Abstract
Background:
Patients who suffer multiple complications have increased risk of prolonged hospital stay and mortality. However, little is known about what places patients at risk for multiple complications or which complications tend to occur in these patients.
Methods:
Surgical patients were identified from the ACS NSQIP database from 2005–2011. The frequency of post-operative complications was assessed. Patients with <2 complications were compared with patients who had multiple complications using chi square and logistic regression analysis. Relationships among post-operative complications were explored by learning a Bayesian network model.
Results:
The study population consisted of 470,108 general surgery patients. The overall complication rate was 15% with multiple complications in 27,032 (6%) patients. Patients with multiple complications had worse post-operative outcomes (p <0.001). The strongest predictors for developing multiple complications were admission from chronic care facility or nursing home, dependent functional status, and higher ASA classification. In patients with multiple complications, the most common complication was sepsis (42%), followed by failure to wean ventilator (31%), and organ space SSI (27%). We found that severe complications were most strongly associated with development of multiple complications. Using a Bayesian network, we were able to identify how strongly associated specific complications were in patients who developed multiple complications.
Conclusions:
Almost half (40%) of patients with complications suffer multiple complications. Patient factors such as frailty and comorbidity strongly predict the development of multiple complications. The results of our Bayesian analysis identify targets for interventions aimed at disrupting the cascade of multiple complications in high risk patients.
Mini-Abstract
An evaluation of the development of multiple post-operative complications using the ACS NSQIP database found worse outcomes in patients with multiple complications. Markers of patient frailty were found to predict the development of multiple complications. A Bayesian network was also developed to demonstrate co-occurrence of complications in post-operative patients.
Background
Post-operative complications are common, occurring in up to 40% of general surgery patients.1–6 Many studies have evaluated predictors of complication development, which include measures of poor overall health such as older age, dependent functional status, ASA classification, and frailty.6–11 Not surprisingly, complications have been found to be associated with poor post-operative outcomes. The development of complications has been found to be associated with longer hospital length of stay, increased risk of mortality, discharge to higher level of care, and increased risk for readmission.7,12–16 While much is known about predictors of post-operative complications and consequences of individual complications, little is known about the development of multiple complications.
In a study of colorectal surgery patients from the SEER Medicare database, Morris and colleagues13 noted multiple complications requiring operative intervention to be rare (0.4%). While this study did not assess predictors of developing multiple complications, the authors did find an increased risk of prolonged length of hospital stay (RR 2.8, 95% CI 2.3–3.2) and post-operative mortality (RR 7.2, 95% CI 5.1–9.7) in patients who developed 2 or more complications. An evaluation of institutional ACS NSQIP data by Strasberg and Hall3 found an incidence of multiple complications at 5%. The authors did not further evaluate risk factors for the development of 2 or more complications or assess outcomes associated with multiple complications.
Anecdotally, we noted that some patients develop one complication and recover, while other patients develop one complication after another and have poor outcomes. Therefore, we sought to further evaluate multiple complications in general surgery patients. Our specific aims were: 1. Assess the prevalence of multiple complications in general surgery patients, 2. Evaluate post-operative outcomes in patients who develop 2 or more complications, 3. Identify predictors for the development of multiple post-operative complications, and 4. Categorize which complications occur in patients who suffer from 2 or more complications, including identification of co-occurrence relationships between complications.
Methods
General surgery patients were identified from the American College of Surgeons National Quality Improvement Program (ACS NSQIP) database from 2005 to 2011. The ACS NSQIP database prospectively collects in hospital and 30 day outcomes data on surgical patients from over 370 hospitals nationwide. Patients were included in this study if they underwent inpatient general surgery procedures, defined by NSQIP as the surgical specialty of the primary surgeon. Patients who underwent emergent or outpatient procedures were excluded from this study.
Explanatory variables included the following patient characteristics: age, gender, race, level of care prior to hospital admission (home, chronic care, acute care), and body mass index (BMI). The following pre-operative comorbidities, as defined by ACS NSQIP, were examined: weight loss, diabetes, smoking status, alcohol use, dyspnea, functional status, chronic obstructive pulmonary disease (COPD), hypertension, history of stroke, cancer, steroid use, and bleeding disorder. Examined operative factors included operation within previous 30 days, wound classification, ASA classification, intra-operative transfusion, and operative time. Wound class included clean, clean contaminated, contaminated, and dirty.
Patients were divided into those who suffered 2 or more complications and those who had zero or one post-operative complication. Complications included all reported ACS NSQIP complications. Additional outcomes measured were hospital length of stay, 30 day mortality, and work related RVUs as reported by ACS NSQIP.
Descriptive statistics were used to characterize the patients who suffered 2 or more post-operative complications. Chi square analysis was used to compare patients who had ≥ 2 complications with patients who suffered <2 complications in terms of length of stay, mortality, and work related RVUs. Chi square analysis and multivariate logistic regression analysis were used to identify independent predictors of developing ≥ 2 complications. In addition, the frequency of each complication was evaluated in patients with multiple complications. In an effort to identify high risk complications, chi square analysis was used to evaluate the association between each complication and the development of 2 or more complications. All of the above statistics were performed in SPSS version 22. P values <0.05 were considered significant.
We then used machine learning to further investigate which post-operative complications occur together. To investigate interactions among specific postoperative complications, we applied a Bayesian network to patients with multiple complications. A Bayesian network is a graphical representation of a joint probability distribution. The network structure was determined using the Chow-Liu algorithm17 implemented in the R (version 3.1.0) library “bnlearn” (version 3.5). Each post-operative complication for each patient was predicted in association with all other post-operative complications using the Bayesian network.
To determine which relationships between complications were most significant, we performed a second analysis in which the risk level of each patient for each complication was inferred using the likelihood that the patient had other post-operative complications. For example, we would query the model to determine the likelihood that a patient experiences post-operative pneumonia given the knowledge that they experienced both cardiac arrest and deep vein thrombosis, but no other complications.
Results
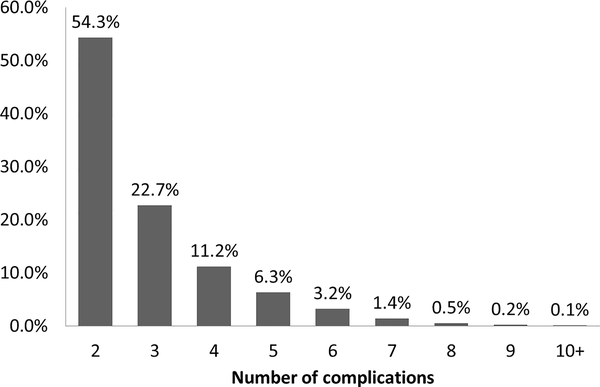
The ACS NSQIP database contained 957, 813 general surgery cases over this 6 year period of time. As demonstrated in Figure 1, the study population consisted of 470,108 patients after exclusion criteria were applied. Approximately 71,000 (15%) patients in the study suffered at least one complication, while 6% of patients suffered multiple complications.
Figure 1:
ACS NSQIP general surgery patient population and breakdown of study population.
Figure 2 demonstrates short term post-operative outcomes in relation to the number of post-operative complications. Patients with multiple complications were found to have a mean length of stay of 21 days as compared with 10 days in patients with one complication and 5 days in patients without complications (p <0.001). A similar trend was noted in 30 day mortality with an increase in mortality rates from 0.4% to 13% in patients with no complications and multiple complications (p <0.001). Patients with multiple complications also required heavier physician workloads, as represented by increased work related RVUs, compared with patients who did not suffer multiple complications (p <0.001).
Figure 2:
The relationship between number of complications and length of stay, mortality, and work related RVUs.
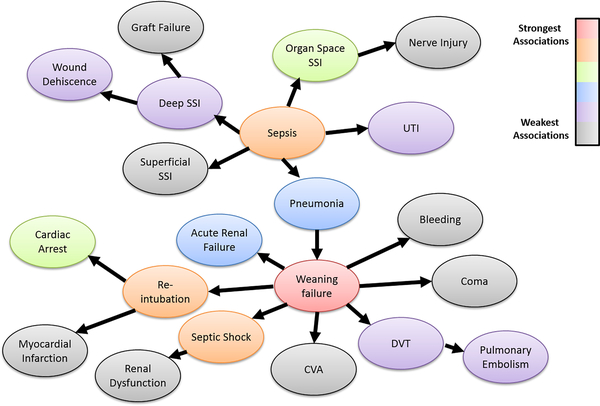
Figure 3 demonstrates the proportion of patients who developed a given number of complications. When evaluating patients with multiple complications, we found that half of these patients developed 2 complications, while over one third had 3–4 complications. Thirty one patients in the study developed 10 or more post-operative complications.
Figure 3:
Frequencies of multiple complications in general surgery patients.
We evaluated patient characteristics, pre-operative comorbidities, and operative variables in association with multiple complications. Results of the univariate analysis are demonstrated in Table 1. All assessed explanatory variables were found to be significantly associated with development of multiple complications. Table 2 lists independent predictors of multiple complications. The patient factors that strongly predicted the development of multiple complications were admission from location other than home, dependent functional status, and higher ASA classification. These results suggest that patients who are more frail pre-operatively are at highest risk for developing multiple complications.
Table 1:
Potential risk factors for development of multiple complications
| 0 – 1 Complication N = 443,076 n (%) | 2+ Complications N = 27,032 n (%) | P value | |
|---|---|---|---|
| Gender | |||
| Female | 278,294 (63) | 13,628 (50) | |
| Male | 163,678 (37) | 13,362 (49) | |
| Unknown | 1,104 (<1) | 42 (<1) | <0.001 |
| Race | |||
| White | 320,732 (72) | 19,830 (73) | |
| Black | 45,978 (10) | 3,359 (12) | |
| Hispanic | 26,119 (6) | 1,187 (4) | |
| American Indian/Alaskan | 3,006 (1) | 181 (1) | |
| Asian/Pacific Islander | 9,816 (2) | 497 (2) | |
| Unknown | 37,425 (8) | 1,978 (7) | <0.001 |
| Previous Level of Care | |||
| Home | 429,902 (97) | 24,202 (90) | |
| Chronic Care/Nursing Home | 4,214 (1) | 980 (4) | |
| Outside ED | 618 (<1) | 96 (<1) | |
| Acute Care | 7,091 (2) | 1,603 (6) | |
| Other | 1,231 (<1) | 151 (<1) | |
| Unknown | 20 (<1) | 0 (0) | <0.001 |
| Age | |||
| 18–64 | 307,681 (69) | 14,602 (54) | |
| 65+ | 135,395 (31) | 12,430 (46) | <0.001 |
| BMI | |||
| <18.5 | 10,519 (2) | 1,186 (4) | |
| 18.5–24.9 | 109,852 (25) | 7,511 (28) | |
| 25–29.9 | 117,777 (27) | 7,333 (27) | |
| ≥ 30 | 197,993 (45) | 10,468 (39) | |
| Unknown | 6,935 (2) | 534 (2) | <0.001 |
| Diabetes | |||
| Absent | 371,269 (84) | 20,887 (77) | |
| Present | 71,807 (16) | 6,145 (23) | <0.001 |
| Smoker | |||
| Absent | 362,467 (82) | 20,872 (77) | |
| Present | 80,609 (18) | 6,160 (23) | <0.001 |
| Alcohol Use | |||
| Absent | 433,405 (98) | 26,013 (96) | |
| Present | 9,671 (2) | 1,019 (4) | <0.001 |
| Dyspnea | |||
| Absent | 389,606 (88) | 21,805 (81) | |
| With Moderate Exertion | 49,344 (11) | 4,093 (15) | |
| At rest | 4,126 (1) | 1,134 (4) | <0.001 |
| Functional Status | |||
| Independent | 422,657 (95) | 21,593 (80) | |
| Partially Dependent | 16,188 (4) | 3,331 (12) | |
| Totally Dependent | 4,202 (1) | 2,100 (8) | |
| Unknown | 29 (<1) | 8 (<1) | <0.001 |
| COPD | |||
| Absent | 425,156 (96) | 24,190 (89) | |
| Present | 17,920 (4) | 2,842 (11) | <0.001 |
| Hypertension | |||
| Absent | 236,283 (53) | 10,968 (41) | |
| Present | 206,793 (47) | 16,064 (59) | <0.001 |
| History of Stroke | |||
| Absent | 428,618 (97) | 25,148 (93) | |
| Present | 14,458 (3) | 1,884 (7) | <0.001 |
| Cancer | |||
| Absent | 428,203 (97) | 24,933 (92) | |
| Present | 14,873 (3) | 2,099 (8) | <0.001 |
| Steroid Use | |||
| Absent | 427,301 (96) | 24,992 (92) | |
| Present | 15,775 (4) | 2,040 (8) | <0.001 |
| Weight Loss | |||
| Absent | 426,920 (96) | 24,403 (90) | |
| Present | 16,156 (4) | 2,626 (10) | <0.001 |
| Bleeding Disorder | |||
| Absent | 424,938 (96) | 24,463 (90) | |
| Present | 18,138 (4) | 2,569 (10) | <0.001 |
| Previous Operation (30d) | |||
| Absent | 434,173 (98) | 25,143 (93) | |
| Present | 8,903 (2) | 1,889 (7) | <0.001 |
| Wound Classification | |||
| Clean | 142,412 (32) | 3,326 (12) | |
| Clean/Contaminated | 237,359 (54) | 16,526 (61) | |
| Contaminated | 39,513 (9) | 3,839 (14) | |
| Dirty | 23,791 (5) | 3,341 (12) | |
| Unknown | 1 (<1) | 0 (0) | <0.001 |
| ASA Classification | |||
| 1 | 21,443 (5) | 257 (1) | |
| 2 | 206,951 (47) | 6,344 (23) | |
| 3 | 196,328 (44) | 15,998 (59) | |
| 4 | 17,743 (4) | 4,288 (16) | |
| 5 | 152 (<1) | 115 (<1) | |
| Unknown | 459 (<1) | 30 (<1) | <0.001 |
| Intraop Transfusion | |||
| Absent | 429,026 (97) | 22,746 (84) | |
| Present | 14,050 (3) | 4,286 (16) | <0.001 |
| Operative Time (Mean, minutes) | 137 | 210 | <0.001 |
Table 2:
Independent predictors of multiple complications
| OR | 95% CI | p value | |
|---|---|---|---|
| Male Gender | 1.211 | 1.179–1.244 | <0.001 |
| Race (White) | |||
| Black | 1.177 | 1.129–1.226 | <0.001 |
| Hispanic | 0.933 | 0.876–0.995 | 0.034 |
| American Indian | 0.962 | 0.819–1.130 | 0.639 |
| Asian/Pacific Islander | 0.891 | 0.809–0.982 | 0.020 |
| Previous Level of Care (Home) | |||
| Chronic Care/Nursing Home | 1.139 | 1.048–1.237 | 0.002 |
| Outside ED | 1.680 | 1.324–2.133 | <0.001 |
| Acute Care | 1.405 | 1.316–1.500 | <0.001 |
| Age ≥ 65 | 1.360 | 1.320–1.402 | <0.001 |
| BMI (18.5–24.9) | |||
| <18.5 | 1.202 | 1.120–1.291 | <0.001 |
| 25–29.9 | 0.918 | 0.918–0.986 | 0.006 |
| ≥ 30 | 0.896 | 0.896–0.961 | <0.001 |
| Weight loss | 1.291 | 1.230–1.356 | <0.001 |
| Diabetes | 0.996 | 0.963–1.030 | 0.803 |
| Smoker | 1.246 | 1.205–1.288 | <0.001 |
| Alcohol use | 1.295 | 1.205–1.392 | <0.001 |
| Dyspnea | |||
| With moderate exertion | 1.156 | 1.113–1.202 | <0.001 |
| At rest | 1.549 | 1.429–1.678 | <0.001 |
| Functional status | |||
| Partially Dependent | 2.040 | 1.946–2.138 | <0.001 |
| Totally Dependent | 3.554 | 3.314–3.810 | <0.001 |
| COPD | 1.365 | 1.300–1.433 | <0.001 |
| Hypertension | 1.158 | 1.124–1.193 | <0.001 |
| History of stroke | 1.132 | 1.071–1.198 | <0.001 |
| Cancer | 1.366 | 1.297–1.440 | <0.001 |
| Steroid use | 1.566 | 1.486–1.650 | <0.001 |
| Bleeding disorder | 1.318 | 1.255–1.384 | <0.001 |
| Prior operation (30 days) | 1.639 | 1.540–1.744 | <0.001 |
| Wound classification (Clean) | |||
| Clean/contaminated | 2.226 | 2.140–2.315 | <0.001 |
| Contaminated | 2.995 | 2.847–3.150 | <0.001 |
| Dirty | 3.434 | 3.250–3.627 | <0.001 |
| ASA Classification (1) | |||
| 2 | 1.813 | 1.597–2.060 | <0.001 |
| 3 | 3.129 | 2.754–3.554 | <0.001 |
| 4 | 5.358 | 4.687–6.125 | <0.001 |
| 5 | 10.505 | 7.748–14.245 | <0.001 |
| Intra-operative transfusion | 1.670 | 1.599–1.743 | <0.001 |
| Operative time (per hour) | 1.319 | 1.311–1.328 | <0.001 |
Baseline comparators are listed in parentheses where appropriate.
Table 3 demonstrates each complication, how frequently each complication occurred in patients with multiple complications, and the risk of developing multiple complications given the complication of interest. Serious complications such as sepsis, failure to wean ventilator, and reintubation occurred commonly among patients with multiple complications and were associated with high rates of multiple complication development. Specifically, Table 3 shows that 42% of patients with multiple complications experienced sepsis while 81% of patients with sepsis experienced multiple complications. Similarly, 31% of patients with multiple complications had “failure to wean ventilator” as a complication, while 88% with failure to wean experienced multiple complications. A less common complication, such as coma, occurred only 1% of time in patients with multiple complications but 94% of the time coma was present with multiple complications. This analysis demonstrates that serious complications are more likely to occur in the setting of multiple complications. Interestingly, the analysis also demonstrates that less severe complications are more likely to occur in isolation. For example, 22% of patients with multiple complications experienced a superficial surgical site infection. However, only 29% of patients with superficial SSI experienced multiple complications, indicating that 71% of patients had a superficial SSI in isolation.
Table 3:
Frequency of each complication in patients with multiple complications and risk for multiple complications given complication of interest
| Complication of Interest | Total Patients w/ Complication | Frequency in Patients w/ Multiple Complications N = 27,032 | Risk for Multiple Complications (by complication) |
|---|---|---|---|
| Sepsis | 14,197 | 42% | 81% |
| Failure to Wean Ventilator | 9,404 | 31% | 88% |
| Organ Space SSI | 10,646 | 27% | 69% |
| Reintubation | 7,762 | 25% | 87% |
| Pneumonia | 9,052 | 24% | 72% |
| Superficial SSI | 20,241 | 22% | 29% |
| Septic Shock | 6,392 | 21% | 91% |
| Urinary Tract Infection | 10,681 | 21% | 52% |
| Bleeding Requiring Transfusion | 7,940 | 13% | 46% |
| Deep SSI | 4,945 | 10% | 53% |
| Dehiscence | 3,808 | 9% | 67% |
| DVT | 4,124 | 9% | 60% |
| Renal Failure | 2,022 | 6% | 83% |
| Cardiac Arrest | 1,826 | 6% | 87% |
| Renal Insufficiency | 2,157 | 6% | 69% |
| Pulmonary Embolism | 2,157 | 5% | 60% |
| Myocardial Infarction | 1,324 | 3% | 62% |
| CVA/Stroke | 856 | 2% | 55% |
| Coma | 318 | 1% | 94% |
| Graft Failure | 531 | 1% | 45% |
| Nerve Injury | 307 | <1% | 30% |
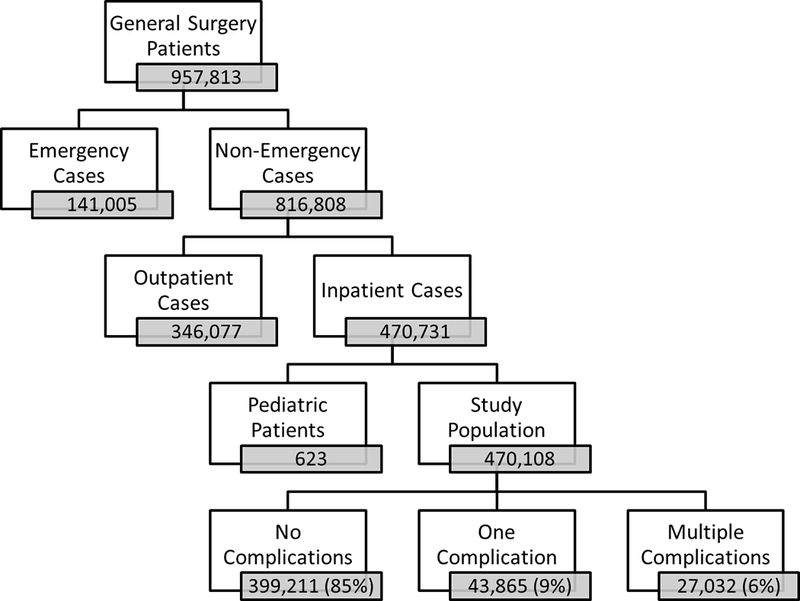
The Bayesian network modeling the relationships among complications in patients who developed multiple complications is demonstrated in Figure 4. Each node in the figure represents a complication and the arrows represent direct relationships among complications. The arrows do not however imply a direction of causality or temporal dependence between complications. Figure 4 also demonstrates how closely related each complication is to the surrounding complications. Complications highlighted in red or orange are more strongly associated with adjacent complications, while complications in purple or black are more weakly associated with surrounding complications. The complication with the strongest associations is weaning failure, followed by sepsis, reintubation, and septic shock. In general more severe complications were more strongly related to other complications.
Figure 4:
Relationships between complications in patients who suffer multiple complications.
Discussion
We sought to characterize multiple complications in general surgery patients, identify risk factors for the development of multiple complications, and assess the effect of ≥ 2 complications on post-operative outcomes. We found multiple complications to occur in 6% of non-emergent general surgery patients. The development of more than 2 post-operative complications was found to be associated with longer length of hospital stay, increased mortality at 30 days, and increased work related RVUs. We also developed a Bayesian network demonstrating the relationships among complications in patients who develop multiple complications.
Previous studies have demonstrated an association between poor overall health, demonstrated by high ASA classification, dependent functional status, or frailty, and risk for post-operative complications.6–11,16 We found similar factors to predict the development of multiple complications, including dependent functional status, ASA classification, and admission from facility other than home. These patient factors are likely markers for patient frailty and it is not surprising that patients who are more frail pre-operatively are more likely to develop a cascade of complications in the post-operative period. While others have described frailty as a predictor of poor surgical outcomes, the relationship between patient comorbidity and the development of multiple complications has not been well described.
Post-operative complications have been shown to correlate with poor outcomes including increased mortality, discharge to higher level of care, and higher risk for readmission.7,12–14 Not surprisingly, we found worse outcomes in patients who developed 2 or more complications compared with patients who developed zero or one complication. Patients with multiple complications had longer length of stay and increased work related RVUs as compared with patients who developed zero or one complication. We identified an over four fold increase in mortality with patients who had multiple complications as compared with 0–1 complications. Further work is needed to evaluate failure to rescue in patients with multiple complications. We theorize there is a snowball effect with post-operative complications and hope to identify ways to intervene to halt the cascade of complications in high risk surgical patients in our future work.
Multiple complications have previously been described to occur in 0.4–5% of general surgery patients.3,13 Morris and colleagues13 assessed colon cancer patients who had surgery and found an overall reoperation rate of 5.8% with 0.4% of patients suffering 2 or more post-operative complications requiring reoperation. This rate is much lower than the rate of multiple complications (6%) we identified in the ACS NSQIP database. While the authors did not evaluate risk factors for developing multiple complications, they did find multiple complications to be associated with increased mortality (RR 7.2, 95% CI 5.1–9.7) and prolonged length of stay (RR 2.8, 95% CI 2.3–3.2).13 Morris et al.13 only included complications that required reoperation, which explains the very low overall complication rate and multiple complication rate described in the study. Other differences between this study and our study include the patient population and data source, Morris et al.13 evaluated colon cancer patients from the SEER Medicare database while we assessed all general surgery patients from the ACS NSQIP database. A study by Strasberg and Hall3 evaluated patients who underwent five common abdominal procedures in the ACS NSQIP database. They found the rate of multiple complications to be 5% in that patient population, which more closely resembles our results. Their study did not assess risk factors for multiple complications or the effect of multiple complications on post-operative outcomes.
We found that 38% of patients who developed complications suffered from 2 or more complications. We also evaluated which complications were most likely to be associated with the development of 2 or more complications and found that more severe complications (coma, septic shock, and failure to wean ventilator) strongly correlated with developing multiple complications. We hypothesize that these severe complications are a common end pathway after the development of multiple less severe complications. The ACS NSQIP puf file contains deidentified data and therefore a more detailed analysis of post-operative complication severity using a classification system such as the Clavien Dindo Classification18 is not feasible. A previous study by Obeid and colleagues19 assessed post-operative complications in colectomy patients in association with frailty. The study translated ACS NSQIP complications into Clavien Dindo class IV (complications with imminent risk for death and need for intensive care) using NSQIP complications with “serious morbidity” and also assigned 30 day mortality data from ACS NSQIP as Clavien Dindo class V (post-operative death) complications. The strength of the Clavien Dindo system lies in the objective classification of complications by required treatment. Therefore grouping of ACS NSQIP complications into Clavien Dindo classes by assuming treatment is likely acceptable for class IV and V complications, but much less reliable for class I, II, and III complications. While we believe that our evaluation of complications by complication type is appropriate and more specific than the Clavien Dindo system in the context of this study, we acknowledge the need for future work that can better assess the severity of complications as complication severity may ultimately be predictive for the development of multiple complications and adverse outcomes in this patient population.
In future studies, we plan to assess multiple complications in surgical subspecialties to identify how multiple complication rates and the relationships between complications differ based on type of operation. We also plan to use machine learning to better understand temporal patterns of complication development. Our ultimate goal is to identify high risk patients and intervene in an effort to avoid the development of multiple complications and subsequent poor outcomes in these patients.
This study has limitations inherent to a retrospective analysis. The complications assessed in this study were those defined by ACS NSQIP. The complication rates in this study are likely an underestimate of actual complication rates as ACS NSQIP does not capture all post-operative complications. Similarly, as patients in the ACS NSQIP national database are not identifiable, we were unable to assess other potential risk factors for developing multiple complications or other post-operative outcomes of interest. The use of the ACS NSQIP database also provides some benefits which strengthen our study. The data is collected in a prospective manner by trained surgical clinical reviewers, complications are strictly defined in the database, and the national database has a large patient population which allows us to assess the <10% of patients who develop multiple complications. Despite the limitations of using ACS NSQIP data, we believe this study outlines the impact of multiple complications on patient outcomes and is an important first step in understanding this high risk group of patients.
In summary, multiple complications are common in general surgery patients occurring in 40% of patients who develop complications. The development of 2 or more complications is associated with worse short term post-operative outcomes. We found markers of patient frailty to be the strongest predictors for developing multiple complications in the post-operative period. We have also demonstrated how complications occur together in patients with multiple complications. The Bayesian model we have developed provides a framework for understanding which complications are likely to occur together post-operatively. Future studies outlining temporal relationships between complication development will provide targets for interventions aimed at preventing the cascade of multiple complications.
Acknowledgements
We would like to acknowledge Glen Leverson PhD, who provided statistical advice on this project. Funding for this study was provided by the NIH training grant T32 CA090217 (S.E.T.), and NIH/NLM training grant T15 LM07359 (A.G.C.). The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427 (M.C.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
The authors have no conflicts of interest to report.
This work was presented at the 2014 American College of Surgeons Clinical Congress.
References
- 1.Longo WE, Virgo KS, Johnson FE, et al. Risk factors for Morbidity and Mortality After Colectomy for Colon Cancer. Diseases of the Colon and Rectum. 2000;43:83–91. [DOI] [PubMed] [Google Scholar]
- 2.Mayo NE, Feldman L, Scott S, et al. Impact of preoperative change in physical function on postoperative recovery: Argument supporting prehabilitation for colorectal surgery. Surgery. 2011;2011:505–514. [DOI] [PubMed] [Google Scholar]
- 3.Strasberg SM, Hall BL. Postoperative morbidity index: a quantitative measure of severity of postoperative complications. J Am Coll Surg. 2011;213:616–626. [DOI] [PubMed] [Google Scholar]
- 4.Cohen ME, Bilimoria KY, Ko CY, Hall BL. Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg. 2009;208:1009–1016. [DOI] [PubMed] [Google Scholar]
- 5.Ghaferi AA, Osborne NH, Birkmeyer JD, Dimick JB. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325–330. [DOI] [PubMed] [Google Scholar]
- 6.Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901–908. [DOI] [PubMed] [Google Scholar]
- 7.Longo WE, Virgo KS, Johnson FE, et al. Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum. 2000;43:83–91. [DOI] [PubMed] [Google Scholar]
- 8.de Silva S, Ma C, Proulx MC, et al. Postoperative complications and mortality following colectomy for ulcerative colitis. Clin Gastroenterol Hepatol. 2011;9:972–980. [DOI] [PubMed] [Google Scholar]
- 9.Saxton A, Velanovich V. Preoperative frailty and quality of life as predictors of postoperative complications. Ann Surg. 2011;253:1223–1229. [DOI] [PubMed] [Google Scholar]
- 10.Karam J, Tsiouris A, Shepard A, Velanovich V, Rubinfeld I. Simplified frailty index to predict adverse outcomes and mortality in vascular surgery patients. Annals of vascular surgery. 2013;27:904–908. [DOI] [PubMed] [Google Scholar]
- 11.Amrock LG, Neuman MD, Lin HM, Deiner S. Can routine preoperative data predict adverse outcomes in the elderly? Development and validation of a simple risk model incorporating a chart-derived frailty score. J Am Coll Surg. 2014;219:684–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris AM, Baldwin LM, Matthews B, et al. Reoperation as a quality indicator in colorectal surgery: a population-based analysis. Ann Surg. 2007;245:73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Legner VJ, Massarweh NN, Symons RG, McCormick WC, Flum DR. The significance of discharge to skilled care after abdominopelvic surgery in older adults. Ann Surg. 2009;249:250–255. [DOI] [PubMed] [Google Scholar]
- 15.Kohlnhofer BM, Tevis SE, Weber SM, Kennedy GD. Multiple complications and short length of stay are associated with postoperative readmissions. Am J Surg. 2014;207:449–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohanty S, Liu Y, Paruch JL, et al. Risk of Discharge to Postacute Care: A Patient-Centered Outcome for the American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator. JAMA Surg. 2015. [DOI] [PubMed] [Google Scholar]
- 17.C C, C L. Approximating discrete probability distributions with dependence trees. IEEE Transactions on Information. 1968;14:462–467. [Google Scholar]
- 18.Clavien P-A, Sanabria JR, Strasberg SM. Proposed classificaiton of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 19.Obeid NM, Azuh O, Reddy S, et al. Predictors of critical care-related complications in colectomy patients using the National Surgical Quality Improvement Program: exploring frailty and aggressive laparoscopic approaches. J Trauma Acute Care Surg. 2012;72:878–883. [DOI] [PubMed] [Google Scholar]