Abstract
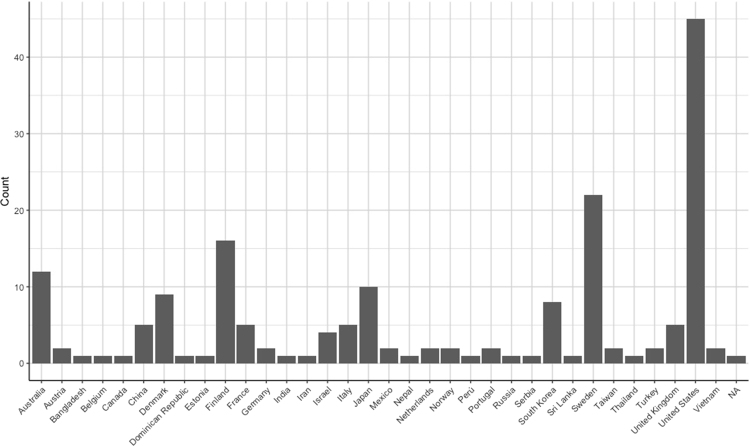
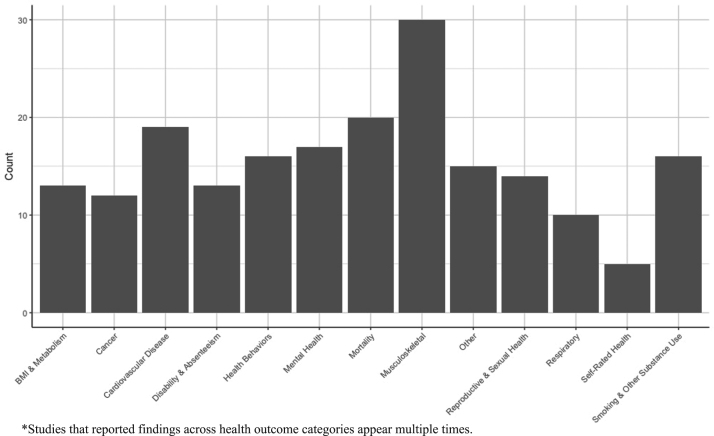
Despite the implications of gender and sex differences for health risks associated with blue-collar work, adverse health outcomes among blue-collar workers has been most frequently studied among men. The present study provides a “state-of-the-field” systematic review of the empiric evidence published on blue-collar women's health. We systematically reviewed literature related to the health of blue-collar women published between January 1, 1990 and December 31, 2015. We limited our review to peer-reviewed studies published in the English language on the health or health behaviors of women who were presently working or had previously worked in a blue-collar job. Studies were eligible for inclusion regardless of the number, age, or geographic region of blue-collar women in the study sample. We retained 177 studies that considered a wide range of health outcomes in study populations from 40 different countries. Overall, these studies suggested inferior health among female blue-collar workers as compared with either blue-collar males or other women. However, we noted several methodological limitations in addition to heterogeneity in study context and design, which inhibited comparison of results across publications. Methodological limitations of the extant literature, alongside the rapidly changing nature of women in the workplace, motivate further study on the health of blue-collar women. Efforts to identify specific mechanisms by which blue-collar work predisposes women to adverse health may be particularly valuable in informing future workplace-based and policy-level interventions.
Keywords: Women's health, Occupational health, Blue-collar, Systematic review
Highlights
-
•
Risks associated with blue-collar jobs are largely studied among men.
-
•
We present a state-of-the-field review of the extant literature on blue-collar women's health
-
•
Our findings span a quarter century, forty countries, and thirteen types of health outcome.
-
•
We find inferior health among blue-collar women, with notable heterogeneity across studies.
1. Introduction
The term “blue-collar work” is frequently used to describe working class jobs that require manual labor. These jobs are often both physically and psychologically demanding, and have been linked with various adverse health outcomes. Evidence suggests, however, that men's and women's exposures and health outcomes in blue-collar jobs may vary considerably. Differences in mortality are consistently noted between men and women in the general population, whereby women outlive men in almost every country in the world and with lower mortality rates observed among women throughout the lifecourse (Åkerstedt et al., 2004, Aittomäki et al., 2003, Ahlgren et al., 2012). Yet women on average exhibit higher rates of morbidity, report inferior self-rated health, and use more health services as compared with men (Case and Paxson, 2005).
Theories explaining the “gender paradox” in morbidity and mortality suggest that biological characteristics and social pressures operating across the lifecourse—both independently and synergistically—contribute to inequalities in men and women's health (Andrés et al., 2010, Ahlgren et al., 2012). Within the context of the relationship between work and health, differences in biological susceptibility to workplace hazards can result from differences in toxicokinetic responses (i.e., absorption, metabolism, and excretion) to occupational chemicals, dust, and other hazardous substances (Arbuckle, 2006). The consequences of nontraditional work hours (e.g., swing shifts, night shifts) can also manifest differently in men and women due to differences in circadian rhythms (Santhi et al., 2016). Lastly, anthropometric differences between men and women can mediate the effects of blue-collar work on health risks: spaces, equipment, and tools that are optimized for the average male worker may be ill-suited for female workers (Arena et al., 1999, Arnold and Bongiovi, 2012, Arbuckle, 2006).
Non-biological differences in susceptibility to health risks include behavioral differences, such as in smoking habits, diet, and use of medications, as well as differences in psychosocial stressors. Women in blue-collar workplaces, for example, are especially vulnerable to experiencing gender discrimination, sexual harassment, social isolation, and work-life conflict (Asztalos et al., 2009, Bakirci et al., 2007, Baigi et al., 2001, Bennett et al., 2007, Berman et al., 1994, Baigi et al., 2002, Bentley et al., 2008).
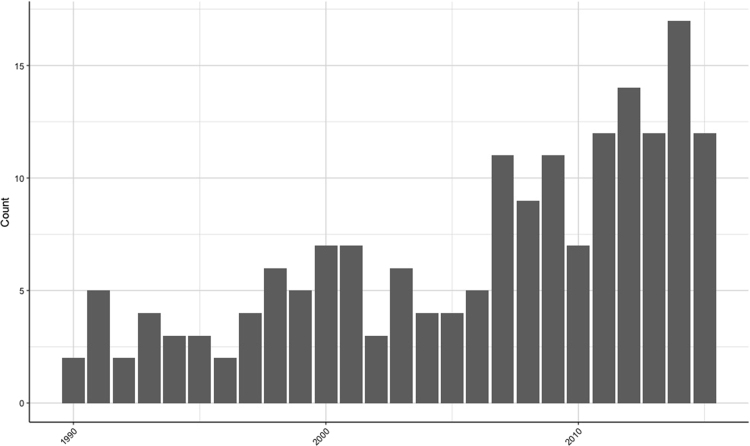
Despite the implications of gender and sex differences for health risks associated with blue-collar work, adverse health outcomes among blue-collar workers has been most frequently studied among men (Asztalos et al., 2009, Biron et al., 2011, Betenia et al., 2012). The present study provides a “state-of-the-field” systematic review of the empiric evidence published on blue-collar women's health from 1990 to 2015. This 25-year period captures major trends in the global economy that may be salient to the health and well-being of contemporary working women, including industry deregulation, computerization and automation of working-class jobs, union decline and weakened institutional protections for workers, and the rise in production in lower income countries (Björkstén et al., 2001, Blue, 1993, von Bonsdorff et al., 2011, von Bonsdorff et al., 2012, Del Bono et al., 2012).
Our specific objectives were to assess: the extent and strength of the existing empiric evidence on the health of blue-collar women; discernable patterns in publication over time, across countries, and among various health outcomes; and the degree to which study findings converge. Our review includes studies that evaluated specific risk factors for morbidity and mortality among blue-collar women, as well as studies that compared the health of blue-collar women with women in other industries or men in blue-collar jobs. Although we provide some analysis of the studies by place, time, and health outcome, differences in study design and specific exposures/outcomes studied inhibited us from offering a quantitative synthesis of the direction and magnitude of associations between work and health. We discuss instead general trends and themes, as well as general methodological limitations of the extant literature. We conclude with future directions for research.
2. Materials and methods
2.1. Identification of papers
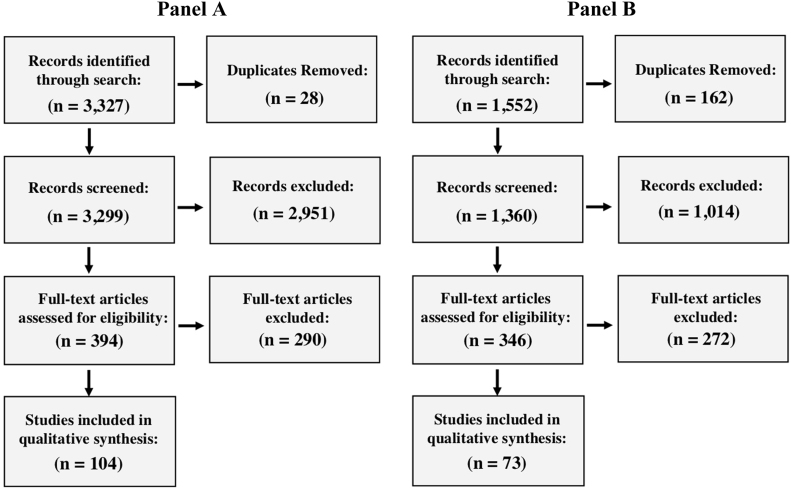
In the present study, we systematically reviewed the peer-reviewed literature related to the health of blue-collar women published between January 1, 1990 and December 31, 2015. We conducted our preliminary search across three major research databases (Google Scholar, Web of Science, and PubMed) for literature relevant to blue-collar women's health, using combinations of the terms “blue-collar,” “health,” and “women” or “female.”
We subsequently employed a second, more flexible, targeted search strategy among these same three databases that integrated synonyms and related terms (e.g. MeSH terms). We additionally expanded our second search to incorporate findings from several smaller research databases from the biomedical, social science, and humanities fields, including: Medline (PubMed), Scopus (Elsevier), Gender Watch (ProQuest), Social Sciences Citation Index (Clarivate), LGBT Life Full Text (EBSCO), CINAHL (EBSCO), Cochrane Library of Systematic Reviews (Cochrane), SafetyLit (SafetyLit Foundation), and Women's Studies Quarterly. Search algorithms were developed specifically for each database by a medical librarian. A complete list of search terms used for identification of papers is provided in Appendix A.
2.2. Selection criteria
We initially identified articles for full-text review based on the contents of the abstract. Studies were deemed eligible for inclusion if they met the following criteria: the study was peer-reviewed and published in the English language; the dependent variable was a health outcome or health behavior (e.g., diet, physical activity, smoking and other substance use); the study population included women who were presently working or had previously worked in a blue-collar job; and the results included a multivariate-adjusted point estimates specific to female blue-collar workers. We defined blue-collar work, consistent with the United States Bureau of Labor Statistics, to include precision production, craft, and repair occupations; machine operators and inspectors; transportation and moving occupations; and handlers, equipment cleaners, helpers, and laborers (U.S. Bureau of Labor Statistics, 2018). Studies were eligible for inclusion regardless of the number, age, or geographic region of blue-collar women in the study sample.
Studies were excluded if there was no empirical quantitative analysis (i.e. qualitative research), if only descriptive and summary statistics were presented (i.e. not multivariate adjusted), if they were not peer reviewed, or if the outcome was deemed unrelated to health. We additionally excluded studies that included blue-collar women in the overall study population but failed to specify results or an exposure unique to blue-collar women. Lastly, we excluded those studies for which we were unable to discern whether blue-collar women were grouped with office and clerical workers in their analyses (Brown et al., 2017, Bromet et al., 1992).
2.3. Data extraction
Two researchers independently assessed and extracted data from the selected articles. The first researcher examined studies published between 1990 and 2002 (A.F.), while the second examined studies published between 2003 and 2015 (H.E.). The researchers cross-checked a random subset of each other's studies in order to ensure that selection criteria were consistently and accurately applied.
We extracted and recorded the following study characteristics from each study: study author(s) and year of publication; title; country of the study subjects; years over which study data were collected; sample size, number of women, and number of blue-collar women; industry subsector; study design (cross-sectional, longitudinal, case-control, or quasi-experimental); independent variable(s); specific health outcome(s); the referent group (i.e., to whom authors compared blue-collar women); a summary of the study's main findings; a brief description of the study population; and country classification.
We classified the country of origin for study subjects as high-, middle- or low-income based on World Bank Country and Lending Groups classification (World Bank, 2018). We classified industry subsector based on the North American Industry Classification System (NAICS). Where insufficient detail was provided to identify industry subsector, we list the industry supersector (e.g., manufacturing). If five or more industry subsectors were represented in the study population or if the study was population-based, we specified “Multiple Industries.” (US Census Bureau, 2017) For a subset of studies that compared the health of male and female blue-collar workers, gender was not considered as a main effect. Similarly, for a subset of studies that compared the health of blue-collar women and women in other industries or job types, occupational class was not considered as a main effect. We use superscripts in the “referent group” column in Table 2 to identify these papers, and we also note which papers were exploratory in nature and considered several independent variables simultaneously.
Table 2.
Empirical studies of blue-collar women's health, organized by health outcome category (n = 177)*.
| Outcome Category | Author (Year) | Title | Country | Years Observed | Sample Size (N) | Women (N) | Blue-Collar Women (N) | Industry Subsector |
|---|---|---|---|---|---|---|---|---|
| BMI & metabolism | Melamed et al. (1995) | Objective and subjective work monotony: effects on job satisfaction, psychological distress, and absenteeism in blue-collar workers | Israel | 1985–1987 | 1278 | 393 | 393 | Manufacturing |
| Nakamura, Nakamura, and Tanaka (2000) | Increased risk of coronary heart disease in Japanese blue-collar workers | Japan | 1993 | 1145 | 492 | 492 | Computer and Electronic Product Manufacturing | |
| Santos and Barros (2003) | Prevalence and determinants of obesity in an urban sample of Portuguese adults | Portugal | NR | 1424 | 868 | 254 | Multiple Industries | |
| Maty et al. (2005) | Education, income, occupation, and the 34-year incidence (1965 -99) of Type 2 diabetes in the Alameda County Study | United States | 1965–1999 | 6147 | 3293 | 417 | Multiple Industries | |
| Bennett, Wolin, and James (2007) | Lifecourse socioeconomic position and weight change among Blacks: the Pitt County Study | United States | 1988–2001 | 1167 | 751 | 573 | Multiple Industries | |
| Forman-Hoffman et al. (2008) | Retirement and weight changes among men and women in the Health and Retirement Study | United States | 1994–2002 | 3725 | 1759 | 994 | Multiple Industries | |
| Yang et al. (2008) | Emergence of socioeconomic inequalities in smoking and overweight and obesity in early adulthood: the National Longitudinal Study of Adolescent Health | United States | 1995–1996, 2001–2002 | 9542 | 4580 | NR | Multiple Industries | |
| Cho and Lee (2012) | The relationship between cardiovascular disease risk factors and gender | South Korea | 2005 | 4556 | 2596 | NR | Multiple Industries | |
| Duffy et al. (2012) | Predictors of Obesity in Michigan Operating Engineers | United States | 2008 | 498 | 37 | 37 | Specialty Trade Contractors | |
| Eshak et al. (2013) | Soft drink, 100% fruit juice, and vegetable juice intakes and risk of diabetes mellitus | Japan | 1990–2000 | 27585 | 15448 | 6565 | Multiple Industries | |
| Miura and Turrell (2014) | Reported consumption of takeaway food and its contribution to socioeconomic inequalities in body mass index | Australia | 2009 | 903 | 480 | 40 | Multiple Industries | |
| Lewin et al. (2014) | Residential neighborhood, geographic work environment, and work economic sector: associations with body fat measured by electrical impedance in the RECORD study | France | 2007–2008 | 4331 | NR | NR | Multiple Industries | |
| Hwang and Lee (2014) | Effect of psychosocial factors on metabolic syndrome in male and female blue-collar workers | South Korea | 2010 | 234 | 80 | 80 | Chemical Manufacturing; Computer and Electronic Product Manufacturing; Fabricated Metal Product Manufacturing; Transportation Equipment Manufacturing; | |
| Cancer | van Loon, Goldbohm, and van den Brandt (1994) | Socioeconomic status and breast cancer incidence: a prospective cohort study | Netherlands | 1986–1989 | 1716 | 1716 | 457 | Multiple Industries |
| van Loon, van den Brandt, and Golbohm (1995) | Socioeconomic status and colon cancer incidence: a prospective cohort study | Netherlands | 1986–1989 | 3658 | 1871 | 494 | Multiple Industries | |
| Cocco, Dosemeci, and Heineman (1998) | Occupational risk factors for cancer of the central nervous system: a case-control study on death certificates from 24 U.S. States | United States | 1984–1992 | 142,080 | 64,900 | NR | Multiple Industries | |
| Pollán & Gustavsson (1999) | High-risk occupations for breast cancer in the Swedish female working population | Sweden | 1971–1989 | 1,101,669 | 1,101,669 | NR | Multiple Industries | |
| Richardi et al. (2004) | Occupational risk factors for lung cancer in men and women: a population-based case-control study in Italy | Italy | 1990–2002 | 2724 | 476 | 476 | Multiple Industries | |
| Thompson et al. (2005) | Occupational exposure to metalworking fluids and risk of breast cancer among female autoworkers | United States | 1941–1994 | 4680 | 4680 | 4680 | Transportation Equipment Manufacturing | |
| Hrubá et al. (2009) | Socioeconomic indicators and risk of lung cancer in Central and Eastern Europe | Czech Republic, Hungary, Poland, Romania, Slovakia, Russia, and the United Kingdom | 1998–2001 | 5979 | 1469 | 617 | Multiple Industries | |
| Colt et al. (2011) | Occupation and bladder cancer in a population-based case-control study in Northern New England | United States | 2001–2004 | 2560 | 634 | 47 | Multiple Industries | |
| Betenia, Costello, and Eisen (2012) | Risk of cervical cancer among female autoworkers exposed to metalworking fluids | United States | 1985–2004 | 4374 | 4374 | 4374 | Transportation Equipment Manufacturing | |
| Oddone et al. (2013) | Female breast cancer in Lombardy, Italy (2002 - 2009): a case-control study on occupational risks | Italy | 2002–2009 | 78349 | 78349 | 36517 | Multiple Industries | |
| Pudrovska et al. (2013) | Higher-status occupations and breast cancer: a life-course stress approach | United States | 1951–2011 | 3682 | 3682 | NR | Multiple Industries | |
| Oddone et al. (2014) | Female breast cancer and electrical manufacturing: results of a nested case-control study | Italy | 2002–2009 | 216 | 216 | 145 | Computer and Electronic Product Manufacturing | |
| Cardiovascular disease | Zhao et al. (1991) | A dose response relation for noise induced hypertension | China | 1985 | 1101 | 1101 | 1101 | Textile Product Mills |
| Hall, Johnson, and Tsou (1993) | Women, occupation, and risk of cardiovascular morbidity and mortality | Sweden | 1977, 1979, 1980, 1981 | 5921 | 5921 | NR | Multiple Industries | |
| Hammar, Alfredsson, and Theorell (1994) | Job characteristics and the incidence of myocardial infarction | Sweden | 1970, 1985, 1976–1981, 1976–1984. | 35396 | 4667 | 2283 | Multiple Industries | |
| Melamed et al. (1995) | Objective and subjective work monotony: effects on job satisfaction, psychological distress, and absenteeism in blue-collar workers | Israel | 1985–1987 | 1278 | 393 | 393 | Manufacturing | |
| Jousilahti et al. (1996) | Symptoms of chronic bronchitis and the risk of coronary disease | Finland | 1972–1985, 1977–1990 | 19444 | 10102 | 766 | Multiple Industries | |
| Melamed et al. (1997) | Industrial noise exposure, noise annoyance e, and serum lipid levels in blue-collar workers--the CORDIS study | Israel | NR | 2079 | 624 | 624 | Manufacturing | |
| Wamala et al. (1997) | Lipid profile and socioeconomic status in health middle aged women in Sweden | Sweden | 1991–1994 | 300 | 300 | 64 | Multiple Industries | |
| Östlin et al. (1998) | Myocardial infarction in male and female dominated occupations | Sweden | 1969–1970, 1970–1990, 1971–1992, 1976–1984 | 140520 | 36708 | NR | Multiple Industries | |
| Baigi, Marklund, and Fridlund (2001) | The association between socio-economic status and chest pain focusing on self-rated health in a primary health care area of Sweden | Sweden | NR | 1145 | 492 | 404 | Multiple Industries | |
| Tsutsumi et al. (2001) | Association between job strain and prevalence of hypertension: a cross sectional analysis in a Japanese working population with a wide range of occupations: the Jichi Medical School cohort study | Japan | 1992–1994 | 6587 | 3400 | 1931 | Multiple Industries | |
| Wamala, Lynch, and Kaplan (2001) | Women's exposure to early and later life socioeconomic disadvantage and coronary heart disease risk: the Stockholm Female Coronary Risk Study | Sweden | 1991–1994 | 585 | 177 | 177 | Multiple Industries | |
| Gallo et al. (2003) | Occupation and subclinical carotid artery disease in women: are clerical workers at greater risk? | United States | 1983–1985 | 362 | 362 | 27 | Multiple Industries | |
| Honjo et al. (2010) | Socioeconomic indicators and cardiovascular disease among Japanese community residents: The Jichi Medical School Cohort Study | Japan | 1992–2005 | 10640 | 6511 | 2084 | Multiple Industries | |
| Clougherty et al. (2011) | Gender and sex differences in job status and hypertension | United States | 1996–2002 | 14618 | 2016 | 793 | Primary Metal Manufacturing; Fabricated Metal Product Manufacturing | |
| Tsutsumi, Kayaba, and Ishikawa (2011) | Impact of occupational stress on stroke across occupational classes and genders | Japan | 1992–2005 | 6553 | 3363 | 1867 | Multiple Industries | |
| Cho and Lee (2012) | The relationship between cardiovascular disease risk factors and gender | South Korea | 2005 | 4556 | 2596 | NR | Multiple Industries | |
| Stokholm et al. (2013) | Occupational noise exposure and the risk of hypertension | Denmark | 2001–2007 | 145190 | 36788 | 15728 | Multiple Industries | |
| Won et al. (2013) | Actual cardiovascular disease risk and related factors: a cross-sectional study of Korean blue-collar workers employed by small businesses | South Korea | 2010 | 238 | 82 | 82 | NR | |
| Fujishiro et al. (2015) | Occupational characteristics and the progression of carotid artery intima-media thickness and plaque over 9 years: the Multi-Ethnic Study of Atherosclerosis (MESA) | United States | 2000–2011 | 3109 | 1610 | 166 | Multiple Industries | |
| Disability & absenteeism | Arber (1991) | Class, paid employment and family roles: making sense of structural disadvantage, gender and health status | United Kingdom | 1985–1986 | 26060 | 13283 | NR | Multiple Industries |
| Guendelman and Silberg (1993) | The health consequences of maquiladora work: women on the US-Mexican border | Mexico | 1990 | 480 | 480 | 241 | Computer and Electronic Products Manufacturing; Apparel Manufacturing; Accommodation and Food Services | |
| Vahtera et al. (1999) | Workplace as an origin of health inequalities | Finland | 1991–1993 | 2793 | 1875 | NR | Multiple Industries | |
| Korda et al. (2002) | The Health of the Australian workforce: 1998-2001 | Australia | 1998–2001 | 9167 | 4107 | 595 | Multiple Industries | |
| Aittomäki, Lahelma, and Roos (2003) | Work conditions and socioeconomic inequalities in work ability | Finland | 2000 | 1827 | 1398 | 161 | Multiple Industries | |
| Väänänen et al. (2004) | Role clarity, fairness, and organizational climate as predictors of sickness absence: a prospective study in the private sector | Finland | 1995–1998 | 3850 | 937 | 385 | Forestry and Logging | |
| Strong & Zimmerman (2005) | Occupational injury and absence from work among African American, Hispanic, and non-Hispanic White workers in the National Longitudinal Survey of Youth | United States | 1988–2000 | 35710 | 16839 | 1890 | Multiple Industries | |
| Christensen et al. (2008) | Explaining the social gradient in long-term sickness absence: a prospective study of Danish employees | Denmark | 2000–2002 | 5221 | 2562 | 671 | Multiple Industries | |
| Niedhammer et al. (2008) | The contribution of occupational factors to social inequalities in health: findings from the national French SUMER survey | France | 2003 | 24468 | 10245 | 1409 | Multiple Industries | |
| Väänänen et al. (2008) | Work-family characteristics as determinants of sickness absence: a large-scale cohort study of three occupational grades | Finland | 2000–2002 | 18366 | 13971 | 1802 | Multiple Industries | |
| von Bonsdorff et al. (2011) | Work ability in midlife as a predictor of mortality and disability in later life: a 28-year prospective follow-up study | Finland | 1981–2009 | 5971 | 3261 | 1692 | Multiple Industries | |
| Gupta et al. (2014) | Face validity of the single work ability item: comparison with objectively measured heart rate reserve over several days | Denmark | NR | 127 | 53 | 53 | Multiple Industries | |
| Heo et al. (2015) | Job stress as a risk factor for absences among manual workers: a 12-month follow-up study | South Korea | 2009–2010 | 2349 | 542 | 542 | Manufacturing | |
| Health behaviors | Burton and Turrell (2000) | Occupation, hours worked, and leisure-time physical activity | Australia | 1995 | 24454 | 11029 | 1972 | Multiple Industries |
| Wu and Porell (2000) | Job characteristics and leisure physical activity | United States | 1992 | 6443 | 2881 | 871 | Multiple Industries | |
| Gang et al. (2002) | Physical activity during leisure and commuting in Tianjin, China | China | 1996 | 3976 | 1974 | 809 | Multiple Industries | |
| Takao et al. (2003) | Occupational class and physical activity among Japanese employees | Japan | 1996–1998 | 20,654 | 3,017 | 1585 | Computer and Electronic Products Manufacturing; Fabricated Metal Product Manufacturing; Primary Metal Manufacturing; Transportation Equipment Manufacturing | |
| McCormack, Giles-Corti, and Milligan (2006) | Demographic and individual correlates of achieving 10,000 steps/day: use of pedometers in a population-based study | Australia | NR | 428 | 223 | 19 | Multiple Industries | |
| Ericson et al. (2007) | Dietary intake of heterocyclic amines in relation to socioeconomic, lifestyle, and other dietary factors: estimates in a Swedish population | Sweden | 1991–1994 | 490 | 490 | 43 | Multiple Industries | |
| Kuiack, Irving, and Faulkner (2007) | Occupation, hours worked, caregiving, and leisure time physical activity | Canada | 2000 | 490 | 490 | 43 | Multiple Industries | |
| Harley et al. (2010) | Multiple health behavior changes in a cancer prevention intervention for construction workers, 2001 - 2003 | United States | 2002–2003 | 582 | 17 | 17 | Construction of Buildings | |
| Mäkinen et al. (2010) | Occupational class differences in leisure-time physical inactivity - contribution of past and current physical workload and other working conditions | Finland | 2000 | 3355 | 1788 | 273 | Multiple Industries | |
| Cleland et al. (2011) | Correlates of pedometer-measured and self-reported physical activity among young Australian adults | Australia | 2004–2006 | 2017 | 923 | NR | Multiple Industries | |
| Cho and Lee (2012) | The relationship between cardiovascular disease risk factors and gender | South Korea | 2005 | 4556 | 2596 | NR | Multiple Industries | |
| Miura and Turrell (2014) | Reported consumption of takeaway food and its contribution to socioeconomic inequalities in body mass index | Australia | 2009 | 903 | 480 | 40 | Multiple Industries | |
| Oliveira, Maia, and Lopes (2014) | Determinants of inadequate fruit and vegetable consumption amongst Portuguese adults | Portugal | 1999–2003 | 2362 | 1455 | NR | Multiple Industries | |
| Uijtdewilligen et al. (2014) | Biological, socio-demographic, work and lifestyle determinants of sitting in young adult women: a prospective cohort study | Australia | 2000, 2003, 2006, 2009 | 11676 | 11676 | NR | Multiple Industries | |
| Hwang et al. (2015) | Predictors of health-promoting behavior associated with cardiovascular diseases among Korean blue-collar workers | South Korea | NR | 234 | 80 | 80 | NR | |
| Uijtdewilligen et al. (2015) | Determinants of physical activity in a cohort of young adult women. Who is at risk of inactive behaviour? | Australia | 2000, 2003, 2006, 2009 | 11695 | 11695 | NR | Multiple Industries | |
| Mental health | Loscocco & Spitze (1990) | Working conditions, social support, and the well-being of female and male factory workers | United States | 1982 | 2222 | 649 | 649 | Multiple Industries |
| Parkinson et al. (1990) | Health effects of long-term solvent exposure among women in blue-collar occupations | United States | NR | 567 | 567 | 567 | Computer and Electronic Product Manufacturing | |
| Bromet et al. (1992) | Effects of occupational stress on the physical and psychological health of women in a microelectronics plant | United States | NR | 552 | 552 | 552 | Computer and Electronic Product Manufacturing | |
| Guendelman and Silberg (1993) | The health consequences of maquiladora work: women on the US-Mexican border | Mexico | 1990 | 480 | 480 | 241 | Computer and Electronic Products Manufacturing; Apparel Manufacturing; Accommodation and Food Services | |
| Melamed et al. (1995) | Objective and subjective work monotony: effects on job satisfaction, psychological distress, and absenteeism in blue-collar workers | Israel | 1985–1987 | 1278 | 393 | 393 | Manufacturing | |
| Kivimäki and Kalimo (1996) | Self-esteem and the occupational stress process: testing two alternative models in a sample of blue-collar workers | Finland | NR | 5450 | 927 | 927 | NR | |
| Goldenhar et al. (1998) | Stressors and adverse outcomes for female construction workers | United States | NR | 211 | 211 | 211 | Construction of Buildings | |
| Rydstedt, Johansson, and Evans (1998) | A longitudinal study of workload, health and well-being among male and female urban drivers | Sweden | 1991–1992 | 56 | 32 | 32 | Transit and Ground Passenger Transportation | |
| Soares, Grossi, and Sundin (2007) | Burnout among women: associations with demographic/socioeconomic, work, life-style and health factors | Sweden | NR | 6000 | 6000 | 745 | Multiple Industries | |
| Andrés, Collings, and Qin (2009) | Sex-specific impact of socio-economic factors on suicide risk: a population-based case-control study in Denmark | Denmark | 1981–1997 | 328608 | 109410 | 19922 | Multiple Industries | |
| Cohidon et al. (2009) | Mental health of workers in Toulouse 2 years after the industrial AZF disaster: first results of a longitudinal follow-up of 3,000 people | France | 2003–2008 | 2847 | 1514 | 53 | Multiple Industries | |
| Asztalos et al. (2009) | Specific associations between types of physical activity and components of mental health | Belgium | 2002–2004 | 1919 | 901 | 140 | Multiple Industries | |
| Brunette, Smith, and Punnett (2011) | Perceptions of working and living conditions among industrial male and female workers in Perú | Perú | 2002 | 1066 | 305 | 305 | Multiple Industries | |
| Moon and Park (2011) | Risk factors for suicidal ideation in Korean middle-aged adults: the role of socio-demographic status | South Korea | 2005 | 7301 | 4087 | 991 | Multiple Industries | |
| Ahlgren, Olsson, and Brulin (2012) | Gender analysis of musculoskeletal disorders and emotional exhaustion: interactive effects from physical and psychosocial work exposures and engagement in domestic work | Sweden | 2008 | 1373 | 515 | 253 | Food Manufacturing; Professional, Scientific and Technical Services | |
| Minh (2014) | Work-related depression and associated factors in a shoe manufacturing factory in Haiphong City, Vietnam | Vietnam | 2012 | 420 | 327 | 227 | Leather and Allied Product Manufacturing | |
| Yoon et al. (2014) | Occupational noise annoyance linked to depressive symptoms and suicidal ideation: a result from nationwide survey of Korea | South Korea | 2007–2009 | 10020 | 4610 | 1934 | Multiple Industries | |
| Mortality | Hall, Johnson, and Tsou (1993) | Women, occupation, and risk of cardiovascular morbidity and mortality | Sweden | 1977, 1979, 1980, 1981 | 5921 | 5921 | NR | Multiple Industries |
| Pekkanen et al. (1995) | Social class, health behaviour, and mortality among men and women in Eastern Finland | Finland | 1970, 1972, 1975, 1977–1987 | 18661 | 9694 | 6376 | Multiple Industries | |
| Chenet et al. (1998) | Deaths from alcohol and violence in Moscow: socio-economic determinants | Russia | 1994–1995 | 86121 | 22619 | NR | Multiple Industries | |
| Arena et al. (1999) | Issues and findings in the evaluation of occupational risk among women high nickel alloys workers | United States | 1948–1988 | 2877 | 2877 | 2877 | Primary Metal Manufacturing | |
| Kareholt (2001) | The relationship between heart problems and mortality in different social classes | Sweden | 1968, 1974, 1981, 1991, 1992, 1968–1996 | 4585 | 2285 | 1170 | Multiple Industries | |
| Baigi et al. (2002) | Cardiovascular mortality focusing on socio-economic influence: the low-risk population f Halland compared to the population of Sweden as a whole | Sweden | 1980–1990 | 3247211 | 1592467 | 1250828 | Multiple Industries | |
| Prescott et al. (2003) | Social position and mortality from respiratory diseases in males and females | Denmark | 1976, 1978, 1981–1983, 1992–1993, 1964–1992 | 29392 | 13992 | NR | Multiple Industries | |
| Akerstedt, Kecklund, and Johansson (2004) | Shift work and mortality | Sweden | 1979–2000 | 22411 | 8401 | 4163 | Multiple Industries | |
| Mamo et al. (2005) | Factors other than risks in the workplace as determinants of socioeconomic differences in health in Italy | Italy | 1981–2001 | 377828 | 136212 | NR | Multiple Industries | |
| Bentley et al. (2007) | Area disadvantage, individual socio-economic position, and premature cancer mortality in Australia 1998 to 2000: a multilevel analysis | Australia | 1998–2000 | 5998961 | 2602424 | 382266 | Cross-Sectional | |
| Hein et al. (2007) | Follow-up study of chrysotile textile workers: cohort mortality and exposure-response | United States | 1916–2001 | 3072 | 1265 | 1256 | Textile Product Mills | |
| Lipton, Cunradi, and Chen (2008) | Smoking and all-cause mortality among a cohort of urban transit operators | United States | 1983–2000 | 1785 | 161 | 161 | Transit and Ground Passenger Transportation | |
| Brockmann, Müller, and Helmert (2009) | Time to retire - time to die? A prospective cohort study of the effects of early retirement on long-term survival | Germany | 1990–2004 | 129675 | 41276 | 26803 | Multiple Industries | |
| von Bonsdorff et al. (2011) | Work ability in midlife as a predictor of mortality and disability in later life: a 28-year prospective follow-up study | Finland | 1981–2009 | 5971 | 3261 | 1692 | Multiple Industries | |
| Dasgupta et al. (2012) | Multilevel determinants of breast cancer survival: association with geographic remoteness and area-level socioeconomic disadvantage | Australia | 1997–2006 | 18568 | 18568 | 715 | Multiple Industries | |
| von Bonsdorff et al. (2012) | Job strain among blue-collar and white-collar employees as a determinant of total mortality: a 28-year population-based follow-up | Finland | 1981–2009 | 5731 | 3261 | 1688 | Multiple Industries | |
| Hirokawa et al. (2013) | Mortality risks in relation to occupational category and position among the Japanese working population: the Jichi Medical School (JMS) cohort study | Japan | 1992–2005 | 6929 | 3596 | 1524 | Multiple Industries | |
| Mattisson, Horstmann, and Bogren (2014) | Relationship of SOC with sociodemographic variables, mental disorders, and mortality | Sweden | 1947, 1957, 1972, 1997–2011 | 1164 | 625 | 325 | Multiple Industries | |
| Costello et al. (2014) | Social disparities in heart disease risk and survivor bias among autoworkers: an examination based on survival models and g-estimation | United States | 1941–1995 | 39412 | 4797 | 4797 | Transportation Equipment Manufacturing | |
| Zhang et al. (2015) | Occupation and risk of sudden death in a United States community: a case-control analysis | United States | 2006–2013 | 1268 | 332 | 62 | Multiple Industries | |
| Musculoskeletal | Vingard et al. (1991) | Occupation and osteoarthrosis of the hip and knee: a register-based cohort study | Sweden | 1960, 1970, 1980, 1981–1983 | 250217 | 42549 | 42549 | Multiple Industries |
| Westgaard and Jansen (1992) | Individual and work related factors associated with symptoms of musculoskeletal complains. II Different risk factors among sewing machine operators | Norway | NR | 245 | 245 | 210 | Textile Product Mills | |
| Iverson and Erwin (1997) | Predicting occupational injury: the role of affectivity | Australia | NR | 362 | 65 | 65 | Manufacturing | |
| Fredriksson et al. (1999) | Risk factors for neck and upper limb disorders: results from 24 years of follow-up | Sweden | 1969–1993 | 484 | 252 | 37 | Multiple Industries | |
| Kaergaard and Andersen (2000) | Musculoskeletal disorders of the neck and shoulders in female sewing machine operators: prevalence, incidence and prognosis | Denmark | 1994–1997 | 243 | 243 | 243 | Textile Product Mills | |
| Murata, Kawakami, and Amari (2000) | Does job stress affect injury due to labor accident in Japanese male and female blue-collar workers? | Japan | 1989–1999 | 168 | 76 | 63 | Chemical Manufacturing | |
| Björkstén et al. (2001) | Reported neck and shoulder problems in female industrial workers: the importance of factors at work and at home | Sweden | NR | 173 | 173 | 173 | Fabricated Metal Product Manufacturing; Food Manufacturing | |
| Khatun, Ahlgren, and Hammarström (2004) | The influence of factors identified in adolescence and early adulthood on social class inequities of musculoskeletal disorders at age 30: a prospective population-based cohort study | Sweden | 1981–1995 | 1044 | 497 | NR | Multiple Industries | |
| Kaila-Kangas et al. (2006) | How consistently distributed are the socioeconomic differences in severe back morbidity by age and gender? A population based study of hospitalisation among Finnish employees | Finland | 1995–1996 | 1517897 | 773936 | 193088 | Multiple Industries | |
| Nakata et al. (2006) | The prevalence and correlates of occupational injuries in small-scale manufacturing enterprises | Japan | 2002 | 1298 | 385 | 138 | Manufacturing | |
| Pollack et al. (2007) | Use of employer administrative databases to identify systematic causes of injury in aluminum manufacturing | United States | 2002–2004 | 9101 | 835 | 835 | Primary Metal Manufacturing | |
| Wang et al. (2007) | Work-organisational and personal factors associated with upper body musculoskeletal disorders among sewing machine operators | United States | 2003–2005 | 520 | 335 | 335 | Textile Product Mills | |
| Niedhammer et al. (2008) | The contribution of occupational factors to social inequalities in health: findings from the national French SUMER survey | France | 2003 | 24468 | 10245 | 1409 | Multiple Industries | |
| Taiwo et al. (2008) | Sex differences in injury patterns among workers in heavy manufacturing | United States | 1996–2005 | 9527 | 692 | 692 | Primary Metal Manufacturing | |
| Roquelaure et al. (2008) | Work increases the incidence of carpal tunnel syndrome in the general population | France | 2002–2004 | 1168 | 819 | 194 | Multiple Industries | |
| Kim et al. (2009) | Depressive symptoms and self-reported occupational injury in small and medium-sized companies | South Korea | 2006–2007 | 1350 | 501 | 404 | Manufacturing | |
| Mattioli et al. (2009) | Risk factors for operated carpal tunnel syndrome: a multicenter population-based case-control study | Italy | 1997–1998, 2001 | 477 | 401 | 172 | Multiple Industries | |
| Roquelaure et al. (2009) | Attributable risk of carpal tunnel syndrome in the general population: implications for intervention programs in the workplace | France | 2002–2004 | 388078 | 194276 | 24090 | Multiple Industries | |
| Nag, Vyas, and Nag (2010) | Gender differences, work stressors, and musculoskeletal disorders in weaving industries | India | 2007 | 516 | 263 | 263 | Textile Product Mills | |
| Brunette, Smith, and Punnett (2011) | Perceptions of working and living conditions among industrial male and female workers in Perú | Perú | 2002 | 1066 | 305 | 305 | Multiple Industries | |
| Motamedzade and Moghimbeigi (2011) | Musculoskeletal disorders among female carpet weavers in Iran | Iran | NR | 626 | 626 | 626 | Textile Product Mills | |
| Ahlgren, Olsson, and Brulin (2012) | Gender analysis of musculoskeletal disorders and emotional exhaustion: interactive effects from physical and psychosocial work exposures and engagement in domestic work | Sweden | 2008 | 1373 | 515 | 253 | Food Manufacturing; Professional, Scientific and Technical Services | |
| Andersen et al. (2012) | Cumulative years in occupation and the risk of knee osteoarthritis in men and women: a register-based follow-up study | Denmark | 1981–2006 | 2117298 | 1100979 | 38485 | Construction of Buildings | |
| Lombardo et al. (2012) | Musculoskeletal symptoms among female garment factory workers in Sri Lanka | Sri Lanka | NR | 1058 | 1058 | 1000 | Apparel Manufacturing | |
| Kubo et al. (2013) | Associations between employee and manager gender: impacts on gender-specific risk of acute occupational injury in metal manufacturing | United States | 2002–2007 | 2645 | 2322 | 2322 | Primary Metal Manufacturing; Fabricated Metal Product Manufacturing | |
| Lipscomb, Schoenfisch, and Cameron (2013) | Work-related injuries involving a hand or fingers among union carpenters in Washington state, 1989 - 2008 | United States | 1989–2008 | 24,830 | 646 | 646 | Specialty Trade Contractors | |
| Hanklang et al. (2014) | Musculoskeletal disorders among Thai women in construction-related work | Thailand | 2011 | 272 | 272 | 272 | Specialty Trade Contractors | |
| Tessier-Sherman (2014) | Occupational injury risk by sex in a manufacturing cohort | United States | 2001–2010 | 23956 | 5063 | 5063 | Primary Metal Manufacturing; Fabricated Metal Product Manufacturing | |
| Cantley et al. (2015) | Expert ratings of job demand and job control as predictors of injury and musculoskeletal disorder risk in a manufacturing cohort | United States | 2004–2005 | 9260 | 946 | 946 | Primary Metal Manufacturing; Fabricated Metal Product Manufacturing | |
| Hallman et al. (2015) | Association between objectively measured sitting time and neck-shoulder pain among blue-collar workers | Denmark | 2011–2012 | 202 | 84 | 84 | Multiple Industries | |
| Other | Parkinson et al. (1990) | Health effects of long-term solvent exposure among women in blue-collar occupations | United States | NR | 567 | 567 | 567 | Computer and Electronic Product Manufacturing |
| Bromet et al. (1992) | Effects of occupational stress on the physical and psychological health of women in a microelectronics plant | United States | NR | 552 | 552 | 552 | Computer and Electronic Product Manufacturing | |
| Grimmer (1993) | Relationship between occupation and episodes of headache that match cervical origin pain patterns | Australia | NR | 417 | 202 | 42 | Multiple Industries | |
| Tsai et al. (1997) | Neurobehavioral effects of occupational exposure to low-level organic solvents among Taiwanese workers in paint factories | Taiwan | 1992–1993 | 298 | 85 | 32 | Chemical Manufacturing | |
| Goldenhar, Swanson, & Hurrell (1998) | Stressors and adverse outcomes for female construction workers | United States | NR | 211 | 211 | 211 | Construction of Buildings | |
| Nguyen et al. (1998) | Noise levels and hearing ability of female workers in a textile factory in Vietnam | Vietnam | NR | 69 | 69 | 69 | Textile Mills | |
| Rydstedt, Johansson, and Evans (1998) | A longitudinal study of workload, health and well-being among male and female urban drivers | Sweden | 1991–1992 | 56 | 32 | 32 | Transit and Ground Passenger Transportation | |
| Juutilainen et al. (2000) | Nocturnal 6-hydroxymelatonin sulfate excretion in female workers exposed to magnetic fields | Finland | NR | 60 | 60 | 39 | Apparel Manufacturing | |
| Shirom, Melamed, and Nir-Dotan (2000) | The relationships among objective and subjective environmental stress levels and serum uric acid: the moderating effect of perceived control | Israel | 1985–1987 | 3680 | 1176 | 1176 | Manufacturing | |
| Korda et al. (2002) | The Health of the Australian workforce: 1998-2001 | Australia | 1998–2001 | 9167 | 4107 | 595 | Multiple Industries | |
| Kovacevic and Belojevic (2006) | Tooth abrasion in workers exposed to noise in the Montenegrin Textile Industry | Serbia | NR | 225 | 225 | 111 | Textile Mills | |
| Potula and Kaye (2006) | The impact of menopause and lifestyle factors on blood and bone lead levels among female former smelter workers: the Bunker Hill Study | United States | 1994, 2000 | 73 | 73 | NR | Primary Metal Manufacturing | |
| Cobankara et al. (2011) | The prevalence of fibromyalgia among textile workers in the city of Denizli in Turkey | Turkey | 2005 | 655 | 523 | 523 | Textile Mills | |
| Choi et al. (2013) | Factors associated with sleep quality among operating engineers | United States | 2008 | 498 | 37 | 37 | Specialty Trade Contractors | |
| Lin et al. (2015) | Risk for work-related fatigue among the employees on semiconductor manufacturing lines | Taiwan | 2007 | 1545 | 428 | 428 | Computer and Electronic Product Manufacturing | |
| Reproductive & sexual health | Eskenazi, Guendelman, and Elkin (1993) | A preliminary study of reproductive outcomes of female maquiladora workers in Tijuana, Mexico | Mexico | 1990 | 360 | 360 | 241 | Computer and Electronic Products Manufacturing; Apparel Manufacturing; Accommodation and Food Services |
| Luoto, Kaprio, and Uutela (1994) | Age at natural menopause and sociodemographic status in Finland | Finland | 1989 | 1505 | 1505 | 511 | Multiple Industries | |
| Evans et al. (2003) | Predictors of seropositivity to herpes simplex virus type 2 in women | United Kingdom | 1992 | 520 | 520 | 88 | Multiple Industries | |
| Gissler et al. (2009) | Trends in socioeconomic differences in Finnish perinatal health 1991 - 2006 | Finland | 1991–2006 | 931285 | 931285 | 154359 | Multiple Industries | |
| Jakobsson and Mikoczy (2009) | Reproductive outcome in a cohort of male and female rubber workers: a registry study | Sweden | 1973–2001 | NR | NR | NR | Plastics and Rubber Products Manufacturing; Food Manufacturing | |
| Lalive & Zweimüller (2009) | How does parental leave affect fertility and return to work? Evidence from two natural experiments | Austria | 1985, 1987, 1990, 1993, 1996 | 6180 | 6180 | NR | Multiple Industries | |
| Sakr et al. (2010) | Reproductive outcomes among male and female workers at an aluminum smelter | United States | 2006 | 419 | 76 | 38 | Primary Metal Manufacturing | |
| Sayem et al. (2010) | An assessment of risk behaviours for HIV/AIDS among young female garment workers in Bangladesh | Bangladesh | 2007 | 300 | 300 | 300 | Apparel Manufacturing | |
| Yingying, Smith, and Suiming (2011) | Changes and correlates in multiple sexual partnerships among Chinese adult women--population based surveys in 2000 and 2006 | China | 2000, 2006 | 4525 | 4525 | 922 | Multiple Industries | |
| del Bono, Weber, and Winter-Ebmer (2012) | Clash of career and family: fertility decisions after job displacement | Austria | 1990–1998 | 227199 | 227199 | NR | Multiple Industries | |
| Pant et al. (2013) | Knowledge of and attitude towards HIV/AIDS and condom use among construction workers in the Kathmandu Valley, Nepal | Nepal | 2013 | 317 | 33 | 33 | Construction of Buildings | |
| Räisänen et al. (2014) | Influence of delivery characteristics and socioeconomic status on giving birth by caesarean section - a cross sectional study during 2000–2010 in Finland | Finland | 2000–2010 | 620463 | 620463 | 90032 | Multiple Industries | |
| von Ehrenstein et al. (2014) | Preterm birth and prenatal maternal occupation: the role of Hispanic ethnicity and nativity in a population-based sample in Los Angeles, California | United States | 2003 | 2543 | 2,543 | 186 | Multiple Industries | |
| Wang et al. (2015) | Sulfur dioxide exposure and other factors affecting age at natural menopause in the Jinchuan cohort | China | 2012 | 3167 | 3167 | 2657 | Primary Metal Manufacturing | |
| Respiratory | Kongerud and Soyseth (1991) | Methacholine responsiveness, respiratory symptoms, and pulmonary function in aluminum potroom workers | Norway | 1988 | 337 | 38 | 38 | Primary Metal Manufacturing |
| Love et al. (1991) | The characteristics of respiratory ill health of wool textile workers | United Kingdom | NR | 620 | 145 | 145 | Textile Mills | |
| Raza et al. (1999) | Ventilatory function and personal breathing zone dust concentrations in Lancashire textile weavers | United Kingdom | NR | 302 | NR | NR | Textile Mills | |
| Seldén et al. (2001) | Exposure to tremolite asbestos and respiratory health in Swedish dolomite workers | Sweden | 1996 | 130 | 16 | 16 | Mining (except oil and gas); Nonmetallic Mineral Product Manufacturing | |
| Takezaki et al. (2001) | Dietary factors and lung cancer risk in Japanese: with special reference to fish consumption and adenocarcinomas | Japan | 1988–1997 | 5198 | 1486 | 178 | Multiple Industries | |
| Bakirci et al. (2007) | Natural history and risk factors of early respiratory responses to exposure to cotton dust in newly exposed workers | Turkey | NR | 157 | 74 | 74 | Textile Mills | |
| Heikkilä et al. (2008) | Asthma incidence in wood-processing industries in Finland in a register based population study | Finland | 1986–1998 | 170963 | 25148 | 16937 | Wood Product Manufacturing; Forestry and Logging | |
| Thilsing et al. (2012) | Chronic rhinosinusitis and occupational risk factors among 20- to 75-year-old Danes--a GA2LEN-based study | Denmark | 2008 | 2531 | 1331 | 550 | Multiple Industries | |
| Storaas et al. (2015) | Incidence of rhinitis and asthma related to welding in Northern Europe | Iceland, Norway, Sweden, Denmark, Estonia | 1990–1994, 1999–2001 | 16191 | 8398 | 219 | Fabricated Metal Product Manufacturing | |
| Wang et al. (2015) | Synergistic impaired effect between smoking and manganese dust exposure on pulmonary ventilation function in Guangxi Manganese-Exposed Workers Healthy Cohort (GXMEWHC) | China | 2011–2012 | 1658 | 620 | 620 | Primary Metal Manufacturing | |
| Self-Rated health | Korda et al. (2002) | The Health of the Australian workforce: 1998-2001 | Australia | 1998–2001 | 9167 | 4107 | 595 | Multiple Industries |
| Niedhammer et al. (2008) | The contribution of occupational factors to social inequalities in health: findings from the national French SUMER survey | France | 2003 | 24468 | 10245 | 1409 | Multiple Industries | |
| Brunette, Smith, and Punnett (2011) | Perceptions of working and living conditions among industrial male and female workers in Perú | Perú | 2002 | 1066 | 305 | 305 | Multiple Industries | |
| Hammarström, Stenlund, and Janlert (2011) | Mechanisms for the social gradient in health: results form a 14-year follow-up of the Northern Swedish Cohort | Sweden | 1981–1995 | 1083 | 495 | NR | Multiple Industries | |
| Landefeld et al. (2014) | The association between a living wage and subjective social status and self-rated health: a quasi-experimental study in the Dominican Republic | Dominican Republic | 2011 | 204 | 134 | 134 | Apparel Manufacturing | |
| Smoking & Other Substance Use | Cunradi, Lipton, and Banerjee (2007) | Occupational correlates of smoking among urban transit operators: a prospective study | United States | 1983–1985; 1993–1995 | 654 | 54 | 54 | Transit and Ground Passenger Transportation |
| Radi, Ostry, and LaMontagne (2007) | Job stress and other working conditions: relationships with smoking behaviors in a representative sample of working Australians | Australia | NR | 1101 | 575 | 74 | Multiple Industries | |
| Yang et al. (2008) | Emergence of socioeconomic inequalities in smoking and overweight and obesity in early adulthood: the National Longitudinal Study of Adolescent Health | United States | 1995–1996, 2001–2002 | 9542 | 4580 | NR | Multiple Industries | |
| Okechukwu, Nguyen, and Hickman (2010) | Partner smoking characteristics: associations with smoking and quitting among blue-collar apprentices | United States | NR | 1767 | 88 | 88 | Construction of Buildings | |
| Sayem et al. (2010) | An assessment of risk behaviours for HIV/AIDS among young female garment workers in Bangladesh | Bangladesh | 2007 | 300 | 300 | 300 | Apparel Manufacturing | |
| Biron, Bamberger, and Noyman (2011) | Work-related risk factors and employee substance use: insights from a sample of Israeli blue-collar workers | Israel | NR | 569 | NR | NR | Manufacturing | |
| Hammarström et al. (2011) | Mechanisms for the social gradient in health: results form a 14-year follow-up of the Northern Swedish Cohort | Sweden | 1981–1995 | 1083 | 495 | NR | Multiple Industries | |
| Chin et al. (2012) | Cigarette smoking in building trades workers: the impact of work environment | United States | 2004–2007 | 1817 | 88 | 88 | Construction of Buildings | |
| Chin et al. (2012) | Occupational factors and smoking cessation among unionized building trades workers | United States | 2004– 2007 | 763 | 44 | 44 | Construction of Buildings | |
| Chin et al. (2013) | Heavy and light/moderate smoking among building trades construction workers | United States | NR | 763 | 63 | 63 | Construction of Buildings | |
| Cho and Lee (2012) | The relationship between cardiovascular disease risk factors and gender | South Korea | 2005 | 4556 | 2596 | NR | Multiple Industries | |
| Fujishiro et al. (2012) | Occupational gradients in smoking behavior and exposure to workplace environmental tobacco smoke: the Multi-Ethnic Study of Atherosclerosis (MESA) | United States | 2000–2002 | 6355 | 3249 | 373 | Multiple Industries | |
| Noonan and Duffy (2012) | Smokeless tobacco use among operating engineers | United States | 2008 | 498 | 37 | 37 | Specialty Trade Contractors | |
| Okechukwu et al. (2012) | Smoking among construction workers: the nonlinear influence of the economy, cigarette prices, and antismoking sentiment | United States | 1992–1993, 1995–1996, 1998–1999, 2001–2002, 2003, 2006–2007 | 52418 | 1479 | 1479 | Construction of Buildings | |
| Cunradi, Ames, and Xiao (2014) | Binge drinking, smoking and marijuana use: the role of women's labor force participation | United States | 2006–2007 | 956 | 956 | 104 | Construction of Buildings | |
| Maron et al. (2015) | Occupational inequalities in psychoactive substance use: a question of conceptualization | Germany | 2012 | 9084 | 5155 | 994 | Multiple Industries |
| Outcome Category | Study Design | Independent Variable(s)** | Specific Outcome | Referent Group | Summary of Study Findings | Brief Description of Study Population | Country Classification | Citation |
|---|---|---|---|---|---|---|---|---|
| BMI & metabolism | Cross-Sectional | Age, sex, education, ethnic origin, repetitive work (short, medium, and long-cycle), work underload, subjective monotony | Serum glucose levels | Exposure-outcome among blue-collar women | Among blue-collar women, short-cycle repetitive work was associated with higher serum glucose (p = 0.05) levels. | Cardiovascular Occupational Risk Factors Determination in Israel Study (CORDIS) | High-Income | (Melamed et al., 1995) |
| Cross-Sectional | Occupational class, marital status | Waist circumference, waist-to-hip ratio | Blue-collar women vs. other women | Among blue-collar women, waist circumference (ß = -2.40, SE = 8.19) and waist to hip ratio (ß = -0.0294, SE = 0.0065) were lower as compared with white-collar women. | Employees from a single Japanese computer and printing manufacturing company | High-Income | (Nakamura et al., 2000) | |
| Cross-Sectional | Age, education, occupational class, marital status, smoking status, regular physical exercise, physical activity tertiles, total energy intake quartiles | Obesity | Blue-collar women vs. other womenC | The odds of obesity among blue-collar women were increased as compared with white-collar women (OR = 3.5, 95% CI 2.21– 5.55). | Adults living in Porto, Portugal recruited with random digit-dialing | High-Income | (Santos & Barros, 2003) | |
| Longitudinal | Education, log-income, occupational class | Type 2 Diabetes | Blue-collar women vs. other women | The hazard of type 2 diabetes among blue-collar women was increased as compared with white-collar women (HR = 0.86, 95% CI 0.53 –1.41). | Alameda County Study | High-Income | (Maty et al., 2005) | |
| Longitudinal | Parental occupation; childhood household deprivation (public assistance, no plumbing, no electricity, food scarcity); adult SEP index; education; occupational class; lifecourse SEP | Weight Change | Blue-collar women vs. other womenC | Blue-collar women demonstrated larger 13- year increases in BMI as compared with white-collar women (5.8 vs. 4.8 kg/m2, p 0.05). | Pitt County Study | High-Income | (Bennett et al., 2007) | |
| Longitudinal | Recent Retirement | Weight loss of 5% or greater; weight gain of 5% or greater | Exposure-outcome among blue-collar women | Among blue-collar women, retirement was inversely associated with a weight loss of 5% or greater (OR = 0.88, 95% 0.57–1.37). Retirement was positively associated with a weight gain of 5% or greater (OR = 1.58, 95% CI 1.13–2.21). | Health and Retirement Study (HRS) | High-Income | (Forman-Hoffman et al., 2008) | |
| Longitudinal | Young adult socioeconomic position (education and occupational class); family socioeconomic position; family structure; family connectedness; smoker in home; easy access to cigarettes; high school; CES-D; number of friends who smoke; BMI during adolescence | Overweight, Obesity | Blue-collar women vs. other womenC | Odds of overweight (OR = 1.04, 0.49–2.21) or obesity (OR = 0.74, 0.29 –1.85) were not increased among blue-collar women as compared to women with further education. | National Longitudinal Study of Adolescent Health | High-Income | (Yang et al., 2008) | |
| Cross-Sectional | Occupational class, education, poverty-income ratio | Obesity | Blue-collar women vs. other womenC | The odds of obesity among blue-collar women were increased as compared with white-collar women (OR = 2.08, 95% CI = 1.43–3.05). | Third Korean National Health and Nutrition Examination Survey (KNHANES III) | High-Income | (Cho and Lee, 2012) | |
| Cross-Sectional | Age, female, white, married, high-school or less, SF-36 pain, self-reported medical comorbidities, depression, smoking, alcohol problem, vegetable intake, fruit intake, fried food intake, physical activity | Obesity | Male vs. female blue-collar workersC | The odds of obesity among female operating engineers were decreased as compared with male operating engineers (OR = 0.283, 95% CI 0.083–0.827). | Convenience sample of operating engineers recruited during a three-day safety training course | High-Income | (Duffy et al., 2012) | |
| Longitudinal | Soft drinks intake, 100% fruit juice intake, vegetable juice intake, age, sports activity, education, occupational class, BMI, Menopausal status | Diabetes Mellitus | Exposure-outcome among blue-collar women | Among blue-collar women, the odds of type 2 diabetes were increased among those who drank soda every day (OR = 2.57, 95% CI 1.25–5.29); those who drank soda 3-4 times per week (OR = 125, 95% CI 0.66–2.35); and those who drank soda two times or less per week (OR = 1.18, 95% CI 0.77–1.80) as compared with those who rarely drank soda. | Japan Public Health Center Study (JPHC) | High-Income | (Eshak et al., 2013) | |
| Cross-Sectional | Education, household income, occupational class | Healthy takeaway food; less healthy takeaway food | Blue-collar women vs. other women | Blue-collar women had increased BMI as compared with professionals and managers (ß = 2.83, SE = 0.99). | Adults randomly selected form the electoral roll of the Brisbane statistical subdivision. | High-Income | (Miura and Turrell, 2014) | |
| Cross-Sectional | Age, individual education, parental education, HDI of country of birth, residential education level, residential density of population, occupational class, home work distance | Fat Mass Index | Blue-collar women vs. other women | There was no significant association between work economic sector and fat mass index (FMI) for women in the manufacturing industry (ß = 0.31, 95% CI 0.04–1.73); construction (ß = 0.18, 95% CI - 2.44 to 2.81); or commercial repair of motor vehicles and motorcycles (ß = 0.43, 95%CI - 0.60 to 1.46) as compared with women in transport and communications. | Residential Environment and Coronary Heart Disease Cohort Study (RECORD) | High-Income | (Lewin et al., 2014) | |
| Cross-Sectional | Overtime work (≥ 60 hours/week), social support, job stress, risk perception, physical exercise (≥ 30 min, ≥ 3 per week) | Metabolic Syndrome | Exposure-outcome among blue-collar women | Among blue-collar women, low job stress (OR = 0.05, p = 0.04), low social support (OR = 1.51, p = 0.009), and risk perception (OR = 1.27, p = 0.023) were associated with metabolic syndrome. | Blue-collar workers at small companies recruited from occupational health centers or worksites during annual health checkups in South Korea. | High-Income | (Hwang and Lee, 2014) | |
| Cancer | Longitudinal | Highest level of education, highest level of education (household), EPG score: last profession, U&S score: last profession | Breast Cancer | Blue-collar women vs. other women | There was no difference in breast cancer risk in blue-collar women and lower white-collar women (RR = 1.01, 95% CI 0.69–1.49); the risk of breast cancer was increased among upper white-collar women as compared with blue-collar women (RR = 1.19, 95% CI 0.80 –1.76). | The Netherlands Cohort Study (NLCS) | High-Income | (Van Loon et al., 1994) |
| Longitudinal | Highest level of education, occupational class, social standing (U&S) score | Colon Cancer | Blue-collar women vs. other women | As compared with blue-collar women, the risk of colon cancer was increased among lower white-collar women (RR = 1.30, 95% CI 0.76–2.22) but decreased among upper white-collar women (RR = 0.63, 95% CI 0.30–1.29) | The Netherlands Cohort Study (NLCS) | High-Income | (Van Loon et al., 1995) | |
| Case-Control | Occupation | Cancer of the CNS | Blue-collar women vs. other women | Industries showing consistent increases in risk for cancer of the CNS by gender and race included textile mills, paper mills, printing and publishing industries, petroleum refining, motor vehicles manufacturing, telephone and electric utilities, department stores, health care services, elementary and secondary schools, and colleges and universities. | United States Vital Statistics Records | High-Income | (Cocco et al., 1999) | |
| Longitudinal | Occupation | Breast Cancer | Blue-collar women vs. other women | Excess risk for breast cancer was found for pharmacists, teachers of theoretical subjects, schoolmasters, systems analysts and programmers, telephone operators, telegraph and radio operators, metal platers and coaters, and hairdressers and beauticians. | All living Swedish women ages 25–64 who were employed at the time of the 1970 census and present in the country during the 1960 census. | High-Income | (Pollán and Gustavsson, 1999) | |
| Case-Control | Exposure to known and suspected lung carcinogens. | Lung Cancer | Exposure-outcome among blue-collar women | Lung cancer risk was increased among female rubber workers exposed to suspected carcinogens versus those unexposed (OR = 2.2, 95% CI = 0.6–7.9); among female glass workers exposed to suspected carcinogens versus those unexposed (OR = 2.8, 95% CI 0.4–22); and among laundry and dry cleaners exposed to suspected carcinogens versus those unexposed (OR = 2.1, 95% CI = 0.8–5.6). | Incident lung cancer cases and population controls in Northern Italy | High-Income | (Richiardi et al., 2004) | |
| Case-Control | Metalworking fluid (MWF) | Breast Cancer | Exposure-outcome among blue-collar women | There was an increase in the odds of breast cancer associated with every mg/m3-year increase of cumulative exposure to soluble MWF over the ten-year study period (OR = 1.18, 95% CI 1.02–1.35). | Female hourly automobile production workers from three large manufacturing plants in Michigan | High-Income | (Thompson et al., 2005) | |
| Case-Control | Occupational class, education | Lung Cancer | Blue-collar women vs. other women | The odds of lung cancer among blue-collar women were decreased as compared with white-collar women (OR = 0.96, 95% CI 0.74–1.25). | Incident lung cancer cases and hospital-based controls in seven Eastern European countries. | High-Income and Upper-Middle-Income | (Hrubá et al., 2009) | |
| Case-Control | Occupation of first employment | Bladder Cancer | Exposure-outcome among blue-collar women | Among women, bladder cancer risk was significantly elevated and increased significantly with duration of employment in the electronic components and accessories industry (OR = 2.2, 95% CI 1.1 to 4.7) and the transportation equipment industry (OR = 8.7, 95% CI 2.0–37). | Incident bladder cancer cases and population controls in Maine, Vermont, and New Hampshire. | High-Income | (Colt et al., 2011) | |
| Longitudinal | Metalworking fluid (MWF) | Cervical Cancer | Exposure-outcome among blue-collar women | There was no difference in cervical cancer risk among blue-collar women exposed or not exposed to straight MWF (RR = 1.0, 95% CI 0.46–2.19). Risk of cervical cancer among blue-collar women exposed to soluble MWF increased as compared with unexposed workers (RR = 1.55, 95% CI 0.66–3.61). Risk of cervical cancer among blue-collar women exposed to synthetic MWF increased as compared with unexposed women (RR = 1.14, 95% CI 0.50–2.60). | Female hourly automobile production workers from three large manufacturing plants in Michigan | High-Income | (Betenia et al., 2012) | |
| Case-Control | Duration of Employment | Breast Cancer | Exposure-outcome among blue-collar women | The odds of breast cancer among women with 20+ years of employment versus those with 0 to 4 years of employment were increased in the iron and steel industry (OR = 1.22, 95% CI 0.72–2.07); mechanical manufacturing (OR = 1.11, 95% CI 0.92–1.34); electrical manufacturing (OR = 1.37, 95% CI 1.10–1.71); the food industry (OR = 1.13, 95% CI 0.83–1.19); the textile industry (OR = 1.13, 95% CI 0.98–1.29); the garment industry (OR = 1.16, 95% CI 1.01–1.34); the wood industry (OR = 1.22, 95% CI 0.80–1.85); the rubber industry (OR = 2.71, 95% CI 1.25–5.87); the building industry (OR = 1.45, 95% CI 0.28–7.59); the transport industry (OR = 1.15, 95% CI 0.34–3.93); the chemical industry (OR = 1.52, 95% CI 0.96–2.42); the alcoholic beverages and wine production industry (OR = 1.46, 95% CI 0.26–8.10); the pharmaceutical industry (OR = 1.31, 95% CI 0.70–2.43); and the dry cleaning sector (OR = 2.29, 95% CI 0.97–5.41) but not for women in healthcare and veterinarian services, the plastic industry, the pottery industry, agriculture, the paper industry, the leather and shoe industry, or the press industry. | Incident cases of female breast cancer and population controls in Lombardy, Italy | High-Income | (Oddone et al., 2013) | |
| Longitudinal | Occupational class in 1993 and 1975; high job authority in 1975; adiposity in 1957; reproductive history in 1975 and 1993; job characteristics in 1975; health behaviors in 1993; work under pressure of time, responsibility outside control, high job autonomy; job satisfaction; high job authority; life-course estrogen cycle; family history of breast cancer | Breast Cancer | Blue-collar women vs. other women | The risk of breast cancer was increased among female crafts/operatives laborers as compared with housewives (HR = 0.87, 95% CI 0.51–1.48). | Wisconsin Longitudinal Survey (WLS) | High-Income | (Pudrovska et al., 2013) | |
| Case-Control | Exposure to lead and lead alloys, chlorinated solvents, lubricant oils, non-ionizing radiation, epoxy resins, and job title | Breast Cancer | Blue-collar women vs. other women | The odds of breast cancer were increased among blue-collar women exposed to chlorinated solvents as compared with unexposed women (OR 1.65, 95% CI 1.04−2.62). There was a two-fold increase among blue-collar women exposed for at least 10 years as compared with unexposed women (OR 2.10, 95% CI 1.21−3.66). | Incident cases of female breast cancer and controls selected from a single, large electrical manufacturing plant near Milan, Italy. | High-Income | (Oddone et al., 2014) | |
| Cardiovascular disease | Cross-Sectional | Sound pressure level, age, working years, salt (high), salt (normal), family history | Hypertension | Exposure-outcome among blue-collar women | Among female textile mill workers, sound pressure levels (SPL) were associated with the prevalence of hypertension (ß = 0.03, SE = 0.015). | Female workers in a textile mill in Beijing, China | Upper-Middle-Income | (Zhao et al., 1991) |
| Longitudinal | Occupational class, work control, work social support, psychological job demand, physical job demand | Cardiovascular morbidity | Exposure-outcome among blue-collar women | Among blue-collar women, cardiovascular morbidity was more prevalent among those with low work social support (OR = 1.19, 95% CI 1.01–1.14) and high physical job demand (OR = 1.15, 95% CI 0.97–1.35). Cardiovascular disease was less prevalent among blue-collar women with high psychological job demand (OR = 0.76, 95% CI = 0.60–0.97). There was no association between work control and cardiovascular morbidity (OR = 1.02, 95% CI 087–1.20). | Survey of Living Conditions | High-Income | (Hall et al., 1993) | |
| Case-Control | Job characteristics | Myocardial Infarction | Exposure-outcome among blue-collar women | Among blue-collar women, increased risk of first MI was associated with monotony (RR = 1.4, 95% CI 0.3–6.9) few possibilities to learn new things (RR = 2.1, 95% CI = 0.9–4.9), long working hours (RR = 1.1, 95% CI 0.7–1.7), low influence on planning of work (RR = 2.0, 95% CI = 0.3–15.6), low influence on working hours (RR = 1.1, 95% CI 0.8–1.7), and noise (RR = 1.4, 95% CI 0.9–2.1). Decreased risk of MI was associated with hectic work (RR = 0.7, 95% CI 0.5–1.1) and low influence on work tempo (RR = 0.7, 95% CI 0.4–1.3) | Incident cases of myocardial infarction and population-based controls in four rural Swedish Counties and Stockholm County. | High-Income | (Hammar et al., 1994) | |
| Cross-Sectional | Age, sex, education, ethnic origin, repetitive work (short, medium, and long-cycle), work underload, subjective monotony | Systolic blood pressure, diastolic blood pressure, total cholesterol, LDL, HDL, triglycerides | Exposure-outcome among blue-collar women | Among blue-collar women, short-cycle repetitive work was associated with higher mean systolic (p = 0.003) and diastolic (p = 0.01) blood pressure; and total cholesterol (p = 0.03). | Cardiovascular Occupational Risk Factors Determination in Israel Study (CORDIS) | High-Income | (Melamed et al., 1995) | |
| Longitudinal | Symptoms of chronic bronchitis | First coronary event | Exposure-outcome among blue-collar women | Among blue-collar women, the risk of first coronary event was increased among those with Grade 1 symptoms (RR = 1.98, 95% CI 0.56–7.01) and those with Grade 2 symptoms (RR = 1.93, 95% CI 0.69–5.39) as compared with blue-collar women with no symptoms. | A random sample of the population of the eastern Finnish provinces of North Karelia and Kuopio. | High-Income | (Jousilahti et al., 1996) | |
| Cross-Sectional | Noise-exposure level, noise annoyance | Cholesterol, LDL, HDL, Cholesterol/HDL, triglycerides | Exposure-outcome among blue-collar women | Among blue-collar women with high noise-exposure and high noise-annoyance, the mean-adjusted cholesterol level was 207 mg/dl (SE = 9.4); LDL levels were 125 mg/dl (SE = 8.6); HDL levels were 57 mg/dl (SE = 3.1); the ratio of Cholesterol to HDL was 4.1 (SE = 0.3) and the mean-adjusted triglyceride level was 126 mg/dl (SE = 14.0). | Cardiovascular Occupational Risk Factors Determination in Israel Study (CORDIS) | High-Income | (Melamed et al., 1997) | |
| Case-Control | Education, occupational level, decision latitude at work | Cholesterol, triglycerides, HDL, Cholesterol/HDL, LDL/HDL, ApoB, ApoA1 | Blue-collar women vs. other women | As compared with white-collar women, cholesterol levels (difference = 0.11, p = 0.42), triglyceride levels (difference = 0.07, p = 0.78), HDL levels (difference = 0.09, p = 0.23), the cholesterol to HDL ratio (difference = 0.36, p = 0.17), the LDL to HDL ratio (difference = 0.31, p = 0.18), and the Apolipoprotein B to apolipoprotein A1 ratio (difference = 0.06, p = 0.63) were higher among blue-collar women. | Stockholm Female Coronary Risk Study (FemCorRisk) | High-Income | (Wamala et al., 1997) | |
| Case-Control | Occupational class, male- or female-dominated occupation | Myocardial Infarction | Blue-collar women vs. other women | Increased risk of MI was found among blue-collar women (RR = 1.41, 95%CI 1.15–1.73) in jobs where men predominate as compared with other women. | Population aged 30-74 residing in one of five Swedish counties including Stockholm. | High-Income | (Ostlin et al., 1998) | |
| Cross-Sectional | Age, occupational class | Pain or discomfort in the chest when excited; pain or discomfort in the chest after a substantial meal; Palpitation of the heart or irregular heartbeat | Blue-collar women vs. other women | As compared with blue-collar women, white-collar women experienced less pain or discomfort in the chest when excited (OR = 0.42, 95% CI 0.26–0.68). There was no difference in the odds of pain or discomfort in the chest after a substantial meal (OR = 1.05, 95% CI 0.45–2.44) or palpitations of the heart or irregular heartbeat (OR = 0.99, 95% CI 0.71–1.38). | A stratified sample of residents aged 18 to 74 in the four primary health care areas of Halland County, Sweden. | High-Income | (Baigi et al., 2001) | |
| Cross-Sectional | Job strain | Hypertension | Exposure-outcome among blue-collar women | There was no association between job strain and hypertension among blue-collar women (OR = 1.01, 95% CI 0.87–1.17). | The Jichi Medical School Cohort Study (JMS) | High-Income | (Tsutsumi et al., 2001) | |
| Case-Control | Short stature, early life socioeconomic disadvantage (large early life family size, singletons, born last, low education), adult life socioeconomic disadvantage (occupational class at labour force entry, blue-collar occupation at examination, economic hardship prior to CHD event). | Coronary heart disease | Blue-collar women vs. other women | The odds of CHD were increased among women whose occupation at labor force entry was blue-collar as compared with women whose occupation at labor force entry was white-collar (OR = 1.80, 95% CI 1.12–3.12). The odds of CHD among women whose occupation at examination was blue-collar as compared to women whose occupation at examination was white-collar (OR = 1.69, 95% CI 0.95–2.88). | Stockholm Female Coronary Risk Study (FemCorRisk) | High-Income | (Wamala et al., 2001) | |
| Cross-Sectional | Age, behavioral risk factors, occupational class | Average carotid intima-media thickness | Blue-collar women vs. other women | Carotid intima-media thickness was reduced among blue-collar women as compared with female clerical workers (ß = -0.064, SE = 0.027). | Healthy Women Study (HWS) | High-Income | (Gallo et al., 2003) | |
| Longitudinal | Occupational class | Total stroke, intraparanchymal hemorrhage, subarachnoid hemorrhage, ischemic stroke, coronary heart disease | Blue-collar women vs. other women | As compared with blue-collar women, white-collar women had lower risk of total stroke (HR = 0.93, 95% CI 0.58–1.51), intraparenchymal hemorrhage (HR = 0.34, 95% CI 0.09–1.21), ischemic stroke (HR = 0.72, 95% CI 0.36–1.47), and coronary heart disease (HR = 0.66, 95% CI 0.20–2.21). Risk of subarachnoid hemorrhage was increased among white-collar women compared with blue-collar women (HR = 2.68, 1.03–6.94). | The Jichi Medical School Cohort Study (JMS) | High-Income | (Honjo et al., 2010) | |
| Longitudinal | Occupational class | Hypertension | Blue-collar women vs. other women | Among women, there was an association between hourly (i.e. blue-collar) status and hypertension among those predicted to be hourly workers based on propensity scores (OR = 1.78, 95% CI 1.34–2.35). | The American Manufacturing Cohort Study (AMC) | High-Income | (Clougherty et al., 2011) | |
| Longitudinal | Job characteristics | Stroke | Exposure-outcome among blue-collar women | Among blue-collar women, there was no association between risk of incident stroke among women with active jobs (HR = 0.9, 95% CI 0.3–24), passive jobs (HR = 1.0, 95% CI 0.4–2.4), or high strain jobs (HR = 1.04, 95% CI 0.4–2.5) as compared to those with low-strain jobs. | The Jichi Medical School Cohort Study (JMS) | High-Income | (Tsutsumi et al., 2011) | |
| Cross-Sectional | Occupational class, education, poverty-income ratio | Hypertension, non-HDL Cholesterol | Blue-collar women vs. other women | The odds of hypertension among blue-collar women were increased (OR = 1.30, 95% CI = 1.04–1.61) and the odds of NHDLC were decreased (OR = 0.74, 95% CI = 0.51–1.09) as compared with white-collar women. | Third Korean National Health and Nutrition Examination Survey (KNHANES III) | High-Income | (Cho and Lee, 2012) | |
| Longitudinal | Cumulative noise exposure, duration of exposure, first year of exposure | Hypertension | Blue-collar women vs. other women | The risk of hypertension among female industrial workers is increased as compared with female financial workers (RR = 1.17, 95% CI 1.09–1.26). | Workers employed in one of 625 companies in the industrial trades and 100 companies in the financial services in Aarhaus County, Denmark. | High-Income | (Stokholm et al., 2013) | |
| Cross-Sectional | Age, gender, education, knowledge of CVD risk, CVD risk perception, waist-to-hip ratio, social support, ERI ratio (job stress), exposure to chemicals or noise, shift work, overtime work | Actual CVD Risk | Male vs. female blue-collar workersC | Actual cardiovascular disease risk among blue-collar women was decreased as compared with blue-collar men (ß = - 0.092, p = 0.709). | Blue-collar workers from companies with fewer than 300 employees recruited through an occupational health center in South Korea. | High-Income | (Won et al., 2013) | |
| Longitudinal | Occupational class | Annual and baseline differences in common carotid intima-media thickness (IMT), carotid plaque score, and prevalence of carotid plaque showing. | Blue-collar women vs. other women | Compared with professional women at baseline, the common carotid IMT was increased (0.005, 95% -0.026 to 0.035), the carotid plaque score was decreased (-0.04, 95% CI - 22.7 to 28.3) and the prevalence of carotid plaque showing was decreased (-12.6, 95% CI - 41.7 to 31.2) in blue-collar women. Compared with professionals, the annual change in common carotid IMT was smaller (-0.001, 95% CI - 0.003 to 0.002), the annual change in carotid plaque score was greater (0.03, 95% CI - 2.0 to 2.7) and the annual change in the prevalence of carotid plaque showing was greater (2.0, 95% CI - 2.9 to 7.1) in blue-collar women. | Multi-Ethnic Study of Atherosclerosis (MESA) | High-Income | (Fujishiro et al., 2015) | |
| Disability & Absenteeism | Cross-Sectional | Occupational class and material circumstances; unemployment and labor force participation; and family roles | Limiting Long-Standing Illness | Blue-collar women vs. other women | The odds of limiting, longstanding illness were increased among unskilled manual (OR = 2.24, p < 0.05); semi-skilled manual (OR = 1.70, p < 0.05); and skilled manual women (OR = 1.79, p < 0.05) as compared with professional women. | British General Household Survey | High-Income | (Arber, 1991) |
| Cross-Sectional | Occupation, months on the job, decision latitude, social supports at work, work dissatisfaction, does not have enough money, economic tensions, family tensions, negative self-image, perceived health status, age, education, number of children < 15 years, number of utilities | Functional impediments | Blue-collar women vs. other women | Female electronics workers reported fewer functional impediments than service workers (ß = - 0.72, 95% CI - 1.39, to 0.03) and female garment workers reported fewer functional impediments than service workers (ß = - 0.21, 95% CI - 0.84,0.42). | Women in Tijuana working as electronic maquiladora workers; garment maquiladora workers; service workers; and those with no labor force history | Upper-Middle-Income | (Guendelman and Silberg, 1993) | |
| Longitudinal | Occupational class | Short periods of sick leave; long periods of sick leave; sick leave because of an infection; sick leave because of musculoskeletal disorder; sick leave because of trauma | Blue-collar women vs. other women | As compared with higher grade white-collar women, the risk of short periods of sick leave (RR = 1.13, 95% CI 0.99 - 1.29), long periods of sick leave (RR = 2.80, 95% CI 2.55–3.06), sick leave because an infection (RR = 1.58, 95% CI 1.34–1.87), sick leave because of a musculoskeletal disorder (RR = 6.90, 95% CI 5.67–8.41), and sick leave because of trauma (RR = 3.42, 95% CI 2.59–4.50) were increased among blue-collar women. | Employees of the local governments in the Finnish towns of Raisio, Valkeakoski, and Nokia. | High-Income | (Vahtera et al., 1999) | |
| Cross-Sectional | Occupational class | Reduced activity days, time off work | Blue-collar women vs. other womenC | As compared with professional women, the odds of having a long-term condition (OR = 0.80, 95% CI 0.62–1.04), a short-term condition (OR = 0.89, 95% CI 0.62–1.04), reduced activity days (OR = 0.87, 95% CI 0.66–1.15), and time off work (OR = 0.95, 95% CI 0.66–1.39) were decreased among blue-collar women. | Campbell National Health Monitor | High-Income | (Korda et al., 2002) | |
| Cross-Sectional | Occupational class | Work ability | Blue-collar women vs. other women | As compared with white-collar women, blue-collar women had increased odds of lowered work ability (OR = 1.11, 95% CI 0.67–1.84). As compared with upper white-collar workers, odds of lowered work ability were also increased among blue-collar women (OR = 2.11, 95% CI 1.06–4.21). | Helsinki Health Study | High-Income | (Aittomäki et al., 2003) | |
| Longitudinal | Role clarity, fairness, organizational climate | Short sickness absence; long sickness absence; very long sickness absence | Exposure-outcome among blue-collar women | Among blue-collar women, the rate of short absence spells for those exposed to poor organizational climate were 1.6 times the rate of short absence spells for those with a favorable organizational climate (HR = 1.6, 95% CI 1.0–2.5). | All employees of a forest industry corporation in Finland | High-Income | (Väänänen et al., 2004) | |
| Longitudinal | Race/ethnicity, age, education, occupation, shift worked, tenure, hourly rate of pay, full-time employment, having 2 jobs | Lost-Worktime Injury or Illness | Blue-collar women vs. other womenC | Among women, the odds of reporting a lost-worktime injury or illness were decreased among machine operators (OR = 0.73, 95% CI 0.38–1.41) and craftswomen (OR = 0.57 (0.24, 1.33) as compared with laborers. The rates of lost-worktime injury or illness were increased among machine operators (IRR = 2.41, 95% CI 0.86–6.74) and decreased among craftswomen (IRR = 0.58, 95% CI 0.19–1.78) as compared with laborers. | National Longitudinal Survey of Youth 1979 (NLSY) | High-Income | (Strong and Zimmerman, 2005) | |
| Longitudinal | Occupational class | Sickness absence | Blue-collar women vs. other women | As compared with female executive managers and academics, the rates of long-term sickness absence were increased among skilled blue-collar women (RR = 2.06, 95% CI 0.69–6.17) and among semiskilled and unskilled women (RR = 2.76, 95% CI 1.00–7.65). | Danish Work Environment Cohort Study (DWECS) | High-Income | (Christensen et al., 2008) | |
| Cross-Sectional | Occupational class | Long sickness absence | Blue-collar women vs. other women | Odds of long-term sickness absence (OR = 2.45, 1.90–3.15) and work injury (OR = 5.63, 3.13-10.16) were higher among blue-collar women as compared to professionals/managers. | SUMER Study | High-Income | (Niedhammer et al., 2008) | |
| Longitudinal | Family type, domestic responsibilities, negative work-family spillover | Sickness absence | Exposure-outcome among blue-collar women | Among blue-collar women, the rates of sickness were increased for those with no children (RR = 1.11, 95% CI 0.96–1.30) and those with children 0–6 years old (RR = 1.11 (0.955–1.3) as compared to those with children 7–18 years old. Rates of sickness absence were increased if domestic responsibilities were the woman's duty alone (RR = 1.08, 0.93-12.4) or shared equally (RR = 1.15, 1.00–1.33) as compared to when they were somebody else's. Rates of sickness absence were increased for high negative work-family spillover (RR = 1.44, 1.25–1.66) and moderate work-family spillover (RR = 1.10, 0.95-1.27) as compared to low work-family spillover. | Finnish 10-Town Study | High-Income | (Väänänen et al., 2008) | |
| Longitudinal | Work ability in midlife | Disability | Blue-collar women vs. other women | As compared with white-collar women in excellent health, the odds of disability were increased among blue-collar women with excellent health (OR = 1.40, 95% CI 0.96–2.05), moderate health (OR = 2.41, 95% CI 1.78–3.26), and poor health (OR = 3.91, 95% CI 2.68–5.70). | Finnish Longitudinal Study on Municipal Employees (FLAME) | High-Income | (von Bonsdorff et al., 2011) | |
| Cross-Sectional | Heart rate reserve | Reduced work ability | Exposure-outcome among blue-collar women | Among blue-collar women, reduced work ability was inversely associated with increased heart rate reserve (OR = 0.30, 95% CI 0.04–2.30). | New method for Objective Measurements of physical Activity in Daily living (NOMAD) study | High-Income | (Gupta et al., 2014) | |
| Longitudinal | Job demand, job control, social support, job insecurity, organizational injustice, lack of reward, discomfort in occupational climate | Absence due to Accident | Exposure-outcome among blue-collar women | Among blue-collar women, the odds of absence due to accidents were increased for women with insufficient job control (OR = 1.95, 95% CI 0.63–6.11), high job insecurity (OR = 1.55, 95% CI 0.48–5.10), high organizational injustice (OR = 1.79, 95% CI 0.54–5.87), lack of reward (OR = 1.54, 95% CI 0.48–4.95), and discomfort in occupational climate (OR = 1.79, 95% CI 0.54–5.87). The odds of absence due to accidents among blue-collar women were decreased among those with high job demand (OR = 0.41, 95% CI 0.12–1.39) and high levels of inadequate social support (OR = 0.81, 95% CI 0.22–2.92). | Workers at 23 manufacturing companies in the Incheon area of South Korea registered for health examinations with the department of occupational and environmental medicine at a university hospital. | High-Income | (Heo et al., 2015) | |
| Health Behaviors | Cross-Sectional | Occupational class, hours worked per week, living arrangement, smoking status, MI, self-reported health | Insufficient physical activity for health | Blue-collar women vs. other women | The odds of insufficient physical activity for health among blue-collar women were 1.55 times the odds of insufficient physical activity for health among professional women (OR = 1.55, 95% CI 1.4–1.8). | Australian National Health Survey (ANHS) | High-Income | (Burton and Turrell, 2000) |
| Cross-Sectional | Physical requirement, stress level, age, education, gender, race (white or black), drinking, smoking, self-reported health, workhours, any children younger than 18, have spouse, spouse working, spouse exercise level | Vigorous Physical Activity | Male vs. female blue-collar workersB | Male blue collar workers were more likely to engage in light physical activity than female blue-collar workers (ß = 0.03, p > 0.05). Male blue-collar workers were significantly more likely to engage in vigorous physical activity as compared with female blue-collar workers (ß = 0.11, p < 0.001). | Health and Retirement Study (HRS) | High-Income | (Wu and Porell, 2000) | |
| Cross-Sectional | Age, education, income, married, occupation, current smoker, commuting physical activity | Leisure-time physical activity | Blue-collar women vs. other womenC | Blue-collar women were less likely to engage in leisure-time physical activity (OR = 0.52, 95% CI = 0.38–0.73), engage in commuting time physical activity (OR = 0.93, 95% CI 0.69–1.26) as compared with blue-collar women. | Residents of Tianjin, China randomly selected using local population registers for 14 randomly selected communities. | Upper-Middle-Income | (Gang et al., 2002) | |
| Cross-Sectional | Age, Education, Occupation | Daily energy expenditure (DEE); weekly physical activity (WPA); leisure-time physical activity (LTPA) | Blue-collar women vs. other women | Among female laborers and machine operators, daily energy expenditures were lower and weekly physical activity was higher as compared with female managers and professionals. Leisure time physical activity was similar in female laborers, machine operators, and managers. | Workers at nine companies or factories located in the east (Kanto) and central (Chubu) areas of Japan. | High-Income | (Takao et al., 2003) | |
| Cross-Sectional | Age, education, occupational class, geographical location, BMI, workplace activity, physical activity level | Achieving 10,000 Steps per Day | Blue-collar women vs. other womenC | Odds of reaching 10,000 steps among blue-collar women are 0.81 times the odds among female managers and professionals (OR = 0.81, 95% CI 0.21–3.06). | Adults in Western Australia randomly selected from the White Pages telephone directory using proportional sampling. | High-Income | (McCormack et al., 2006) | |
| Longitudinal | Age, education, occupational class, smoking status, leisure-time physical activity, BMI | Heterocyclic Amine (HCA) Intake | Blue-collar women vs. other womenC | As compared to blue-collar women, the likelihood of falling in the highest quintile of HCA intake was lower among medium-status white-collar women (OR = 0.81, 95% CI 0.69-0.96), high-status white-collar women (OR = 0.76, 95% CI 0.59-0.97) and among self-employed women (OR = 0.97, 95% CI 0.78–1.21). No differences were found between low-status white-collar women and blue-collar women (OR = 1.00, 95% CI 0.89–1.14). | The Malmö Diet and Cancer (MDC) Study | High-Income | (Ericson et al., 2007) | |
| Cross-Sectional | Occupational class, hours at job, hours on unpaid care, dependents (<18 years) in the home, smoking status, weight status, perceived physical health | Physical activity | Blue-collar women vs. other women | The odds of leisure-time physical activity among blue-collar women were 2.25 times the odds of leisure-time physical activity among women in professional jobs (OR = 2.25, 95% CI 0.92–5.50). | 2000 Kings County Genuine Progress Indicators Survey | High-Income | (Kuiack et al., 2007) | |
| Longitudinal | Sex, education, native language, eating at work to cope with stress, intention to change fruit and vegetable intake, smoking status | Change in fruit and vegetable consumption | Exposure-outcome among blue-collar women | Female construction workers participating in the Tools for Health cancer prevention intervention decreased their fruit and vegetable consumption (ß = -0.36, 95% CI - 2.18 to1.46) over the course of follow-up. | Tools for Health (TFH) | High-Income | (Harley et al., 2010) | |
| Cross-Sectional | Occupational Class | Leisure-time physical inactivity | Blue-collar women vs. other women | Blue-collar women were more likely be inactive during leisure time as compared with white-collar women (OR = 1.50, 95% CI 1.12–2.00). | Finnish Health 2000 Survey | High-Income | (Mäkinen et al., 2010) | |
| Longitudinal | Age, education, employment, occupational class, live births, smoking status, alcohol intake, extra foods, self-rated health, SF12 physical and mental health measures | Pedometer- and self-reported physical activity | Blue-collar women vs. other womenC | Blue-collar women engaged in 2.85 more minutes per week of physical activity as compared with white-collar women (ß = 2.85, 95% CI = - 0.10 - 5.81). | Childhood Determinants of Adult Health (CDAH) Study | High-Income | (Cleland et al., 2011) | |
| Cross-Sectional | Occupational class, education, poverty-income ratio | Physical inactivity | Blue-collar women vs. other women | The odds of physical inactivity were decreased among blue-collar women as compared with white-collar women (OR = 0.64, 95% CI 0.57–0.72). | Third Korean National Health and Nutrition Examination Survey (KNHANES III) | High-Income | (Cho and Lee, 2012) | |
| Cross-Sectional | Education, household income, occupational class | Healthy takeaway food; less healthy takeaway food | Blue-collar women vs. other women | Blue-collar women were less likely to eat healthy takeaway food (ß = 0.73, SE = 2.02) and more likely to eat less healthy takeaway food (ß = 3.67 (1.49) as compared with female managers and professionals. | Adults randomly selected from the electoral roll of the Brisbane statistical subdivision in Australia. | High-Income | (Miura and Turrell, 2014) | |
| Cross-Sectional | Age, education, occupational class, marital status, smoking status, regular exercise, BMI, energy intake, alcohol intake | Inadequate fruit and vegetable consumption (<5 servings per day) | Blue-collar women vs. other womenC | The odds of inadequate fruit and vegetable intake among female blue-collar women were 1.56 times the odds of inadequate fruit and vegetable intake among white-collar women (OR = 1.56, 95% CI 1.20–2.02). | The EPIPorto Study | High-Income | (Oliveira et al., 2014) | |
| Longitudinal | BMI, country of birth, area of residence, educational qualification, marital status, number of children, occupational class, hours worked per week, being active, smoking status, alcohol consumption, being somewhat stressed | Week-day sitting, Weekend-day sitting | Blue-collar women vs. other womenC | Blue-collar women engaged in less weekday sitting as compared with professional women (ß = - 1.30, 95% CI - 1.48, to 1.13). Weekend-day sitting was comparable among blue-collar women and professional women (ß = 0.06, 95% CI - 0.21, 0.10). | Australian Longitudinal Study on Women's Health (ALSWH) | High-Income | (Uijtdewilligen et al., 2014) | |
| Cross-Sectional | Actual CVD risk, age, gender, education, knowledge of CVD risk, perceived general health, family function, social support, decision latitude, exposure to chemicals/noise, shift work | Health-promoting behaviors | Male vs. female blue-collar workersC | Health risk scores among blue-collar women were increased as compared with blue-collar men (ß = 0.116, p = 0.120). | Blue-collar workers at small companies recruited from occupational health centers or worksites during annual health checkups in South Korea. | High-Income | (Hwang et al., 2015) | |
| Longitudinal | BMI, country of birth, area of residence, educational qualification, marital status, number of children, occupational class, hours worked per week, smoking status, alcohol status | Physically Active | Blue-collar women vs. other womenC | Odds of being physically active among blue-collar women were 0.94 times the odds of being physically active among professional women (OR = 0.94, 95% CI 0.83–1.05). | Australian Longitudinal Study on Women's Health (ALSWH) | High-Income | (Uijtdewilligen et al., 2015) | |
| Mental Health | Cross-Sectional | Job demands, job characteristics, physical environment, work-related social support, marriage, children, age, race, education | Distress, happiness | Exposure-outcome among blue-collar women | Distress was inversely associated with substantive complexity of the job (ß = -0.048, p > 0.05); autonomy (ß = -0.013, p > 0.05); income (ß = -0.008, p > 0.05); satisfaction with co-workers (ß = -0.132, p < 0.01); company programs (ß = -.101, p > 0.05); being married (ß = -0.059, p > 0.05); age (p = -0.008, p > 0.05); race (ß = -0.108, p < 0.01); and education (ß = -0.002, p > 0.05). There was no association between distress and overtime or span of control. | Employees at plants in seven manufacturing industries in south central Indiana | High-Income | (Loscocco and Spitze, 1990) |
| Cross-Sectional | Age, current smoker, moderate/heavy alcohol, sever obesity, chronic disease, clean room, current chemical exposure | Depression | Exposure-outcome among blue-collar women | The odds of depression among blue-collar with current chemical exposure were 1.46 times the odds of depression among blue-collar women without current chemical exposure (OR = 1.46, p > 0.05). There was no association between working in the clean room and depression among blue-collar women (OR = 1.00, p > 0.05 | Female workers at a semi-conductor manufacturing plant in Pennsylvania represented by the International Brotherhood of Electrical Workers (IBEW). | High-Income | (Parkinson et al., 1990) | |
| Cross-Sectional | Age, education, marriage, income, smoking, obesity, major illness, life events, solvent exposure, job demands, job conflict, co-worker support, supervisor support, friend/relative support | Depression | Exposure-outcome among blue-collar women | The odds of depression were increased among blue-collar women who smoked (ß = 0.21, p > 0.05); had a major illness (ß = 0.46, p < 0.05); had a life event (ß = 0.44, p < 0.001); were exposed to solvents (ß = 0.27, p < 0.05); or experienced increased job demands (ß = 0.19, p > 0.05) or job conflict (ß = 0.62, p < 0.001). Odds of depression were decreased among blue-collar women who were obese (ß = - 0.31, p > 0.05); and among those with support from co-workers (ß = -0.35, p < 0.05), supervisors (ß = -0.02, p > 0.05), or friends and relatives (ß = -0.50, p < 0.01). | Female workers at a semi-conductor manufacturing plant in Pennsylvania represented by the International Brotherhood of Electrical Workers (IBEW). | High-Income | (Bromet et al., 1992) | |
| Cross-Sectional | Occupation, months on the job, decision latitude, social supports at work, work dissatisfaction, does not have enough money, economic tensions, family tensions, negative self-image, perceived health status, age, education, number of children < 15 years, number of utilities | Depression, nervousness, sense of control | Blue-collar women vs. other women | The odds of depression were increased among garment workers as compared with service workers (ß = 0.77, 95% CI - 0.93 to 2.46) and decreased among electronic workers as compared with service workers (ß = -0.88, 95% CI - 2.57, 0.81). | Women in Tijuana working as electronic maquiladora workers; garment maquiladora workers; service workers; and those with no labor force history | Upper-Middle-Income | (Guendelman and Silberg, 1993) | |
| Cross-Sectional | Age, sex, education, ethnic origin, subjective monotony | Psychological Distress | Exposure-outcome among blue-collar women | Among blue-collar women, psychological distress is associated with subjective monotony (ß = 0.49, p < 0.005). | Cardiovascular Occupational Risk Factors Determination in Israel Study (CORDIS) | High-Income | (Melamed et al., 1995) | |
| Cross-Sectional | Monotony, lack of control, self-esteem | Psychological Distress | Exposure-outcome among blue-collar women | Among blue-collar women ≤ 35 years, psychological distress was positively associated with monotony (ß = 0.23, p > 0.05); lack of control (ß = 0.009, p > 0.05) and self-esteem (ß = 0.066, p > 0.05). Among blue-collar women > 35 years old, psychological distress was positively associated with monotony (ß = 0.050, p < 0.05) and self-esteem (ß = 0.099, p < 0.05), but inversely associated with lack of control (ß = -0.003, p > 0.05). | Blue-collar workers at 37 factories of an industrial company in Finland | High-Income | (Kivimäki and Kalimo, 1996) | |
| Cross-Sectional | Responsibility for the safety of others, skill underutilization, sexual harassment and discrimination, overcompensation at work | Psychological symptoms | Exposure-outcome among blue-collar women | Among female construction workers, having responsibility for the safety of others (ß = 0.456, p < 0.001), skill underutilization (ß = 0.399, p < 0.001), experiencing sexual harassment and discrimination on the job (ß = 0.258, p < 0.001), and having to overcompensate at work (ß = 0.254, p < 0.001). | Female members of the Laborers' International Union of North America (LIUNA) in Seattle, Washington and Portland, Oregon. | High-Income | (Goldenhar et al., 1998) | |
| Longitudinal | Gender, workload score | Psychosomatic complaints, intake of stress-related drugs | Male vs. female blue-collar workers | Intake of stress-related drugs was less frequent among female bus-drivers as compared with male bus drivers (ß = - 0.05, p > 0.05) and there was a negative interaction between gender and workload score (ß = - 0.03, p > 0.05). Psychosomatic complaints were less frequent among female bus-drivers as compared with male bus-drivers (ß = - 0.08, p > 0.05), and there was a positive interaction between gender and workload (ß = 0.18, p > 0.05). | Full-time, employed urban bus drivers working at the same terminal in central Stockholm, Sweden. | High-Income | (Rydstedt et al., 1998) | |
| Cross-Sectional | Age, marital status, foreign background, education, occupational class, current financial support, weekly working hours, financial strain, work stress, drinking, smoking, psychoactive medication, somatic medication, cardiovascular disease, gastro-intestinal diseases, other diseases, pain, depression | Burnout | Blue-collar women vs. other womenC | Odds of burnout among blue-collar women were 0.795 times the odds of burnout among women in other occupations (OR = 0.795, 95% CI 0.324–1.95). | Adult women randomly selected from the general population resident in Stockholm County, Sweden. | High-Income | (Soares et al., 2007) | |
| Case-Control | Occupational class and labor market status; gross income; marital status; parenthood; place of residence; ethnicity | Suicide | Blue-collar women vs. other women | Odds of suicide were among skilled blue-collar women were 1.1 times the odds of suicide among salaried female employees (OR = 1.1, 95% 0.8–1.5) and the odds of suicide among unskilled blue-collar women were 0.9 times the odds of suicide among salaried female employees (OR = 0.9, 95% CI 0.8–1.0). | Incident cases of suicide and population controls drawn from a 5% random subsample of the total Danish population in the IDA database. | High-Income | (Andrés et al., 2010) | |
| Longitudinal | Distance from site; saw people dead or injured; participation in rescue operations; physical injuries; history of depression; harm to close friend or family member (injured or died); job relocation or temporary layoff; sick-leave; lives alone; occupational class | Psychological distress | Blue-collar women vs. other womenA | The odds of psychological distress among female workers at the Toulouse industrial AZF disaster were 1.24 times the odds of psychological distress among female managers and professionals (OR = 1.24, 95% CI 0.48–3.41). | Workers in the metropolitan area of Toulouse, France | High-Income | (Cohidon et al., 2009) | |
| Cross-Sectional | Housework, leisure active transport, biking to/from work, walking to/from work, sports | Stress, distress | Exposure-outcome among blue-collar women | The risks of stress (RR = 2.661, 95% CI 1.098 - 6.447) and distress (RR = 2.911, 95% CI 1.055–8.031) were increased among blue-collar women engaging housework versus those not not. The risks of stress (RR = 1.114, 95% CI 0.478–2.597) and distress (RR = 1.008, 95% CI 0.478–2.344) were increased among blue-collar women engaging in leisure active transport versus those not. The risk of stress was decreased (RR = 0.714, 95% CI 0.266–1.918) and the risk of distress was increased (RR = 2.366, 95% CI 0.863–6.487) among blue-collar women walking to and from work versus those not. The risks of stress (RR = 1.564, 95% CI 0.607–4.030) and distress (RR = 2.202, 95% CI 0.793–6.115) were increased among blue-collar women participating in sports versus those not. | Adults randomly selected from 46 randomly chosen Flemish municipalities. | High-Income | (Asztalos et al., 2009) | |
| Cross-Sectional | Work hours per day, overtime, salary; exposure to chemicals and toxic vapors/substances, exposure to vibration and dangerous equipment, high temperatures, physical dangers/unhealthy conditions at work, poor air/ventilation, crowded workstations and uncomfortable working postures, having a safe work environment, adequate protective clothing and equipment, adequate work-related welfare facilities; psychological job demands/workload, work is interesting, company informs about its achievements, on-site training courses, resources/help and equipment availability, supervisor-related, discrimination - intimidation or threats; household income inadequacy, social and family working hours fit, adequate sanitary living conditiolns/potable water, children under 18. | Mental distress | Exposure-outcome among blue-collar women | Multiple associations reported between various measures of working hours and salary; safety and health; tasks and organizational aspects; extra-organizational factors and mental distress among blue-collar women. | Blue-collar workers from 12 manufacturing companies in Lima, Perú. | Upper-Middle-Income | (Brunette et al., 2011) | |
| Cross-Sectional | Marital status, occupational category, household income, alcohol use, functional limitations, level of stress, experience of depressed feelings | Suicidal Ideation | Blue-collar women vs. other womenC | Suicidal ideation was more prevalent among middle-aged women engaged in manual labor (OR = 2.77, 95% CI 1.20–6.42) as compared with female non-manual workers. | Seoul Citizens Health and Social Indicators Survey | High-Income | (Moon and Park, 2012) | |
| Cross-Sectional | Age, smoking, company's gender equality index, employment hours, occupational class, high engagement in domestic work, number of children < 18 years, work demands, work control, work support, constrained physical heavy work load, work-home imbalance | Emotional exhaustion | Blue-collar women vs. other women | Multiple point estimates reported for the association between emotional exhaustion and exposure to engagement in domestic work and exposure to psychosocial and physical work factors and work-home imbalance. | Employees at 9 companies in computer science and 12 companies in the food industry in Sweden. | High-Income | (Ahlgren et al., 2012) | |
| Cross-Sectional | Psychological demand, social support, sex, marital status, age, education level, duration of employment, perceived work conditions, perceived work protection materials, work absenteeism | Depression | Male vs. female blue-collar workersC | The odds of depression were increased among blue-collar women as compared with blue-collar men (OR = 2.1, 95% CI 0.7–5.2). | Workers at the Le Lai II Shoe Manufacturing Factory in Haiphong City, Vietnam. | Lower-Middle-Income | (Minh, 2014) | |
| Cross-Sectional | Noise annoyance, sleeping time, education, occupational class, household income, smoking, alcohol drinking | Depressive symptoms, suicidal ideation | Blue-collar women vs. other womenA | The odds of suicidal ideation were increased among blue-collar women as compared with white-collar women (OR = 1.27, 95% CI 0.96–1.67), and the odds of depressive symptoms were similar in blue- and white-collar women (OR = 1.02, 95% CI 0.76–1.37). | Third Korean National Health and Nutrition Examination Survey (KNHANES III) | High-Income | (Yoon et al., 2014) | |
| Mortality | Longitudinal | Occupational class, work control, work social support, psychological job demand, physical job demand | Cardiovascular mortality | Exposure-outcome among blue-collar women | Among blue-collar women, odds of cardiovascular mortality were increased for those with high physical job demand (OR = 1.23, 95% CI 0.87–1.73) and decreased for those with high psychological demand (OR = 0.71, 95% CI 0.41–1.24). There was no association between work control (OR = 1.07, 95% CI 0.74–1.47) or work social support (OR = 1.04, 95% CI 0.74–1.47) and cardiovascular mortality among blue-collar women. | Survey of Living Conditions | High-Income | (Hall et al., 1993) |
| Longitudinal | Social class | All-cause mortality, mortality from cardiovascular disease | Blue-collar women vs. other women | As compared with white-collar women, the risks of CHD mortality were higher among skilled (HR = 1.25, 95% CI 0.73–2.13) and unskilled (HR = 1.85, 95% CI 1.11–3.09) blue-collar women. The risks of all-cause mortality were higher for skilled (HR = 1.34, 95% CI 1.04–1.73) and unskilled (HR = 1.50, 95% CI 1.15–1.94) blue-collar women. The risks for all-cause mortality were increased among skilled (HR = 1.34, 95% CI 1.04–1.73) and unskilled (HR = 1.50, 95% CI 1.15–1.94). | A random sample of the population of the eastern Finnish provinces of North Karelia and Kuopio. | High-Income | (Pekkanen et al., 1995) | |
| Case-Control | Occupational Class | Deaths from Accidents, Violence, and Alcohol | Blue-collar women vs. other women | Alcohol-related deaths were more common in blue-collar women as compared with women in non-manual occupations (OR = 3.97, 2.86–5.52); deaths due to accidents and violence were more common in blue-collar women as compared with women in non-manual occupations (OR = 2.07, 95% CI 1.77–2.41). | Incident cases of (i) alcohol-related deaths and (ii) deaths from accidents or violence in Moscow, Russia and controls with cancer-related causes of death. | Upper-Middle-Income | (Chenet et al., 1998) | |
| Longitudinal | Occupational Class | All-cause mortality; mortality due to malignant neoplasms (various), diabetes mellitus, cerebrovascular disease, all heart disease, ischemic heart disease, nonmalignant respiratory disease, cirrhosis of the liver, and external causes | Blue-collar women vs. other women | Relative risks for all causes (0.98), all cancers (0.90), lung cancer (1.34), and breast cancer (0.96) were nonsignificant when mortality was compared to the US female population. No relationship between mortality and length of time employed in the industry or work area was identified. | Workers from 13 high nickel alloys plants located throughout the United States. | High-Income | (Arena et al., 1999) | |
| Longitudinal | Age, occupational class, heart problems | All-cause mortality | Blue-collar women vs. other women | The risk of mortality was increased among female workers as compared with female white-collar workers (RR = 1.16, p = 0.07). | Level of Living Survey (LLS) | High-Income | (Kåreholt, 2001) | |
| Longitudinal | Occupational class | Cardiovascular mortality | Blue-collar women vs. other women | The risk of observed mortality from cardiovascular disease was decreased among white-collar women as compared with blue-collar women (RR = .56, 95% CI 0.50–0.63). | All residents of Halland, Sweden registered in the Population and housing censuses (FoB) | High-Income | (Baigi et al., 2002) | |
| Longitudinal | Education, housing, occupational class, gross income, family type, smoking | Mortality due to respiratory disease | Blue-collar women vs. other womenC | As compared with blue-collar women, mortality from respiratory diseases was lower among white-collar women (HR = 0.68, 95% CI 0.47–0.99) and women outside of the workforce (HR = 0.94, 95% CI 0.63–1.39). | The Copenhagen City Heart Study (CCHS) and the Glostrup Population Studies (GPS) | High-Income | (Prescott et al., 2003) | |
| Longitudinal | Shift work | All-cause mortality | Exposure-outcome among blue-collar women | Among blue-collar women, the risk of all-cause mortality was decreased among those exposed to shift work as compared with those working day shifts (HR = 0.79, 0.50–1.26). | National Survey of Living Conditions (ULF) | High-Income | (Åkerstedt et al., 2004) | |
| Longitudinal | Occupational class | All-cause mortality | Blue-collar women vs. other women | As compared with high and middle bourgeoisie women, the risk of all-cause mortality was increased among unskilled blue-collar women (RR = 1.14, 95% CI 1.08–1.21) and skilled blue-collar women (RR = 1.06, 95% CI 1.00–1.12). | Turin Longitudinal Study | High-Income | (Mamo et al., 2005) | |
| Cross-Sectional | Occupational class | All-cause cancer mortality; lung cancer mortality | Blue-collar women vs. other women | There was no difference in cancer mortality risk among blue-collar women as compared with professional women (RR = 1.03, 95% CI 0.96–1.11). As compared with professional women, the risk of cancer mortality was increased among blue-collar women when breast cancer was excluded (RR = 1.12, 95% CI 1.02–1.22) and the risk of lung cancer mortality was increased among blue-collar women (RR = 1.12, 95% CI 1.02–1.22). | The adult population of Australia nested within Statistical Local Areas (SLA) | High-Income | (Bentley et al., 2008) | |
| Longitudinal | Gender, race, age, exposure to chrysotile fibers | Lung cancer mortality; Asbestosis Mortality; Pneumoconiosis and other respiratory diseases mortality | Exposure-outcome among blue-collar women | As compared with women whose cumulative exposure to chrysotile fibers was less than 1.5 fibre-years/ml, the risk of lung cancer mortality was decreased among those exposed to between 1.5 and 5 fibre-years/ml (RR = 0.59, 95% CI 0.22–1.61); but was increased among those exposed to between 5 and 15 fibre-years/ml (RR = 1.51, 95% CI 0.69–3.33), between 15 and 60 fibre-years/ml (0.69–3.33), between 60 and 120 fibre-years/ml (RR = 3.40, 95% CI 1.52–7.60), and more than 120 fibre-years/ml (RR = 3.84, 95% CI 1.41–10.5). | Workers exposed to chrysotile in a South Carolina asbestos textile plant. | High-Income | (Hein et al., 2007) | |
| Longitudinal | Years smoked, drinks per week, age, male gender, race/ethnicity | All-cause mortality | Male vs. female blue-collar workersC | All-cause mortality risk was increased among male urban transit operators as compared with female urban transit operators (HR = 1.464, 95% CI 0.767–2.795). | San Francisco MUNI Health and Safety Study | High-Income | (Lipton et al., 2008) | |
| Longitudinal | Age of retirement for old-age pensioners, age of retirement for reduced earning capacity pensioners, year, age, family status, occupational class | All-cause mortality | Blue-collar women vs. other womenA | As compared with blue-collar women, the all-cause mortality rate is lower among white-collar women (HR = 0.83, 95% CI 0.73–0.93). | All insured embers of the Gmünder Ersatzkasse (GEK) compulsory health insurance fund who retired between the ages of 50 and 65 | High-Income | (Brockmann et al., 2009) | |
| Longitudinal | Work ability in midlife | All-cause mortality | Blue-collar women vs. other women | As compared with white-collar women in excellent health, the rate of all-cause mortality was increased among blue-collar women with excellent health (HR = 1.30, 95% CI 0.97–1.74), moderate health (HR = 1.15, 95% CI 0.89–1.46), and poor health (HR = 1.44, 95% CI 1.10–1.89). | Finnish Longitudinal Study on Municipal Employees (FLAME) | High-Income | (von Bonsdorff et al., 2011) | |
| Longitudinal | Area-remoteness index of Australia, index of relative socio-economic disadvantage (IRSD), time (years after diagnosis) and time squared, age, indigenous status, occupational class, marital status, cancer stage | Breast Cancer Mortality | Blue-collar women vs. other womenC | The odds of breast cancer mortality were increased among blue-collar women as compared with professional women (OR = 1.27, 95% CI 1.08–1.51). | Queensland Cancer Registry (QCR) | High-Income | (Dasgupta et al., 2012) | |
| Longitudinal | Job strain | All-cause mortality | Exposure-outcome among blue-collar women | Among blue-collar women the odds of all-cause mortality were decreased for active work versus low strain work (OR = 0.77, 95% 0.56–1.07) and increased for passive work versus low strain work (OR = 1.17, 95% CI 0.89–1.55). There was no difference in the odds of all-cause mortality among blue-collar women engaged in high- versus low-strain work (OR = 0.97, 95% CI 0.73–1.29). | Finnish Longitudinal Study on Municipal Employees (FLAME) | High-Income | (von Bonsdorff et al., 2012) | |
| Longitudinal | Occupational class, occupational position (manager vs. non-manager) | All-cause mortality; CVD mortality; Cancer mortality | Blue-collar women vs. other women | The rates of all-cause mortality among blue-collar women were decreased as compared with white collar women (HR = 0.73, 95% CI 0.43–1.25), the rates of cardiovascular mortality were decreased among blue-collar women as compared with white-collar women (HR = 0.78, 95% CI 0.22–2.81) and the rates of cancer mortality were decreased among blue-collar women as compared with white-collar women (HR = 0.76, 95% CI 0.37–1.56). | The Jichi Medical School Cohort Study (JMS) | High-Income | (Hirokawa et al., 2013) | |
| Longitudinal | Age; marital status; occupational class; SOC (comprehensibility, manageability, meaningfulness); psychiatric diagnoses (organic disorder, psychotic, dementia, alcohol use disorder) | All-cause mortality | Blue-collar women vs. other womenA | The rate of all-cause mortality among blue-collar women was 1.63 times the rate of all-cause mortality among white-collar women (HR = 1.63, 95% CI 1.06–2.52). | The Lundby Study Cohort | High-Income | (Mattisson et al., 2014) | |
| Longitudinal | Metalworking fluid | Ischaemic Heart Disease Mortality | Exposure-outcome among blue-collar women | Among white female auto-workers, the risk of ischemic heart disease mortality was increased among those with cumulative exposure to soluble metalworking fluid of more than 3.44 mg/m3-year (HR = 1.89, 95% CI 0.74–4.86); between 1.81 and 3.44 mg/m3-year (HR = 2.44, 95% CI 0.96–6.22); between 0.77–1.80 mg/m3-year (HR = 2.40, 95% CI 0.97–5.9); and between 0–0.76 mg/m3-year (HR = 1.84, 95% CI 0.76–4.50) as compared with white female autoworkers with no exposure to soluble metalworking fluids. Risk was increased among those with cumulative exposure to synthetic metalworking fluid greater than 0.65 mg/m3-year (HR = 1.37, 95% CI 0.82–2.29) and between 0–0.65 mg/m3-year (HR = 1.29, 95% CI 0.80–2.07) as compared with white female autoworkers with no exposure to synthetic metalworking fluids. | Female hourly automobile production workers from three large manufacturing plants in Michigan | High-Income | (Costello et al., 2014) | |
| Case-Control | Occupational class, current smoking, African American | Sudden Cardiac Death | Blue-collar women vs. other women | Odds of sudden cardiac among white-collar women were 1.49 times the odds of sudden cardiac death among blue-collar women (OR = 1.49, 95% CI 0.81–2.75). | Oregon Sudden Unexpected Death Study | High-Income | (Zhang et al., 2015) | |
| Musculoskeletal | Longitudinal | Physical Workload | Occupation and osteoarthrosis of the hip and knee | Exposure-outcome among blue-collar women | Among blue-collar women born in 1905–1924, the risks were increased for hospitalization due to osteoarthrosis of the hip (RR = 1.6, 95% CI 0.9–3.1) and knee (RR = 1.4, 95% CI 0.6–3.2) among those with high versus low exposure occupations. Among blue-collar women born in 1925–1945, the risk was increased for hospitalization for osteoarthrosis of the hip (RR = 1.1, 95% CI 0.9–1.5) and knee (RR = 1.9, 95% CI 1.3–2.9) among those with high versus low exposure occupations. | Residents of one of 13 Swedish counties who reported the same occupation in the 1960 and 1970 census. | High-Income | (Vingård et al., 1991) |
| Cross-Sectional | Previous pain symptoms, muscle tension, age, psychological problems, working hours, family relationship | Pain symptoms of the head, neck, shoulders/upper arms, lower arms, low back, hip, thighs, knee and ankles | Exposure-outcome among blue-collar women | The main individual risk factor identified was experience of previous similar symptoms in the same body region. Other individual factors were signs of psychological problems and tendency of muscle tension. | Female production workers employed by a single Norwegian clothing manufacturing companies. | High-Income | (Westgaard and Jansen, 1992) | |
| Cross-Sectional | Positive affectivity, negative affectivity, age, sex, education, tenure, alcohol involvement, autonomy, routinization, job hazards, role ambiguity, role conflict, work overload, supervisory support, co-worker support | Occupational injury | Male vs. female blue-collar workersB | Blue-collar men were less likely to experience occupational injury than blue-collar women (ß = -0.29, p < 0.05). | Blue-collar unionized employees at a single manufacturing plant in Victoria, Australia | High-Income | (Iverson and Erwin, 1997) | |
| Longitudinal | High mental load at work, monotonous work, overtime work, dissatisfactory leisure time, high mental load at work + dissatisfactory leisure time | Disorders of the neck; disorders of the shoulder | Exposure-outcome among blue-collar women | Among blue-collar women, reported medical treatment or consultation for disorders of the shoulder were associated with high mental load at work (PR = 1.2, 95% CI 0.3–4.4), overtime work, (PR = 2.7, 95% CI 1.1–6.9), and high mental load at work with unsatisfactory leisure time (PR = 1.7, 95% CI 0.6–4.8) relative to potential risk factors in 1969. Unsatisfactory leisure time was associated with decreased reported medical treatment or consultation for disorders of the shoulder (PR = 0.7, 95% CI 0.3–1.7). | The REBUS Study | High-Income | (Fredriksson et al., 1999) | |
| Longitudinal | Duration of exposure, age, smoking, BMI, living alone with children, job strain, social support, stress | Shoulder Disorders | Exposure-outcome among blue-collar women | Among female sewing machine operators, the risk of developing a shoulder disorder for those wit high versus low shoulder support (RR = 3.72, 95% CI 1.22–11.30), increased neck-shoulder pain scores (RR = 1.02, 95% CI 1.00–1.05), smoking (RR = 3.93, 95% CI 1.33–11.58), and living alone with children (RR 3.58, 95% CI 0.87–14.68). | Danish Project on Research and Intervention in Monotonous Work (PRIM Study) | High-Income | (Kaergaard and Andersen, 2000) | |
| Longitudinal | Job demand, job control, supervisor support, coworker support, age, work duration | Work injury | Exposure-outcome among blue-collar women | The odds of work injury among blue-collar were increased among those with high job demand (OR = 1.30, SE = 0.08331). Odds of work injury were decreased among those with high job control (OR = 0.94, SE = 0.03650) and high coworker support (OR = 0.71, SE = 0.18003). There was no association between work injury and supervisor support (OR = 1.02, SE = 0.12049), age (OR = 1.02, SE = 0.04177), and working duration (OR = 1.03, SE = 0.05987). | Employees of a small aerosol products manufacturing plant in Japan | High-Income | (Murata et al., 2000) | |
| Case-Control | Stature; body weight; sitting with neck bent forward; arms, hands at/above shoulder height; decision latitude index, precision movements required; fixed working postures; uncomfortable work postures; civil status | Neck and shoulder problems | Exposure-outcome among blue-collar women | Increased odds of neck and shoulder problems among blue-collar women were associated with the number of hours per day spent with the arms or hands at or above shoulder height (OR = 1.087, 95% CI 1.031–1.365), decision latitude index (OR = 1.175, 95% CI 1.040 1.327), required precision movement (OR = 1.714, 95% CI 0.589–4.989), fixed work postures (OR = 1.947, 95% CI 0.796–4.766), uncomfortable work postures (OR = 1.700, 95% CI 0.697–4.149), and partnership with children under 13 years (OR = 3.357, 95% CI 0.996–11.31), partnership with no children under 13 years (OR = 3.473, 95% CI 1.019–11.84), and being single with children under 13 years (OR = 4.278, 95% CI 0.823–22.25). Decreased odds of neck and shoulder problems were associated with increased stature (OR = 0.784, 95% CI 0.563–1.092). Body weight (OR = 0.991, 95% CI 0.817–1.202) and hours per day spent with arms or hands at or above shoulder height (OR = 1.039, 95% CI 0.879–1.229) were not associated with neck and shoulder problems. | Women employed at one of 26 companies in the metal and food industries from three Swedish counties. | High-Income | (Björkstén et al., 2001) | |
| Longitudinal | Occupational class at age 30; parents' occupational class, school grade, smoking, and physical activity at age 16; being single at age 21; job control and physical working condition at age 30. | Musculoskeletal Disorders | Blue-collar women vs. other women | The odds of a musculoskeletal disorder at age 21 among blue-collar women were 1.43 times the odds of a musculoskeletal disorder at age 21 among white-collar women (OR = 1.43, 95% CI 0.97–2.11). | Follow-up of a baseline survey of 16 year old pupils in their last year of compulsory schooling in the industrial Northern Swedish town of Lulea. | High-Income | (Khatun et al., 2004) | |
| Cross-Sectional | Years of formal education, occupational class | Hospitalization because of back disorders | Blue-collar women vs. other women | The risk of hospitalization because of back disorders were increased among blue-collar women age 25-34 (RR = 1.6, 95% CI 1.2–2.2), age 35-44 (RR = 1.4, 95% CI 1.2–1.6), age 45-54 (RR = 1.3, 95% CI 1.1–1.4), and age 55–64 (RR = 1.3, 95% CI 1.1–1.5) as compared to their white-collar counterparts. | Population of Finland | High-Income | (Kaila-Kangas et al., 2006) | |
| Cross-Sectional | Gender, age, smoking, insomnia symptoms, job type, industrial sector, work experience | Occupational injuries | Blue-collar women vs. other womenC | Odds of occupational injuries among female manufacturers were 4.26 times the odds of occupational injury among female managers and clerical workers (OR = 4.26, 95% CI 2.23-8.13). | Workers of small-scale manufacturing factories (those with less than 50 workers) in Yashio city, Saitama prefecture, Japan. | High-Income | (Nakata et al., 2006) | |
| Longitudinal | Sex, age category, education, time since hire, time in current job, physical demand, race, plant type | Traumatic Injury; OSHA Recordable Injuries | Male vs. female blue-collar workersC | The odds of traumatic injury among blue-collar women were increased as compared with blue-collar men (OR = 1.57, 95% CI 1.33–1.85). The odds of OSHA recordable injuries among blue-collar women were increased as compared with blue-collar men (OR = 1.72, 95% CI 1.34–2.20). | The American Manufacturing Cohort Study (AMC) | High-Income | (Pollack et al., 2007) | |
| Cross-Sectional | Gender, age group, ethnicity, education level, marital status, living with children, supporting families outside of household, BMI, physical activity, smoking behavior, physician diagnosed systemic illness, years of employment in garment industry | Neck, Shoulder, and Distal Upper Extremity Pain | Male vs. female blue-collar workersC | The odds of neck and shoulder pain were decreased among blue-collar men as compared with blue-collar women (OR = 0.5, 95% CI 0.28–0.90). The odds of distal upper extremity pain among blue-collar men were decreased as compared with blue-collar women (OR = 0.55, 95% CI 0.28–1.09). | Sewing machine operators working at one of 13 garment shops in Los Angeles selected using convenience sampling. | High-Income | (Wang et al., 2007) | |
| Cross-Sectional | Occupational class | Work Injury | Blue-collar women vs. other women | Odds of poor self-rated health were increased among blue-collar women as compared to female professionals managers (OR = 2.02, 95% CI 1.57–2.61). Among blue-collar women, odds of long-term sickness absence (OR = 2.45, 95% CI 1.90–3.15) and work injury (OR = 5.63, 95% CI 3.13-10.16) were also increased as compared to female managers and professionals. | SUMER Study | High-Income | (Niedhammer et al., 2008) | |
| Longitudinal | Sex | Acute Injuries; MSD-Related Injuries | Male vs. female blue-collar workers | The odds of acute injuries among female smelters were increased as compared with male smelters (OR = 1.201, 95% CI 1.151–1.295). The odds were also increased for total recordable acute injuries (OR = 1.158, 95% CI 1.012–1.326) lost-work-day acute injuries (OR = 1.097, 95% CI 0.512–2.348); MSD-related injuries (OR = 1.119, 95% CI 1.097–1.311); total recordable MSD-related injuries (OR = 1.334, 95% CI 1.174–1.515) and lost-work-day MSD-related injuries (OR = 1.285, 95% CI 0.783–2.109) among female smelters as compared with male smelters. | The American Manufacturing Cohort Study (AMC) | High-Income | (Taiwo et al., 2008) | |
| Longitudinal | Occupational class | Carpal tunnel syndrome | Blue-collar women vs. other women | The risk of carpal tunnel syndrome was increased among blue-collar women as compared with non-working person (RR = 3.0, 95% CI 2.5–3.6). Risk was increased among women in agriculture (RR = 2.5, 95% CI 2.0–3.2), construction (RR = 4.7, 95% CI 1.0–13.0) and manufacturing (RR = 2.1, 95% CI 1.7–2.5) as compared to non-working women. | Adult residents of the Maine and Loire (M&L) region in west-central France. | High-Income | (Roquelaure et al., 2008) | |
| Longitudinal | Depressive symptoms | Occupational injury | Exposure-outcome among blue-collar women | Among blue-collar women, risk of occupational injury was increased among those with depressive symptoms (RR = 2.04, 95% CI 1.41–2.95). | Workers at 35 small- or medium-sized manufacturing companies in the Incheon area of South Korea in the Group Occupational Health Service at Inha University Hospital. | High-Income | (Kim et al., 2009) | |
| Case-Control | Occupational class, BMI, height, parity | Surgically treated CTS | Blue-collar women vs. other women | The odds of surgically-treated carpal tunnel syndrome among blue-collar women were increased as compared with white-collar women (OR = 9.1, 95% CI 4.8–17.4). | Cases of surgically-treated CTS and controls selected among blue- and white-collar workers, other workers, and housewives living in the Region of Tuscany, Italy. | High-Income | (Mattioli et al., 2009) | |
| Longitudinal | Occupational class, industrial sector | Carpal tunnel syndrome | Blue-collar women vs. other women | The risk of carpal tunnel syndrome (CTS) among blue-collar women was increased as compared with female farmers (RR = 2.9, 95% CI 2.5–3.4). The risk of CTS among women in construction was increased as compared with women in manufacturing (RR = 2.0, 95% CI 1.7–2.4). | Adult residents of the Maine and Loire (M&L) region in west-central France. | High-Income | (Roquelaure et al., 2009) | |
| Cross-Sectional | Pain severity, weaver's selection of remedial measures, weaver's perception to the cause of pain, age, working hours, marital status, job tenure, literacy, psychosocial variables | Musculoskeletal Disorders | Exposure-outcome among blue-collar women | The odds of musculoskeletal disorders were increased among female handloom workers older than 25 (OR = 2.9, 95% CI 1.2–7.4), with more than 10 years of tenure (OR = 2.1, 95% CI 1.1–4.6), with mental overload (OR = 3.7, 95% CI 1.0–13.8) and among those who were literate (OR = 2.2, 95% CI 1.2–3.9). | Weavers working at handloom or powerloom units in the Ahmedabad district of India. | Lower-Middle-Income | (Nag et al., 2010) | |
| Cross-Sectional | Work hours per day, overtime, salary; exposure to chemicals and toxic vapors/substances, exposure to vibration and dangerous equipment, high temperatures, physical dangers/unhealthy conditions at work, poor air/ventilation, crowded workstations and uncomfortable working postures, having a safe work environment, adequate protective clothing and equipment, adequate work-related welfare facilities; psychological job demands/workload, work is interesting, company informs about its achievements, on-site training courses, resources/help and equipment availability, supervisor-related, discrimination - intimidation or threats; household income inadequacy, social and family working hours fit, adequate sanitary living conditions/potable water, children under 18. | Musculoskeletal Pain | Exposure-outcome among blue-collar women | Multiple associations reported between various measures of working hours and salary; safety and health; tasks and organizational aspects; extra-organizational factors, and musculoskeletal pain among blue-collar women. | Blue-collar workers from 12 manufacturing companies in Lima, Perú. | Upper-Middle-Income | (Brunette et al., 2011) | |
| Cross-Sectional | Age, marital status, type of carpet-weaving loom, weaving style, stature, work hours, work experience | Elbow pain; Forearm pain; Wrist pain | Exposure-outcome among blue-collar women | Among female carpet-weavers, type of carpet weaving loom (fixed vs. moving vertical) was significantly associated with shoulder pain (OR = 3.422, 95% CI 2.026-6.124); elbow pain (OR = 2.439, 95% CI 1.565-3.801); forearm pain (OR = 2.621, 95% CI 1.715-4.006); and wrist pain (OR = 2.299, 95% CI 1.539-3.433). | Stratified random sample of carpet weavers in urban and rural regions within the Kerman, Esfahan, and East Azerbaijan provinces. | Upper-Middle-Income | (Motamedzade and Moghimbeigi, 2012) | |
| Cross-Sectional | Age, smoking, company's gender equality index, employment hours, occupational class, high engagement in domestic work, number of children < 18 years, work demands, work control, work support, constrained physical heavy work load, work-home imbalance | Neck and shoulder disorders; low back disorders | Blue-collar women vs. other womenA | There was no evidence of a difference between blue- and white-collar women's risk for neck and shoulder disorders (OR = 1.0, 95% CI = 0.5–1.7) | Employees at 9 companies in computer science and 12 companies in the food industry in Sweden. | High-Income | (Ahlgren et al., 2012) | |
| Longitudinal | Occupation | Surgically treated osteoarthritis in the hip or knee | Blue-collar women vs. other women | Among female construction workers, the rate for surgically-treated osteoarthritis of the hip as compared with female office workers (HR = 1.21, 95% CI 1.03–1.43), and the rates of surgically-treated osteoarthritis of the knee were increased as compared with female office workers (HR = 1.37, 95% CI 1.14–1.64). | Danish residents employed in one of five occupational groups: floor- and bricklayers, construction workers, farmers, healthcare assistants, and office workers. | High-Income | (Andersen et al., 2012) | |
| Cross-Sectional | Age, BMI, job type, education, time in industry, monthly income | Musculoskeletal complaints of the back, knee, and upper limb | Blue-collar women vs. other womenC | As compared with female sewing machine operators, the odds were decreased for back complaints (OR = 0.62, 95% CI 0.28–1.39) and knee complaints (OR = 0.70, 95% CI 0.21–2.34), and increased for upper limb complaints (OR = 1.28, 95% CI 0.36–4.50) as compared with female quality control assistants. | Female garment workers employed in factories in the Koggala FTZ in Sri Lanka. | Lower-Middle-Income | (Lombardo et al., 2012) | |
| Longitudinal | Gender, manager type, location, year, race/ethnicity, age when started in department, tenure when started in department, department is high demand | First-aid injury, reportable injury | Male vs. female blue-collar workers | The rates for first acute injury were increased among blue-collar women as compared with blue-collar men (HR = 1.21, 95% CI 1.06, 1.39). | The American Manufacturing Cohort Study (AMC) | High-Income | (Kubo et al., 2013) | |
| Longitudinal | Age, sex, time in the union, predominant work | Hand and Finger Injuries | Male vs. female blue-collar workersC | Among those with or paid lost time, the rates of hand and finger injuries among blue-collar women is increased as compared with blue-collar men (RR = 1.2, 95% CI 1.0–1.5). Among those with paid lost time, the rates of hand and finger injuries is also increased among blue-collar women as compared with blue-collar men (RR = 1.8, 95% CI 1.1–3.0). | Union carpenters working in Washington State. | High-Income | (Lipscomb et al., 2013) | |
| Cross-Sectional | Work experience, prolonged working hours, awkward posture, perceived high job demand | Musculoskeletal Disorders | Exposure-outcome among blue-collar women | Among blue-collar women, the odds of musculoskeletal disorders were increased among those with five or more years of work experience (OR = 1.79, 95% CI 0.72–4.44), with prolonged working yours (OR = 7.63, 95% CI 2.06, 28.31), with awkward work postures (OR = 43.79, 95% CI 17.09–112.20), and perceived high job demand (OR = 1.16, 95% CI 0.34–3.98). | Randomly sampled female workers using hand-operated rebar benders in a northeast province of Thailand. | Upper-Middle-Income | (Hanklang et al., 2014) | |
| Longitudinal | Gender | Injury | Male vs. female blue-collar workers | The odds of injury among blue-collar women were increased as compared with blue-collar men (OR = 1.58, 95% CI 1.48–1.67). | The American Manufacturing Cohort Study (AMC) | High-Income | (Tessier-Sherman et al., 2014) | |
| Longitudinal | Physical demand, exposure to heat, psychological demand, job control, race/ethnicity, job tenure, age, sex | First aid injury and first aid MSD; Serious injury and serious MSD; First aid MSD only; Serious MSD only | Male vs. female blue-collar workersB | Among blue-collar women, the risk was increased for first aid injury (RR = 1.51, 95% CI 1.31–1.73), serious injury and serious musculoskeletal disorder (RR = 1.55, 95% CI 1.23–1.93), first aid musculoskeletal disorder only (RR = 1.26, 95% CI 1.00–1.59) and serious musculoskeletal disorder only (RR = 1.75, 95% CI 1.25–2.46) as compared with blue-collar men. | The American Manufacturing Cohort Study (AMC) | High-Income | (Cantley et al., 2016) | |
| Cross-Sectional | Total sitting time per day | Neck and shoulder pain intensity | Exposure-outcome among blue-collar women | Among blue-collar women, the odds of NSP were increased for high total sitting time vs. moderate total sitting time (OR = 1.19, 95% CI 0.31–4.15) and the decreased for low total sitting time vs. moderate total sitting time (OR = 0.80, 95% CI 0.21–2.99). The odds for NSP were increased for high work sitting vs. moderate work sitting (OR = 1.17, 95% CI 0.32–4.33) and the odds for NSP were the same low work sitting vs. moderate work sitting (OR = 1.01, 95% CI 0.28–3.59). The odds for NSP for were the same high leisure sitting vs. moderate work sitting (OR = 1.02, 95% CI 0.28–3.74) and were decreased for NSP for low leisure sitting vs. moderate leisure sitting (OR = 0.86, 95% CI 0.25–3.02). | New method for Objective Measurements of physical Activity in Daily living (NOMAD) Study | High-Income | (Hallman et al., 2015) | |
| Other | Cross-Sectional | Age, current smoker, moderate/heavy alcohol, sever obesity, chronic disease, clean room, current chemical exposure | Memory loss, headaches, head exploding light-headed, room spinning, tremor, coordination, numbness, cold hands/feet, appetite change, funny taste, swallowing, palpitations, weakness/fatigue, rashes, chronic cough, abdominal pain | Exposure-outcome among blue-collar women | Among blue-collar women with current chemical exposure, the odds were increased for memory loss (OR = 1.23, p > 0.05), headaches (OR = `.40, p > 0.05), light-headedness (OR = 1.12, p > 0.05), room spinning (OR = 1.14, p > 0.05), tremor (OR = 1.07, p > 0.05), coordination (OR = 1.43, p > 0.05), numbness (OR = 1.16, p > 0.05), and cold hands and feet (OR = 1.42, p > 0.05) as compared to blue-collar women without current chemical exposure. Odds of symptoms of "head exploding" were decreased among those with current chemical exposure (OR = 0.93, p > 0.05). | Workers at microelectronics plant represented by IBEW in Pennsylvania | High-Income | (Parkinson et al., 1990) |
| Cross-Sectional | Age, education, marriage, income, smoking, obesity, major illness, life events, solvent exposure, job demands, job conflict, co-worker support, supervisor support, friend/relative support | Headache, lightheaded, vertigo, weakness, memory loss, abdominal pain, rash, multiple symptoms | Exposure-outcome among blue-collar women | Among blue-collar women with current solvent exposure, the odds were increased for depression (ß = 0.19, p < 0.05), lightheadedness (ß = 0.29, p < 0.01), vertigo (ß = 0.39, p < 0.01), weakness (ß = 0.33, p < 0.005), memory loss ( ß = 0.33, p < 0.005), abdominal pain (ß = 0.54, p < 0.005), rash (ß = 0.20, p = 0.07), and multiple symptoms (ß = 0.23, p < 0.01). | Workers at semiconductor plant represented by IBEW in the mid-Eastern US | High-Income | (Bromet et al., 1992) | |
| Cross-Sectional | Occupation | Headaches that match cervical origin pain patterns | Blue-collar women vs. other women | As compared with blue-collar women, the odds of cervical origin headache were increased among female managers and professionals (OR = 2.94, 95% CI 1.3–6.6), and female clerical workers (OR = 1.37, 95% CI 0.6–3.2). | Residents of two adjoining Tasmanian municipalities randomly sampled from electoral rolls. | High-Income | (Grimmer, 1993) | |
| Cross-Sectional | Age, education, sex, alcohol, solvent exposure index | Continuous performance test; pattern comparison (latencies); pattern memory (latencies) | Male vs. female blue-collar workersB | Continuous performance test scores were decreased among blue-collar men as compared with blue-collar women (ß =–0.019, SE = 0.014), and pattern comparison (ß = 0.031, SE = 0.033) and pattern memory (ß = 0.020, SE = 0.029) were increased among blue-collar men as compared with blue-collar women. | Workers in six paint manufacturing plants in northern Taiwan | High-Income | (Tsai et al., 1997) | |
| Cross-Sectional | Overcompensating at work, job certainty, sexual harassment and discrimination | Insomnia, nausea, headaches | Exposure-outcome among blue-collar women | Among female construction workers, the odds of insomnia were increased among those who overcompensated at work (OR = 1.41, 95% CI 1.14–1.74) and decreased among those with job certainty (OR = 0.85, 95% CI 0.771–0.942). The odds of nausea were increased among those experiencing sexual harassment and discrimination (OR = 1.33, 95% CI 1.11–1.60). The odds of headache were increased among those experiencing sexual harassment and discrimination (OR = 1.21, 95% CI 1.02–1.43). | Female members of the Laborers' International Union of North America (LIUNA) in Seattle, Washington and Portland, Oregon. | High-Income | (Goldenhar et al., 1998) | |
| Cross-Sectional | Age, area of factory | Hearing impairment | Exposure-outcome among blue-collar women | Audiometric tests performed on 69 female workers from the weaving section revealed that workers with more than 10 years of noise exposure had the worst hearing threshold levels at 1,000 and 4,000 Hz. | Female workers from the weaving section of a textile factory in Hanoi, Vietnam | Lower-Middle-Income | (Nguyen et al., 1998) | |
| Longitudinal | Gender, workload score | Fatigue spillover | Male vs. female blue-collar workers | Fatigue spillover was less frequent among female bus-drivers as compared with male bus drivers (ß = - 0.05, p > 0.05) and there was a negative interaction between gender and workload score (ß = - 0.24, p > 0.05). | Full-time, employed urban bus drivers working at the same terminal in central Stockholm, Sweden. | High-Income | (Rydstedt et al., 1998) | |
| Cross-Sectional | Magnetic field exposure, smoking, age, light at night, duration of sleep, depression, miscarriages | Nocturnal 6-hydroxymelatonin sulfate excretion | Blue-collar women vs. other women | Normalized 6-OHMS secretion was decreased among blue-collar women exposed to magnetic fields (ß = -4.06, SE = 1.51) as compared to office workers not exposed to magnetic fields. | Female workers from a garment factory in Kuopio, Finland and a reference group of employees of a governmental organization and university staff members. | High-Income | (Juutilainen et al., 2000) | |
| Cross-Sectional | Age, BMI, Illness, ergonomic stress level, environmental annoyance, perceived control | Serum Uric Acid | Exposure-outcome among blue-collar women | Among blue-collar women, serum urine acid levels were negatively associated with ergonomic stress levels (ß = -0.18, SE = 0.10), environmental annoyance (ß = - 0.05, SE = 0.03), and perceived control (ß = - 0.03, SE = 0.02). | Cardiovascular Occupational Risk Factors Determination in Israel Study (CORDIS) | High-Income | (Shirom et al., 2000) | |
| Cross-Sectional | Occupational class | Long-term condition, short-term condition | Blue-collar women vs. other women | As compared with professional women, the odds of long-term conditions were decreased among blue-collar women (OR = 0.80, 95% CI 0.62–1.04) and the odds of short-term conditions were decreased among blue-collar women (OR = 0.89, 95% CI 0.64–1.24). | Campbell National Health Monitor | High-Income | (Korda et al., 2002) | |
| Cross-Sectional | Noise level | Tooth abrasion | Exposure-outcome among blue-collar women | Among blue-collar women, the odds of tooth abrasion were increased among those exposed to intense noise as compared with those in the preparation department (OR = 3.74, 95% CI 1.42–7.85). | Workers at a large wool-producing company in Montenegro, Serbia. | Upper-Middle-Income | (Kovacevic and Belojevic, 2006) | |
| Longitudinal | Technical job, natural menopause, smoking > 10 cigarettes per day, technical and community education, education, 1-2 pregnancies, age category | Blood Lead Levels, Calcaneus Bone Lead Content | Blue-collar women vs. other women | Blood lead levels among women in technical jobs (for example, miners) were higher than blood lead levels among women in administrative support or sales (ß = 0.242, 95% CI = -0.115 - 0.599). | Bunker Hill Study | High-Income | (Potula and Kaye, 2006) | |
| Cross-Sectional | Age, gender, annual income level, marital status | Fibromyalgia | Male vs. female blue-collar workersC | The odds of fibromyalgia were increased among blue-collar women as compared with blue-collar men (OR = 15.01, 95% CI 1.90–118.50). | Female workers at four textile factories in Denizli, Turkey. | Upper-Middle-Income | (Cobankara et al., 2011) | |
| Cross-Sectional | Age, sex, race, marital status, education, pain, number of medical comorbidities, depressive symptoms, alcohol problems, smoking, physical activity obesity | Sleep Quality | Male vs. female blue-collar workersC | Sleep score quality was decreased among blue-collar women as compared with blue-collar men (ß = - 0.100, p = 0.041). | A convenience sample of operating engineers coming to either an apprentice certification or Hazardous Materials (Hazmat) refresher course in Michigan. | High-Income | (Choi et al., 2013) | |
| Cross-Sectional | Former rotating shift work, recent rotating shift work, persistent rotating shift work; academic educational level; married/cohabitating, child-rearing responsibility; hepatitis B carrier, metabolic syndrome, anemia | High need for recovery after work | Exposure-outcome among blue-collar women | Among blue-collar women, work-related fatigue was decreased among those currently married or cohabiting (OR = 0.5, 95% CI 0.2–0.9), and increased among those with child-rearing responsibilities (OR = 1.9, 95% CI 1.0–3.7). | Workers at a single semiconductor manufacturing company receiving compulsory periodic health checkups. | High-Income | (Lin et al., 2015) | |
| Reproductive & Sexual Health | Cross-Sectional | Occupation, age, smoking, parity, years of education | Birthweight of most recent birth | Blue-collar women vs. other women | As compared with women who were service workers during pregnancy, lower birth weight infants were born to women who were garment workers (ß = - 653, 95% CI - 1,041 to 265) or electronics workers (ß = - 337, 95% CI - 682 to 9). | Women in Tijuana working as electronic maquiladora workers; garment maquiladora workers; service workers; and those with no labor force history | Upper-Middle-Income | (Eskenazi et al., 1993) |
| Cross-Sectional | Occupation, education, place of residence | Natural Menopause | Blue-collar women vs. other women | As compared with lower white-collar workers, the odds of natural menopause were increased among blue-collar factory workers (OR = 1.17, 95% CI 0.96–1.42). | Adult women randomly selected form the Finnish Population Register | High-Income | (Luoto et al., 1994) | |
| Cross-Sectional | Race, age, occupational class, smoking, contraception, coitarche, partners last year, total partners, anal intercourse, sexual intercourse with partner from abroad, no non-regular partners, diagnosis with other STI, past history of STI, high vaginal swab | HSV-2 Infection | Blue-collar women vs. other women | Odds of HSV-2 infection among blue-collar women were increased as compared with white-collar women (OR = 4.14, 95% CI 1.33–12.92). | Women newly attending a genitourinary clinic in London | High-Income | (Evans et al., 2003) | |
| Longitudinal | Occupational class | Prematurity, low birth weight, SGA, LGA, perinatal mortality, birth weight | Blue-collar women vs. other women | As compared with upper white-collar workers, the odds of prematurity were increased (OR = 1.14, 95% CI 1.07–1.22), the odds of low birth weight were increased (OR = 1.25, 95% CI 1.16–1.34), the odds of SGA were increased (OR = 1.44, 95% CI 1.31–1.58), the odds of LGA were increased (OR = 1.24, 95% CI 1.14–1.36), and the odds of perinatal mortality were increased (OR = 1.44, 95% CI 1.13–1.83) among blue-collar women between 2003 and 2006. | Finnish Medical Birth Register | High-Income | (Gissler et al., 2009) | |
| Longitudinal | Rubber cohort membership | Birth weight | Blue-collar women vs. other women | Among women who were rubber workers during pregnancy, the odds were increased for having a girl (OR = 1.15, 95% CI 1.02–1.13) and having a small-for-gestational age child (OR = 2.15, 95% CI 1.45–3.18) as compared with food workers. | Female workers at 12 Swedish rubber production facilities and female members of the Food Worker's Union. | High-Income | (Jakobsson and Mikoczy, 2009) | |
| Quasi-Experimental | Parental leave | Fertility | Exposure-outcome among blue-collar women | Among blue-collar women, the effect of the 1990 reform was an increase in the probability of having an additional birth in 0–36 months (ß = 0.048, SE = 0.016), in 0–120 months (ß = 0.036, SE = 0.016), and 17–28 months (ß = 0.078, SE = 0.013). The probability of having an additional birth was decreased in 0 - 16 months (ß = -0.031, SE = 0.009) and 29–120 months (ß = -0.008, SE = 0.016). | Women giving birth to their first child recorded in the Austrian Social Security Database. | High-Income | (Lalive and Zweimüller, 2009) | |
| Cross-Sectional | Age, education, year of conception, employment area, medical conditions during pregnancy, smoked during pregnancy, drank alcohol during pregnancy | Adverse Pregnancy Outcomes | Blue-collar women vs. other women | The odds of congenital anomalies among female laboratory workers in an aluminum smelter were increased during employment as compared with women who gave birth prior to employment (OR = 7.89, 95% CI 1.16–53.77). | The American Manufacturing Cohort Study (AMC) | High-Income | (Sakr et al., 2010) | |
| Cross-Sectional | Age, marital status, education, age at first sexual exposure, sources of knowledge on HIV/AIDS | Use of condoms; sex with multiple partners; drug abuse | Exposure-outcome among blue-collar women | Among female garment workers, increased knowledge score was associated with increased odds of using a condom at last intercourse (OR = 1.482, p = 0.10), decreased odds of sex with multiple partners (OR = 0.832, p = 0.036), and decreased odds of drug abuse (OR = 0.766, p = 0.034). | Female workers randomly selected from five garment factories in Dhaka, Bangladesh | Lower-Middle-Income | (Sayem, 2010) | |
| Cross-Sectional | Age, education, monthly income, occupation, marital status, health status, sexual norms and other behaviors, rural residency, communist party membership | Lifetime multiple sexual partnerships | Blue-collar women vs. other womenC | As compared with women in other occupations, the odds of having multiple sexual partners were increased among women in manual labor (OR = 3.347, 95% CI 1.069–10.476). | China Health and Family Life Survey (CHFLS) of 2000 and 2006 Survey of Chinese People's Sexuality | Upper-Middle-Income | (Yingying et al., 2011) | |
| Quasi-Experimental | Displacement and firm closure | Fertility | Exposure-outcome among blue-collar women | There were minimal effects of firm closure on fertility among blue-collar women for births in the three years following firm closure (ß = 0.002, SE = 0.016) and in the six years following firm closure (ß = - 0.013, SE = 0.023). | Women in Austria affected by a firm closure compared to a control group of nondisplaced women. | High-Income | (Del Bono et al., 2012) | |
| Cross-Sectional | Age, gender, nationality, marital status, level of education, level of knowledge, level of attitude | Use of condom in last sexual intercourse | Male vs. female blue-collar workersC | As compared with blue-collar men, the odds of using a condom during last sexual intercourse were increased among blue-collar women (OR = 8.790, 95% CI 2.009–38.467). | Workers at eight different construction Sites in the Kathmandu Valley of Nepal. | Low-Income | (Pant et al., 2013) | |
| Cross-Sectional | Maternal age, birth weight, male fetal sex, smoking status, occupational class, induction, preeclampsia, gestational diabetes, maternal diabetes mellitus, fear of childbirth, placental abruption, placenta previa, in vitro fertilization, prior terminations, prior miscarriages, prior caesarean section, time period | Planned Caesarian Section; Non-Planned Caesarian Section | Blue-collar women vs. other women | As compared to white-collar women, the odds of were increased for planned Caesarian section (OR = 1.11, 95% CI 1.03–1.19) and non-planned Caesarian section (OR = 1.19, 95% CI 1.13–1.25) among nulliparous blue-collar women. Among multiparous blue-collar women, the odds were also increased for planned C-section (OR = 1.14, 95% CI 1.08–1.22) and unplanned C-section (OR = 1.22, 95% CI 1.14–1.30). | Population of Finland | High-Income | (Räisänen et al., 2014) | |
| Case-Control | Occupation | Preterm birth | Blue-collar women vs. other women | As compared with women in office and administrative support occupations, the odds of preterm birth were increased among women in building and grounds cleaning (OR = 1.86, 95% CI 0.95–3.63) and among women in production occupations (OR = 1.43, 95% CI 0.83–2.45). | University of California, Los Angeles, Environment and Pregnancy Outcomes Study | High-Income | (von Ehrenstein et al., 2014) | |
| Cross-Sectional | Years Exposed to Sulfur Dioxide | Age at natural menopause; Early Menopause | Exposure-outcome among blue-collar women | Among blue-collar women, the rate of natural menopause was greatest among those with 21-25 years of sulfur dioxide exposure as compared to those with no sulfur dioxide exposure (HR = 1.290, 95% CI 1.035–1.608). The odds of early menopause were greatest among blue-collar women with 21–25 years of sulfur dioxide exposure as compared to those with no sulfur dioxide exposure (OR = 1.817, 95% CI 1.112–2.968). | Jinchuan Cohort | Upper-Middle-Income | (Wang et al., 2015) | |
| Respiratory | Cross-Sectional | Sex, age, smoking habits, atopy, familial asthma, SFEV1, airway protection | Methacholine Responsiveness | Male vs. female blue-collar workersC | The odds of methacholine responsiveness among female potroom workers was increased as compared with male potroom workers (OR = 5.7, 95% CI 2.2–14.8). | Potroom Workers at Ardal aluminum plant in Western Norway | High-Income | (Kongerud and Soyseth, 1991) |
| Cross-Sectional | Smoking, age, height, weight, mill number, dust concentration | Lung Function | Exposure-outcome among blue-collar women | Among European blue-collar women, increased dust concentration on the logarithmic scale was associated with decreased FEV1 (ß = -0.011, p > 0.05), increased FVC (ß = 0.022, p > 0.05), and a decreased FEV1:FVC (ß = -0.785, p < 0.05). | Wool textile workers at five mills in West Yorkshire, United Kingdom | High-Income | (Love et al., 1991) | |
| Cross-Sectional | Cumulative smoking, Asian ethnicity, age, gender, not working in the weaving shed, total dust (pd1) | Lung function | Male vs. female blue-collar workersC | As compared with female blue-collar workers FEV1 was increased among male blue-collar workers (ß = 4.9, SE = 1.09) and FVC was increased among male blue-collar workers (ß = 5.96, SE = 1.05). | Workers at 16 mills in the Lancashire area of the United Kingdom. | High-Income | (Raza et al., 1999) | |
| Cross-Sectional | Sex, age, BMI, duration of employment, overall mean exposure to dust, current exposure to dust | Vital capacity, FEV1 | Male vs. female blue-collar workersC | Among women, the observed mean vital capacity was 3.86 (SD 0.80) and among men the observed mean FEV1 was 3.20 (SE 0.76). | Workers at two dolomite mines with adherent production facilities located in the Bergslagen area of central Sweden. | High-Income | (Seldén et al., 2001) | |
| Case-Control | Age, smoking status, occupational class, prior lung disease | Adenocarcinoma of the lung; squamous cell and small cell carcinoma of the lung | Blue-collar women vs. other womenA | As compared with white-collar women, the odds were increased among blue-collar women for adenocarcinoma of the lung (OR = 1.85, 95% CI 1.26–2.72) and for squamous and small cell carcinoma of the lung (OR = 1.67, 95% CI 0.79–3.52). | Hospital-Based Epidemiologic Research Program at Aichi Cancer Center (HERPACC) | High-Income | (Takezaki et al., 2001) | |
| Cross-Sectional | Gender | Acute airway response | Male vs. female blue-collar workersB | The rate of acute airway response was increased among blue-collar women as compared with blue-collar men (HR = 1.51, 95% CI 1.01–2.24). | Newly hired workers at one of three cotton mills close to Istanbul, Turkey. | Upper-Middle-Income | (Bakirci et al., 2007) | |
| Longitudinal | Occupational class | Asthma | Blue-collar women vs. other women | Compared with female administrators, managers, and clerical workers, the risk of asthma was increased among all blue-collar women (RR = 1.4, 95% CI 1.2–1.6), female woodworkers (RR = 1.5, 95% CI 1.2–1.7), and other blue-collar women (RR = 1.4, 95% CI 1.2–1.6). | All residents of Finland employed in wood-processing industries. | High-Income | (Heikkilä et al., 2008) | |
| Cross-Sectional | Occupational class; job exposure to gasses, fumes, dust or smoke; left or changed job because of respiratory symptoms | Chronic Rhinosinusitis | Blue-collar women vs. other womenC | As compared with white-collar women, the odds of chronic rhinosinusitis were increased among blue-collar women (OR = 1.91. 95% CI 1.27–2.86). | Global Asthma and Allergy European Network Study (GA2LEN) | High-Income | (Thilsing et al., 2012) | |
| Longitudinal | Welding | Rhinitis | Blue-collar women vs. other women | The rate of rhinitis among female ever-welders was increased as compared with female never-welders (HR = 1.9, 95% CI 1.4–2.6). | Respiratory Health in Northern Europe (RHINE) Study | High-Income | (Storaas et al., 2015) | |
| Cross-Sectional | Manganese Cumulative Exposure Index | Pulmonary Function | Exposure-outcome among blue-collar women | No significant effect of Mn dust exposure on the pulmonary function was found in the female workers (all p>0.05). | Guangxi Manganese-Exposed Workers Healthy Cohort (GXMEWHC) | Upper-Middle-Income | (Wang et al., 2015) | |
| Self-Rated Health | Cross-Sectional | Occupational class | Good health, poor health | Blue-collar women vs. other womenC | As compared with professional women, the odds of self-reported good health were increased among blue-collar women (OR = 1.39, 95% CI 1.05–1.83). The odds of self-reported poor health were similar in blue-collar women and professional women (OR = 0.98, 95% CI 0.95–1.47). | Campbell National Health Monitor | High-Income | (Korda et al., 2002) |
| Cross-Sectional | Occupational class | Poor Self-Reported Health | Blue-collar women vs. other women | As compared with female professionals and managers, the odds of poor self-rated health were increased among blue-collar women (OR = 2.02, 95% CI 1.57–2.61). | SUMER Study | High-Income | (Niedhammer et al., 2008) | |
| Cross-Sectional | Work hours per day, overtime, salary; exposure to chemicals and toxic vapors/substances, exposure to vibration and dangerous equipment, high temperatures, physical dangers/unhealthy conditions at work, poor air/ventilation, crowded workstations and uncomfortable working postures, having a safe work environment, adequate protective clothing and equipment, adequate work-related welfare facilities; psychological job demands/workload, work is interesting, company informs about its achievements, on-site training courses, resources/help and equipment availability, supervisor-related, discrimination - intimidation or threats; household income inadequacy, social and family working hours fit, adequate sanitary living conditions/potable water, children under 18. | Health Status | Exposure-outcome among blue-collar women | As-compared with female professionals and managers, the odds of poor self-rated health were increased among blue-collar women (OR = 2.02, 95% CI 1.57–2.61). | Blue-collar workers from 12 manufacturing companies in Lima, Perú. | Upper-Middle-Income | (Brunette et al., 2011) | |
| Longitudinal | Working class parents, household appliances, and poor somatic health at age 16; time in paid work, poor cash margin, and having children at age 21; months unemployment, financial strain, physically heavy work, high demands, low control, violence, and daily smoking at day 30 | Somatic health | Blue-collar women vs. other women | As compared with white-collar women with good somatic health at age 30, the odds were decreased for poor somatic health at age 16 (OR = 0.53, 95% CI 0.23–1.24) blue-collar women with poor somatic health at age 30. As compared with white-collar women with good somatic health at age 30, the odds of daily smoking (OR = 2.72, 95% CI 1.22–6.06) were increased in blue-collar women with poor somatic health at age 30. | Northern Swedish Cohort | High-Income | (Hammarström et al., 2011) | |
| Quasi-Experimental | Living wage | Global self-rated health; comparative self-rated health | Exposure-outcome among blue-collar women | Odds of "excellent" or "much better" global self-rated health were increased among women in the intervention factory as compared with women the control factory (OR = 1.4, 95% CI 0.61–3.0). Odds of "excellent" or "much better" comparative self-rated health were increased among women in the intervention factory as compared with women the control factory (OR = 1.4, 95% CI 1.4–6.7). | Workers at intervention and control factories in the Dominican Republic | Upper-Middle-Income | (Landefeld et al., 2014) | |
| Smoking & Other Substance Use | Longitudinal | Gender, race, age, alcohol, burnout, job problems, unwind time, years driving | Smoking increase, initiation, and maintenance | Male vs. female blue-collar workersB | The odds of smoking were decreased among male bus drivers as compared with female bus drivers (OR = 0.60, 95% CI 0.33–1.09). | San Francisco MUNI Health and Safety Study | High-Income | (Cunradi et al., 2007) |
| Cross-Sectional | Job demand and control; effort and reward; over commitment; physical demand; shift work; working hours; job pressure | Current Smoking; Former Smoking | Exposure-outcome among blue-collar women | Both job strain and passive jobs were associated with smoking among blue-collar women (OR = 2.6 and 3.7, respectively), and physical demand was associated with smoking among blue-collar women (OR = 16.8). No confidence intervals reported. | A random sample of White Pages listings in the sate of Victoria in Australia. | High-Income | (Radi et al., 2007) | |
| Longitudinal | Young adult socioeconomic position (education and occupational class); family socioeconomic position; family structure; family connectedness; smoker in home; easy access to cigarettes; high school; CES-D; number of friends who smoke; smoked during adolescence | Heavy and Light-to-Moderate Smoking | Blue-collar women vs. other women | As compared to women with further education, the odds were increased among blue-collar women for light-to-moderate smoking (OR = 1.88, 95% CI 1.28–2.78), heavy smoking (OR = 3.12, 95% CI 2.10–4.63). As compared to women with further education, there was no difference in odds of overweight among blue-collar women (OR = 1.04, 95% CI 0.49–2.21) and the odds of overweight were decreased (OR = 0.74, 95% CI 0.29–1.85). | National Longitudinal Study of Adolescent Health | High-Income | (Yang et al., 2008) | |
| Longitudinal | Partner cessation request, partner smoking, intervention group, age, gender, race/ethnicity, education, income, smoking quantity (per day) | Smoking Abstinence at 1- and 6-Months Post Intervention Follow-Up | Male vs. female blue-collar workersB | As compared with men, the odds of smoking at baseline among women were 0.36 times the odds of smoking at baseline among men (0.14, 0.91). The OR for smoking one-month post-intervention in women versus men was 0.71 (0.23–2.18) and the OR for prolonged cessation (six-months after baseline) in women vs. men was 1.19 (0.25, 5.80). | The MassBUILT Study | High-Income | (Okechukwu et al., 2010) | |
| Cross-Sectional | Age, marital status, education, age at first sexual exposure, sources of knowledge on HIV/AIDS | Use of condoms; sex with multiple partners; drug abuse | Exposure-outcome among blue-collar women | Among female garment workers, increased knowledge score was associated with increased odds of using a condom at last intercourse (OR = 1.482, p = 0.10), decreased odds of sex with multiple partners (OR = 0.832, p = 0.036), and decreased odds of drug abuse (OR = 0.766, p = 0.034). | Female workers randomly selected from five garment factories in Dhaka, Bangladesh | High-Income | (Sayem, 2010) | |
| Cross-Sectional | Gender, age, education, ethnicity, negative affectivity, social desirability, drinking norms, policy enforcement, role overload, job insecurity, job hazards, decision involvement, self-estrangement, social interactions | Quantity of alcohol consumption; Frequency of alcohol consumption; Frequency of Drug Use | Male vs. female blue-collar workersB | As compared with blue-collar men, blue-collar women consumed greater quantities of alcohol (ß = 0.161, p > 0.05), consumed alcohol with greater frequency (ß = 0.260, p > 0.050), and used drugs less frequently (ß = -0.845, p < 0.01). | Random sample of workers from a single manufacturing firm in Israel employed at plants with 80 or more workers. | High-Income | (Biron et al., 2011) | |
| Longitudinal | Working class parents, household appliances, and poor somatic health at age 16; time in paid work, poor cash margin, and having children at age 21; months unemployment, financial strain, physically heavy work, high demands, low control, violence, and daily smoking at day 30 | Somatic health | Blue-collar women vs. other women | As compared with white-collar women with good somatic health at age 30, the odds were decreased for poor somatic health at age 16 (OR = 0.53, 95% CI 0.23–1.24) blue-collar women with poor somatic health at age 30. As compared with white-collar women with good somatic health at age 30, the odds of daily smoking (OR = 2.72, 95% CI 1.22–6.06) were increased in blue-collar women with poor somatic health at age 30. | Northern Swedish Cohort | High-Income | (Hammarström et al., 2011) | |
| Cross-Sectional | Age, gender, race, income, education, self-rated health, occupational factors, union commitment, job satisfaction, exposure to occupational factors | Current smoking | Male vs. female blue-collar workersB | The odds of current smoking among blue-collar women were increased as compared with blue-collar men (OR = 1.37, 95% CI 0.87–2.17). | The MassBUILT Study | High-Income | (Chin et al., 2012) | |
| Longitudinal | Intervention status, age, gender, race, income, education, smoking intensity, union commitment, exposure to occupational hazards, concern about exposure to occupational hazards | Smoking Cessation at 1- and 6-months post-intervention monitoring | Male vs. female blue-collar workersB | Odds of smoking cessation one-month post-intervention were increased among blue-collar women as compared with blue-collar men (OR = 2.19, 95% CI 0.61–7.89). Odds of prolonged cessation six months post-intervention among blue-collar women were increased as compared with blue-collar men (OR = 1.20, 95% CI 0.24 – 6.06). | The MassBUILT Study | High-Income | (Chin et al., 2012) | |
| Cross-Sectional | Age, gender, race, income, education, time to first cigarette, age of smoking initiation, intention to quit at 30 days, self-efficacy for quitting 30 days, temptation to smoke, decisional balance, household smoking, dust exposure at work, chemical exposure at work, concern about exposure to occupational hazards | Heavy smoking | Male vs. female blue-collar workersC | The odds of heavy smoking among blue-collar men were increased as compared with blue-collar women (OR = 4.55, 95% CI 1.62–12.79). | The MassBUILT Study | High-Income | (Chin et al., 2013) | |
| Cross-Sectional | Occupational class, education, poverty-income ratio | Smoking | Blue-collar women vs. other women | The odds of smoking among blue-collar women were increased as compared with white-collar women (6.65, 95% CI 4.90–9.03). | Third Korean National health and Nutrition Examination (KNHANES III) | High-Income | (Cho and Lee, 2012) | |
| Cross-Sectional | Occupational class, exposure to workplace environmental tobacco smoke (ETS) | Never smoking; Exposure to workplace ETS; Smoking cessation; Smoking intensity | Blue-collar women vs. other women | The odds of being a never-smoking were similar among blue-collar women and female managers and professionals (OR = 1.08, 95% CI 0.75–1.55). The odds of workplace environmental tobacco smoker were increased among blue-collar women as compared with female managers and professionals (OR = 1.53, 95% CI 1.01–2.30). | Multi-Ethnic Study of Atherosclerosis (MESA) | High-Income | (Fujishiro et al., 2012) | |
| Cross-Sectional | Age, sex, past month cigarette use, AUDIT (alcohol problem), race, education | Smokeless Tobacco Use | Male vs. female blue-collar workersC | The odds of smokeless tobacco use were increased among male operating engineers as compared with female operating engineers (OR = 5.06, 95% CI 0.66–38.75). | Operating engineers coming to either an apprentice certification or Hazardous Materials (Hazmat) refresher course in Michigan. | High-Income | (Noonan and Duffy, 2012) | |
| Longitudinal | Labor market shock, cigarette prices, state anti-smoking sentiment, age, sex, education, race/ethnicity, employment status, family income, data collection year | Smoking status | Male vs. female blue-collar workersB | The odds of smoking among female construction workers were increased as compared with male construction workers (OR = 1.08, 95% CI 0.90 1.29). | Tobacco Use supplement to the Current Population Survey (TUS-CPS) | High-Income | (Okechukwu et al., 2012) | |
| Cross-Sectional | Occupational class, race/ethnicity, age, education, adverse childhood events | Monthly binge drinking, past-30 day smoking, past year marijuana use, polysubstance use (2+ more) | Blue-collar women vs. other women | As compared with women employed in non-physically demanding occupations, the odds were increased for binge drinking (OR = 4.01, 95% CI 1.68–9.49), past 30-day smoking (OR = 1.94, 95% CI 1.18–3.21), marijuana use (OR = 1.37, 95% CI 0.59–3.20), and polysubstance use (OR = 3.21, 95% CI 1.40–7.38) among blue-collar women. | A purposive sample of workers and their spouses or cohabitating partners sampled from a large union representing construction industry workers in Northern California. | High-Income | (Cunradi et al., 2014) | |
| Cross-Sectional | Occupational class; occupational status (high, upper, intermediate, simple, low); employment status | Cigarette smoking, heavy smoking; alcohol consumption, excessive heavy drinking; cannabis use; analgesic use; weekly analgesics use | Blue-collar women vs. other women | As compared with white-collar women, the 30-day prevalence of smoking (OR = 1.10, 95% CI = 0.88–1.38); the odds of smoking ≥ 20 cigarettes per day in the past 30 days (OR = 1.15, 95% CI 0.70–1.90); the 12-month prevalence of cannabis use (OR = 1.08, 95% CI 0.56–2.10); and the 30-day prevalence of analgesic use (OR = 1.23, 95% CI 0.93 - 1.63) were increased among blue-collar women. The 30-day prevalence of alcohol consumption (OR = 0.74, 95% CI 0.60 - 0.92); the 30-day prevalence of excessive heavy drinking (OR = 0.78, 95% CI 0.59 - 1.03), and the 30-day prevalence of analgesic use (OR = 0.88. 95% CI 0.73–1.07) were decreased among blue-collar women as compared with white-collar women. | German Epidemiological Survey of Substance Use | High-Income | (Maron et al., 2016) |
NR = Not Reported.
We included only those independent variables for which authors reported results.
Denotes studies in which occupational class was not the primary independent variable.
Denotes studies in which sex/gender was not the primary independent variable.
Denotes exploratory studies that considered multiple independent variables simultaneously.
We organized studies by the following health outcome categories: BMI and metabolism, cancer, cardiovascular disease, disability and absenteeism, health behaviors, mental health, mortality (all-cause and cause-specific), musculoskeletal disorders, reproductive and sexual health, respiratory diseases, self-rated health, and smoking and other substance use. Studies reporting on multiple health outcomes were listed under each relevant health outcome.
We did not attempt meta-analysis because the majority of studies either lacked raw data, used the same or similar data sources, and because substantial variability in study design precluded meaningful quantitative synthesis. We did not attempt a formal assessment of risk of bias due to heterogeneity in study design, analytic method, and scientific question. Data extracted and summarized in Table 2 (e.g. sample size and study design), however, provides a preliminary indication of whether study findings may be subject to various biases.
3. Results
We identified 3327 records through our first search, assessed 394 full articles, and retained and extracted data from 104 studies. We identified 1522 records through our second search, assessed 346 full articles and retained and extracted data from 73 studies. (Fig. 1) We included 177 articles in our review in total and note an increase in the number of articles published each year between 1990 and 2015 (Fig. 2).
Fig. 1.
PRISMA flow diagram. The first search (Panel A) was conducted between January and June 2016 in three major databases (Google Scholar, Web of Science, and Pub Med) with combinations of the terms “blue-collar,” “health,” and “women” or “female.” The second search (Panel B) was conducted between March and June of 2017 using integrated synonyms and related terms of major concepts. This search was expanded to include several additional databases: Medline (PubMed); Scopus (Elsevier); Gender Watch (ProQuest); Social Sciences Citation Index (Clarivate); LGBT Life Full Text (EBSCO); CINAHL(EBSCO); Cochrane Library of Systematic Reviews (Cochrane); SafetyLit (SafetyLit Foundation); and Women's Studies Quarterly.
Fig. 2.
Number of studies published per year, 1990–2015.
Two patterns related to the publication of studies are worth noting. First, the study of specific cohorts occasionally predominated findings from a given country. For example, of the 14 studies from Australia, five were studies onphysical activity. Of the 11 studies from South Korea, five used data from KNHANES, and four recruited study participants from the City of Incheon. Of the five studies from Israel, four used data from the CORDIS study and were published prior to 2001. Both studies from Mexico evaluated the helath of female maquiladoras in Tijuana. Of the 16 studies on smoking and other substance use, 10 were from the U.S. and four of these studies used baseline data from the MassBUILT study. Of the seven U.S. studies on musculoskeletal disorders, six used data from the American Manufacturing Cohort.
Second, although studies were included from 40 different countries across North and South America, Europe, Asia, and Australia (Table 1A), these were primarily from high-income nations (N = 24, 60.0%). The majority of studies were based either in the United States (N = 45, 25.4%) or in Scandinavian Countries (N = 52, 29.4%). Only 21 studies (11.8%) were based in middle- or low-income countries (Table 1B). Fourteen of these studies were in middle income countries. Upper-middle income countries included China, the Dominican Republic, Iran, Mexico, Peru, Romania, Russia, Serbia, Thailand, Turkey; and lower-middle income countries included Bangladesh, India, Vietnam, and Sri Lanka. One low-income country, Nepal, was included as well. These studies generally included fewer blue-collar women (Median = 286, 203.8 – 671.8) relative to the studies from high-income countries. With the exception of one quasi-experimental study, all studies conducted in low- and middle-income countries were cross-sectional in design. The most commonly studied health outcomes were those related to sexual and reproductive health, musculoskeletal disorders, and mental health outcomes.
Table 1A.
Descriptive Statistics for Study Sample (N = 177).
| Countries included in study sample - N | 40 |
| Country classification – N (%)a | |
| High-Income | 24 (60.0) |
| Upper-Middle income | 11 (27.5) |
| Low-Middle income | 4 (10.0) |
| Low-Income | 1 (2.5) |
| Most frequently studied countries – N (%)b | |
| United States | 45 (25.4) |
| Sweden | 23 (13.0) |
| Finland | 16 (9.0) |
| Australia | 12 (6.8) |
| Japan | 10 (5.6) |
| Health outcomesc | |
| BMI & metabolism | 13 (7.3) |
| Cancer | 12 (6.8) |
| Cardiovascular diseases | 19 (10.7) |
| Disability & absenteeism | 13 (7.3) |
| Health behaviors | 16 (9.0) |
| Mental health | 17 (9.6) |
| Mortality | 20 (11.3) |
| MSK | 30 (16.9) |
| Other | 15 (8.5) |
| Reproductive & sexual health | 14 (7.9) |
| Respiratory | 14 (7.9) |
| Self-Rated health | 5 (2.8) |
| Smoking & other substance use | 16 (9.0) |
| Study design | |
| Cross-sectional | 85 (48.0) |
| Case-Control | 18 (10.2) |
| Longitudinal | 71 (40.1) |
| Quasi-Experimental | 3 (1.7) |
| Type of point estimate presented – N (%) | |
| Blue-collar women vs. blue-collar men | 31 (17.5) |
| Blue-collar women vs. other women | 91 (51.4) |
| Exposure-outcome among blue-collar women | 55 (31.1) |
| Number of women included – Median (IQR)d | 946 (305–4,580) |
| Number of blue-collar women included – Median (IQR)e | 422.5 (100–1,196) |
Percentages are calculated based on the number of unique countries.
Percentages are calculated based on the number of studies.
Percentages do not sum to 100% because several studies report for multiple health outcomes.
Missing for 4 studies.
Missing for 25 studies.
Table 1B.
Descriptive Statistics for Lower and Middle-Income Countries (N = 21).
| Countries included in study sample - N | 16 |
| Most frequently studied countries – N (%)a | |
| China | 5 (23.8) |
| Mexico | 2 (9.5) |
| Turkey | 2 (9.5) |
| Vietnam | 2 (9.5) |
| Health outcomesb | |
| BMI & metabolism | 1 (4.8) |
| Cancer | 3 (14.3) |
| Cardiovascular | 1 (4.8) |
| Disability & Absenteeism | 1 (4.8) |
| Health behaviors | 1 (4.8) |
| Mental health | 3 (14.3) |
| Mortality | 1 (4.8) |
| MSK | 5 (23.8) |
| Other | 3 (14.3) |
| Reproductive & sexual health | 5 (23.8) |
| Respiratory | 2 (9.5) |
| Self-Rated health | 2 (9.5) |
| Smoking and other substance use | 1 (4.8) |
| Study design | |
| Cross-sectional | 19 (90.5) |
| Case-Control | 1 (4.8) |
| Quasi-Experimental | 1 (4.8) |
| Type of point estimate presented – N (%) | |
| Blue-collar women vs. blue-collar men | 4 (19.0) |
| Blue-collar women vs. other women | 6 (28.6) |
| Exposure-outcome among blue-collar women | 11 (52.3) |
| Number of women included – Median (IQR)c | 360 (263–1,058) |
| Number of blue-collar women included – Median (IQR)d | 286 (203.8–671.8) |
Percentages are calculated based on the number of studies.
Percentages do not sum to 100% because several studies report for multiple health outcomes.
Missing for 1 study.
Missing for 2 studies.
3.1. Study design and analysis
Summary statistics related to study design and analysis are reported in Table 1A. Approximately half of studies were cross-sectional (N = 85, 48.0%). The remainder employed a longitudinal, case-control, or quasi-experimental study design. The median number of blue-collar women included across studies was 422.5 (IQR 100–1,196).
Across studies, authors characterized the health of blue-collar women to one or more of three different referent groups: (1) studies compared the health of blue-collar women and blue-collar men; (2) studies compared the health of blue-collar women to women in other industries or job types, including white-collar women, office and clerical workers, and women in the general population; (3) studies examined independent risk factors for disease among blue-collar women. The minority of studies included in this review compared the health of blue-collar women and blue-collar men (N = 31, 17.5%). Approximately half of studies compared the health of blue-collar women to a female referent group, and nearly one-third of studies reported a specific exposure-outcome association among blue-collar women (N = 55, 31.1%).
3.2. Health outcomes
We report characteristics for each study in Table 2 within each health outcome category. The two most commonly studied outcomes were musculoskeletal disorders (N = 30, 16.9%), followed by all-cause and cause-specific mortality (N = 20, 11.3%) and cardiovascular diseases (N = 19, 10.7%) (Fig. 3). Cross-sectional design predominated among studies of mental health outcomes, reproductive and sexual health, and smoking and other substance use. By contrast, the majority of mortality studies were longitudinal, and studies on cancer were either longitudinal or case-control design. (Fig. 4)
Fig. 3.
Number of Studies Published by Country.
Fig. 4.
Number of Studies by health outcome category*. *Studies that reported findings across health outcome categories appear multiple times.
Overall, study findings across health outcome categories suggested inferior health among female blue-collar workers as compared with blue-collar men or women in other industries or job types. Of studies that compared the health of blue-collar men and women, the majority considered musculoskeletal, respiratory, or smoking-related outcomes. Studies on musculoskeletal disorders consistently showed increased risk for pain and work-related injuries in blue-collar women as compared with men (Chin et al., 2012, Carlsson and Karlsson, 1970, Centre for Social Development et al., 2018, Chenet et al., 1998, Case and Paxson, 2005, Catalano and Bruckner, 2006, Chin et al., 2012, Cantley et al., 2016). Similarly, blue-collar women exhibited inferior respiratory health compared with blue-collar men based on results from pulmonary function tests and airway responsiveness (Choi et al., 2013, Chin et al., 2013, Cho and Lee, 2012, Christensen et al., 2008). Comparisons of smoking frequency in male and female blue-collar workers, however, yielded inconsistent findings (Cocco et al., 1999, Cohidon et al., 2009, Colt et al., 2011, Cleland et al., 2011, Clougherty et al., 2010, Clougherty et al., 2011, Cobankara et al., 2011).
Inferior health was also observed among blue-collar women for a wide range of health outcomes as compared with women in other industries or job types. Increased risk for cardiovascular disease – including myocardial infarction, chest discomfort, coronary heart disease, hypertension, and stroke – was consistently observed in blue-collar women as compared with white-collar women (Costello et al., 2016, Cunradi et al., 2014, Cunradi et al., 2007, Cullen et al., 2015, Costello et al., 2014, Dasgupta et al., 2012, Courville et al., 1991, Duffy et al., 2012). The majority of studies on all-cause and cause-specific mortality found increased risk in blue-collar women as compared with other working women (Eskenazi et al., 1993, Frankenhaeuser et al., 1989, Fujishiro et al., 2015, Fredriksson et al., 1999, Gallo et al., 2003, Ericson et al., 2007, Frone, 2000, Eshak et al., 2013, Forman-Hoffman et al., 2008, Fujishiro et al., 2012, von Ehrenstein et al., 2014, Evans et al., 2003). Two studies found decreased risk of all-cause and cause-specific mortality in blue-collar women as compared with women in the general population (Gang et al., 2002, Gissler et al., 2009), a finding which may reflect the fact that employed persons tend to be healthier on average as compared with members of the general population. Studies also find increased risk for various musculoskeletal disorders (Hammarström et al., 2011, Goldenhar et al., 1998, Gold et al., 2006, Hammar et al., 1994, Hallman et al., 2015, Grimmer, 1993, Guendelman and Silberg, 1993, Hall et al., 1993, Gupta et al., 2014), adverse pregnancy-related outcomes (Hanklang et al., 2014, Hein et al., 2007, Harley et al., 2010, Heikkilä et al., 2008, Hirokawa et al., 2013, Heo et al., 2015), and smoking (Cunradi et al., 2007, Honjo et al., 2010, Howard et al., 2017, House, 1980, Hocschild and Machung, 2012) in blue-collar women as compared with women in other occupations and job types.
Of note, comparisons of risk of overweight and obesity in blue-collar women as compared with women in other industries or job types yielded mixed findings. Studies on health behaviors also did not consistently show whether levels of physical activity were increased or decreased in blue-collar women as compared with other women. This discrepancy persisted even in studies that only considered leisure time physical activity.
Studies that focused on identifying risk factors for morbidity and mortality among blue-collar women typically focused either on the physical risks associated with blue-collar, job demand, or organizational climate. Several studies identified chemical exposures a risk factor not only for cancers among blue-collar women (Hwang and Lee, 2014, Iverson and Erwin, 1997, Hrubá et al., 2009, Hwang et al., 2015), but also for psychiatric distress and depression (Jousilahti et al., 1996, Jakobsson and Mikoczy, 2009). Increased job demand, job conflict, subjective monotony, skill underutilization and sexual harassment were all identified as risk factors for psychiatric distress (Juutilainen et al., 2000, Kaergaard and Andersen, 2000, Kaila-Kangas et al., 2006), although reduced psychological distress was observed among blue-collar women with adequate social support (Jousilahti et al., 1996, Kalleberg, 2009). Factors such as work control, job strain, and occupational stress do not appear to be associated with cardiovascular disease among blue-collar women (Kalleberg, 2012, Karasek, 1979, Kåreholt, 2001). We include a complete discussion of study findings on the health of female blue-collar workers in Appendix B.
4. Discussion
The primary objectives of this systematic review were to catalogue the extent and strength of the existing empiric evidence on the health of blue-collar women; identify patterns in publication over time, across countries, and among various health outcomes; and to evaluate the degree to which study findings converge. We examined literature published between 1990 and 2015, a 25-year period selected to capture major trends in the global economy that may be salient to contemporary working women's health.
Our search identified 177 peer-reviewed studies published over the past 25 years across 40 different countries on a wide range of health outcomes. Findings from these studies suggests that blue-collar women experience worse health than either blue-collar men or other women. This finding emerged as a general pattern across a diverse array of studies with different target populations, designs, analyses, times, contexts, and referent groups. The following factors, however, may preclude direct comparison between many of the studies included in this review.
First, substantial heterogeneity across geographies implies heterogeneity in sociopolitical and cultural contexts, which in turn may influence labor regimes, gendered norms around labor force participation, and ultimately any findings on the association between gender, occupational class or the work environment, and health.
Second, while several studies reported findings on a specific exposure-outcome relationship among blue-collar women, the majority compared disease risk among blue-collar women to disease risk among another group of women (such as female white-collar workers). Fewer studies compared disease risk among blue-collar men and blue-collar women. These three different types of measures of association cannot be directly compared with one another. Interpretation of study findings that contrast risk of morbidity and mortality among blue-collar men and blue-collar women is further complicated by the fact that any differences may be attributable to differences in biological sex, socially-constructed gender, or some combination thereof. Interpretation of study findings that contrast the risk of morbidity and mortality among two groups of women distinguished by their occupational class is complicated by the fact that measures of associations likely reflect some combination of the effects of occupational class and indirect selection processes (i.e. selection of more or less educated women into a particular occupational class) (Klumb and Lampert, 2004).
Third, study findings were influenced by age- and cohort-effects that were not always addressed or adjusted for in analyses. Age effects result from the physiological state of aging and the social influences associated with a certain age, while cohort effects stem from influences associated with membership to a particular birth cohort (Carlsson and Karlsson, 1970). Although most studies controlled for age as a potential confounder, we note substantial heterogeneity in the age range to which the study population was restricted. Some studies, for example, limited participation to older adults (Duffy et al., 2012, Kivimäki et al., 2007), while others included any adult over the age of 18 in their study samples (McCormack, Giles-Corti, & Milligan, 2006).
Because risk for nearly all diseases increases with age, studies that limited their samples to older adults are not comparable to those that included a broader range of ages. Cohort effects also hinder cross-study comparisons because different birth cohorts may have been exposed to certain risk or protective factors that differentially influenced their likelihood of morbidity or mortality. Changes over time in societal norms or other social, political, and environmental factors related to gender and work potentially influenced patterns of health outcomes. As men and women's exposure to job-related chemicals and substances, ergonomic demands, and psychosocial stressors have varied over time, the statistical significance of study findings may depend on the specific birth cohorts included in the study population.
Fourth, because we did not limit our review to studies whose primary research question pertained to the causal effects of gender and occupational class on health, estimates for sex/gender or occupational class were often considered as secondary variables. Direct interpretation of the effect estimates for secondary risk factors, therefore, do not necessarily represent total effect estimates, and may be confounded even when the effect estimate for the main exposure is not (Westreich and Greenland, 2013). This phenomenon can occur when the set of variables used for adjustment are selected with the goal of isolating the causal effect of the main exposure, not the secondary variables. The appropriate set of control variables for a causal study of the effect of any of the secondary variables may be different, however, from the set presented in the current study. We therefore encourage readers to be cautious in drawing conclusions from studies that controlled for gender or occupational class but did not consider either as a main effect in their analysis. We indicate which studies did not consider gender or occupational class as a main effect with superscripts in the “reference group” column in Table 2.
Fifth, the generalizability of results in this review is limited by the over-representation of high-income nations. Although 40 different countries were represented in our synthesis, the majority were based on the experiences of women in industrialized, high-income countries – particularly the Scandinavian countries and the United States. The percentage of women employed in blue collar jobs in these countries has held steady over the past 30 years (Korda et al., 2002, Kongerud and Soyseth, 1991), with growth of women in blue collar work occurring predominantly in middle and low-income countries (Centre for Social Development et al., 2018). A concerted effort to study the health of blue-collar women in lower and middle-income countries will be essential in order to gain a comprehensive understanding of how work influences women's health in varied geographic contexts amidst changing sociopolitical contexts, gender norms, and labor laws. Generalizability is further complicated by the fact that single study populations were represented multiple times among several of the papers, and by variability in the composition of blue-collar industries represented by the study population. While studies focused on workers from the same industry subsector (e.g. primary metals manufacturing, textile mills) may be more readily compared to one another, population-based studies where multiple blue-collar industries are represented have the potential to offer more general information about blue-collar workers’ health.
Sixth, studies of working populations can yield biased findings due to the healthy hire and the healthy worker survivor effects. The healthy hire effect is the processes whereby healthier workers are more likely to seek and gain employment (Lea et al., 1999), a phenomenon that is particularly problematic for studies that directly compared blue-collar women with women in the general population or women outside of the workforce (Eshak et al., 2013, Kubo et al., 2013). A related point is that other dimensions of social class that precede employment status – namely educational attainment – may explain both entry into blue collar jobs and inferior health. Approximately half of studies included in this review (N = 89, 50.2%) did not adjust for educational attainment, which raises the possibility that differences in educational attainment offer a partial explanation for the observed inferior health of blue-collar women as compared with blue-collar men and women in other occupations or job types. Very few studies included in our review employed methods to address the potential for increased likelihood of null-biased results in longitudinal studies where a systematic attrition of unhealthy workers occurs over time (Hwang and Lee, 2014, Kuiack et al., 2007, Lalive and Zweimüller, 2009).
Finally, the majority of studies—and nearly all studies reporting on the health of blue-collar women in low- and middle-income countries—employed a cross-sectional design, which naturally raises questions regarding the temporal ordering of exposure and outcome. The notable exceptions were the quasi-experimental studies, one of which evaluated the effects of exogenous wage increases among factory workers in the Dominican Republic (Landefeld et al., 2014). The other two studies exploited changes in parental leave policies and firm closures in Austria (Lederer, 1981, Lea et al., 1999). We also note many studies that were limited by modest sample sizes, which decreases the power to detect real statistical associations, particularly among blue-collar women who often comprise a small minority of the study population. Threats to statistical power were particularly common among studies evaluating health outcomes with a low prevalence, such as cancer or cause-specific mortality.
5. Conclusion
In this “state-of-the-field” review, we find that research on the health of blue-collar women over the past quarter century generally suggests that blue-collar women experience worse health than blue-collar men or women in other occupational classes. Methodological limitations and notable heterogeneity across study populations, however, introduce uncertainty into the interpretation of such findings. These factors, alongside the rapidly changing nature of women in the workplace, motivate further study on the health of blue-collar women. Efforts to identify specific mechanisms by which blue-collar work may predispose women to adverse health may be particularly valuable in informing future workplace-based and policy-level interventions. For example, future reviews may focus on the synthesis of evidence on sex differences in response to physical hazards in the workplace so as to inform regulatory guidelines to improve occupational safety and health (Lewin et al., 2014, Lin et al., 2015). Alternatively, future efforts may focus on synthesizing the evidence on the effects of various aspects of organizational climate on women's health and well-being in historically male-dominated industries and occupations.
Expanding research into other countries, particularly less developed nations, will be useful in order to gain understanding of how differences in labor laws, working conditions, workplace safety, and in cultural norms and attitudes toward women and work contribute to the health of blue collar women. With much blue-collar work in middle and low-income countries remaining in the informal sector, studies on the experiences of these “invisible women,” at least from the economic sense, are needed.
Acknowledgements
The authors would like to thank Dr. Ellicott Matthay for her thoughtful comments on an earlier version of this manuscript. This research was supported by the National Institute of Health National Institute on Aging grant R01-AG026291; the National Institute on Occupational Health and Safety grant 5T42OH008429-13; and by the National Institute on Mental Health grant F31 MH 112246. The conclusions expressed are solely those of the authors.
Acknowledgments
Ethics approval
Ethics approval is not required for this paper, as this is a systematic review that does not directly involve data collected from human subjects.
Contributor Information
Holly Elser, Email: holly.stewart@berkeley.edu.
April M. Falconi, Email: afalconi@stanford.edu.
Michelle Bass, Email: michellebbass@stanford.edu.
Mark R. Cullen, Email: mrcullen@stanford.edu.
Appendix A. List of search algorithms
| Database | Search terms |
|---|---|
| Google Scholar | health, “blue collar women” |
| health “female blue collar” | |
| PubMedA | Preliminary Search: |
| health, “blue collar women” | |
| health “female blue collar” | |
| Updated Search: | |
| ((((sex[tiab] OR female[tiab])) OR (("Sex Factors"[Mesh]) OR (("Women's Health"[Mesh]) OR "Women, Working"[Mesh])))) AND (((((((("Industrial Development"[Mesh:NoExp]) OR "Manufacturing Industry"[Mesh:NoExp]) OR "Construction Industry"[Mesh:NoExp]) OR "Extraction and Processing Industry"[Mesh]) OR "Textile Industry"[Mesh]) OR "Tobacco Industry"[Mesh])) OR ("blue collar"[tw] OR "blue-collar"[tw])) | |
| Web of Science A | Preliminary Search: |
| health, “blue collar women” | |
| health “female blue collar” | |
| Updated Search: | |
| (TS = (“blue collar”) OR TI = (“blue-collar”)) AND (TS = (women OR female OR “women work*”) OR TI = (Women OR female OR “women work*”)) | |
| SCOPUS | (TITLE-ABS-KEY ("blue collar" OR "blue-collar") AND TITLE-ABS KEY (women OR female) AND TITLE-ABS-KEY (industr* OR "women work*") AND TITLE-ABS-KEY (health)) |
| Contemporary Women's Issues | Words and phrases: blue collar |
| Subject: health general | |
| Women's Studies Quarterly | blue collar AND health |
| Social Sciences Citation Index | TOPIC:(blue collar) OR TITLE: (blue collar) AND TOPIC:(women) OR TITLE:(women) AND TOPIC:(health) OR TITLE:(health) |
| LGBT Life with Full Text | Women AND Blue Collar |
| SafetyLit | Women AND Blue Collar |
| CINAHL | MH blue collar workers OR TI blue collar OR AB blue collar OR SU blue collar OR MH industry AND (MH "Women+") OR (MH "Women, Working+") |
| Gender Watch | ((SU.EXACT("Gender") OR SU.EXACT("Women") OR SU.EXACT("Female employees") OR SU.EXACT("Gender differences")) OR all(women OR "women work*")) AND ((SU.EXACT("Manufacturing") OR SU.EXACT("Blue collar workers") OR SU.EXACT("Manual workers") OR SU.EXACT("Construction industry")) OR all("blue-collar" OR "blue collar")) |
| Cochrane | “Blue collar” AND women |
AFor Web of Science and PubMed we report our preliminary search strategy as well as the updated strategy developed by the medical librarian.
Appendix B. Description of findings by health outcome category
Studies that met the inclusion criteria for this systematic review were classified into one of 11 health outcome categories: BMI and metabolism; cancer; cardiovascular diseases; disability and absenteeism; mental health; all-cause and cause-specific mortality; musculoskeletal disorders; reproductive and sexual health; respiratory diseases; self-rated health; and smoking and other substance use. Disease endpoints that did not fit into one of these categories were classified as “other.” Below, we summarize study findings within each health outcome category. For each health outcome category, we first summarize results from studies that compared male and female blue-collar workers, we then summarize results from studies that compared blue-collar women to women in other industries or job types. Finally, we discuss specific risk factors for disease identified among blue-collar women. Where possible, we synthesize results and note consistency of findings.
BMI & metabolism (N = 13 Studies)
In one cross-sectional study of Michigan operating engineers, the odds of obesity were decreased in women versus men (Duffy, Cohen, Choi, McCullagh, & Noonan, 2012). Findings on risk of obesity or increased BMI in female blue-collar workers, however, yield mixed findings. While several studies note increased odds of obesity and increased BMI among blue-collar women as compared with either white-collar workers or professionals (Lombardo et al., 2012, Cunradi et al., 2007, Van Loon et al., 1995, Lipton et al., 2008), others reported equivalent odds of overweight and obesity in blue-collar women and women with further education (Yang et al., 2008); lower waist circumference and waist-to-hip ratio in blue-collar women versus white-collar women (Nakamura, Nakamura, & Tanaka, 2000); and no increase in fat mass index (FMI) in blue-collar women versus those working in the transport and communications industry (Lewin et al., 2014). These discrepancies may reflect differences in the reference group selected by the investigators or differences in the specific outcomes considered. The one study that compared diabetes risk in blue- and white-collar women found increased risk for type 2 diabetes in blue-collar women (Maty, Everson-Rose, Haan, Raghunathan, & Kaplan, 2005).
Among blue-collar women, retirement was associated with weight gain; type 2 diabetes was associated with soda drinking; work-related factors such as low job stress, low social support, and repetitive work were associated with metabolic syndrome and elevated serum glucose levels (Mäkinen et al., 2010, Luoto et al., 1994, Mammen and Paxson, 2000, Kaila-Kangas et al., 2006).
Cancer (N = 12 Studies)
No studies in this review compared cancer risk in blue-collar men and women. Women working in a wide-range of blue-collar industries - including textile mills, paper mills, printing and publishing industries, petroleum refining, and motor vehicles manufacturing – were at increased risk for cancers of the central nervous system (Cocco, Heineman, & Dosemeci, 1999). Comparisons of breast cancer risk in blue-collar women versus women in other industries and job types yielded mixed findings. While one study from the Netherlands found no difference in breast cancer risk in blue- and white-collar women, results from a Swedish case-control study suggest excess breast cancer risk among metal platers and coaters and results from a longitudinal U.S. study suggest increased breast cancer risk in female crafts/operatives as compared with housewives (Maron et al., 2016, Mattioli et al., 2009, Mattisson et al., 2014). However, studies suggest decreased risk for lung cancer and colon cancer in blue- versus white-collar women (Maty et al., 2005, McCormack et al., 2006).
Among blue-collar women, studies consistently identified increased risk for cancers of the lung, breast, and cervix associated with exposure to occupational hazards such as chlorinated organic solvents or metalworking fluids (Hwang and Lee, 2014, Iverson and Erwin, 1997, Hrubá et al., 2009, Hwang et al., 2015). Greater duration of employment in blue-collar jobs was also associated with increased risk for cancers of the breast and bladder (Melamed et al., 1997, Melamed et al., 1995).
Cardiovascular Diseases (N = 19 Studies)
One cross-sectional study from South Korea found that cardiovascular disease risk equivalent in blue-collar men and women (Won, Hong, & Hwang, 2013). However blue-collar women's cardiovascular health is consistently noted as inferior to women in other industries and job types. Studies find increased risk for a wide range of cardiovascular diseases including myocardial infarction, chest discomfort, coronary heart disease, hypertension, and stroke as well as elevated lipid levels in blue- versus white-collar women (Costello et al., 2016, Cunradi et al., 2007, Cunradi et al., 2014, Cullen et al., 2015, Costello et al., 2014, Dasgupta et al., 2012, Duffy et al., 2012, Courville et al., 1991). However, two studies find reduced intima-media thickness in blue-collar women as compared with clerical workers and professional women, respectively (Messing and Stevenson, 1996, Minh, 2014).
Studies of risk factors for cardiovascular diseases among blue-collar women consider not only a wide range of risk factors, but also a wide range of specific disease endpoints, making it difficult to compare or synthesize study findings. Cross-sectional studies conducted in China and Israel identified sound pressure levels and short-cycle repetitive work, respectively, as risk factors for hypertension (Kaila-Kangas et al., 2006, Miura and Turrell, 2014). Scandinavian studies identified limited possibilities to learn new things, monotony, and noise (Hammar, Alfredsson, & Theorrell, 1994) as well as severity of symptoms with risk of first myocardial infarction (Jousilahti, Vartiainen, Tuomilehto, & Puska, 1996). Cardiovascular morbidities in general were more common in blue-collar women with low work social support and increased physical demand in one Swedish cohort (Hall et al., 1993), and noise exposure has also been linked with elevated serum cholesterol in Israeli blue-collar women (Melamed, Froom, Kristal-Boneh, Gofer, & Ribak, 1997). Risk for cardiovascular diseases were decreased among blue-collar women with increased psychological job demand, and no association was observed between work control and cardiovascular morbidity, job strain and hypertension, or occupational stress and stroke among blue-collar women (Kalleberg, 2012, Kåreholt, 2001, Karasek, 1979).
Disability & Absenteeism (N = 13 Studies)
No studies included in this review compared risk of disability or absenteeism in male and female blue-collar workers. Studies did consistently find that blue-collar women were more likely to have a limiting, long-standing illness or disability (Nag et al., 2010, Fredriksson et al., 1999); report sickness absence (Nakata et al., 2006, Guendelman and Silberg, 1993, Nakamura et al., 2000); have lowered work ability (Aittomäki, Lahelma, & Roos, 2003); or report lost worktime injury or illness (Strong and Zimmerman, 2005) as compared to women in other industries or occupations. By contrast, two studies found decreased likelihood of functional impairment in Mexican blue-collar women (Guendelman and Silberg, 1993) and decreased odds of having a long-term condition, reduced activity days, or time off work among Australian blue-collar women (Korda, Strazdins, Broom, & Lim, 2002) as compared with their respective counterparts in white-collar jobs. Only three studies considered determinants of disability and absenteeism among blue-collar women, and identify risk factors ranging from organizational climate (Oddone et al., 2013, Oddone et al., 2014) and work-family conflict (Väänänen et al., 2008) to reduced heart rate reserve (Gupta et al., 2014).
Health behaviors (N = 16 Studies)
Both studies that compared health behaviors in blue-collar men and women found inferior health among blue-collar women as measured by levels of physical activity (Wu and Porell, 2000) and health risk scores (Hwang, Hong, & Rankin, 2015). The majority of studies that compared health behaviors in blue-collar women and women in other industries or job types found that blue-collar women were less likely to engage in physical activity and exhibited less healthy dietary patterns (Oliveira et al., 2014, Pant et al., 2013, Ostlin et al., 1998, Parkinson et al., 1990, Kivimäki and Kalimo, 1996, Van Loon et al., 1995, Pekkanen et al., 1995). However, several studies reported that blue-collar women were more physically active as compared with women in other industries and job types (Cunradi et al., 2007, Potula and Kaye, 2006, Pollán and Gustavsson, 1999, Pollack et al., 2007, Prescott et al., 2003, Pudrovska et al., 2013). Discrepant findings on physical activity in blue-collar women versus other women persist even among studies that only considered physical activity during leisure time. One study found that blue-collar women who participated in a cancer prevention intervention decreased their fruit and vegetable consumption over the course of follow-up (Harley et al., 2010).
Mental health (N = 17 Studies)
Overall, findings on the mental health of blue-collar women yielded mixed findings. Both studies that compared mental health outcomes in blue-collar men and women found that blue-collar women were more likely to be depressed (Minh, 2014) and to use stress-related drugs (Rydstedt, Johansson, & Evans, 1998). Findings from studies that compared the mental health of women in blue-collar jobs to women in other industries and job types were mixed. Two studies from South Korea found increased risk of suicidal ideation among blue-collar women (Richiardi et al., 2004, Rieker and Bird, 2005); increased odds of depression were noted in female garment workers as compared with service workers (Guendelman and Silberg, 1993); and female workers at the Toulouse AZF disaster were more likely to experience psychological distress (Cohidon et al., 2009). By contrast, three studies from Scandinavia find no evidence of a difference in burnout, suicide, or emotional exhaustion in blue-collar women as compared with women in other occupations (Roquelaure et al., 2008, Rydstedt et al., 1998, Kubo et al., 2013).
Among blue-collar women, studies linked psychological distress to work-related physical and psychological stressors including sexual harassment (Jousilahti et al., 1996, Kalleberg, 2009, Juutilainen et al., 2000, Santhi et al., 2016, Sakr et al., 2010, Kaila-Kangas et al., 2006, Jakobsson and Mikoczy, 2009); domestic arrangements (Santos and Barros, 2003, Juutilainen et al., 2000, Santhi et al., 2016); and individual-level factors such as self-esteem, smoking, and BMI (Jousilahti et al., 1996, Sakr et al., 2010, Santhi et al., 2016). Reduced psychological distress was observed among blue-collar women with adequate social support (Jousilahti et al., 1996, Kalleberg, 2009).
Mortality (N = 20 Studies)
One study on smoking and all-cause mortality in urban transit operators reported increased risk for all-cause mortality in male drivers as compared with female drivers (Lipton, Cunradi, & Chen, 2008). Several studies reported comparisons blue-collar women versus women in other industries or job types, and the majority find increased risk for both all-cause and cause-specific mortality among blue-collar women (Eskenazi et al., 1993, Frankenhaeuser et al., 1989, Fredriksson et al., 1999, Gallo et al., 2003, Ericson et al., 2007, Frone, 2000, Fujishiro et al., 2012, Eshak et al., 2013, Forman-Hoffman et al., 2008, Fujishiro et al., 2015, von Ehrenstein et al., 2014, Evans et al., 2003). Only one study found decreased mortality risk among blue-collar women as compared with white-collar women (Hirokawa, Tsutsumi, & Kayaba, 2013). Two studies found decreased risk of all-cause and cause-specific mortality in blue-collar women as compared with women in the general population (Gang et al., 2002, Gissler et al., 2009), a finding which may reflect the fact that working populations tend to be healthier on average as compared with members of the general population. Risk factors for mortality identified among blue-collar women included physical demand and exposure to metalworking fluid (Sheehan and Lam, 2015, Kalleberg, 2012), although shift work, active work, and increased psychological demand appeared protective against mortality (Soares et al., 2007, Shirom et al., 2000, Kalleberg, 2012)
Musculoskeletal Disorders (N = 30 Studies)
Nearly all studies of musculoskeletal disorders find increased risk among blue-collar women as compared with blue-collar men or as compared with women in other industries or job types. Studies that compared blue-collar women and men find women at increased risk for pain in the neck, shoulder, and distal upper extremity (Wang et al., 2007). Women were also at increased risk for various work-related injuries (Chin et al., 2012, Carlsson and Karlsson, 1970, Centre for Social Development et al., 2018, Chenet et al., 1998, Case and Paxson, 2005, Catalano and Bruckner, 2006, Chin et al., 2012), as compared with men, although five of these seven studies were based on the same study population of primary metal and fabricated metal product manufacturers in the US (Chin et al., 2012, Centre for Social Development et al., 2018, Catalano and Bruckner, 2006, Chin et al., 2012, Case and Paxson, 2005). As compared with women in other industries or job types, blue-collar women were at increased risk for musculoskeletal disorders in general (Khatun et al., 2004); hospitalization for back disorders (Kaila-Kangas et al., 2006); injuries (Grimmer, 1993, Guendelman and Silberg, 1993); carpal-tunnel syndrome (Hallman et al., 2015, Gupta et al., 2014, Hall et al., 1993); and disorders of the hip, back, and knee (Hammarström et al., 2011, Hammar et al., 1994). Higher risk for musculoskeletal disorders among blue-collar women are most likely attributable to the physical nature of jobs in blue-collar industries, and only one study found no evidence of a difference between blue and white-collar women's risk for neck and shoulder disorders (Ahlgren et al., 2012).
Several studies assessed risk factors for musculoskeletal disorders among blue-collar women. Specific risk factors identified included psychological or physical strain (Stokholm et al., 2013, Storaas et al., 2015, Strong and Zimmerman, 2005, Taiwo et al., 2008, Takao et al., 2003, Takezaki et al., 2001, Tessier-Sherman et al., 2014) uncomfortable or inadequate work arrangements (Stokholm et al., 2013, Strong and Zimmerman, 2005, Thilsing et al., 2012, Thompson et al., 2005); age (Tsai et al., 1997, Takao et al., 2003, Takezaki et al., 2001); tenure (Strong and Zimmerman, 2005, Tsai et al., 1997, Takao et al., 2003); household arrangement (Stokholm et al., 2013, Thilsing et al., 2012); and sitting time (Hallman, Gupta, Mathiassen, & Holtermann, 2015). The majority of these studies were conducted either in Scandinavian countries (e.g. Sweden, Norway, Denmark) or in low- and middle-income countries (e.g. India, Perú, Thailand, Iran). Although similar risk factors are noted across these various geographic contexts, most are based on very limited sample sizes.
Reproductive & sexual health (N = 14 Studies)
Only one study conducted in the Kathmandu Valley compared the sexual health of blue-collar men and women, and found substantially increased odds of condom use among female factory workers as compared with men (Pant, Kanato, Thapa, & Ratanasiri, 2013). The majority of studies compared blue-collar women to an all-female referent group and consistently noted increased risk for a wide range of adverse pregnancy-related outcomes – including low birth weight and small for gestational age (Hanklang et al., 2014, Harley et al., 2010, Heikkilä et al., 2008), prematurity (Harley et al., 2010, Hein et al., 2007), perinatal mortality (Gissler et al., 2009), congenital anomalies (Sakr et al., 2010), and Caesarian section (Räisänen et al., 2014) – in blue-collar women as compared with women employed in other industries. Studies also found that blue-collar women were more likely to have multiple sexual partners, HSV-2 infection, and earlier natural menopause (US Census Bureau, 2017, Uijtdewilligen et al., 2015, Uijtdewilligen et al., 2014).
Two quasi-experimental studies evaluated the effects of parental leave policies and plant closures and fertility outcomes, respectively, among blue-collar women in Austria. These studies found that parental leave reform increased fertility but found minimal effects on fertility up to six years following plant closure (Lederer, 1981, Lea et al., 1999). Increased knowledge on HIV/AIDS was associated with increased condom use and decreased odds of sex with multiple partners among garment workers in Bangladesh (Sayem, 2010), and sulfur dioxide was identified as an independent risk factor for early natural menopause among blue-collar women in China (Wang et al., 2015).
Respiratory diseases (N = 14 Studies)
Studies that compared the blue-collar women to that of blue-collar men or women in other industries consistently found inferior respiratory health among blue-collar women. As compared with blue-collar men, women were noted increased methacholine responsiveness; decreased FEV1 and FVC; and increased acute airway response (Choi et al., 2013, Chin et al., 2013, Cho and Lee, 2012, Christensen et al., 2008). Increased risk for asthma, chronic rhinosinusitis and lung cancers was observed blue-collar women as compared with women in other industries (Väänänen et al., 2008, Wamala et al., 2001, Vahtera et al., 1999, Vingård et al., 1991). Among European blue-collar women, increased dust concentration was associated with decreased lung capacity (as measured by FVC and FEV1) (Love, Muirhead, Collins, & Soutar, 1991), although no significant effects of manganese exposure on pulmonary function was observed among female metalworkers in China (Wang et al., 2015).
Self-Rated health (N = 5 Studies)
Studies on self-rated health that compared blue-collar women and white-collar women yielded inconsistent findings (Kalleberg, 2009, Howard et al., 2017, Noonan and Duffy, 2012, Guendelman and Silberg, 1993). In one quasi-experimental study of the effect of a living wage policy, affected factory workers “excellent” or “much better” global and comparative self-rated health as compared with workers in control factories (Landefeld et al., 2014).
Smoking & Other Substance Use (N = 16 Studies)
Comparisons of smoking frequency in male and female blue-collar workers yield inconsistent findings (Cleland et al., 2011, Clougherty et al., 2010, Clougherty et al., 2011). Notably, results from three studies that compared frequency of smoking in male and female construction workers are inconsistent even though based on the MassBUILT study population (Cocco et al., 1999, Cohidon et al., 2009, Colt et al., 2011, Cobankara et al., 2011). However, studies consistently find that blue-collar women smoked more frequently as compared with white-collar women, managers and professionals, and women with further education (Cunradi et al., 2007, Honjo et al., 2010, Howard et al., 2017, House, 1980, Hocschild and Machung, 2012), with job strain, passive work, and physical demand identified as risk factors for smoking in a cross-sectional study from Australia (Radi, Ostry, & LaMontagne, 2007). Findings on alcohol and other substance use are limited and inconsistent (Wang et al., 2007, Westgaard and Jansen, 1992, House, 1980, U.S. Bureau of Labor Statistics, 2018).
Other health outcomes (N = 15 Studies)
Other health outcomes studied included work-related fatigue, insomnia, melatonin production, and sleep quality (Won et al., 2013, Juutilainen et al., 2000, World Bank, 2018, Westreich and Greenland, 2013, Raza et al., 1999); fibromyalgia (Cobankara, Unal, Kaya, Bozkurt, & Ozturk, 2011); headache, cognition, and other neurobehavioral effects (Jousilahti et al., 1996, Juutilainen et al., 2000, Yang et al., 2008, Jakobsson and Mikoczy, 2009, Yingying et al., 2011); serum uric acid production (Shirom, Melamed, & Nir-Dotan, 2000); blood and bone lead levels (Potula and Kaye, 2006); tooth abrasion (Kovacevic and Belojevic, 2006); hearing loss (Nguyen et al., 1998); and the prevalence long and short-term health conditions (Korda et al., 2002).
References
- Ahlgren C., Malmgren Olsson E.-B., Brulin C. Gender analysis of musculoskeletal disorders and emotional exhaustion: Interactive effects from physical and psychosocial work exposures and engagement in domestic work. Ergonomics. 2012;55(2):212–228. doi: 10.1080/00140139.2011.646319. [DOI] [PubMed] [Google Scholar]
- Aittomäki A., Lahelma E., Roos E. Work conditions and socioeconomic inequalities in work ability. Scandinavian Journal of Work, Environment & Health. 2003:159–165. doi: 10.5271/sjweh.718. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T., Kecklund G., Johansson S.-E. Shift work and mortality. Chronobiology International. 2004;21(6):1055–1061. doi: 10.1081/cbi-200038520. [DOI] [PubMed] [Google Scholar]
- Andersen S., Thygesen L.C., Davidsen M., Helweg-Larsen K. Cumulative years in occupation and the risk of hip or knee osteoarthritis in men and women: A register-based follow-up study. Occupational and Environmental Medicine. 2012;69(5):325–330. doi: 10.1136/oemed-2011-100033. [DOI] [PubMed] [Google Scholar]
- Andrés A.R., Collings S., Qin P. Sex-specific impact of socio-economic factors on suicide risk: A population-based case–control study in Denmark. The European Journal of Public Health. 2010;20(3):265–270. doi: 10.1093/eurpub/ckp183. [DOI] [PubMed] [Google Scholar]
- Applebaum K.M., Ray R.M., Astrakianakis G., Gao D.L., Thomas D.B., Christiani D.C.…Eisen E.A. Evidence of a paradoxical relationship between endotoxin and lung cancer after accounting for left truncation in a study of Chinese female textile workers. Occupational and Environmental Medicine. 2013 doi: 10.1136/oemed-2012-101240. oemed-2012-101240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arber S. Class, paid employment and family roles: Making sense of structural disadvantage, gender and health status. Social Science & Medicine. 1991;32(4):425–436. doi: 10.1016/0277-9536(91)90344-c. [DOI] [PubMed] [Google Scholar]
- Arbuckle T.E. Are there sex and gender differences in acute exposure to chemicals in the same setting? Environmental Research. 2006;101(2):195–204. doi: 10.1016/j.envres.2005.08.015. [DOI] [PubMed] [Google Scholar]
- Arena V.C., Costantino J.P., Sussman N.B., Redmond C.K. Issues and findings in the evaluation of occupational risk among women high nickel alloys workers. American Journal of Industrial Medicine. 1999;36(1):114–121. doi: 10.1002/(sici)1097-0274(199907)36:1<114::aid-ajim16>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Arnold D., Bongiovi J.R. Precarious, informalizing, and flexible work: Transforming concepts and understandings. American Behavioral Scientist. 2012;57(3):289–308. [Google Scholar]
- Asztalos M., Wijndaele K., De Bourdeaudhuij I., Philippaerts R., Matton L., Duvigneaud N., Thomis M., Duquet W., Lefevre J., Cardon G. Specific associations between types of physical activity and components of mental health. Journal of Science and Medicine in Sport. 2009;12(4):468–474. doi: 10.1016/j.jsams.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Baigi A., Fridlund B., Marklund B., Oden A. Cardiovascular mortality focusing on socio-economic influence: The low-risk population of Halland compared to the population of Sweden as a whole. Public Health. 2002;116(5):285–288. doi: 10.1038/sj.ph.1900877. [DOI] [PubMed] [Google Scholar]
- Baigi A., Marklund B., Fridlund B. The association between socio-economic status and chest pain, focusing on self-rated health in a primary health care area of Sweden. The European Journal of Public Health. 2001;11(4):420–424. doi: 10.1093/eurpub/11.4.420. [DOI] [PubMed] [Google Scholar]
- Bakirci N., Kalaca S., Francis H., Fletcher A.M., Pickering C.A.C., Tumerdem N., Niven R. Natural history and risk factors of early respiratory responses to exposure to cotton dust in newly exposed workers. Journal of Occupational and Environmental Medicine. 2007;49(8):853–861. doi: 10.1097/JOM.0b013e3180dca598. [DOI] [PubMed] [Google Scholar]
- Bennett G.G., Wolin K.Y., James S.A. Lifecourse socioeconomic position and weight change among blacks: The Pitt County study. Obesity. 2007;15(1):172. doi: 10.1038/oby.2007.522. [DOI] [PubMed] [Google Scholar]
- Bentley R., Kavanagh A.M., Subramanian S., Turrell G. Area disadvantage, individual socio-economic position, and premature cancer mortality in Australia 1998 to 2000: A multilevel analysis. Cancer Causes & Control. 2008;19(2):183–193. doi: 10.1007/s10552-007-9084-7. [DOI] [PubMed] [Google Scholar]
- Berman E., Bound J., Griliches Z. Changes in the demand for skilled labor within US manufacturing: Evidence from the annual survey of manufacturers. The Quarterly Journal of Economics. 1994;109(2):367–397. [Google Scholar]
- Betenia N., Costello S., Eisen E.A. Risk of cervical cancer among female autoworkers exposed to metalworking fluids. Scandinavian Journal of Work, Environment & Health. 2012:78–83. doi: 10.5271/sjweh.3193. [DOI] [PubMed] [Google Scholar]
- Biron M., Bamberger P.A., Noyman T. Work-related risk factors and employee substance use: Insights from a sample of Israeli blue-collar workers. Journal of Occupational Health Psychology. 2011;16(2):247. doi: 10.1037/a0022708. [DOI] [PubMed] [Google Scholar]
- Björkstén M., Boquist B., Talbäck M., Edling C. Reported neck and shoulder problems in female industrial workers: The importance of factors at work and at home. International Journal of Industrial Ergonomics. 2001;27(3):159–170. [Google Scholar]
- Blue C.L. Women in nontraditional jobs. AAOHN Journal. 1993;41:235–240. [PubMed] [Google Scholar]
- Del Bono E., Weber A., Winter‐Ebmer R. Clash of career and family: Fertility decisions after job displacement. Journal of the European Economic Association. 2012;10(4):659–683. [Google Scholar]
- von Bonsdorff M.B., Seitsamo J., von Bonsdorff M.E., Ilmarinen J., Nygård C.-H., Rantanen T. Job strain among blue-collar and white-collar employees as a determinant of total mortality: A 28-year population-based follow-up. BMJ Open. 2012;2(2):e000860. doi: 10.1136/bmjopen-2012-000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Bonsdorff M.B., Seitsamo J., Ilmarinen J., Nygård C.-H., von Bonsdorff M.E., Rantanen T. Work ability in midlife as a predictor of mortality and disability in later life: A 28-year prospective follow-up study. Canadian Medical Association Journal. 2011;183(4):E235–E242. doi: 10.1503/cmaj.100713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockmann H., Müller R., Helmert U. Time to retire–Time to die? A prospective cohort study of the effects of early retirement on long-term survival. Social science & medicine. 2009;69(2):160–164. doi: 10.1016/j.socscimed.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Bromet E.J., Dew M.A., Parkinson D.K., Cohen S., Schwartz J.E. Effects of occupational stress on the physical and psychological health of women in a microelectronics plant. Social Science & Medicine. 1992;34(12):1377–1383. doi: 10.1016/0277-9536(92)90146-h. [DOI] [PubMed] [Google Scholar]
- Brown D.M., Picciotto S., Costello S., Neophytou A.M., Izano M.A., Ferguson J.M., Eisen E.A. The healthy worker survivor effect: Target parameters and target populations. Current Environmental Health Reports. 2017;4(3):364–372. doi: 10.1007/s40572-017-0156-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunette M.J., Smith M.J., Punnett L. Perceptions of working and living conditions among industrial male and female workers in Perú. Work. 2011;38(3):211–223. doi: 10.3233/WOR-2011-1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton N.W., Turrell G. Occupation, hours worked, and leisure-time physical activity. Preventive Medicine. 2000;31(6):673–681. doi: 10.1006/pmed.2000.0763. [DOI] [PubMed] [Google Scholar]
- Cantley L.F., Tessier-Sherman B., Slade M.D., Galusha D., Cullen M.R. Expert ratings of job demand and job control as predictors of injury and musculoskeletal disorder risk in a manufacturing cohort. Occupational and Environmental Medicine. 2016;73(4):229–236. doi: 10.1136/oemed-2015-102831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsson G., Karlsson K. Age, cohorts and the generation of generations. American Sociological Review. 1970:710–718. [Google Scholar]
- Case A., Paxson C. Sex differences in morbidity and mortality. Demography. 2005;42(2):189–214. doi: 10.1353/dem.2005.0011. [DOI] [PubMed] [Google Scholar]
- Catalano R., Bruckner T. Secondary sex ratios and male lifespan: Damaged or culled cohorts. Proceedings of the National Academy of Sciences. 2006;103(5):1639–1643. doi: 10.1073/pnas.0510567103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Social Development, Humanitarian Affairs, UNICEF, United Nations Population Fund, United Nations Development Fund for Women, United Nations Statistical Division, United Nations Office for Project Services, World Food Programme, Inter-parliamentary Union, World Health Organization. The World's Women 2015: Trends and Statistics. 〈https://unstats.un.org/unsd/gender/worldswomen.html〉 Accessed 13 July 2018.
- Chenet L., Leon D., McKee M., Vassin S. Deaths from alcohol and violence in Moscow: socio-economic determinants. European Journal of Population. 1998;14(1):19–37. doi: 10.1023/a:1006012620847. [DOI] [PubMed] [Google Scholar]
- Chin D.L., Hong O., Gillen M., Bates M.N., Okechukwu C.A. Occupational factors and smoking cessation among unionized building trades workers. Workplace Health & Safety. 2012;60(10):445–452. doi: 10.1177/216507991206001006. [DOI] [PubMed] [Google Scholar]
- Chin D.L., Hong O., Gillen M., Bates M.N., Okechukwu C.A. Cigarette smoking in building trades workers: The impact of work environment. American Journal of Industrial Medicine. 2012;55(5):429–439. doi: 10.1002/ajim.22031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin D.L., Hong O., Gillen M., Bates M.N., Okechukwu C.A. Heavy and light/moderate smoking among building trades construction workers. Public Health Nursing. 2013;30(2):128–139. doi: 10.1111/j.1525-1446.2012.01041.x. [DOI] [PubMed] [Google Scholar]
- Cho C.-M., Lee Y.-M. The relationship between cardiovascular disease risk factors and gender. Health. 2012;4(06):309. [Google Scholar]
- Choi S.H., Terrell J.E., Pohl J.M., Redman R.W., Duffy S.A. Factors associated with sleep quality among operating engineers. Journal of Community Health. 2013;38(3):597–602. doi: 10.1007/s10900-013-9656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen K.B., Labriola M., Lund T., Kivimäki M. Explaining the social gradient in long-term sickness absence: A prospective study of Danish employees. Journal of Epidemiology and Community Health. 2008;62(2):181–183. doi: 10.1136/jech.2006.056135. [DOI] [PubMed] [Google Scholar]
- Cleland V.J., Schmidt M.D., Salmon J., Dwyer T., Venn A. Correlates of pedometer-measured and self-reported physical activity among young Australian adults. Journal of Science and Medicine in Sport. 2011;14(6):496–503. doi: 10.1016/j.jsams.2011.04.006. [DOI] [PubMed] [Google Scholar]
- Clougherty J.E., Eisen E.A., Slade M.D., Kawachi I., Cullen M.R. Gender and sex differences in job status and hypertension. Occupational and Environmental Medicine. 2011;68(1):16–23. doi: 10.1136/oem.2009.049908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty J.E., Souza K., Cullen M.R. Work and its role in shaping the social gradient in health. Annals of the New York Academy of Sciences. 2010;1186(1):102–124. doi: 10.1111/j.1749-6632.2009.05338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobankara V., Unal U.O., Kaya A., Bozkurt A.I., Ozturk M.A. The prevalence of fibromyalgia among textile workers in the city of Denizli in Turkey. International Journal of Rheumatic Diseases. 2011;14(4):390–394. doi: 10.1111/j.1756-185X.2011.01620.x. [DOI] [PubMed] [Google Scholar]
- Cocco P., Heineman E.F., Dosemeci M. Occupational risk factors for cancer of the central nervous system (CNS) among US women. American Journal of Industrial Medicine. 1999;36(1):70–74. doi: 10.1002/(sici)1097-0274(199907)36:1<70::aid-ajim10>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- Cohidon C., Diène E., Carton M., Fatras J.-Y., Goldberg M., Imbernon E. Mental health of workers in Toulouse 2 years after the industrial AZF disaster: First results of a longitudinal follow-up of 3000 people. Social Psychiatry and Psychiatric Epidemiology. 2009;44(9):784. doi: 10.1007/s00127-009-0500-z. [DOI] [PubMed] [Google Scholar]
- Colt J.S., Karagas M.R., Schwenn M., Baris D., Johnson A., Stewart P.…Ward M.H. Occupation and bladder cancer in a population-based case–control study in Northern New England. Occupational and Environmental Medicine. 2011;68(4):239–249. doi: 10.1136/oem.2009.052571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello S., Neophytou A.M., Brown D.M., Noth E.M., Hammond S.K., Cullen M.R., Eisen E.A. Incident ischemic heart disease after long-term occupational exposure to fine particulate matter: Accounting for 2 forms of survivor bias. American Journal of Epidemiology. 2016;183(9):861–868. doi: 10.1093/aje/kwv218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello S., Picciotto S., Rehkopf D.H., Eisen E.A. Social disparities in heart disease risk and survivor bias among autoworkers: an examination based on survival models and g-estimation. Occupational and Environmental Medicine. 2014 doi: 10.1136/oemed-2014-102168. oemed-2014-102168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courville J., Vézina N., Messing K. Comparison of the work activity of two mechanics: A woman and a man. International Journal of Industrial Ergonomics. 1991;7(2):163–174. [Google Scholar]
- Cullen M.R., Baiocchi M., Eggleston K., Loftus P., Fuchs V. National Bureau of Economic Research; 2015. The weaker sex? Vulnerable men, resilient women, and variations in sex differences in mortality since 1900. [Google Scholar]
- Cunradi C.B., Ames G.M., Xiao H. Binge drinking, smoking, and marijuana use: The role of women's labor force participation. Journal of Workplace Behavioral Health. 2014;29(3):210–223. doi: 10.1080/15555240.2014.928600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunradi C.B., Lipton R., Banerjee A. Occupational correlates of smoking among urban transit operators: A prospective study. Substance Abuse Treatment, Prevention, and Policy. 2007;2(1):36. doi: 10.1186/1747-597X-2-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta P., Baade P.D., Aitken J.F., Turrell G. Multilevel determinants of breast cancer survival: Association with geographic remoteness and area-level socioeconomic disadvantage. Breast Cancer Research and Treatment. 2012;132(2):701–710. doi: 10.1007/s10549-011-1899-y. [DOI] [PubMed] [Google Scholar]
- Duffy S.A., Cohen K.A., Choi S.H., McCullagh M.C., Noonan D. Predictors of obesity in Michigan operating engineers. Journal of Community Health. 2012;37(3):619–625. doi: 10.1007/s10900-011-9492-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Ehrenstein O.S., Wilhelm M., Wang A., Ritz B. Preterm birth and prenatal maternal occupation: The role of Hispanic ethnicity and nativity in a population-based sample in Los Angeles, California. American Journal of Public Health. 2014;104(S1):S65–S72. doi: 10.2105/AJPH.2013.301457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ericson U., Wirfält E., Mattisson I., Gullberg B., Skog K. Dietary intake of heterocyclic amines in relation to socio-economic, lifestyle and other dietary factors: Estimates in a Swedish population. Public Health Nutrition. 2007;10(06):616–627. doi: 10.1017/S1368980007352518. [DOI] [PubMed] [Google Scholar]
- Eshak E.S., Iso H., Mizoue T., Inoue M., Noda M., Tsugane S. Soft drink, 100% fruit juice, and vegetable juice intakes and risk of diabetes mellitus. Clinical Nutrition. 2013;32(2):300–308. doi: 10.1016/j.clnu.2012.08.003. [DOI] [PubMed] [Google Scholar]
- Eskenazi B., Guendelman S., Elkin E.P. A preliminary study of reproductive outcomes of female maquiladora workers in Tijuana, Mexico. American Journal of Industrial Medicine. 1993;24(6):667–676. doi: 10.1002/ajim.4700240603. [DOI] [PubMed] [Google Scholar]
- Evans B., Kell P., Bond R., MacRae K., Slomka M., Brown D. Predictors of seropositivity to herpes simplex virus type 2 in women. International Journal of STD & AIDS. 2003;14(1) doi: 10.1258/095646203321043237. [DOI] [PubMed] [Google Scholar]
- Forman-Hoffman V.L., Richardson K.K., Yankey J.W., Hillis S.L., Wallace R.B., Wolinsky F.D. Retirement and weight changes among men and women in the health and retirement study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2008;63(3):S146–S153. doi: 10.1093/geronb/63.3.s146. [DOI] [PubMed] [Google Scholar]
- Frankenhaeuser M., Lundberg U., Fredrikson B.M., Toumisto M., Myrsten A.L. Stress on and off the job as related to sex and occupational status in white-collar workers. Journal of Organizational Behaviour. 1989;10:321–346. [Google Scholar]
- Fredriksson K., Alfredsson L., Köster M., Thorbjörnsson C.B., Toomingas A., Torgén M., Kilbom A. Risk factors for neck and upper limb disorders: Results from 24 years of follow up. Occupational and Environmental Medicine. 1999;56(1):59–66. doi: 10.1136/oem.56.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frone M.R. Work–family conflict and employee psychiatric disorders: The national comorbidity survey. Journal of Applied Psychology. 2000;85(6):888–895. doi: 10.1037/0021-9010.85.6.888. [DOI] [PubMed] [Google Scholar]
- Fujishiro K., Diez-Roux A.V., Landsbergis P., Kaufman J.D., Korcarz C.E., Stein J.H. Occupational characteristics and the progression of carotid artery intima-media thickness and plaque over 9 years: The Multi-Ethnic Study of Atherosclerosis (MESA) Occupational and Environmental Medicine. 2015;72(10):690–698. doi: 10.1136/oemed-2014-102311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujishiro K., Stukovsky K.D.H., Diez-Roux A.V., Landsbergis P., Burchfiel C. Occupational gradients in smoking behavior and exposure to workplace environmental tobacco smoke: The Multi-Ethnic Study of Atherosclerosis (MESA) Journal of Occupational and Environmental Medicine. 2012;54(2):136. doi: 10.1097/JOM.0b013e318244501e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo L.C., Troxel W.M., Matthews K.A., Jansen-McWilliams L., Kuller L.H., Sutton-Tyrrell K. Occupation and subclinical carotid artery disease in women: Are clerical workers at greater risk? Health Psychology. 2003;22(1):19. [PubMed] [Google Scholar]
- Gang H., Pekkarinen H., Hänninen O., Yu Z., Huiguang T., Zeyu G., Nissinen A. Physical activity during leisure and commuting in Tianjin, China. Bulletin of the World Health Organization. 2002;80(12):933–938. [PMC free article] [PubMed] [Google Scholar]
- Gissler M., Rahkonen O., Arntzen A., Cnattingius S., Andersen A.-M.N., Hemminki E. Trends in socioeconomic differences in Finnish perinatal health 1991–2006. Journal of Epidemiology and Community Health. 2009 doi: 10.1136/jech.2008.079921. jech. 2008.079921. [DOI] [PubMed] [Google Scholar]
- Gold L.S., De Roos A.J., Ray R.M., Wernli K., Fitzgibbons E.D., Gao D.-L.…Checkoway H. Brain tumors and occupational exposures in a cohort of female textile workers in Shanghai, China. Scandinavian Journal of Work, Environment & Health. 2006:178–184. doi: 10.5271/sjweh.996. [DOI] [PubMed] [Google Scholar]
- Goldenhar L.M., Swanson N.G., Hurrell J.J., Ruder A., Deddens J. Stressors and adverse outcomes for female construction workers. Journal of Occupational Health Psychology. 1998;3(1):19. doi: 10.1037/1076-8998.3.1.19. [DOI] [PubMed] [Google Scholar]
- Grimmer K. Relationship between occupation and episodes of headache that match cervical origin pain patterns. Journal of Occupational and Environmental Medicine. 1993;35(9):929–935. doi: 10.1097/00043764-199309000-00017. [DOI] [PubMed] [Google Scholar]
- Guendelman S., Silberg M.J. The health consequences of maquiladora work: Women on the US-Mexican border. American Journal of Public Health. 1993;83(1):37–44. doi: 10.2105/ajph.83.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta N., Jensen B.S., Søgaard K., Carneiro I.G., Christiansen C.S., Hanisch C., Holtermann A. Face validity of the single work ability item: Comparison with objectively measured heart rate reserve over several days. International Journal of Environmental Research and Public Health. 2014;11(5):5333–5348. doi: 10.3390/ijerph110505333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall E.M., Johnson J.V., Tsou T.-S. Women, occupation, and risk of cardiovascular morbidity and mortality. Occupational Medicine. 1993;8(4):709–719. [PubMed] [Google Scholar]
- Hallman D.M., Gupta N., Mathiassen S.E., Holtermann A. Association between objectively measured sitting time and neck–shoulder pain among blue-collar workers. International Archives of Occupational and Environmental Health. 2015;88(8):1031–1042. doi: 10.1007/s00420-015-1031-4. [DOI] [PubMed] [Google Scholar]
- Hammar N., Alfredsson L., Theorrell T. Job characteristics and the incidence of myocardial infarction. International Journal of Epidemiology. 1994;23(2):277–284. doi: 10.1093/ije/23.2.277. [DOI] [PubMed] [Google Scholar]
- Hammarström A., Stenlund H., Janlert U. Mechanisms for the social gradient in health: Results from a 14-year follow-up of the Northern Swedish Cohort. Public Health. 2011;125(9):567–576. doi: 10.1016/j.puhe.2011.06.010. [DOI] [PubMed] [Google Scholar]
- Hanklang S., Kaewboonchoo O., Silpasuwan P., Mungarndee S.S. Musculoskeletal disorders among Thai women in construction-related work. Asia Pacific Journal of Public Health. 2014;26(2):196–202. doi: 10.1177/1010539512466429. [DOI] [PubMed] [Google Scholar]
- Harley A.E., Devine C.M., Beard B., Stoddard A.M., Hunt M.K., Sorensen G. Multiple health behavior changes in a cancer prevention intervention for construction workers, 2001–2003. Preventing Chronic Disease. 2010;7(3) [PMC free article] [PubMed] [Google Scholar]
- Heikkilä P., Martikainen R., Kurppa K., Husgafvel-Pursiainen K., Karjalainen A. Asthma incidence in wood-processing industries in Finland in a registerbased population study. Scandinavian Journal of Work, Environment & Health. 2008:66–72. doi: 10.5271/sjweh.1191. [DOI] [PubMed] [Google Scholar]
- Hein M.J., Stayner L., Lehman E., Dement J.M. Follow-up study of chrysotile textile workers: Cohort mortality and exposure-response. Occupational and Environmental Medicine. 2007 doi: 10.1136/oem.2006.031005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heo Y.-S., Leem J.-H., Park S.-G., Jung D.-Y., Kim H.-C. Job stress as a risk factor for absences among manual workers: A 12-month follow-up study. Industrial Health. 2015;53(6):542–552. doi: 10.2486/indhealth.2015-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirokawa K., Tsutsumi A., Kayaba K. Mortality risks in relation to occupational category and position among the Japanese working population: The Jichi Medical School (JMS) cohort study. BMJ Open. 2013;3(8):e002690. doi: 10.1136/bmjopen-2013-002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hocschild A., Machung A. Penguin Books; 2012. The second shift: Working families and the revolution at home. [Google Scholar]
- Honjo K., Tsutsumi A., Kayaba K., Group JMSCS Socioeconomic indicators and cardiovascular disease incidence among Japanese community residents: The Jichi Medical School Cohort Study. International Journal of Behavioral Medicine. 2010;17(1):58–66. doi: 10.1007/s12529-009-9051-7. [DOI] [PubMed] [Google Scholar]
- House J.S. Survey Research Center, Institute for Social REsearch, Univeristy of Michigan; 1980. Occupational stress and the mental and physical health of factory workers. [Google Scholar]
- Howard J., Piacentino J., MacMahon K., Schulte P. Using systematic review in occupational safety and health. American Journal of Industrial Medicine. 2017;60(11):921–929. doi: 10.1002/ajim.22771. [DOI] [PubMed] [Google Scholar]
- Hrubá F., Fabiánová E., Bencko V., Cassidy A., Lissowska J., Mates D.…Janout V. Socioeconomic indicators and risk of lung cancer in Central and Eastern Europe. Central European Journal of Public Health. 2009;17(3):115. doi: 10.21101/cejph.a3516. [DOI] [PubMed] [Google Scholar]
- Hwang W.J., Hong O.S., Rankin S.H. Predictors of health-promoting behavior associated with cardiovascular diseases among Korean blue-collar workers. Asia Pacific Journal of Public Health. 2015;27(2):NP691–NP702. doi: 10.1177/1010539513500338. [DOI] [PubMed] [Google Scholar]
- Hwang W.J., Lee C.Y. Effect of psychosocial factors on metabolic syndrome in male and female blue‐collar workers. Japan Journal of Nursing Science. 2014;11(1):23–34. doi: 10.1111/j.1742-7924.2012.00226.x. [DOI] [PubMed] [Google Scholar]
- Iverson R.D., Erwin P.J. Predicting occupational injury: The role of affectivity. Journal of Occupational and Organizational Psychology. 1997;70(2):113–128. [Google Scholar]
- Jakobsson K., Mikoczy Z. Reproductive outcome in a cohort of male and female rubber workers: A registry study. International Archives of Occupational and Environmental Health. 2009;82(2):165–174. doi: 10.1007/s00420-008-0318-0. [DOI] [PubMed] [Google Scholar]
- Jousilahti P., Vartiainen E., Tuomilehto J., Puska P. Symptoms of chronic bronchitis and the risk of coronary disease. The Lancet. 1996;348(9027):567–572. doi: 10.1016/S0140-6736(96)02374-4. [DOI] [PubMed] [Google Scholar]
- Juutilainen J., Stevens R.G., Anderson L.E., Hansen N.H., Kilpeläinen M., Kumlin T.…Wilson B.W. Nocturnal 6‐hydroxymelatonin sulfate excretion in female workers exposed to magnetic fields. Journal of Pineal Research. 2000;28(2):97–104. doi: 10.1034/j.1600-079x.2001.280205.x. [DOI] [PubMed] [Google Scholar]
- Kaergaard A., Andersen J.H. Musculoskeletal disorders of the neck and shoulders in female sewing machine operators: Prevalence, incidence, and prognosis. Occupational and Environmental Medicine. 2000;57(8):528–534. doi: 10.1136/oem.57.8.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaila-Kangas L., Keskimäki I., Notkola V., Mutanen P., Riihimäki H., Leino-Arjas P. How consistently distributed are the socioeconomic differences in severe back morbidity by age and gender? A population based study of hospitalisation among Finnish employees. Occupational and Environmental Medicine. 2006;63(4):278–282. doi: 10.1136/oem.2005.021642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalleberg A.L. Precarious work, insecure workers: Employment relations in transition. American Sociological Review. 2009;74:1–22. [Google Scholar]
- Kalleberg A.L. Job quality and precarious work: Clarifications, controversies, and challenges. Work and Occupations. 2012;39(4):427–448. [Google Scholar]
- Karasek R.A. Job demands, job decision latitude, and mental strain: Implications for job redesign. Administrative Science Quarterly. 1979:285–308. [Google Scholar]
- Kåreholt I. The relationship between heart problems and mortality in different social classes. Social Science & Medicine. 2001;52(9):1391–1402. doi: 10.1016/s0277-9536(00)00246-x. [DOI] [PubMed] [Google Scholar]
- Khatun M., Ahlgren C., Hammarström A. The influence of factors identified in adolescence and early adulthood on social class inequities of musculoskeletal disorders at age 30: A prospective population-based cohort study. International Journal of Epidemiology. 2004;33(6):1353–1360. doi: 10.1093/ije/dyh237. [DOI] [PubMed] [Google Scholar]
- Kim H.-C., Park S.-G., Min K.-B., Yoon K.-J. Depressive symptoms and self-reported occupational injury in small and medium-sized companies. International Archives of Occupational and Environmental Health. 2009;82(6):715. doi: 10.1007/s00420-008-0365-6. [DOI] [PubMed] [Google Scholar]
- Kivimäki M., Honkonen T., Wahlbeck K., Elovainio M., Pentti J., Klaukka T.…Vahtera J. Organisational downsizing and increased use of psychotropic drugs among employees who remain in employment. Journal of Epidemiology & Community Health. 2007;61(2):154–158. doi: 10.1136/jech.2006.050955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki M., Kalimo R. Self-esteem and the occupational stress process: Testing two alternative models in a sample of blue-collar workers. Journal of Occupational Health Psychology. 1996;1(2):187–196. doi: 10.1037//1076-8998.1.2.187. [DOI] [PubMed] [Google Scholar]
- Klumb P.L., Lampert T. Women, work, and well-being 1950–2000: A review and methodological critique. Social Science & Medicine. 2004;58(6):1007–1024. doi: 10.1016/s0277-9536(03)00262-4. [DOI] [PubMed] [Google Scholar]
- Kongerud J., Soyseth V. Methacholine responsiveness, respiratory symptoms and pulmonary function in aluminum potroom workers. European Respiratory Journal. 1991;4(2):159–166. [PubMed] [Google Scholar]
- Korda R.J., Strazdins L., Broom D.H., Lim L.L.Y. The health of the Australian workforce: 1998–2001. Australian and New Zealand Journal of Public Health. 2002;26(4):325–331. doi: 10.1111/j.1467-842x.2002.tb00179.x. [DOI] [PubMed] [Google Scholar]
- Kovacevic M., Belojevic G. Tooth abrasion in workers exposed to noise in the Montenegrin textile industry. Industrial Health. 2006;44(3):481–485. doi: 10.2486/indhealth.44.481. [DOI] [PubMed] [Google Scholar]
- Krieger N. Genders, sexes, and health: What are the connections—and why does it matter? International Journal of Epidemiology. 2003;32(4):652–657. doi: 10.1093/ije/dyg156. [DOI] [PubMed] [Google Scholar]
- Kubo J.T., Cullen M.R., Desai M., Modrek S. Associations between employee and manager gender: impacts on gender-specific risk of acute occupational injury in metal manufacturing. BMC Public Health. 2013;13(1):1053. doi: 10.1186/1471-2458-13-1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiack S., Irving H., Faulkner G. Occupation, hours worked, caregiving, and leisure time physical activity. Michigan Family Review. 2007;12(1) [Google Scholar]
- Lalive R., Zweimüller J. How does parental leave affect fertility and return to work? Evidence from two natural experiments. The Quarterly Journal of Economics. 2009;124(3):1363–1402. [Google Scholar]
- Landefeld J.C., Burmaster K.B., Rehkopf D.H., Syme S.L., Lahiff M., Adler-Milstein S., Fernald L.C. The association between a living wage and subjective social status and self-rated health: A quasi-experimental study in the Dominican Republic. Social Science & Medicine. 2014;121:91–97. doi: 10.1016/j.socscimed.2014.09.051. [DOI] [PubMed] [Google Scholar]
- Lea C.S., Hertz-Picciotto I., Andersen A., Chang-Claude J., Olsen J.H., Pesatori A.C.…Boffetta P. Gender differences in the healthy worker effect among synthetic vitreous fiber workers. American Journal of Epidemiology. 1999;150(10):1099–1106. doi: 10.1093/oxfordjournals.aje.a009935. [DOI] [PubMed] [Google Scholar]
- Lederer M. Blue-collar jobs for women. National Forum. 1981;61(4):20. [Google Scholar]
- Lewin A., Pannier B., Méline J., Karusisi N., Thomas F., Chaix B. Residential neighborhood, geographic work environment, and work economic sector: associations with body fat measured by bioelectrical impedance in the RECORD Study. Annals of Epidemiology. 2014;24(3):180–186. doi: 10.1016/j.annepidem.2013.12.001. [DOI] [PubMed] [Google Scholar]
- Lin Y.-C., Chen Y.-C., Hsieh H.-I., Chen P.-C. Risk for work-related fatigue among the employees on semiconductor manufacturing lines. Asia Pacific Journal of Public Health. 2015;27(2):NP1805–NP1818. doi: 10.1177/1010539513490788. [DOI] [PubMed] [Google Scholar]
- Lipscomb H.J., Schoenfisch A., Cameron W. Work-related injuries involving a hand or fingers among union carpenters in Washington State, 1989 to 2008. Journal of Occupational and Environmental Medicine. 2013;55(7):832–838. doi: 10.1097/JOM.0b013e31828dc969. [DOI] [PubMed] [Google Scholar]
- Lipton R., Cunradi C., Chen M.-J. Smoking and all-cause mortality among a cohort of urban transit operators. Journal of Urban Health. 2008;85(5):759–765. doi: 10.1007/s11524-008-9295-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardo S.R., Vijitha de Silva P., Lipscomb H.J., Østbye T. Musculoskeletal symptoms among female garment factory workers in Sri Lanka. International Journal of Occupational and Environmental health. 2012;18(3):210–219. doi: 10.1179/1077352512Z.00000000029. [DOI] [PubMed] [Google Scholar]
- Van Loon A., Van den Brandt P., Golbohm R. Socioeconomic status and colon cancer incidence: A prospective cohort study. British Journal of Cancer. 1995;71(4):882. doi: 10.1038/bjc.1995.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Loon A.J.M., Goldbohm R.A., Van Den Brandt P.A. Socioeconomic status and breast cancer incidence: A prospective cohort study. International Journal of Epidemiology. 1994;23(5):899–905. doi: 10.1093/ije/23.5.899. [DOI] [PubMed] [Google Scholar]
- Loscocco K.A., Spitze G. Working conditions, social support, and the well-being of female and male factory workers. Journal of Health and Social Behavior. 1990:313–327. [PubMed] [Google Scholar]
- Love R., Muirhead M., Collins H., Soutar C. The characteristics of respiratory ill health of wool textile workers. Occupational and Environmental Medicine. 1991;48(4):221–228. doi: 10.1136/oem.48.4.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luoto R., Kaprio J., Uutela A. Age at natural menopause and sociodemographic status in Finland. American Journal of Epidemiology. 1994;139(1):64–76. doi: 10.1093/oxfordjournals.aje.a116936. [DOI] [PubMed] [Google Scholar]
- Mäkinen T., Kestilä L., Borodulin K., Martelin T., Rahkonen O., Leino-Arjas P., Prättälä R. Occupational class differences in leisure-time physical inactivity-contribution of past and current physical workload and other working conditions. Scandinavian Journal of Work, Environment & Health. 2010:62–70. doi: 10.5271/sjweh.2879. [DOI] [PubMed] [Google Scholar]
- Mammen K., Paxson C. Women's work and economic development. The Journal of Economic Perspectives. 2000;14(4):141–164. [Google Scholar]
- Mamo C., Marinacci C., Demaria M., Mirabelli D., Costa G. Factors other than risks in the workplace as determinants of socioeconomic differences in health in Italy. International Journal of Occupational and Environmental Health. 2005;11(1):70–76. doi: 10.1179/oeh.2005.11.1.70. [DOI] [PubMed] [Google Scholar]
- Maron J., Kraus L., Pogarell O., Gomes de Matos E., Piontek D. Occupational inequalities in psychoactive substance use: A question of conceptualization? Addiction Research & Theory. 2016;24(3):186–198. [Google Scholar]
- Mattioli S., Baldasseroni A., Curti S., Cooke R.M., Mandes A., Zanardi F.…Violante F. Incidence rates of surgically treated idiopathic carpal tunnel syndrome in blue-and white-collar workers and housewives in Tuscany, Italy. Occupational and Environmental Medicine. 2009;66(5):299–304. doi: 10.1136/oem.2008.040212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattisson C., Horstmann V., Bogren M. Relationship of SOC with sociodemographic variables, mental disorders and mortality. Scandinavian Journal of Public Health. 2014;42(5):434–445. doi: 10.1177/1403494814527188. [DOI] [PubMed] [Google Scholar]
- Maty S.C., Everson-Rose S.A., Haan M.N., Raghunathan T.E., Kaplan G.A. Education, income, occupation, and the 34-year incidence (1965–99) of type 2 diabetes in the Alameda County Study. International Journal of Epidemiology. 2005;34(6):1274–1281. doi: 10.1093/ije/dyi167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack G., Giles-Corti B., Milligan R. Demographic and individual correlates of achieving 10,000 steps/day: Use of pedometers in a population-based study. Health Promotion Journal of Australia. 2006;17(1):43–47. doi: 10.1071/he06043. [DOI] [PubMed] [Google Scholar]
- Melamed S., Ben-Avi I., Luz J., Green M.S. Objective and subjective work monotony: Effects on job satisfaction, psychological distress, and absenteeism in blue-collar workers. Journal of Applied Psychology. 1995;80(1):29. doi: 10.1037/0021-9010.80.1.29. [DOI] [PubMed] [Google Scholar]
- Melamed S., Froom P., Kristal-Boneh E., Gofer D., Ribak J. Industrial noise exposure, noise annoyance, and serum lipid levels in blue-collar workers–the CORDIS Study. Archives of Environmental Health: An International Journal. 1997;52(4):292–298. doi: 10.1080/00039899709602201. [DOI] [PubMed] [Google Scholar]
- Messing K., Ostlin P. Gender equality, work, and health: A review of the evidence. 〈http://www.who.int/occupational_health/publications/genderwork/en/〉 Accessed 13 July 2018.
- Messing K., Stevenson J. Women in procrustean beds: Strength testing and the workplace. Gender Work & Organization. 1996;3(3):156–167. [Google Scholar]
- Minh K. Work-related depression and associated factors in a shoe manufacturing factory in Haiphong City, Vietnam. International Journal of Occupational Medicine and Environmental Health. 2014;27(6):950–958. doi: 10.2478/s13382-014-0323-3. [DOI] [PubMed] [Google Scholar]
- Miura K., Turrell G. Reported consumption of takeaway food and its contribution to socioeconomic inequalities in body mass index. Appetite. 2014;74:116–124. doi: 10.1016/j.appet.2013.12.007. [DOI] [PubMed] [Google Scholar]
- Moon S.-S., Park S.-M. Risk factors for suicidal ideation in Korean middle-aged adults: The role of socio-demographic status. International Journal of Social Psychiatry. 2012;58(6):657–663. doi: 10.1177/0020764011433626. [DOI] [PubMed] [Google Scholar]
- Motamedzade M., Moghimbeigi A. Musculoskeletal disorders among female carpet weavers in Iran. Ergonomics. 2012;55(2):229–236. doi: 10.1080/00140139.2011.582539. [DOI] [PubMed] [Google Scholar]
- Murata K., Kawakami N., Amari N. Does job stress affect injury due to labor accident in Japanese male and female blue-collar workers? Industrial Health. 2000;38(2):246–251. doi: 10.2486/indhealth.38.246. [DOI] [PubMed] [Google Scholar]
- Nag A., Vyas H., Nag P. Gender differences, work stressors and musculoskeletal disorders in weaving industries. Industrial Health. 2010;48(3):339–348. doi: 10.2486/indhealth.48.339. [DOI] [PubMed] [Google Scholar]
- Nakamura S., Nakamura K., Tanaka M. Increased risk of coronary heart disease in Japanese blue-collar workers. Occupational Medicine. 2000;50(1):11–17. doi: 10.1093/occmed/50.1.11. [DOI] [PubMed] [Google Scholar]
- Nakata A., Ikeda T., Takahashi M., Haratani T., Hojou M., Swanson N.G.…Araki S. The prevalence and correlates of occupational injuries in small-scale manufacturing enterprises. Journal of Occupational Health. 2006;48(5):366–376. doi: 10.1539/joh.48.366. [DOI] [PubMed] [Google Scholar]
- Navarro V. The labor process and health: A historical materialist interpretation. International Journal of Health Services. 1982;12(1):5–29. doi: 10.2190/MVRB-XD8G-RTM6-05KP. [DOI] [PubMed] [Google Scholar]
- Nguyen A.L., Van Le. T., Hoang M.H., Nguyen S., Jonai H., Villanueva M.B.G.…Sudo A. Noise levels and hearing ability of female workers in a textile factory in Vietnam. Industrial Health. 1998;36(1):61–65. doi: 10.2486/indhealth.36.61. [DOI] [PubMed] [Google Scholar]
- Niedhammer I., Chastang J.-F., David S., Kelleher C. The contribution of occupational factors to social inequalities in health: Findings from the national French SUMER survey. Social Science & Medicine. 2008;67(11):1870–1881. doi: 10.1016/j.socscimed.2008.09.007. [DOI] [PubMed] [Google Scholar]
- Noonan D., Duffy S.A. Smokeless tobacco use among operating engineers. Journal of Addictions Nursing. 2012;23(2):132–136. doi: 10.3109/10884602.2012.669421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oddone E., Edefonti V., Scaburri A., Vai T., Bai E., Modonesi C.…Imbriani M. Female breast cancer and electrical manufacturing: results of a nested case-control study. Journal of Occupational Health. 2014;56(5):369–378. doi: 10.1539/joh.14-0034-oa. [DOI] [PubMed] [Google Scholar]
- Oddone E., Edefonti V., Scaburri A., Vai T., Crosignani P., Imbriani M. Female breast cancer in Lombardy, Italy (2002–2009): A case–control study on occupational risks. American Journal of Industrial Medicine. 2013;56(9):1051–1062. doi: 10.1002/ajim.22205. [DOI] [PubMed] [Google Scholar]
- O’Farrell B. Women in blue collar and related occupations at the end of the millennium. The Quarterly Review of Economics and Finance. 1999;39(5):699–722. [Google Scholar]
- Okechukwu C., Bacic J., Cheng K.-W., Catalano R. Smoking among construction workers: The nonlinear influence of the economy, cigarette prices, and antismoking sentiment. Social Science & Medicine. 2012;75(8):1379–1386. doi: 10.1016/j.socscimed.2012.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okechukwu C.A., Nguyen K., Hickman N.J. Partner smoking characteristics: Associations with smoking and quitting among blue‐collar apprentices. American Journal of Industrial Medicine. 2010;53(11):1102–1108. doi: 10.1002/ajim.20890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira A., Maia B., Lopes C. Determinants of inadequate fruit and vegetable consumption amongst Portuguese adults. Journal of Human Nutrition and Dietetics. 2014;27(s2):194–203. doi: 10.1111/jhn.12143. [DOI] [PubMed] [Google Scholar]
- Ostlin P., Alfredsson L., Hammar N., Reuterwall C. Myocardial infarction in male and female dominated occupations. Occupational and Environmental Medicine. 1998;55(9):642–644. doi: 10.1136/oem.55.9.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pant A., Kanato M., Thapa P., Ratanasiri A. Knowledge of and attitude towards HIV/AIDS and condom use among construction workers in the Kathmandu Valley, Nepal. Journal of the Medical Association of Thailand. 2013;96:S107–16. [PubMed] [Google Scholar]
- Parkinson D.K., Bromet E.J., Cohen S., Dunn L.O., Dew M.A., Ryan C., Schwartz J.E. Health effects of long‐term solvent exposure among women in blue‐collar occupations. American Journal of Industrial Medicine. 1990;17(6):661–675. doi: 10.1002/ajim.4700170602. [DOI] [PubMed] [Google Scholar]
- Pekkanen J., Tuomilehto J., Uutela A., Vartiainen E., Nissinen A. Social class, health behaviour, and mortality among men and women in eastern Finland. BMJ. 1995;311(7005):589–593. doi: 10.1136/bmj.311.7005.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack K.M., Agnew J., Slade M.D., Cantley L., Taiwo O., Vegso S.…Cullen M.R. Use of employer administrative databases to identify systematic causes of injury in aluminum manufacturing. American Journal of Industrial Medicine. 2007;50(9):676–686. doi: 10.1002/ajim.20493. [DOI] [PubMed] [Google Scholar]
- Pollán M., Gustavsson P. High-risk occupations for breast cancer in the Swedish female working population. American Journal of Public Health. 1999;89(6):875–881. doi: 10.2105/ajph.89.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potula V., Kaye W. The impact of menopause and lifestyle factors on blood and bone lead levels among female former smelter workers: The Bunker Hill Study. American Journal of Industrial Medicine. 2006;49(3):143–152. doi: 10.1002/ajim.20262. [DOI] [PubMed] [Google Scholar]
- Prescott E., Godtfredsen N., Vestbo J., Osler M. Social position and mortality from respiratory diseases in males and females. European Respiratory Journal. 2003;21(5):821–826. doi: 10.1183/09031936.03.00047502. [DOI] [PubMed] [Google Scholar]
- Pudrovska T., Carr D., McFarland M., Collins C. Higher-status occupations and breast cancer: A life-course stress approach. Social Science & Medicine. 2013;89:53–61. doi: 10.1016/j.socscimed.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radi S., Ostry A., LaMontagne A.D. Job stress and other working conditions: Relationships with smoking behaviors in a representative sample of working Australians. American Journal of Industrial Medicine. 2007;50(8):584–596. doi: 10.1002/ajim.20492. [DOI] [PubMed] [Google Scholar]
- Räisänen S., Gissler M., Kramer M.R., Heinonen S. Influence of delivery characteristics and socioeconomic status on giving birth by caesarean section – A cross sectional study during 2000–2010 in Finland. BMC Pregnancy and Childbirth. 2014;14(1):120. doi: 10.1186/1471-2393-14-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raza S., Fletcher A., Pickering C., Niven R.M., Faragher E. Ventilatory function and personal breathing zone dust concentrations in Lancashire textile weavers. Occupational and Environmental Medicine. 1999;56(8):520–526. doi: 10.1136/oem.56.8.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richiardi L., Boffetta P., Simonato L., Forastiere F., Zambon P., Fortes C., Gaborieau V., Merletti F. Occupational risk factors for lung cancer in men and women: A population-based case–control study in Italy. Cancer Causes & Control. 2004;15(3):285–294. doi: 10.1023/B:CACO.0000024223.91059.ed. [DOI] [PubMed] [Google Scholar]
- Rieker P.P., Bird C.E. Rethinking gender differences in health: Why we need to integrate social and biological perspectives. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(Special Issue 2):S40–S47. doi: 10.1093/geronb/60.special_issue_2.s40. [DOI] [PubMed] [Google Scholar]
- Roquelaure Y., Ha C., Fouquet N., Descatha A., Leclerc A., Goldberg M.…Imbernon E. Attributable risk of carpal tunnel syndrome in the general population: Implications for intervention programs in the workplace. Scandinavian Journal of Work, Environment & Health. 2009;35(5):342. doi: 10.5271/sjweh.1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roquelaure Y., Ha C., Pelier‐Cady M.C., Nicolas G., Descatha A., Leclerc A., Imbernon E. Work increases the incidence of carpal tunnel syndrome in the general population. Muscle & Nerve. 2008;37(4):477–482. doi: 10.1002/mus.20952. [DOI] [PubMed] [Google Scholar]
- Rydstedt L.W., Johansson G., Evans G.W. A longitudinal study of workload, health and well‐being among male and female urban bus drivers. Journal of Occupational and Organizational Psychology. 1998;71(1):35–45. [Google Scholar]
- Sakr C.J., Taiwo O.A., Galusha D.H., Slade M.D., Fiellin M.G., Bayer F.…Cullen M.R. Reproductive outcomes among male and female workers at an aluminum smelter. Journal of Occupational and Environmental Medicine. 2010;52(2):137. doi: 10.1097/JOM.0b013e3181cb59bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santhi N., Lazar A.S., McCabe P.J., Lo J.C., Groeger J.A., Dijk D.-J. Sex differences in the circadian regulation of sleep and waking cognition in humans. Proceedings of the National Academy of Sciences. 2016;113(19):E2730–E2739. doi: 10.1073/pnas.1521637113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos A.-C., Barros H. Prevalence and determinants of obesity in an urban sample of Portuguese adults. Public Health. 2003;117(6):430–437. doi: 10.1016/S0033-3506(03)00139-2. [DOI] [PubMed] [Google Scholar]
- Sayem A. An assessment of risk behaviours for HIV/AIDS among young female garment workers in Bangladesh. International Journal of STD & AIDS. 2010;21(2):133–137. doi: 10.1258/ijsa.2008.008455. [DOI] [PubMed] [Google Scholar]
- Seldén A., Berg N., Lundgren E., Hillerdal G., Wik N., Ohlson C., Bodin L. Exposure to tremolite asbestos and respiratory health in Swedish dolomite workers. Occupational and Environmental Medicine. 2001;58(10):670–677. doi: 10.1136/oem.58.10.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan M.C., Lam J. Use of systematic review and meta-analysis in environmental health epidemiology: A systematic review and comparison with guidelines. Current Environmental Health Reports. 2015;2(3):272–283. doi: 10.1007/s40572-015-0062-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirom A., Melamed S., Nir-Dotan M. The relationships among objective and subjective environmental stress levels and serum uric acid: The moderating effect of perceived control. Journal of Occupational Health Psychology. 2000;5(3):374. doi: 10.1037//1076-8998.5.3.374. [DOI] [PubMed] [Google Scholar]
- Soares J., Grossi G., Sundin Ö. Burnout among women: Associations with demographic/socio-economic, work, life-style and health factors. Archives of Women's Mental Health. 2007;10(2):61–71. doi: 10.1007/s00737-007-0170-3. [DOI] [PubMed] [Google Scholar]
- Stokholm Z.A., Bonde J.P., Christensen K.L., Hansen Å.M., Kolstad H.A. Occupational noise exposure and the risk of hypertension. Epidemiology. 2013;24(1):135–142. doi: 10.1097/EDE.0b013e31826b7f76. [DOI] [PubMed] [Google Scholar]
- Storaas T., Zock J.-P., Morano A.E., Holm M., Bjørnsson E., Forsberg B.…Omenaas E. Incidence of rhinitis and asthma related to welding in Northern Europe. European Respiratory Journal. 2015 doi: 10.1183/13993003.02345-2014. ERJ-02345-2014. [DOI] [PubMed] [Google Scholar]
- Strong L.L., Zimmerman F.J. Occupational injury and absence from work among African American, Hispanic, and non-Hispanic White workers in the national longitudinal survey of youth. American Journal of Public Health. 2005;95(7):1226–1232. doi: 10.2105/AJPH.2004.044396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taiwo O.A., Cantley L.F., Slade M.D., Pollack K.M., Vegso S., Fiellin M.G., Cullen M.R. Sex differences in injury patterns among workers in heavy manufacturing. American Journal of Epidemiology. 2008;169(2):161–166. doi: 10.1093/aje/kwn304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takao S., Kawakami N., Ohtsu T. Occupational class and physical activity among Japanese employees. Social Science & Medicine. 2003;57(12):2281–2289. doi: 10.1016/s0277-9536(03)00134-5. [DOI] [PubMed] [Google Scholar]
- Takezaki T., Hirose K., Inoue M., Hamajima N., Yatabe Y., Mitsudomi T.…Tajima K. Dietary factors and lung cancer risk in Japanese: With special reference to fish consumption and adenocarcinomas. British Journal of Cancer. 2001;84(9):1199. doi: 10.1054/bjoc.2001.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessier-Sherman B., Cantley L.F., Galusha D., Slade M.D., Taiwo O.A., Cullen M.R. Occupational injury risk by sex in a manufacturing cohort. Occupational and Environmental Medicine. 2014 doi: 10.1136/oemed-2014-102083. oemed-2014-102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thilsing T., Rasmussen J., Lange B., Kjeldsen A.D., Al‐Kalemji A., Baelum J. Chronic rhinosinusitis and occupational risk factors among 20‐to 75‐year‐old Danes—A GA2LEN‐based study. American Journal of Industrial Medicine. 2012;55(11):1037–1043. doi: 10.1002/ajim.22074. [DOI] [PubMed] [Google Scholar]
- Thompson D., Kriebel D., Quinn M.M., Wegman D.H., Eisen E.A. Occupational exposure to metalworking fluids and risk of breast cancer among female autoworkers. American Journal of Industrial Medicine. 2005;47(2):153–160. doi: 10.1002/ajim.20132. [DOI] [PubMed] [Google Scholar]
- Tsai S.-Y., Chen J.-D., Chao W.-Y., Wang J.-D. Neurobehavioral effects of occupational exposure to low-level organic solvents among Taiwanese workers in paint factories. Environmental Research. 1997;73(1–2):146–155. doi: 10.1006/enrs.1997.3704. [DOI] [PubMed] [Google Scholar]
- Tsutsumi A., Kayaba K., Ishikawa S. Impact of occupational stress on stroke across occupational classes and genders. Social Science & Medicine. 2011;72(10):1652–1658. doi: 10.1016/j.socscimed.2011.03.026. [DOI] [PubMed] [Google Scholar]
- Tsutsumi A., Kayaba K., Tsutsumi K., Igarashi M. Association between job strain and prevalence of hypertension: A cross sectional analysis in a Japanese working population with a wide range of occupations: The Jichi Medical School cohort study. Occupational and Environmental Medicine. 2001;58(6):367–373. doi: 10.1136/oem.58.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uijtdewilligen L., Peeters G.M., Van Uffelen J.G., Twisk J.W., Singh A.S., Brown W.J. Determinants of physical activity in a cohort of young adult women. Who is at risk of inactive behaviour? Journal of Science and Medicine in Sport. 2015;18(1):49–55. doi: 10.1016/j.jsams.2014.02.005. [DOI] [PubMed] [Google Scholar]
- Uijtdewilligen L., Twisk J.W., Singh A.S., Chinapaw M.J., van Mechelen W., Brown W.J. Biological, socio-demographic, work and lifestyle determinants of sitting in young adult women: A prospective cohort study. International Journal of Behavioral Nutrition and Physical Activity. 2014;11(1):7. doi: 10.1186/1479-5868-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Census Bureau. North American industry classification system. 〈https://www.census.gov/eos/www/naics/2017NAICS/2017_NAICS_Manual.pdf〉 Accessed 13 July 2017.
- U.S. Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey. 〈https://www.bls.gov/cps/cpsaat18.htm〉 Accessed 13 July 2018.
- Väänänen A., Kalimo R., Toppinen-Tanner S., Mutanen P., Peiró J.M., Kivimäki M., Vahtera J. Role clarity, fairness, and organizational climate as predictors of sickness absence: A prospective study in the private sector. Scandinavian Journal of Social Medicine. 2004;32(6):426–434. doi: 10.1080/14034940410028136. [DOI] [PubMed] [Google Scholar]
- Väänänen A., Kumpulainen R., Kevin M.V., Ala-Mursula L., Kouvonen A., Kivimäki M.…Vahtera J. Work-family characteristics as determinants of sickness absence: A large-scale cohort study of three occupational grades. Journal of Occupational Health Psychology. 2008;13(2):181. doi: 10.1037/1076-8998.13.2.181. [DOI] [PubMed] [Google Scholar]
- Vahtera J., Virtanen P., Kivimäki M., Pentti J. Workplace as an origin of health inequalities. Journal of Epidemiology and Community Health. 1999;53(7):399–407. doi: 10.1136/jech.53.7.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vingård E., Alfredsson L., Goldie I., Hogstedt C. Occupation and osteoarthrosis of the hip and knee: A register-based cohort study. International Journal of Epidemiology. 1991;20(4):1025–1031. doi: 10.1093/ije/20.4.1025. [DOI] [PubMed] [Google Scholar]
- Wamala S.P., Lynch J., Kaplan G.A. Women's exposure to early and later life socioeconomic disadvantage and coronary heart disease risk: The Stockholm Female Coronary Risk Study. International Journal of Epidemiology. 2001;30(2):275–284. doi: 10.1093/ije/30.2.275. [DOI] [PubMed] [Google Scholar]
- Wamala S.P., Wolk A., Schenck-Gustafsson K., Orth-Gomér K. Lipid profile and socioeconomic status in healthy middle aged women in Sweden. Journal of Epidemiology and Community Health. 1997;51(4):400–407. doi: 10.1136/jech.51.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Wang M., Cheng N., Zheng T., Hu X., Li H.…Bai Y. Sulfur dioxide exposure and other factors affecting age at natural menopause in the Jinchuan cohort. Climacteric. 2015;18(5):722–732. doi: 10.3109/13697137.2015.1015514. [DOI] [PubMed] [Google Scholar]
- Wang F., Zou Y., Shen Y., Zhong Y., Lv Y., Huang D.…Xia B. Synergistic impaired effect between smoking and manganese dust exposure on pulmonary ventilation function in Guangxi manganese-exposed workers healthy cohort (GXMEWHC) PLoS One. 2015;10(2):e0116558. doi: 10.1371/journal.pone.0116558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P.-C., Rempel D., Harrison R., Chan J., Ritz B. Work-organizational and personal factors associated with upper body musculoskeletal disorders among sewing machine operators. Occupational and Environmental Medicine. 2007 doi: 10.1136/oem.2006.029140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westgaard R., Jansen T. Individual and work related factors associated with symptoms of musculoskeletal complaints. II. Different risk factors among sewing machine operators. Occupational and Environmental Medicine. 1992;49(3):154–162. doi: 10.1136/oem.49.3.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westreich D., Greenland S. The Table 2 fallacy: Presenting and interpreting confounder and modifier coefficients. American Journal of Epidemiology. 2013;177(4):292–298. doi: 10.1093/aje/kws412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Won J.U., Hong O.S., Hwang W.J. Actual cardiovascular disease risk and related factors: a cross-sectional study of Korean blue collar workers employed by small businesses. Workplace Health & Safety. 2013;61(4):163–171. doi: 10.1177/216507991306100404. [DOI] [PubMed] [Google Scholar]
- World Bank. World Bank Country and Lending Groups. 〈https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups〉 Accessed 13 July 2018.
- Wu B., Porell F. Job characteristics and leisure physical activity. Journal of Aging and Health. 2000;12(4):538–559. doi: 10.1177/089826430001200405. [DOI] [PubMed] [Google Scholar]
- Yang S., Lynch J., Schulenberg J., Roux A.V.D., Raghunathan T. Emergence of socioeconomic inequalities in smoking and overweight and obesity in early adulthood: the national longitudinal study of adolescent health. American Journal of Public Health. 2008;98(3):468–477. doi: 10.2105/AJPH.2007.111609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yingying H., Smith K., Suiming P. Changes and correlates in multiple sexual partnerships among Chinese adult women–population-based surveys in 2000 and 2006. AIDS Care. 2011;23(sup1):96–104. doi: 10.1080/09540121.2010.516350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon J.-H., Won J.-U., Lee W., Jung P.K., Roh J. Occupational noise annoyance linked to depressive symptoms and suicidal ideation: A result from nationwide survey of Korea. PLoS One. 2014;9(8):e105321. doi: 10.1371/journal.pone.0105321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahm S.H., Pottern L.M., Lewis D.R., Ward M.H., White D.W. Inclusion of women and minorities in occupational cancer epidemiologic research. Journal of Occupational and Environmental Medicine. 1994;36(8):842–847. [PubMed] [Google Scholar]
- Zhang L., Narayanan K., Suryadevara V., Teodorescu C., Reinier K., Uy-Evanado A., Jui J. Occupation and risk of sudden death in a United States community: A case–control analysis. BMJ Open. 2015;5(12):e009413. doi: 10.1136/bmjopen-2015-009413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Zhang S., Selvin S., Spear R.C. A dose response relation for noise induced hypertension. Occupational and Environmental Medicine. 1991;48(3):179–184. doi: 10.1136/oem.48.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]