
| Li, 2017 | 60 | 1.18 [1.12, 1.24] | P < 0.00001 | 15% | Random effects |
| Liu, 2009 | 60 | 1.18 [1.12, 1.24] | P < 0.00001 | 17% | Random effects |
| Liu and Yan, 2016 | 180 | 1.19 [1.13, 1.25] | P < 0.00001 | 8% | Random effects |
| Qian and Wan, 2013 | 60 | 1.17 [1.12, 1.22] | P < 0.00001 | 13% | Random effects |
| Song, 2010 | 60 | 1.17 [1.12, 1.23] | P < 0.00001 | 17% | Random effects |
| Sun et al., 2016 | 60 | 1.17 [1.12, 1.23] | P < 0.00001 | 15% | Random effects |
| Wen, 2015 | 120 | 1.16 [1.11, 1.21] | P < 0.00001 | 0% | Random effects |
| Wu, 2001 | 63 | 1.17 [1.12, 1.23] | P < 0.00001 | 15% | Random effects |
| Zeng, 2009 | 64 | 1.18 [1.12, 1.24] | P < 0.00001 | 15% | Random effects |
| Zhang, 2009 | 60 | 1.17 [1.11, 1.23] | P < 0.00001 | 15% | Random effects |
| Zhang, 2014 | 80 | 1.17 [1.11, 1.23] | P < 0.00001 | 15% | Random effects |
| Zhang, 2014 | 72 | 1.18 [1.13, 1.24] | P < 0.00001 | 12% | Random effects |
| Zhang X., 2016 | 94 | 1.19 [1.13, 1.24] | P < 0.00001 | 0% | Random effects |
| Zhao, 2014b | 71 | 1.17 [1.12, 1.23] | P < 0.00001 | 17% | Random effects |
| Zheng et al., 2013 | 117 | 1.17 [1.11, 1.22] | P < 0.00001 | 12% | Random effects |
Discussion
Summary of main results
Acupuncture was more effective for short-term treatment compared with no treatment. Compared with medication, manual acupuncture resulted in better efficacy or safety, especially at follow-up times of up to 3 months after treatment, but it exhibited results with statistical heterogeneity. In the comparison between acupuncture and sham acupuncture, participants exhibited better pain relief and improved quality of life at follow-up times of up to 3 months after treatment, although with statistical heterogeneity. In the subgroup analysis, most results did not change significantly. Sensitivity analysis demonstrated that the results of this meta-analysis were stable, and the trials causing asymmetry were mainly due to reporting bias.
Possible explanation of the findings
Despite our findings that acupuncture is superior to sham acupuncture, some trials reported that sham acupuncture had similar effects to medication or acupuncture. Moreover, some heterogeneity still could not be explained by subgroup analysis. Thus, this paper will consider possible explanations.
Potential sources of heterogeneity
Owing to the aim of this research, which was to evaluate the efficacy of acupuncture for migraine, the possible acupuncture techniques should be considered. Specifically, different operators provided different stimulation parameters, which may result in different effects for participants. Additionally, different acupoints were selected for the included trials, which may also cause clinical heterogeneity. Considering the clinical acupuncture procedure, different stimulation parameters and acupoints may be potential sources of heterogeneity.
Low quality of evidence
Some studies have reported that there are few studies regarding acupuncture for migraine with a high quality of evidence (Zhang et al., 2008; Yang et al., 2012). Correspondingly, when selecting literature, 33 papers were excluded for data errors. Further, it is difficult to completely blind all participants and operators, especially for acupuncture operators. Blinding could only be applied for statistic staff and evaluators. Thus, blinding may have some influence on results. In our analysis, most of the included trials did not describe the details of the blinding, and some trials inappropriately designed the sham acupuncture procedure, such as the needle not piercing the skin. Inappropriate sham procedures obviously differ from acupuncture, so patients can easily see through the blinding, which will influence the results.
Lacking unified standards for sham acupuncture
There are no uniform standards for sham acupuncture, and disputes have arisen regarding sham acupuncture methods used in clinical research (Lund et al., 2009; Jiang et al., 2011; Zhou, 2017). Even some so-called sham acupuncture procedures may have the same effects as the acupuncture. According to current research, sham acupuncture using superficial insertion at acupoints, is also a common therapy, such as eye-acupuncture or ear-acupuncture. A previous study also indicated that even if there is no insertion, placebo needling could also stimulate the amyelinic afferent nerve, thereby affecting the pain transduction (Lund and Lundeberg, 2006). Therefore, superficial insertion cannot simply be regarded as a sham acupuncture. Further, in related trials in which verum and sham acupuncture had similar effects, it is not possible to determine that acupuncture only had a placebo effect. In terms of nonacupoint sham procedures, these are problematic in that the range of acupoint areas has not been defined or confirmed. Further, a study held that acupoints would exhibit sensitization and that the range of acupoints could be enlarged under disease (Qi et al., 2017). Thus, it cannot be determined if areas nearby the acupoints belong to nonacupoint areas.
Quality of the evidence
The methodological quality of the included trials was variable. Methods for sequence generation, data handling for dropout or loss to follow-up and reporting were appropriate in most trials. However, ~1/3 of trials were at high risk for allocation concealment, and 1/3 were unclear without detailed allocation concealment. Furthermore, blinding was not adequately described in most studies. This analysis determined that the overall quality of the evidence for most outcomes was of low to moderate quality. Reasons for diminished quality consist of the following: no mentioned or inadequate allocation concealment, great probability of reporting bias, study heterogeneity, sub-standard sample size, and dropout without analysis.
Strength and limitations
Agreements and disagreements with other studies or reviews
16 systematic reviews have evaluated the effects of acupuncture for migraine (Gao et al., 2011; Zheng and Cui, 2012; Chen, 2014; Yang et al., 2014, 2015; Zhao, 2014a, 2016; Dai and Lin, 2015; Jiang, 2015; Linde et al., 2016; Pu, 2016; Pu et al., 2016, 2017; Song et al., 2016; Xian, 2016; Chen et al., 2018) and the related details are available in Table 2. Results from those researches all showed that acupuncture had certain effects for migraine and were consistent with our meta-analysis. A recent Cochrane systematic review (Linde et al., 2016) reported that acupuncture had an effect for migraine over sham acupuncture, but this effect was small. Acupuncture might be at least similarly effective as treatment with prophylactic drugs. According to Dai et al. Dai and Lin (2015), the effective rate is high in acupuncture than in medication while the cure rates is similar between acupuncture and medication. However, unlike previous results, our analysis found that acupuncture is obviously better than sham acupuncture and medication.
Table 2.
List and information of previous systematic reviews analyzing acupuncture therapy for migraine.
| Researches | Language | Type | No. of trials | Comparisons | Primary outcomes | Search fields |
|---|---|---|---|---|---|---|
| Gao et al., 2011 | Chinese | Migraine | 12 | AC vs. SA | Effective rates, days of migraine | PubMed, Cochrane Library, CBM |
| Linde et al., 2016 | English | Episodic migraine | 22 | AC vs. NT, AC vs. SA, AC vs. ME | headache frequency at completion of treatment and at follow-up (closest to 6 months after randomization), response (at least 50% reduction in migraine), number of participants dropping out due to adverse effects | Cochrane Library, MEDLINE, EMBASE, AMED, ICTRP, Clinical Trials.gov, reference lists of all eligible studies |
| Song et al., 2016 | Chinese | Migraine | 18 | AC/EA (or with placebo) vs. ME (or with placebo) | Shor-term effective rates (1–3 months), long-term effective rates (>3 months), days of migraine, adverse events | Cochrane Library, PubMed, Medline, CNKI, VIP, Wanfang data, Google website and Baidu website |
| Zheng and Cui, 2012 | Chinese | Migraine | 33 | AC vs. ME, AC vs. TCM, AC vs. SA | Effective rates | PubMed, EMbase, CBM, CNKI, VIP, Wanfang data |
| Pu, 2016 | Chinese | Acute migraine | 5 | AC vs. SA | VAS scores (2 h after treatment) | PubMed, Medline, Cochrane Library, CBM, CNKI, Wanfang data |
| Yang et al., 2014 | Chinese | Migraine | 10 | AC vs. Flunarizine | Shor-term effective rates, long-term effective rates, migraine index, adverse events | PubMed, Cochrane Library, CNKI, VIP, Wanfang data |
| Zhao, 2016 | Chinese | Menstrual migraine | 30 | AC vs. ME, AC vs. TCM, BT vs. TCM, AC with ear-acupuncture vs. ME | Total effective rates, migraine index, headache level, lasting time of migraine, adverse events | CBM, CNKI, VIP, CMCC, PubMed, EMBASE, SCI, Cochrane Library |
| Dai and Lin, 2015 | Chinese | Migraine | 2 | AC vs. ME | Cure rates, Significantly effective rates, effective rates | PubMed, Cochrane Library, CNKI, VIP, Wanfang data |
| Xian, 2016 | Chinese | Migraine prophylaxis | 26 | AC vs. NT, AC vs. SA, AC vs. ME | Effective rates, days of migraine, frequency of migraine, headache level, medication use, lasting time of migraine attack, PDI, MIDAS, SF-36, SF-12, adverse events | PubMed, Cochrane Library, EMBASE, CNKI, VIP, Wanfang data, CBM, TCM database |
| Jiang, 2015 | Chinese | Migraine | 18 | EA vs. ME, EA with other therapy vs. ESA and EA vs. AC | Total effective rates, VAS scores | Medline, Cochrane Library, EMBASE, CNKI, VIP, Wanfang data, CBM |
| Chen, 2014 | Chinese | Migraine | 18 | AC vs. ME, AC vs. Other Chinese therapy, AC vs. Other treatment | Effective rates, Migraine attack, lasting time of migraine, accompanying symptoms, TCD results, VAS scores, adverse events | Medline, Cochrane Library, EMBASE, CNKI, VIP, Wanfang data, CBM |
| Pu, 2016 | Chinese | Migraine | 7 | AC vs. ME | Effective rates, days of migraine, migraine attack, medication use, rates of adverse events | Medline, Cochrane Library, EMBASE, CNKI, VIP, Wanfang data, CBM |
| Zhao, 2011 | Chinese | Migraine | 17 | EA vs. ME, EA with other therapy vs. ME, EA vs. AC | Effective rates, VAS scores | PubMed, Cochrane Library, EMBASE, CNKI, VIP, CBM |
| Chen et al., 2018 | Chinese | Migraine | 18 | AC vs. ME | Total effective rates, rates of adverse events, recurrence rate | CNKI, VIP, Wanfang data |
| Pu et al., 2017 | Chinese | Migraine prophylaxis | 7 | AC vs. ME | Effective rates, days of migraine, VAS scores, rates of adverse events | PubMed, Cochrane Library, EMBASE, CNKI, VIP, Wanfang data, CBM |
| Yang et al., 2015 | Chinese | Migraine | 10 | AC vs. SA | Overall response, headache characteristics, accompanying symptoms, medication use, adverse events | PubMed, Cochrane Library, Web of Science, CNKI, VIP, Wanfang data, CBM |
No, number; AC, acupuncture; SA, sham acupuncture; ME, medication; EA, electroacupuncture; SEA, sham electroacupuncture; TCM, traditional Chinese medicine; BT, bleeding therapy; NT, no treatment.
Compared with previous researches, we focused on the effect of manual acupuncture, other than the broadly-defined acupuncture and excluded studies of acupoint injection, eye-acupuncture, etc. We found that 43.8% of systematic reviews only included one comparison; while in our research, the control group received no treatment, sham acupuncture or medication so that the range of comparisons could be more comprehensive. Besides, both search fields and time range we searched was broader than that in the previous meta-analysis. Moreover, we included more trials with the latest evidence than the previous researches. It could be that the range we searched and analyzed were more comprehensive than before. In addition, the outcomes that we measured were more comprehensive. All the previous meta-analysis included outcomes related to efficacy or safety of treatment. Specifically, our focuses on primary outcomes included not only efficacy and safety but also the evaluated patient-related outcomes, such as MSQ scores and SDS scores. Through MSQ scores and SDS scores, we could evaluate the psychological states and life quality after treatment. By assessing the efficacy of treatment and quality of life in migraine patients, we aimed to comprehensively verify acupuncture's improvement of the quality of life in migraine patients. Thus, this analysis could evaluate many aspects of the effectiveness of acupuncture for migraine, which is significantly different from previous systematic reviews. Furthermore, our study also considered the sources of heterogeneity and conducted subgroup analysis. Therefore, our research analyzed the included studies more systematically than previous researches and the results of this study are reliable.
Limitations of study
It is possible that some trials were published in other languages and were therefore not included in this analysis. Besides, it cannot rule out that some trials with small sample size have not been published. In future research, we would aim to identify these studies. Additionally, taken the vast difference in the number of acupoints, the theory of acupoint selection, and the operation, we only evaluated the overall efficacy and safety of acupuncture rather than the acupoint itself. The different acupoints and their combination may cause different effect, which deserves further exploration.
Implications
Implications for practice
Acupuncture has certain efficacy both in the treatment and prevention of migraine and is superior to no treatment, sham acupuncture and medication. Additionally, acupuncture is safer than medication. Acupuncture may be an appropriate treatment for migraine, especially for patients who cannot tolerate preventive pharmacotherapy or the accompanying adverse events.
Implications for research
Based on the less rigorous design used in most acupuncture clinical trials, there is an urgent need to improve the quality of evidence in the design phase. First, appropriate randomized methods should be used, such as tables of random numbers and computer-controlled random sequence generation. Blinding should also be implemented for participants, statistics staff and assessors. Additionally, it may be better to separate participants into different groups, to avoid communication with each other. If sham acupuncture is used as a comparison, some well-designed placebo needles, such as the Streiberger needle, should be utilized (Xie et al., 2013). Further, sample size calculations should be made before trials.
For the population, none of the included studies reported the races of the populations, the researchers should specify the research objects that the results are applicable to. For outcomes, pain-related outcomes can directly reflect the relief of migraine, while outcomes like MSQ, SDS and SAS scores can show the efficacy on living quality and psychology etc. We suggest researchers use different outcomes to evaluate the efficacy for migraine instead of a single effective rate. To optimize the outcome evaluation, we are planning to establish a core outcome set for migraine. For research follow-up, trials with more than 6-months follow-up are rare. The current researches mainly focus on the short-term efficacy. More longitudinal studies evaluating the long-term effects of acupuncture for migraine are needed.
Moreover, the clinical trials on migraine lack uniform criteria regarding diagnosis, outcome selection, and reports. If both patients and doctors can be involved in setting these standards, it will be helpful for establishing standard criteria regarding migraine diagnosis, treatment and reports. In addition, it would be helpful to develop an optimal design of acupuncture that quantifies and regulates acupoints selection, manipulation, depth, angle, frequency, etc. Data from large studies with a high quality of evidence, such as clinical RCTs, may help doctors to select the most suitable treatment. Thus, further well-designed comparisons regarding acupuncture are needed.
Conclusions
Acupuncture is superior to no treatment, sham acupuncture and medication, both in terms of efficacy and safety. Acupuncture could be recommended as one of the effective therapies for migraine. However, evidence are not enough to guide the operation of acupuncture for migraine, including the acupoints selection, the best course and frequency of treatment. Further large-sample, well-designed studies examining the effectiveness of acupuncture are needed.
Author contributions
YJ, PB, and HC contributed equally to this paper. G-HT, Y-PL and YJ developed the research ideas and then designed the search strategy. G-HT, X-YT, X-LW, X-YL, and H-QC screened the abstract and full text. G-HT, X-YT, X-LW, X-YL, H-QC, and Y-YH extracted the data. X-YT, H-QC, and Y-YH evaluated the risks of bias. X-YT analyzed the data and is the guarantor. YJ, H-QC and X-YT wrote the first draft of the manuscript. PB and HC interpreted the results, refined the idea of the study. X-YZ revised the draft, including the language and managed the submission. All authors interpreted the data analysis and critically revised the manuscript.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The reviewer TS and handling Editor declared their shared affiliation.
Acknowledgments
We would like to thank the following individuals: Yan Liu, China Academy of Chinese Medical Sciences, for his guidance in data analysis, and Jin-hui Tian, Evidence-Based Medicine Center of Lanzhou University, for developing the searches.
Footnotes
Funding. This article was funded by the National Natural Science Foundation of China (81674050).
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2018.01190/full#supplementary-material
References
- Alecrim-Andrade J., Maciel-Junior J., Carne X., Severino Vasconcelos G., Correa-Filho H. (2008). Acupuncture in migraine prevention: a randomized sham controlled study with 6-months posttreatment follow-up. Clin. J. Pain 24, 98–105. 10.1097/AJP.0b013e3181590d66 [DOI] [PubMed] [Google Scholar]
- Alecrim-Andrade J., Maciel-Junior J., Cladellas X., Correa-Filho H., Machado H. (2006). Acupuncture in migraine prophylaxis: a randomized sham-controlled trial. Cephalalgia 26, 520–529. 10.1111/j.1468-2982.2006.01062.x [DOI] [PubMed] [Google Scholar]
- Alecrim-Andrade J., Maciel-Júnior J., Cladellas XC. (2005). Efficacy of acupuncture in migraine attack prophylaxis: a randomized sham-controlled trial. Cephalalgia 25:942. [DOI] [PubMed] [Google Scholar]
- Allais G., De Lorenzo C., Quirico P., Airola G., Tolardo G., Mana O., et al. (2002). Acupuncture in the prophylactic treatment of migraine without aura: a comparison with flunarizine. Headache 42, 855–861. 10.1046/j.1526-4610.2002.02203.x [DOI] [PubMed] [Google Scholar]
- Bodeker G., Ong C. K., Grundy C., Burford G., Shein K. (2005). WHO Global Atlas of Traditional, Complementary and Alternative Medicine. Kobe: WHO Center for Health Development. [Google Scholar]
- Burke A., Upchurch D., Dye C., Chyu L. (2006). Acupuncture use in the United States: findings from the National Health Interview Survey. J. Alter. Complement. Med. 12, 639–648. 10.1089/acm.2006.12.639 [DOI] [PubMed] [Google Scholar]
- Chai L. (2009). Observation on acupuncture for refractory migraine. World Health Digest. 6, 6–7. 10.3969/j.issn.1672-5085.2009.33.002 [DOI] [Google Scholar]
- Chang X., Liu W., Liu M. (2012). Acupuncture at shaoyang specific acupoints for acute migraine and its VAS scores and headache intensity of immdediate effects in different phases, in Collection of Academic Papers for The Twelfth Session National Acupuncture and Moxibustion Symposium of China Association for Acupuncture and Moxibustion. Guiyang. [Google Scholar]
- Chen F. (2016). Clinical observation of ashi point treating migraine with syndrome of hyperactivity of liver Yang. J. Pract. Trad. Chin. Med. 32, 259–260. 10.3969/j.issn.1004-2814.2016.03.051 [DOI] [Google Scholar]
- Chen H. (2009). Clinical Study on Acupuncture Therapy of Migraine with Shaoyang Specific Acupoints. [M. Medicine]. Hunan University of Chinese Medicine, Changsha. [Google Scholar]
- Chen L., He X., Xu H., Zhou Z., Liu C., Yang Q. (2018). A Meta-analysis on randomized controlled trials of acupuncture for migraine. Hunan J. Tradit. Chin. Med. 34, 125–129. 10.16808/j.cnki.issn1003-7705.2018.02.064 [DOI] [Google Scholar]
- Chen W. (2014). Systematic Review for Short-Term Effects of Acupuncture in Treating Migraine. [M. Medicine]. Chengdu: Chengdu University of Traditional Chinese Medicine. [Google Scholar]
- Cranz H. (1990). Over-the-counter drugs. Drug Saf. 5, 120–125. 10.2165/00002018-199000051-00019 [DOI] [PubMed] [Google Scholar]
- Dai M., Jin M., Shen W. (2011). Clinical observation on acupuncture for migraine. J. Acupuncture Tuina Sci. 9, 84–87. 10.1007/s11726-011-0477-5 [DOI] [Google Scholar]
- Dai X., Lin C. (2015). A meta-analysis of treating migraine by acupuncture. Clin. J. Chin. Med. 7, 1–3. 10.3969/j.issn.1674-7860.2015.35.001 [DOI] [Google Scholar]
- Diener H., Solbach K., Holle D., Gaul C. (2015). Integrated care for chronic migraine patients: epidemiology, burden, diagnosis and treatment options. Clin. Med. 15, 344–350. 10.7861/clinmedicine.15-4-344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facco E., Liguori A., Petti F., Fauci A., Cavallin F., Zanette G. (2013). Acupuncture versus valproic acid in the prophylaxis of migraine without aura: a prospective controlled study. Minerva Anestesiol. 79, 634–642. [PubMed] [Google Scholar]
- Feng Z., Wang Y., Jin S., Wu L., He W. (2014). Observation of the clinical curative of Xing Nao Kai Qiao acupuncture with differentiation in the treatment of migraine of migraine of Tan Zhuo Shang Rao Type. Chinese Commun Doctors 82–85. [Google Scholar]
- Gao X., Wang B., Song Y., Qi H., Rong Z., Wang H. (2011). A systematic review and meta-analysis on acupuncture for migraine. Chin. J. Clin. Pharm. Therap. 16, 530–537. [Google Scholar]
- Gao Y. (2012). Dynamic Impact of the Specific Acupoints of the Shaoyang Meridian on Brain Function of Migraineurs: a fMRI Study. Ph.D. thesis. Chengdu: Chengdu University of Chinese Medicine. [Google Scholar]
- group CMAopchp (2016). Guide to the prevention and treatment of migraine in China. Chin. J. Pain Med. 22, 721–727. 10.3969/j.issn.1006-9852.2016.10.001 [DOI] [Google Scholar]
- Hartel U., Volger E. (2004). Use and acceptance of classical natural and alternative medicine in Germany–findings of a representative population-based survey. Forsch. Komplementarmed. Klass. Naturheilkund. 11, 327–334. 10.1159/000082814 [DOI] [PubMed] [Google Scholar]
- Higgins J., Green S. (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0: The Cochrane Collaboration. Available online at: www.cochrane-handbook.org
- Holland S., Silberstein S., Freitag F., Dodick D., Argoff C., Ashman E. (2012). Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the quality standards subcommittee of the american academy of neurology and the american headache society. Neurology 78, 1346–1353. 10.1212/WNL.0b013e3182535d0c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang G., Sun Q., Huang R. (2017). Observation on the curative effect of acupuncture combined with gabapentin in the treatment of migraine. Clin. Med. Eng. 24, 615–616. 10.3969/j.issn.1674-4659.2017.05.0615 [DOI] [Google Scholar]
- Jes O. (2004). The international classification of headache disorders. Am. J. Ophthalmol. 138:689.15488823 [Google Scholar]
- Jiang C. (2011). A Study of Effects and fMRI: Acupuncture for Treating Migraine With Acupoints and Non-acupoints. [M. Medicine]. Chengdu: Chengdu University of TCM. [Google Scholar]
- Jiang J., Zheng Y. (2016). Clinical observation of acupuncture on the treatment of migraine and its influence on headache integral. Hebei J. Tradit. Chin. Med. 38, 1382–1384. 10.3969/j.issn.1002-2619.2016.09.026 [DOI] [Google Scholar]
- Jiang X. (2015). Systematic Review for Effects and Safety of Electro-Acupuncture in Treating Migraine. [M. Medicine]. Chengdu: Chengdu University of Traditional Chinese Medicine. [Google Scholar]
- Jiang Y., Yin L., Wang Y., Shan C., Liu Y., Xu Y., et al. (2011). Assessments of different kinds of sham acupuncture applied in randomized controlled trials. J. Acupuncture Tuina Sci. 9, 199–203. 10.1007/s11726-011-0511-7 [DOI] [Google Scholar]
- Li D. (2017). Clinical Study on Treatment of Migraine with Hyperactivity of Liver Yang by means of “Ping Wan Li Zhi Acupuncture Manipulation”. [M. Medicine]. Kunming: Yunnan University of TCM. [Google Scholar]
- Li D., Jia B. (2009). Clinical study on excessive rising of liver migraine with acupuncture. Liaon. J. Tradit. Chin. Med. 36, 1579–1581. 10.13192/j.ljtcm.2009.09.143.lidm.053 [DOI] [Google Scholar]
- Li Y., Zheng H., Witt C., Roll S., Yu S., Yan J., et al. (2012). Acupuncture for migraine prophylaxis: a randomized controlled trial. CMAJ 184, 401–410. 10.1503/cmaj.110551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z. (2004). Evaluation of Clinical Effectiveness of Acupuncture for Migraine on the Basis of Evidence-Based Medicine. [M. Medicine]. Harbin: Heilongjiang University of Chinese Medicine. [Google Scholar]
- Liang R., Zhang S., Xie Y. (2016). Study about influence of brain metabolism in patients with chronic migraine after acupuncture at shaoyang specific acupoints. Chin. Arch. Tradit. Chin. Med. 34, 918–920. 10.13193/j.issn.1673-7717.2016.04.045 [DOI] [Google Scholar]
- Linde K., Allais G., Brinkhaus B., Fei Y., Mehring M., Vertosick E., et al. (2016). Acupuncture for the prevention of episodic migraine. Cochrane Database Syst. Rev. 28:Cd001218 10.1002/14651858.CD001218.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde K., Allais G., Brinkhaus B., Manheimer E., Vickers A., White A. (2009). Acupuncture for migraine prophylaxis. Cochrane Database of Syst. Rev. 21:Cd001218 10.1002/14651858.CD001218.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde K., Streng A., Hoppe A., Brinkhaus B., Witt C., Hammes M., et al. (2006). Treatment in a randomized multicenter trial of acupuncture for migraine (ART migraine). Forsch. Komplementarmed. 13, 101–108. 10.1159/000091999 [DOI] [PubMed] [Google Scholar]
- Linde K., Streng A., Jurgens S., Hoppe A., Brinkhaus B., Witt C., et al. (2005). Acupuncture for patients with migraine: a randomized controlled trial. Jama. 293, 2118–2125. 10.1001/jama.293.17.2118 [DOI] [PubMed] [Google Scholar]
- Lipton R., Newman L., Solomon S. (1994). Over-the-counter medication and the treatment of migraine. Headache 34, 547–548. 10.1111/j.1526-4610.1994.hed3409547.x [DOI] [PubMed] [Google Scholar]
- Liu B., Yan J. (2016). Observation of clinical effect about syndrome differentiation acupuncture therapy on chronic migraine and autonomic nerve function. Hanghai J. Tradit. Chin. Med. 50, 65–67. 10.16305/j.1007-1334.2016.03.020 [DOI] [Google Scholar]
- Liu F. (2009). Clinical Observation on the Acupunture Therapying the Menstruation Migraine. [M. Medicine]. Guangzhou: Guangzhou University of Chinese Medicine. [Google Scholar]
- Liu L. (2017). Clinical study on acupuncture for migraine. Contemp. Med. Forum. 15, 128–129. 10.3969/j.issn.2095-7629.2017.12.095 [DOI] [Google Scholar]
- Liu P., Guo X., Lu G., Li J. (2013). Observation on curative effect of acupoint injection in treatment of menstrual migraine. Matern. Child Health Care China.28, 4542–4543. 10.7620/zgfybj.j.issn.1001-4411.2013.28.42 [DOI] [Google Scholar]
- Liu Q., Qin X., Zhang Y. (2017). Warming-unblocking needling for migraine without aura: 30 cases. TCM Res. 30, 37–40. 10.3969/j.issn.1001-6910.2017.09.16 [DOI] [Google Scholar]
- Lund I., Lundeberg T. (2006). Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupuncture Med. 24, 13–15. 10.1136/aim.24.1.13 [DOI] [PubMed] [Google Scholar]
- Lund I., Naslund J., Lundeberg T. (2009). Minimal acupuncture is not a valid placebo control in randomised controlled trials of acupuncture: a physiologist's perspective. Chin. Med. 30:1 10.1186/1749-8546-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meissner K., Fassler M., Rucker G., Kleijnen J., Hrobjartsson A., Schneider A., et al. (2013). Differential effectiveness of placebo treatments: a systematic review of migraine prophylaxis. JAMA Intern. Med. 173, 1941–1951. 10.1001/jamainternmed.2013.10391 [DOI] [PubMed] [Google Scholar]
- Min D. (2012). Acupuncture Hand-Foot-Shaoyang Meridian Points Treat the Migraine and Clinical Observation Immediate Analgesic Effect and Long Term Curative Effect. [M. Medicine]. Harbin: Heilongjiang University of Chinese Medicine. [Google Scholar]
- Pu S. (2016). Effectiveness and Safety of Acupuncture Versus Drug Treatment for Migraine Prophylaxis: A Meta-Analysis. [M. Medicine]. Chongqing: Chongqing Medical University. [Google Scholar]
- Pu S., Tan G., Deng Y., Li L., Zhu Q., Jiang H. (2017). Effectiveness and safety of acupuncture versus drug treatment for migraine prophylaxis: a meta-analysis. J. Chongqing Med. Univ. 42, 1293–1298. 10.13406/j.cnki.cyxb.001397 [DOI] [Google Scholar]
- Pu S., Tan G., Wang D., Chen J., Jiang L. (2016). Analgesic effect of acupuncture during migraine acute attack: a meta analysis. Chongqing Med. 45, 1353–1356. 10.3969/j.issn.1671-8348.2016.10.018 [DOI] [Google Scholar]
- Qi P. (2011). Clinical Study on Penetrated Needling on Preventive Treatment for Common Migraine. [M. Medicine]. Beijing: Beijing University of Chinese Medicine. [Google Scholar]
- Qi Z., Chen L., Kan Y., Zhang X., He W., Xiu Y., et al. (2017). Pressure pain threshold change between acupoints on patients of functional bowel disease and intestinal cancer. World Chin. Med. 12, 1911–1914. 10.3969/j.issn.1673-7202.2017.08.047 [DOI] [Google Scholar]
- Qian L., Wan Q. (2013). Acupuncture treatment of paroxysmal migraine random parallel control study. Shiyong zhong yineike zazhi. 27, 76–78. 10.3969/j.issn.1671-7813.2013.09 [DOI] [Google Scholar]
- Qu X., Shen Y. (2015). Comparison between acupuncture with flunarizine hydrochloride for preventive treatment of migraine. Shananxi Zhongyi 723–724. [Google Scholar]
- Ren J. (2010). Acupuncture for migriane: 120 cases. Shanghai J. Acup. Moxib. 731. 10.3969/j.issn.1005-0957.2010.11.731 [DOI] [Google Scholar]
- Rodriguez A. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 386, 743–800. 10.1016/S0140-6736(15)60692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu W., Peng T., Huang X., Hu S., Zhou C., Xie G., et al. (2017). Observations on the efficacy of intermittent liver-nourishing and mind-regulating acupuncture in preventive treatment of migraine. Shanghai J. Acup. Moxib. 36, 727–730. 10.13460/j.issn.1005-0957.2017.06.0727 [DOI] [Google Scholar]
- Silberstein S., Holland S., Freitag F., Dodick D., Argoff C., Ashman E. (2012a). Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the quality standards subcommittee of the american academy of neurology and the american headache society. Neurology. 78, 1337–1345. 10.1212/WNL.0b013e3182535d20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberstein S., Young W. (1995). Analgesic rebound headache. How great is the problem and what can be done? Drug safety 13, 133–144. 10.2165/00002018-199513030-00001 [DOI] [PubMed] [Google Scholar]
- Silberstein S. D., Latsko M., Schoenen J. (2012b). Preventive antimigraine drugs, in Multidisciplinary Management of Migraine, eds Fernandez-de-las-Penas C., Chaitow L., Schoenen J. (Burlington, MA: Jones & Bartlett Learning; ), 91–102. [Google Scholar]
- Song Q., Zhao S., Li L., Shen Y., Wang S. (2016). Acupuncture for preventive treatment of migraine compared with medication: a meta-analysis. Liaon. J. Tradit. Chin. Med. 43, 821–826. 10.13192/j.issn.1000-1719.2016.04.053 [DOI] [Google Scholar]
- Song W. (2010). Clinical on Treatment of Migraine Primary by Acupuncture FENGCHI (GB20). [M. Medicine]. Harbin: Heilongjiang University of Chinese Medicine. [Google Scholar]
- Steiner T., Stovner L., Birbeck G. (2013). Migraine: the seventh disabler. Cephalalgia 33, 289–290. 10.1177/0333102412473843 [DOI] [PubMed] [Google Scholar]
- Sterne J. A., Sutton A. J., Ioannidis J. P. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- Su H., Li J., Du Y. (2016). Observation of acupuncture by tiaoshen shugan needling therapy for migraine: 35 cases. Hunan J. Tradit. Chin. Med. 32, 102–103. 10.16808/j.cnki.issn1003-7705.2016.08.046 [DOI] [Google Scholar]
- Sun Y., Guo W., Sun Y. (2016). Observation on acupuncture for migraine without aura. J. Front. Med. 6, 307–308. [Google Scholar]
- Vos T., Flaxman A., Naghavi M., Lozano R., Michaud C., Ezzati M., et al. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study (2010). Lancet 380, 2163–2196. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallasch T., Weinschuetz T., Mueller B., Kropp P. (2012). Cerebrovascular response in migraineurs during prophylactic treatment with acupuncture: a randomized controlled trial. J. Alter. Complement. Med. 18, 777–783. 10.1089/acm.2011.0308 [DOI] [PubMed] [Google Scholar]
- Wan M., Huang Y., Liang X., He W., Liang F., Jia H., et al. (2013). The study on efficacy evaluation of treatment the type of hyperactivity of liver yang of migraine without Aura by meridian. Lishizhen Med. Mater. Med. Res. 24, 986–988. 10.3969/j.issn.1008-0805.2013.04.102 [DOI] [Google Scholar]
- Wang Y., Xue C., Helme R., Da Costa C., Zheng Z. (2015). Acupuncture for frequent migraine: a randomized, patient/assessor blinded, controlled trial with one-year follow-up. Evid. Based Complement. Alter. Med. 2015:920353. 10.1155/2015/920353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen L. (2015). Clinical curation effect evaluation of acupuncture treatment of migraine in acute stage. Chin. Commun. Doctors. 31, 98–99. 10.3969/j.issn.1007-614x.2015.14.60 [DOI] [Google Scholar]
- Wu F. (2014). The Clinical Curative Effect of Acupuncture for Migraine at Acupoints on Involved Meridian and Its Impact on Plasma. [M. Medicine]. Chengdu: Chengdu University of Chinese Medicine. [Google Scholar]
- Wu J. (2001). Study on Clinical Effect and Biochemistry Mechanism of Migraine with Acupuncture Therapy. [M. Medicine]. Harbin: Heilongjiang University of Chinese Medicine. [Google Scholar]
- Xian J. (2016). A Systematic Review and Correlation Analysis of Selected Acupoint of Acupuncture for Migraine Prophylaxis. [M. Medicine]. Jinan: Shandong University of Traditional Chinese Medicine. [Google Scholar]
- Xie C., Wen X., Jiang L., Xie M., Fu W. (2013). Validity of the “Streitberger” needle in a chinese population with acupuncture: a randomized, single-blinded, and crossover pilot study. Evid. Based Complement. Alter. Med. 2013:251603. 10.1155/2013/251603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C., Liu H., Zhang Y., Wang L. (2012). Reports quality evaluation on acupuncture for treating acute attacks of migraine. Chin. J. Evid. Based Med. 12, 365–370. 10.3969/j.issn.1672-2531.2012.03.020 [DOI] [Google Scholar]
- Yang J., Shen Y., Wang S. (2014). Systematic review on efficacy for migraine treatment by acupuncture and flunarizine. Modernization of Traditional Chinese Medicine and Materia Materia-World Science and Technology. 16. [Google Scholar]
- Yang X. (2013). Study on curative effects of acupuncture for treatment of migraine. J. Zhejiang Univ. Tradit. Chin. Med. 5, 617–619. 10.3969/j.issn.1005-5509.2013.05.044 [DOI] [Google Scholar]
- Yang Y., Que Q., Ye X., Zheng G. (2015). Verum versus sham manual acupuncture for migraine: a systematic review of randomised controlled trials. Acupunct. Med. 34,76–83. 10.1136/acupmed-2015-010903 [DOI] [PubMed] [Google Scholar]
- Yu S., Liu R., Zhao G., Yang X., Qiao X., Feng J., et al. (2012). The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache 52, 582–591. 10.1111/j.1526-4610.2011.02061.x [DOI] [PubMed] [Google Scholar]
- Yu W., Shen F., Weng Z., Hu D., Wu J., Chen G. (2000). Clinical research in acupuncture treatment of acute attack of vascular headache. Shanghai J Acup Moxib. 19, 18–19. 10.13460/j.issn.1005-0957.2000.02.009 [DOI] [Google Scholar]
- Zeng L., Li G. (2015). Effect of acupuncture in migraine patients and its influence on serum MMP -2 Activity. Liaon. J. Tradit. Chin. Med. 42, 1971–1974. 10.13192/j.issn.1000-1719.2015.10.060 [DOI] [Google Scholar]
- Zeng S. (2009). Clinical Observation on Acupunctue Treatment with Migraine Without Aura. [M. Medicine]. Chengdu: Chengdu University of TCM. [Google Scholar]
- Zhang M., Huang Z. (2014). Acupuncture for migraine: 40 cases. Nei Mongol J. Tradit. Chin. Med. 33, 34–35. 10.16040/j.cnki.cn15-1101.2014.13.025 [DOI] [Google Scholar]
- Zhang X. (2009). Observation on the Penetration Acupuncture at the Head Acupoint of ShaoYang Meridian to Treat Migraine. [M. Medicine]. Guangzhou: Guangzhou University of Chinese Medicine. [Google Scholar]
- Zhang X. (2016). Clinical Research of Acupuncture Treatment of Vestibular Migraine (Dizzy-Wind Yang Interference). [M. Medicine]. Jilin: Changchun University of Traditional Chinese Medicine. [Google Scholar]
- Zhang Y. (2016). Clinical Study on Warming-unblocking Needling for Migraine of Blood Stasis Type. [M. Medicine]. Lanzhou: Gansu University of Chinese Medicine. [Google Scholar]
- Zhang Y., Liu H., Wang L. (2008). Evaluation of the quality of reports on acupuncture for migraine prophylaxis. Chin. J. Evid. Based Med. 6, 461–465. 10.3969/j.issn.1672-2531.2008.06.024 [DOI] [Google Scholar]
- Zhang Z. (2014). The Clinical Research of Migraine Treated by Acupuncture in Special Points of Shaoyang Meridian. Ph. D. thesis. Guangzhou: Guangzhou University of Chinese Medicine. [Google Scholar]
- Zhao D. (2014a). System Evaluation and Regularity of Selected acupoint about Electro-acupuncture Treatment on Migraine. [M. Medicine]. Jinan: Shandong University of Traditional Chinese Medicine. [Google Scholar]
- Zhao D. (2014b). Treatment of Migraine without Aura by Penetration Acupuncture at the Acupoint of Shaoyang Meridian. [M. Medicine]. Beijing: Beijing University of Chinese Medicine. [Google Scholar]
- Zhao L. (2011). Functional Connectivity Network involved in Acupuncture Along Meridians Based on fMRI Study. Ph.D. thesis, Chengdu: Chengdu University of TCM. [Google Scholar]
- Zhao Y. (2016). Dataming and Systematic review of Modern Acupuncture Treatment for Menstrual Migraine. [M. Medicine]. Chengdu: Chengdu University of Traditional Chinese Medicine. [Google Scholar]
- Zheng C. (2016). Through Clinical Observation of Acupoint Needle Head with Shaoyang Meridian in Treatment of Chronic Migraine. [M. Medicine]. Harbin: Heilongjiang University of Traditional Chinese Medicien. [Google Scholar]
- Zheng S., Cui H. (2012). Acupuncture for migraine:a meta analysis. Chin J Inf Tradit Chin Med.19, 20–23. 10.3969/j.issn.1005-5304.2012.06.009 [DOI] [Google Scholar]
- Zheng S., Wu Y., Jiao J., Wei L., Xu M., Lian J., et al. (2013). Clinical efficacy of Chifeng Yingyuan manipulation for migraine and its effects on endothelin and nitric oxide. World J. Acupunct. Moxibustion. 29, 45–48. 10.3969/j.issn.1005-0779.2013.06.018 [DOI] [Google Scholar]
- Zhou Z. (2017). Clinical research on chronic migraine treated by nourishing liver and kidney acupuncture therapy. Si Chuan Zhong Yi. 35, 204–206. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.