Abstract
Background and Purpose:
Depression affects millions of adolescents in the United States each year. This population may benefit from targeted preventive interventions. We sought to understand the internal factors that affect the ability of healthcare organizations to implement an intervention that involves mental health screening and depression prevention treatment of at-risk adolescents in primary care settings.
Methods:
From November 2011 to July 2016 we conducted a study of the implementation of a multisite (N=30) phase 3 randomized clinical trial of an Internet-based depression prevention intervention program (CATCH-IT). We describe the prevalence of internal barriers on the screening and enrollment process by reporting REACH (the proportion of target audience exposed to the intervention).
Results:
A total of 369 adolescents were randomized into the intervention or control program. Mean REACH values for the study clinics were 0.216 for screening and 0.181 for enrollment to CATCH-IT. Mean REACH enrollment lost due to internal barriers was 0.233. This translated to 4,691 adolescents lost at screening and 2,443 adolescents lost at enrollment due to internal barriers.
Conclusion:
We propose a model of the implementation process that emphasizes the importance of positive relational work that assists in overcoming internal barriers to REACH. We also provide implications for policy and practice.
Keywords: mental health, adolescent, primary health care, health care reform, delivery of health care
Introduction
It is estimated that 13–20% of adolescents living in the United States experience depression in any given year (Angold et al., 2002; National Research Council and Institute of Medicine, 2009; World Health Organization, 2014). Adolescents with depression have a higher incidence of physical illness and social problems (Janssens, Rosmalen, Ormel, van Oort, & Oldehinkel, 2010; Khalil et al., 2010; Knapp, King, Healey, & Thomas, 2011), and are at elevated risk for suicide and recurrent depressive episodes throughout their lifetimes (Keenan-Miller, Hammen, & Brennan, 2007; Pettit, Lewinsohn, Roberts, Seeley, & Monteith, 2009). In the last decade, the field of public health has begun exploring complex psychosocial preventive interventions that use technology to target high-cost conditions such as depression (Arnberg, Linton, Hultcrantz, Heintz, & Jonsson, 2014; Lokkerbol et al., 2014; Van Voorhees et al., 2011). We developed CATCH-IT (Competent Adulthood Transition with Cognitive-Behavioral Humanistic and Interpersonal Training), a 14-module Internet-based depression prevention intervention, to help address the needs of adolescents who are not receiving adequate mental health services.
External Barriers
Implementation of an intervention may be affected by political, organizational, and behavioral factors—both external and internal to healthcare organizations—that may delay or inhibit administration. Examples of external barriers include unanticipated events such as economic downturn, strict healthcare regulations, and terrorist attacks; these factors may restrict the time available for clinics to participate in an intervention or force a clinic to redistribute resources (McAlearney, Walker, Livaudais-Toman, Parides, & Bickell, 2016). Governmental policy regulations such as the Affordable Care Act of 2010 and the Health Insurance Portability and Accountability Act of 1996 may have complex overlapping policies and regulations that are designed to protect patient policy but actually impede the ability of policy makers to implement interventions (Bova, Drexler, & Sullivan-Bolyai, 2012; Midkiff et al., 2016; Ness, 2007). These external barriers may reduce the proportion of the target population that receives an intervention. However, it is difficult to quantify how much participation is reduced because of these external events and policies.
Internal Barriers
We now focus on internal barriers potentially relevant to successful implementation of our intervention. Our previous studies on the implementation of CATCH-IT during a phase 2 clinical trial, conducted from 2007–2010, considered internal barriers that prevented the intervention from reaching the target population. Internal barriers may relate to parent, adolescent, and primary care stakeholders. Our previous work describing such internal barriers included the varying intrinsic levels of motivation in adolescents who entered the study and the perceived authority of the physician from the adolescent perspective (Iloabachie et al., 2011; Ruby, Marko-Holguin, Fogel, & Van Voorhees, 2013; Van Voorhees et al., 2009). Other organizational internal barriers may include limited time and reimbursement for services, poor staff education and training, general disinterest or lack of knowledge in mental health prevention, poor administrative support for clinic staff during screenings, and lack of effective communication between members of the medical team (Hacker et al., 2013; Josyula & Lyle, 2013).
Internal barriers to successful implementation of an intervention can be quantified using the REAIM framework [Reach Effectiveness – Adoption Implementation Maintenance], which assesses the public health impact of an intervention in a real-world setting. We incorporated this framework with a focus of REACH on the proportion of the target audience exposed to the intervention (Eisen et al., 2013) to measure a site’s ability to screen at-risk adolescents. If an intervention focused on prevention cannot reach the target at-risk population, it is unlikely, no matter how effective the intervention, to significantly contribute to public health. Understanding REACH lost, and the contributory internal barriers, is a key step to successfully implementing a public health intervention in the current healthcare system. While several studies report REACH lost to various causes (Chung, Lee, Morrison, & Schuster, 2006; Sareen et al., 2007; Uema, Vega, Armando, & Fontana, 2008), to our knowledge this is the first report that quantifies and examines these internal barriers in relation to adolescent mental healthcare.
The focus of this paper is on the implementation of the recruitment process. We sought to describe the potential impact of internal barriers, how study staff worked to surmount these barriers, and the capability to implement mental health screening and treatment of at-risk adolescents within seven health systems.
Methods
Study Design
From February 2012 to July 2016, we recruited participants for a phase 3 randomized clinical trial comparing the efficacy of CATCH-IT to a general health education control intervention program for preventing the onset of depressive episodes in an intermediate to high-risk group of adolescents. Recruitment occurred at a total of 30 sites centered in pediatric primary clinics in seven healthcare systems within urban and suburban areas of Chicago, IL, and Boston, MA. The analyses in this study involved clinics with medical assistants and/or registered nurses who conducted screenings for at least four months.
Adolescents between the ages of 13 and 18 were screened in a two-step process. First, at the primary care office, they answered a two-item questionnaire based on the Patient Health Questionnaire-Adolescent (PHQ-A) (Richardson et al., 2010). Next, as a part of the phone screening process, they were assessed using a 10-item shortened scale of the Center for Epidemiologic Studies Depression (CES-D) (Garrison, Addy, Jackson, McKeown, & Waller, 1991). In addition to this routine screening, letters inviting participation were sent to registered patients, or their parents, who had visited the clinics in the previous two years and were within this age range; interested families contacted us for a phone screen to determine eligibility. Inclusion criteria included either a past major depressive disorder diagnosis, or a CES-D score of 8–17 (scores of 18–20 were considered with permission of the principal investigators). Anyone with a current diagnosis of major depressive disorder, comorbid mental health diagnosis of schizophrenia (current or past) or bipolar affective disorder, serious suicide risk, or alcohol/drug disorder was excluded. A complete description of the intervention and trial methods has been previously published (Gladstone et al., 2015).
Staff Training and Monitoring
The original communication and management strategy was revised during the course of the trial. We originally intended to show a professionally produced comprehensive study training video for 55 minutes. The intent of the video was to expedite implementation, reduce staff time devoted to training sites, and ensure consistency by essentially following a corporate training model. Similarly, we intended for staff to follow a very carefully developed communication strategy with adolescent and family participants to guarantee there was no confounding of study arms with extensive conversation at enrollment and the follow-up assessment points. These strategies did not resonate with staff and participants. Office staff reported feeling “off put” and “disengaged” from these videos and the structured communication strategies, which resulted in minimal participation in the study model. With regard to adolescent participants, we noted substantial problems maintaining interest and engagement in the trial. Additionally, study participants reported they felt study staff “were like robots” in conducting carefully scripted structured psychiatric interviews at baseline. Therefore, this training model was re-evaluated and revised as we were enrolling participants.
The principal investigators and staff developed new models placing all elements of the project into a relationship-centered and authentic (nonviolent) communication model (Nosek, 2012) with a particular focus on maintaining authenticity and sincerity. Based on work with theory of healthcare teams (DeFrino, 2009; Mickan & Rodger, 2005), staff were retrained to work on relationship building to develop trust before their actual training. Similarly, a consultant was engaged to revise the corporate engagement model. This revised approach included the shared motivations of the stakeholders to successfully complete the trial.
Sample/Data Collection
Over 40,000 adolescents were contacted for this study. A total of 439 participants were recruited and enrolled; of these, 369 were randomized into the CATCH-IT or health education program. The rest were dis-enrolled after the baseline assessment due to exclusion criteria that were found in the assessment. In this design, participants were assessed at time points of 2, 6, 12, 18, and 24 months. We collected data for each clinic from the beginning of the potential recruitment period through July 2016.
Measures Development of REACH Screening and Enrollment
We estimated that 21% of adolescents would initially screen positive based on PHQ-A scores, and that adolescents visit their primary care provider (PCP) once every 18 months (Uema, Vega, Armando, & Fontana, 2008; Van Voorhees, Melkonian, Marko, Humensky, & Fogel, 2010). Based on these estimates, we developed an equation to measure the proportion of the target audience that was assessed at each clinic of REACH screening. For those sites where months of screening participation was greater than 18 months we capped the value at 18 months. This was done because after 18 months, we assumed that all patients would have circulated through the clinic once.
Enrollment was defined as adolescents who completed baseline assessments. We determined that 6.8% of adolescents we screened would meet the criteria for study enrollment and be at risk for MDE (Jones, 2008). The proportion of the target audience at each clinic that was exposed to the intervention was calculated by REACH enrollment. For those sites where months of screening participation was greater than 18 months we capped the value at 18 months. This was done because after 18 months, we assumed that all patients would have circulated through the clinic once.
REACH Enrollment Lost to Internal Barriers
REACH enrollment lost to internal barriers was quantified by the difference between the theoretical gold standard for REACH enrollment and the REACH enrollment performance at each site. We defined the gold standard as the mean value of the three largest REACH enrollment values excluding the top outlying clinic with the highest REACH. Sites with negative values were considered as 0.00 REACH lost, as these sites would have performed better than the gold standard. Sites that were included in the calculation for mean value were considered to have REACH lost if the REACH enrollment value was above the gold standard value.
Analyses
The REACH Screening equation was: (number of positive screens)/[(total number of adolescent patients) × (0.21) × (months of screening participation/18)]. The REACH enrollment equation was: (number of enrollments)/[(total number of adolescent patients) × (0.068) × (months of participation/18)]. REACH enrollment lost to internal barriers was: (Gold standard REACH enrollment - REACH enrollment at the individual site).
We calculated the number of adolescents we expected to screen positive = (total number of adolescent patients) × (0.21). Our measure of total adolescents lost to screening barriers = expected positive screens – observed positive screens. We calculated the number of adolescents at risk for MDE = (total number of adolescent patients) × (0.068). Adolescents lost to enrollment barriers = adolescents at risk for MDE – number of adolescents enrolled. A negative value for lost to enrollment was considered as 0.
Results
REACH Screening and Enrollment
Of the 30 participating clinics, there were 42,310 adolescents with data available from 29 clinics. Table 1 shows that for the Chicago sites, clinics yielded an average REACH screening of 0.216 (range: 0.034 to 0.591). As positive screen totals were not collected at the Boston sites, we could not calculate REACH screening for those sites. Across all clinics (N=30), 439 were enrolled through screening over an average of 27.6 months per site. Among clinics with total patients screened (N=29) the average REACH Enrollment was 0.181 (range: 0.009 to 1.023). Table 2 shows that 2,877 were identified as at risk for a major depressive episode.
Table 1.
REACH Lost at Chicago and Boston Sites
| PATH Site | Patients | Months of Screening | Positive Screens | REACH Screeninga | Number Enrolled | REACH Enrollmentb | REACH Lost to Internal Barriersc |
|---|---|---|---|---|---|---|---|
| Chicago 1 | --- | 8 | 68 | --- | 3 | --- | --- |
| Chicago 2 | 1,568 | 15 | 33 | 0.120 | 10 | 0.113 | 0.276 |
| Chicago 3 | 2,500 | 44 | 95 | 0.181 | 35 | 0.206 | 0.183 |
| Chicago 4 | 4,120 | 8 | 102 | 0.265 | 12 | 0.096 | 0.293 |
| Chicago 5 | 1,947 | 6 | 8 | 0.059 | 8 | 0.181 | 0.208 |
| Chicago 6 | 1,200 | 23 | 43 | 0.171 | 15 | 0.184 | 0.205 |
| Chicago 7 | 2,500 | 23 | 88 | 0.168 | 36 | 0.212 | 0.177 |
| Chicago 8 | 1,400 | 25 | 148 | 0.503 | 28 | 0.294 | 0.095 |
| Chicago 9 | 800 | 14 | 14 | 0.107 | 2 | 0.047 | 0.342 |
| Chicago 10 | 1,485 | 12 | 7 | 0.034 | 1 | 0.015 | 0.374 |
| Chicago 11 | 589 | 44 | --- | --- | 8 | 0.200 | 0.189 |
| Chicago 12 | 862 | 44 | 107 | 0.591 | 20 | 0.341 | 0.048 |
| Chicago 13 | 1,568 | 44 | 20 | 0.061 | 1 | 0.009 | 0.380 |
| Chicago 14 | 5,091 | 54 | 488 | 0.456 | 86 | 0.248 | 0.141 |
| Chicago 15 | 500 | 33 | 24 | 0.229 | 2 | 0.059 | 0.330 |
| Chicago 16 | 500 | 34 | 19 | 0.181 | 1 | 0.029 | 0.360 |
| Chicago 17 | 450 | 33 | 25 | 0.265 | 14 | 0.458 | 0.000 |
| Chicago 18 | 1,487 | 24 | 46 | 0.147 | 4 | 0.040 | 0.349 |
| Chicago 19 | 450 | 34 | 12 | 0.127 | 2 | 0.065 | 0.324 |
| Boston 1 | 733 | 50 | --- | --- | 51 | 1.023 | 0.000 |
| Boston 2 | 320 | 19 | --- | --- | 8 | 0.368 | 0.021 |
| Boston 3 | 1,922 | 41 | --- | --- | 33 | 0.252 | 0.137 |
| Boston 4 | 803 | 39 | --- | --- | 10 | 0.183 | 0.206 |
| Boston 5 | 3,000 | 32 | --- | --- | 15 | 0.074 | 0.315 |
| Boston 6 | 800 | 31 | --- | --- | 7 | 0.129 | 0.260 |
| Boston 7 | 1,015 | 29 | --- | --- | 8 | 0.116 | 0.273 |
| Boston 8 | 350 | 9 | --- | --- | 1 | 0.084 | 0.305 |
| Boston 9 | 550 | 7 | --- | --- | 1 | 0.069 | 0.320 |
| Boston 10 | 2,000 | 34 | --- | --- | 11 | 0.081 | 0.308 |
| Boston 11 | 1,800 | 15 | --- | --- | 6 | 0.059 | 0.330 |
| Total | 42,310 | 828 | 1,347 | NA | 439 | NA | NA |
| Mean | 1,458.97 | 27.60 | 74.83 | 0.216 | 14.63 | 0.181 | 0.233 |
Note: NA=not applicable
Proportion of the total number of adolescents seen at each clinic who screened positive during the screening months and were expected to screen positive
Proportion of the total number of adolescents seen at each clinic who were enrolled during the study and were expected to enroll
Difference between the average REACH enrollment of the top-performing sites and the proportion of adolescents enrolled at each clinic
Table 2.
Adolescents Lost at Screening and Enrollment
| PATH Site | Expected Positive Screens | At Risk for MDE | Lost Screening | Lost Enrollment |
|---|---|---|---|---|
| Chicago 1 | --- | --- | --- | --- |
| Chicago 2 | 329 | 107 | 296 | 97 |
| Chicago 3 | 525 | 170 | 430 | 135 |
| Chicago 4 | 865 | 280 | 763 | 268 |
| Chicago 5 | 409 | 132 | 401 | 124 |
| Chicago 6 | 252 | 82 | 209 | 67 |
| Chicago 7 | 525 | 170 | 437 | 134 |
| Chicago 8 | 294 | 95 | 146 | 67 |
| Chicago 9 | 168 | 54 | 154 | 52 |
| Chicago 10 | 312 | 101 | 305 | 100 |
| Chicago 11 | 124 | 40 | --- | 32 |
| Chicago 12 | 181 | 59 | 74 | 39 |
| Chicago 13 | 329 | 107 | 309 | 106 |
| Chicago 14 | 1,069 | 346 | 581 | 260 |
| Chicago 15 | 105 | 34 | 81 | 32 |
| Chicago 16 | 105 | 34 | 86 | 33 |
| Chicago 17 | 95 | 31 | 70 | 17 |
| Chicago 18 | 312 | 101 | 266 | 97 |
| Chicago 19 | 95 | 31 | 83 | 29 |
| Boston 1 | 154 | 50 | --- | 0 |
| Boston 2 | 67 | 22 | --- | 14 |
| Boston 3 | 404 | 131 | --- | 98 |
| Boston 4 | 169 | 55 | --- | 45 |
| Boston 5 | 630 | 204 | --- | 189 |
| Boston 6 | 168 | 54 | --- | 47 |
| Boston 7 | 213 | 69 | --- | 61 |
| Boston 8 | 74 | 24 | --- | 23 |
| Boston 9 | 116 | 37 | --- | 36 |
| Boston 10 | 420 | 136 | --- | 125 |
| Boston 11 | 378 | 122 | --- | 116 |
| Total | 8,885 | 2,877 | 4,691 | 2,443 |
Note: MDE=Major Depressive Episode
REACH Lost to Internal Barriers
Table 1 shows that the top three performing clinics from both the Chicago and Boston sites, excluding the top outlier clinic, obtained REACH Enrollments of 0.458, 0.368, and 0.341, providing a gold standard (based on the “average” of these high performing clinics) of 0.389. REACH lost to internal barriers had a mean of 0.233 across all sites. A total of 4,691 adolescents were lost to screening barriers, and 2,443 adolescents were lost to enrollment barriers.
Implementation Model
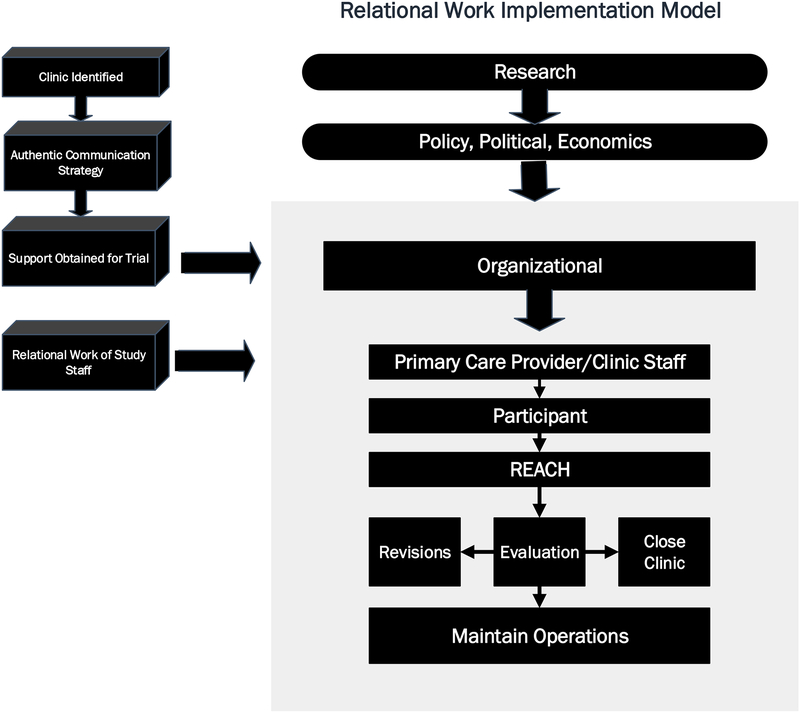
We developed a Relational Work Implementation Model (Figure 1) based upon our study experience that we describe below. The participant is the focus of this process, with the outcome of the research process embedded in the participant. As the model shows, the study staff works with the PCP and clinic staff to engage the participant. However, this participant engagement process can be potentially hindered by various internal organizational barriers of clinic operational challenges. Ongoing relational communication work with study staff increases motivation among PCPs and clinic staff to continue the screening and participation in the study.
Figure 1:
The Relational Work Implementation Model is based on a participant-centered approach to the research process
The specific relational work that was used to affect REACH included the impact of the PCP influence on the medical staff and the participant, the relationship between the clinic staff and the participant, and the importance of consistent, relational communication between the study staff and the clinic staff. For optimal screening, there had to be consistent and welcomed interaction between study staff and clinic staff where troubleshooting, appreciation, and gratitude were regularly expressed to the clinic staff and PCPs. This genuine acknowledgement of appreciation and occasional apologies for difficulties with the study, in any situation, was effective and necessary.
Further, relational work is key to motivating and maintaining active adherence in the study despite the mounting barriers. For example, PCP involvement in discussing the clinical experiences of treating adolescents with depression helped motivation in the study. The feeling of professional obligation to address mental health concerns in adolescents encouraged PCPs to fight through the daily internal barriers. In a similar manner, certain medical assistants developed a sustained motivation by recognizing the importance of their role in mental health screening in the care of adolescent patients. As the study progressed, an increased confidence in the staffs’ ability to deliver the screening tool was recognized, which improved communication with the patients.
Throughout, the Relational Work Implementation Model is a fluid and consistent evaluation by study staff. It is strengthened by relational involvement in evaluation of the progression of the study within the clinic. If the study staff are able to surmount internal organizational barriers, then any necessary revisions can be made and then incorporated into the study staff’s work with the PCPs and clinic staff.
Discussion
Using the REACH component of the RE-AIM model to quantify the portion of adolescents at risk for depression who were identified through screening, we found a mean REACH screening of 0.216. The mean REACH enrollment was 0.181 across all sites, with the included gold standard sites achieving REACH enrollments of 0.458, 0.368, and 0.341 respectively. Internal barriers to screening and enrollment accounted for a mean REACH lost of 0.233.
REACH enrollment in this study may be lower than that observed for other prevention services. When investigating the success of the currently accepted prevention protocols for osteoporosis, human papillomavirus (HPV), and colon cancer, approximately 45–65% of eligible patients adhere to screening recommendations (Frazier, Colditz, Fuchs, & Kuntz, 2000; Meissner, Breen, Klabunde, & Vernon, 2006; Miller et al., 2005; Zhang et al., 2012), and 60–75% of these patients return for follow-up with their physicians (Paskett, White, Carter, & Joseph, 1990; Vijan, Hwang, Hofer, & Hayward, 2001). Averaging these REACH values yields a mean REACH enrollment of 0.292, which is higher compared to the 0.181 obtained in this study. However, as a trial screening protocol, we believe our approach is a feasible preventive intervention for adolescent depression. Barriers specific to our particular intervention, mental health prevention, and/or the present healthcare environment may explain this difference (Baker et al., 2010; Carnevale, 2013).
Internal barriers are important to address in the early stages of implementation. In this study, over 2,000 adolescents were not enrolled in the intervention because of internal barriers. Screening and engaging adolescents in primary care for the purpose of depression prevention involves both the choreography of complex practice activities and also a heightened level of emotional engagement between staff, adolescents, and parents. Others too have noted the challenge of introducing into the busy primary care workflow conversations with substantial prospect of emotional content which may cause either distress by staff from contact with these emotions or slow the medical activities of the practice.(Asarnow, Jaycox, & Anderson, 2002; Meredith et al., 1999).
Relational work between the PCPs, medical staff, parents, study staff, and the adolescents can help alleviate the REACH lost to internal barriers in clinical practice (Becker & Maiman, 1980; Charlton, Dearing, Berry, & Johnson, 2008; Gittell, Godfrey, & Thistlethwaite, 2013; Kaplan, Greenfield, & Ware, 1989). We found that working with the staff to instill a high level of motivation in the study by maintaining relational communication between study staff and clinic staff can strengthen and sustain a high efficacy of screening and enrollment. Also, as adolescents see the dedication and motivation of their PCP and medical staff, they are more likely to fill out the screening questionnaire and follow-through with treatment. In such situations, REACH improves (Kyngäs, Hentinen, & Barlow, 1998). Study staff, PCPs, and clinic staff members must maintain open and frequent conversations to move forward with the study and maintain momentum.
The Relational Work Implementation Model demonstrates the plausible internal barriers that ultimately impact the participant or, in nonresearch settings, the patient and population as a whole. It brings further explanatory power to the implementation process. Our model is similar to a nonlinear theory model cited in Coryn and colleagues (2011) that assesses planning and implementation of a program. Their model, like ours, includes a change model that actively responds to occurrences and needs during the implementation process. We too consider how internal barriers impact study implementation. Our model allows researchers and all stakeholders a clear view of how a study is implemented, in addition to whether the intervention is successful.
To our knowledge this is the first report that quantifies barriers to an adolescent preventive mental health intervention in primary care. A strength of our study is our use of actual clinics instead of simulated encounters, which allowed us to observe the problems that routinely arise in the current healthcare system. The study is highly generalizable due to the large sample of participants and clinics involved, and their locations in urban and suburban locations. Furthermore, our study spanned five years.
Limitations
Limitations of the study include the methods by which REACH lost to internal barriers was constructed in reference to the definition of “gold standard.” Due to the limited research available on the utilization of depression prevention interventions, and also more specifically among adolescents, it is difficult to determine the optimal clinical value of REACH. Another study weakness is the low enrollment values as compared to the expected positive screens. However, this could be secondary to an overestimated value of at-risk adolescents circulating within the clinics, as the actual number of at-risk adolescents may vary considerably from clinic to clinic and between the Chicago and Boston areas. Also, the narrow range of the depressive symptom instrument of the CES-D, although increasing the specificity for enrollment, leaves the possibility of a significant number of false negatives being excluded. Finally, we are unable to quantify external barriers such as time lost due to terrorism, economic downturn, or regulations imposed by the government. Although we recognize they are responsible for time lost in the study, there are many factors that influence the participation of a clinic, and these factors may be outside the control of study staff.
Conclusion
Our findings have implications for policy and practice. Our results may challenge our understanding of the impact of healthcare reform and corporatization of medicine. Well-intentioned policies and integration strategies may ironically increase barriers to innovation both by adding new steps and process barriers and by simply fatiguing staff in clinical practice. Similarly, in the modern regulatory state, complex overlapping policies and regulations may actually impede the ability of policy makers to implement new and innovative strategies. It is now ironic, and perhaps fitting, that in trying to develop and implement mass prevention models for prevention of mental disorders such as depression, the very trends (e.g., social isolation, anonymity) that may contribute to the elevated risk of depression in our society may in fact impede preventing it. The answer may be a refocus on the relational work that may at least humanize work environments and ease the burden of the increasing regulatory and corporate structural burdens. Successful implementation needs to address the competing demands of health policy that focuses on population health improvements and the emphasis by providers on personalized medical care that focuses on an individual’s needs. For the prevention of mental disorders in children and adolescents in primary care, this can only be done by maintaining and increasing the humanitarian aspects of the practices while availing practices of the all the improved managerial systems of corporate healthcare.
Acknowledgment
Research reported in this article was supported by the National Institute of Mental Health of the National Institutes of Health under award number R01MH090035. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Special thanks to Ruth Ross, PhD, for her contribution to the initial intervention design. Hema Pokharna, PhD, instructed the principal investigator (Van Voorhees) in nonviolent communication methods as a management consultant.
Footnotes
Disclosures: Benjamin W. Van Voorhees has served as a consultant to Prevail Health Solutions, Inc, Mevident Inc, San Francisco and Social Kinetics, Palo Alto, CA, and the Hong Kong University to develop Internet-based interventions.
References
- Angold A, Erkanli A, Farmer EMZ, Fairbank JA, Burns BJ, Keeler G, & Costello EJ (2002). Psychiatric disorder, impairment, and service use in rural African American and white youth. Archives of General Psychiatry, 59(10), 893–901. doi: 10.1001/archpsyc.59.10.893 [DOI] [PubMed] [Google Scholar]
- Arnberg FK, Linton SJ, Hultcrantz M, Heintz E, & Jonsson U (2014). Internet-delivered psychological treatments for mood and anxiety disorders: A systematic review of their efficacy, safety, and cost-effectiveness: E98118. PLoS One, 9(5). doi: 10.1371/journal.pone.0098118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Jaycox LH, & Anderson M (2002). Depression among youth in primary care: Models for delivering mental health services. Child and Adolescent Psychiatric Clinics of North America, 11(3), 477–497. [DOI] [PubMed] [Google Scholar]
- Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, & Robertson N (2010). Tailored interventions to overcome identified barriers to change: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews (Online), 3(3), CD005470. doi: 10.1002/14651858.CD005470.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker MH, & Maiman LA (1980). Strategies for enhancing patient compliance. Journal of Community Health, 6(2), 113–135. doi: 10.1007/BF01318980 [DOI] [PubMed] [Google Scholar]
- Bova C, Drexler D, & Sullivan-Bolyai S (2012). Reframing the influence of the health insurance portability and accountability act on research. Chest, 141(3), 782–786. doi: 10.1378/chest.11-2182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnevale TD (2013). Universal adolescent depression prevention programs: A review. The Journal of School Nursing, 29(3), 181–195. doi: 10.1177/1059840512469231 [DOI] [PubMed] [Google Scholar]
- Charlton CR, Dearing KS, Berry JA, & Johnson MJ (2008). Nurse practitioners’ communication styles and their impact on patient outcomes: An integrated literature review. Journal of the American Academy of Nurse Practitioners, 20(7), 382–388. doi: 10.1111/j.1745-7599.2008.00336.x [DOI] [PubMed] [Google Scholar]
- Chung PJ, Lee TC, Morrison JL, & Schuster MA (2006). Preventive care for children in the United States: Quality and barriers. Annual Review of Public Health, 27(1), 491–515. doi: 10.1146/annurev.publhealth.27.021405.102155 [DOI] [PubMed] [Google Scholar]
- Coryn CLS, Noakes LA, Westine CD, & Schroter DC (2011). A systematic review of theory-driven evaluation practice from 1990 to 2009. American Journal of Evaluation, 32(2):199–226. [Google Scholar]
- DeFrino DT (2009). A theory of the relational work of nurses. Research and Theory for Nursing Practice, 23(4), 294–311. [DOI] [PubMed] [Google Scholar]
- Eisen JC, Marko-Holguin M, Fogel J, Cardenas A, Bahn M, Bradford N, … Van Voorhees BW (2013). Pilot study of implementation of an internet-based depression prevention intervention (CATCH-IT) for adolescents in 12 US primary care practices: Clinical and Management/Organizational behavioral perspectives. The Primary Care Companion for CNS Disorders, 15(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier AL, Colditz GA, Fuchs CS, & Kuntz KM (2000). Cost-effectiveness of screening for colorectal cancer in the general population. Journal of the American Medical Association, 284(15), 1954–1961. doi: 10.1001/jama.284.15.1954 [DOI] [PubMed] [Google Scholar]
- Garrison CZ, Addy CL, Jackson KL, McKeown RE, & Waller JL (1991). The CES-D as a screen for depression and other psychiatric disorders in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 30(4), 636–641. doi: 10.1097/00004583-199107000-00017 [DOI] [PubMed] [Google Scholar]
- Gittell JH, Godfrey M, & Thistlethwaite J (2013). Interprofessional collaborative practice and relational coordination: Improving healthcare through relationships. Journal of Interprofessional Care, 27(3), 210–213. doi: 10.3109/13561820.2012.730564 [DOI] [PubMed] [Google Scholar]
- Gladstone T, Marko-Holguin M, Rothberg P, Nidetz J, Diehl A, DeFrino D, … Van Voorhees, B. (2015). An internet-based adolescent depression preventive intervention: Study protocol for a randomized control trial. Trials, 16(1), 203. doi: 10.1186/s13063-015-0705-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker K, Goldstein J, Link D, Sengupta N, Bowers R, Tendulkar S, & Wissow L (2013). Pediatric provider processes for behavioral health screening, decision making, and referral in sites with colocated mental health services. Journal of Developmental and Behavioral Pediatrics, 34(9), 680–687. doi: 10.1097/01.DBP.0000437831.04723.6f [DOI] [PubMed] [Google Scholar]
- Iloabachie C, Wells C, Goodwin B, Baldwin M, Vanderplough-Booth K, Gladstone T, … Van Voorhees BW (2011). Adolescent and parent experiences with a primary care/Internet-based depression prevention intervention (CATCH-IT). General Hospital Psychiatry, 33(6), 543–555. doi: 10.1016/j.genhosppsych.2011.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssens KAM, Rosmalen JGM, Ormel J, van Oort Floor V. A, & Oldehinkel AJ (2010). Anxiety and depression are risk factors rather than consequences of functional somatic symptoms in a general population of adolescents: The TRAILS study. Journal of Child Psychology and Psychiatry, 51(3), 304–312. doi: 10.1111/j.1469-7610.2009.02174.x [DOI] [PubMed] [Google Scholar]
- Jones RC (2008). The effects of depressed mood on academic outcomes in adolescents and young adults (Doctoral dissertation). University of South Florida, Tampa, FL: Available at http://scholarcommons.usf.edu/cgi/viewcontent.cgi?article=1321&context=etd Accessed October 15, 2016. [Google Scholar]
- Josyula LK, & Lyle RM (2013). Barriers in the implementation of a physical activity intervention in primary care settings: Lessons learned. Health Promotion Practice, 14(1), 81–87. doi: 10.1177/1524839910392991 [DOI] [PubMed] [Google Scholar]
- Kaplan SH, Greenfield S, & Ware JE (1989). Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care, 27(3), S110–S127. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Hammen CL, & Brennan PA (2007). Health outcomes related to early adolescent depression. Journal of Adolescent Health, 41(3), 256–262. doi: 10.1016/j.jadohealth.2007.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalil AH, Rabie MA, Abd-El-Aziz MF, Abdou TA, El-Rasheed AH, & Sabry WM (2010). Clinical characteristics of depression among adolescent females: A cross-sectional study. Child and Adolescent Psychiatry and Mental Health, 4(1), 26. doi: 10.1186/1753-2000-4-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp M, King D, Healey A, & Thomas C (2011). Economic outcomes in adulthood and their associations with antisocial conduct, attention deficit and anxiety problems in childhood. Journal of Mental Health Policy and Economics, 14(3), 137–147. [PubMed] [Google Scholar]
- Kyngäs H, Hentinen M, & Barlow JH (1998). Adolescents’ perceptions of physicians, nurses, parents and friends: Help or hindrance in compliance with diabetes self-care? Journal of Advanced Nursing, 27(4), 760–769. doi: 10.1046/j.1365-2648.1998.00608.x [DOI] [PubMed] [Google Scholar]
- Lokkerbol J, Adema D, Cuijpers P, Reynolds C, Schulz R, Weehuizen R, & Smit F (2014). Improving the cost-effectiveness of a healthcare system for depressive disorders by implementing telemedicine: A health economic modeling study. American Journal of Geriatric Psychiatry, 22(3), 253–262. doi: 10.1016/j.jagp.2013.01.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlearney AS, Walker DM, Livaudais-Toman J, Parides M, & Bickell NA (2016). Challenges of implementation and implementation research: Learning from an intervention study designed to improve tumor registry reporting. SAGE Open Medicine, 4. doi: 10.1177/2050312116666215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meissner HI, Breen N, Klabunde CN, & Vernon SW (2006). Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiology Biomarkers & Prevention, 15(2), 389–394. doi: 10.1158/1055-9965.EPI-05-0678 [DOI] [PubMed] [Google Scholar]
- Meredith LS, Rubenstein LV, Rost K, Ford DE, Gordon N, Nutting P, … Wells KB (1999). Treating Depression in Staff-Model Versus Network-Model Managed Care Organizations. Journal of General Internal Medicine, 14(1), 39–48. 10.1046/j.1525-1497.1999.00279.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mickan SM, & Rodger SA (2005). Effective health care teams: A model of six characteristics developed from shared perceptions. Journal of Interprofessional Care, 19(4), 358–370. doi: 10.1080/13561820500165142 [DOI] [PubMed] [Google Scholar]
- Midkiff KD, Andrews EB, Gilsenan AW, Deapen DM, Harris DH, Schymura MJ, & Hornicek FJ (2016). The experience of accommodating privacy restrictions during implementation of a large-scale surveillance study of an osteoporosis medication: Are privacy restrictions impeding health research? Pharmacoepidemiology and Drug Safety, 25(8), 960–968. doi: 10.1002/pds.4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RG, Ashar BH, Cohen J, Camp M, Coombs C, Johnson E, & Schneyer CR (2005). Disparities in osteoporosis screening between at-risk African-American and White women. Journal of General Internal Medicine, 20(9), 847–851. doi: 10.1111/j.1525-1497.2005.0157.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council and Institute of Medicine. (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, DC: The National Academies Press. doi: 10.17226/12480 [DOI] [PubMed] [Google Scholar]
- Ness RB, for the Joint Policy Committee, Societies of Epidemiology. (2007). Influence of the HIPAA Privacy Rule on Health Research. Journal of the American Medical Association, 298(18), 2164–2170. doi: 10.1001/jama.298.18.2164 [DOI] [PubMed] [Google Scholar]
- Nosek M (2012). Nonviolent communication: A dialogical retrieval of the ethic of authenticity. Nursing Ethics, 19(6), 829–837. doi: 10.1177/0969733012447016 [DOI] [PubMed] [Google Scholar]
- Paskett ED, White E, Carter WB, & Joseph C (1990). Improving follow-up after an abnormal pap smear: A randomized controlled trial. Preventive Medicine, 19(6), 630–641. doi: 10.1016/0091-7435(90)90060-W [DOI] [PubMed] [Google Scholar]
- Pettit JW, Lewinsohn PM, Roberts RE, Seeley JR, & Monteith L (2009). The long-term course of depression: Development of an empirical index and identification of early adult outcomes. Psychological Medicine, 39(3), 403–412. doi: 10.1017/S0033291708003851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson LP, Rockhill C, Russo JE, Grossman DC, Richards J, McCarty C, … Katon W (2010). Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics, 125(5), e1097–e1103. doi: 10.1542/peds.2009-2712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruby A, Marko-Holguin M, Fogel J, & Van Voorhees BW (2013). Economic analysis for an accountable care organization centered primary care Internet-based depression prevention intervention. Journal of Mental Health Policy and Economics, 16(3), 121–130. [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Jagdeo A, Cox BJ, Clara I, Ten Have M, Belik S, … Stein MB (2007). Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Services, 58(3), 357–364. doi: 10.1176/appi.ps.58.3.357 [DOI] [PubMed] [Google Scholar]
- Uema SA, Vega EM, Armando PD, & Fontana D (2008). Barriers to pharmaceutical care in argentina. Pharmacy World & Science, 30(3), 211–215. doi: 10.1007/s11096-007-9167-2 [DOI] [PubMed] [Google Scholar]
- Van Voorhees BW, Fogel J, Reinecke MA, Gladstone T, Stuart S, Gollan J, … Bell C (2009). Randomized clinical trial of an internet-based depression prevention program for adolescents (project CATCH-IT) in primary care: 12-week outcomes. Journal of Developmental and Behavioral Pediatrics, 30(1), 23–37. doi: 10.1097/DBP.0b013e3181966c2a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees BW, Mahoney N, Mazo R, Barrera AZ, Siemer CP, Gladstone TRG, & Muñoz RF (2011). Internet-based depression prevention over the life course: A call for behavioral vaccines. Psychiatric Clinics of North America, 34(1), 167–183. doi: 10.1016/j.psc.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees BW, Melkonian S, Marko M, Humensky J, & Fogel J (2010). Adolescents in primary care with sub-threshold depressed mood screened for participation in a depression prevention study: Co-morbidity and factors associated with depressive symptoms. The Open Psychiatry Journal, 4, 10–18. [PMC free article] [PubMed] [Google Scholar]
- Vijan S, Hwang EW, Hofer TP, & Hayward RA (2001). Which colon cancer screening test? A comparison of costs, effectiveness, and compliance. The American Journal of Medicine, 111(8), 593–601. doi: 10.1016/S0002-9343(01)00977-9 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2014, August). Mental health: A state of well-being. Available at http://www.who.int/features/factfiles/mental_health/mental_health_facts/en/ Accessed September 1, 2016.
- Zhang J, Delzell E, Zhao H, Laster AJ, Saag KG, Kilgore ML, … Curtis JR (2012). Central DXA utilization shifts from office-based to hospital-based settings among Medicare beneficiaries in the wake of reimbursement changes. Journal of Bone and Mineral Research, 27(4), 858–864. doi: 10.1002/jbmr.1534 [DOI] [PubMed] [Google Scholar]