Abstract
Few studies have compared atypical sensory characteristics and food selectivity between children with and without autism spectrum disorder (ASD). We compared oral sensory processing between children with (n=53) and without ASD (n=58), ages 3–11 years. We also examined the relationships between atypical oral sensory processing, food selectivity, and fruit/vegetable consumption in children with ASD. We found that more children with ASD presented with atypical sensory processing than children without ASD. Among children with ASD, those with atypical oral sensory sensitivity refused more foods and ate fewer vegetables than those with typical oral sensory sensitivity. The findings suggest that efforts to address food selectivity in children with ASD may be enhanced by including strategies that address oral sensory processing.
Keywords: autism spectrum disorder, food selectivity, sensory sensitivity
Autism spectrum disorder is a developmental disability characterized by deficits in communication, social interaction, and restrictive, repetitive behavioral patterns that impair social, occupational, and daily functioning (American Psychiatric Association 2013). This disorder is also often associated with sensory processing difficulties, which includes over- or under-sensitivity to sensory stimuli in the environment. The prevalence of ASD in the United States is currently estimated to affect 1 in 68 children with higher rates among males and non-Hispanic whites (Christensen et al. 2016). ASD poses a major health and educational challenge for parents and caretakers as it affects many aspects of daily living. Feeding and mealtimes are especially challenging for these children and their caretakers (Curtin et al. 2015; Zobel-Lachiusa et al. 2015). Parents and clinicians frequently report that children with ASD are overly selective in their eating patterns; they consume less varied diets with very few fruits and vegetables (Ahearn et al. 2001; Bandini et al. 2010; Cermak et al. 2010; Emond et al. 2010; Johnson et al. 2008; Ledford & Gast 2006; Marí-Bauset et al. 2014; Martins et al. 2008; Ranjan & Nasser 2015; Schreck et al. 2004; Sharp et al. 2013; Zimmer et al. 2012). The lack of food variety may put individuals at risk for nutritional inadequacies (Bandini et al. 2010; Ma et al. 2016; Zimmer et al. 2012). One recent review estimated that children with ASD have a five-fold risk of feeding problems compared to children without ASD (Sharp et al. 2013). While longitudinal data are limited, two recent studies suggest that food selective behaviors may persist over time (Bandini et al. 2017; Suarez et al. 2014). Therefore, addressing the underlying factors associated with food selectivity may be necessary to mitigate the comorbidities associated with long-term inadequate nutritional intake in this population.
In recent years, it has been suggested that food selectivity in individuals with ASD may be related to sensory processing dysfunction, specifically oral sensory sensitivity (Cermak et al. 2010; Suarez 2012; Zobel-Lachiusa et al. 2015). Sensory processing refers to the ability to register, process, and organize sensory information and to execute appropriate responses to environmental demands, which may manifest as over- or under-sensitivity to the stimuli (Dunn, 2001). Atypical sensory processing has been a recognized feature of ASD since the condition was first described by Kanner (1943), occurring in 45–95% in persons with ASD (Ben-Sasson et al. 2009; Schreck & Williams 2006; Tomchek & Dunn 2007). Anecdotal reports from parents of children with ASD and autobiographies of individuals with ASD often attribute food selectivity to aversions to color, taste, smell, and/or texture, which suggests an underlying sensory component to this behavior (Shore 2001; Whiteley et al. 2000; Williams et al. 2000). Several studies have suggested that sensory sensitivity may lead children with ASD to restrict their intake to foods of preferred, tolerable, and manageable textures. The texture of foods has consistently been identified as a related aspect of food acceptance. (Ahearn et al. 2001; Hubbard et al. 2014; Postorino et al. 2015; Schreck & Williams 2006; Schreck et al. 2004; Williams et al. 2005). For example, using data from the current study, Hubbard et al. (2014) found that texture and consistency of foods are highly correlated with parent report of food refusal in a sample of 53 children with ASD ages 3–11 years. While a small number of studies have suggested that there is a significant relationship between atypical oral sensory processing and food selectivity in children with ASD, the methodologies used to elucidate this relationship have been limited by the use of parent report of food selectivity rather than the use of validated dietary measures. For example, studies have used a variety of parent-report tools such as the Eating Profile (Nadon et al. 2011), the Child Eating Behavior Questionnaire (Kral et al. 2015), the Brief Assessment of Mealtime Behavior Inventory (BAMBI) (Lane et al. 2014) or a single question about food selectivity on a parent questionnaire (Suarez et al. 2014). The inconsistency in measures and the lack of a standardized definition of food selectivity limits the ability to compare results across studies.
The purpose of the current study was to evaluate the relationship between oral sensory processing and food selectivity in children with ASD using quantitative measures of food selectivity. We also included a comparison group of TD children to assess differences in oral sensory processing compared to children with ASD. The aims of the study were to: 1) compare oral sensory processing function between children with and without ASD; 2) examine the relationship between atypical oral sensory processing and food selectivity in children with ASD; and 3) examine the relationship between atypical oral sensory processing and fruit and vegetable consumption. We hypothesized that atypical oral sensory processing would be greater in children with ASD, and would be associated with higher levels of food selectivity and with decreased fruit and vegetable variety.
METHODS
This study used data from the Children’s Activity and Meal Patterns Study (CHAMPS), a cross-sectional study conducted in 2007–2008 at the University of Massachusetts Medical School’s Eunice Kennedy Shriver Center. CHAMPS was designed to assess and compare dietary patterns, mealtimes, and physical activity patterns between children with and without ASD. Recruitment, exclusion criteria, and the procedures for verifying participants’ diagnosis of ASD have been previously described (Bandini et al. 2010). Participants included 53 children with ASD and 58 TD children ages 3–11 years. The study was approved by the Institutional Review Board at the University of Massachusetts Medical and parents provided written informed consent.
Parents completed a demographic/medical questionnaire, a Food Frequency Questionnaire (FFQ), and a 3-day food record. The Vineland Adaptive Behavior Scales (VABS) were used to characterize children’s adaptive skills and the Differential Abilities Scales (DAS) were administered to assess cognitive ability in children with ASD.
Parents also completed the Sensory Profile (Dunn 1999), a 125-item caregiver questionnaire frequently used in clinical practice to identify sensory processing challenges in children with ASD. It is a standardized tool that compares the child’s score to data from a reference sample of 1,200 children without disabilities and identifies the sensory systems that are affected by the child’s sensitivity to stimuli and contribute to functional impairments. Parents reported their child’s responses to sensory stimuli using a 5-point Likert scale (always, frequently, occasionally, seldom, never). Questions were scored along nine factors of sensory processing difficulties including Sensory Seeking, Emotionally Reactive, Low Endurance/Tone, Oral Sensory Sensitivity, Inattention/Distractibility, Poor Registration, Sensory Sensitivity, Sedentary, Fine Motor/Perceptual. Children scoring within the one standard deviation, or within the 84th percentile of the reference sample, are classified as “Typical”, which indicates typical sensory processing ability for each factor. Children who scored one or more standard deviations from the mean of the reference group (>85th percentile) were classified as “Atypical”, which is indicative of a likelihood of sensory processing difficulty for that factor. Within the Atypical classification, participants were further classified as having “probable” sensory processing issues (corresponding to between one and two standard deviations below the mean, or between the 2nd and 16th percentiles) or a “definite” sensory processing disorder (two standard deviations below the mean, or children scoring in the lowest 2%). (Dunn, 1999).
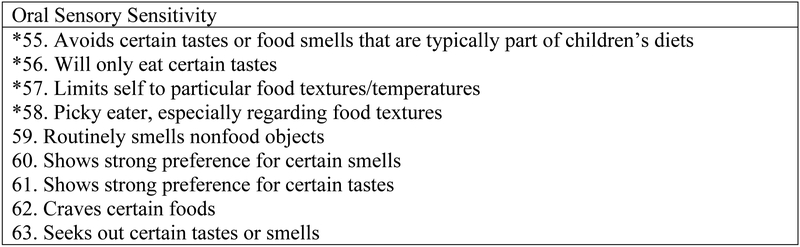
In order to explore the relationship between oral sensory over-sensitivity and food selectivity, we analyzed a subset of four questions from the Oral Sensory Sensitivity factor that measure over-sensitivity or a low tolerance for taste/smell stimuli (Figure 1) (Dunn 1999; McIntosh et al. 1999). These items comprised: (1) Avoids certain tastes or food smells that are typically part of children’s diets; (2) Will only eat certain tastes; (3) Limits self to particular food textures/temperatures; and (4) Picky eater, especially regarding food textures. The subscale is scored using the same approach as described above. We refer to this subscale as Oral Sensory Over-sensitivity.
Figure 1. Factor 4 Oral Sensory Sensitivity (OSS) Items on the Sensory Profile and Taste/Smell Sensitivity (TSS) Questions on the Short Sensory Profile.
* Indicates questions on Oral Over-Sensitivity measure
Relative to food selectivity, we used a quantitative approach to define this phenomenon that includes two distinct domains: food refusal and limited food repertoire (Bandini et al. 2010). Briefly, to assess food refusal, parents were asked to complete a modified version of the Youth/Adolescent Food Frequency Questionnaire (Rockett et al. 1997). We modified the FFQ to measure the refusal and frequency of consumption of 131 common food items during the past year based on parent report. The food refusal score was expressed as the percentage of foods refused of those offered to the child. Food repertoire was operationally defined as the absolute number of unique foods the child consumed (including beverages) over three days using a 3-day food record. Parents were asked to complete the 3-day food record for two weekdays and one weekend day, including food consumed at school. In addition, we examined fruit and vegetable variety, which was determined by the number of unique fruits and vegetables consumed on the FFQ, which included 13 fruits and 20 vegetables.
Data Analysis
Differences in participant characteristics between children with and without ASD were compared using independent samples t-tests for continuous variables and chi-square tests for categorical variables. Differences in sensory processing measures between children with and without ASD were compared using non-parametric Wilcoxon Rank Sum tests. After dichotomizing Oral Sensory Sensitivity and the Oral Sensory Over-sensitivity scores into Typical and Atypical, we used independent samples t-tests to compare the mean difference in food selectivity measures and fruit and vegetable variety between the groups. Linear regression was used to assess the impact of age on the relationship between food selectivity measures and Typical vs. Atypical sensory sensitivity. Statistical significance was declared when p<0.05. All analyses were conducted in SAS Version 9.3 (SAS Institute, Cary, NC) and IBM SPSS Statistics Version 21 (Armonk, NY: IBM Corp).
RESULTS
Demographic characteristics of the 53 children with ASD and 58 TD children are presented in Table 1. There were no significant differences in age, sex, or race/ethnicity between the two groups. TD children were more likely to be an only child than were children with ASD (26% and 11% respectively, p=0.05). However, whether or not a child was an only child was unrelated to any aspect of food selectivity. Characteristics of food selectivity for the ASD and TD groups are also shown. Compared to the TD group, children with ASD had significantly higher levels of food refusal, significantly lower levels of food repertoire, and less variety of fruits and vegetables.
Table 1.
Participant Characteristics
| Participant Characteristics | Children with ASD (n=53) |
TD Children (n=58) |
p-value |
|---|---|---|---|
| Age, years: mean (SD) | 6.6 (2.1) | 6.7 (2.4) | 0.75 |
| Sex, male (%) | 83% | 78% | 0.47 |
| Race, white (%) | 83% | 76% | 0.35 |
| Vineland Adaptive Behavior Scales (VABS) | 71.1 (12.4) | -- | -- |
| Score: mean (sd) | |||
| Differential Abilities Scales General | 85.8 (22.1) | -- | -- |
| Conceptual Ability Score (DAS): mean (sd)a | |||
| Child is an only child (%) | 11% | 26% | 0.05 |
| Food Refusal, mean (sd) | 41.7 (21.1) | 18.9 (15.6) | <0.001 |
| Food Repertoire, mean (sd) | 19.0 (4.9) | 22.5 (4.6) | <0.001 |
| Fruit Variety, mean (sd) | 6.5 (3.3) | 9.4 (2.9) | <0.001 |
| Vegetable Variety, mean (sd) | 5.9 (4.9) | 10.8 (4.8) | <0.001 |
n=47
To address the question of group differences in sensory processing, we examined scores on the Sensory Profile (Table 2). On average, children with ASD scored lower on the Sensory Profile than TD children, indicating more atypical sensory processing. Scores between the two groups differed significantly across all 9 factors. Mean scores in the TD group were classified in the typical performance range for all nine subscales, while mean scores in the ASD group fell in the atypical range for seven of nine subscales.
Table 2.
Comparison of Sensory Sensitivity Questionnaire Subscale Scores between Children with ASD and TD Children
| Children with ASD (n=53*) | TD Children (n=58*) | ||||
|---|---|---|---|---|---|
| FACTOR | Mean (sd) | Median | Mean (sd) | Median | p-valuea |
| Sensory Seeking | 54.7 (9.6) | 54 | 71.3 (9.7) | 73.0 | <0.001 |
| Emotionally Reactive | 46.6 (12.4) | 47 | 68.6 (7.2) | 70.0 | <0.001 |
| Low endurance/Tone | 35.0 (9.0) | 37.5 | 43.6 (2.7) | 45.0 | <0.001 |
| Oral Sensitivity | 29.6 (8.4) | 30.0 | 40.6 (5.2) | 42.0 | <0.001 |
| Inattention/Distractibility | 18.6 (4.2) | 19.0 | 28.6 (3.5) | 29.0 | <0.001 |
| Poor registration | 28.9 (4.5) | 29.0 | 38.0 (2.5) | 39.0 | <0.001 |
| Sensory Sensitivity | 16.4 (3.9) | 17.0 | 19.0 (1.7) | 20.0 | <0.001 |
| Sedentary | 12.4 (4.4) | 13 | 15.1 (2.9) | 15.0 | <0.001 |
| Fine Motor/Perceptual | 8.5 (2.8) | 9.0 | 12.6 (2.6) | 13.0 | <0.001 |
Sample sizes vary slightly due to missing data
non-parametric Wilcoxon test
Performance classifications for Oral Sensory Sensitivity and Oral Sensory Over-sensitivity for both groups are presented in Table 3. More children with ASD were classified as Atypical for Oral Sensory Sensitivity and Oral Sensory Over-sensitivity compared to TD children. Among TD children, only 7% were classified as Atypical based on their Oral Sensory Sensitivity scores and 9% as Atypical based on their Oral Sensory Over-sensitivity scores. Conversely, among children with ASD, 64% were classified as Atypical based on their Oral Sensory Sensitivity scores and 66% were classified as Atypical based on their Oral Sensory Over-sensitivity scores. Whereas there was no significant difference in mean age between the ASD subgroups for Oral Sensory Sensitivity, those characterized as Typical on the Oral Sensory Over-sensitivity were slightly older than those characterized as Atypical (7.5 years (median=7.9) vs. 6.2 years (median=5.5), p=0.03). Sex was not significantly associated with either of these variables.
Table 3.
Summary of Number (and %) of Children in Each Group in the Typical, Probable Difference, and Definite Difference Range in the Oral Sensory Sensitivity and Taste/Smell Sensitivity Subscales
| Factor | ASD | TD |
|---|---|---|
| Oral Sensory Sensitivity | n (%) | n (%) |
| Typical | 18 (36) | 54 (93) |
| Atypical | 32 (64) | 4 (7) |
| Probable Difference | 14 (28) | 2 (3) |
| Definite Difference | 18 (36) | 2 (3) |
| Oral Sensory Over-Sensitivity | n (%) | n (%) |
| Typical | 17 (34) | 53 (91) |
| Atypical | 33 (66) | 5 (9) |
| Probable Difference | 5 (10) | 4 (7) |
| Definite Difference | 28 (56) | 1 (2) |
In order to evaluate the relationship between typical and atypical oral sensory processing with food selectivity and fruit/vegetable variety in children with ASD, we stratified measures of food selectivity among children with Typical versus Atypical Oral Sensory Sensitivity and Oral Sensory Over-sensitivity (Table 4). Analysis of this association was limited to children with ASD as the sample size was too small in the Atypical Oral Sensory Sensitivity and Oral Sensory Over-sensitivity subgroup among TD children. Children with ASD who scored in the Atypical versus Typical range for Oral Sensory Sensitivity had significantly higher levels of food refusal (48.2% vs. 33.2%, respectively, p=0.01). Compared to children with ASD who scored in the Typical range for Oral Sensory Over-sensitivity, those who scored in the Atypical range had twice the level of food refusal (52% vs. 25%, p<0.001).. Fruit variety was significantly lower for children who scored in the Atypical versus Typical range for Oral Sensory Over-sensitivity (5.3 vs. 8.2, p=0.003) but was not significantly different for those who scored in the Atypical versus Typical range on the Oral Sensory Sensitivity measure. Children who were categorized as Atypical for Oral Sensory Sensitivity and Oral Sensory Over-sensitivity had significantly lower levels of vegetable variety compared to children who scored in the Typical range (4.2 vs. 8.6 and 4.2 vs. 8.9, p<0.01), respectively. When age was included as a covariate in multivariable linear regression models, the statistical significance of the findings remained unchanged.
Table 4.
Food Selectivity Among Children with ASD with Typical versus Atypical Oral Sensory Sensitivity and Taste/Smell Sensitivity
| Oral Sensory Sensitivity | Oral Sensory Over-Sensitivity | |||||
|---|---|---|---|---|---|---|
| Typical (n=18) |
Atypical (n=32) |
Typical (n=17) |
Atypical (n=33) | |||
| Mean (sd) | Mean (sd) | p-valuea | Mean (sd) | Mean (sd) | p-valuea | |
| Food Refusalb | 33.2 (19.1) | 48.2 (20.3) | 0.013 | 24.9 (17.7) | 52.0 (16.2) | <0.001 |
| Food aRepertoirec |
19.8 (3.9) | 18.3 (5.7) | 0.34 | 20.7 (4.2) | 17.9 (5.3) | 0.08 |
| Fruit Varietyd | 7.1 (3.2) | 5.9 (3.3) | 0.23 | 8.2 (2.6) | 5.3 (3.2) | 0.003 |
| Vegetable Varietyd |
8.6 (5.4) | 4.2 (3.6) | 0.005 | 8.9 (4.7) | 4.2 (4.0) | <0.001 |
p-value from independent samples t-test
Percentage of foods refused of those offered
Number of unique foods consumed from 3-day food record
Unique number of fruits/ vegetables consumed based on the FFQ, which included 13 fruits and 20 vegetables
DISCUSSION
Our results are consistent with findings from other studies that demonstrate that children with ASD had significantly greater Oral Sensory Sensitivity or Oral Sensory Over-sensitivity compared to children without ASD (Ermer & Dunn 1998; Hazen et al. 2014; Leekam et al. 2007; Nadon et al. 2011; Rogers et al. 2003; Tomchek & Dunn 2007). In our study, the majority of children with ASD scored outside the typical range for seven of the nine factors. However, scores spanned the entire range of performance classifications for the group (typical, probable and definite difference). The distribution of scores across the three performance categories is consistent with data reported by earlier studies, which supports the increased recognition that children with ASD are not a homogenous population (Brockevelt et al. 2013; Tomchek & Dunn 2007; Watling et al. 2001).
The primary objective of this study was to evaluate the relationship between oral sensory sensitivity and food selectivity among children with ASD. We previously reported that children with ASD exhibit more food selectivity than their TD peers (Bandini et al. 2010). Various factors can contribute to food selectivity and our aim was to evaluate the extent that food selectivity relates to atypical oral sensory processing. In the present study, we found that children with ASD were more likely than TD children to score in the Atypical range for both Oral Sensory Sensitivity and Oral Sensory Over-sensitivity. Among children with ASD, those with Atypical Oral Sensory Sensitivity refused more foods and ate fewer vegetables compared to those with Typical Oral Sensory Sensitivity. Children with ASD with Atypical Oral Sensory Over-sensitivity exhibited more food refusal, a narrower food repertoire, and less variety of fruits and vegetables compared to those with Typical Oral Sensory Over-sensitivity. These data suggest that children with ASD and Oral Sensory Sensitivity, and possibly more so with Oral Sensory Over-sensitivity, may exhibit food selectivity and restrictive eating behaviors. Children with Oral Sensory Sensitivity may restrict their diet to foods with preferred, tolerable, or manageable sensory features (Cermak et al. 2010). Whole grains, lean protein, fresh fruits, and vegetables are foods that are nutrient-dense, but often characterized by strong flavors and textures; our data support the observation that children with ASD who exhibit oral sensory sensitivity may be less likely to accept these types of foods, which consequently may put them at risk for inadequate nutrition.
Our findings are consistent with studies that have shown a correlation between sensory sensitivity and food selectivity, although prior studies have been limited by the methodology for measurement of food selectivity. Using the Sensory Profile, Kral et al. (2015) reported that children with ASD had significantly higher levels of oral sensory sensitivity compared to TD children, and, among children with ASD, those with atypical oral sensory sensitivity had significantly greater food neophobia, greater food fussiness, and increased under-eating due to negative emotions compared to children with ASD and typical oral sensory sensitivity. However, food selectivity was based on parent responses to questions on the Child Eating Behavior Questionnaire (CEBQ) rather than a quantitative measure of food selectivity as was used in our research. Similarly, in a study of 95 children with ASD ages 3–10 years, Nadon et al. (2011) reported that participants with atypical scores on the Short Sensory Profile (SSP) for Taste/Smell Sensitivity had significantly more eating problems than children with typical performance, measured using the parent-reported Eating Profile. This tool did not directly capture quantitative measures of food selectivity but rather, evaluated eating problems across 6 domains focusing on developmental eating milestones, mealtime behaviors, impact on the daily life of the family and feeding problems. Lane et al. (2014) also found Taste/Smell Sensitivity as measured with the SSP to be significantly associated with limited variety (r=−0.73, P<0.05) and food refusal (r=0.46, P<0.01), which were measured with the Brief Assessment of Mealtime Behavior Inventory (BAMBI). Scores for limited variety, food refusal, and autism-specific behaviors at mealtime on the BAMBI were based on parent-report of 18 eating behavior items using a 5-point Likert scale. While Lane et al. (2014) included 3-day food records, these were used to determine nutrient intake and not to quantify food selectivity. Suarez et al. (2014) conducted one of the few longitudinal studies on this topic, reporting that higher levels of hypersensitivity were associated with consuming fewer variety of foods, and that this behavior remained stable over the 20-month study period. However, food selectivity methodology was again a limitation as investigators utilized a questionnaire that asked parents to select a category representing how many foods their child accepts as part of his or her regular diet (i.e. less than 5, 6–10, 11–20, 21–30, and 30+). In light of the extant literature and the findings for the current study, there appears to be convincing evidence to confirm that children with ASD with more sensory sensitivity demonstrate higher levels of food selectivity. Practitioners working with this population should be aware of this relationship, and the potential impact this may have on the quality of the child’s diet.
Our study is one of the first to report a significant association between oral sensory processing and variety of fruit and vegetables consumed by children with ASD. Children with ASD exhibiting Oral Sensory Over-sensitivity were found to consume significantly less variety of fruits and vegetables compared to children with ASD without Oral Sensory Over-sensitivity. Fruits and vegetables are important components of a healthy diet and provide key nutrients for growth and development. Previous studies have reported that children with ASD consume fewer fruits and vegetables overall (Bandini et al. 2010; Emond et al. 2010; Johnson et al. 2008; Martins et al. 2008; Sharp et al. 2013; Suarez & Crinion 2015), and authors have speculated that avoidance of fruits and vegetables may be related to their flavor, texture, and/or consistency (Cermak et al. 2010; Schreck et al. 2004; Suarez et al. 2014). However, few studies have quantified the association between sensory sensitivity and the consumption of fruit and vegetables, and no studies have measured this association in children with ASD. The findings of our study suggest that efforts to increase consumption of fruits and vegetables in this population may be enhanced by including strategies that address oral sensory processing.
While our study suggests that there may be sensory processing factors that manifest as food selectivity in the child with ASD, additional studies are needed to fully elucidate the nature of the relationship. Several studies have proposed neurobiological mechanisms to explain how oral sensory sensitivity may result in food selective behaviors. Tavassoli & Baron-Cohen (2012) reported differences in taste identification as measured using taste strips between adults with ASD and a control group. Bennetto, et al. (2007) found that individuals with ASD perceived olfaction and taste stimuli differently than those without ASD; however, there were no differences in detection thresholds using stimuli presented via electrodes on the tongue. Thus, it is possible that individuals with Oral Sensory Sensitivity may present with differences in the brain that affect their ability to perceive taste. However, other factors may influence food selectivity as well, such as restricted interests and/or behavioral rigidity which are frequently characteristic of persons with ASD (Johnson et al. 2014; Schreck et al. 2004; Suarez et al. 2014). Sharp et al. (2014) suggests that there are medical, biological, environmental, parental, and behavioral factors at play that influence food selectivity in individuals with ASD.
We acknowledge several limitations in the present study. The study was advertised as a study about mealtime and physical activity; this may have resulted in a biased sample, as parents of children with feeding difficulties may have been more interested in participating in the study. We attempted to minimize this potential bias by recruiting children with and without autism and emphasizing that we were seeking children whether or not their parents had concerns in these areas in our recruitment. Because the present study was cross-sectional in design, we cannot establish a causal relationship between sensory sensitivity and food selectivity. In addition, we determined food selectivity based on the modified FFQ and 3-day food records, which have limitations for use that have been previously discussed (Bandini et al. 2010). These tools did not allow us to determine if a child was not offered a food by the parent based on the child’s presumed or historical refusal of that food. Fruit and vegetable items were disaggregated on the FFQ based on our desire to accurately measure refusal of these foods. However, foods such as mixed-food entrees were kept aggregated to minimize participant burden; this may have introduced error, which would likely be non-differential. The FFQ may not have accurately captured everything each child ate because the assessment was limited to items found on FFQ. This list was limited to fruit and vegetables commonly consumed in western diets, although there was an opportunity to write in any foods eaten more than once per week. Also, the 3-day food record may not adequately capture the repertoire of a typical diet, and our coding decisions may have affected our estimation of variety, although it is expected that any errors introduced in this way would have affected both groups similarly. There were also several limitations of the Sensory Profile tool used to assess oral sensory sensitivity in the study. Identification of sensory sensitivities were based on parent report rather than observed directly, and may have been affected by caregiver bias and observational abilities. Studies using direct observation rather than parent-reported data would likely address the limitations of this methodology, however this approach is not as practical for larger-scale studies. This study also did not collect information on parental food preferences, and thus it remains unknown whether parents’ food choices and preferences had an influence on what was served. Parents whose own food repertoire is limited may not offer a wide variety of foods to the family, which would result in limited food repertoires on the part of children. However, our measure of food refusal was based on food refused from those offered. We observed in this study and in our analyses of these data (Bandini, 2010; Curtin, 2015) that children with ASD had higher rates of food refusal than TD children. In this study, food refusal was positively and significantly associated with oral sensory sensitivities. Finally, lack of representation by a wider range of racial/ethnic groups of varying socio-economic status limits the generalizability of our findings.
Although the current study did not assess oral sensory under-sensitivity, delineating differences between over- and under-sensitivity to oral stimuli may provide insight into particular food selective eating behaviors in children with ASD. For example, oral over-sensitivity may result in difficulty with textures while oral under-sensitivity, in which the child does not appear to adequately perceive sensations, may result in the child consuming large amounts of a particular food and/or stuffing his mouth (Cermak et al. 2010). No studies to date have examined over- versus under-sensitivity to taste/smell stimuli for children with ASD, although previous studies have reported varying frequencies of overall sensory under-sensitivity and over-sensitivity in this population (Baranek et al. 2006; Ben-Sasson et al. 2009). Further study in this area is warranted.
The present study assessed the relationship between oral sensory processing and food selectivity in a moderate-sized sample of children with ASD with an age-matched control group. To the best of our knowledge, no similar studies have used direct measures of food intake to determine food selectivity. In contrast to earlier studies on this topic, this study quantified food selectivity using validated food measures and operationalized definitions of food refusal and limited food repertoire. Additionally, while most studies proceeded with unverified diagnoses of ASD, our study ensured that ASD was independently verified using the Autism Diagnostic Interview-Revised (Rutter et al. 2003) a gold-standard assessment of ASD and ASD severity. Use of two measures of oral sensory processing ability (Oral Sensory Sensitivity and Oral Sensory Over-sensitivity) also allowed us to differentiate between overall oral sensory sensitivity (including items reflecting both over and under-sensitivity) and specifically oral sensory over-sensitivity, which allow for more specificity when characterizing oral sensory processing dysfunction in this population.
CONCLUSION
Our study shows that more children with ASD present with atypical sensory characteristics compared to children without ASD. Among children with ASD, those with Atypical Oral Sensory Sensitivity refused more foods and ate fewer vegetables compared to those with Typical Oral Sensory Sensitivity. Further, Atypical Oral Sensory Over-sensitivity, a measure of sensory hyper-sensitivity for taste and smell sensory input, was associated with higher rates of food refusal, a narrower food repertoire and consumption of fewer unique fruits and vegetables. Early identification of and intervention for sensory processing abnormalities in children with ASD is critical for addressing problematic behaviors associated with eating and mealtimes. These findings suggest that children with ASD who have Atypical Oral Sensory Sensitivity and food selectivity may benefit from working with a multidisciplinary team of specialists, including speech pathologists, occupational therapists, and dietitians to improve sensory experiences related to eating and to increase adequacy and variety of the diet. Strategies may include changing the texture and consistency of foods to more manageable sensory characteristics, and using a sensory integration approach to decrease sensory sensitivity. More importantly, treatment plans should be individualized to the unique sensory characteristics of each child. Future areas of study should focus on the relationship between oral sensory sensitivity and neurobiological factors and the specific sensory characteristics of food, as well as differentiate between sensory over- and under-sensitivity. Direct observations of sensory processing ability may address the limitations of using a parent-reported tool. Longitudinal studies are needed to fully elucidate the nature of the relationship between sensory sensitivity and food selectivity in children with ASD and how it persists over time.
Acknowledgements
This research was funded by the following grants: R21HD048989–01A2 (NICHD; Diet, Activity and Obesity in Children with Autism); UA3MC25735–01-00 (MCHB; MCH Research Network on Promoting Healthy Weight (HWRN) among Children with Autism Spectrum Disorders (ASD) and other Developmental Disabilities); 2P30HD004147–33A2 (NICHD; Interdisciplinary Research in Intellectual & Developmental Disabilities); and P30DK046200 (NIH; Boston Nutrition Obesity Research Center).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Contributor Information
Liem T. Chistol, Boston University, Sargent College of Health & Rehabilitation Sciences, 635 Commonwealth Avenue, Boston, MA 02215.
Linda G. Bandini, E.K. Shriver Center, UMass Medical School, 55 Lake Avenue North, Worcester, MA 01655 and Department of Health Sciences, Boston University, 635 Commonwealth Ave., Boston, MA 02215.
Aviva Must, Tufts University School of Medicine, Dept. of Public Health and Community Medicine, 136 Harrison Ave., Boston, MA 02111.
Sarah Phillips, Tufts University School of Medicine, Dept. of Public Health and Community Medicine, 136 Harrison Ave., Boston, MA 02111.
Sharon A. Cermak, University of Southern California, Division of Occupational Science and Occupational Therapy at the Herman Ostrow School of Dentistry, 1540 Alcazar Street CHP-133, Los Angeles, CA 90089.
Carol Curtin, E.K. Shriver Center, UMass Medical School, Dept. of Family Medicine & Community Health, 55 Lake Avenue North, Worcester, MA 01655, carol.curtin@umassmed.edu, 774-455-6527.
REFERENCES
- Ahearn W, Castine T, Nault K, & Green G (2001). An assessment of food acceptance in children with autism or pervasive developmental disorder-not otherwise specified. Journal of Autism and Developmental Disorders, 31(5), 505–511. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders : DSM-5. (5th ed.). Washington, D.C.: American Psychiatric Association. [Google Scholar]
- Bandini L, Curtin C, Phillips S, Anderson S, Maslin M, & Must A (2017). Changes in food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(2), 439–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, et al. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics, 157(2), 259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranek GT, David FJ, Poe MD, Stone WL, & Watson LR (2006). Sensory Experiences Questionnaire: discriminating sensory features in young children with autism, developmental delays, and typical development. Journal of Child Psychology and Psychiatry, 47(6), 591–601. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, & Gal E (2009). A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Bennetto L, Kuschner ES, & Hyman SL (2007). Olfaction and taste processing in autism. Biological Psychiatry, 62(9), 1015–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockevelt BL, Nissen R, Schweinle WE, Kurtz E, & Larson KJ (2013). A comparison of the Sensory Profile scores of children with autism and an age- and gender-matched sample. South Dakota Medicine, 66(11), 459, 461, 463–455. [PubMed] [Google Scholar]
- Cermak SA, Curtin C, & Bandini LG (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110(2), 238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen DL, Baio J, Van Naarden Braun K, Bilder D, Charles J, Constantino JN, et al. (2016). Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years--Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveill Summ, 65(3), 1–23.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin C, Hubbard K, Anderson SE, Mick E, Must A, & Bandini LG (2015). Food selectivity, mealtime behavior problems, spousal stress, and family food choices in children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(10), 3308–3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn W (1999). The Sensory Profile: User’s Manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Dunn W (2001). The sensations of everyday life: empirical, theoretical, and pragmatic considerations. The American Journal of Occupational Therapy, 55(6), 608–620. [DOI] [PubMed] [Google Scholar]
- Emond A, Emmett P, Steer C, & Golding J (2010). Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics, 126(2), e337. [DOI] [PubMed] [Google Scholar]
- Ermer J, & Dunn W (1998). The sensory profile: a discriminant analysis of children with and without disabilities. The American Journal of Occupational Therapy, 52(4), 283–290. [DOI] [PubMed] [Google Scholar]
- Hazen EP, Stornelli JL, O’Rourke JA, Koesterer K, & McDougle CJ (2014). Sensory symptoms in autism spectrum disorders. Harvard Review of Psychiatry, 22(2), 112–124. [DOI] [PubMed] [Google Scholar]
- Hubbard KL, Anderson SE, Curtin C, Must A, & Bandini LG (2014). A comparison of food refusal related to characteristics of food in children with autism spectrum disorder and typically developing children. Journal of the Academy of Nutrition and Dietetics, 114(12), 1981–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson C, Handen B, Mayer-Costa M, & Sacco K (2008). Eating habits and dietary status in young children with autism. Journal Of Developmental And Physical Disabilities, 20(5), 437–448. [Google Scholar]
- Johnson CR, Turner K, Stewart PA, Schmidt B, Shui A, Macklin E, et al. (2014). Relationships between feeding problems, behavioral characteristics and nutritional quality in children with ASD. Journal of Autism and Developmental Disorders, 44(9), 2175–2184. [DOI] [PubMed] [Google Scholar]
- Kanner L (1943). Autistic disturbances of affective contact. Nervous Child, 217–250. [PubMed] [Google Scholar]
- Kral TV, Souders MC, Tompkins VH, Remiker AM, Eriksen WT, & Pinto-Martin JA (2015). Child eating behaviors and caregiver feeding practices in children with autism spectrum disorders. Public Health Nursing, 32(5), 488–497. [DOI] [PubMed] [Google Scholar]
- Lane AE, Geraghty ME, Young GS, & Rostorfer JL (2014). Problem eating behaviors in autism spectrum disorder are associated with suboptimal daily nutrient intake and Oral Sensory Over-sensitivity. ICAN: Infant, Child, & Adolescent Nutrition, 6(3), 172–180. [Google Scholar]
- Ledford JR, & Gast DL (2006). Feeding Problems in Children with Autism Spectrum Disorders: A Review. Focus on Autism and Other Developmental Disabilities, 21(3), 153–166. [Google Scholar]
- Leekam SR, Nieto C, Libby SJ, Wing L, & Gould J (2007). Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37(5), 894. [DOI] [PubMed] [Google Scholar]
- Ma NS, Thompson C, & Weston S (2016). Brief Report: Scurvy as a Manifestation of Food Selectivity in Children with Autism. Journal of Autism and Developmental Disorders, 46(4), 1464–1470. [DOI] [PubMed] [Google Scholar]
- Marí-Bauset S, Zazpe I, Mari-Sanchis A, Llopis-González A, & Morales-Suárez-Varela M (2014). Food selectivity in autism spectrum disorders. Journal of Child Neurology, 29(11), 1554–1564. [DOI] [PubMed] [Google Scholar]
- Martins Y, Young RL, & Robson DC (2008). Feeding and eating behaviors in children with autism and typically developing children. Journal of Autism and Developmental Disorders, 38(10), 1878–1887. [DOI] [PubMed] [Google Scholar]
- McIntosh DN, Miller LJ, & Shyu V (1999). Development and validation of the short sensory profile In Dunn W (Ed.), Sensory Profile Manual (pp. 59–73). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Nadon G, Feldman DE, Dunn W, & Gisel E (2011). Association of Sensory Processing and Eating Problems in Children with Autism Spectrum Disorders. Autism Research and Treatment. Epub 2011 Sep 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postorino V, Sanges V, Giovagnoli G, Fatta LM, De Peppo L, Armando M, et al. (2015). Clinical differences in children with autism spectrum disorder with and without food selectivity. Appetite, 92, 126–132. [DOI] [PubMed] [Google Scholar]
- Ranjan S, & Nasser J (2015). Nutritional Status of Individuals with Autism Spectrum Disorders: Do We Know Enough? Advances In Nutrition, 6(4), 397–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockett HRH, Breitenbach M, Frazier AL, Witschi J, Wolf AM, Field AE, et al. (1997). Validation of a youth/adolescent food frequency questionnaire. Preventive Medicine, 26(6), 808–816. [DOI] [PubMed] [Google Scholar]
- Rogers S, Hepburn S, & Wehner E (2003). Parent reports of sensory symptoms in toddlers with autism and those with other developmental disorders. Journal of Autism and Developmental Disorders, 33(6), 631–642. [DOI] [PubMed] [Google Scholar]
- Rutter M, Le Couteur AL, & Lord C (2003). Autism Diagnostic Interview-Revised. Los Angeles: Western Psychological Services. [Google Scholar]
- Schreck KA, & Williams K (2006). Food Preferences and Factors Influencing Food Selectivity for Children with Autism Spectrum Disorders. Research in Developmental Disabilities: A Multidisciplinary Journal, 27(4), 353–363. [DOI] [PubMed] [Google Scholar]
- Schreck KA, Williams K, & Smith AF (2004). A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders, 34(4), 433–438. [DOI] [PubMed] [Google Scholar]
- Sharp WG, Berry RC, McCracken C, Nuhu NN, Marvel E, Saulnier CA, et al. (2013). Feeding problems and nutrient intake in children with autism spectrum disorders: a meta-analysis and comprehensive review of the literature. Journal of Autism and Developmental Disorders, 43(9), 2159–2173. [DOI] [PubMed] [Google Scholar]
- Shore SM (2001). Beyond the wall : personal experiences with Autism and Asperger syndrome (1st ed.). Shawnee Mission, KS: Autism Asperger Publisher Co. [Google Scholar]
- Suarez MA (2012). Sensory processing in children with autism spectrum disorders and impact on functioning. Pediatr Clin North Am, 59(1), 203–214. [DOI] [PubMed] [Google Scholar]
- Suarez MA, & Crinion KM (2015). Food choices of children with autism spectrum disorders. International Journal of School Health, 2(3). [Google Scholar]
- Suarez MA, Nelson NW, & Curtis AB (2014). Longitudinal follow-up of factors associated with food selectivity in children with autism spectrum disorders. Autism, 18(8), 924–932. [DOI] [PubMed] [Google Scholar]
- Tavassoli T, & Baron-Cohen S (2012). Taste Identification in Adults with Autism Spectrum Conditions. Journal of Autism and Developmental Disorders, 42(7), 1419–1424. [DOI] [PubMed] [Google Scholar]
- Tomchek S, & Dunn W (2007). Sensory Processing in Children With and Without Autism: A Comparative Study Using the Short Sensory Profile. The American Journal of Occupational Therapy, 61(2), 190–200. [DOI] [PubMed] [Google Scholar]
- Watling R, Deitz J, & White O (2001). Comparison of sensory profile scores of young child with and without autism spectrum disorders. American Journal of Occupational Therapy, 55(4), 416–423. [DOI] [PubMed] [Google Scholar]
- Whiteley P, Rodgers J, & Shattock P (2000). Feeding Patterns in Autism. Autism, 4(2), 207–211. [Google Scholar]
- Williams K, Gibbons B, & Schreck K (2005). Comparing selective eaters with and without developmental disabilities. Journal Of Developmental And Physical Disabilities, 17(3), 299–309. [Google Scholar]
- Williams PG, Dalrymple N, & Neal J (2000). Eating habits of children with autism. Pediatr Nurs, 26(3), 259–264. [PubMed] [Google Scholar]
- Zimmer MH, Hart LC, Manning-Courtney P, Murray DS, Bing NM, & Summer S (2012). Food variety as a predictor of nutritional status among children with autism. J Autism Dev Disord, 42(4), 549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zobel-Lachiusa J, Andrianopoulos MV, Mailloux Z, & Cermak SA (2015). Sensory differences and mealtime behavior in children with autism. Am J Occup Ther, 69(5), 6905185050. [DOI] [PMC free article] [PubMed] [Google Scholar]