Abstract
Background:
Few studies have investigated the differences in proximal femoral geometry and risk factors between patients with different types of hip fracture, especially in elderly Chinese. This study aimed to assess the differences in proximal femoral geometry parameters between patients with femoral neck fractures and patients with intertrochanteric fractures to provide guidance for individualized customized prosthesis and accurate reconstruction of proximal femurs in elderly Chinese patients.
Methods:
We retrospectively studied the electronic medical records of 198 elderly patients over 65 years of age who were admitted to the orthopedic department with hip fractures between January 2017 and December 2017 in The Third Hospital, Hebei Medical University. Age, fracture site, gender, and proximal femoral geometry parameters (neck shaft angle [NSA], center edge angle [CEA], femoral head diameter [FHD], femoral neck diameter [FND], femoral neck axial length [FNAL], hip axial length [HAL], and femoral shaft diameter [FSD]) were recorded. Student's t-test was used to compare the continuous variables, Chi-square test was used to analyze categorical variables, and multiple logistic stepwise regression analysis was used to evaluate the influencing factors of hip fracture type.
Results:
Statistically significant differences in NSA (137.63 ± 4.56° vs. 132.07 ± 4.17°, t = 1.598, P < 0.001), CEA (37.62 ± 6.77° vs. 43.11 ± 7.09°, t = 5.597, P < 0.001), FND (35.21 ± 3.25 mm vs. 34.09 ± 3.82 mm, t = 2.233, P = 0.027), and FNAL (99.30 ± 7.91 mm vs. 103.58 ± 8.39 mm, t = 3.715, P < 0.001) were found between the femoral neck fracture group and femoral intertrochanteric fracture group. FHD, FND, FSD, HAL, and FNAL were different between sexes (all P < 0.001). The greater NSA was the risk factor for femoral neck fractures (odds ratio [OR]: 0.70, P < 0.001), greater CEA and longer FNAL were risk factors for femoral intertrochanteric fractures (OR: 1.15, 1.17, all P < 0.001), and greater FND was a protective factor for femoral intertrochanteric fractures (OR: 0.74, P < 0.001).
Conclusions:
We demonstrate differences in geometric morphological parameters of the proximal femur in different hip fracture types, as well as an effect of sex. These differences should be considered in the selection of prostheses for fracture internal fixation and hip replacements. These data could help guide the design of individualized customized prostheses and improve the accurate reconstruction of the proximal femur for elderly Chinese hip fracture patients.
Keywords: Chinese Population, Elderly, Femoral Neck Fractures, Hip Geometry, Intertrochanteric Fractures of the Femur, Risk Factor
摘要
背景:
很少有研究调查不同类型的髋部患者股骨近端几何形态参数和危险因素的差异性,尤其是在中国老年人群中开展这种研究十分罕见。本研究旨在探讨股骨颈骨折和股骨转子间骨折患者的股骨近端几何形态参数的差异性,为设计符合国人的个体化定制型假体提供依据,并为股骨近端的精准重建提供指导。
方法:
采用回顾性研究的方法,对河北医科大学第三医院2017年1月到2017年12月间198例老年髋部骨折患者的临床资料进行研究,其中男性44例,女性154例,股骨颈骨折患者101例,股骨转子间骨折患者97例。通过医学图像阅读软件(RadiAnt Dicom Viewer)测量每位患者的颈干角(Neck Shaft Angle, NSA),中心边缘角(Center Edge Angle, CEA),股骨头直径(Femoral Head Diameter, FHD),股骨颈直径(Femoral Neck Diameter, FND),股骨颈轴长(Femoral Neck Axial Length, FNAL),髋轴长(Hip Axial Length, HAL)和股骨干直径(Femoral Shaft Diameter, FSD)七个形态参数,并记录患者年龄,性别和骨折部位。采用t检验对连续变量进行比较,卡方检验分析分类变量以及使用多重Logistic 回归分析比较股骨颈骨折患者和股骨转子间骨折的股骨近端形态参数间的差异,并比较不同性别的髋部骨折患者几何形态参数的差异。
结果:
两组不同髋部骨折类型的骨折患者的NSA,CEA,FND和FNAL有显著的统计学差异(P<0.001, P<0.001, P=0.027和P<0.001)。NSA为股骨颈骨折的危险因素(OR 0.70, P<0.001),CEA和FNAL为股骨转子间骨折的危险因素(OR 1.15, 1.17, P均<0.001)。FND为股骨转子间骨折的保护因素 (OR 0.74, P<0.001)。
结论:
我们的研究证实了不同类型的髋部骨折患者股骨近端几何形态参数存在着差异性,同时髋部几何形态参数存在着性别差异。在骨折内固定及髋关节置换术中假体选择方面应考虑到不同髋部骨折类型和不同性别的股骨近端几何形态参数的差异性。同时可指导设计符合国人的个体化定制型假体,并对老年髋部骨折患者股骨近端的精准重建提供依据。
INTRODUCTION
The incidence of hip fractures in the elderly is increasing year by year. Hip fractures in the elderly are commonly referred to as femoral neck fractures and intertrochanteric fractures occurring in the elderly, aged 65 years and over.[1] Hip fractures account for 7% of all adult whole-body fractures and 24% in geriatric populations.[2,3] Hip fractures are related to high mortality, long-term disability, and reduced quality of life, and thus, they are the most serious complication of osteoporosis,[4] imposing a heavy burden on the individual, family, society, and health-care system of China.[5,6]
The increase in the incidence of hip fractures in the elderly is due to decreased bone mass and bone quality. This results in a decrease in proximal femur strength and the increased occurrence of hip fractures despite low-energy injuries, such as lateral falls.[7] A growing number of studies have confirmed that hip bone density and geometry structure are two important determinants of proximal femoral bone strength.[8,9,10,11,12] Therefore, it is of great significance to study the geometric parameters of the hips of elderly patients with hip fractures. Some clinical studies have found that results of European and American studies are not entirely applicable to Asian or Chinese people,[13,14,15] showing differences in shape, size, and geometry in the proximal femur between racial groups. Current prosthesis selection in Chinese clinical practice is based on the results of foreign studies, such as the Nobel index of femoral medullary morphology.[16] Many other studies have focused on the morphology of hips in Caucasians, but corresponding studies in Asian populations are limited, particularly data on proximal femoral geometric parameters in Han Chinese.[16] Our study analyzed the geometric parameters of the hip in 198 patients with hip fractures compared to different types of hip fractures. Our goal was to provide evidence and guidance for selection and manufacture of clinical prostheses, as well as providing evidence for the accurate reconstruction of proximal femurs in Chinese hip fracture patients.
METHODS
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of The Third Hospital, Hebei Medical University.
Patients
From January 2017 to December 2017, 198 patients (44 males and 154 females, mean age ± standard deviation [SD]: 77 ± 7 years) with hip fractures were studied. Of the 198 cases of geriatric hip fracture patients, 101 patients had femoral neck fractures, and 97 patients had intertrochanteric fractures. Inclusion criteria were the following: (1) older than 65 years; (2) acute fresh femoral neck fractures and intertrochanteric fractures; (3) first unilateral fractures; (4) patients undergoing operative treatment; (5) patients with no thyroid or parathyroid disease in their medical history; (6) patients with no bone tumor or tumor-like diseases; (7) hip fractures caused by spontaneous falls on the ground; and (8) X-ray films of the pelvis and proximal femur before and after operation with standard posture. Exclusion criteria were the following: (1) second hip fracture; (2) bilateral hip fracture; (3) pathological fracture; (4) primary and secondary bone tumor disease, tumor-like disease, tuberculosis, chemotherapy, radiotherapy, and Paget's disease; (5) patients having a history of acute stroke and poliomyelitis; (6) patients having a history of anti-osteoporosis treatment; (7) multiple fractures; and (8) congenital dysplasia and deformity of the femur and pelvis.
The study sample was divided into the femoral neck fracture group (n = 101) and femoral intertrochanteric fracture group (n = 97) based on X-ray diagnostic criteria.
Measurement methods
The radiographic images of 198 patients with pelvic and bilateral hip joint pre- and post-operation were carefully reviewed by the hospital picture archiving and communication system and downloaded to a private computer in digital imaging and communication (DICOM) format. RadiAnt DICOM Viewer (Medixant Company, Poland) was used to measure the geometric morphological parameters of patients’ images and was cross-referenced to the electronic medical records, including age, sex, site of fracture, surgical methods, and internal fixation materials.
Measurement parameters
The seven proximal femur geometric parameters of each patient, including the neck shaft angle (NSA), center edge angle (CEA), femoral head diameter (FHD), femoral neck diameter (FND), femoral neck axial length (FNAL), hip axial length (HAL), and femoral shaft diameter (FSD) were measured according to published guidelines in the literature.[17] Measurements were performed in triplicate by one person, and the mean of the three measurements was taken. The precision of our measurements is 0.001 mm for lengths and 0.01° for angles, respectively.
Measurement procedures
We measured the NSA by selecting the line through the center of the femoral head and neck on the standard pelvis or proximal femur as the anatomical axis of the femoral head and neck. In addition, the midpoint line of the line between the proximal end of the femoral shaft and the medial and lateral cortex of the femoral shaft was chosen as the anatomical axis of the proximal end of the femur. The medial intersection of these two lines is the NSA [Figure 1]. The CEA is the angle between the line from the center of the femoral head to the outer edge of the acetabulum and the line through the vertical line of the femoral head [Figure 2].[18] The measurement method of FHD is an assumption that the femoral head is a circle on hip joint radiograph or pelvic radiography. The maximum distance from the outer superior edge to the inner and inferior edge of the femoral head is defined as the FHD. The diameter of the femoral neck is defined as the shortest distance between the outer superior edge of the femoral neck and the lateral cortex of the medial and inferior margin. The proximal end of the femoral head-and-neck anatomic axis line extends to the apex of the femoral head, and the distal end extends to the lateral femoral cortex.
Figure 1.
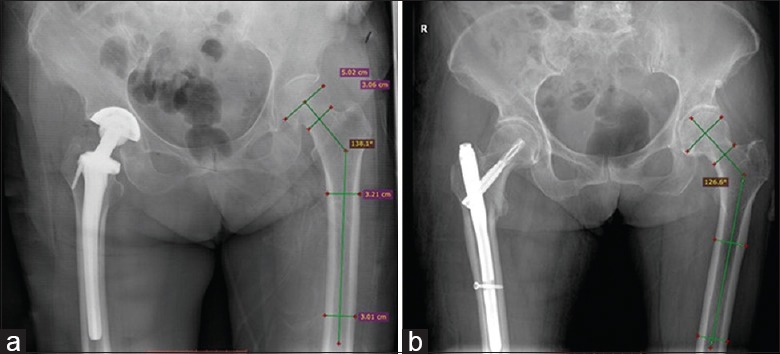
Schematic photograph of measurement method on neck shaft angle in femoral neck fracture group (a) and femoral intertrochanteric fracture group (b) on postoperative X-ray image.
Figure 2.
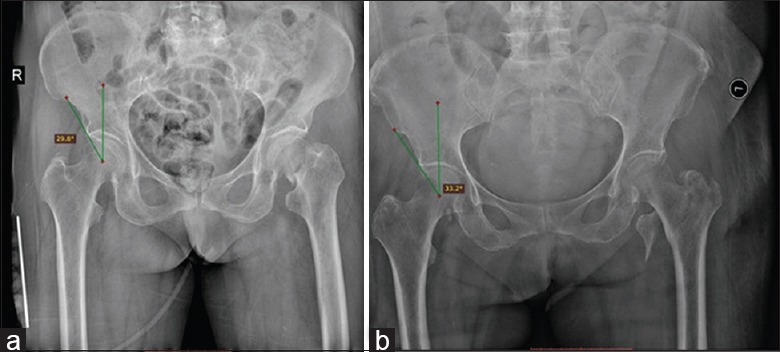
Schematic photograph of measurement method on center edge angle in femoral neck fracture group (a) and femoral intertrochanteric fracture group (b) on preoperative X-ray image.
The junction of the lateral cortex of the femur and the apex of the femoral head with the anatomical axis of the femoral head and neck is defined as FNAL. The proximal end of FNAL extends to the medial point of the medial border of the pelvis, and the distance from this point to the lateral femoral cortex is defined as the HAL [Figure 3]. To determine the diameter of the femoral shaft, we examined the femoral shaft in the two planes of the lower margin of the trochanter and the middle and upper segment of the shaft of the femur and then made a vertical line of the anatomical axis of the femoral shaft at the bottom edge of the trochanter, which extended 2 cm to the distal end of the shaft, as previously described.[19] The distance between the vertical line and the medial and lateral cortical intersections of femoral shaft is the diameter of femoral shaft [Figure 4].
Figure 3.
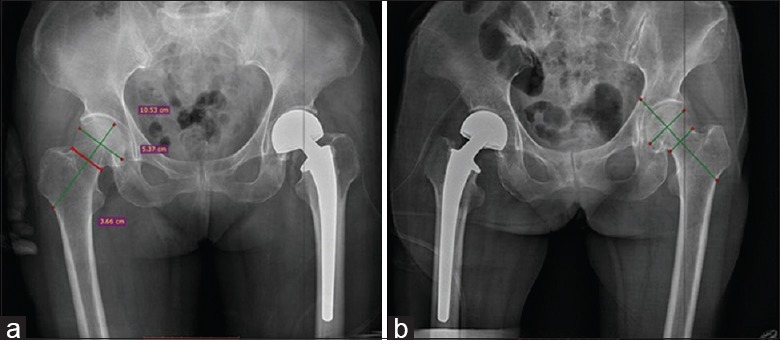
Schematic photograph of measurement method on femoral head diameter, femoral neck diameter, femoral neck axial length, (a) and hip axial length (b) on postoperative X-ray image of hip fracture patients.
Figure 4.
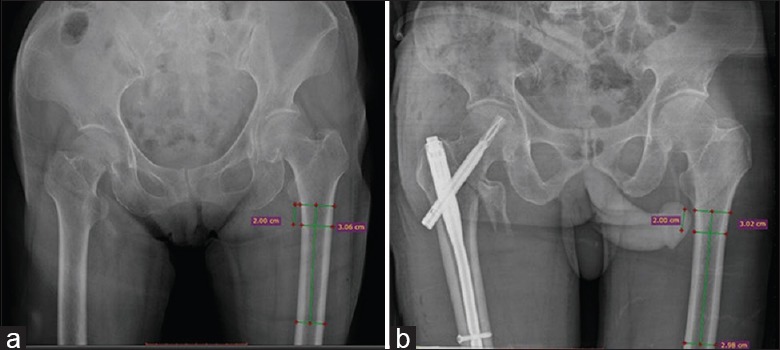
Schematic photograph of measurement method on femoral shaft diameter in femoral neck fracture group (a) and femoral intertrochanteric fracture group (b) on X-ray image.
Statistical analysis
We used SPSS 22.0 software (IBM, USA) to analyze the data. For continuous variables, the Shapiro-Wilk test was used to determine the normal distribution. We used mean ± SD to express continuous variables. Student's t-test was used to compare continuous variables between patients with femoral neck fractures and patients with femoral intertrochanteric fractures. The Chi-squared test was used to classify categorical variables, and multiple logistic stepwise regression analysis was further used to determine the influence of hip geometry parameter on hip fracture type. Results were expressed by the odds ratio (OR), to the 95% confidence interval. P < 0.05 was considered statistically significant.
RESULTS
The clinical characteristics of the two different types of hip fractures are shown in Table 1. Geometric parameters of the hips in patients with femoral neck fractures and femoral trochanter fractures are shown in Table 2.
Table 1.
Comparison of the clinical characteristics of two groups
| Group | N | Gender, n | Fracture site, n | Age (years), mean ± SD | ||
|---|---|---|---|---|---|---|
| Male | Female | Left | Right | |||
| Femoral neck fracture | 101 | 23 | 78 | 54 | 47 | 76.3 ± 7.3 |
| Intertrochanteric fracture | 97 | 21 | 76 | 46 | 51 | 78.9 ± 7.5 |
| χ2/t | 0.036* | 0.723* | 2.607† | |||
| P | 0.849 | 0.395 | 0.014 | |||
*: χ2 values, †: t values. SD: Standard deviation.
Table 2.
Comparisons of the proximal femoral parameters between two groups
| Parameter | Total group (N = 198) | Femoral neck fracture (n = 101) | Intertrochanteric fracture (n = 97) | t | P |
|---|---|---|---|---|---|
| NSA (°) | 134.85 ± 5.17 | 137.63 ± 4.56 | 132.07 ± 4.17 | 1.598 | <0.001 |
| CEA (°) | 40.37 ± 7.45 | 37.62 ± 6.77 | 43.11 ± 7.09 | 5.597 | <0.001 |
| FHD (mm) | 51.03 ± 3.88 | 51.09 ± 3.52 | 50.96 ± 4.23 | 0.244 | 0.807 |
| FND (mm) | 34.65 ± 3.58 | 35.21 ± 3.25 | 34.09 ± 3.82 | 2.233 | 0.027 |
| FNAL (mm) | 101.44 ± 8.41 | 99.30 ± 7.91 | 103.58 ± 8.39 | 3.715 | <0.001 |
| HAL (mm) | 119.10 ± 9.56 | 118.23 ± 8.73 | 119.97 ± 10.29 | 1.285 | 0.200 |
| FSD (mm) | 31.09 ± 3.37 | 30.71 ± 2.68 | 31.47 ± 3.93 | 1.598 | 0.112 |
NSA: Neck shaft angle; CEA: Center edge angle; FHD: Femoral head diameter; FND: Femoral neck diameter; FNAL: Femoral neck axial length; HAL: Hip axial length; FSD: Femoral shaft diameter.
The geometric parameters of the two groups were found to be significantly different in patients with different hip fractures (NSA, P < 0.001, CEA, P < 0.001, FND, P = 0.027, and FNAL, P < 0.001, respectively). The femoral neck fracture group had larger NSA, smaller CEA, wider FND, and shorter FNAL compared to those with intertrochanteric fractures. There was no significant difference in FHD, FSD, and HAL between the two groups (P = 0.807, 0.112, and 0.200 respectively), as shown in Table 2.
Multiple logistic regression analysis of proximal geometric parameters is shown in Table 3. The geometric parameters of the hips of patients with different hip fracture types were analyzed by multiple logistic regression analysis. The results show that greater NSA was the risk factor for femoral neck fractures (OR: 0.70, P < 0.001), and greater CEA was the risk factor for femoral intertrochanteric fractures (OR: 1.15, P < 0.001). Longer FNAL was the risk factor for femoral intertrochanteric fractures (OR: 1.17, P < 0.001), and greater FND was the protective factor of femoral intertrochanteric fractures (OR: 0.74, P < 0.001).
Table 3.
Risk factors of proximal femoral geometry parameters for femoral intertrochanteric fractures compared with femoral neck fractures by logistic regression
| Parameter | OR | 95% CI | P |
|---|---|---|---|
| NSA | 0.70 | 0.62–0.79 | <0.001 |
| CEA | 1.15 | 1.08–1.22 | <0.001 |
| FNAL | 1.17 | 1.09–1.25 | <0.001 |
| FND | 0.74 | 0.63–0.86 | <0.001 |
| FHD | 1.14 | 0.93–1.39 | 0.200 |
| HAL | 0.94 | 0.84–1.05 | 0.306 |
| FSD | 0.97 | 0.82–1.15 | 0.709 |
| Age | 1.01 | 0.95–1.07 | 0.759 |
| Female sex | 1.97 | 0.55–7.11 | 0.298 |
OR: Odds ratio; CI: Confidence interval; NSA: Neck shaft angle; CEA: Center edge angle; FHD: Femoral head diameter; FND: Femoral neck diameter; FNAL: Femoral neck axial length; HAL: Hip axial length; FSD: Femoral shaft diameter.
There was a significant difference in proximal femoral geometric parameters between sexes [Table 4]. Males had larger FHD, FND, FSD, and longer HAL and FNAL compared to female patients. There was no difference in NSA, CEA, and patient age between the sexes.
Table 4.
Comparisons of the proximal femoral geometry parameters between male and female patients
| Parameter | Male (n = 44) | Female (n = 154) | t | P |
|---|---|---|---|---|
| NSA (°) | 135.49 ± 5.19 | 132.07 ± 4.17 | 0.969 | 0.334 |
| CEA (°) | 41.72 ± 6.76 | 39.95 ± 7.62 | 1.434 | 0.153 |
| FHD (mm) | 54.89 ± 3.16 | 49.84 ± 3.26 | 9.357 | <0.001 |
| FND (mm) | 38.75 ± 2.77 | 33.39 ± 2.76 | 11.631 | <0.001 |
| FNAL (mm) | 107.47 ± 8.86 | 99.59 ± 7.36 | 5.535 | <0.001 |
| HAL (mm) | 127.53 ± 9.41 | 116.51 ± 8.00 | 7.912 | <0.001 |
| FSD (mm) | 32.59 ± 2.70 | 30.63 ± 3.43 | 3.578 | <0.001 |
| Age (years) | 77.1 ± 8.2 | 77.8 ± 7.3 | 0.546 | 0.586 |
NSA: Neck shaft angle; CEA: Center edge angle; FHD: Femoral head diameter; FND: Femoral neck diameter; FNAL: Femoral neck axial length; HAL: Hip axial length; FSD: Femoral shaft diameter.
DISCUSSION
Neck shaft angle and hip fracture type
NSA is a relatively independent geometric parameter of the proximal femur. In this study, the NSA in 198 patients was 134.85 ± 5.17°, consistent with other studies in Chinese samples.[20] The result of the average angle of NSA as measured by X-ray is 138.48°.[21] The range of NSA in Europeans and Americans was found to be 125–135° as reported by Peng,[22] which is slightly lower than that in our Chinese patients. This difference should be considered in the design and manufacture of prostheses in Chinese patients. In the current study, the average NSA of 101 patients with femoral neck fractures was 137.63 ± 4.56°, and the average NSA of 97 patients with intertrochanteric fractures of the femur was 132.07 ± 4.17°. The further study found that the patients with femoral neck fractures had larger NSAs than those with intertrochanteric fractures of the femur, consistent with other reports in the literature.[23,24] Gnudi et al.[23] reported that patients with femoral neck fractures had larger NSAs compared to those with intertrochanteric fractures of the femur, leading to the suspicion that increased NSA is a major risk factor for hip fractures. Partanen et al.[24] also reported that patients with femoral neck fractures in the group had a larger NSA than patients with intertrochanteric fractures. In the current study, multiple logistic regression analysis showed that femoral NSA was a risk factor for femoral neck fractures (OR: 0.70, P < 0.001). New research suggests that NSA may be a risk factor for hip fracture types.[18] Patients with femoral neck fractures have larger NSAs than patients with intertrochanteric fractures.[25] The reason may be because the NSA continues to change in adults, even after the bone is fully developed, along with age, physical exercise, and long-term weight-bearing. Bone remodeling at the proximal end of the femur may eventually lead to a decrease in NSA. This study also supports the fact that patients with intertrochanteric fractures are older than patients with femoral neck fractures.
The NSA increases the range of movement of the lower extremities and conveys trunk strength to the wider base of femoral neck. Restoration of normal NSA is vital for treatment of hip fractures and evaluation of anatomical reduction quality of hip fractures and also of great importance to restoration of normal offset of hip joints and equal lengths of lower extremities. Thus, construction of normal biomechanical environment of the hip has very important clinical significance for hip surgery. The current study can guide the accurate reconstruction of proximal femurs and has very important clinical significance for making individualized prosthesis design in accordance with the Chinese population.
Center edge angle and the type of hip fracture
CEA, also known as the central margin angle, was proposed by Wiberg[26] to evaluate the stability of the hip joint. In the current study, we found that patients with intertrochanteric fractures had larger CEA values than those with femoral neck fractures. Patients with intertrochanteric fractures tend to have more pointed and longer osteophytes compared to those with femoral neck fractures, which can lead to an increased CEA on radiographs of the pelvis or hip joint. Previous studies have confirmed that patients with intertrochanteric fractures have narrower joint spaces and more severe hip osteoarthritis than those with femoral neck fractures. Studies have shown a significant correlation between hip osteoarthritis and hip fracture types. The size of the osteophyte is an indicator of the severity of hip osteoarthritis. In the occurrence of hip fractures, studies have confirmed that the occurrence of femoral neck fractures is caused by the impact of a fall on the outer upper cortex of the femoral neck and the posterior edge of the acetabulum.[18] As osteophyte proliferation of the posterior edge of the acetabulum is more obvious in the patients with intertrochanteric fracture of the femur, the point of the impact between the posterior edge of the acetabulum and the posterior edge of the femoral neck will be closer to the intertrochanteric area of the femur during the same fall. This may explain the greater incidence of an intertrochanteric fracture over a femoral neck fracture during the same fall. Thus, the data suggest that CEA is a major risk factor for intertrochanteric fractures of the femur. CEA is an index used to evaluate hip joint stability. Different types of hip fracture patients have different CEAs, which can be used to guide preoperative planning and accurate reconstruction of acetabular abduction angles.
Femoral head diameter and hip fracture type
In the current study, the male femoral head on average is larger than that of the female, consistent with the results of Pi et al.,[27] who also reported that male femoral heads were larger than female femoral heads. This could be due to body mass in men, which would call for greater femoral head size to support the higher weight and need for hip stability. Studies have shown that the diameter of the femoral head in the Chinese population is smaller than that in Western Caucasians. Therefore, the size of hip prostheses or implants should take into account ethnic and gender differences between the Chinese and Western Caucasians.
Femoral neck diameter and hip fracture types
In the current study, the femoral intertrochanteric fracture group had a smaller FND. We suspect that this may be associated with reduced cortical bone thickness in the femoral neck area, as patients with intertrochanteric fractures have more severe osteoporosis and lower bone mass, as manifested in the femoral neck area. The thickness of cortical bone was decreased, and the internal cortical bone appeared loose and porous. Moreover, the femoral neck is a special anatomical region that lacks the periosteum. With age, osteogenesis effect of the periosteum in the femoral neck is reduced and becomes weaker. Multiple logistic regression analysis found that FND was the protective factor of intertrochanteric fractures, and the increase in FND could reduce the occurrence of intertrochanteric fracture.
Johannesdottir et al.[28] found that the thickness of the lower cortex of the femoral neck rarely changes and that the thickness of the cortex above the femoral neck plays a more important role in the weakening of the bone strength of the femoral neck. Previous studies[29,30] have found that the thickness of the subquadrant bone cortex of the femoral neck does not change with age, but the thickness of the upper quadrant becomes thinner with age. However, when the lateral fall occurs, the thinner upper quadrant bone cortex will bear a large impact, which can lead to fracture.
In our study, men had greater FNDs than women, which might explain why women have a higher incidence of hip fractures. The cortical thickness of the femoral neck, especially in the anterior superior quadrant, is an independent predictor of fracture risk or specifically a predictor for resisting femoral neck fracture.[28] With age, the area covered by the periosteum will increase bone formation. The increase in the outer diameter of the present bone compensates for reduced bone strength, especially in men.[31,32]
The FND is an important morphological parameter in the internal fixation of the proximal femur fracture and the replacement of the hip joint. The diameter of the femoral neck also has important clinical references for the selection of the type of internal fixation screws, the number (such as three or four hollow compression screws), and the direction of the puncture.
Femoral neck axial length and hip fracture types
Patients with femoral intertrochanteric fractures had higher FNAL than those with femoral neck fractures. This is consistent with Lu et al.,[33] who found that the FNAL of patients with intertrochanteric fractures of the femur was 90.68 mm compared to the femoral neck fracture group (88.64 mm). From the biomechanical point of view, the longer axis of the femoral neck causes the greater trochanter of the femur to protrude more, and thus, the possibility of intertrochanteric fracture increases when an external force impacts the femoral trochanter. The long axial length of femoral neck and the high risk of proximal femoral fractures have been recognized by most scholars.
FNAL is an important morphological parameter in the internal fixation of proximal femoral fractures and hip arthroplasty. Restoration of normal FNAL before fracture has important clinical significance for accurate restoration of normal hip geometry parameters and can be beneficial for better hip function.
Hip axial length and hip fracture types
From the definition, it can be concluded that the HAL is greater than the FNAL with the hip joint space and the thickness of the acetabular wall. Taken together with the results of the FNAL, the patients with intertrochanteric femur fractures have a narrower hip joint space than those with femoral neck fractures, which will lead to the reduction of HAL in patients in the intertrochanteric fracture group. We did not find a relationship between HAL and hip fracture type in this study. A previous study found that HAL can be independent of age and bone mineral density as a single predictor of femoral neck fracture.[34] Chin et al.[35] confirmed that the HAL of Chinese women was significantly lower than that of European women and concluded that the low incidence of hip fractures in Chinese women may be due to shorter HALs.
Femoral shaft diameter and type of hip fracture
The FSD in patients with intertrochanteric fracture was higher than that in patients with femoral neck fractures. However, there was no significant statistical difference between the two groups (P = 0.112). Multiple logistic regression analysis showed no correlation between FSD and hip fracture type (P = 0. 709).
There was no difference in FSD between intertrochanteric and femoral neck fracture patients. However, FSD was greater in male patients (P < 0.001), suggesting that a larger FSD leads to stronger bones in men. This is consistent with the trend that women have lower femur bone strength and higher hip fracture rates compared to men. Studies have shown that the FSD increases compensatively with age due to the osteogenesis of the periosteum, thus reducing the weakening of bone strength due to the decline in bone mass, which appears to be more evident in men.[36,37]
There were some limitations in our study. First, the sample was small, and it was mainly because of the strict inclusion and exclusion criteria. Second, this study was a retrospective research study, and as such, retrospective bias was inevitable. Future studies should expand the sample size and carry out a randomized, controlled prospective study to further clarify the differences in the geometric morphological parameters and risk factors of the proximal femur in two different types of elderly patients with hip fractures.
In conclusion, there were differences in hip-geometric morphological parameters and risk factors between elderly Chinese patients with femoral neck fractures and intertrochanteric fractures. NSA was the major risk factor for femoral neck fractures, while CEA and FNAL were the major risk factors for intertrochanteric fractures. The FND was found to be the major protective factor for intertrochanteric fractures. The results suggest that the geometric parameters of the hip may play an important role in the occurrence and type of hip fractures. Therefore, the differences of geometric morphological parameters of proximal femurs of different hip fractures and different sexes should be considered in the selection of prostheses during fracture internal fixation and hip replacement. These data can provide guidance for the design of individualized customized prostheses and provide the evidence for accurate reconstruction of proximal femurs for elderly Chinese hip fracture patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Qiang Shi
REFERENCES
- 1.Zhang SM, Li HF, Yu GY. Clinical treatment procedure of hip fracture in the elderly (in Chinese) Orthop J China. 2005;13:1365–8. doi: 10.3969/j.issn.1005-8478.2005.18.001. [Google Scholar]
- 2.Zhang YZ. A guide to hip fracture in adults (in Chinese) Chin J Surg. 2015;53:57–62. doi: 10.3760/cma.j.issn.0529-5815.2015.01.014. [Google Scholar]
- 3.Zhang YZ. Clinical Epidemiology of Orthopedic Trauma. New York: Thieme; 2012. [Google Scholar]
- 4.Tian FM, Zhang L, Zhao HY, Liang CY, Zhang N, Song HP, et al. An increase in the incidence of hip fractures in Tangshan, China. Osteoporos Int. 2014;25:1321–5. doi: 10.1007/s00198-013-2600-6. doi: 10.1007/s00198-013-2600-6. [DOI] [PubMed] [Google Scholar]
- 5.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–7. doi: 10.1016/S0140-6736(02)08657-9. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 6.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–9. doi: 10.1001/jama.2009.1462. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sambrook P, Cooper C. Osteoporosis. Lancet. 1996;348:1085. doi: 10.1016/S0140-6736(88)91826-0. [Google Scholar]
- 8.Einhorn TA. Bone strength: The bottom line. Calcif Tissue Int. 1992;51:333–9. doi: 10.1007/BF00316875. doi: 10.1007/BF00316875. [DOI] [PubMed] [Google Scholar]
- 9.Turner CH. Bone strength: Current concepts. Ann N Y Acad Sci. 2006;1068:429–46. doi: 10.1196/annals.1346.039. doi: 10.1196/annals.1346.039. [DOI] [PubMed] [Google Scholar]
- 10.Davison KS, Siminoski K, Adachi JD, Hanley DA, Goltzman D, Hodsman AB, et al. Bone strength: The whole is greater than the sum of its parts. Semin Arthritis Rheum. 2006;36:22–31. doi: 10.1016/j.semarthrit.2006.04.002. doi: 10.1016/j.semarthrit.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Ammann P, Rizzoli R. Bone strength and its determinants. Osteoporos Int. 2003;14(Suppl 3):S13–8. doi: 10.1007/s00198-002-1345-4. doi: 10.1007/s00198-002-1345-4. [DOI] [PubMed] [Google Scholar]
- 12.van der Meulen MC, Jepsen KJ, Mikić B. Understanding bone strength: Size isn’t everything. Bone. 2001;29:101–4. doi: 10.1016/s8756-3282(01)00491-4. doi: 10.1016/S8756-3282(01)00491-4. [DOI] [PubMed] [Google Scholar]
- 13.Chang SM, Song DL, Ma Z, Tao YL, Chen WL, Zhang LZ, et al. Mismatch of the short straight cephalomedullary nail (PFNA-II) with the anterior bow of the femur in an Asian population. J Orthop Trauma. 2014;28:17–22. doi: 10.1097/BOT.0000000000000022. doi: 10.1097/BOT.0000000000000022. [DOI] [PubMed] [Google Scholar]
- 14.Feng W, Yu B, Hao T, Hao ZT. Geometric match assessment of three intramedullary nailing systems for Chinese proximal femurs (in Chinese) Chin J Orthop Trauma. 2011;13:1029–33. doi: 10.3760/cma.j.issn.1671-7600.2011.11.007. [Google Scholar]
- 15.Du XR, Lu SB. Research progress on anatomical study of the proximal femoral canal (in Chinese) Chin J Clin Anat. 2004;22:674–6. doi: 10.3969/j.issn.1001-165X.2004.06.035. [Google Scholar]
- 16.Jiang N, Peng L, Al-Qwbani M, Xie GP, Yang QM, Chai Y, et al. Femoral version, neck-shaft angle, and acetabular anteversion in Chinese han population: A retrospective analysis of 466 healthy adults. Medicine (Baltimore) 2015;94:e891. doi: 10.1097/MD.0000000000000891. doi: 10.1097/MD.0000000000000891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pulkkinen P, Partanen J, Jalovaara P, Jämsä T. Combination of bone mineral density and upper femur geometry improves the prediction of hip fracture. Osteoporos Int. 2004;15:274–80. doi: 10.1007/s00198-003-1556-3. doi: 10.1007/s00198-003-1556-3. [DOI] [PubMed] [Google Scholar]
- 18.Yamauchi K, Naofumi M, Sumida H, Fukuta S, Hori H. Comparison of morphological features in the femur between femoral neck fractures and femoral intertrochanteric fractures. Surg Radiol Anat. 2016;38:775–80. doi: 10.1007/s00276-016-1626-9. doi: 10.1007/s00276-016-1626-9. [DOI] [PubMed] [Google Scholar]
- 19.Im GI, Lim MJ. Proximal hip geometry and hip fracture risk assessment in a korean population. Osteoporos Int. 2011;22:803–7. doi: 10.1007/s00198-010-1301-7. doi: 10.1007/s00198-010-1301-7. [DOI] [PubMed] [Google Scholar]
- 20.Jiang N, Peng L, Al-Qwbani M, Xie GP, Yang QM, Chai Y, et al. Femoral version, neck-shaft angle, and acetabular anteversion in Chinese han population: A retrospective analysis of 466 healthy adults. Medicine (Baltimore) 2015;94:e891. doi: 10.1097/MD.0000000000000891. doi: 10.1097/MD.0000000000000891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang ZH, Yeoh CS, Tan GM. Radiographic study of the proximal femur morphology of elderly patients with femoral neck fractures: Is there a difference among ethnic groups? Singapore Med J. 2017;58:717–20. doi: 10.11622/smedj.2016148. doi: 10.11622/smedj.2016148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng AQ. Principles of Surgical Treatment of Fractures (in Chinese) 3rd ed. Beijing: People's Health Publishing House; 2007. [Google Scholar]
- 23.Gnudi S, Ripamonti C, Lisi L, Fini M, Giardino R, Giavaresi G, et al. Proximal femur geometry to detect and distinguish femoral neck fractures from trochanteric fractures in postmenopausal women. Osteoporos Int. 2002;13:69–73. doi: 10.1007/s198-002-8340-2. doi: 10.1007/s198-002-8340-2. [DOI] [PubMed] [Google Scholar]
- 24.Partanen J, Jämsä T, Jalovaara P. Influence of the upper femur and pelvic geometry on the risk and type of hip fractures. J Bone Miner Res. 2001;16:1540–6. doi: 10.1359/jbmr.2001.16.8.1540. doi: 10.1359/jbmr.2001.16.8.1540. [DOI] [PubMed] [Google Scholar]
- 25.Tal S, Gurevich A, Sagiv S, Guller V. Differential impact of some risk factors on trochanteric and cervical hip fractures. Geriatr Gerontol Int. 2015;15:443–8. doi: 10.1111/ggi.12294. doi: 10.1111/ggi.12294. [DOI] [PubMed] [Google Scholar]
- 26.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteo-arthritis. JAMA. 1940;115:81. doi: 10.1001/jama.1940.02810270083037. [Google Scholar]
- 27.Pi Y, Zhao Y, Wang W, He Z, Mao X. Measurement of proximal femoral morphology and analysis of 500 cases in Hunan Province (in Chinese) Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2013;38:925–30. doi: 10.3969/j.issn.1672-7347.2013.09.010. doi: 10.3969/j.issn.1672-7347.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 28.Johannesdottir F, Poole KE, Reeve J, Siggeirsdottir K, Aspelund T, Mogensen B, et al. Distribution of cortical bone in the femoral neck and hip fracture: A prospective case-control analysis of 143 incident hip fractures; the AGES-REYKJAVIK study. Bone. 2011;48:1268–76. doi: 10.1016/j.bone.2011.03.776. doi: 10.1016/j.bone.2011.03.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poole KE, Mayhew PM, Rose CM, Brown JK, Bearcroft PJ, Loveridge N, et al. Changing structure of the femoral neck across the adult female lifespan. J Bone Miner Res. 2010;25:482–91. doi: 10.1359/jbmr.090734. doi: 10.1359/jbmr.090734. [DOI] [PubMed] [Google Scholar]
- 30.Mayhew PM, Thomas CD, Clement JG, Loveridge N, Beck TJ, Bonfield W, et al. Relation between age, femoral neck cortical stability, and hip fracture risk. Lancet. 2005;366:129–35. doi: 10.1016/S0140-6736(05)66870-5. doi: 10.1016/S0140-6736(05)66870-5. [DOI] [PubMed] [Google Scholar]
- 31.Seeman E. Pathogenesis of bone fragility in women and men. Lancet. 2002;359:1841–50. doi: 10.1016/S0140-6736(02)08706-8. doi: 10.1016/S0140-6736(02)08706-8. [DOI] [PubMed] [Google Scholar]
- 32.Seeman E. Periosteal bone formation – A neglected determinant of bone strength. N Engl J Med. 2003;349:320–3. doi: 10.1056/NEJMp038101. doi: 10.1056/NEJMp038101. [DOI] [PubMed] [Google Scholar]
- 33.Lu YG, Hao YQ, Shi DW, Wang XP. Evaluation of proximal femoral geometry with computerized tomography in patients with hip fragility fractures (in Chinese) Chin J Osteoporos. 2011;17:195–8. doi: 10.3969/j.issn.1006-7108.2011.03.003. [Google Scholar]
- 34.Faulkner KG, Cummings SR, Black D, Palermo L, Glüer CC, Genant HK, et al. Simple measurement of femoral geometry predicts hip fracture: The study of osteoporotic fractures. J Bone Miner Res. 1993;8:1211–7. doi: 10.1002/jbmr.5650081008. doi: 10.1002/jbmr.5650081008. [DOI] [PubMed] [Google Scholar]
- 35.Chin K, Evans MC, Cornish J, Cundy T, Reid IR. Differences in hip axis and femoral neck length in premenopausal women of polynesian, Asian and European origin. Osteoporos Int. 1997;7:344–7. doi: 10.1007/BF01623775. doi: 10.1007/BF01623775. [DOI] [PubMed] [Google Scholar]
- 36.Ruff CB, Hayes WC. Subperiosteal expansion and cortical remodeling of the human femur and tibia with aging. Science. 1982;217:945–8. doi: 10.1126/science.7112107. doi: 10.1126/science.7112107. [DOI] [PubMed] [Google Scholar]
- 37.Ruff CB, Hayes WC. Sex differences in age-related remodeling of the femur and tibia. J Orthop Res. 1988;6:886–96. doi: 10.1002/jor.1100060613. doi: 10.1002/jor.1100060613. [DOI] [PubMed] [Google Scholar]


