Abstract
Background:
Many clinical studies over the past decade have indicated positive outcomes for patients treated with Dynesys dynamic stabilization for lumbar degenerative disease. However, long-term outcomes of Dynesys for lumbar spinal stenosis are rarely reported. The aim of this study was to analyze the long-term clinical and radiologic outcomes for patients with lumbar spinal stenosis treated with Dynesys stabilization.
Methods:
Thirty-eight patients with lumbar spinal stenosis were treated with Dynesys stabilization from July 2008 to March 2010. The minimal duration of follow-up was 72 months. The patients were divided into stenosis and spondylolisthesis groups according to degenerative spondylolisthesis. Clinical outcomes were evaluated using the Oswestry Disability Index (ODI) and visual analog scale (VAS). Radiographic evaluations included range of motion (ROM) and the disc heights of stabilized segments and the upper adjacent segments. We also evaluated the occurrence of radiographic and symptomatic adjacent segment degeneration (ASD).
Results:
There were 23 patients in stenosis group and 15 patients in spondylolisthesis group. The ODI scores were significantly improved at the final follow-up evaluation, as compared to the baseline values (16.1 ± 5.7 vs. 57. 2 ± 14.2, t = 61.41, P < 0.01). The VAS scores for back and leg pain were significantly improved from 4.82 ± 0.89 and 4.04 ± 0.82 preoperatively to 0.93 ± 0.61 and 0.54 ± 0.51 postoperatively (t = 6.59, P < 0.01, and t = 5.91, P < 0.01, respectively). There were no differences between the two groups with respect to VAS and ODI scores. The ROM of stabilized segments decreased significantly from 7.8° ± 2.4° to 4.5° ± 1.5° (t = 7.18, P < 0.05), while the upper adjacent segments increased significantly from 8.3° ± 2.4° to 10.4° ± 2.4° (t = 2.87, P = 0.01). The change in disc height of stabilized segments was not significant (11.9 ± 2.1 preoperatively vs. 12.5 ± 1.5 postoperatively, t = 1.43, P = 0.15), whereas the decrease in disc height of the upper adjacent segments was significant (12.5 ± 2.0 preoperatively vs. 11.0 ± 1.7 postoperatively, t = 2.94, P = 0.01). The occurrence of radiographic and symptomatic ASD was 16% (6/38) and 3% (1/38), respectively.
Conclusions:
Decompression and Dynesys stabilization for lumbar stenosis with or without spondylolisthesis showed good long-term clinical and radiographic results. Lumbar stenosis with or without Grade I spondylolisthesis, particularly in patients <60 years of age with mild-to-moderate lumbar disc degeneration, would be one of the main indications for the Dynesys system.
Keywords: Adjacent Segment Degeneration, Dynamic Stabilization, Dynesys, Lumbar Spinal Stenosis, Lumbar Spondylolisthesis
摘要
背景:
在过去十几年中有大量研究显示,Dynesys动态固定系统治疗腰椎退变性疾病取得良好的短期疗效,但是关于Dynesys系统治疗腰椎管狭窄症的长期随访研究较少。本研究的目的即是评估Dynesys动态稳定系统治疗腰椎管狭窄症的长期临床和影像学疗效。
方法:
回顾分析2008年7月-2010年3月采用Dynesys 动态固定治疗的腰椎管狭窄症患者38例,最短随访时间为72个月。所有患者根据是否存在腰椎退变滑脱分为腰椎管狭窄组和滑脱组。临床评价指标包括Oswestry 功能障碍指数(Oswestry disability index,ODI)和疼痛视觉模拟量表(visual analogue scale,VAS) 评分。影像学评估指标包括手术节段和近侧邻近节段活动度(range of motion, ROM)和椎间高度,以及影像学和症状学邻近节段退变的发生情况。
结果:
腰椎管狭窄组共有23例患者,滑脱组有15例患者。与术前相比,在末次随访时患者ODI评分显著改善(16.1 ± 5.7 vs. 57. 2± 14.2,t = 61.41,P < 0.01)。患者腰部和腿部VAS评分分别由术前的4.82 ± 0.89分和4.04 ± 0.82降至末次随访时的0.93 ± 0.61 分和 0.54 ± 0.51分 (t = 6.59,P < 0.01和 t = 5.91,P < 0.01)。两组患者末次随访时VAS和DOI评分差异无统计学意义。所有患者手术节段ROM由术前平均(7.8±2.4)°保留至末次随访时的(4.5±1.5)° (t = 7.18,P < 0.05),近侧邻近节段ROM由术前的(8.3±2.4)°增加至末次随访时的(10.4±2.4)° (t = 2.87,P = 0.01)。手术节段椎间高度末次随访和术前相比差异无统计学意义(术前11.9 ± 2.1 mm vs. 12.5 ± 1.5 mm,t = 1.43,P = 0.15),近侧邻近节段椎间高度在末次随访时较术前显著降低(术前12.5 ± 2.0 mm vs. 术后11.0 ± 1.7 mm,t = 2.94,P = 0.01)。影像学和症状学ASD发生情况分别为16%(6/38)和3%(1/38)。
结论:
减压结合Dynesys动态固定系统治疗腰椎管狭窄症伴/不伴滑脱能够获得良好的长期临床疗效。腰椎管狭窄症伴或不伴I度滑脱,年龄小于60岁,腰椎间盘轻到中度退变是Dynesys动态固定系统的主要适应证之一。
INTRODUCTION
Decompression and spinal fusion are considered to be the gold standard for lumbar degenerative disease; however, the benefit of spinal fusion is associated with higher complications, such as significant instrumentation failure, infection, and accelerated degeneration of adjacent segments.[1,2,3] Dynamic stabilization is a potential alternative to rigid lumbar fusion for lumbar degenerative disease.[4]
The Dynesys Dynamic Stabilization System (Zimmer Inc., Warsaw, IN, USA) was introduced in 1994 as a posterior dynamic stabilization device.[5] Dynamic stabilization is an attempt to overcome the disadvantages of fusion and provide sufficient stability to restore normal segmental kinematics, prevent instability, and avoid adjacent segment degeneration (ASD). Many short-term follow-up studies have shown positive outcomes for lumbar spinal stenosis with or without spondylolisthesis;[6,7] however, long-term studies are limited.[8] Moreover, some recently published studies have reported contradictory results, indicating that Dynesys may not provide a significant advantage for outcomes.[9,10] This retrospective study presented a 6.6-year follow-up (range, 72–96 months) study of lumbar spinal stenosis treated with decompression and Dynesys stabilization.
METHODS
Ethical approval
This study was approved by the Institutional Review Board of Army General Hospital of Chinese People's Liberation Army with a waiver of informed consent for its retrospective nature.
Patient selection
This retrospective study included 45 consecutive patients who underwent decompression and Dynesys stabilization for lumbar spinal stenosis from July 2008 to March 2010. The symptoms included intermittent claudication, axial back pain, leg pain, or any combination of the above. All patients had at least three months of conservative treatment before surgery. Every patient underwent preoperative X-ray and magnetic resonance imaging (MRI) examinations. The patients were divided into stenosis and spondylolisthesis groups according to degenerative spondylolisthesis.
The inclusion criteria were degenerative lumbar spinal stenosis with or without Grade I spondylolisthesis and disc height >1/2 of the height of the average adjacent segments. The exclusion criteria were prior lumbar surgery, degenerative scoliosis >10°, disc height <1/2 of the height of the average adjacent segments, more than two levels of lumbar stenosis, severe osteoporosis (bone mineral density test T-score <−2.5), and severe spinal deformity.
Surgical technique
Dynesys stabilization was performed as an open procedure with a midline skin incision. After the midline incision and subperiosteal dissection of the erector spinae muscles, the facet joints and the entering points for the pedicle screws were exposed. The Dynesys conical titanium alloy pedicle screws were then placed transpedicularly without destruction of the facet joints, and the position of the screws was confirmed by the C-arm. Then, the ligamentum flavum was resected and the dura was exposed, after that a standard fenestration laminectomy was cautiously performed to achieve proper decompression of the spinal canal. For cases of severe stenosis or far lateral stenosis, extensive decompression was performed, during which the medial border of the superior facet was partially removed to provide a clear view of the involved nerve root.[11] After adequate decompression, the constructs, polycarbonate-urethane spacers, and tension cords then were assembled. Postoperatively, patients wore a soft lumbar brace for three months. After three months, patients were allowed to return to their normal activities without restriction.
Clinical outcome evaluations
The patients were reviewed after a minimum follow-up period of 72 months by an independent surgeon. Clinical outcomes were evaluated using the Oswestry Disability Index (ODI) and visual analog scale (VAS) for back and leg pain. VAS scores were determined on a scale ranging from 0 (no pain) to 10 (worst pain imaginable).
Radiographic evaluations
Plain radiographs (anteroposterior and lateral) and functional radiographs with flexion and extension lateral views were obtained preoperatively and at each follow-up visit using a digital picture archiving and communication system. On plain radiographs, the following variables were measured: segmental range of motion (ROM) and the disc heights of stabilized segments and the upper adjacent segments. Because ASD occurs frequently above the operated segment, we only evaluated the upper adjacent segments.[12] The segmental ROM was calculated as the difference between the segmental angulations in flexion and extension. The disc height was determined on lateral radiographs by calculating the mean of the anterior and posterior disc heights. The occurrence of radiographic and symptomatic ASD was also evaluated, as described in a previous study.[11] Implant failure, such as screw loosening (“double halo” sign on plain radiographs) or breakage, was also noted.[13]
Statistical analysis
Continuous variables were compared using an independent two-sample t-test and categorical variables were compared using a Chi-square test or Fisher's exact test. The results of improvement differences from baseline (preoperatively) to final follow-up evaluation were assessed using a paired t-test. All data were analyzed using SPSS 19.0 statistical software (IBM, Chicago, IL, USA). Statistical significance was set at a P < 0.05.
RESULTS
Thirty-eight patients, with a mean age of 53.4 years (range, 38.0–60.0 years), were available for evaluation after a mean follow-up time of 6.6 years (range, 72–96 months). Seven patients were lost to follow-up. Fifteen patients (40%) had degenerative spondylolisthesis, as determined by preoperative radiographic evaluation. Twenty-eight patients (74%) underwent one-level surgeries and 10 patients (26%) underwent two-level surgeries. There were no significant differences between the two groups when compared in terms of age, gender, follow-up time, and levels of surgeries. Patient demographic and baseline characteristics are shown in Table 1.
Table 1.
Demographic and baseline data of patients with lumbar spinal stenosis
| Variables | Total | Stenosis group (n = 23) | Spondylolisthesis group (n = 15) | Statistics | P |
|---|---|---|---|---|---|
| Age (years) | 53.4 ± 5.8 | 52.2 ± 6.1 | 55.3 ± 5.0 | 1.64* | 0.10 |
| Gender (male/female), n | 23/15 | 14/9 | 9/6 | 0.01† | 0.96 |
| Follow-up time (months) | 78.9 ± 6.9 | 79.0 ± 7.5 | 78.7 ± 6.0 | 0.13* | 0.90 |
| Operating levels, n | |||||
| Single level | 28 | 17 | 11 | 0.01† | 0.97 |
| Two levels | 10 | 6 | 4 | ||
| ROM (°) | |||||
| Stabilized segment | 7.8 ± 2.4 | 7.6 ± 2.5 | 8.2 ± 2.3 | 0.75* | 0.46 |
| The upper adjacent segment | 8.3 ± 2.4 | 8.6 ± 2.7 | 7.7 ± 2.0 | 1.11* | 0.28 |
| Disc height (mm) | |||||
| Stabilized segment | 11.9 ± 2.1 | 12.1 ± 2.1 | 11.7 ± 2.2 | 0.56* | 0.58 |
| Upper adjacent segment | 12.4 ± 1.8 | 12.4 ± 1.7 | 12.5 ± 2.1 | 0.16* | 0.87 |
| Surgical duration (min) | 120.3 ± 24.4 | 117.6 ± 26.6 | 124.3 ± 20.9 | 0.82* | 0.39 |
| Intraoperative blood loss (ml) | 279.2 ± 73.6 | 270.0 ± 82.2 | 293.3 ± 57.8 | 0.95* | 0.35 |
*Independent two-sample t-test; †Chi-square test. Values are presented as the mean ± standard deviation or n. ROM: Range of motion.
Preoperatively, there were no significant differences between groups in clinical outcomes (VAS and ODI) and radiographic measurements (ROM and disc heights). The operative time and intraoperative blood loss were similar in the stenosis group compared with the spondylolisthesis group [117.6 ± 26.6 min vs. 124.3 ± 20.9 min, P = 0.39, and 270.0 ± 82.2 ml vs. 293.3 ± 57.8 ml, P = 0.35, respectively; Table 1].
Clinical outcomes
The ODI scores were significantly improved at the final follow-up evaluation, as compared to the baseline values [16.1 ± 5.7 vs. 57. 2 ± 14.2, t = 61.41, P < 0.01; Table 2]. Specifically, the ODI scores were both significantly improved in the two groups at the final follow-up evaluation as compared to the baseline values, but the postoperative difference between the two groups was not significant [Table 2].
Table 2.
Clinical outcomes of the two groups of patients with lumbar spinal stenosis
| Groups | Preoperative | Postoperative | t | P |
|---|---|---|---|---|
| ODI (%) | ||||
| Total | 57.2 ± 14.2 | 16.1 ± 5.7 | 61.41 | <0.01 |
| Stenosis group | 54.4 ± 14.2* | 15.5 ± 5.5* | 50.31 | <0.01 |
| Spondylolisthesis group | 61.4 ± 13.7* | 16.9 ± 6.1* | 40.71 | <0.01 |
| VAS (back pain) | ||||
| Total | 4.82 ± 0.89 | 0.93 ± 0.61 | 6.59 | <0.01 |
| Stenosis group | 4.73 ± 0.71* | 0.90 ± 0.59* | 4.99 | <0.01 |
| Spondylolisthesis group | 5.01 ± 1.12* | 1.02 ± 0.73* | 3.66 | <0.01 |
| VAS (leg pain) | ||||
| Total | 4.04 ± 0.82 | 0.54 ± 0.51 | 5.91 | <0.01 |
| Stenosis group | 3.92 ± 0.78* | 0.52 ± 0.50* | 4.47 | <0.01 |
| Spondylolisthesis group | 4.18 ± 0.83* | 0.60 ± 0.51* | 3.30 | <0.01 |
Values are presented as the mean ± SD. *No significant difference preoperatively and at the final follow-up between the stenosis (n = 23) and spondylolisthesis (n = 15) groups using the independent two-sample t-test, P>0.05. SD: Standard deviation; ODI: Oswestry Disability Index; VAS: Visual analog scale.
The VAS scores for back and leg pain were significantly improved from 4.82 ± 0.89 and 4.04 ± 0.82 preoperatively to 0.93 ± 0.61 and 0.54 ± 0.51 postoperatively [t = 6.59, P < 0.01, and t = 5.91, P < 0.01, respectively; Table 2]. There were significant improvements in both groups with respect to VAS scores for back and leg pain; however, there were no significant differences in postoperative VAS for back and leg pain between the two groups [Table 2].
Radiographic outcomes
The ROM of stabilized segments decreased significantly from 7.8° ± 2.4° preoperatively to 4.5° ± 1.5° at the final follow-up evaluation [t = 7.18, P < 0.01; Table 3]. The ROM of the upper segments increased significantly from 8.3° ± 2.4° preoperatively to 10.4° ± 2.4° postoperatively [t = 2.87, P = 0.01; Table 3]. The changes in the ROM of stabilized and upper segments were similar in both groups at the final follow-up evaluation [Table 3]. There were no significant differences in the ROM of stabilized and upper segments between the two groups postoperatively [Table 3].
Table 3.
Radiographic outcomes of the two groups of patients with lumbar spinal stenosis
| Groups | Preoperative | Postoperative | t | P |
|---|---|---|---|---|
| ROM of stabilized segment (°) | ||||
| Total | 7.8 ± 2.4 | 4.5 ± 1.5 | 7.18 | <0.01† |
| Stenosis group | 7.6 ± 2.5* | 4.4 ± 1.5* | 4.20 | <0.01† |
| Spondylolisthesis group | 8.2 ± 2.3* | 4.7 ± 1.4* | 3.20 | <0.01† |
| ROM of the upper adjacent segment (°) | ||||
| Total | 8.3 ± 2.4 | 10.4 ± 2.4 | 2.87 | 0.01† |
| Stenosis group | 8.6 ± 2.7* | 10.7 ± 2.5* | 2.76 | 0.01† |
| Spondylolisthesis group | 7.7 ± 2.0* | 10.1 ± 2.2* | 2.20 | 0.01† |
| Disc height of stabilized segment (mm) | ||||
| Total | 11.9 ± 2.1 | 12.5 ± 1.5 | 1.43 | 0.15 |
| Stenosis group | 12.0 ± 2.1* | 12.4 ± 1.4* | 0.53 | 0.45 |
| Spondylolisthesis group | 11.7 ± 2.2* | 12.6 ± 1.8* | 0.82 | 0.23 |
| Disc height of the upper adjacent segment (mm) | ||||
| Total | 12.5 ± 2.0 | 11.0 ± 1.7 | 2.94 | 0.01† |
| Stenosis group | 12.4 ± 1.8* | 11.0 ± 1.6* | 2.56 | 0.01† |
| Spondylolisthesis group | 12.6 ± 2.3* | 10.9 ± 1.6* | 2.35 | 0.03† |
Values are presented as the mean ± SD. *No significant difference preoperatively and at the final follow-up between the stenosis (n = 23) and spondylolisthesis (n = 15) groups using the independent two-sample t-test, P>0.05; †Significant difference between pre- and post-operative condition in each group using the paired t-test. ROM: Range of motion; SD: Standard deviation.
The disc heights of stabilized segments increased slightly from 11.9 ± 2.1 mm preoperatively to 12.5 ± 1.5 mm postoperatively (t = 1.43, P = 0.15), and the changes were similar in both groups at the final follow-up evaluation [Table 3]. The disc heights of the upper segments decreased significantly from 12.5 ± 2.0 mm preoperatively to 11.0 ± 1.7 mm postoperatively [t = 2.94, P = 0.01; Table 3]. The decreases in disc heights of the upper segments were significant in both groups at the final follow-up evaluation [12.4 ± 1.8 mm preoperatively vs. 11.0 ± 1.6 mm postoperatively, t = 2.56, P = 0.01, and 12.6 ± 2.3 mm preoperatively vs. 10.9 ± 1.6 mm postoperatively, t = 2.35, P = 0.03, respectively; Table 3]; however, the difference was not significant between the two groups at the final follow-up evaluation [Table 3].
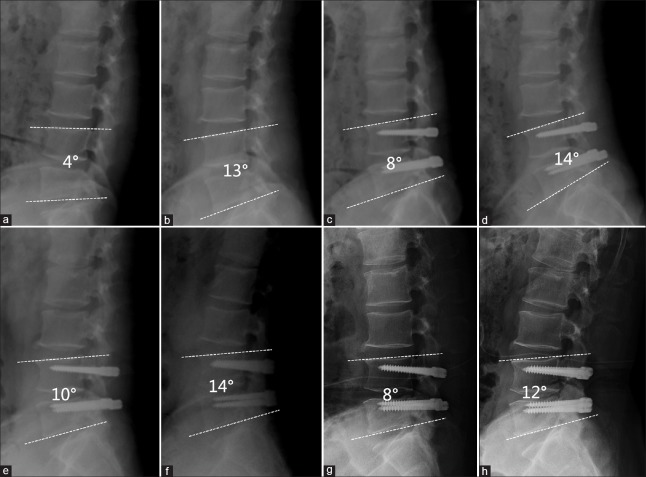
The occurrence of radiographic ASDs was 16% (6/38) after 6.6 years of follow-up. Specifically, there were both three radiographic ASDs in each group at the final follow-up evaluation; the difference was not significant (χ2= 0.33, P = 0.57). Only one symptomatic ASD (3% [1/38]) occurred in the stenosis group; the patient underwent a second surgical procedure 18 months postoperatively. The radiographs and MRI of a typical patient are shown in Figure 1.
Figure 1.
The radiological data of a patient with lumbar spinal stenosis without spondylolisthesis. A 53-year-old male patient underwent Dynesys stabilization due to lumbar spinal stenosis in L4/5. (a and b) The preoperative flexion and extension X-rays, the ROM of L4/5 was 9°; (c and d) the flexion and extension X-rays 3 months postoperatively, the ROM of L4/5 was 6°; (e and f) the flexion and extension X-rays 48 months postoperatively, the ROM of L4/5 was 4°; (g and h) the flexion and extension X-rays 96 months postoperatively, the ROM of L4/5 was also 4°. ROM: Range of motion.
Complications
There was screw loosening without clinical symptoms in 6 of 38 patients (16%) and 7 of 172 screws (4%). There were no significant differences in the occurrence of screw loosening in patients between the stenosis and spondylolisthesis groups (3 vs. 3, χ2= 0.33, P = 0.57, and 4 vs. 3, χ2= 0.04, P = 0.85, respectively). There was no screw breakage or other complications in either group at the final follow-up evaluation.
DISCUSSION
Only a few long-term studies focusing on the use of Dynesys stabilization for lumbar spinal stenosis with or without spondylolisthesis have been published. The current study indicated that Dynesys stabilization, in combination with decompression for lumbar spinal stenosis with or without spondylolisthesis, yielded good long-term outcomes. The clinical and radiographic results were similar in both groups with or without spondylolisthesis at the final follow-up evaluation.
In recent years, ASD has become a relatively common complication of lumbar fusion. Moreover, clinical ASD due to spinal stenosis involving the adjacent segments potentially requires re-operation.[14] Preservation of the ROM at the stabilized segment could prevent ASD by decreasing stress and preventing hypermobility.[15] The Dynesys system is a dynamic stabilization system that is used worldwide for lumbar degenerative diseases, such as disk herniation,[16] degenerative spondylolisthesis,[8,17,18] spinal stenosis,[19,20,21] degenerative scoliosis,[22,23] and mixed indications.[11,24,25]
Most studies have indicated favorable clinical outcomes for patients treated with the Dynesys system.[5,6,7,8,9,11,15,16,17,18,23,25,26] A meta-analysis[27] compared the clinical and radiologic outcomes between the Dynesys system and posterior lumbar interbody fusion (PLIF) and indicated that lumbar degenerative disease with or without Grade I spondylolisthesis, particularly in patients who require a quicker recovery, would likely constitute the main indication for the Dynesys system. The present study included patients <60 years of age with mild-to-moderate lumbar disc degeneration (disc height >1/2 the height of the average adjacent segments). The results showed that, at a mean follow-up duration of 6.6 years, the ODI and VAS scores for low back and leg pain in groups with or without spondylolisthesis were significantly improved compared to the baseline scores. This finding was in agreement with previously published data.[8,17,18] We therefore concluded that Dynesys stabilization is an acceptable alternative to PLIF for the treatment of lumbar stenosis.
Although the Dynesys system was designed to preserve motion of stabilized segments and prevent degeneration at the adjacent segments by decreasing stress and preventing hypermobility, it is still controversial whether or not dynamic stabilization can prevent the occurrence of ASD. A number of studies have indicated that the Dynesys system can preserve the ROM of the operated segments[9,11,28,29,30] and prevent radiographic ASD;[9,11,31] however, some studies showed negative radiographic results with long-term follow-up.[10,20,24] The severity of diseases included in these studies was relatively severe and the age of the patients was relatively advanced, especially in the St-Pierre study,[10] in which no patient was excluded based on age; the average age was 76.7 years, 19 patients were in their 80s, and 1 patient was 91 years old at the time of surgery. Of the patients, 15.4% (8/52) had prior ASD and 25% (13/52) had previous spine surgery, which may be relative contraindications for Dynesys stabilization. This study showed that Dynesys was associated with a high rate of ASD over long-term follow-up, despite maintaining a low fusion rate; however, this conclusion should be considered with caution. The authors also indicated that the patients were selected on the basis of having a presumed higher risk of ASD, likely resulting in an increased incidence of clinical ASD. It is entirely possible that a fusion procedure in that context would have yielded an even higher rate of clinical ASD.
A recent systematic review suggested relative success of the posterior dynamic stabilization in protecting against ASD and disease.[32] Bredin et al.[9] reported that at a minimum follow-up duration of 5.5 years, radiologic ASD was significantly greater in the fusion group than the Dynesys group (36.0% vs. 12.1%, P = 0.01). The current study showed that Dynesys stabilization partially preserved the ROM of stabilized segments from 7.8° ± 2.4° preoperatively to 4.5° ± 1.5° at the final follow-up evaluation. The occurrence of radiographic ASD was 15.8% (6/38) and that of symptomatic ASD was 2.6% (1/38). The occurrence rate was much lower in comparison with reports of fusion in the literature,[14] in which the occurrence of radiographic and symptomatic ASD was 26.5% and 8.5%, respectively.
Screw loosening is one of the most frequently reported complications following Dynesys stabilization.[33] A previous long-term follow-up study reported that the occurrence of screw loosening was 20.5% (22/107), and three patients underwent re-operations.[34] In the present study, the screw-loosening rate was 15.7% (6/38) in patients and 4.1% (7/172) for screws; however, there were no clinical symptoms in the patients with screw loosening. This finding might be due to the long-term repetitive high demands on construct durability and mechanical strength for the Dynesys system. There was no screw breakage and other complications at the final follow-up evaluation.
In conclusion, decompression and Dynesys stabilization for lumbar stenosis with or without spondylolisthesis showed good long-term clinical and radiographic results. The lumbar canal stenosis with or without Grade I spondylolisthesis, particularly in patients <60 years of age with mild-to-moderate lumbar disc degeneration, would be one of the main indications for the Dynesys system.
Financial support and sponsorship
This work was supported by a grant from the Youth Project of the “Twelfth Five-year Plan” for Medical Science Development of Chinese People's Liberation Army (No. 13QNP010).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Shao Guo
REFERENCES
- 1.Puvanesarajah V, Cancienne JM, Werner BC, Jain A, Singla A, Shimer AL, et al. Perioperative complications associated with posterolateral spine fusions: A Study of elderly medicare beneficiaries. Spine (Phila Pa 1976) 2018;43:16–21. doi: 10.1097/BRS.0000000000001771. doi: 10.1097/BRS.0000000000001771. [DOI] [PubMed] [Google Scholar]
- 2.Gu W, Tu L, Liang Z, Wang Z, Aikenmu K, Chu G, et al. Incidence and risk factors for infection in spine surgery: A prospective multicenter study of 1764 instrumented spinal procedures. Am J Infect Control. 2018;46:8–13. doi: 10.1016/j.ajic.2017.09.025. doi: 10.1016/j.ajic.2017.09.025. [DOI] [PubMed] [Google Scholar]
- 3.Ghasemi AA. Adjacent segment degeneration after posterior lumbar fusion: An analysis of possible risk factors. Clin Neurol Neurosurg. 2016;143:15–8. doi: 10.1016/j.clineuro.2016.02.004. doi: 10.1016/j.clineuro.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Prud’homme M, Barrios C, Rouch P, Charles YP, Steib JP, Skalli W, et al. Clinical outcomes and complications after pedicle-anchored dynamic or hybrid lumbar spine stabilization: A Systematic literature review. J Spinal Disord Tech. 2015;28:E439–48. doi: 10.1097/BSD.0000000000000092. doi: 10.1097/BSD.0000000000000092. [DOI] [PubMed] [Google Scholar]
- 5.Fayyazi AH, Ordway NR, Park SA, Fredrickson BE, Yonemura K, Yuan HA, et al. Radiostereometric analysis of postoperative motion after application of dynesys dynamic posterior stabilization system for treatment of degenerative spondylolisthesis. J Spinal Disord Tech. 2010;23:236–41. doi: 10.1097/BSD.0b013e3181a4bb0b. doi: 10.1097/BSD.0b013e3181a4bb0b. [DOI] [PubMed] [Google Scholar]
- 6.Hu Y, Gu YJ, Xu RM, Zhou LJ, Ma WH. Short-term clinical observation of the dynesys neutralization system for the treatment of degenerative disease of the lumbar vertebrae. Orthop Surg. 2011;3:167–75. doi: 10.1111/j.1757-7861.2011.00142.x. doi: 10.1111/j.1757-7861.2011.00142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li HP, Li F, Guan K, Zhao GM, Shan JL, Sun TS, et al. Dynesys dynamic stabilization system for the lumbar degenerative disease: A preliminary report from China. Chin Med J. 2013;126:4265–9. doi: 10.3760/cma.j.issn.0366-6999.20121013. [PubMed] [Google Scholar]
- 8.Hoppe S, Schwarzenbach O, Aghayev E, Bonel H, Berlemann U. Long-term outcome after monosegmental L4/5 stabilization for degenerative spondylolisthesis with the dynesys device. Clin Spine Surg. 2016;29:72–7. doi: 10.1097/BSD.0b013e318277ca7a. doi: 10.1097/BSD.0b013e318277ca7a. [DOI] [PubMed] [Google Scholar]
- 9.Bredin S, Demay O, Mensa C, Madi K, Ohl X. Posterolateral fusion versus dynesys dynamic stabilization: Retrospective study at a minimum 5.5 years’ follow-up. Orthop Traumatol Surg Res. 2017;103:1241–4. doi: 10.1016/j.otsr.2017.07.020. doi: 10.1016/j.otsr.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 10.St-Pierre GH, Jack A, Siddiqui MM, Henderson RL, Nataraj A. Nonfusion does not prevent adjacent segment disease: Dynesys long-term outcomes with minimum five-year follow-up. Spine (Phila Pa 1976) 2016;41:265–73. doi: 10.1097/BRS.0000000000001158. doi: 10.1097/BRS.0000000000001158. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Y, Shan JL, Liu XM, Li F, Guan K, Sun TS, et al. Comparison of the dynesys dynamic stabilization system and posterior lumbar interbody fusion for lumbar degenerative disease. PLoS One. 2016;11:e0148071. doi: 10.1371/journal.pone.0148071. doi: 10.1371/journal.pone.0148071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hikata T, Kamata M, Furukawa M. Risk factors for adjacent segment disease after posterior lumbar interbody fusion and efficacy of simultaneous decompression surgery for symptomatic adjacent segment disease. J Spinal Disord Tech. 2012;27:70–5. doi: 10.1097/BSD.0b013e31824e5292. doi: 10.1097/BSD.0b013e31824e5292. [DOI] [PubMed] [Google Scholar]
- 13.Dakhil-Jerew F, Jadeja H, Cohen A, Shepperd JA. Inter-observer reliability of detecting dynesys pedicle screw using plain X-rays: A study on 50 post-operative patients. Eur Spine J. 2009;18:1486–93. doi: 10.1007/s00586-009-1071-0. doi: 10.1007/s00586-009-1071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xia XP, Chen HL, Cheng HB. Prevalence of adjacent segment degeneration after spine surgery: A systematic review and meta-analysis. Spine (Phila Pa 1976) 2013;38:597–608. doi: 10.1097/BRS.0b013e318273a2ea. doi: 10.1097/BRS.0b013e318273a2ea. [DOI] [PubMed] [Google Scholar]
- 15.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: A multi-center study of a novel non-fusion system. Eur Spine J. 2002;11(Suppl 2):S170–8. doi: 10.1007/s00586-002-0438-2. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu C, Wang L, Tian JW. Early clinical effects of the dynesys system plus transfacet decompression through the wiltse approach for the treatment of lumbar degenerative diseases. Med Sci Monit. 2014;20:853–9. doi: 10.12659/MSM.890292. doi: 10.12659/MSM.890292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976) 2008;33:E636–42. doi: 10.1097/BRS.0b013e31817d2435. doi: 10.1097/BRS.0b013e31817d2435. [DOI] [PubMed] [Google Scholar]
- 18.Fay LY, Wu JC, Tsai TY, Wu CL, Huang WC, Cheng H, et al. Dynamic stabilization for degenerative spondylolisthesis: Evaluation of radiographic and clinical outcomes. Clin Neurol Neurosurg. 2013;115:535–41. doi: 10.1016/j.clineuro.2012.05.036. doi: 10.1016/j.clineuro.2012.05.036. [DOI] [PubMed] [Google Scholar]
- 19.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the dynesys semirigid fixation system for the lumbar spine: Surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976) 2005(30):324–31. doi: 10.1097/01.brs.0000152584.46266.25. doi: 10.1097/01.brs.0000152584.46266.25. [DOI] [PubMed] [Google Scholar]
- 20.Cakir B, Carazzo C, Schmidt R, Mattes T, Reichel H, Käfer W, et al. Adjacent segment mobility after rigid and semirigid instrumentation of the lumbar spine. Spine (Phila Pa 1976) 2009(34):1287–91. doi: 10.1097/BRS.0b013e3181a136ab. doi: 10.1097/BRS.0b013e3181a136ab. [DOI] [PubMed] [Google Scholar]
- 21.Würgler-Hauri CC, Kalbarczyk A, Wiesli M, Landolt H, Fandino J. Dynamic neutralization of the lumbar spine after microsurgical decompression in acquired lumbar spinal stenosis and segmental instability. Spine (Phila Pa 1976) 2008(33):E66–72. doi: 10.1097/BRS.0b013e31816245c0. doi: 10.1097/BRS.0b013e31816245c0. [DOI] [PubMed] [Google Scholar]
- 22.Di Silvestre M, Lolli F, Bakaloudis G, Parisini P. Dynamic stabilization for degenerative lumbar scoliosis in elderly patients. Spine (Phila Pa 1976) 2010(35):227–34. doi: 10.1097/BRS.0b013e3181bd3be6. doi: 10.1097/BRS.0b013e3181bd3be6. [DOI] [PubMed] [Google Scholar]
- 23.Lee SE, Jahng TA, Kim HJ. Decompression and nonfusion dynamic stabilization for spinal stenosis with degenerative lumbar scoliosis: Clinical article. J Neurosurg Spine. 2014;21:585–94. doi: 10.3171/2014.6.SPINE13190. doi: 10.3171/2014.6.SPINE13190. [DOI] [PubMed] [Google Scholar]
- 24.Haddad B, Makki D, Konan S, Park D, Khan W, Okafor B, et al. Dynesys dynamic stabilization: Less good outcome than lumbar fusion at 4-year follow-up. Acta Orthop Belg. 2013;79:97–103. [PubMed] [Google Scholar]
- 25.Yu SW, Yang SC, Ma CH, Wu CH, Yen CY, Tu YK, et al. Comparison of dynesys posterior stabilization and posterior lumbar interbody fusion for spinal stenosis L4L5. Acta Orthop Belg. 2012;78:230–9. [PubMed] [Google Scholar]
- 26.Kuo CH, Chang PY, Wu JC, Chang HK, Fay LY, Tu TH, et al. Dynamic stabilization for L4-5 spondylolisthesis: Comparison with minimally invasive transforaminal lumbar interbody fusion with more than 2 years of follow-up. Neurosurg Focus. 2016;40:E3. doi: 10.3171/2015.10.FOCUS15441. doi: 10.3171/2015.10.FOCUS15441. [DOI] [PubMed] [Google Scholar]
- 27.Lee CH, Jahng TA, Hyun SJ, Kim CH, Park SB, Kim KJ, et al. Dynamic stabilization using the dynesys system versus posterior lumbar interbody fusion for the treatment of degenerative lumbar spinal disease: A clinical and radiological outcomes-based meta-analysis. Neurosurg Focus. 2016;40:E7. doi: 10.3171/2015.10.FOCUS15426. doi: 10.3171/2015.10.FOCUS15426. [DOI] [PubMed] [Google Scholar]
- 28.Wu H, Pang Q, Jiang G. Medium-term effects of dynesys dynamic stabilization versus posterior lumbar interbody fusion for treatment of multisegmental lumbar degenerative disease. J Int Med Res. 2017;45:1562–73. doi: 10.1177/0300060517708104. doi: 10.1177/0300060517708104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang C, Wang L, Hou T, Luo L, Zhao C, Gan Y, et al. The influence of L4-S1 dynesys® dynamic stabilization versus fusion on lumbar motion and its relationship with lumbar degeneration: A retrospective study. J Orthop Surg Res. 2017;12:99. doi: 10.1186/s13018-017-0597-9. doi: 10.1186/s13018-017-0597-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fei H, Xu J, Wang S, Xie Y, Ji F, Xu Y, et al. Comparison between posterior dynamic stabilization and posterior lumbar interbody fusion in the treatment of degenerative disc disease: A prospective cohort study. J Orthop Surg Res. 2015;10:87. doi: 10.1186/s13018-015-0231-7. doi: 10.1186/s13018-015-0231-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Putzier M, Hoff E, Tohtz S, Gross C, Perka C, Strube P, et al. Dynamic stabilization adjacent to single-level fusion: Part II. No clinical benefit for asymptomatic, initially degenerated adjacent segments after 6 years follow-up. Eur Spine J. 2010;19:2181–9. doi: 10.1007/s00586-010-1517-4. doi: 10.1007/s00586-010-1517-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou ZJ, Xia P, Zhao X, Fang XQ, Zhao FD, Fan SW, et al. Can posterior dynamic stabilization reduce the risk of adjacent segment deterioration? Turk Neurosurg. 2013;23:579–89. doi: 10.5137/1019-5149.JTN.6573-12.1. doi: 10.5137/1019-5149.JTN.6573-12.1. [DOI] [PubMed] [Google Scholar]
- 33.Pham MH, Mehta VA, Patel NN, Jakoi AM, Hsieh PC, Liu JC, et al. Complications associated with the dynesys dynamic stabilization system: A comprehensive review of the literature. Neurosurg Focus. 2016;40:E2. doi: 10.3171/2015.10.FOCUS15432. doi: 10.3171/2015.10.FOCUS15432. [DOI] [PubMed] [Google Scholar]
- 34.Sapkas G, Mavrogenis AF, Starantzis KA, Soultanis K, Kokkalis ZT, Papagelopoulos PJ, et al. Outcome of a dynamic neutralization system for the spine. Orthopedics. 2012;35:e1497–502. doi: 10.3928/01477447-20120919-19. doi: 10.3928/01477447-20120919-19. [DOI] [PubMed] [Google Scholar]