Abstract
Purpose of Review:
Alcohol and drug use are common among youth. Rates are especially high among sexual and gender minority youth (SGMY; lesbian, gay, bisexual, transgender). We conducted a scoping review of research on risk and protective factors for substance use among SGMY published between 2013–2017.
Recent Findings:
Ninety-seven studies met our inclusion criteria. Most focused on individual-level minority stress risk factors, particularly stigma. Fewer studies addressed protective factors such as social support or affirming policies, and few focused on gender minority youth (GMY). We identified important, yet understudied differences by race/ethnicity, sex assigned at birth, and sexual orientation.
Summary:
Findings highlight growing interest in this topic as well as methodological/topical gaps in the literature. Research is needed to examine SGMY substance use in nationally representative samples; expand information about GMY; investigate racial/ethnic and sex/gender differences; improve measurement; and increase translation of findings to support prevention and treatment interventions for this at-risk population.
Keywords: Sexual minority, gender minority, substance use, alcohol, drug, youth
INTRODUCTION
Substance use is a major public health concern in the United States (US) and globally. The World Health Organization [1] estimates that alcohol, tobacco, and drug use contributed to 12.4% of deaths globally in 2000, and 2002–2030 projections by the Global Burden of Disease Project [2] estimate that five of the six fastest growing causes of global mortality are related to substance use. Many individuals begin using alcohol and drugs in adolescence [3], with 20% of adults with a substance use disorder having begun use before age 20 [4]. In the 2015 Youth Risk Behavior Surveillance System (YRBSS) survey of US 9th to 12th graders, 63.2% reported lifetime alcohol use (17.2% before age 13), 32.8% reported past-month alcohol consumption, 38.6% had used cannabis, and 16.8% reported prescription drug misuse [5].
Adolescence and young adulthood are also periods of identity exploration and consolidation, including sexual orientation and gender identity [6], which may confer additional risk. In this scoping review, we focus on risk and protective factors for alcohol and drug use among sexual and gender minority youth (SGMY)—a term that includes both sexual minority youth (SMY; e.g., lesbian, gay, bisexual, queer) and gender minority youth (GMY; e.g., transgender, genderqueer) as well as youth who are unsure of their sexual orientation and/or gender identity. We use the terms heterosexual and cisgender (individuals whose sex assigned at birth and current gender identity align) to describe individuals who are not SMY or GMY, respectively.
In 2011, the Institute of Medicine (now the National Academies of Medicine) [7] published its landmark report on sexual and gender minority health and concluded that SMY individuals face multiple health disparities beginning in childhood (e.g., suicidality, family rejection, homelessness, victimization, psychological distress). The 2015 YRBSS [5] found further evidence of alcohol and drug use disparities among SMY as compared to heterosexual youth. Although there is notably less research about GMY, existing findings suggest that this group is also at greater risk of heavy episodic drinking (HED), negative alcohol-related consequences, and drug use [8, 9]. Bisexual and questioning youth may be at particularly high risk for hazardous drinking and drug use [10]. Other demographic factors such as race/ethnicity and sex assigned at birth may impact substance use among SGMY. In some studies, racial/ethnic minority SMY have reported similar or lower rates of lifetime alcohol [11, 12] and drug use [13, 14], compared to White SMY. In analyses using YRBSS data, Talley et al [12] found multiple significant interaction effects between sexual orientation and sex, indicating larger alcohol-use disparities among young sexual minority women (SMW) than young sexual minority men (SMM). Adolescent (high-school age) SMW also reported higher rates of lifetime alcohol use and past-month HED than adolescent SMM, heterosexual girls, or heterosexual boys. Reducing these alcohol and drug use disparities among SGMY requires understanding risk and protective factors relevant to this particular population.
METHODS
We conducted a scoping review using the following research question: “What risk and protective factors are associated with alcohol and drug use among SGMY?” Scoping reviews are well-suited for broad topics areas that contain primarily emerging literature. Such reviews differ from systematic reviews in that they aim to broadly describe trends and gaps in a particular literature [15], rather than rigorously critiquing study methodology.
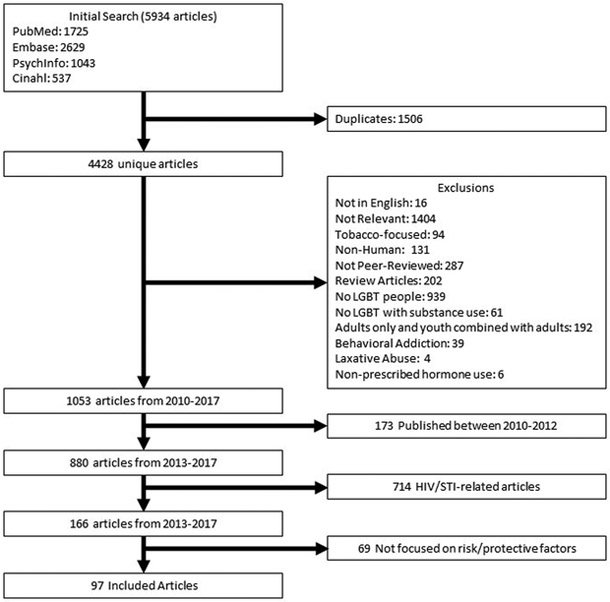
Figure 1 illustrates the literature search and article screening process. In September 2017, we searched four databases to identify articles: PubMed [16], PsycInfo [17], Embase [18], and CINAHL [19]. We initially focused on articles published between 2010–2017 by combining three clusters (sexual orientation/gender identity, alcohol/drug, and youth) of search terms and subject headings (e.g., MeSH terms) (see Appendix A). This resulted in 4428 unique references. Next, we reviewed each article and selected those that were peer-reviewed, written in English, and focused on alcohol and/or drug use among SGMY using quantitative or qualitative methods. In keeping with the United Nations research definition of “youth,” we excluded articles focusing on individuals over age 24 [20]. We excluded articles focused on nicotine and tobacco use, behavioral addictions (e.g., gambling disorder), laxative abuse, or non-prescribed hormone use. Given the volume of relevant articles published between 2010–2017 (n=1053), we further restricted our review to the more recent publication years 2013–2017. We also excluded articles related to HIV/STI transmission (the topic of the large majority of SGMY research [21]). Finally, we excluded all articles not related to risk or protective factors (e.g., those that focused on prevalence). This resulted in 97 articles. Consistent with Arskey and O’Malley [22], we extracted information about methodology and key findings from each of the 97 articles to produce a thematic analysis of recent literature. We paid special attention to methodologic trends, the range and scope of findings, and gaps in the literature.
Figure 1.
Literature search and article screening process.
RESULTS
Table 1 summarizes study design characteristics and measurement of sexual orientation and gender identity in the 97 studies. Table 2 summarizes the alcohol and drug-related measures used. Below, we first summarize findings related to substance use generally, followed by separate summaries of alcohol and drug use findings. We then describe risk and protective factors for GMY and adolescent (high-school age) SMY. Finally, we comment on racial/ethnic- and sex-specific findings.
Table 1.
Study design, sample characteristics, and measures of sexual orientation and gender identity in the 97 articles reviewed.
| STUDY DESIGN AND SAMPLE CHARACTERISTICS | |
|---|---|
| Category | # of Articles (% of total n=97) |
| Samplea | |
| Representative/Population-Based | 29 (29.9) |
| Convenience | 63 (64.9) |
| Other | 8 (8.2) |
| Study Design | |
| Cross-sectional | 75 (77.3) |
| Longitudinal | 21 (21.6) |
| Other | 1 (1.0) |
| Separated findings by sex/gender | |
| Young SMM | 36 (37.1) |
| Young SMW | 22 (22.7) |
| Transfeminine GMY | 5 (5.1) |
| Transfeminine GMY | 2 (2.1) |
| Examined differences among SGMY by sex/gender | 32 (33.0) |
| Examined difference among SGMY by race/ethnicity | 20 (20.6) |
| Non-US based | 14 (14.4) |
| Included findings for adolescent (high-school age) groups | 37 (38.1) |
| SEXUAL ORIENTATION & GENDER IDENTITY MEASURES | |
| Category | # of Articles (% of total n=97) |
| Domains of sexual orientationa | |
| Sexual identity | 75 (77.3) |
| Sexual attraction | 22 (22.7) |
| Sexual behavior | 30 (30.9) |
| Assessed gender identity | 23 (23.7) |
| Assessed gender identity using both current identity and sex-assigned-at-birth | 5 (5.1) |
| Combined all SMY in the analysis (e.g., LGB) | 51 (52.6) |
| Combined all SGMY in the analysis (e.g., LGBT) | 10 (10.3) |
| Examined differences by SMY identity (e.g., lesbian vs gay vs bisexual) | 31 (31.9) |
| Presented risk/protective factors separately for GMY | 9 (9.3) |
| Single sex/gender samples | 41 (42.3) |
| Included a heterosexual (vs SMY) or cisgender (vs GMY) comparison group | 46 (47.4) |
Some studies used more than one sampling strategy or measured multiple domains of sexual orientation, therefore column frequencies and percentages do not add up to 97 or 100%, respectively.
Table 2.
Alcohol and drug use measures in the 97 studies included in the scoping review.
| ALCOHOL USE (n=77; 79.4% of articles reviewed) | |||||
|---|---|---|---|---|---|
| Category | # articles (% total alcohol articles n=77) | ||||
| Time-frame of frequency measure | |||||
| Lifetime | 7 (9.1) | ||||
| Past-year | 23 (29.9) | ||||
| Past 30-days | 28 (36.4) | ||||
| Other | 34 (44.1) | ||||
| Type of alcohol use assessed | |||||
| Heavy episodic drinking | 37 (48.0) | ||||
| Risky drinking (NIAAA criteria* or validated measure) | 20 (26.0) | ||||
| Alcohol-related consequences | 14 (18.2) | ||||
| DSM-IV alcohol use disorder | 1 (1.3) | ||||
| Method for measuring use | |||||
| Self-report | 77 (100) | ||||
| Other | 0 | ||||
| DRUG USE (n=66; 68.0% of articles reviewed) | |||||
| Category | (# Articles; % total drug articles n=66) | Time Frame Assessed (# Articles) | |||
| Lifetime | Past-Year | Past 30-days | Other | ||
| Drug use | 19 (28.8) | 4 | 4 | 3 | 8 |
| Non-cannabis drug use | 16 (24.2) | 4 | 4 | 3 | 5 |
| Cannabis | 37 (56.1) | 3 | 8 | 14 | 12 |
| Cocaine (crack or powder) | 15 (22.7) | 6 | 3 | 3 | 3 |
| Benzodiazepines | 5 (7.6) | 3 | 0 | 0 | 2 |
| Amphetamines/Methamphetamine | 14 (21.2) | 7 | 4 | 1 | 2 |
| MDMA/GHB/Ketamine | 12 (18.2) | 5 | 2 | 2 | 3 |
| Hallucinogens | 6 (9.1) | 2 | 2 | 1 | 1 |
| Inhalants (including poppers) | 8 (12.1) | 4 | 1 | 2 | 1 |
| Opioids (heroin, oxycodone, etc) | 12 (18.2) | 7 | 3 | 0 | 2 |
| General prescription drug misuse | 18 (27.3) | 3 | 3 | 3 | 9 |
| Anabolic steroids | 5 (7.6) | 4 | 0 | 0 | 1 |
| Method for assessing drug use | # of articles (% of total drug articles n=66) | ||||
| Self-report measure | 66 (100) | ||||
| Other | 0 (0) | ||||
Note: Column percentages do not add to 100% because some studies used more than one time-frame or measured more than one drug.
NIAAA Risky Drinking Criteria: For men, more than four drinks in a single day or more than 14 in a week. For women, more than three drinks in a single day or more than six in a week.
Substance Use Findings: Minority Stress Predictors Predominate the Literature
Over one-third (n=35; 36.1%) of the articles examined minority stress [23] as a predictor of substance use. Enacted stigma (e.g., assault, homophobia, discrimination) and anti-SMY policies were directly associated with overall substance use [24–30] and adverse substance use-related outcomes such as family conflict, car accidents, and legal consequences [11, 31]. School-based victimization was associated with heavier and more frequent substance use-related consequences [32], an association that was partially explained by differences in peers’ substance use norms. Studies that measured multiple sources of victimization reported mixed findings [33, 34], with familial factors potentially accounting for sexual identity differences in the association between victimization and substance use [34]. One study [35] also found that substance use was indirectly associated with prior suicide attempts via a three-way interaction of substance use with depressive and post-traumatic stress disorder (PTSD) symptoms.
Alcohol Use Findings: SMY
Seventy-seven studies (79.4%) examined alcohol use and these primarily focused on individual-level risk factors. Enacted stigma [24–26, 36–38] and perceived homophobia [39] generally predicted elevated rates of alcohol use [24–26] and adverse alcohol-related outcomes [11]. Intimate partner violence (IPV) was also associated with greater odds for alcohol use among adolescent SMM [40]. Generalized anxiety disorder, which has been associated with trauma [41–43], also predicted weekly alcohol consumption among college-age SMW [44]. Findings related to felt stigma (e.g., internalized homophobia, concealment, rejection sensitivity) and alcohol use were more mixed, particularly for adolescent SMM [26, 45].
Several factors were protective against risky alcohol use, including higher educational attainment [46], school engagement [47], and earlier SMY self-identification [48]. Adaptive personality traits (e.g., being ambitious, open to new experiences, less narcissistic) mitigated the adverse relationship between discrimination and alcohol misuse among SMY [49]. At least one study [38] found that connection to the sexual minority community was protective, while other studies either only found this association among a subset of SMY (e.g., gay-identified youth) or found no association at all [50, 51, 45, 52]. This inconsistency in findings may be partially explained by differences in peer group drinking norms [50, 53]. Parental attachment moderated the relationship between bisexual identity and HED risk in at least one study [10]. Finally, SMY-affirming structural factors (i.e., school-based Gay-Straight Alliances and anti-bullying policies) played a protective role and were associated with lower alcohol consumption among both SMY and heterosexual youth [31, 54, 55].
Drug Use Findings: SMY
Drug-related studies (n=66; 68.0%) similarly focused on individual-level risk and protective factors from a minority stress point of view. Enacted stigma predicted increased cocaine, methamphetamine, heroin, injection drug [24], and cannabis [56] use among SMY, and stimulant misuse among adolescent SMM [28]. Physical victimization and bullying were important risk factors [24, 25, 57]. For example, anti-SMY bullying predicted increased risk for anabolic steroid use among adolescent SMM [58], a group already at greater risk for steroid use than heterosexual adolescents [59]. Ioerger et al [60] also found that gender-variance-based victimization was associated with “other” drug use among both cisgender SMY and cisgender heterosexual adolescents, when controlling for sexual attraction. IPV had a more complicated relationship with drug use. Two studies [61, 62] found no association. However, Stults et al. [40] found that IPV victimization and perpetration were associated with significantly greater odds of cannabis, stimulant, and other drug use among adolescent SMM. Further, the longer-term sequelae of victimization may predict substance use; adolescent SMW with higher levels of PTSD symptoms reported more frequent cannabis use than adolescent girls with lower-level symptomatology [63].
Felt stigma was also associated with drug use. Perceived homophobia predicted significantly higher levels of overall drug use [39] and club drug dependence among SMY [64] and opioid/sedative misuse among adolescent SMM [28]. In contrast and counter-intuitively, one study [64] found that internalized homophobia was associated with less club drug use among SMY.
Several factors were protective against SMY drug use including higher socioeconomic status [65], school connectedness [66], and higher self-esteem [67]. In fact, school enrollment itself predicted less past-3-month drug use in a predominantly Black and Latino SMY sample [68]. At the individual level, Wang et al [69] found that inhaled nitrite (poppers) use was inversely related to Health Belief Model [70] constructs of perceived drug-use severity and perceived self-efficacy and directly related to perceived barriers to reducing use among Chinese young SMM. Parental attachment moderated cannabis risk among bisexual youth [10] and was associated with reduced overall drug use among Chinese young SMM involved in sex work [71]. In contrast, SMY community connectedness did not mitigate general drug use disparities [50, 51, 72, 52, 45], possibly due to differences in peer drug use norms [51]. Finally, policies at the state (e.g., employment non-discrimination; marriage equality) and school levels (e.g., anti-bullying) were associated with lower rates of both general drug and cannabis use [27], and drug-related consequences [31].
Substance Use among Gender Minority Youth (GMY): A Gap in the Literature
Only nine articles (9.3%) presented findings specific to GMY and these focused primarily on individual-level minority stressors. Enacted stigma was associated with overall substance use. For example, healthcare discrimination was related to greater levels of alcohol and drug use among transmasculine youth (assigned female at birth and identify on a masculine-spectrum) [73]. Bullying also partially explained higher rates of alcohol and drug use [74]. Among transfeminine youth (assigned male at birth and identify on a feminine-spectrum), experiences of gender-related discrimination increased the odds of alcohol use compared to transfeminine youth without such experiences [75]; sexual-minority transfeminine youth showed even higher odds of HED than heterosexual transfeminine youth [76]. Internalizing symptoms and felt stigma were also related to alcohol and drug use among GMY. In particular, GMY were more likely than cisgender peers to report drinking alcohol to mitigate stress or interpersonal problems [77]. Additionally, psychological problems, gender-related discrimination, and parental alcohol/drug problems were associated with elevated odds of drug use among transfeminine youth [75]. No studies examined protective factors among GMY.
Substance Use among Adolescent (High-School Age) SMY: A Subset of the Literature
Thirty-seven articles (38.1%) presented data specifically related to adolescent, or high-school age, SMY. Unfortunately, none focused on adolescent GMY. Adolescent SMY are distinct from older youth in that they are typically enrolled full-time in secondary (high) school, reside with adult caregivers, and are legally prohibited from purchasing alcohol in the US. This developmental period is also when many SMY begin questioning their sexual identity [6].
General Substance Use Findings
Among adolescent SMY, substance use was associated with psychological distress [14] and discrimination based on sexual orientation [78], race [78], or weight [32]. Related to these findings, cisgender adolescent SMM who reported being reprimanded in childhood for gender nonconforming behavior were more likely to report alcohol and cannabis use as well as depressive and anxiety symptoms [79]. Additionally, compared to heterosexual peers, adolescent SMY reported greater overall substance use among their peers and more permissive peer attitudes toward substance use [51]. Both factors mediated the relationship between sexual-minority status and lifetime substance use.
Alcohol Use Findings: Adolescent SMY
Alcohol use was frequently studied in this sub-set of SMY. Earlier SMY self-identification was associated with lower rates of adult HED [48], whereas more frequent changes in self-reported sexual orientation on longitudinal follow-up during this adolescent-young adult period were associated with higher rates of HED among adolescent SMM [80]. Subjective reasons for drinking also played an important role. For example, adolescent SMM who cited stress reduction as a primary drinking motive reported more frequent past-month alcohol use than those who drank for other reasons [81]. Findings related to enacted-stigma in this age group were more mixed, with some studies finding an association [32, 24, 25, 39, 82, 36] and others failing to do so [52, 83]. Additionally, findings indicated that bullying may indirectly predict alcohol use via its association with depression [83], which itself predicted adolescent SMY alcohol use [25, 84].
Some individual, interpersonal, and structural factors were protective against alcohol use among adolescent SMY. At the individual level, use of harm reduction strategies (e.g., not drinking when driving or engaging in sexual activity) was associated with reduced risk of alcohol-related consequences [85]. Social support was also an important protective factor, with perceived parental support predicting lower risk of HED (particularly among adolescent SMW) [86] and peer support being particularly protective for bisexual adolescents [52]. However, these associations were moderated by peer alcohol use norms in one study [50]. School connectedness and overall social support were also associated with lower rates of heavy drinking during high school [66] and adulthood [47]. Finally, the environment in which adolescent SMY learn may impact drinking. Attending an SMY-affirming school was associated with significantly fewer heavy drinking days [55] as well as lower odds of risky drinking and past-year alcohol consequences, both for adolescent SMY generally and in particular for adolescent SMW [54, 31]. However, Coulter et al [55] did not find school climate to be protective for bisexual or questioning youth.
Drug Use Findings: Adolescent SMY
Drug-use studies among adolescent SMY also focused on minority stress factors. Bullying [25, 57, 58, 24], perceived homophobia [39], low self-esteem [67], gender-expression-based discrimination [60], stigmatizing school policies [27], and lack of Gay-Straight Alliances [87] were associated with higher drug use. Cannabis, cocaine, methamphetamine, opioid, prescription medication, and injection drug use were associated with perceived school safety [24], bullying [25], sexual violence victimization [24], and neighborhood-level rates of anti-SGM hate crimes [56]. Depressive symptoms were associated with both cannabis [25] and anabolic steroid use [58]. Suicidal ideation, physical victimization, and past-month drug use were also associated with anabolic steroid use [58]. Finally, greater sexual orientation fluidity during adolescence [80] and experiencing racial discrimination [78] predicted higher rates of cannabis use. Other demographic factors such as unstable housing and lack of enrollment in school were associated with concurrent use of multiple drugs [88].
Drug-use protective factors were similar to those for alcohol use and included school connectedness and social support. Both were protective against past-month cannabis, inhalant, and non-prescribed pain medication use [66]. Although adolescent SMY with an adult mentor were less likely than other SMY to report cannabis and non-cannabis drug use [89], they were still more likely than heterosexual youth to have used drugs. Additionally, Pearson et al [86] found that higher levels of parental closeness were associated with greater drug use among adolescent SMM; an association that was not present among adolescent SMW.
Racial/Ethnic Similarities and Differences among SMY
Fewer studies (n=20; 20.6%) compared differences in substance use by race/ethnicity among SMY; no studies focused on racial/ethnic differences among GMY. Existing studies tended to dichotomously compare White SMY and racial/ethnic minority SMY and focused on risk factors (rather than protective factors). Swann et al [90] observed racial/ethnic differences among young SMM in the trajectory of substance use over the adolescent and young adulthood period. Black young SMM reported slower increases in alcohol, cannabis, and non-cannabis drugs, compared to White young SMM. In contrast, Latino young SMM reported steeper increases in alcohol use but slower increases in poly-drug use (3 or more substances). Black and Latino adolescent SMM were also more likely than Whites to report lifetime anabolic steroid use [59], a disparity that was associated with depressive symptomatology [58]. Asian young SMM reported decreasing rates of inhalant use over time, a finding not observed in other racial/ethnic groups [65]. Among Black SMY, race-based discrimination was also associated with adolescent HED and cannabis use [78]. Black SMY with higher levels of life stress had higher odds of past-year cannabis, cocaine, and prescription opioid use [91]. In contrast, school enrollment was associated with less drug use among Black SMY [68]. Compared to Whites, racial/ethnic minority adolescent SMY also reported disproportionately high rates of stigma [92], physical threats/victimization, and feeling unsafe at school [28]. Each of these was associated with greater risk of substance use [78, 58, 24, 36, 39]. Findings for Asian adolescent SMY showed a particularly strong association between victimization and substance use [36], compared to other racial/ethnic minority SMY.
Sex-Specific Findings among SMY: An Understudied Area
Thirty-two studies (33%) reported sex-specific findings. Minority stress was the most common theoretical framework used in these studies. In particular, violence (enacted stigma) was a major area of sex-specific inquiry. For example, peer victimization was more strongly associated with substance use among young SMW than among young SMM [36]. Researchers found higher rates of verbal aggression among female same-sex couples than different-sex couples; however, verbal aggression was not associated with HED or cannabis use [61]. Adolescent SMW were more likely than their age-matched heterosexual counterparts to report cyber and school-based peer bullying [37, 24], experiences that were associated with alcohol and drug use [25, 84, 57, 58, 24]. Bullying was a particularly strong predictor of risky alcohol use among bisexual youth, a finding that was not consistently found for other SGMY sub-groups [37]. Across a number of studies, felt stigma was also associated with substance use, but adolescent SMW reported significantly higher levels of felt stigma than adolescent SMM [64]. Interestingly, coping with such stressors was more commonly cited by adolescent SMM than adolescent SMW as a primary reason for alcohol use [81]. Regarding social and structural factors, young SMW college athletes were more likely than female heterosexual athletes to report prescription and non-prescription drug use; however, athletic participation was only associated with non-prescription drug use among young SMM [93]. School-based Gay-Straight Alliances and anti-bullying policies, while protective for all adolescent SMY, were most protective against risky alcohol use and substance-use-related consequences for adolescent SMW [31]. Finally, there may also be sex differences in how previous substance use predicts current substance use among SMY. For example, in a study comparing SMY to same-sex heterosexual peers, adolescent tobacco use was predictive of young adult substance use among young SMW. In contrast, adolescent alcohol use was a stronger antecedent for adolescent heterosexual and bisexual SMM [94].
CONCLUSIONS
As evidenced by the number of research reports included in our review, there is growing interest in risk and protective factors associated with substance use among SGMY. However, substantially more attention has been given to risk rather than protective factors. Despite difficulties in comparing findings across studies because of variations in how substance use and SGMY status were operationalized, findings suggest that SGMY experience discrimination, bullying, and violence at higher rates than heterosexual youth, and the preponderance of studies found evidence of positive, small-to-medium strength associations between these experiences and substance use. However, it is difficult to make cross-study comparisons because analytic methods, outcome measures, and adjustment for confounding variables varied widely among studies. Additionally, findings suggest that individual coping strategies and institutional policies/programs that promote acceptance of SGMY youth can protect against risky substance use. Peer and parental support also partially mitigated risk of alcohol and drug use among some SGMY, and such support has also been shown to protect against other negative outcomes such as suicidal ideation [95]. Although more research is needed to better understand factors that protect against risk and promote resilience among SGMY, particularly GMY, findings highlight the need for intervention efforts aimed at preventing discrimination and victimization and equipping SGMY youth with tools for coping with these experiences when they occur.
There were several noteworthy methodologic trends observed in the review. First, the majority of SMY-focused studies and all GMY-focused studies used a cross-sectional design or only presented cross-sectional findings from longitudinal studies; far fewer followed youth longitudinally. Although such studies provide valuable insights into substance use among SGMY, they are unable to draw conclusions about causality. Additionally, most studies used volunteer or convenience samples, which limits generalizability. While convenience sampling can provide in-depth information about a particular group of SGMY [96], these types of studies are subject to selection bias such that SGMY who participate are more likely to be open about and comfortable with their SGMY status [97]. Because of the challenges involved in obtaining representative samples of SGMY, many researchers rely on national probability samples to overcome the limitations of convenience sampling. Therefore, it is important that measures of sexual orientation and gender identity be administered confidentially and included in all nationally representative studies (contrary to recent US Department of Health and Human Services proposals to remove such survey items [98, 99]).
The use of varying sexual orientation and gender identity measures limited our ability to compare results across studies. Most studies classified SMY based on sexual identity and did not take into account sexual attraction. Sexual attraction is particularly relevant when studying SMY because it allows researchers to identify youth whose sexual identity may not be stable or who may not yet be sexually active [100]. Few studies included assessment of youth who were “questioning” or otherwise unsure of their sexual orientation; those that did found this group to be at particular risk. Additionally, several studies cited sample size concerns to justify combining all SMY into a single category, thereby increasing statistical power but obscuring within-group differences. Similarly, when gender identity was assessed, GMY were often either dropped from the analysis or combined with SMY. Studies that reported GMY-specific findings tended to use only self-reported gender identity rather than the recommended operational definition based on a combination of current gender identity and sex assigned at birth [101]. When possible, data from GMY should be examined separately from SMY to understand variations in risk and resilience in these groups.
Measures of alcohol and drug use also varied substantially across studies. Some focused simply on use (over a variety of time-periods) while others examined risk (e.g., HED or use-related consequences). Such variation limited cross-study comparisons. All studies relied on self-report, which is subject to recall and social desirability bias. Triangulating self-report with objective measures (e.g., urine toxicology) could improve reliability. Additionally, certain measures may be more appropriate for certain sub-groups of SGMY than others. For example, “lifetime use” might be appropriate for adolescent SGMY but less clinically meaningful in college-age youth, when overall use is more common and when risky use and use-related consequences are of particular interest. Developing accepted measurement standards for alcohol and drug use in this population could alleviate some of this variability and permit more accurate cross-study comparisons and meta-analyses.
Aside from Wang et al [69], most studies focused on minority stressors (e.g., discrimination, stigma, prejudice) or related concepts (e.g., victimization) as risk factors. In part, this is appropriate because research has linked minority stress to myriad SGMY health disparities [23]. However, additional research is needed to investigate other theoretical models (e.g., Theory of Gender and Power [102], Health Belief Model [70]) and factors that are likely associated with substance use among SGMY (e.g., gender dysphoria, access to health care, gender-affirming medical/surgical interventions). Information is also needed about factors (e.g., discrimination) that are associated with substance use treatment acceptability and engagement among SGMY.
Finally, few of the recent studies investigated racial/ethnic, sex, or sexual orientation differences in risk/protective factors despite earlier findings that suggest important differences. Improved understanding of how such demographic factors interact to affect risk could support the development of tailored interventions that target SGMY at highest risk. For example, Swann et al [90] found that increases in substance use during adolescence and young adulthood occurred more slowly among Black young SMM compared to White young SMM. It is conceivable that such findings could lead to treatment interventions that attempt to harness and lengthen this lag period. It is important that researchers strive to increase racial/ethnic diversity of samples and to include both young SMM and SMW. Equally important, research is needed to investigate potential racial/ethnic and sex/gender differences, rather than simply controlling for these demographic variables.
Limitations of this scoping review include restriction of the sample to peer-reviewed articles published between 2013–2017 and omitting so-called “gray-literature” (e.g., doctoral dissertations, practice guidelines, government reports). We also omitted articles in which the samples included youth under 25 but which did not conduct age comparisons to support distinct youth-focused conclusions. The authors are also all US-based and therefore our inclusion/exclusion criteria may not fully reflect the research priorities or cultural contexts of substance use in other locations. Although we did not specifically exclude research conducted outside the US, many non-US-based articles were excluded because they focused solely on prevalence or involved populations defined by HIV/STI risk. Our restriction to non-HIV/STI-focused risk and protective factor research was intentional. Prevalence studies and HIV/STI-defined populations make up the bulk of research in this area [21], and narrowing our focus allowed us to comment on and draw attention to other segments of the literature. Understanding general risk and protective factors for substance use among SGMY is a necessary prerequisite for developing targeted or tailored treatment interventions.
Our results highlight the field’s interest in risk and protective factors for substance use among SGMY—and the particular focus on minority stress as an important risk factor. Results also highlight important methodologic and theoretical limitations in the currently available literature. Future directions include continued examination of SGMY substance use in nationally representative samples; expanded inquiry among GMY; further examination of racial/ethnic and sex/gender differences among SGMY; improved standardization of sexual orientation, gender identity, and alcohol/drug use measures; and increased efforts to translate what is known about alcohol and drug use among SGMY into clinical and public health interventions that address the well-documented substance use disparities in this at-risk population.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank the many researchers whose primary findings contributed to this review.
Funding: Dr. Kidd’s participation in this research was made possible through a training grant from the National Institute on Drug Abuse (T32-DA007294–24, PI Dr. Frances Levin). Dr. Jackman is partially supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (3R01AA013328–11, PI: Dr. Tonda Hughes). Dr. Margaret Wolff has a training grant (T32 MH019139; PI: Theodorus Sandfort, Ph.D.) from the National Institute of Mental Health at the HIV Center for Clinical and Behavioral Studies at the New York State Psychiatric Institute and Columbia University (P30-MH43520; Center Principal Investigator: Robert Remien, PhD). Dr. Veldhuis’ participation in this research was made possible through an NIH/NIAAA Ruth Kirschstein Postdoctoral Research Fellowship (F32AA025816; PI C. Veldhuis). Dr. Hughes is currently funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (3R01AA013328–11).
Abbreviations
- GMY
gender minority youth
- HED
heavy episodic drinking
- IPV
intimate partner violence
- PTSD
post-traumatic stress disorder
- SGMY
sexual and gender minority youth
- SMM
sexual minority men
- SMW
sexual minority women
- SMY
sexual minority youth
- US
United States
- YRBSS
Youth Risk Behavior Surveillance System
Footnotes
Conflicts of Interest
The authors have no financial conflicts of interest to declare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Jeremy D. Kidd, Division on Substance Use Disorders, Department of Psychiatry, Columbia University/New York State Psychiatric Institute, 1051 Riverside Drive, Unit 66, New York, NY 10032, Jeremy.Kidd@nyspi.columbia.edu, Phone: (646) 774-5563.
Kasey B. Jackman, School of Nursing, Columbia University.
Margaret Wolff, HIV Center for Clinical and Behavioral Studies; Division of Gender, Sexuality, and Health; Columbia University/New York State Psychiatric Institute.
Cindy B. Veldhuis, School of Nursing, Columbia University.
Tonda L. Hughes, School of Nursing and Department of Psychiatry, Columbia University.
REFERENCES
- 1.World Health Organization. Management of substance abuse: the global burden. 2018. http://www.who.int/substance_abuse/facts/global_burden/en/. Accessed February 26, 2018.
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rasberry CN, Tiu GF, Kann L, McManus T, Michael SL, Merlo CL et al. Health-related behaviors and academic achievement among high school students - United States, 2015. MMWR-Morbid Mortal W. 2017;66(35):921–7. doi: 10.15585/mmwr.mm6635a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dennis M, Babor TF, Roebuck MC, Donaldson J. Changing the focus: the case for recognizing and treating cannabis use disorders. Addiction. 2002;97(Suppl 1):4–15. doi: 10.1046/j.1360-0443.97.s01.10.x. [DOI] [PubMed] [Google Scholar]
- 5.Kann L, Olsen EO, McManus T, Harris WA, Shanklin SL, Flint KH et al. Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12 - United States and selected sites, 2015. MMWR Surveill Summ 2016;65(9):1–202. doi: 10.15585/mmwr.ss6509a1. [DOI] [PubMed] [Google Scholar]
- 6.Saewyc EM. Research on adolescent sexual orientation: development, health disparities, stigma and resilience. J Res Adolesc 2011;21(1):256–72. doi: 10.1111/j.1532-7795.2010.00727.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington, D.C.: The National Academies Press.; 2011. [PubMed] [Google Scholar]
- 8.Coulter RW, Blosnich JR, Bukowski LA, Herrick AL, Siconolfi DE, Stall RD. Differences in alcohol use and alcohol-related problems between transgender- and nontransgender-identified young adults. Drug Alcohol Depend. 2015;154:251–9. doi: 10.1016/j.drugalcdep.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Day JK, Fish JN, Perez-Brumer A, Hatzenbuehler ML, Russell ST. Transgender youth substance use disparities: results from a population-based sample. J Adolescent Health. 2017;61(6):729–35. doi: 10.1016/j.jadohealth.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koeppel MD, Bouffard LA, Koeppel-Ullrich ER. Sexual orientation and substance use: the moderation of parental attachment. Deviant Behav 2015;36(8):657–73. doi: 10.1080/01639625.2014.951582. [DOI] [Google Scholar]
- 11.Wilson SM, Gilmore AK, Rhew IC, Hodge KA, Kaysen DL. Minority stress is longitudinally associated with alcohol-related problems among sexual minority women. Addict Behav 2016;61:80–3. doi: 10.1016/j.addbeh.2016.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Talley AE, Hughes TL, Aranda F, Birkett M, Marshal MP. Exploring alcohol-use behaviors among heterosexual and sexual minority adolescents: intersections with sex, age, and race/ethnicity. Am J Public Health. 2014;104(2):295–303. doi: 10.2105/AJPH.2013.301627. [DOI] [PMC free article] [PubMed] [Google Scholar]; *This study was Important because it utilized population-based adolescent data (YRBSS) and investigated differences by race/ethnicity, sex assigned at birth, and sexual orientation in the same sample of adolescents; describing important differences among various sub-groups of SMY.
- 13.Newcomb ME, Ryan DT, Greene GJ, Garofalo R, Mustanski B. Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug Alcohol Depend. 2014;141:65–71. doi: 10.1016/j.drugalcdep.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craig SL, Keane G. The mental health of multiethnic lesbian and bisexual adolescent females: the role of self-efficacy, stress and behavioral risks. J Gay Lesbian Ment Health. 2014;18(3):266–83. doi: 10.1080/19359705.2013.879846. [DOI] [Google Scholar]
- 15.Armstrong R, Hall BJ, Doyle J, Waters E. Cochrane update: ‘Scoping the scope’ of a Cochrane review. J Public Health. 2011;33(1):147–50. doi: 10.1093/pubmed/fdr015. [DOI] [PubMed] [Google Scholar]
- 16.National Library of Medicine - National Center for Biotechnology Information. PubMed. Bethesda, MD: 2018. https://www.ncbi.nlm.nih.gov/pubmed/. Accessed February 26, 2018. [Google Scholar]
- 17.American Psychological Association. PsycInfo. 2018. http://www.apa.org/pubs/databases/psycinfo/index.aspx. Accessed February 26, 2018.
- 18.Elsevier. Embase. 2018. https://www.elsevier.com/solutions/embase-biomedical-research. Accessed March 11, 2018.
- 19.EBSCO Health. CINAHL Complete. 2018. https://www.ebscohost.com/nursing/products/cinahl-databases/cinahl-complete. Accessed February 26, 2018.
- 20.United Nations. Definition of youth. 2013. http://www.un.org/esa/socdev/documents/youth/fact-sheets/youth-definition.pdf. Accessed February 26, 2018.
- 21.Coulter RW, Kenst KS, Bowen DJ, Scout. Research funded by the National Institutes of Health on the health of lesbian, gay, bisexual, and transgender populations. Am J Public Health. 2014;104(2):e105–12. doi: 10.2105/AJPH.2013.301501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 23.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lowry R, Johns MM, Robin LE, Kann LK. Social stress and substance use disparities by sexual orientation among high school students. Am J Prev Med 2017. doi: 10.1016/j.amepre.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Marshal MP, Burton CM, Chisolm DJ, Sucato GS, Friedman MS. Cross-sectional evidence for a stress-negative affect pathway to substance use among sexual minority girls. Clin Transl Sci 2013;6(4):321–2. doi: 10.1111/cts.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Soc Sci Med. 2014;103:67–75. doi: 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hatzenbuehler ML, Jun HJ, Corliss HL, Bryn Austin S. Structural stigma and sexual orientation disparities in adolescent drug use. Addict Behav 2015;46:14–8. doi: 10.1016/j.addbeh.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]; **This important study correlated individual-level substance use data from a representative sample of adolescents with state-level indices of anti-SMY structural stigma (e.g., US Census data on same-sex couples, presence/absence of school-based Gay-Straight Alliances, relevant policies/legislation). Authors found that all SMY reported greater cannabis and non-cannabis drug use compared to heterosexual peers. However, these disparities were significantly more pronounced in states with greater levels of structural stigma.
- 28.Kecojevic A, Wong CF, Corliss HL, Lankenau SE. Risk factors for high levels of prescription drug misuse and illicit drug use among substance-using young men who have sex with men (YMSM). Drug Alcohol Depend. 2015;150:156–63. doi: 10.1016/j.drugalcdep.2015.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coulter RW, Kinsky SM, Herrick AL, Stall RD, Bauermeister JA. Evidence of syndemics and sexuality-related discrimination among young sexual-minority women. LGBT Health. 2015;2(3):250–7. doi: 10.1089/lgbt.2014.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bauer GR, Flanders C, MacLeod MA, Ross LE. Occurrence of multiple mental health or substance use outcomes among bisexuals: a respondent-driven sampling study. BMC Public Health. 2016;16:497. doi: 10.1186/s12889-016-3173-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Konishi C, Saewyc E, Homma Y, Poon C. Population-level evaluation of school-based interventions to prevent problem substance use among gay, lesbian and bisexual adolescents in Canada. Prev Med 2013;57(6):929–33. doi: 10.1016/j.ypmed.2013.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huebner DM, Thoma BC, Neilands TB. School victimization and substance use among lesbian, gay, bisexual, and transgender adolescents. Prev Sci 2015;16(5):734–43. doi: 10.1007/s11121-014-0507-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mustanski B, Andrews R, Herrick A, Stall R, Schnarrs PW. A syndemic of psychosocial health disparities and associations with risk for attempting suicide among young sexual minority men. Am J Public Health. 2014;104(2):287–94. doi: 10.2105/AJPH.2013.301744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Donahue K, Langstrom N, Lundstrom S, Lichtenstein P, Forsman M. Familial factors, victimization, and psychological health among sexual minority adolescents in Sweden. Am J Public Health. 2017;107(2):322–8. doi: 10.2105/ajph.2016.303573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith BC, Armelie AP, Boarts JM, Brazil M, Delahanty DL. PTSD, depression, and substance use in relation to suicidality risk among traumatized minority lesbian, gay, and bisexual youth. Arch Suicide Res 2016;20(1):80–93. doi: 10.1080/13811118.2015.1004484. [DOI] [PubMed] [Google Scholar]
- 36.Rosario M, Corliss HL, Everett BG, Russell ST, Buchting FO, Birkett MA. Mediation by peer violence victimization of sexual orientation disparities in cancer-related tobacco, alcohol, and sexual risk behaviors: pooled youth risk behavior surveys. Am J Public Health. 2014;104(6):1113–23. doi: 10.2105/AJPH.2013.301764. [DOI] [PMC free article] [PubMed] [Google Scholar]; *This study was important both because it relied on representative sampling and because it looked at racial/ethnic and sex differences among adolescent SMY. The authors found that peer-violence victimization mediated the association between SMY status and substance use outcomes, a finding that was particularly strong for adolescent SMW and Asian/Pacific Islander SMY.
- 37.Phillips G, Turner B, Salamanca P, Birkett M, Hatzenbuehler ML, Newcomb ME et al. Victimization as a mediator of alcohol use disparities between sexual minority subgroups and sexual majority youth using the 2015 National Youth Risk Behavior Survey. Drug Alcohol Depend. 2017;178:355–62. doi: 10.1016/j.drugalcdep.2017.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woodford MR, Kulick A, Atteberry B. Protective factors, campus climate, and health outcomes among sexual minority college students. J Divers High Educ 2015;8(2):73–87. doi: 10.1037/a0038552. [DOI] [Google Scholar]
- 39.Kelly J, Davis C, Schlesinger C. Substance use by same sex attracted young people: prevalence, perceptions and homophobia. Drug Alcohol Rev 2015;34(4):358–65. doi: 10.1111/dar.12158. [DOI] [PubMed] [Google Scholar]
- 40.Stults CB, Javdani S, Greenbaum CA, Kapadia F, Halkitis PN. Intimate partner violence and substance use risk among young men who have sex with men: the P18 cohort study. Drug Alcohol Depend. 2015;154:54–62. doi: 10.1016/j.drugalcdep.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Parker M, Duran B, Walters K. The relationship between bias-related victimization and generalized anxiety disorder among American Indian and Alaskan Native lesbian, gay, bisexual, transgender, and two-spirit community members. Int J Indig Health. 2017;12(2):64–83. doi:DOI: 10.18357/ijih122201717785. [DOI] [Google Scholar]
- 42.Lowe SR, Joshi S, Galea S, Aiello AE, Uddin M, Koenen KC et al. Pathways from assaultive violence to post-traumatic stress, depression, and generalized anxiety symptoms through stressful life events: longitudinal mediation models. Psychol Med 2017;47(14):2556–66. doi: 10.1017/S0033291717001143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bandoli G, Campbell-Sills L, Kessler RC, Heeringa SG, Nock MK, Rosellini AJ et al. Childhood adversity, adult stress, and the risk of major depression or generalized anxiety disorder in US soldiers: a test of the stress sensitization hypothesis. Psychol Med 2017;47(13):2379–92. doi: 10.1017/S0033291717001064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Litt DM, Lewis MA, Blayney JA, Kaysen DL. Protective behavioral strategies as a mediator of the generalized anxiety and alcohol use relationship among lesbian and bisexual women. J Stud Alcohol Drugs. 2013;74(1):168–74. [DOI] [PMC free article] [PubMed] [Google Scholar]; *The study used a large convenience sample (n=1083) to provided valuable insights into protective factors against alcohol use, an identified gap in the literature. In particular, specific behavioral strategies aimed at either limiting drinking or reducing harm (e.g., not combining alcohol with sexual activity) were associated with lower odds of alcohol-related negative consequences among SMY.
- 45.Flood J, McLaughlin C, Prentice G. Minority stress, homonegativity, alcohol use and mental health among college gay males. J Gay Lesbian Ment Health. 2013;17(4):367–86. doi: 10.1080/19359705.2013.800006. [DOI] [Google Scholar]
- 46.Lee CM, Blayney J, Rhew IC, Lewis MA, Kaysen D. College status, perceived drinking norms, and alcohol use among sexual minority women. Psychol Sex Orientat Gend Divers. 2016;3(1):104–12. doi: 10.1037/sgd0000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Watson RJ, Russell ST. Disengaged or bookworm: academics, mental health, and success for sexual minority youth. J Res Adolescence. 2016;26(1):159–65. doi: 10.1111/jora.12178. [DOI] [Google Scholar]
- 48.Fish JN, Pasley K. Sexual (minority) trajectories, mental health, and alcohol use: a longitudinal study of youth as they transition to adulthood. J Youth Adolescence. 2015;44(8):1508–27. doi: 10.1007/s10964-015-0280-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Livingston NA, Christianson N, Cochran BN. Minority stress, psychological distress, and alcohol misuse among sexual minority young adults: a resiliency-based conditional process analysis. Addict Behav 2016;63:125–31. doi: 10.1016/j.addbeh.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 50.Hatzenbuehler ML, McLaughlin KA, Xuan Z. Social networks and sexual orientation disparities in tobacco and alcohol use. J Stud Alcohol Drugs. 2015;76(1):117–26. [PMC free article] [PubMed] [Google Scholar]
- 51.Mereish EH, Goldbach JT, Burgess C, DiBello AM. Sexual orientation, minority stress, social norms, and substance use among racially diverse adolescents. Drug Alcohol Depend. 2017;178:49–56. doi: 10.1016/j.drugalcdep.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Austin A, Craig SL. Support, discrimination, and alcohol use among racially/ethnically diverse sexual minority youths. J Gay Lesbian Soc Serv 2013;25(4):420–42. doi: 10.1080/10538720.2013.833067. [DOI] [Google Scholar]
- 53.Gilmore AK, Koo KH, Nguyen HV, Granato HF, Hughes TL, Kaysen D. Sexual assault, drinking norms, and drinking behavior among a national sample of lesbian and bisexual women. Addict Behav 2014;39(3):630–6. doi: 10.1016/j.addbeh.2013.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Poteat V, Sinclair KO, DiGiovanni CD, Koenig BW, Russell ST. Gay-Straight Alliances are associated with student health: a multischool comparison of LGBTQ and heterosexual youth. J Res Adolescence. 2013;23(2):319–30. doi: 10.1111/j.1532-7795.2012.00832.x. [DOI] [Google Scholar]
- 55.Coulter RW, Birkett M, Corliss HL, Hatzenbuehler ML, Mustanski B, Stall RD. Associations between LGBTQ-affirmative school climate and adolescent drinking behaviors. Drug Alcohol Depend. 2016;161:340–7. doi: 10.1016/j.drugalcdep.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]; **This study used population-based data from 14 YRBSS jurisdictions and found that heterosexual and gay/lesbian youth living in SGMY-affirming jurisdictions reported significantly fewer past 30-day heavy drinking days, compared to youth in less affirming areas. However, this relationship did not hold true for bisexual or questioning youth.
- 56.Duncan DT, Hatzenbuehler ML, Johnson RM. Neighborhood-level LGBT hate crimes and current illicit drug use among sexual minority youth. Drug Alcohol Depend. 2014;135(1):65–70. doi: 10.1016/j.drugalcdep.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ballard ME, Jameson JP, Martz DM. Sexual identity and risk behaviors among adolescents in rural Appalachia. J Rural Mental Health. 2017;41(1):17–29. doi: 10.1037/rmh0000068. [DOI] [Google Scholar]
- 58.Blashill AJ, Safren SA. Sexual orientation and anabolic-androgenic steroids in US adolescent boys. Pediatrics. 2014;133(3):469–75. doi: 10.1542/peds.2013-2768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blashill AJ, Calzo JP, Griffiths S, Murray SB. Anabolic steroid misuse among US adolescent boys: disparities by sexual orientation and race/ethnicity. Am J Public Health. 2017;107(2):319–21. doi: 10.2105/ajph.2016.303566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ioerger M, Henry KL, Chen PY, Cigularov KP, Tomazic RG. Beyond same-sex attraction: gender-variant-based victimization is associated with suicidal behavior and substance use for other-sex attracted adolescents. PLoS ONE 2015;10(6). doi: 10.1371/journal.pone.0129976. [DOI] [PMC free article] [PubMed] [Google Scholar]; **This study was significant and unique because it focused on gender-expression-based victimization in cisgender adolescents, finding that such bullying victimization was associated with drug use among heterosexual cisgender adolescents and with suicidality among both adolescent SMY and their heterosexual peers.
- 61.Reuter TR, Sharp C, Temple JR. An exploratory study of teen dating violence in sexual minority youth. Partner Abuse 2015;6(1):8–28. doi: 10.1891/1946-6560.6.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reuter TR, Newcomb ME, Whitton SW, Mustanski B. Intimate partner violence victimization in LGBT young adults: demographic differences and associations with health behaviors. Psychol Violence. 2017;7(1):101–9. doi: 10.1037/vio0000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dworkin ER, Kaysen D, Bedard-Gilligan M, Rhew IC, Lee CM. Daily-level associations between PTSD and cannabis use among young sexual minority women. Addict Behav. 2017;74:118–21. doi: 10.1016/j.addbeh.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lea T, de Wit J, Reynolds R. Minority stress in lesbian, gay, and bisexual young adults in Australia: associations with psychological distress, suicidality, and substance use. Arch Sex Behav 2014;43(8):1571–8. doi: 10.1007/s10508-014-0266-6. [DOI] [PubMed] [Google Scholar]
- 65.Halkitis PN, Siconolfi DE, Stults CB, Barton S, Bub K, Kapadia F. Modeling substance use in emerging adult gay, bisexual, and other YMSM across time: the P18 cohort study. Drug Alcohol Depend. 2014;145:209–16. doi: 10.1016/j.drugalcdep.2014.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.De Pedro KT, Esqueda MC, Gilreath TD. School protective factors and substance use among lesbian, gay, and bisexual adolescents in California public schools. LGBT Health. 2017;4(3):210–6. doi: 10.1089/lgbt.2016.0132. [DOI] [PubMed] [Google Scholar]
- 67.Wilkerson JM, Lawler SM, Romijnders KA, Armstead AB, Bauldry J. Exploratory analyses of risk behaviors among GLBT youth attending a drop-in center. Health Educ Behav 2017:1090198117715668. doi: 10.1177/1090198117715668. [DOI] [PubMed] [Google Scholar]
- 68.Traube DE, Holloway IW, Schrager SM, Smith L, Kipke MD. Illicit substance use among emerging adults in the Los Angeles house and ball community. J HIV AIDS Soc Serv 2014;13(2):144–62. doi: 10.1080/15381501.2013.768950. [DOI] [Google Scholar]
- 69.Wang Z, Li D, Lau JT, Yang X, Shen H, Cao W. Prevalence and associated factors of inhaled nitrites use among men who have sex with men in Beijing, China. Drug Alcohol Depend. 2015;149:93–9. doi: 10.1016/j.drugalcdep.2015.01.021. [DOI] [PubMed] [Google Scholar]
- 70.Champion VL, Skinner CS. The health belief model In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008. p. 45–65. [Google Scholar]
- 71.Yang GL, Zhang AD, Yu Y, Liu H, Long FY, Yan J. Drug use and its associated factors among money boys in Hunan Province, China. Public Health. 2016;140:213–20. doi: 10.1016/j.puhe.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 72.Kuyper L, Bos H. Mostly heterosexual and lesbian/gay young adults: differences in mental health and substance use and the role of minority stress. J Sex Res. 2016;53(7):731–41. doi: 10.1080/00224499.2015.1071310. [DOI] [PubMed] [Google Scholar]
- 73.Reisner SL, Pardo ST, Gamarel KE, White Hughto JM, Pardee DJ, Keo-Meier CL. Substance use to cope with stigma in healthcare among U.S. female-to-male trans masculine adults. LGBT health. 2015;2(4):324–32. doi: 10.1089/lgbt.2015.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender minority social stress in adolescence: disparities in adolescent bullying and substance use by gender identity. J Sex Res 2015;52(3):243–56. doi: 10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]; **This study was important because it focused on GMY, an identified gap in the literature. The authors found that GMY were more likely than cisgender boys to report past-year alcohol, cannabis, and non-cannabis drugs use. Furthermore, among GMY, substance use was associated with bullying victimization.
- 75.Rowe C, Santos GM, McFarland W, Wilson EC. Prevalence and correlates of substance use among trans*female youth ages 16–24 years in the San Francisco Bay Area. Drug Alcohol Depend. 2015;147:160–6. doi: 10.1016/j.drugalcdep.2014.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Arayasirikul S, Pomart WA, Raymond HF, Wilson EC. Unevenness in health at the intersection of gender and sexuality: sexual minority disparities in alcohol and drug use among transwomen in the San Francisco Bay Area. J Homosex. 2017:1–14. doi: 10.1080/00918369.2017.1310552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tupler LA, Zapp D, DeJong W, Ali M, O’Rourke S, Looney J et al. Alcohol-related blackouts, negative alcohol-related consequences, and motivations for drinking reported by newly matriculating transgender college students. Alcoholism Clin Exp Res 2017;41(5):1012–23. doi: 10.1111/acer.13358. [DOI] [PMC free article] [PubMed] [Google Scholar]; **This study used a college-age, convenience sample to compare cisgender youth and GMY. GMY reported greater frequency of alcohol-related blackouts and negative consequences. Transfeminine youth reported both outcomes more frequently than transmasculine youth. Importantly, GMY were more likely than cisgender youth to cite stress reduction and management of social anxiety and low self-esteem as drinking motives.
- 78.Thoma BC, Huebner DM. Health consequences of racist and antigay discrimination for multiple minority adolescents. Cult Divers Ethn Min 2013;19(4):404–14. doi: 10.1037/a0031739. [DOI] [PMC free article] [PubMed] [Google Scholar]; *This study looked specifically at risk and protective factors among racial/ethnic minority adolescent SMY and found that experiences of racist discrimination were associated with both past-year HED and cannabis use.
- 79.Bauermeister JA, Connochie D, Jadwin-Cakmak L, Meanley S. Gender policing during childhood and the psychological well-being of young adult sexual minority men in the United States. Am J Mens Health. 2017;11(3):693–701. doi: 10.1177/1557988316680938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ott MQ, Wypij D, Corliss HL, Rosario M, Reisner SL, Gordon AR et al. Repeated changes in reported sexual orientation identity linked to substance use behaviors in youth. J Adolescent Health. 2013;52(4):465–72. doi: 10.1016/j.jadohealth.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bos H, van Beusekom G, Sandfort T. Drinking motives, alcohol use, and sexual attraction in youth. J Sex Res 2016;53(3):309–12. doi: 10.1080/00224499.2015.1020355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dermody SS, Marshal MP, Burton CM, Chisolm DJ. Risk of heavy drinking among sexual minority adolescents: indirect pathways through sexual orientation-related victimization and affiliation with substance-using peers. Addiction. 2016;111(9):1599–606. doi: 10.1111/add.13409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tucker JS, Ewing BA, Espelage DL, Green HD, de la Haye K, Pollard MS. Longitudinal associations of homophobic name-calling victimization with psychological distress and alcohol use during adolescence. J Adolescent Health. 2016;59(1):110–5. doi: 10.1016/j.jadohealth.2016.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pesola F, Shelton KH, van den Bree MB. Sexual orientation and alcohol problem use among U.K. adolescents: an indirect link through depressed mood. Addiction. 2014;109(7):1072–80. doi: 10.1111/add.12528. [DOI] [PubMed] [Google Scholar]
- 85.Ebersole RC, Moorer KD, Noble JJ, Madson MB. Protective behavioral strategies, alcohol consumption, and alcohol-related negative consequences among lesbian, gay, and bisexual college students. J Gay Lesbian Ment Health. 2015;19(2):184–200. doi: 10.1080/19359705.2014.991957. [DOI] [Google Scholar]
- 86.Pearson J, Wilkinson L. Family relationships and adolescent well-being: are families equally protective for same-sex attracted youth? J Youth Adolescence. 2013;42(3):376–93. doi: 10.1007/s10964-012-9865-5. [DOI] [PubMed] [Google Scholar]
- 87.Heck NC, Flentje A, Cochran BN. Offsetting risks: High school gay-straight alliances and lesbian, gay, bisexual, and transgender (LGBT) youth. Psychol Sex Orientat Gend Divers 2013;1(S):81–90. doi: 10.1037/2329-0382.1.S.81. [DOI] [Google Scholar]
- 88.Yu G, Goldsamt LA, Clatts MC, Giang LM. Sexual initiation and complex recent polydrug use patterns among male sex workers in Vietnam: a preliminary epidemiological trajectory. Arch Sex Behav 2016;45(4):975–81. doi: 10.1007/s10508-015-0667-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Seil KS, Desai MM, Smith MV. Sexual orientation, adult connectedness, substance use, and mental health outcomes among adolescents: findings from the 2009 New York City Youth Risk Behavior Survey. Am J Public Health. 2014;104(10):1950–6. doi: 10.2105/AJPH.2014.302050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Swann G, Bettin E, Clifford A, Newcomb ME, Mustanski B. Trajectories of alcohol, marijuana, and illicit drug use in a diverse sample of young men who have sex with men. Drug Alcohol Depend. 2017;178:231–42. doi: 10.1016/j.drugalcdep.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Voisin DR, Hotton AL, Schneider JA. The relationship between life stressors and drug and sexual behaviors among a population-based sample of young Black men who have sex with men in Chicago. AIDS Care. 2017;29(5):545–51. doi: 10.1080/09540121.2016.1224303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bruce D, Stall R, Fata A, Campbell RT. Modeling minority stress effects on homelessness and health disparities among young men who have sex with men. J Urban Health. 2014;91(3):568–80. doi: 10.1007/s11524-014-9876-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kroshus E, Davoren AK. Mental health and substance use of sexual minority college athletes. J Am Coll Health. 2016;64(5):371–9. doi: 10.1080/07448481.2016.1158179. [DOI] [PubMed] [Google Scholar]
- 94.Kecojevic A, Jun HJ, Reisner SL, Corliss HL. Concurrent polysubstance use in a longitudinal study of US youth: associations with sexual orientation. Addiction. 2017;112(4):614–24. doi: 10.1111/add.13681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coulter RWS, Kessel Schneider S, Beadnell B, O’Donnell L. Associations of outside- and within-school adult support on suicidality: moderating effects of sexual orientation. Am J Orthopsychiatr 2017;87(6):671–9. doi: 10.1037/ort0000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Drabble LA, Trocki KF, Korcha RA, Klinger JL, Veldhuis CB, Hughes TL. Comparing substance use and mental health outcomes among sexual minority and heterosexual women in probability and non-probability samples. Drug Alcohol Depend. 2018;185:285–92. doi: 10.1016/j.drugalcdep.2017.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Macapagal K, Coventry R, Arbeit MR, Fisher CB, Mustanski B. “I won’t out myself just to do a survey”: sexual and gender minority adolescents’ perspectives on the risks and benefits of sex research. Arch Sex Behav 2017;46(5):1393–409. doi: 10.1007/s10508-016-0784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kellman L Associated Press: Census suggests counting LGBTQ, then corrects and deletes. March 29, 2017. https://apnews.com/619704d091da4b54968a23720aadee0f/no-lgbtq-category-included-census-proposal-2020-count. Accessed February 27, 2018. [Google Scholar]
- 99.The Williams Institute - UCLA School of Law. Media advisory: Trump Administration proposes to end important data collection on LGBT elders and people with disabilities. March 20, 2017. https://williamsinstitute.law.ucla.edu/press/press-releases/media-advisory-trump-administration-proposes-to-end-important-data-collection-on-lgbt-elders-and-people-with-disabilities/. Accessed February 28, 2018. [Google Scholar]
- 100.Temkin D, Belford J, McDaniel T, Stratford B, Parris D. Improving measurement of sexual orientation and gender identity among middle and high school students. 2017. https://www.childtrends.org/wp-content/uploads/2017/06/2017-22LGBTSurveyMeasures-1.pdf. Accessed March 12, 2018.
- 101.Reisner SL, Conron KJ, Scout., Baker K, Herman JL, Lombardi E et al. “Counting” transgender and gender-nonconforming adults in health research: recommendations from the gender identity in US surveillance group. Transgender Studies Quarterly. 2015;2(1):34–57. [Google Scholar]
- 102.Wingood G, DiClemente RJ. The theory of gender and power: a social structural theory for guiding public health interventions In: Diclemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research: strategies for improving public health. San Francisco, CA: Jossey-Bass; 2002. p. 313–46. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.