Abstract
Background:
Understanding variation in physical activity (PA) and sleep is necessary to develop novel intervention strategies targeting adolescents’ health behaviors. We examined the extent to which PA and sleep vary by aspects of the physical environment.
Participants:
We performed a cross-sectional analysis of 669 adolescents in the Project Viva cohort.
Methods:
We estimated total PA, sleep duration, sleep efficiency and sleep midpoint timing from wrist accelerometers. We used multivariable linear regression models and generalized estimated equations to assess associations of PA and sleep with season and daily weather conditions obtained from the National Oceanic and Atmospheric Administration archive.
Results:
Mean age was 12.9 (SD 0.6) years; 51% were female and 68% were white. Mean sleep duration was 466 (SD 42) minutes per night and total PA was 1652 (SD 431) counts per minute per day. Sleep midpoint time was 41 (95%CI: 27 to 54) minutes later in summer and 28 (95%CI: −41 to −14) minutes earlier in spring and 29 (95%CI: −43 to −15) minutes earlier in autumn compared to winter. Higher temperature and longer day length both were associated with small reductions of nightly sleep duration. Adolescents were less physically active during winter and on rainy and short sunlight days. There was an inverse U-shaped relationship between PA and mean temperature.
Conclusions:
Season was associated with large changes in sleep timing, and smaller changes in other sleep and PA measurements. Given the importance of sleep and circadian alignment, future health behavioral interventions may benefit by targeting “season-specific” interventions.
Keywords: Adolescents, Physical Activity, Season, Weather
Introduction
Sufficient sleep and adequate physical activity (PA) are critical factors for adolescent health (Chen, Wang, & Jeng, 2006; Hallal, Victora, Azevedo, & Wells, 2006). Adolescence is a time when decline in sleep duration and PA is often reported, supporting the need to better understand these behaviors in this developmental period (Dumith, Gigante, Domingues, & Kohl, 2011; Owens, 2014). Accelerometry yields objective assessments of PA and sleep and has a number of advantages over self- or parent-report. However, use of accelerometry also poses several methodological questions, some of which have been previously summarized (Quante et al., 2015). A recent systematic review suggests that adolescents with higher PA levels are more likely to experience good sleep, assessed both subjectively and objectively (Lang et al., 2016). However, other individual, social and environmental factors may influence both PA and sleep (Moore et al., 2011; Stanley, Ridley, & Dollman, 2012). Recently, associations of PA with season have been explored in children, showing declining PA in winter compared to other seasons (Gracia-Marco et al., 2013; Rich, Griffiths, & Dezateux, 2012; Shen, Alexander, Milberger, & Jen, 2013). A few studies have addressed the associations of meteorological variables with PA in children and found higher PA during warmer and rain-free days (Belanger, Gray-Donald, O’Loughlin, Paradis, & Hanley, 2009; Duncan, Hopkins, Schofield, & Duncan, 2008; Edwards et al., 2015; Harrison et al., 2011; Harrison, van Sluijs, Corder, Ekelund, & Jones, 2015; Oliver, Schluter, Schofield, & Paterson, 2011; Yildirim et al., 2014). In contrast, little is known regarding the association between season and sleep patterns in children and findings are inconclusive (Hense et al., 2011; Hjorth et al., 2013). We are not aware of any study which has investigated associations between weather and sleep in adolescents. An improved understanding of the associations of season and of daily weather conditions with both PA and sleep in adolescents may: 1) help inform the design and interpretation of epidemiological research in sleep and PA in adolescents across the year and meteorological conditions; and 2) identify seasonal and meteorological conditions to be considered in the design of interventions for improving sleep and PA in adolescents. Thus, the primary aim of this study was to examine the extent to which objectively measured PA and sleep vary by aspects of the physical environment, specifically by season, weather and day-length.
Methods
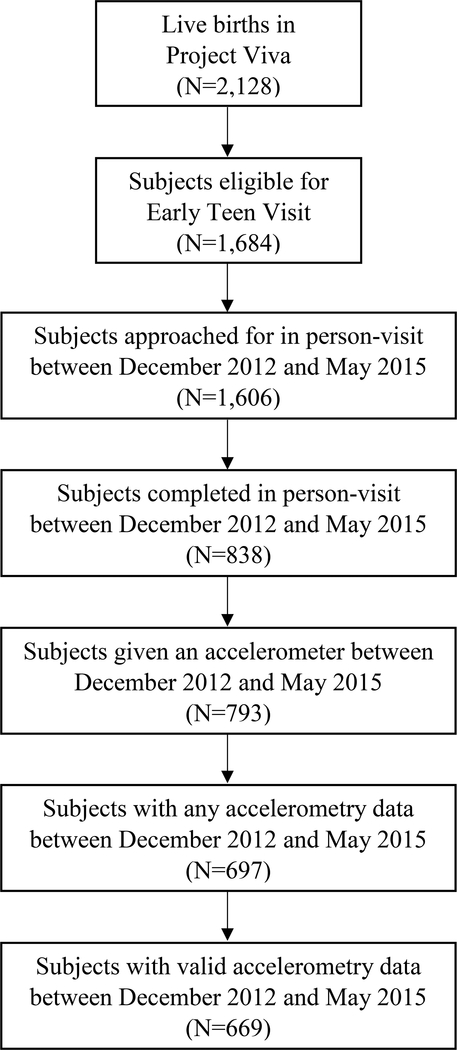
We studied participants in Project Viva, a longitudinal pre-birth cohort study of 2,128 children and their mothers. From 1999–2002, Project Viva recruited pregnant women at in-person visits in the first trimester of pregnancy from eight Atrius Harvard Vanguard Medical Associates practices in eastern Massachusetts. Mother-child in-person visits occurred in infancy, early childhood, and mid-childhood, and additional information was collected from medical records and annual questionnaires. For this analysis, we analyzed a data subset of the ongoing “Early Teen” visit (at ages 12–14 years, mean age 12.9 [SD 0.6] years). We included 669 adolescents who provided valid accelerometry data for at least 3 days and nights from December 2012 through May 2015 (Figure 1). We compared the characteristics between the 669 participants and the remaining 1,459 children who originally enrolled during infancy in the cohort, and found some differences, e.g., the included mothers were more educated (72% versus 61% ≥ college education) and had higher household incomes (67% versus 58% >$70,000 at enrollment), but did not differ on race/ethnicity or child sex. Details of the study protocol and recruitment/retention procedures are available elsewhere (Oken et al., 2015). Institutional review boards of Harvard Pilgrim Health Care, Brigham and Women’s Hospital, and Beth Israel Deaconess Medical Center approved the study protocols and all mothers provided written informed consent.
Figure 1.
Flow of participants.
“Early Teen” visits took place in eastern Massachusetts across all seasons. We defined season of assessment by a four-level categorical variable according to the meteorological definition of seasons determined by range of temperature: Spring: March 1st-May 31th; Summer: June 1st –August 30th, Autumn: September 1st – November 30th, Winter: December 1st – February 28th. From the National Oceanic and Atmospheric Administration archive (Logan International Airport weather station, Boston, MA), we obtained daily data for four weather variables: mean temperature (Fahrenheit), mean wind speed (mph), water equivalent and snow fall (rain and/or amount of water obtained by melting a snow sample [inch]), as well as day-length (time difference between sunrise and sunset [hours]) (“National Oceanic and Atmospheric Administration: Daily Weather Observations at Logan International Airport, Boston, MA,” Accessed from www.ncdc.noaa.gov on 10 November 2015). Each adolescent was studied during one seven day period, with visits scheduled across the year.
We measured sleep and daytime PA using Actigraph™ accelerometers (GT3X+) and ActiLife 6® analysis software (ActiGraph, Inc. Pensacola, Fl.). Accelerometers collected activity data in 60-sec epochs. We asked adolescents to wear the device on their non-dominant wrist for 7 to 10 consecutive days and nights and to complete a daily sleep log. The sleep log was a standardized paper form with predefined questions in which the adolescents recorded bedtimes, accelerometer non-wear times and naps. For each day, we manually identified a main rest interval as the primary sleep period based on self-completed logs and observation of a sharp decrease/increase in activity. We considered the primary sleep period invalid if the device was removed for 1 hour or more within the in-bed interval. Once we defined rest intervals, we applied the Cole-Kripke sleep algorithm to classify each epoch as a sleep or wake period (Kripke et al., 2010; Meltzer, Walsh, Traylor, & Westin, 2012). Sleep variables of interest were based on the overnight sleep periods and included each individual’s average values for nightly sleep duration (minutes), sleep maintenance efficiency (proportion of sleep time during the sleep period, defined as sleep onset to sleep offset, percentage), sleep midpoint time (midpoint between sleep onset and sleep offset, minutes from midnight) and wake after sleep onset (amount of time spent awake after sleep onset, minutes). Before analysis of PA, we excluded sleep periods and non-wear times (Troiano et al., 2008). We considered a day valid if ≥10 hours of activity counts were collected. PA was expressed as total PA (vertical axis counts per min [cpm]), where time was measured as wear-time. We also assessed PA asking mothers the following two questions: “In the past month, how many hours per week does your child spend engaged in light or moderate recreational activities or sports such as biking, skateboarding, dancing, gymnastics, baseball, playing outdoors, or other similar activities? (Do not include walking.)” and “In the past month, on average, how many hours per week does your child spend engaged in vigorous recreational activities or sports such as swimming, running, basketball, soccer, hockey, football, rollerblading, tennis, karate, or other similar activities?”
Child height and weight were directly measured at an in-person visit: (to derive body mass index [BMI] in kg/m2]) (Kuczmarski et al., 2002). Adolescents reported pubertal stage using a self-administered, validated rating scale for pubertal development (Carskadon & Acebo, 1993). Demographic data were obtained using questionnaires or from caregiver interviews. We asked information on school attendance with the sleep logs.
We used Pearson’s correlation analysis to describe the association between accelerometry PA counts and parent-reported PA. Differences in mean (across days in each recording period) measures of PA counts and sleep indices by season were assessed using a multivariable linear regression model adjusting for sex, age, maternal education, household income, race/ethnicity, BMI z-score and pubertal development scale. We conducted analyses of associations between daily weather variables and day length with PA and sleep using the generalized estimating equation (GEE) approach. Since a quadratic relationship between temperature and PA has been described in the literature (Chan & Ryan, 2009), we included a mean-centered quadratic temperature term at 52°F (11.1°C) in the GEE model for PA. Similarly, we identified a non-linear association between sleep midpoint and temperature from visual exploration of the relationships using in spline plots, and therefore also used a quadratic term for temperature in the sleep midpoint model. We adjusted the GEE models for all of the same covariates as in the linear model, plus school attendance. We only adjusted for school attendance in the GEE models since the regression models used summary measures across days in each recording period, which includes both school and non-school days. We also assessed PA as a potential mediator of the observed association of sleep midpoint time with season, using methodology described by Baron and Kenny (R. M. Baron & Kenny, 1986). This approach involves fitting a series of regression models to elucidate the associations among the exposure, the mediator and the outcome and to assess the influence of including mediator in the model on the association between the exposure and the outcome. We performed all analyses using SAS 9.3 (SAS Institute, Inc., Cary, NC).
Results
The sample consisted of equal proportions of girls and boys. Approximately one-third of children were of minority ethnicity/race (Table 1). Adolescents from the analytical sample provided a mean of 7.5 (SD 1.2) nights and 7.2 (SD 1.4) days of valid data. Adolescents slept an average of 466 (SD 42) min/night and accumulated an average of 1652 (SD 431) cpm per day of total PA. 42.5% of the valid days and 44.4% of the valid nights were on days with school attendance. The mean ambient temperatures in Boston ranged from an average high temperature of 75.8°F (24.3°C) in July to an average low temperature of 28.7°F (−1.8°C) in January.
Table 1.
Descriptive characteristics of the study population, total and according to season (N=669).
| Characteristic | Total | Winter | Spring | Summer | Autumn | |
|---|---|---|---|---|---|---|
| n=669 | n=160 | n=181 | n=187 | n=141 | ||
| N values | N (%) | |||||
| Mother | ||||||
| College graduate | 668 | 478 (71.6) | 113 (70.6) | 132 (72.9) | 133 (71.5) | 100 (70.9) |
| Annual household income >$70,000 | 650 | 510 (78.5) | 114 (73.6) | 139 (79.9) | 147 (79.9) | 110 (80.3) |
| Married or cohabitating | 669 | 563 (84.2) | 125 (78.1) | 154 (85.1) | 166 (88.8) | 118 (83.7) |
| Child | ||||||
| Female | 669 | 341 (51.0) | 80 (50.0) | 86 (47.5) | 102 (54.6) | 73 (51.8) |
| Child race/ethnicity | 604 | |||||
| White | 408 (67.6) | 92 (63.0) | 112 (70.4) | 114 (66.7) | 90 (70.3) | |
| Black | 85 (14.1) | 18 (12.3) | 28 (17.6) | 31 (18.1) | 8 (6.3) | |
| Hispanic | 16 (2.7) | 6 (4.1) | 3 (1.9) | 2 (1.2) | 5 (3.9) | |
| Asian | 15 (2.5) | 5 (3.4) | 4 (2.5) | 2 (1.2) | 4 (3.1) | |
| Other | 80 (13.3) | 25 (17.1) | 12 (7.6) | 22 (12.9) | 21 (16.4) | |
| Mean (SD) | ||||||
| Age, years | 669 | 12.9 (0.6) | 13.0 (0.6) | 12.9 (0.6) | 12.8 (0.5) | 13.0 (0.6) |
| Pubertal development scale (units, range 1–4) | 669 | 2.4 (0.8) | 2.5 (0.8) | 2.4 (0.8) | 2.4 (0.8) | 2.4 (0.8) |
| BMI (kg/m2) | 668 | 20.7 (4.5) | 21.2 (4.8) | 20.9 (4.8) | 20.4 (4.2) | 20.0 (4.2) |
| BMI z-score | 668 | 0.4 (1.1) | 0.46 (1.08) | 0.43 (1.09) | 0.34 (1.09) | 0.18 (1.07) |
| Sleep duration (min/night) | 664 | 466.3 (42.4) | 467.4 (42.5) | 464.7 (40.4) | 470.3 (41.5) | 461.9 (45.8) |
| Sleep midpoint time (hours) | 664 | 3:20 (1:05) | 3:27 (1:03) | 2:56 (0:47) | 3:57 (1:15) | 2:53 (0:46) |
| Wake after sleep onset (min) | 664 | 54.2 (21.7) | 54.3 (21.1) | 48.8 (19.1) | 61.0 (23.4) | 52.2 (21.1) |
| Sleep efficiency (%) | 664 | 88.6 (3.8) | 88.5 (4.0) | 89.4 (3.5) | 87.6 (3.8) | 88.8 (3.7) |
| Total physical activity (cpm) | 656 | 1652 (431) | 1523 (363) | 1684 (433) | 1723 (484) | 1663 (397) |
| Light-to-moderate physical activity (hrs/week), parent-report |
658 | 4.5 (4.5) | 3.3 (3.3) | 4.9 (4.6) | 5.6 (5.6) | 3.9 (3.3) |
| Vigorous physical activity (hrs/week), parent-report |
661 | 4.1 (4.0) | 3.6 (3.8) | 4.3 (4.0) | 4.2 (4.4) | 4.4 (3.9) |
Associations of Season with Sleep Patterns and Physical Activity
Table 2 shows the association of season with sleep patterns and PA after multivariate adjustment. Compared to winter, sleep midpoint time was 41 (95% confidence interval [CI]: 27 to 54) minutes later in summer and 28 (95%CI: −41 to −14) minutes earlier in spring and 29 (95%CI: - 43 to −15) minutes earlier in autumn. This relationship did not appear to be explained by varying PA levels across season; after adjusting for total PA in the model, the association between season and sleep midpoint time remained highly significant and the change in magnitude was small (data not shown). Sleep efficiency was slightly higher in spring compared to winter. Similarly, wake after sleep onset was approximately 6 minutes lower in the spring. We observed opposite results in the summer, with slightly lower sleep efficiency and about 6 minutes more wake after sleep onset compared to winter. There was no association of season with average nightly sleep duration.
Table 2.
Associations of physical activity and sleep patterns with season. Data from 669 participants, age 12–14 years, in Project Viva.
| Winter | Spring | Summer | Autumn | Global | |
|---|---|---|---|---|---|
| β (95% CI) | p-value | ||||
| Sleep duration (min/night) | 0.0 (ref) | −2.9 (−12.0, 6.2) | 0.5 (−8.5, 9.4) | −9.4 (−18.8, 0.0) | 0.15 |
| Sleep midpoint time (min) | 0.0 (ref) | −28 (−41, −14) | 41 (27, 54) | −29 (−43, −15) | <.001 |
| Wake after sleep onset (min) | 0.0 (ref) | −5.5 (−10.5, −0.5) | 5.9 (1.0, 10.8) | −2.1 (−7.2, 3.0) | <.001 |
| Sleep efficiency (%) | 0.0 (ref) | 1.0 (0.1, 1.8) | −0.8 (−1.7, 0.0) | 0.3 (−0.6, 1.2) | <.001 |
| Total physical activity (cpm) | 0.0 (ref) | 140 (42, 238) | 181 (84, 277) | 126 (24, 227) | 0.002 |
| Light-to-moderate PA (hrs/week), self-report | 0.0 (ref) | 1.6 (0.6, 2.6) | 2.3 (1.3, 3.3) | 0.5 (−0.5, 1.5) | <.001 |
| Vigorous PA (hrs/week), self-report | 0.0 (ref) | 1.0 (0.0, 1.9) | 0.9 (0.0, 1.8) | 1.0 (0.0, 2.0) | 0.12 |
Linear regression models adjusted for maternal education status, household income, and child race/ethnicity, sex, age, BMI z-score and pubertal development scale. Abbreviations: β=effect estimate; CI=confidence interval.
Compared to winter, PA counts were higher during spring, summer and autumn, respectively.
The correlations between accelerometry counts and parent-reported light-to-moderate and vigorous PA were modest (r = 0.20 and r = 0.21, respectively; p< 0.001), and the variation of PA recorded by accelerometry with season generally paralleled parent-reported PA.
Associations of Weather and Day Length with Sleep Patterns and Physical Activity
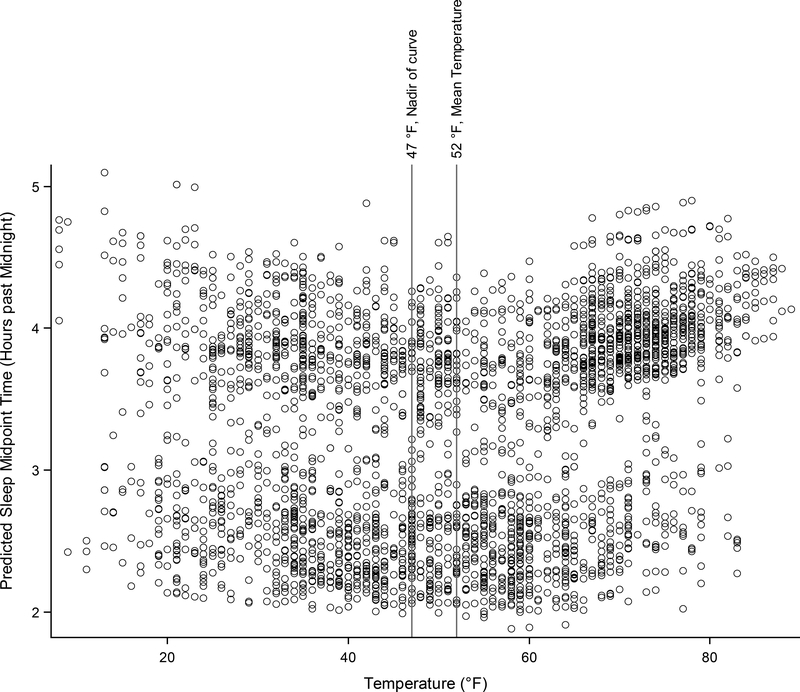
Associations of sleep patterns and PA with local weather conditions and day length are shown in Table 3. After multivariate adjustment, each additional hour of day length was associated with 2.11 minutes (95%CI: −3.68 to −0.54) less average nightly sleep duration. Each additional higher temperature degree was associated with 0.33 minutes (95%CI: −0.50 to −0.17) less average nightly sleep. Sleep midpoint time followed a U-shaped relationship with temperature (Figure 2, and 3). As temperature increased up to 47°F (8.3°C), sleep midpoint time became earlier and then became later with increasing temperature. The rate of change in sleep midpoint was 0.10 min/°F (95%CI: −0.14 to 0.34) at 52°F (11.1°C). Snowfall was positively associated with average sleep duration (ß = 2.00 minutes per inch, 95%CI: 0.63 to 3.37). Each additional degree in temperature was associated with a small (less than 1%) decrease in sleep efficiency and every 10 inches of snowfall were associated with an increased wake after sleep onset by about 7 minutes.
Table 3.
Associations of physical activity and sleep patterns with daily weather conditions. Data from 669 participants, age 12–14 years, in Project Viva.
| Exposure | Parameter | Estimate | 95% CI | P Value | |
|---|---|---|---|---|---|
| Nightly sleep duration (min) | Temperature (°F) | β1 | −0.33 | −0.50,−0.17 | <.001 |
| Wind speed (mph) | β1 | 0.16 | −0.39, 0.72 | 0.57 | |
| Water equivalent (inch) | β1 | 0.89 | −4.92, 6.70 | 0.76 | |
| Day length (hours) | β1 | −2.11 | −3.68,−0.54 | 0.01 | |
| Snow fall (inch) | β1 | 2.00 | 0.63, 3.37 | 0.004 | |
| Sleep midpoint time (min) | Temperature (°F) | β1 | 0.10 | −0.14, 0.34 | 0.41 |
| β2 | 0.01 | 0.00, 0.02 | 0.01 | ||
| Wind speed (mph) | β1 | −0.10 | −0.55, 0.36 | 0.68 | |
| Water equivalent (inch) | β1 | 2.88 | −2.16, 7.92 | 0.26 | |
| Day length (hours) | β1 | 2.18 | −0.27, 4.63 | 0.08 | |
| Snow fall (inch) | β1 | 0.67 | −0.62, 1.95 | 0.31 | |
| Wake after sleep onset (min) | Temperature (°F) | β1 | 0.09 | 0.00, 0.18 | 0.05 |
| Wind speed (mph) | β1 | −0.03 | −0.26, 0.20 | 0.81 | |
| Water equivalent (inch) | β1 | −0.90 | −3.31, 1.51 | 0.46 | |
| Day length (hours) | β1 | 0.47 | −0.52, 1.45 | 0.35 | |
| Snow fall (inch) | β1 | 0.71 | 0.03, 1.40 | 0.04 | |
| Sleep efficiency (%) | Temperature (°F) | β1 | −0.02 | −0.03,−0.01 | 0.01 |
| Wind speed (mph) | β1 | 0.00 | −0.04, 0.04 | 0.98 | |
| Water equivalent (inch) | β1 | 0.21 | −0.20, 0.62 | 0.31 | |
| Day length (hours) | β1 | −0.11 | −0.27, 0.06 | 0.20 | |
| Snow fall (inch) | β1 | −0.07 | −0.17, 0.03 | 0.18 | |
| Total physical activity (cpm) | Temperature (°F) | β1 | 2.63 | 1.13, 4.12 | 0.001 |
| β2 | −0.08 | −0.14,−0.02 | 0.01 | ||
| Wind speed (mph) | β1 | −2.04 | −5.75, 1.66 | 0.28 | |
| Water equivalent (inch) | β1 | −94.90 | −134,−56.2 | <.001 | |
| Day length (hours) | β1 | 40.80 | 24.17,57.42 | <.001 | |
| Snow fall (inch) | β1 | −7.91 | −17.1, 1.29 | 0.09 | |
Generalized estimating equations adjusted for maternal education status, household income, and child race/ethnicity, sex, age, BMI z-score, pubertal development scale and school attendance. β1=linear term; β2=quadratic term.
Figure 2.
Predicted sleep midpoint time versus temperature.
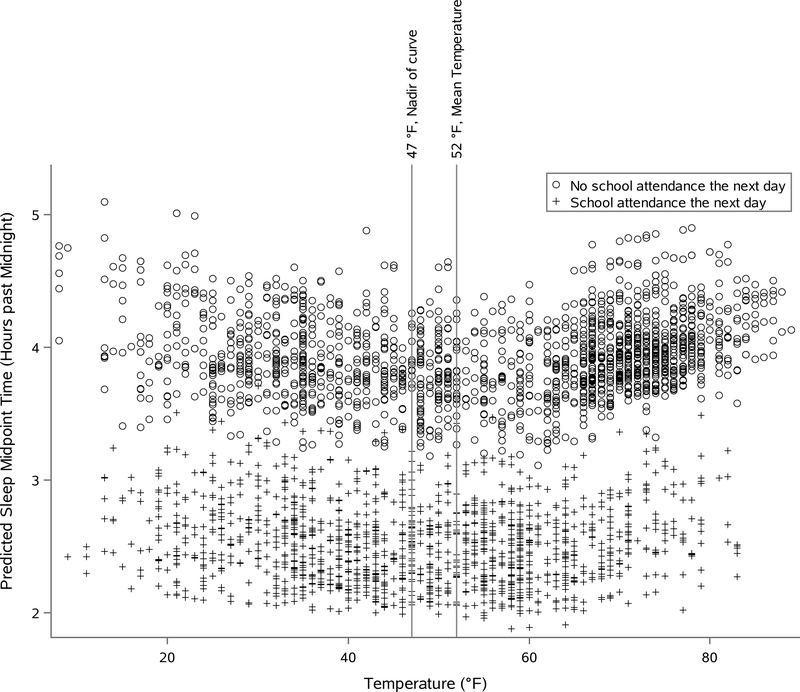
Figure 3.
Predicted sleep midpoint time versus temperature with indication of school attendance the next day. The open dots represent the predicted sleep midpoint time on days with no school attendance the next day, while the crosses indicate the predicted sleep midpoint time on days with school attendance the next day.
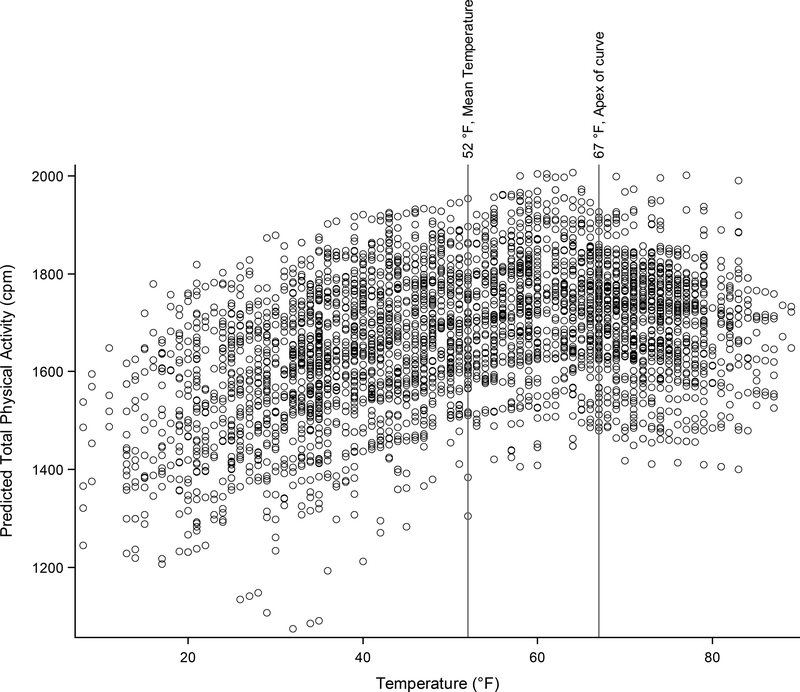
Each inch of daily rain or snowfall was associated with a total average daily decrease in PA of 94.90 cpm (95%CI: −134 to −56.2). We found an inverse U-shaped relationship between PA and temperature (Figure 4). As temperature increased, PA increased up to 68°F (20°C) and then declined. The rate of change in PA was 2.63 cpm/°F (95%CI: 1.13 to 4.12) at 52°F (11.1°C). Each additional hour of day length was associated with 40.80 cpm (95% CI: 24.17 to 57.42) more PA.
Figure 4.
Predicted total physical activity versus temperature.
Discussion
This study provides several novel contributions to the literature regarding the association of season and daily weather conditions with sleep in adolescents. In a U.S. community-based sample of adolescents, we found that sleep midpoint time was significantly later in summer and earlier in spring and autumn compared to winter, indicating seasonal variation in the timing of the sleep period. Sleep midpoint time also varied with temperature, with associations showing a U-shaped distribution across a temperature range of 8°F (−13.3°C) to 89°F (31.7°C). Although sleep duration did not vary by season, daily measurements of temperature and day length showed that higher temperature and longer day length both were associated with small reductions in nightly sleep duration. Consistent with previous reports, we also showed that adolescents were less physically active during winter and on rainy and short sunlight days (Belanger et al., 2009; Carson & Spence, 2010; Goodman, Paskins, & Mackett, 2012; Gracia-Marco et al., 2013; Rich et al., 2012; Yildirim et al., 2014). We observed an inverse U-shaped relationship between PA and temperature: PA first increased then decreased as temperature increased across the range of temperature, similar to the results reported in a sample of adults (Togo, Watanabe, Park, Shephard, & Aoyagi, 2005). Finally, we did not find evidence that variation in PA explained a significant portion of the variability in the association between sleep timing and season.
Compared to winter, sleep midpoint time was 41 minutes later in summer and 28 to 29 minutes earlier in spring and autumn. Sleep midpoint time also varied non-linearly with temperature - shifting to earlier times as temperature increased from 8°F (−13.3°C) to 47°F (8.3°C), and then shifting to later times as temperature increased from 47°F (8.3°C) to 89 °F (31.7°C). The importance of timing of sleep relates to its potential to disrupt circadian rhythms; i.e., sleeping at times misaligned to circadian rhythms can disrupt circadian processes that may adversely affect metabolism and increase risk for weight gain, cancer, and diabetes (Buxton et al., 2012; Leproult, Holmback, & Van Cauter, 2014; Sahar & Sassone-Corsi, 2009). A study of adults has shown that “later” sleepers (sleep midpoint time after 5:30 AM) consumed more calories after 8:00 PM, more fast food and sugar-sweetened beverages, and less fruit and vegetables (K. G. Baron, Reid, Kern, & Zee, 2011). In a study of 2,200 children, aged 9–16 years studied as part of the 2007 Australian National Children’s Nutrition and Physical Activity Survey, Golley et al.(Golley, Maher, Matricciani, & Olds, 2013) reported that a delayed sleep phase (i.e., later bedtimes and late wake up time categories) was associated with poorer diet quality, independent of sleep duration, physical activity and sociodemographic characteristics. Jarrin et al. (Jarrin, McGrath, & Drake, 2013) showed that youth reporting later weekend bedtimes and exhibiting a delayed sleep phase on school days (that is, later sleep and wake times) had larger obesity measures, regardless of sleep duration.
The delayed sleep midpoint time during the summer that we observed in an adolescent population suggests that the summer may be a period when there is a propensity for obesogenic behaviors and adverse metabolism. The extent, to which this association reflects meteorological aspects of the summer season, or differences in social schedules, is difficult to disentangle. Nonetheless, there seems to be a trend in increased weight gain among children during summer versus school year, particularly for high-risk groups (Franckle, Adler, & Davison, 2014). Future research aimed at understanding seasonal variation of eating behaviors as well as metabolism may provide new avenues for promoting health in adolescents.
The timing of sleep onset is governed by both homeostatic drive (or sleep “pressure,” reflecting a buildup of sleep need) and the circadian timing system (Borbely & Achermann, 1999), which is strongly influenced by light (Khalsa, Jewett, Cajochen, & Czeisler, 2003). Morning light exposure facilitates earlier sleep times, while evening light promotes later sleep times. We found that a day length difference of 5 hours between summer and winter was associated with only a marginally significant difference of 11 minutes for sleep duration and a non-significant difference in sleep midpoint of 11 minutes. Small differences in sleep, however, may have clinical relevance. For example, Boergers et al. (Boergers, Gable, & Owens, 2014) found that an average increase of school night sleep duration of 29 minutes resulted in significant reductions of daytime sleepiness, fatigue, and caffeine use in adolescents. An experimental sleep extension of only about 13 minutes in adolescents with chronically insufficient sleep was reported to result in a significant decrease of insomnia and depressive symptoms compared to the control group (Dewald-Kaufmann, Oort, & Meijer, 2014). Data from animal models and human in-laboratory studies suggest an exaggerated phase-delay response to light exposure in the evening in teens compared to adults (Hagenauer & Lee, 2013; Hagenauer, Perryman, Lee, & Carskadon, 2009). In other words, these data suggest that teenagers have an internal clock that interprets environmental time cues differently from adults. Interestingly, Crowley et al. found that pre- to mid-pubertal adolescents have a greater sensitivity to evening light compared to late to post-pubertal adolescents. Of note, the majority of our participants were classified as pre- to mid-pubertal based on the self-rating scale for pubertal development (Crowley, Cain, Burns, Acebo, & Carskadon, 2015).
No significant overall associations were observed between season and sleep duration, and only small differences were observed for sleep efficiency. In contrast, Hjorth et al. (Hjorth et al., 2013) estimated that sleep duration was 2% longer during winter compared to spring in a sample of 730 children from 9 Danish municipal schools, ages 8–11 years. In 519 seven-year-old children of the Auckland Birthweight Collaborative Study, compared to summer, the mean sleep duration was 41 minutes longer in winter, 31 minutes longer in autumn and 15 minutes longer in spring (Nixon et al., 2008). A lack of an association with season in our study may reflect the overlap in weather conditions within seasons in the Northeast US. Our findings are consistent with a large study of 8,542 children, aged 2 to 9 years from eight European countries that showed no effect of season on the nightly sleep duration (Hense et al., 2011).
Increasing outdoor temperature was associated with both lower sleep duration and lower sleep efficiency, although associations were small in magnitude. The effects of changes in temperature on sleep regulation have been described in a review by Van Someren et al. (Van Someren, 2006). The lack of data on indoor temperature limits our ability to fully evaluate the impact of ambient temperature on the natural sleep of adolescents.
Interestingly, we found that snowfall was associated with slightly longer sleep duration. Fresh snow absorbs sound and there is a muted silence that follows a snowfall, potentially promoting sleep. The higher sleep duration with snowfall also may reflect differences in school schedules (e.g., school cancellations) or other influences not recorded.
We also observed variation of PA with both season and meteorological exposures. To understand the practical relevance of this study’s findings, we interpret our estimates relative to the average difference in day length between summer and winter and consider precipitation on an average rainy day. The difference in day length between summer and winter in eastern Massachusetts is about 5 hours, which results in a predicted difference in total daily PA of 204 cpm. The average amount of precipitation on rainy days was 0.24 inches, which would be associated with 23 cpm less PA. Crouter et al. have developed prediction models for estimates of energy expenditure and time spent in different activities using the wrist GT3X+ accelerometer placement in youth (Crouter, Flynn, & Bassett, 2015). Based on their work, we estimate that 105 cpm are approximately equivalent to 2 METs (metabolic equivalent) (Crouter et al., 2015). The rate of energy expenditure while at rest is 1 MET and therefore a 2 MET activity expends 2 times the energy used by the body at rest. Thus, differences in PA level between summer and winter may approximate 4 METs. Studies attempting to estimate “average” PA across the year using data from only a single season may need to statistically adjust for these differences. Our data provide objective evidence that good weather and more daylight are associated with higher PA levels. Similar results have been shown by Goodman et al. who reported in a sample of 325 primary school children in South-East England more PA on long days (Goodman et al., 2012). Days are longer in summer, when children usually spend more time outdoors, suggesting a role for specific strategies for encouraging outdoor activities in winter months (Ajja et al., 2014).
Weather may influence other variables besides PA and sleep. For example, individuals tend to select lower calorie food on hot days (Stroebele & De Castro, 2004) and television viewing also may vary with weather (Eisinga, Franses, & Vergeer, 2011). Thus, some associations of the natural environment on adolescent PA and sleep may be mediated through dietary habits, screen time, school/vacation schedules or other factors. Further understanding those influences in future research may help develop “counter-measures” to optimize PA and/or sleep in the settings of high precipitation, longer day lengths, and extreme temperatures.
Our study has a number of strengths, including its large sample, objective PA and sleep measurements over 24 hours, use of longitudinal data analysis methods to quantify associations between day-to-day variability in weather and sleep/PA, and inclusion of a racially diverse group. This study also had several limitations. Measures of PA were from wrist accelerometry, which limited our analysis of PA to counts per minute of activity. The participating families in this study were ethnically diverse but overall highly educated. Thus, findings may not be generalizable to other populations. Traditionally PA is assessed from hip worn accelerometers and cut-points are used to categorize intensities of PA. However, recent large scale studies such as the National Health and Nutrition Examination Survey, as well as Project Viva, use wrist-based accelerometers due to the higher wear-time compliance rates (Quante et al., 2015). Unfortunately hip and wrist placement provide non-comparable data with wrist placement overestimating PA compared to hip placement (Fairclough et al., 2016). Therefore, we report total PA counts per minute, which incorporates the full continuum of intensities and thus enhances comparisons between studies. We could not determine if activity took place indoors or outdoors and did not have data on the indoor environment. Furthermore, data collection occurred both during school days and vacation and large overlap between season and vacation prevented us from isolating the influence of vacation from season. Finally, we did not have direct measurements of circadian rhythms. Although we interpreted the delayed mid-point in the summer as suggestive of circadian misalignment, it is possible that sleep and circadian rhythms are more aligned during the summer season when sleep/wake patterns are unrestrained by school schedules (Crowley, Acebo, Fallone, & Carskadon, 2006).
In summary, our study quantifies the association between factors in the natural environment and adolescents’ PA and sleep. Except for sleep midpoint time, weather-related factors and season were associated with only small to modest differences in sleep and PA. We suggest that simple adjustments for season may be appropriate when collecting data across the year for most sleep and PA measurements. However, variation in sleep, particularly sleep timing, and the variation of PA with season and meteorological variables suggest opportunities to design season-specific health promotion activities.
Acknowledgments:
This Project Viva study was funded by National Institutes of Health (NIH) grants (U54CA116847) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R37HD034568). This publication was partially supported by a Year 4 Within-Center Developmental Award and a Year 5 Cross-Center Developmental Award from the National Cancer Institute Centers for Transdisciplinary Research on Energetics and Cancer (TREC) (U54CA155626). Dr. Quante was supported by a scholarship from the Max Kade Foundation (NY) and from the Tuebinger Program for the Advancement of Women in Science. Dr. Redline has received grant support from Jazz Pharmaceuticals and Beckman Coulter, Inc. unrelated to the study. The authors have indicated no financial conflicts of interest. We thank the Project Viva participants and staff.
Abbreviations:
- PA
Physical activity
- BMI
Body mass index
- CI
Confidence interval
- CPM
Counts per minute
- GEE
Generalized estimating equation approach
- MET
Metabolic equivalent
Footnotes
The views expressed in this article do not necessarily represent the views of the US Government, the Department of Health and Human Services or the National Institutes of Health.
References
- Ajja R, Clennin MN, Weaver RG, Moore JB, Huberty JL, Ward DS, . . . Beets MW. (2014). Association of environment and policy characteristics on children’s moderate-to-vigorous physical activity and time spent sedentary in afterschool programs. Preventive medicine, 69 Suppl 1, S49–54. doi: 10.1016/j.ypmed.2014.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron KG, Reid KJ, Kern AS, & Zee PC (2011). Role of sleep timing in caloric intake and BMI. Obesity, 19(7), 1374–1381. doi: 10.1038/oby.2011.100 [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Belanger M, Gray-Donald K, O’Loughlin J, Paradis G, & Hanley J (2009). Influence of weather conditions and season on physical activity in adolescents. Annals of epidemiology, 19(3), 180–186. doi: 10.1016/j.annepidem.2008.12.008 [DOI] [PubMed] [Google Scholar]
- Boergers J, Gable CJ, & Owens JA (2014). Later school start time is associated with improved sleep and daytime functioning in adolescents. Journal of developmental and behavioral pediatrics : JDBP, 35(1), 11–17. doi: 10.1097/DBP.0000000000000018 [DOI] [PubMed] [Google Scholar]
- Borbely AA, & Achermann P (1999). Sleep homeostasis and models of sleep regulation. Journal of Biological Rhythms, 14(6), 557–568. [DOI] [PubMed] [Google Scholar]
- Buxton OM, Cain SW, O’Connor SP, Porter JH, Duffy JF, Wang W, . . . Shea SA. (2012). Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Science translational medicine, 4(129), 129–143. doi: 10.1126/scitranslmed.3003200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, & Acebo C (1993). A self-administered rating scale for pubertal development. The Journal of adolescent health : official publication of the Society for Adolescent Medicine, 14(3), 190–195. [DOI] [PubMed] [Google Scholar]
- Carson V, & Spence JC (2010). S easonal variation in physical activity among children and adolescents: a review. Pediatric exercise science, 22(1), 81–92. [DOI] [PubMed] [Google Scholar]
- Chan CB, & Ryan DA (2009). Assessing the effects of weather conditions on physical activity participation using objective measures. International journal of environmental research and public health, 6(10), 2639–2654. doi: 10.3390/ijerph6102639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen MY, Wang EK, & Jeng YJ (2006). Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC public health, 6, 59. doi: 10.1186/1471-2458-6-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouter SE, Flynn JI, & Bassett DR Jr. (2015). Estimating physical activity in youth using a wrist accelerometer. Medicine and science in sports and exercise, 47(5), 944–951. doi: 10.1249/MSS.0000000000000502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley SJ, Acebo C, Fallone G, & Carskadon MA (2006). Estimating dim light melatonin onset (DLMO) phase in adolescents using summer or school-year sleep/wake schedules. Sleep, 29(12), 1632–1641. [DOI] [PubMed] [Google Scholar]
- Crowley SJ, Cain SW, Burns AC, Acebo C, & Carskadon MA (2015). Increased Sensitivity of the Circadian System to Light in Early/Mid-Puberty. The Journal of clinical endocrinology and metabolism, 100(11), 4067–4073. doi: 10.1210/jc.2015-2775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewald-Kaufmann JF, Oort FJ, & Meijer AM (2014). The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. Journal of child psychology and psychiatry, and allied disciplines, 55(3), 273–283. doi: 10.1111/jcpp.12157 [DOI] [PubMed] [Google Scholar]
- Dumith SC, Gigante DP, Domingues MR, & Kohl HW 3rd. (2011). Physical activity change during adolescence: a systematic review and a pooled analysis. International Journal of Epidemiology, 40(3), 685–698. doi: 10.1093/ije/dyq272 [DOI] [PubMed] [Google Scholar]
- Duncan JS, Hopkins WG, Schofield G, & Duncan EK (2008). Effects of weather on pedometer-determined physical activity in children. Medicine and science in sports and exercise, 40(8), 1432–1438. doi: 10.1249/MSS.0b013e31816e2b28 [DOI] [PubMed] [Google Scholar]
- Edwards NM, Myer GD, Kalkwarf HJ, Woo JG, Khoury PR, Hewett TE, & Daniels SR (2015). Outdoor Temperature, Precipitation, and Wind Speed Affect Physical Activity Levels in Children: A Longitudinal Cohort Study. Journal of physical activity & health, 12(8), 1074–1081. doi: 10.1123/jpah.2014-0125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisinga R, Franses PH, & Vergeer M (2011). Weather conditions and daily television use in the Netherlands, 1996–2005. International Journal of Biometeorology, 55(4), 555–564. doi: 10.1007/s00484-010-0366-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairclough SJ, Noonan R, Rowlands AV, Van Hees V, Knowles Z, & Boddy LM (2016). Wear Compliance and Activity in Children Wearing Wrist- and Hip-Mounted Accelerometers. Medicine and science in sports and exercise, 48(2), 245–253. doi: 10.1249/MSS.0000000000000771 [DOI] [PubMed] [Google Scholar]
- Franckle R, Adler R, & Davison K (2014). Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Preventing chronic disease, 11, E101. doi: 10.5888/pcd11.130355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golley RK, Maher CA, Matricciani L, & Olds TS (2013). Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. International Journal of Obesity, 37(4), 546–551. doi: 10.1038/ijo.2012.212 [DOI] [PubMed] [Google Scholar]
- Goodman A, Paskins J, & Mackett R (2012). Day length and weather effects on children’s physical activity and participation in play, sports, and active travel. Journal of physical activity & health, 9(8), 1105–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gracia-Marco L, Ortega FB, Ruiz JR, Williams CA, Hagstromer M, Manios Y, . . . Sjostrom M. (2013). Seasonal variation in physical activity and sedentary time in different European regions. The HELENA study. Journal of Sports Sciences, 31(16), 1831–1840. doi: 10.1080/02640414.2013.803595 [DOI] [PubMed] [Google Scholar]
- Hagenauer MH, & Lee TM (2013). Adolescent sleep patterns in humans and laboratory animals. Hormones and Behavior, 64(2), 270–279. doi: 10.1016/j.yhbeh.2013.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagenauer MH, Perryman JI, Lee TM, & Carskadon MA (2009). Adolescent Changes in the Homeostatic and Circadian Regulation of Sleep. Developmental Neuroscience, 31(4), 276–284. doi: 10.1159/000216538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallal PC, Victora CG, Azevedo MR, & Wells JC (2006). Adolescent physical activity and health: a systematic review. Sports medicine, 36(12), 1019–1030. [DOI] [PubMed] [Google Scholar]
- Harrison F, Jones AP, Bentham G, van Sluijs EM, Cassidy A, & Griffin SJ (2011). The impact of rainfall and school break time policies on physical activity in 9–10 year old British children: a repeated measures study. The international journal of behavioral nutrition and physical activity, 8, 47. doi: 10.1186/1479-5868-8-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison F, van Sluijs EM, Corder K, Ekelund U, & Jones A (2015). The changing relationship between rainfall and children’s physical activity in spring and summer: a longitudinal study. The international journal of behavioral nutrition and physical activity, 12, 41. doi: 10.1186/s12966-015-0202-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hense S, Barba G, Pohlabeln H, De Henauw S, Marild S, Molnar D, . . . Ahrens W. (2011). Factors that influence weekday sleep duration in European children. Sleep, 34(5), 633–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorth MF, Chaput JP, Michaelsen K, Astrup A, Tetens I, & Sjodin A (2013). Seasonal variation in objectively measured physical activity, sedentary time, cardio-respiratory fitness and sleep duration among 8–11 year-old Danish children: a repeated-measures study. BMC public health, 13, 808. doi: 10.1186/1471-2458-13-808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrin DC, McGrath JJ, & Drake CL (2013). Beyond sleep duration: distinct sleep dimensions are associated with obesity in children and adolescents. International Journal of Obesity, 37(4), 552–558. doi: 10.1038/ijo.2013.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SB, Jewett ME, Cajochen C, & Czeisler CA (2003). A phase response curve to single bright light pulses in human subjects. The Journal of physiology, 549(Pt 3), 945–952. doi: 10.1113/jphysiol.2003.040477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Hahn EK, Grizas AP, Wadiak KH, Loving RT, Poceta JS, . . . Kline LE(2010). Wrist actigraphic scoring for sleep laboratory patients: algorithm development. Journal of sleep research, 19(4), 612–619. doi: 10.1111/j.1365-2869.2010.00835.x [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, . . . Johnson CL. (2002). 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics. Series 11, Data from the national health survey(246), 1–190. [PubMed] [Google Scholar]
- Lang C, Kalak N, Brand S, Holsboer-Trachsler E, Puhse U, & Gerber M (2016). The relationship between physical activity and sleep from mid adolescence to early adulthood. A systematic review of methodological approaches and meta-analysis. Sleep medicine reviews, 28, 32–45. doi: 10.1016/j.smrv.2015.07.004 [DOI] [PubMed] [Google Scholar]
- Leproult R, Holmback U, & Van Cauter E (2014). Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes, 63(6), 1860–1869. doi: 10.2337/db13-1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Walsh CM, Traylor J, & Westin AM (2012). Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep, 35(1), 159–166. doi: 10.5665/sleep.1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, & Redline S (2011). Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics. Sleep medicine, 12(3), 239–245. doi: 10.1016/j.sleep.2010.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Oceanic and Atmospheric Administration: Daily Weather Observations at Logan International Airport, Boston, MA: (Accessed from www.ncdc.noaa.gov on 10 November 2015). [Google Scholar]
- Nixon GM, Thompson JM, Han DY, Becroft DM, Clark PM, Robinson E, . . . Mitchell EA. (2008). Short sleep duration in middle childhood: risk factors and consequences. Sleep, 31(1), 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken E, Baccarelli AA, Gold DR, Kleinman KP, Litonjua AA, De Meo D, . . . Gillman MW. (2015). Cohort profile: project viva. International Journal of Epidemiology, 44(1), 37–48. doi: 10.1093/ije/dyu008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver M, Schluter PJ, Schofield GM, & Paterson J (2011). Factors related to accelerometer-derived physical activity in Pacific children aged 6 years. Asia-Pacific journal of public health / Asia-Pacific Academic Consortium for Public Health, 23(1), 44–56. doi: 10.1177/1010539510370992 [DOI] [PubMed] [Google Scholar]
- Owens J (2014). Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics, 134(3), e921–932. doi: 10.1542/peds.2014-1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quante M, Kaplan ER, Rueschman M, Cailler M, Buxton OM, & Redline S (2015). Practical considerations in using accelerometers to assess physical activity, sedentary behavior, and sleep. Sleep Health: Journal of the National Sleep Foundation, 1(4), 275–284. doi: 10.1016/j.sleh.2015.09.002 [DOI] [PubMed] [Google Scholar]
- Rich C, Griffiths LJ, & Dezateux C (2012). Seasonal variation in accelerometer-determined sedentary behaviour and physical activity in children: a review. The international journal of behavioral nutrition and physical activity, 9, 49. doi: 10.1186/1479-5868-9-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahar S, & Sassone-Corsi P (2009). Metabolism and cancer: the circadian clock connection. Nature reviews. Cancer, 9(12), 886–896. doi: 10.1038/nrc2747 [DOI] [PubMed] [Google Scholar]
- Shen B, Alexander G, Milberger S, & Jen KL (2013). An exploratory study of seasonality and preschoolers’ physical activity engagement. Journal of physical activity & health, 10(7), 993–999. [DOI] [PubMed] [Google Scholar]
- Stanley RM, Ridley K, & Dollman J (2012). Correlates of children’s time-specific physical activity: a review of the literature. The international journal of behavioral nutrition and physical activity, 9, 50. doi: 10.1186/1479-5868-9-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebele N, & De Castro JM (2004). Effect of ambience on food intake and food choice. Nutrition, 20(9), 821–838. doi: 10.1016/j.nut.2004.05.012 [DOI] [PubMed] [Google Scholar]
- Togo F, Watanabe E, Park H, Shephard RJ, & Aoyagi Y (2005). Meteorology and the physical activity of the elderly: the Nakanojo Study. International Journal of Biometeorology, 50(2), 83–89. doi: 10.1007/s00484-005-0277-z [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise, 40(1), 181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Van Someren EJ (2006). Mechanisms and functions of coupling between sleep and temperature rhythms. Progress in Brain Research, 153, 309–324. doi: 10.1016/S0079-6123(06)53018-3 [DOI] [PubMed] [Google Scholar]
- Yildirim M, Schoeni A, Singh AS, Altenburg TM, Brug J, De Bourdeaudhuij I, . . . Chinapaw MJ (2014). Daily variations in weather and the relationship with physical activity and sedentary time in European 10- to 12-year-olds: The ENERGY-Project. Journal of physical activity & health, 11(2), 419–425. doi: 10.1123/jpah.2012-0102 [DOI] [PubMed] [Google Scholar]