Abstract
Moyamoya disease (MMD) is a chronic progressive, occlusive cerebrovascular disease in the circle of Willis and the feeding arteries. Morning glory disc anomaly (MGDA) is characterized by an abnormal excavated optic disc with radial emergence of blood vessels from the rim of the disc. We describe a case of moyamoya syndrome (MMS), a rare entity among Indian ethnicity, associated with MGDA and regressed facial capillary hemangiomas, which are relatively less reported presentations of MMD. This report emphasizes on the role of neuroimaging in MGDA, so as to facilitate early detection and management of life-threatening intracranial pathologies such as MMS.
Keywords: Hemangioma, Indian ethnicity, morning glory anomaly, moyamoya, ocular manifestations
Moyamoya (MMD) is an occlusive cerebrovascular disease, rare in Indian population. We describe the association of Morning glory disc anomaly (MGDA) and regressed facial hemangiomas in a 16 year old female with MMD. This report stresses on the importance of brain imaging in cases with MGDA, which may be critical in the early management of life threatening neurological problems like MMD.
Case Report
A 16-year-old girl of Indian ethnicity presented with defective vision of left eye (LE), noticed 3 years ago. She was diagnosed of moyamoya disease (MMD) following evaluation for sudden weakness of the right side of the body and had undergone encephalo-duro-angio-synangiosis (EDAS) in 2012. In 2013, she was diagnosed of compromised blood flow to the left side of the body and underwent EDAS.
She was the second of an uneventful twin pregnancy; she had significant delay in milestones and poor scholastic performance at school. Her twin brother does not have any significant medical illness.
Examination showed scars of regressed capillary hemangiomas over the lips [Fig. 1]. Higher mental functions were normal. Gait was abnormal with grade 3 power of all the four limbs. Cardiovascular and respiratory systems were within normal limits.
Figure 1.

Clinical photograph showing regressed hemangiomas over the lips and chin
On ocular examination, best-corrected visual acuity of the right eye (RE) was 6/6 and that of the LE was 1/60. Retinoscopy of LE showed −16 D of myopia. Slit lamp examination was normal; there were no abnormal vessels over the iris. Pupillary reactions were normal; there was no afferent pupillary defect. Goniscopy showed open angles and no vascular abnormalities in the angle. Intraocular pressure was 16 mm Hg in both eyes.
Fundus examination of LE revealed large optic disc with a central core of whitish glial tissue, with the blood vessels emerging from the rim of the optic disc in a radial pattern, suggestive of morning glory disc anomaly (MGDA), with peripapillary chorioretinal pigmentary disturbances. Macula was normal, and background retina was tessellated [Fig. 2]. Dilated fundus examination was normal in the RE. There was no arteriolar constriction, venous dilation, or mid peripheral hemorrhages.
Figure 2.
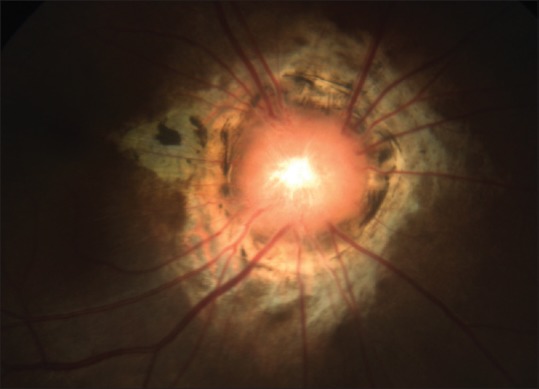
Fundus photograph of the left eye showing the large optic disc with a central core of whitish glial tissue, with the blood vessels emerging from the rim of the optic disc in a radial pattern, suggestive of morning glory disc anomaly, with peripapillary chorioretinal pigmentary disturbances
Diagnosis was: Left eye: Morning Glory Disc Anomaly, high myopia, with anisometropic amblyopia; moyamoya syndrome (MMS), post EDAS.
Magnetic Resonance angiogram (MRA) of the brain showed multiple flow voids in the basal ganglia on both sides with bright sulci (leptomeningio-ivy sign), curvilinear filling defects in the ambient cistern, with severe stenosis of left Internal Carotid artery (ICA), and multiple enlarged collateral lenticulostriate vessels, consistent with moyamoya vessels [Fig. 3]. The right subclavian artery had an aberrant origin, directly from the arch of aorta. Cervical branch of right ICA showed anastomosis with the right basilar artery. Anastomotic branches were also present between right superficial temporal artery and right middle cerebral artery (MCA).
Figure 3.
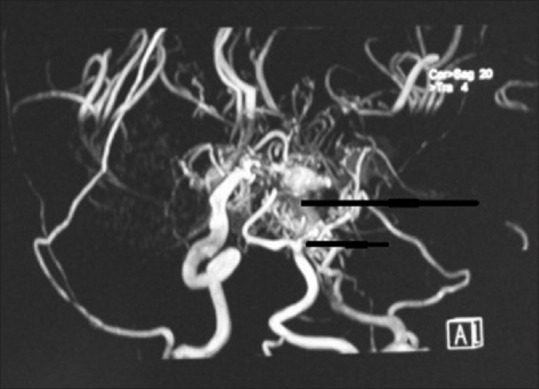
Magnetic resonance angiogram showing multiple enlarged collateral lenticulostriate vessels (long arrow mark) and severe stenosis of left ICA (short arrow mark), consistent with moyamoya vessels
Complete blood count, erythrocyte sedimentation rate, random blood sugar, C-reactive protein, antinuclear antibody titers, and coagulation profile were normal. Chest X-ray, echocardiography, and ultrasonogram of the abdomen were unremarkable.
Discussion
MMD is a chronic progressive, occlusive cerebrovascular disease involving the circle of Willis and the feeder arteries. “Moyamoya” (Japanese word meaning “puff of smoke in the air”) is the term used to describe the smoky angiographic appearance of the vascular collateral network that develops adjacent to the stenotic intracranial vessels.[1] Japan has the highest prevalence of MMD (3.16 cases per 100,000).[1] MMD is an idiopathic disorder with female predominance.
Clinical manifestations of MMD include transient ischemic attacks, ischemic stroke, hemorrhagic stroke, and epilepsy in adults. Children may have hemiparesis, monoparesis, sensory impairment, involuntary movements, headaches, dizziness, seizures, mental retardation, persistent neurologic deficits, and so on. MMS refers to moyamoya angiopathy associated with other neurological or extraneurological symptoms, or due to a well-identified acquired or inherited cause.
Ocular manifestations of MMD are rare. Central retinal artery occlusion,[2] central retinal vein occlusion,[3] and anterior ischemic optic neuropathy[4] have been reported in adults. MMD is also associated with optic nerve hypoplasia and chorioretinal coloboma.[5]
MGDA is a congenital, usually unilateral condition characterized by an abnormal optic disc with central core of whitish glial tissue of persistent hyaloid remnants within the base and with the blood vessels emerging from the rim of the disc in a radial pattern. MGDA is generally attributed to mesoectodermal dysgenesis and the failure of closure of embryonic fissure leading to defective formation of posterior part of sclera.
The vascular abnormalities in MMD usually predominate in the anterior artery and MCA, and the posterior cerebral artery could be involved later. Our patient had abnormal communications between the anterior circulation and the basilar and vertebral arteries and definite involvement of the posterior circulation also. She also had intellectual disability, attributed to the deleterious effect of chronic cerebral hypoxia in MMD.[6]
Hanson et al.[7] have described MGDA associated with multiple facial hemangiomas in MMD. Massaro et al.[8] have described a patient with MCA occlusion and moyamoya vessels associated with MGDA on the same side. Bakri et al.[5] and Krishnan et al.[9] have reported association of MGDA, choroidal coloboma, and MMD. Holmström and Taylor[10] speculated that the association of extensive capillary hemangiomas and MGDA could be attributed to the common timing of the faulty mesectodermal dysgenesis during the first trimester.
This case confirms the association of MMS with MGDA. In contrast to all the previous cases with unilateral MMD and MGDA, our patient had bilateral moyamoya vessels and facial hemangiomas along with a normal optic disc in the fellow eye.
MMS is a rare disease in Indian ethnicity, and association with MGDA and facial hemangiomas is relatively less reported. It is important that ophthalmologists be aware of these rare associations of MGDA, as the patient may be initially presenting to the ophthalmologist for evaluation of defective vision.
The association of MGDA with intracranial vascular anomalies has probably not received adequate recognition in literature, as brain imaging is not routinely done in MGDA. We recommend neuroimaging in all patients with MGDA so as to rule out brain anomalies. The recognition of vascular abnormalities may be critical in the early management of life-threatening neurological problems associated with MMD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kim JS. Moyamoya disease: Epidemiology, clinical features, and diagnosis. J Stroke. 2016;18:2–11. doi: 10.5853/jos.2015.01627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar MA, Ganesh BA. CRAO in moyamoya disease. J Clin Diagn Res. 2013;7:545–7. doi: 10.7860/JCDR/2013/4579.2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slamovits TL, Klingele TG, Burde RM, Gado MH. Moyamoya disease with central retinal vein occlusion. Case report. J Clin Neuroophthalmol. 1981;1:123–7. [PubMed] [Google Scholar]
- 4.Chen CS, Lee AW, Kelman S, Wityk R. Anterior ischemic optic neuropathy in moyamoya disease: A first case report. Eur J Neurol. 2007;14:823–5. doi: 10.1111/j.1468-1331.2007.01819.x. [DOI] [PubMed] [Google Scholar]
- 5.Bakri SJ, Siker D, Masaryk T, Luciano MG, Traboulsi EI. Ocular malformations, moyamoya disease, and midline cranial defects: A distinct syndrome. Am J Ophthalmol. 1999;127:356–7. doi: 10.1016/s0002-9394(98)00317-1. [DOI] [PubMed] [Google Scholar]
- 6.Kossorotoff M. Cognitive decline in moyamoya: Influence of chronic cerebral hypoxia, history of stroke, or comorbid conditions? Dev Med Child Neurol. 2012;54:5–6. doi: 10.1111/j.1469-8749.2011.04159.x. [DOI] [PubMed] [Google Scholar]
- 7.Hanson MR, Price RL, Rothner AD, Tomsak RL. Developmental anomalies of the optic disc and carotid circulation. A new association. J Clin Neuroophthalmol. 1985;5:3–8. [PubMed] [Google Scholar]
- 8.Massaro M, Thorarensen O, Liu GT, Maguire AM, Zimmerman RA, Brodsky MC, et al. Morning glory disc anomaly and moyamoya vessels. Arch Ophthalmol. 1998;116:253–4. [PubMed] [Google Scholar]
- 9.Krishnan C, Roy A, Traboulsi E. Morning glory disk anomaly, choroidal coloboma, and congenital constrictive malformations of the internal carotid arteries (moyamoya disease) Ophthalmic Genet. 2000;21:21–4. [PubMed] [Google Scholar]
- 10.Holmström G, Taylor D. Capillary haemangiomas in association with morning glory disc anomaly. Acta Ophthalmol Scand. 1998;76:613–6. doi: 10.1034/j.1600-0420.1998.760521.x. [DOI] [PubMed] [Google Scholar]


