Abstract
Purpose:
To evaluate the relationship between tear meniscus height (TMH) values measured by optical coherence tomography (OCT) and the severity of epiphora (Munk scoring).
Methods:
In this prospective cross-sectional study, consecutive patients with epiphora were studied. All patients underwent Munk epiphora scoring, lacrimal syringing, and detailed ophthalmological examination. Using OCT, the TMH (i.e., the line intersecting level of tear meniscus and lower eyelid) values were calculated. The relationship between TMH and epiphora was analyzed by comparing TMH values across various grades of epiphora using Kruskal–Wallis test.
Results:
A total of 38 patients (56 eyes) were included. The mean age was 55 ± 11.1 years with equal distribution of males and females. The mean TMH values were 238 ± 141.3, 396.6 ± 159.5, 707.1 ± 288.8, and 809.5 ± 419.4 μm in grades 1, 2, 3, and 4 of epiphora, respectively. A significant difference in TMH was found among grades 2, 3, and 4 (P = 0.0007). On post hoc analysis, only grade 2 was significantly different from grades 3 and 4 (P = 0.0008 and P = 0.002 respectively), but grades 3 and 4 were comparable (P = 0.62).
Conclusion:
Levels of TMH were found to increase with increasing severity of epiphora. TMH values were comparable in Munk grades 3 and 4.
Keywords: Epiphora, lacrimal, optical coherence tomography, tear film height
Epiphora constitutes one of the commonest presenting complaints to an ophthalmologist's practice. Several tests have been described for evaluation of lacrimal drainage pathways such as irrigation, probing, and dacryocystography.[1] Over the years, qualitative assessment of epiphora has been performed with Munk scoring system.[2] Physiological tests such as fluorescein dye disappearance test (FDDT), Jones test, and dacryoscintigraphy have been used as objective indicators of the lacrimal drainage pathways and to define the outcomes of dacryocystorhinostomy.[1,3,4,5] Tear meniscus height (TMH) measurements have been proposed as a diagnostic indicator of nasolacrimal duct obstruction (NLDO) and successful dacryocystorhinostomy.[3,4,5,6] It is not known whether TMH levels truly reflect patient's symptomatology. To the best of our knowledge, a quantitative analysis of the relationship between TMH levels and epiphora grading has not been performed before. This study aims to evaluate the relationship between Munk score and TMH levels [measured with spectral domainoptical coherence tomography (SD-OCT)] irrespective of the underlying etiology.
Methods
Institutional review board approval was obtained and the study adhered to the tenets of the Declaration of Helsinki. A prospective case series study was performed of the patients seen for complaints of chronic epiphora (>3 months) at the oculoplastics services at a tertiary eye care center. The purpose and study design were explained to all the subjects and written consents were obtained. Consecutive patients presenting with chronic epiphora (>3 months duration) to our oculoplastics department were included as the study subjects. Patients with artificial eyes, history of any lacrimal surgery or ocular surface procedures, inferior corneal scarring, eyelid malpositions, ocular surface disease, thyroid eye disease, and unwilling to consent were excluded. All subjects underwent routine ophthalmologic examination by a single examiner, including visual acuity testing, slit-lamp biomicroscopy especially focusing on punctal size and its position, position of plica and caruncle, noncontact intraocular pressure measurement, and posterior segment evaluation.
Epiphora evaluation
Munk's scoring system was used to grade epiphora [Table 1]. All subjects were subjected to syringing through upper punctum in both the eyes. Syringing through lower canaliculus was performed in cases with upper punctal/canalicular obstruction. Schirmer's I test without anesthesia was performed to rule out reflex epiphora associated with dry eyes. Detailed ocular surface evaluation in the form of fluorescein staining and tear break-up time was performed by a trained cornea specialist especially in cases with patent irrigation. FDDT was performed in cases with patent irrigation to differentiate between lacrimal drainage abnormality from ocular surface disease.
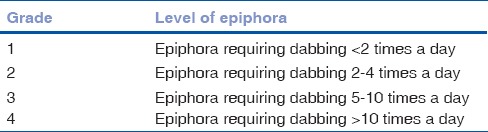
Table 1.
Modified Munk's scoring system for epiphora
Tear meniscus height
A certified technician who was masked to clinical details of the patient performed OCT measurements. SD-OCT-based Cirrus® HD-OCT (Carl Zeiss Meditec, Dublin, CA, USA) with an axial resolution of 7 μm was used. A high-resolution corneal scan protocol with a line scan of 10 mm length and a penetration depth of 3 mm was used. Room temperature and humidity were maintained between 22° and 25°C and 50% and 60%, respectively. No eye drops were used for at least 1 h before OCT imaging. Subjects were asked to rest their foreheads against the headrest with their chins placed on the chin-rest and to gaze at the built-in target and blink normally. Image with a scan quality of more than 7 was captured. A built-in caliper was used to measure TMH levels inferiorly at 6′O clock. The line connecting the point at which the meniscus intersected with the cornea (superiorly) and eyelid (inferiorly) was measured as TMH [Fig. 1].
Figure 1.
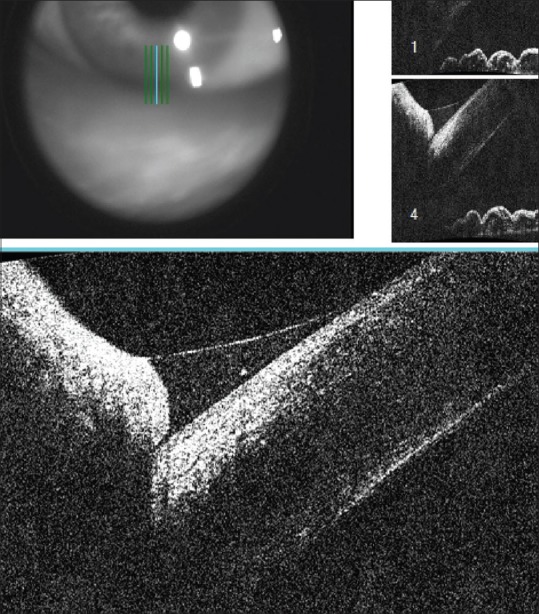
Tear meniscus seen on anterior segment optical coherence tomography (line intersecting ocular surface and lower eyelid)
Statistical analysis was performed using the software Origin v7.0 (OriginLab Corporation, Northampton, MA, USA). Continuous data were checked for normality using Shapiro–Wilk test and were described by means and standard deviation (normal distribution). Categorical data were described by proportions. The equality of variance among continuous data was assessed by Levene test. Kruskal–Wallis test was applied to compare the TMH levels among the various grades of epiphora. A P value <0.05 was considered statistically significant. Post hoc analysis was performed by Mann–Whitney test with the level of significance of P value (0.025) adjusted for Bonferroni correction. Rank-order correlation was performed to check whether there is a relationship between age and TMH.
Results
A total of 38 patients (56 eyes) were included in the study. The mean age of the subjects was 55 ± 11.1 years (range, 29–80 years). There was an equal distribution of males and females. Eighteen patients (47.4%) had bilateral involvement; only right eye was involved in 15 patients (39.4%) and only left eye in 5 patients (13.2%).
The eyes were divided into four groups according to Munk's grading of epiphora. Three eyes had grade 1 Munk score (5.4%), 17 had grade 2 (30.3%), 22 had grade 3 (39.3%), and 14 had grade 4 epiphora (25%). Schirmer's I test was within the normal range in all eyes (mean of 14 ± 3 mm). A total of 37 eyes had patent syringing (66.1%), 7 eyes had both upper and lower proximal canalicular obstruction (12.5%), 6 eyes had punctal stenosis grade 2 (14.3%), and 6 eyes had NLDO (7.1%). These 37 eyes were categorized as functional epiphora owing to patent syringing with delayed FDDT more than grade 2 (grade 3 in 26 eyes; grade 4 in 11 eyes) and absent eyelid or ocular surface abnormalities. The mean TMH according to the underlying diagnosis was 894 μm for NLDO, 824 μm for punctal stenosis, 790 μm for proximal canalicular obstruction, and 503 μm for functional epiphora.
The mean TMH in grade 1 epiphora was 238 ± 141.3 μm [range, 106–387 μm and 95% confidence intervals (CI), 113–589 μm], 396.6 ± 159.5 μm in grade 2 (range, 115–813 μm and 95% CI, 314.6–478.6 μm), 707.1 ± 288.8 μm in grade 3 (range, 211–1197 μm and 95% CI, 579.1–835.2 μm), and 809.5 ± 419.4 μm in grade 4 (range, 275–1720 μm and 95% CI, 567.4–1051.7 μm). Distribution of TMH across various grades is shown in bar diagram [Fig. 2]. Since only three eyes had grade 1 epiphora, they were excluded from statistical analysis of relationship between TMH and grades of epiphora. A significant difference in the TMH values was found between grades 2, 3, and 4 of epiphora (P = 0.0007). Post hoc analysis revealed that only grade 2 was significantly different from grades 3 and 4 (P = 0.0008 and P = 0.002, respectively); but grades 3 and 4 were comparable (P = 0.62). There was no relationship between age and TMH values (P = 0.17).
Figure 2.
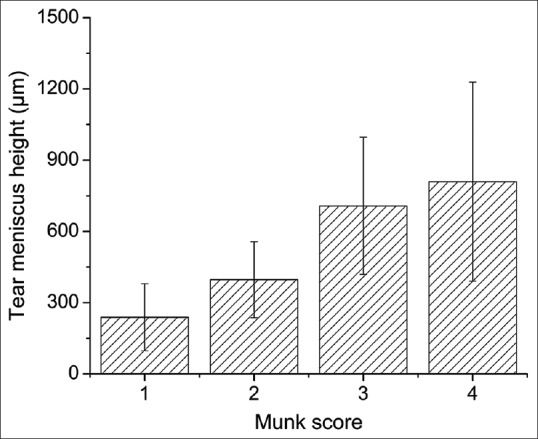
Bar diagram showing distribution of tear meniscus height across various grades of epiphora
Discussion
In this study, increasing levels of TMH were observed with increasing severity of epiphora. Increased TMH levels in Munk grades 1 and 2 turned out to be significantly different from higher grades 3 and 4. However, TMH readings were comparable in Munk grades 3 and 4.
Assessment of TMH was introduced as complementary to the existing evaluation techniques such as Jones, irrigation, and imaging tests. Increased TMH levels were reported as an accurate diagnostic indicator of NLDO in a retrospective study of 62 patients. However, only patients with epiphora due to NLDO alone were included.[4] Its role was further evaluated in another series of NLDO by Roh and Chi. Assessment of the efficacy of FDDT, TMH, and tear symptom score in diagnosis and postoperative assessment of NLDO revealed significantly elevated values among NLDO patients compared with control group.[3] These values decreased significantly post-dacryocystorhinostomy. Tear symptom score had a good correlation with TMH levels. However, the mean tear symptom score was 4.2 ± 0.4 (out of 5), which points toward the inclusion of only severe cases. This study differs from the previous ones by including a whole spectrum of epiphora irrespective of irrigation status. Increasing TMH levels with epiphora severity point toward it being a useful indicator of lacrimal drainage disorders. This test is easy to perform and reproducible. However, its application in assessing or following up epiphora patients is limited, since higher grades can show similar levels of TMH. We do not intend to say that the management of epiphora will depend on TMH levels.
TMH measurement using anterior segment OCT does not involve application of fluorescein contrary to videomeniscometer where tear volume gets altered with fluorescein drop instillation.[6,7] Most of the published studies have used video dacryomeniscometry for TMH measurements in epiphora evaluation.[3,4] The mean TMH in patients with NLDO was 894 μm in this study, which is more compared with previously reported values (530 μm).[3] The technique of video dacryomeniscometry requires image capturing with slit-lamp photography and then TMH is calculated with the help of Adobe Photoshop software manually and proportionately converted to its real value. The OCT machine has inbuilt software for calculating the TMH. The differences in measurement techniques might be responsible for the difference in TMH values observed between this study and readings documented in previous studies.
We have used Munk grading system to denote severity of epiphora. This grading system depends on patient's reporting of frequency of dabbing in a day. We found similar levels of TMH in higher grades of epiphora, thereby reflecting on the existing lacunae in epiphora grading. Unfortunately, a robust grading system does not exist for epiphora.
Conclusion
TMH measurements appear to increase with the increasing patient-reported Munk's scores for epiphora. However, TMH levels may not play a major role in differentiating higher grades of epiphora (Munk grades 3 and 4), and finding its position and niche is more complex as it will always be only part of the assessment of epiphora.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Guzek JP, Ching AS, Hoang TA, Dure-Smith P, Llaurado JG, Yau DC, et al. Clinical and radiologic lacrimal testing in patients with epiphora. Ophthalmology. 1997;104:1875–81. doi: 10.1016/s0161-6420(97)30013-x. [DOI] [PubMed] [Google Scholar]
- 2.Munk PL, Lin DT, Morris DC. Epiphora: Treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology. 1990;177:687–90. doi: 10.1148/radiology.177.3.2243969. [DOI] [PubMed] [Google Scholar]
- 3.Roh JH, Chi MJ. Efficacy of dye disappearance test and tear meniscus height in diagnosis and postoperative assessment of nasolacrimal duct obstruction. Acta Ophthalmol. 2010;88:e73–7. doi: 10.1111/j.1755-3768.2010.01873.x. [DOI] [PubMed] [Google Scholar]
- 4.Burkat CN, Lucarelli MJ. Tear meniscus level as an indicator of nasolacrimal obstruction. Ophthalmology. 2005;112:344–8. doi: 10.1016/j.ophtha.2004.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Kim SE, Lee SJ, Lee SY, Yoon JS. Outcomes of 4-snip punctoplasty for severe punctal stenosis: Measurement of tear meniscus height by optical coherence tomography. Am J Ophthalmol. 2012;153:769–73. doi: 10.1016/j.ajo.2011.09.026. 773.e1-2. [DOI] [PubMed] [Google Scholar]
- 6.Stahl U, Francis IC, Stapleton F. Prospective controlled study of vapor pressure tear osmolality and tear meniscus height in nasolacrimal duct obstruction. Am J Ophthalmol. 2006;141:1051–6. doi: 10.1016/j.ajo.2005.12.051. [DOI] [PubMed] [Google Scholar]
- 7.Savini G, Barboni P, Zanini M. Tear meniscus evaluation by optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2006;37:112–8. [PubMed] [Google Scholar]


