Abstract
Background:
In a complex health system, it is important to establish a systematic and data-driven approach to identifying needs. The Diabetes Clinical Community (DCC) of Johns Hopkins Medicine’s Armstrong Institute for Patient Safety and Quality developed a gap analysis tool and process to establish the system’s current state of inpatient diabetes care.
Methods:
The collectively developed tool assessed the following areas: program infrastructure; protocols, policies, and order sets; patient and health care professional education; and automated data access. For the purposes of this analysis, gaps were defined as those instances in which local resources, infrastructure, or processes demonstrated a variance against the current national evidence base or institutionally defined best practices.
Results:
Following the gap analysis, members of the DCC, in collaboration with health system leadership, met to identify priority areas in order to integrate and synergize diabetes care resources and efforts to enhance quality and reduce disparities in care across the system. Key gaps in care identified included lack of standardized glucose management policies, lack of standardized training of health care professionals in inpatient diabetes management, and lack of access to automated data collection and analysis. These results were used to gain resources to support collaborative diabetes health system initiatives and to successfully obtain federal research funding to develop and pilot a pragmatic diabetes educational intervention.
Conclusion:
At a health system level, the summary format of this gap analysis tool is an effective method to clearly identify disparities in care to focus efforts and resources to improve care delivery.
Health systems are working to develop efficient, integrated approaches to delivering care that enhances value for the patients they care for and the populations they serve. In the state of Maryland, hospitals and health systems receive fixed annual revenue.1 This approach to health care financing will be adopted more broadly across the United States in the near future, and it will be important for health systems to systematically identify areas to enhance quality in a cost-effective manner by reducing hospital admissions and potentially avoidable health care utilization. For this reason, our article is targeted not only at clinicians who care for patients with diabetes in the hospital (for example, physicians, nurses, advanced practice clinicians, nutritionists, pharmacists) but also at health system administrators and executives who are trying to determine where the gaps are in a complex system with an eye toward prioritizing strategic, high-value interventions to address these gaps by aligning all health care partners around these goals.
Johns Hopkins Health System (JHHS) consists of five adult hospitals (two academic, three community based) and a children’s hospital. The Armstrong Institute for Patient Safety and Quality (AI), founded by Johns Hopkins Medicine (JHM) in 2011, has been tasked with advancing training, research, and operations in patient safety and quality by engaging university researchers and supporting dissemination of evidence-based practices across JHHS.2 To address this need, AI formed clinical communities as a strategy to achieve better outcomes and value (safe, high-quality, and cost-effective care).2 Clinical communities, which are led by clinicians and have interdisciplinary membership, identify the goals and approaches to achieving them, focus on patient safety and quality improvement for a specific population or process, and connect frontline providers from the different hospitals across our health system.2 Given that diabetes care is an area of preventable harm and high health care costs, a Diabetes Clinical Community (DCC) was established within our health system.
We previously identified and implemented key elements of successful inpatient glucose management programs at Johns Hopkins Hospital (JHH) based on recommendations from the American Diabetes Association (ADA), American Association of Clinical Endocrinologists (AACE), and The Joint Commission Inpatient Diabetes Certification Program.3 Our program resulted in a significant and sustained reduction in institutionwide hypoglycemia.3 When the AI DCC was formed, representatives from the other adult JHHS hospitals were interested in implementing our model; however, prior to proceeding we believed it was important to establish a systematic and data-driven approach to identifying needs within the system—a “gap analysis”—to guide us in strategically setting our initial goals and priorities from the diverse and at times competing possibilities vying for attention. A gap analysis can assess existing personnel and nonpersonnel resources within a health system, identify areas for integration of health care delivery, and uncover areas of potential safety and liability risk for a single overarching topic area (for example, infection prevention, inpatient glucose management) across diverse entities either within or across institutions. The purposes of this manuscript are to (1) present our gap analysis tool and process for performing a health system diabetes needs assessment and (2) illustrate how the results of this gap analysis, conducted by the AI DCC, has led to collaborative diabetes health system initiatives and successful attainment of National Institutes of Health funding to develop and pilot a pragmatic diabetes educational intervention. We believe that the components of our gap analysis tool are applicable to assessing health system needs in other areas of acute and chronic disease management.
METHODS
Formation and Goals of the AI Diabetes Clinical Community
The DCC was established in November 2013. The membership includes diabetes care providers/stakeholders (physicians, advanced practice clinicians, nurses, dietitians, pharmacists) from each of the five adult hospitals in JHHS, which includes two urban academic medical centers in the Baltimore-Washington, DC, region (JHH and Johns Hopkins Bayview Medical Center) and three community medical centers (Howard County General Hospital, Sibley Memorial Hospital, and Suburban Hospital). The purpose of the AI DCC is to develop a diabetes management algorithm for provision of safe, high-quality diabetes care across the continuum of care (from the inpatient setting to the outpatient setting to home) using evidence/consensus-based guidelines. This goal will be accomplished by doing the following:
Developing a network that will drive improvements in patient outcomes and increased value of diabetes care throughout each of the JHM entities
Creating a culture of inclusion and collaboration through generating a clearinghouse for institution-specific diabetes evidence-based best practices that will enable sharing relevant experiences, challenges, successes, policies, procedures and protocols, and educational materials across JHHS
Sharing improvement initiatives that are measureable and important to all members
Development of the Gap Analysis Tool
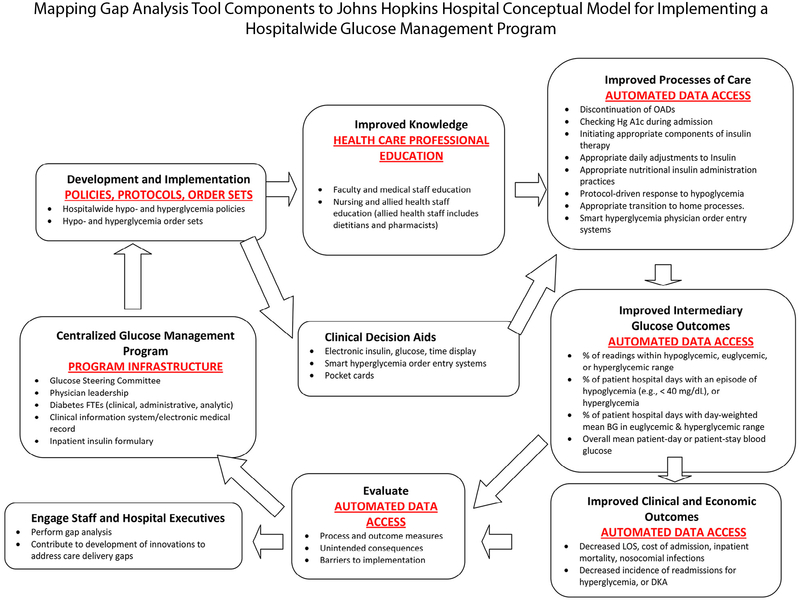
To establish the current state of inpatient diabetes care delivery in our health system, we collectively developed a gap analysis tool—based on our previously published conceptual model for implementing hospitalwide glucose management programs3—to identify priority areas in order to integrate and synergize diabetes care resources and efforts, as shown in Table 1 and Figure 1. As noted, we previously identified and implemented key elements of successful in-patient glucose management programs based on recommendations from the ADA, AACE, and The Joint Commission Inpatient Diabetes Certification Program.3–6 These include centralized glucose management program infrastructure, uniform policies and order sets for management of hypoglycemia and hyperglycemia, staff and patient diabetes education, patient glucose self-management education, clinical decision support incorporated into the electronic health record (EHR), and automated data access to assess intermediary glucose outcomes and clinical/economic outcomes3 (Table 1).
Table 1.
Diabetes Gap Analysis Tool Components Derived from a Conceptual Model for Implementing Hospitalwide Glucose Management Programs
| Johns Hopkins Hospital Glucose Management Program Conceptual Framework Component* | Gap Analysis Tool Component | Program Components Assessed with Gap Analysis Tool | Assessment Method in Gap Analysis Tool† |
|---|---|---|---|
| Centralized Glucose Management Program | Program Infrastructure | Physician leadership Program support and structure Inpatient and outpatient diabetes FTEs (advanced practice clinicians, nurses, dietitians, certified diabetes educators), administrative support FTEs, data analysis FTEs, availability of on-site podiatry services Centralized Glucose Steering Committee Clinical information system used Inpatient insulin formulary |
Name of program champion listed # of FTEs for program support and structure entered Drop-down menu options: yes or no Drop-down menu of several options used in the health system |
| Development and Implementation of Glucose Management Program | Protocols, Policies, and Order Sets | Inpatient hyperglycemia management (for subcutaneous insulin) Inpatient hypoglycemia management Intravenous insulin infusion management Insulin management for continuous enteral nutrition Inpatient insulin pump management Insulin pen management Point-of-care testing guidelines Diabetic ketoacidosis/hyperglycemic hyperosmolar state management Outpatient hyperglycemia management (for subcutaneous insulin) Outpatient hypoglycemia management |
Drop-down menu options: enforced policy, protocol or guideline, or none |
| Improved Knowledge | Health Care Professional Education | Faculty/Medical Staff Education Estimating total daily insulin dose and dividing it into basal, nutritional, and correction insulin Adjusting insulin to prevent or treat hypo- and hyperglycemia Avoiding insulin stacking Prescriber responsibilities for insulin pump use Oral and non-insulin injectable antidiabetic agents Nursing and Support Staff Education Understanding basal/nutritional/correction insulin therapy Oral antidiabetic agents Prevention and treatment of hypoglycemia Diabetic ketoacidosis Type 1 versus type 2 diabetes Blood glucose monitoring Insulin administration and documentation Medical devices: insulin pumps (nursing responsibilities), insulin pens, glucometers Transitions of care (inpatient area to inpatient area; inpatient to outpatient) Parenteral and enteral nutrition Patient diabetes education Carbohydrate identification and counting |
Drop-down menu options: mandatory, optional, not offered |
| Improved Knowledge | Patient Education | Standard teaching plan Blood glucose monitoring and maintaining a log Diabetes and sick day management Diabetes education guide Diabetes and foot care Diabetes and periodontal disease Diabetes and small vessel disease Gestational diabetes Living with diabetes Exercise and physical activity High blood glucose management Low blood glucose management Insulin injections Know your numbers (blood pressure, cholesterol, body mass index, hemoglobin A1c) Diet/carbohydrate counting |
Drop down menu options: yes or no |
| Evaluate Glucose Management Program | Automated Data Access | Identification of patients with diabetes (inpatient and outpatient) Inpatient glucose readings Identification of inpatients with diabetes treated with insulin Glucose-related patient safety events |
Drop-down menu options: yes or no |
Figure 1:
The conceptual model for implementing hospitalwide glucose management programs was used to identify priority areas to integrate and synergize diabetes care resources and efforts. Adapted from Munoz M, et al. Implementing and evaluating a multicomponent inpatient diabetes management program: Putting research into practice. Jt Comm J Qual Patient Saf. 2012;38:195–206. FTE, full-time equivalent; OAD, oral antidiabetic drug; BG, blood glucose; LOS, length of stay; DKA, diabetic ketoacidosis.
The gap analysis tool was developed in Microsoft Excel (Microsoft Corp., Redmond, Washington) and was organized and formatted in such a way as to ensure that all respondents could easily access, navigate, and complete the tool despite variances in available computer resources and information technology skills across the participating sites (Appendix 1, available in online article). Table 1 summarizes how glucose management program components were assessed in the Excel spreadsheet. For program infrastructure, some items were typed in (for example, program leader’s name, EHR used), the number of program full-time equivalents was entered numerically, and insulin formulary was selected from a drop-down menu of insulin options. Protocols, policies, and order sets were selected from drop-down menu options of “enforced policy,” “protocol or guideline,” or “none.” In our system we define policies as rules and overarching principles that govern clinical practice and must be adhered to in patient care. They are approved by our hospitals’ medical boards, and our staff and providers are held accountable to them. Protocols are care management steps, processes, and algorithms that are followed for patient care—they may stand alone or be incorporated into a policy. Guidelines are a set of evidence-based recommendations usually approved by an authoritative body. Order sets are practical tools to allow implementation of policies, protocols, and guidelines. Health care provider education topics were selected from drop-down menu options of “mandatory,” “optional,” or “not offered.” Patient education topics and data elements were selected from drop-down menu options of “yes” or “no.”
The diabetes champion from each hospital completed the tool, and the responses were collated into one workbook. We used a color-coding system enabled by Excel’s “conditional formatting” functionality to assist with quick and easy identification of the presence or absence of diabetes program components. Boxes on the Excel spreadsheet were coded as green, yellow, or red if a program component was fully present, partially present, or absent, respectively. Excel’s “data validation” functionality was also utilized to restrict responses entered into the tool to a series of predefined options (summarized above) to enable successful summarization across sites, though a free-text “comment” cell was also provided where applicable for respondents who for clarity’s sake felt the need to elaborate further on their responses. The tool was developed during February 2014, and diabetes champions at each hospital completed their assessments using the tool in March 2014. The results were collated and summarized, as we now outline, during April 2014.
For the purposes of this analysis, gaps were defined as those instances in which local resources, infrastructure, or processes demonstrated a variance against the current national evidence base or institutionally defined best practices.4–6 We assessed the following areas using our gap analysis tool: diabetes program infrastructure; protocols, policies, and order sets; patient and health care professional education; and data access (Table 1). These areas were identified and the assessment questions within each area composed based on the key structural components and activities of the JHH Inpatient Glucose Management Program,3 as identified by its physician leadership, standards by The Joint Commission Inpatient Diabetes Certification Program, ADA, AACE, and consensus opinion provided by the DCC (Table 1).
RESULTS
The first steps in any quality improvement process are to define, measure, and analyze the problem at hand. At a health system level, a gap analysis tool addresses each of these key steps and is an effective method of focusing efforts to improve care delivery. In this study, our gap analysis revealed significant variation in the structure, processes, resources, and leadership for diabetes care across our health system. We used the gap analysis results to demonstrate to our health system leadership that our current number of diabetes clinical full-time equivalent (CFTE) care providers is not adequate to meet the demands for outpatient diabetes care at our two academic hospitals. The summary format demonstrated gaps very clearly and enabled us to receive a commitment to grow our ambulatory diabetes program.
Identifying Gaps in Diabetes Care
Program Infrastructure.
We found significant variability in physician leadership for diabetes care, with three hospitals having a physician champion, and two hospitals having none (Table 2). There was significant variability in the inpatient and outpatient CFTEs across JHHS; for example, only one hospital had a centralized Glucose Steering Committee providing governance for issues related to inpatient glucose management. All of our hospitals lacked data analysis support. At the time of our survey, there was variability in the clinical information systems used, with two hospitals using Epic (Epic Systems Corporation, Verona, Wisconsin) only; one hospital using physician order entry (POE) inpatient and Epic ambulatory; one using MEDITECH (Medical Information Technology, Inc., Westwood, Massachusetts), Epic, and QS (GE Healthcare, Barrington, Illinois); and one using McKesson (McKesson Technology Solutions, Alpharetta, Georgia). The health system lacked a standardized method to collect data on hypoglycemic events and compliance with best-practice protocols.
Table 2.
inpatient Diabetes Program Infrastructure Gap Analysis Summary
| Overview | AH1 | AH2 | CH1 | CH2 | CH3 |
| Total Beds | 505 | 1059 | 256 | 318 | 233 |
| Physician Leadership | Yes | Yes | Yes | None | None |
| Program Support & Structure | AH1 | AH2 | CH1 | CH2 | CH3 |
| Diabetes FTEs: Inpatient RN | 0.0 | 0.5 | 0.0 | 0.3 | 0.3 |
| Diabetes FTEs: Inpatient NP | 1.0 | 2.5 | 0.0 | 0.0 | 0.0 |
| Diabetes FTEs: Inpatient RD | 1.0 | 0.0 | 0.0 | 0.0 | 1.0 |
| Certified Diabetes Educator (CDE) present | Yes | Yes | Yes | Yes | No |
| Number of Administrative Support FTEs | 0.3 | 1.0 | 0.0 | 0.0 | 0.0 |
| Number of Data Analysis FTEs | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Department/Committee That Program Reports to: | Education Program, Clinical Nutrition | Patient Safety Committee | Education, Training, and Research | None | Nursing Education |
| Centralized Glucose Steering Committee in Place? | No | Yes | No | No | No |
| Podiatry Services Available | Yes | No | No | No | No |
AH, academic hospital; CH, community hospital; FTE, full-time equivalent; NP, nurse practitioner; RD, registered dietitian
Protocols, Policies, and Order Sets.
Without centralized Glucose Steering Committees and variability in dedicated resources at each hospital, we found significant variation across JHHS in policies and protocols to ensure optimal inpatient glucose management, as shown in Table 3. Although there was little consistency in the types of protocols, most of our hospitals had protocols governing hypoglycemia management and point-of-care testing for glucose fingersticks. Most hospitals had order sets addressing intravenous and subcutaneous insulin management, although the content was variable and not uniform across the system.
Table 3.
Glucose Management Protocols and Policies Gap Analysis Summary
| Protocols and Policies | AH1 | AH2 | CH1 | CH2 | CH3 |
|---|---|---|---|---|---|
| Inpatient Hyperglycemic Management (for subcutaneous insulin) | None | Enforced Policy | Protocol or Guideline | Protocol or Guideline | Enforced Policy |
| Inpatient Hypoglycemic Management | Enforced Policy | Enforced Policy | Enforced Policy | Protocol or Guideline | Enforced Policy |
| IV Infusion Management | Protocol or Guideline | Enforced Policy | Enforced Policy | Protocol or Guideline | None |
| Continuous Tube Feeding Management | None | Protocol or Guideline | Enforced Policy | None | Enforced Policy |
| Inpatient Insulin Pump Management (external) | None | Enforced Policy | Enforced Policy | Protocol or Guideline | None |
| Insulin Pen Management | None | None | Enforced Policy | Protocol or Guideline | None |
| Point-of-Care Testing | Protocol or Guideline | Enforced Policy | Enforced Policy | Protocol or Guideline | Enforced Policy |
| Diabetic Ketoacidosis/Hyperosmolar State Management | Protocol or Guideline | Protocol or Guideline | None | Protocol or Guideline | None |
| Outpatient Hyperglycemic Management (for subcutaneous insulin) | None | None | Enforced Policy | None | None |
| Outpatient Hypoglycemic Management | None | None | Enforced Policy | None | None |
| Insulin Pump Essential Information Form and | None | Enforced Policy | None | None | Enforced Policy |
| Insulin Pump Basal/Bolus Daily Worksheet |
AH, academic hospital; CH, community hospital; IV, intravenous.
Patient Education.
All of our hospitals had patient education resources on almost every topic, and modalities varied from handouts to online videos. The sources of patient education materials varied across the system.
Health Care Professional Education.
Most of our hospitals lacked any form of formal training on inpatient glucose management principles for physicians/medical staff, and there was variability in diabetes education available for nursing, allied health (for example, dietitians, pharmacists), and support staff (Table 4).
Table 4.
Health Professional Education Gap Analysis Summary
| Faculty/Medical Staff Education | AH1 | AH2 | CH1 | CH2 | CH3 |
| Estimating total daily insulin dose required by patients. Howto divide it into basal, nutritional, and correction insulin. | Optional | Mandatory | Not offered | Not offered | Not offered |
| Guidelines for empirical adjustment of insulin to prevent hypoglycemia | Optional | Mandatory | Not offered | Not offered | Not offered |
| Guidelines for adjustment of insulin in response to hypo- or hyperglycemia | Optional | Mandatory | Not offered | Not offered | Not offered |
| Guidelines for avoiding insulin stacking | Optional | Mandatory | Not offered | Not offered | Not offered |
| Prescriber responsibilities for insulin pump use | Optional | Mandatory | Not offered | Not offered | Not offered |
| Oral and non-insulin injectable antidiabetic agents | Optional | Mandatory | Not offered | Not offered | Not offered |
| Nursing & Support Staff Education | |||||
| Understanding basal/nutritional/correction insulin therapy | Mandatory | Mandatory | Not offered | Not offered | Not offered |
| Oral antidiabetic agents | Optional | Optional | Not offered | Not offered | Not offered |
| Prevention and treatment of hypoglycemia | Mandatory | Mandatory | Not offered | Mandatory | Not offered |
| Diabetic ketoacidosis | Optional | Optional | Not offered | Not offered | Not offered |
| Type 1 versus type 2 diabetes | Mandatory | Mandatory | Not offered | Not offered | Not offered |
| Blood glucose monitoring | Mandatory | Mandatory | Not offered | Mandatory | Mandatory |
| Insulin administration and documentation | Mandatory | Mandatory | Not offered | Mandatory | Mandatory |
| Medical devices: Insulin pumps (nursing responsibilities) | Mandatory | Mandatory | Not offered | Mandatory | Mandatory |
| Medical devices: Insulin pens, glucometers | Mandatory | Mandatory | Not offered | Mandatory | Not offered |
| Transitions of care (inpatient area to inpatient area; inpatient to outpatient) | Mandatory | Mandatory | Not offered | Not offered | Not offered |
| Parenteral and enteral nutrition | Mandatory | Mandatory | Not offered | Not offered | Not offered |
| Patient diabetes education | Mandatory | Mandatory | Not offered | Not offered | Not offered |
| Carbohydrate identification and counting | Optional | Mandatory | Not offered | Not offered | Not offered |
AH, academic hospital; CH, community hospital.
Data Access.
At the time of our gap analysis, there was systemwide variation in the data systems that housed inpatient glucose readings and allowed identification of patients with diabetes. Consequently there was a systemwide inability to collect and analyze basic data related to glucose management. This limited our ability to plan and evaluate quality improvement interventions.
Development and Implementation of Interventions to Address Gaps in Diabetes Care
After completing the gap analysis, all members of the DCC met to identify priority areas in order to integrate and synergize diabetes care resources and efforts to enhance quality and reduce disparities in diabetes care across our health system. Through discussions with our institutional leaders and members of the DCC, we prioritized the gaps in program infrastructure; protocol, policies, and order sets; health care professional education; and automated data access—but not patient education—as shown in Table 5, which also summarizes our interventions to address them. The results of our analysis were presented in several executive leadership forums to help garner resources to support progress in these areas.
Table 5.
Priority Areas and Proposed Interventions to Reduce Disparities in Diabetes Care Delivery Across Johns Hopkins Health System
| Johns Hopkins Hospital Glucose Management Program Conceptual Framework Component* | Gap Analysis Tool Component | Primary Identified Gap | Interventions |
|---|---|---|---|
| Centralized Glucose Management Program | Program Infrastructure | Only one hospital with centralized Inpatient Glucose Management Program and Steering Committee Variability in diabetes clinicians Variability in clinical information system used Lack of data analysis support at all hospitals Lack of diabetes-focused practitioners at each institution Lack of uniform podiatry services |
To be addressed |
| Development and Implementation of Glucose Management Program | Protocols, Policies, and Order Sets | Lack of standardization in glucose management policies and practice |
|
| Improved Knowledge | Health Care Professional Education | Lack of standardized approach to training health professionals on inpatient glucose management | National Institutes of Health-funded grant to:
|
| Improved Knowledge | Patient Education | No significant gap identified | — |
| Evaluate Glucose Management Program | Automated Data Access | Lack of standardization in obtaining glucose management, economic, and quality diabetes elements |
|
See Reference 3.
Program Infrastructure: Variability in Inpatient Diabetes Management Program Infrastructure
At the time of our survey in March 2014, only one adult hospital in our system had a centralized glucose management program overseen by a steering committee, and three of five hospitals had physician champions. Based on the success of our program at JHH, one of our community hospitals hired a full-time inpatient diabetes endocrinolo-gist who has established a successful hospitalwide Glucose Steering Committee and is harmonizing the hospital’s glucose management policies with those of the two JHHS academic adult hospitals. We are working collaboratively with one of our other community hospitals to prepare a business plan to support the hiring of inpatient diabetes clinicians. We still have a dearth of podiatry services in our health system, and the DCC will address this with our leadership in the future. In March 2014 there was also variability in the clinical information systems used in our health system; however, as of July 1, 2016, all of our hospitals will use Epic in the ambulatory and inpatient setting as the EHR. This will also enable us to develop and abstract uniform glucose metrics with analytic support provided across the system through the AI DCC.
Protocols, Policies, and Order Sets
Lack of Standardization in Glucose Management Policies and Practices.
Because all of our hospitals will now use the same EHR, the DCC saw this as an opportunity to harmonize our current glucose management order sets and practices. The two hospitals in our academic divisions have harmonized their Epic order sets for management of intravenous and subcutaneous insulin and treatment of hypoglycemia in the hospital. These efforts have been facilitated by a dedicated programmer and a project team provided by our institution to support this important work. Our academic division hospitals have also aligned their policies to be consistent and plan to have this fully implemented by July 1, 2016. Two of our community division hospitals now have physician champions, and they have also expressed interest in adopting the same order sets and policies as those in our academic division. The DCC is also spear-heading development of an ambulatory diabetes management algorithm that will be integrated into Epic and used by all of the ambulatory practices in our health system. Our ultimate goal is to have an evidence-based, unified JHHS approach to inpatient and outpatient diabetes management, and we plan to develop a JHHS Glucose Steering Committee through the DCC to oversee ongoing protocol, policy, and order set harmonization.
Health Care Professional Education
Lack of Standardized Approach to Training Health Professionals on Inpatient Glucose Management.
Insulin is one of the highest-risk medications used in the hospital, and glucose mismanagement can contribute to patient harm in this setting;7–10 therefore it is critical for our health professionals, particularly physicians and nurses, to be trained in safe, evidence-based glucose management principles. One area that stood out in the gap analysis was the disparity in prescriber (for example, physician) and nursing staff diabetes education throughout our health system. Given the importance of prescriber and nursing education in improving clinical outcomes in hospitalized patients with diabetes, the DCC prioritized this area for synergy and integration.
We previously showed that development of a diabetes nursing “superuser” program at one of our academic hospitals was critical to implementing the hypoglycemia policy nursing interventions. Following the establishment of hospitalwide glucose management policies and order sets for hypoglycemia and hyperglycemia, the nursing diabetes superuser education program, and clinical decision support tools for prescribers, there was a significant and sustained reduction in the incidence of hypoglycemia (~20%) over a three-year time period.3,11 However, the incidence of severe hyperglycemia was not significantly reduced by these interventions,3,11 indicating a differential impact of the program on hyperglycemia compared to hypoglycemia. We believe that this disparity was due to the hypoglycemia policy being implemented by the nursing staff, whereas the hyper-glycemia policy and order set were implemented by prescribers (for example, house staff, hospitalists). Given our nursing program’s success in contributing to sustained reduction in hypoglycemia, we hypothesize that an analogous diabetes prescriber superuser program, targeting physicians, will be an effective educational approach to addressing persistent hyperglycemia. To support development of the physician education program, we submitted and were successful in obtaining a grant proposal in response to the National Institute of Diabetes Digestive and Kidney Diseases PAR-13–367, “Planning Grants for Pragmatic Research in Healthcare Settings to Improve Diabetes Prevention and Care (R34).” We were able to use the summary tables from the gap analysis as preliminary data in our grant application to visually demonstrate the lack of a consistent approach to educating physician and nursing staff across our health system. This also demonstrated to our reviewers that key stakeholders in diabetes management across our health system are aligned around the same priorities, making our efforts likely to be successful. Our specific aims are as follows:
To develop the diabetes prescriber superuser educational curriculum through JHHS stakeholder community engagement
To refine and package the JHH diabetes nursing and prescriber superuser educational curricula into an electronic toolkit and disseminate it locally to the two JHHS hospitals, based on stakeholder feedback
To evaluate the impact of implementing the JHH diabetes nursing and prescriber superuser programs at two JHHS hospitals on glycemic clinical outcome measures. We will secondarily assess the program’s impact on glycemic process and economic measures.
If our educational approach is successful, we will disseminate it to the remaining two community hospitals in our system and apply for a larger grant to disseminate it into other health systems in need of health care provider diabetes education tools.
Automated Data Access
Lack of Access to Automated Data Collection and Analytics.
One barrier to collecting and analyzing systemwide data related to glucose management was the variability in clinical information systems. As mentioned, all JHHS hospitals will be using Epic, which will enhance our ability to generate a systemwide dashboard to summarize in-patient and outpatient glycemic metrics as well as economic measures (for example, hospital length of stay). Having a functional, dynamic, systemwide glucose/diabetes dashboard will allow us to identify areas of our system in need of interventions, to evaluate the impact of those interventions, and to determine the sustainability of our interventions.
Benefits of Standardization and Integration
There is a natural tension between standardization and improvements in care championed locally by clinicians. There are several benefits to standardizing care across a health system:(1) enhancing patient safety by implementing clinical care delivery guidelines known to improve outcomes and reducing errors when clinicians practice at multiple sites within a system; (2) eliminating practice patterns that lack a strong evidence base for improving clinical outcomes; and (3) decreasing costs by negotiating better contracts for supplies, medications, and equipment as a system instead of individual institutions. Even with standardization, however, it is important to allow flexibility for local adaptation within these guidelines of excellence to ensure clinician engagement and adherence and to allow for innovations as new evidence-based approaches emerge.
Gap Analysis Methodology
Various methods and resources have been used to conduct gap analyses in health care, including experience and expertise of planning members, stakeholder engagement, literature review, population health data, government policy, clinical care guidelines, and public opinion.12 Examples of gap analysis tools include spreadsheets, tables, fishbone analyses, and surveys. The Agency for Healthcare Research and Quality has developed a gap analysis tool, which organizes relevant information in a table format,13 and is adaptable in multiple settings. Although gap analyses can inform improvement efforts, there is not clear evidence to favor a specific method or software in conducting a gap analysis. The advantages to using a gap analysis tool to inform quality improvement efforts is that it allows for a detailed and systematic assessment of multiple aspects of a health care system or program that is based on objective evidence. The use of a tool also facilitates its dissemination to other organizations and adaptation to the local environment. In addition, data collected using a gap analysis tool can assist a health care organization in assessing its resources and performance as part of a larger assessment required to identify areas for intervention to produce operationally excellent and performance- and culture-driven organizations using a framework such as the Shingo Prize for Operational Excellence14 or the Malcolm Baldrige Excellence Framework.15 For example, in the “Measurement, Analysis, and Knowledge Management” category, the Baldrige assessment asks, “How do you select, collect, align, and integrate data and information to use in tracking daily operations and overall organizational performance?”15 In this setting, a gap analysis tool can complement tools within the framework to help identify areas for standardization, alignment, and integration. The disadvantage is that it requires a time commitment to adequately assess each component of the tool and is more complex to score than a simpler checklist.
We chose an Excel-based gap analysis tool, given widespread familiarity with this software and ease of use. It has proven to be an important tool to summarize care delivery disparities in a succinct and easy-to-digest manner, allowing us to garner additional resources—both intramural and extramural—to support our diabetes quality improvement and integration efforts. A limitation of our approach is that we did not use a formal stakeholder engagement process, such as the Delphi method, which uses iterative rounds of response by group members, providing aggregated feedback about other members’ responses until consensus is reached among stakeholders.16 Although we did not use this formal process to reach consensus on initial priority areas of focus, we did have engagement from key stakeholders at each hospital in our health system and aligned our priorities with our institution’s overall focus.
CONCLUSION
We have developed a gap analysis tool that is adaptable to assessing resources and gaps in care in other disease areas in a health system with both inpatient and ambulatory components. Systematic ways to identify disparities in quality of care across a system are critical to developing effective, value-based approaches to delivering safe, high-quality care. Further studies are needed to compare the effectiveness of different gap analysis methodologies in improving health care delivery processes.
Supplementary Material
Acknowledgments.
The authors thank the Armstrong Institute for Patient Safety and Quality of Johns Hopkins Medicine for its support of the Diabetes Clinical Community. We acknowledge the members of their Diabetes Clinical Community who assisted in completing the gap analysis tool at their institutions: Theresa Kemmerer, RN, MSc, APN, CDE, and Holly Bashura, RN, CRNP, CDE (Johns Hopkins Hospital); Susan Yesavage, MA, RD, CDE (Johns Hopkins Bayview Medical Center); Mike Taylor, RN, MHA, CDE (Howard County General Hospital); Rose Oshinsky, RN, CDE (Sibley Memorial Hospital); and Patricia Rios, RN (Suburban Hospital).
Funding Support.
Dr. Sherita Golden was supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R34 DK105460).
Footnotes
Conflicts of Interest.
All authors report no conflicts of interest.
ONLINE-ONLY CONTENT
See the online version of this article for Appendix 1. Johns Hopkins Health System Diabetes Care Gap Analysis Tool
REFERENCES
- 1.Maryland Health Services Cost Review Commission. Completed Agreements Under the All-Payer Model: Global Budget Revenue Overview Presentation. Accessed Oct 30, 2016 http://www.hscrc.maryland.gov/gbr-tpr.cfm.
- 2.Gould LJ, et al. Clinical communities at Johns Hopkins Medicine: an emerging approach to quality improvement. Jt Comm J Qual Patient Saf. 2015;41:387–395. [DOI] [PubMed] [Google Scholar]
- 3.Munoz M, et al. Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt Comm J Qual Patient Saf. 2012;38:195–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ACE/ADA Task Force on Inpatient Diabetes. American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control. Endocr Pract. 2006;12(suppl 3):4–13. [DOI] [PubMed] [Google Scholar]
- 5.Moghissi ES, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32:1119–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Joint Commission. Certification in Inpatient Diabetes. Accessed Oct 30, 2016 http://www.jointcommission.org/certification/inpatient_diabetes.aspx.
- 7.Amori RE, et al. Inpatient medical errors involving glucose-lowering medications and their impact on patients: review of 2,598 incidents from a voluntary electronic error-reporting database. Endocr Pract. 2008;14:535–542. [DOI] [PubMed] [Google Scholar]
- 8.Brutsaert E, Carey M, Zonszein J. The clinical impact of inpatient hypoglycemia. J Diabetes Complications. 2014;28:565–572. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, et al. National trends in patient safety for four common conditions, 2005–2011. N Engl J Med. 2014. January 23; 370:341–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eiland L, et al. Inpatient hypoglycemia: a challenge that must be addressed. Curr Diab Rep. 2014;14:445. [DOI] [PubMed] [Google Scholar]
- 11.Kemmerer T, et al. The impact of nursing and advanced practice clinicians on the implementation and outcomes of an inpatient glucose management orogram. AADE Pract. 2015;3:17–25. [Google Scholar]
- 12.University of Toronto Faculty of Medicine, Office of Continuing Education and Professional Development. Quick Tips: Initiating a Learning Needs Assessment—Gap Analysis of Health Care Issues. Accessed Oct 30, 2016 http://www.cpd.utoronto.ca/newsletter/2009_fall/Quick_Tips_initiating_a_learning_needs_assesment__Gap_Analysis_of_health_care_issues.pdf.
- 13.Agency for Health Care Research and Quality. Toolkit for Using the AHRQ Quality Indicators. 2016. Accessed Oct 30, 2016 http://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/qitoolkit/combined/combined_toolkit.pdf.
- 14.Shingo Institute. The Shingo Prize for Operational Excellence. Accessed Oct 30, 2016 http://www.shingoprize.org/challengefortheprize.
- 15.Baldrige Performance Excellence Program. 2015–2016 Baldrige Excellence Framework: A Systems Approach to Improving Your Organization’s Performance (Health Care). Gaithersburg, MD: US Department of Commerce, National Institute of Standards and Technology, 2015. [Google Scholar]
- 16.Delbecq AL, van de Ven AH, Gustafson DH. Group Techniques for Program Planning: A Guide to Nominal Group and Delphi Processes. Glenview, IL: Scott, Foresman, 1975. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.