Abstract
Purpose:
To determine the role of primary limbal stem cell transplantation (LSCT) in managing extensive ocular surface squamous neoplasia (OSSN) with more than 3 quadrants of limbal involvement to prevent manifestations of limbal stem cell deficiency.
Methods:
A multi-center, comparative, and interventional clinical study of cases and historical controls was done. Patients with a limbal mass suggestive of OSSN involving more than 3 quadrants of limbus (> 9 clock hours) and no local, regional or systemic metastasis, who underwent primary surgical excision with or without adjuvant chemotherapy and had a minimum follow-up of 12 months were included in this study. Two historical controls underwent tumor excision with only amniotic membrane grafting. Three cases underwent tumor excision along with LSCT in the form of conjunctival limbal autograft (CLAG) or simple limbal epithelial transplant (SLET).
Results:
None of the eyes had any recurrences of OSSN during the follow-up period. Cases with primary LSCT with tumor excision showed better ocular surface stability in the long term.
Conclusion:
Concomitant LSCT either in the form of CLAG or SLET appears to provide better long-term outcomes and is advocated while excision of extensive OSSN involving the limbus.
Keywords: Conjunctival limbal autograft, limbal stem cell deficiency, limbal stem cell transplantation, ocular surface squamous neoplasia, simple limbal epithelial transplantation
Ocular surface squamous neoplasia (OSSN) refers to a broad spectrum of neoplastic squamous epithelial abnormalities, including squamous dysplasia, conjunctival intraepithelial neoplasia, and invasive squamous cell carcinoma (SCC).[1] Ever since Von Graefe first reported these tumors in 1860, the terminology used to identify them has been evolving and so have their management strategies such as surgical excision, topical chemotherapy, immunotherapy, and plaque or external beam radiotherapy or extended enucleation or orbital exenteration for advanced cases. Complete tumor freedom, prevention of any recurrence or metastasis, and maintaining a good ocular surface are the goals of treatment of OSSN. Wide excision of the tumor with 4 mm clear margin for conjunctival extension, alcohol keratoepitheliectomy with 2 mm clear corneo-limbal margins, and adjuvant cryotherapy (double freeze-thaw cycles) followed by ocular surface reconstruction using amniotic membrane or conjunctival graft remains the mainstay for invasive OSSN management.[2] This treatment protocol results in excellent outcomes when performed for smaller lesions. However, in large tumors with extensive involvement of the limbus and cornea, reconstruction of large excised areas often results in significant loss of limbal stem cells. For ensuring a good functional and cosmetic result, several surgical techniques being used for ocular surface reconstruction are amniotic membrane transplantation (AMT) with or without conjunctivo-limbal autografts (CLAG), oral mucosal transplantation or limbal stem cell transplantation (LSCT) in the form of kerato-limbal autografting, ex-vivo cultivated limbal epithelial transplantation (CLET), and more recently, simple limbal epithelial transplantation (SLET).
Methods
This was a multi-center, comparative, and interventional clinical study of 5 cases and historical controls performed at Cornea and Anterior Segment services and Ocular oncology services of 3 centers from January 2009 to June 2015. The study adhered to the tenets of Declaration of Helsinki and was approved by the appropriate institutional review boards. A written and informed consent was obtained from all patients for all the surgical procedures, photo documentation, and investigations. Patients with a limbal mass suggestive of OSSN involving more than 3 quadrants of limbus (> 9 clock hours), who underwent primary surgical excision with or without adjuvant chemotherapy and had a minimum follow-up of 12 months were included in this study. The diagnosis of OSSN was depending on clinical features. Systemic examination was performed to look for any signs of loco-regional or systemic metastasis. Patients with previous history of OSSN occurrence, immune-compromise, or xeroderma pigmentosum were excluded from the study.
Data Collection: The demographic and clinical data were collected in a predesigned form that included the age and gender of the patient, any systemic disease, duration of the limbal mass prior to presentation, morphologic variant of tumor, quadrantic location and extent over cornea, limbus or conjunctiva, number of clock hours of limbal involvement and any regional lymph node involvement, type of surgical intervention, clinical condition after surgery especially the signs of limbal stem cell deficiency (LSCD) (absence of the limbal palisades of Vogt, dull and irregular corneal epithelium, superficial corneal vascularization, persistent epithelial defects, and conjunctival overgrowth on the corneal surface such as pannus, symblepharon, or pseudopterygium)[3] the time and extent of their occurrence, pre- and post-operative best corrected visual acuity (BCVA), and the histopathological findings.
Surgical Technique: The surgeries were performed under peribulbar anesthesia. All patients underwent extended tumor excision along with double freeze thaw cryotherapy and amniotic membrane graft (AMG). The limbal tumors were excised along with a 4 mm zone of clinically clear conjunctiva around the tumor using the “No touch technique” as described by Shields et al.[2] Absolute alcohol was used to loosen the epithelium of cornea adjacent to the mass, and the corneal component of the mass was then gently lifted up along the sub-epithelial plane thus created along with 2 mm of clinically tumor-free corneal epithelium. Free edges of the excised conjunctiva and the involved limbus were then treated with cryotherapy with two freeze-thaw cycles. Bare sclera was covered with preserved human AMG, secured with fibrin glue (Tisseel Kit, Baxter AG, Vienna, Austria). Patients 1 and 2 were treated with the above mentioned technique only. Three patients underwent simultaneous LSCT. Patients 3 and 4 also received a standard CLAG from the contralateral healthy eye and were glued onto the entire bare sclera and limbus with proper orientation, prior to the AMT. Patient 5 underwent simple limbal epithelial stem cell transplant or SLET after excision of the tumor as described above. The surgical technique was similar to one described by Sangwan et al.[4] and Mittal et al.[5] In brief, it had the following steps: A 3×2 mm size limbal biopsy was harvested from the contra-lateral healthy donor eye from the superior limbus prior to limbal mass excision. Sub-conjunctival dissection was continued until the limbus followed by a shallow dissection 1 mm into the clear cornea. The excess conjunctiva was reposited and sealed with fibrin glue. This limbal tissue was excised and kept in balanced salt solution. After tumor tissue was excised, the bleeding vessels were cauterized, and AMG was placed over the bare ocular surface and sealed with fibrin glue. Donor tissue was cut into multiple small pieces, (limbal transplants), with either Vannas scissors (Joja Surgicals, Kolkata, India). Limbal transplants were then uniformly distributed on the AMG leaving a clear visual axis and were held in place with fibrin glue. A correct orientation of lenticules, epithelial side up, was maintained, and it was ensured that the explants covered all quadrants. At the end of the surgery, a soft bandage contact lens (BCL) was placed over the cornea. The recipient eye was patched overnight.
Postoperative management and Follow-up: Topical prednisolone acetate 1% 6 times a day was started in the donor eye the same day after surgery and in the recipient eye from the following day. It was tapered over 4 weeks in the healthy donor eye (in cases 3, 4, and 5) and up to 3 months in the diseased eye depending upon the ocular surface inflammation. Topical moxifloxacin 0.5% was used 4 times a day until the ocular surface epithelialized in both eyes, usually for a week in the donor and 2 weeks in the diseased eye. Preservative free lubricants were used in both eyes of all cases. The BCL was left in situ for 6 weeks. Postoperative medications for controls included topical antibiotics for 2 weeks and tapering dose of topical steroids over 6 weeks. BCL was removed after 1 week. All patients were seen on postoperative day 1, weekly in first month, then monthly for 3 months, and then every 3 months till last follow-up. Presence or absence of LSCD after tumor control was the primary outcome measure.
Results
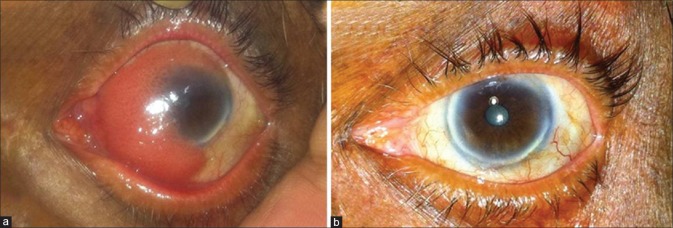
Five eyes of five patients fulfilled the inclusion criteria. The patient details and results are summarized in Table 1. The median age was 62.8 years (range 26–80 years). All patients were males. The tumor features in the form of clock hours of involvement and mean basal dimensions were comparable for both groups. Mean follow-up was 90 months (8 and 7 years) for the non LSCT group and 50 months (62, 57, and 31 months) for the LSCT group.
Table 1.
Demographic and clinical data of patients with limbal mass
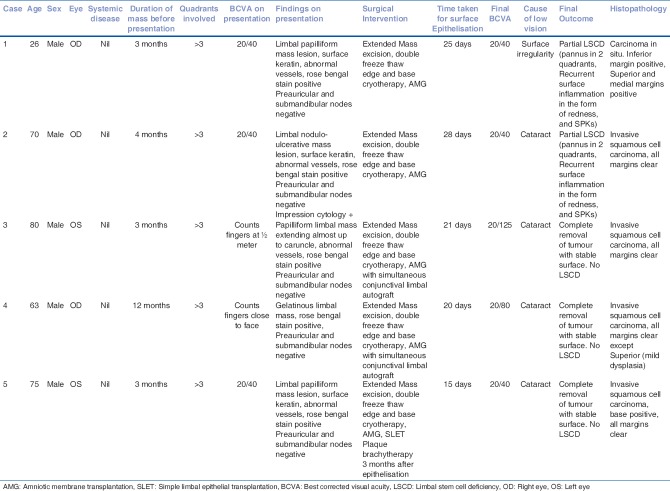
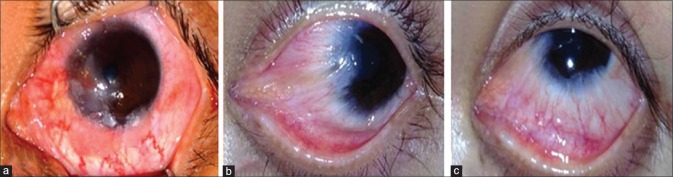
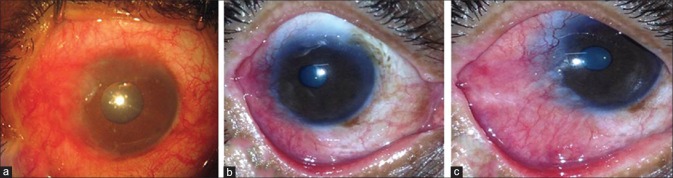
Three out of five patients underwent limbal epithelial cell transplant along with primary tumor excision. The first two patients during the early period of this study [Figs. 1a and 2a] underwent surgery for tumor control and AMG only. The average time taken for surface re-epithelialization in the first 2 cases was 26.5 days; whereas the rest of the eyes took an average of 18.67 days to re-epithelialize after either autografting or SLET. None of the patients had any regional lymphatic or systemic metastasis at the time of presentation. We observed that both patients in whom no additional intervention was done to restore limbal stem cells developed signs of partial LSCD as evidenced by pseudo-pterygium or pannus formation in at least 2 quadrants within the first year of surgery [Figs. 1b, c and 2b, c]. There were recurrent episodes of ocular surface inflammation and superficial punctate keratopathy (SPKs) causing frequent redness, watering, foreign body sensation in both these patients, which were managed medically. In contrast, patients 3, 4, and 5 in whom either CLAG [Fig. 3a and b] or SLET[5] was done showed a much more stable ocular surface. The recovery was faster, and patients were more comfortable postoperatively. None of these patients developed any sign of local recurrence or loco-regional or systemic metastasis till the last follow-up. Histopathology revealed carcinoma in situ in one eye and invasive SCC with base negative for tumor in 3 cases [Table 1]. One of the cases which underwent LSCT in the form of SLET has been reported elsewhere[5], and anticipating chemoreduction before surgery, 1 cycle of mitomycin C 0.04% (4 times a day, 4 days a week for 3 weeks with 1 week off) was given to this patient. However, it was discontinued because of the patient's intolerance and as no change in the size or thickness of tumor was noticed. As the histopathology report showed invasive SCC with cords and nests of tumor cells infiltrating the base, this patient received plaque brachytherapy after 3 months and did not show any LSCD later on.[5] The first 2 patients who had developed LSCD will be undergoing LSCT in the form of a secondary SLET for surface stabilization.
Figure 1.
(a) Preoperative clinical pictures of ocular surface squamous neoplasia in patient 1 (historical control) involving more than 3 quadrants of limbal area; (b and c) postoperative clinical pictures showing scarring and limbal stem cell deficiency manifesting in the form of pseudopterygium at last follow-up visit
Figure 2.
(a) Preoperative clinical picture of ocular surface squamous neoplasia in patient 2 (historical control) involving more than 3 quadrants of limbal area; (b and c) postoperative clinical pictures showing scarring and limbal stem cell deficiency manifesting in the form of pannus at last follow-up visit
Figure 3.
(a) Preoperative clinical picture of tumor in Patient 3 with more than 3 quadrants of limbal area involvement, who underwent limbal stem cell transplantation in the form of conjunctivo-limbal autografting; (b) postoperative clinical picture showing stable ocular surface and no signs of limbal stem cell deficiency during follow-up
Discussion
In the present communication, we report 2 cases of OSSN with extensive disease, dealt by us during the early course of this study, wherein only AMT was done to restore the ocular surface following tumor excision. These patients continued to suffer from various ill effects of LSCD. This prompted us to look for a better management approach. In this quest, we share our experience with 3 cases of extensive OSSN successfully managed with simultaneous limbal stem cell restoration. We, as separate surgeons from different centers, were consistently able to achieve a stable ocular surface even after extensive limbal tissue loss during excision of very large tumors. The aim of LSCT was to provide a smooth epithelial surface for maintenance of better optical clarity of cornea and to reduce patient morbidity postoperatively. Palamar et al. have studied utility of AMT after surgery for large and multifocal conjunctival tumors and found it an effective modality for surface reconstruction.[6] Asoklis et al. in their series of OSSN (with mean of 4 clock hours of limbal involvement) showed that AMT could suffice for primary surface reconstruction, but signs of LSCD developed in few of the cases.[7] AMT alone may not be enough when dealing with more extensive disease. Advanced corneoscleral limbal spread of OSSN can lead to destruction of the epithelial stem cells that reside in limbal palisades of Vogt. OSSN itself has been reported as a rare cause of LSCD.[8] Wide surgical excision is often undertaken in these cases, as the treatment of choice for invasive SCC of conjunctiva. This has a deleterious impact on the survival of stem cells in the involved region, resulting in large conjunctival and often corneal epithelial defects. Many reports substantiate the prevalence of LSCD following wide tumor excision, leading to performance of secondary procedures to restore the limbal stem cells.[9,10] In anticipation of total LSCD following the surgical removal of such large tumors where sufficient uninvolved margins have been taken and free edges treated with adjuvant cryotherapy, one may consider performing LSCT in the same sitting. This would avoid additional procedures later (with probably lesser effective outcomes), thus decreasing the overall morbidity while managing these patients. Various techniques have been described to establish a new source of limbal stem cells. In unilateral cases, the other eye can serve as a donor.[9,10,11] Lyall et al. have reported successful outcome of conjunctival autograft coupled with surgical tumor excision in one patient with extensive OSSN.[8] A novel technique of restoring limbal stem cell niche, namely SLET, has proven to be very effective. Apart from avoidance of additional procedures, an autograft or SLET also have the added advantage of not requiring systemic immunosuppression. None of these cases showed any sign of LSCD at the end of follow-up, and all the patients were tumor free with no signs of recurrence locally or systemically. We observed that the LSCT procedures either in the form of CLAG or SLET had been performed at different operative centers by various surgeons for comparable lesions, but the results were similar and repeatable. Hence, as recommended, our study did not suffer any institutional bias. A recent study[12] mentioned that primary SLET was done for all the cases including 2 quadrants of limbal involvement. However, we believe that smaller lesions may not always need extensive LSCT in the form of concomitant SLET or LSCT. Our study included extensively large tumors, and results indicated that LSCT is required as a concomitant procedure along with tumor excision of such extensive lesions.
Limitations of our study are its retrospective nature and a small sample size. OSSN being a rare disease and cases with more than 3 quadrants of limbus involvement being even rarer; a large sample size for the study was not possible. Further, studies on refinements in the techniques of LSCT might help in improving the postoperative outcomes in these patients. The authors believe that restoration of limbal stem cells in an extensive OSSN in the primary setting itself is pertinent to a good outcome in such cases either in the form of CLAG or SLET. However, caution needs to be exercised in cases of OSSN in xeroderma pigmentosum as these tumors are usually bilateral and may affect both the eyes, thereby rendering autografting unadvisable.[13]
Conclusion
To summarize, our study describes the importance of LSCT in any form (either a conjunctival limbal autograft or SLET) in extensive OSSN with more than 3 quadrants of limbal involvement to prevent manifestations of stem cell deficiency. When performed along with the primary tumor excision itself, it seems to be a very promising treatment with reduced postoperative morbidity, leading to faster healing time, better and longer lasting ocular surface stability, and decreased morbidity, particularly in invasive SCC.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kiire CA, Srinivasan S, Karp CL. Ocular surface squamous neoplasia. Int Ophthalmol Clin. 2010;50:35–46. doi: 10.1097/IIO.0b013e3181e246e5. [DOI] [PubMed] [Google Scholar]
- 2.Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors. The 1994 lynn B. McMahan lecture. Arch Ophthalmol. 1997;115:808–15. doi: 10.1001/archopht.1997.01100150810025. [DOI] [PubMed] [Google Scholar]
- 3.Gichuhi S, Ohnuma S, Sagoo MS, Burton MJ. Pathophysiology of ocular surface squamous neoplasia. Exp Eye Res. 2014;129:172–82. doi: 10.1016/j.exer.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sangwan VS, Basu S, MacNeil S, Balasubramanian D. Simple limbal epithelial transplantation (SLET): A novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br J Ophthalmol. 2012;96:931–4. doi: 10.1136/bjophthalmol-2011-301164. [DOI] [PubMed] [Google Scholar]
- 5.Mittal V, Narang P, Menon V, Mittal R, Honavar S. Primary simple limbal epithelial transplantation along with excisional biopsy in the management of extensive ocular surface squamous neoplasia. Cornea. 2016;35:1650–2. doi: 10.1097/ICO.0000000000000953. [DOI] [PubMed] [Google Scholar]
- 6.Palamar M, Kaya E, Egrilmez S, Akalin T, Yagci A. Amniotic membrane transplantation in surgical management of ocular surface squamous neoplasias: Long-term results. Eye (Lond) 2014;28:1131–5. doi: 10.1038/eye.2014.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Asoklis RS, Damijonaityte A, Butkiene L, Makselis A, Petroska D, Pajaujis M, et al. Ocular surface reconstruction using amniotic membrane following excision of conjunctival and limbal tumors. Eur J Ophthalmol. 2011;21:552–8. doi: 10.5301/EJO.2010.6192. [DOI] [PubMed] [Google Scholar]
- 8.Lyall DA, Srinivasan S, Roberts F. Limbal stem cell failure secondary to advanced conjunctival squamous cell carcinoma: A clinicopathological case report. BMJ Case Rep 2009. 2009 doi: 10.1136/bcr.09.2009.2272. pii: bcr09.2009.2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dua HS, Azuara-Blanco A. Autologous limbal transplantation in patients with unilateral corneal stem cell deficiency. Br J Ophthalmol. 2000;84:273–8. doi: 10.1136/bjo.84.3.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Copeland RA, Jr, Char DH. Limbal autograft reconstruction after conjunctival squamous cell carcinoma. Am J Ophthalmol. 1990;110:412–5. doi: 10.1016/s0002-9394(14)77023-0. [DOI] [PubMed] [Google Scholar]
- 11.Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96:709–22. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- 12.Kaliki S, Mohammad FA, Tahiliani P, Sangwan VS. Concomitant simple limbal epithelial transplantation after surgical excision of ocular surface squamous neoplasia. Am J Ophthalmol. 2017;174:68–75. doi: 10.1016/j.ajo.2016.10.021. [DOI] [PubMed] [Google Scholar]
- 13.Gupta N, Sachdev R, Tandon R. Ocular surface squamous neoplasia in xeroderma pigmentosum: Clinical spectrum and outcome. Graefes Arch Clin Exp Ophthalmol. 2011;249:1217–21. doi: 10.1007/s00417-011-1679-8. [DOI] [PubMed] [Google Scholar]