Abstract
Objectives. To describe disparities in HIV infection and syphilis among gay, bisexual, and other men who have sex with men (MSM) in US states through ratio-based measures and graphical depictions of disparities.
Methods. We used state-level surveillance data of reported HIV and syphilis cases in 2015 and 2016, and estimates of MSM population sizes to estimate HIV and syphilis prevalence by race/ethnicity and rate ratios (RRs) and to visually display patterns of disparity and prevalence among US states.
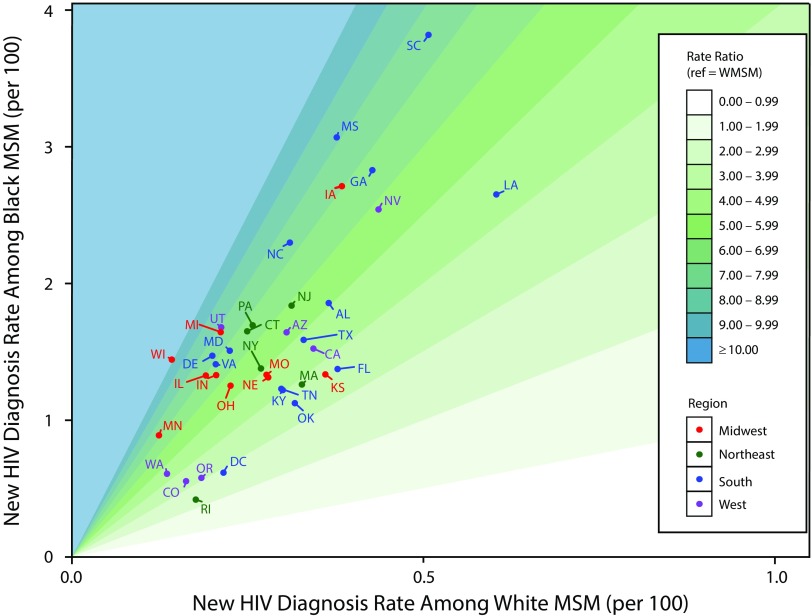
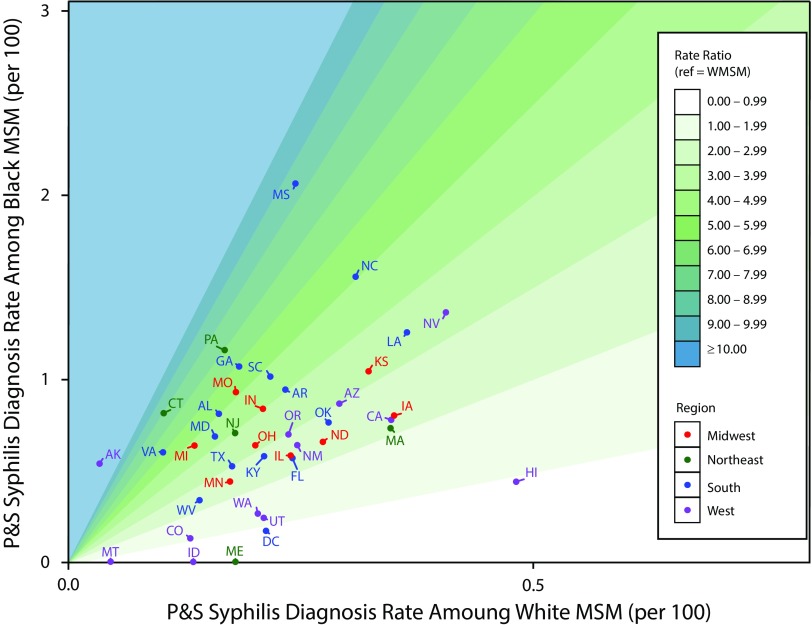
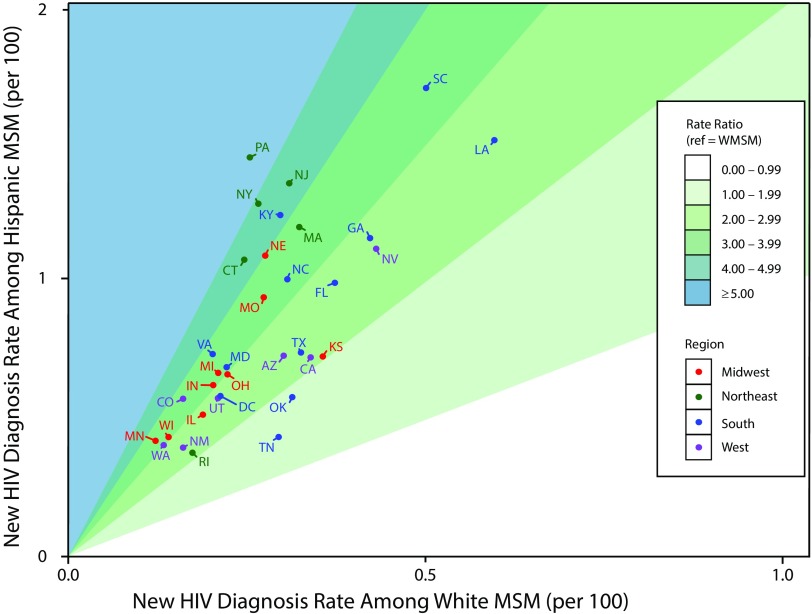
Results. State-specific rates of new HIV diagnoses were higher for Black than for White MSM (RR range = 2.35 [Rhode Island] to 10.12 [Wisconsin]) and for Hispanic than for White MSM (RR range = 1.50 [Tennessee] to 5.78 [Pennsylvania]). Rates of syphilis diagnoses were higher for Black than for White MSM in 42 of 44 states (state RR range = 0.89 [Hawaii] to 17.11 [Alaska]). Scatterplots of HIV diagnosis rates by race showed heterogeneity in epidemic scenarios, even in states with similar ratio-based disparity measures.
Conclusions. There is a widely disparate impact of HIV and syphilis among Black and Hispanic MSM compared with White MSM. Between-state variation suggests that states should tailor and focus their prevention responses to best address state data.
Racial/ethnic disparities in sexually transmitted infections (STIs) among gay, bisexual, and other men who have sex with men (MSM) have existed since at least early in the HIV epidemic. Disparities arise for complex reasons, including structural factors,1 and infectious disease disparities are often interwoven with complex and broader patterns of health disparities (i.e., syndemics).2 In the United States, an important national prevention goal is reducing disparities in new diagnoses of HIV among MSM and young Black and African American (hereafter “Black”) MSM by at least 15% by 2020.3 National goals are critical aspirational targets and important for setting national policies and priorities but will only be achieved as racial/ethnic disparities in HIV and other STIs are mitigated in local settings. Although disparities are well understood nationally, understanding how racial/ethnic disparities play out in specific states is an important step in achieving national goals for reducing disparities. Developing state-specific estimates of race-specific rates and disparities also allows the visualization of data in novel ways that might help increase insights into the patterns of disparities in US states.
HIV and syphilis affect non-Hispanic Black and Hispanic people (note that Hispanic people may self-categorize along a continuum that includes Black, White, and other races) to a degree that is disproportionate to their presence in the population.4 Blacks make up more than 12% of the US population but accounted for 44% of HIV diagnoses and 29% of the new primary and secondary (P&S) syphilis infections in 2016. Latinos make up 17% of the population and accounted for 25% of HIV diagnoses and 20% of new P&S syphilis infections in 2016.5,6
HIV and syphilis are related in terms of susceptible populations, behavioral risks, and biology. Thus, HIV and syphilis are often linked when considering sexual health outcomes among MSM. Syphilis causes inflammatory genital ulcers and lesions that can increase the risk of HIV transmission.7 A syphilis infection can also cause an increase in viral load for someone who is living with HIV.8 The disparities among minority MSM in both HIV and syphilis can be partly attributed to various social determinants of health.9 Kelley et al. found that high sexual network prevalence of HIV, increased poverty rates, and lack of access to medical care lead to disparities in HIV and other STIs among Black MSM.10,11
Disparities by race/ethnicity also exist in the subgroup of Americans most affected by the HIV epidemic: MSM.8,9,12 Both new HIV infections and P&S syphilis diagnoses have been increasing among MSM in the United States since about 2000.13,14 MSM made up roughly 2% of the population but 54% of people living with HIV in the United States in 2015.5 Of the 27 814 syphilis cases that were reported in 2016, 3049 were among women, 24 724 were among men, and about 58% of all cases were among MSM.15 In 2016, P&S syphilis rates for Black and Hispanic men were, respectively, 4.6 and 2.2 times the rate of White men.15 For US states overall in 2016, Black–White disparities in HIV diagnoses and syphilis diagnoses are lower among MSM than among women (2016: HIV RR = 15.4; syphilis RR = 7.1) and for the US population overall (2016 HIV RR = 8.8; syphilis RR = 4.8). For US states overall, Hispanic–White disparities in HIV diagnoses are higher among MSM than among women (2016 HIV RR = 3.1) and for the US population overall (2016 HIV RR = 3.7).15
To better describe the pattern of disparities in HIV infection and syphilis among MSM in the United States, we used state-level surveillance data of reported HIV and syphilis cases and state-level estimates of MSM population sizes derived from a small area estimation method.16 We used these data sources to provide estimates of HIV and syphilis prevalence for US states by race and derived prevalence ratios as a measure of disparities in HIV and syphilis. Because rate ratios (RRs) do not directly provide information about the magnitude of rates of diagnoses (ratios only provide information on the relative magnitude), we also used a data visualization approach to allow additional insights into the patterns of disparities.
METHODS
To calculate rates of HIV prevalence, HIV diagnoses, and syphilis diagnoses among MSM by state and race/ethnicity, we first calculated numerators (disease numbers) and denominators (population numbers) by state and race/ethnicity. To examine disparities, we calculated RRs by state, comparing non-Hispanic Black MSM to non-Hispanic White MSM (i.e., HIV prevalence, HIV diagnoses, and syphilis diagnoses) and Hispanic MSM to non-Hispanic White MSM (i.e., HIV prevalence and HIV diagnoses). Because of low syphilis case counts in most states for Hispanic MSM, we have not presented syphilis RRs for Hispanic compared with non-Hispanic White MSM.
HIV and Syphilis
We extracted national and state-level (plus the District of Columbia) counts of persons living with an HIV diagnosis (2015) and those with new HIV diagnoses (2016) among MSM from public Centers for Disease Control and Prevention (CDC) and AIDSVu.org data sources, with de-identified information reported to the CDC by state, county, and local health departments.17 Health departments’ surveillance data include age, race/ethnicity, and transmission category, including male-to-male sexual contact.18 Data on male–male sex come from a summary of directly reported risk data and imputed risk data.18 We followed standard publication practices for HIV surveillance data to protect privacy and to ensure stability of rates by suppressing data in states with fewer than 12 diagnoses in a state or subgroup.16,18 Suppressed state data contributed to national estimates.
For syphilis, we included new diagnoses of P&S syphilis for MSM by jurisdiction and by race/ethnicity in 2016 as reported to the CDC as part of the National Notifiable Diseases Surveillance System.19 The CDC directly provided data at this level of stratification, and these data do not appear in any other surveillance reports. Case reports include data on sex and race/ethnicity. Furthermore, jurisdictions record information on the sex of partners—whether male, female, or both male and female—and in 2016, 49 states reported these data to the CDC.15 We considered men who reported male partners (whether or not they also reported female partners) to be MSM. We suppressed data for states in which data about sex of partners was reported on fewer than 70% of P&S cases, and we excluded 3 states with less than 50% reporting of sex of partners on P&S cases.15
Number of Men Who Have Sex With Men by State and Race
Denominator data came from an update to our previously published method that estimated 2016 race/ethnicity-specific numbers of adult MSM in each state and the District of Columbia.16,20 Rates of HIV prevalence, HIV diagnoses, and syphilis diagnoses were previously reported through 2014.21 For rates of HIV diagnoses, we subtracted prevalent cases of HIV from the MSM denominator when calculating rates, because previously diagnosed persons cannot be newly diagnosed.
Rates and Rate Ratios
To calculate RRs, for each state, we took the disease rates previously calculated and divided the rates for non-Hispanic Black MSM by rates for non-Hispanic White MSM and the rates for Hispanic MSM by rates for non-Hispanic White MSM (HIV only). We calculated 95% confidence intervals (CIs) of the RRs overall using a bootstrapping approach that accounted for the random error from the MSM denominators in the numerator and denominator rates. As described earlier, we estimated the race-specific state-level MSM denominators from formulas that used American Community Survey responses regarding same-sex male households and 2 national estimates of MSM populations.22 We used the following procedure to account for random error in our ratio estimates: for each of 100 000 simulation runs (1) take a random draw from normal distributions defined by each of these 3 inputs’ point estimates and standard errors, (2) recalculate the MSM denominator for each state and race, and (3) merge in diagnosis data and compute RRs. We ranked the resulting 100 000 RRs for each disease and race comparison and used the 2.5th and 97.5th percentiles to construct the 95% CI.23
Data Visualization
To further illustrate the components of the disparity measures, we created race/ethnicity-specific scatterplots that illustrate the 2 race/ethnicity-specific rates and the summary RRs for HIV (i.e., Black–White, Hispanic–White) and for syphilis (Black–White only). We inspected these plots to identify patterns of race-specific rates and resulting RRs.
RESULTS
In the United States overall, 2016 rates of prevalent HIV diagnoses and new HIV diagnoses were higher for Black than for non-Hispanic White MSM (prevalent: RR = 3.29; new diagnoses: RR = 5.87) and were higher for Hispanic than for non-Hispanic White MSM (prevalent: RR = 1.72; new diagnoses: RR = 2.97). In all states with reportable data, the state-specific Black–White and Hispanic–White RRs for HIV diagnoses were greater than 1.0, indicating a disparate impact among MSM of color in recent diagnoses.
Nonetheless, there was substantial heterogeneity in state-specific measures of disparity (Table 1). For prevalent HIV infections in Black MSM, the highest state-specific disparity was in North Dakota (RR = 7.14), and the lowest was in Hawaii (RR = 1.20). For prevalent HIV infections in Hispanic MSM, the highest state-specific disparity was in Vermont (RR = 5.17), and the lowest was in Hawaii (RR = 0.73; 1 of 2 states with a Hispanic–White RR < 1.0). For new HIV diagnoses in Black MSM, the highest state-specific disparity was in Wisconsin (RR = 10.12), and the lowest was in Rhode Island (RR = 2.35). For new HIV diagnoses in Hispanic MSM, the highest state-specific disparity was in Pennsylvania (RR = 5.78), and the lowest was in Tennessee (RR = 1.50).
TABLE 1—
Rate Ratios for Prevalent HIV Diagnoses (2015), New HIV Diagnoses (2016), and Primary and Secondary Syphilis Diagnoses (2016) Among Men Who Have Sex With Men, by Race/Ethnicity: United States, 2015–2016
| Prevalent HIV Diagnoses (2015) |
New HIV Diagnoses (2016) |
P&S Syphilis Diagnoses (2016) |
|||
| Area | Black–White, RR (95% CI) | Hispanic–White, RR (95% CI) | Black–White, RR (95% CI) | Hispanic–White, RR (95% CI) | Black–White, RR (95% CI) |
| Alabama | 4.05 (3.70, 4.43) | 1.64 (1.58, 1.71) | 5.08 (4.66, 5.56) | 1.72 (1.64, 1.78) | 5.05 (4.63, 5.52) |
| Alaska | 3.14 (2.61, 9.59) | 1.76 (1.66, 1.91) | a | a | 17.11 (14.49, 37.34) |
| Arizona | 2.12 (2.05, 2.23) | 1.20 (1.12, 1.22) | 5.37 (5.18, 5.65) | 2.47 (2.34, 2.52) | 2.97 (2.86, 3.12) |
| Arkansas | 3.71 (3.36, 4.14) | 1.48 (1.36, 1.67) | 5.47 (4.91, 6.03) | 2.62 (2.38, 2.98) | 4.06 (3.65, 4.48) |
| California | 2.14 (2.05, 2.30) | 1.06 (1.02, 1.12) | 4.42 (4.22, 4.78) | 2.15 (2.08, 2.30) | 2.23 (2.13, 2.41) |
| Colorado | 2.11 (1.93, 2.39) | 1.15 (1.09, 1.26) | 3.39 (3.11, 3.83) | 3.61 (3.42, 3.96) | 1.00 (0.92, 1.13) |
| Connecticut | 2.97 (2.77, 3.30) | 2.59 (2.44, 2.85) | 6.60 (6.14, 7.32) | 4.43 (4.17, 4.86) | 8.09 (7.53, 8.97) |
| Delaware | 2.88 (2.63, 3.22) | 1.40 (1.33, 1.49) | 7.34 (6.66, 8.25) | a | b |
| District of Columbia | 1.94 (1.94, 1.94) | 1.46 (1.46, 1.46) | 2.86 (2.86, 2.86) | 2.77 (2.77, 2.77) | 0.80 (0.80, 0.80)c |
| Florida | 2.14 (2.02, 2.29) | 1.23 (1.12, 1.40) | 3.63 (3.44, 3.88) | 2.70 (2.46, 3.05) | 2.35 (2.24, 2.52) |
| Georgia | 4.14 (3.93, 4.40) | 1.76 (1.66, 1.88) | 6.61 (6.28, 7.02) | 2.78 (2.62, 2.97) | 5.86 (5.57, 6.22) |
| Hawaii | 1.20 (0.95, 1.73) | 0.73 (0.69, 0.89) | 3.20 (2.55, 4.74) | 1.41 (1.33, 1.79) | 0.89 (0.71, 1.31) |
| Idaho | 6.30 (5.73, 7.25) | 1.38 (1.20, 1.50) | a | 2.58 (2.28, 2.81) | d |
| Illinois | 3.37 (3.05, 3.81) | 1.56 (1.43, 1.73) | 6.95 (6.30, 7.84) | 2.77 (2.54, 3.09) | 2.43 (2.20, 2.74) |
| Indiana | 3.07 (2.64, 3.58) | 1.69 (1.56, 1.84) | 6.48 (5.55, 7.60) | 3.12 (2.88, 3.39) | 4.03 (3.45, 4.72) |
| Iowa | 3.61 (3.20, 4.48) | 2.63 (2.48, 2.89) | 6.97 (6.14, 8.67) | 2.81 (2.66, 3.09) | 2.25 (1.99, 2.81) |
| Kansas | 3.75 (3.25, 4.46) | 2.33 (2.13, 2.54) | 3.68 (3.20, 4.38) | 2.07 (1.89, 2.27) | 3.22 (2.79, 3.82) |
| Kentucky | 2.93 (2.53, 3.53) | 2.07 (1.88, 2.38) | 4.05 (3.49, 4.90) | 4.23 (3.85, 4.87) | 2.75 (2.37, 3.33) |
| Louisiana | 2.57 (2.30, 2.85) | 1.29 (1.15, 1.47) | 4.40 (3.92, 4.89) | 2.58 (2.29, 2.92) | 3.45 (3.07, 3.84) |
| Maine | 3.85 (3.27, 4.76) | 4.75 (4.49, 5.09) | a | a | d |
| Maryland | 4.47 (3.92, 5.00) | 2.31 (2.19, 2.46) | 6.74 (5.94, 7.50) | 3.14 (2.98, 3.36) | 4.41 (3.89, 4.91) |
| Massachusetts | 1.95 (1.65, 2.28) | 1.90 (1.67, 2.13) | 3.86 (3.28, 4.49) | 3.77 (3.32, 4.24) | 2.11 (1.79, 2.46) |
| Michigan | 5.28 (4.60, 6.10) | 2.18 (2.00, 2.37) | 7.72 (6.75, 8.92) | 3.23 (2.97, 3.52) | 4.75 (4.15, 5.49) |
| Minnesota | 3.29 (3.01, 3.67) | 2.45 (2.33, 2.61) | 7.16 (6.57, 7.99) | 3.49 (3.31, 3.71) | 2.54 (2.33, 2.84) |
| Mississippi | 4.80 (4.39, 5.12) | 2.65 (2.50, 2.85) | 8.16 (7.38, 8.77) | 0.90 (0.84, 0.97) | 8.52 (7.72, 9.17) |
| Missouri | 3.11 (2.72, 3.66) | 1.76 (1.58, 1.99) | 4.79 (4.17, 5.74) | 3.48 (3.13, 4.01) | 5.17 (4.50, 6.20) |
| Montana | 4.38 (3.52, 9.82) | 2.28 (1.86, 4.34) | a | a | d |
| Nebraska | 4.59 (3.84, 7.78) | 2.43 (2.26, 3.88) | 4.53 (3.78, 7.96) | 3.88 (3.60, 6.00) | e |
| Nevada | 2.50 (2.23, 6.33) | 1.29 (1.21, 2.15) | 5.60 (4.99, 14.25) | 2.60 (2.43, 4.49) | 3.22 (2.87, 8.20) |
| New Hampshire | f | f | f | f | d |
| New Jersey | 4.03 (3.42, 4.75) | 2.44 (2.10, 2.83) | 5.87 (4.99, 6.91) | 4.46 (3.84, 5.17) | 3.95 (3.36, 4.66) |
| New Mexico | 2.26 (2.15, 2.57) | 1.13 (1.08, 1.21) | a | 2.49 (2.41, 2.70) | 2.55 (2.44, 3.44) |
| New York | 3.35 (3.04, 3.78) | 3.72 (3.38, 4.21) | 5.09 (4.63, 5.76) | 4.87 (4.43, 5.52) | e |
| North Carolina | 4.61 (4.39, 4.86) | 1.80 (1.71, 1.92) | 7.41 (7.05, 7.82) | 3.34 (3.15, 3.55) | 5.05 (4.80, 5.33) |
| North Dakota | 7.14 (6.44, 9.86) | 1.36 (1.20, 1.74) | a | 14.96 (13.23, 20.59) | 2.34 (2.09, 3.68) |
| Ohio | 3.22 (2.90, 3.65) | 1.89 (1.78, 2.03) | 5.54 (4.99, 6.28) | 3.01 (2.83, 3.23) | 3.18 (2.87, 3.61) |
| Oklahoma | 2.50 (2.24, 2.89) | 0.97 (0.89, 1.06) | 3.53 (3.17, 4.09) | 1.87 (1.73, 2.06) | 2.72 (2.44, 3.14) |
| Oregon | 2.07 (1.81, 2.40) | 1.23 (1.17, 1.28) | 3.14 (2.74, 3.62) | 1.97 (1.89, 2.05) | 2.95 (2.58, 3.41) |
| Pennsylvania | 4.52 (3.81, 5.41) | 2.69 (2.46, 3.03) | 6.58 (5.56, 7.91) | 5.78 (5.30, 6.48) | 6.94 (5.87, 8.34) |
| Rhode Island | 2.03 (1.83, 2.38) | 1.36 (1.21, 1.60) | 2.35 (2.13, 2.77) | 2.18 (1.95, 2.59) | e |
| South Carolina | 4.81 (4.27, 5.17) | 1.97 (1.88, 2.07) | 7.58 (6.79, 8.11) | 3.45 (3.28, 3.62) | 4.72 (4.23, 5.05) |
| South Dakota | 2.89 (2.49, 3.55) | 1.76 (1.66, 1.90) | a | a | d |
| Tennessee | 2.90 (2.49, 3.47) | 1.31 (1.18, 1.49) | 4.10 (3.50, 4.93) | 1.50 (1.34, 1.69) | b |
| Texas | 2.90 (2.70, 3.37) | 1.38 (1.26, 1.52) | 4.77 (4.45, 5.58) | 2.31 (2.09, 2.55) | 2.96 (2.77, 3.47) |
| Utah | 4.27 (3.90, 6.53) | 1.75 (1.63, 2.16) | 7.78 (7.06, 12.39) | 2.78 (2.58, 3.51) | 1.13 (1.03, 1.80) |
| Vermont | 3.54 (2.92, 4.18) | 5.17 (4.88, 5.46) | a | a | d |
| Virginia | 4.02 (3.81, 4.26) | 1.60 (1.50, 1.75) | 6.89 (6.46, 7.32) | 3.69 (3.45, 4.02) | 6.03 (5.66, 6.40) |
| Washington | 2.29 (2.12, 2.53) | 1.66 (1.57, 1.73) | 4.49 (4.17, 4.95) | 3.08 (2.93, 3.21) | 1.30 (1.21, 1.43) |
| West Virginia | 3.16 (2.79, 3.78) | 2.74 (2.37, 3.13) | 3.39 (3.00, 4.04) | a | 2.41 (2.13, 2.87) |
| Wisconsin | 4.33 (3.51, 5.43) | 2.29 (1.98, 2.66) | 10.12 (8.23, 12.69) | 3.14 (2.72, 3.65) | e |
| Wyoming | 4.16 (3.41, 4.82) | 2.79 (2.59, 3.05) | a | a | b |
Note. CI = confidence interval; P&S = primary and secondary; RR = rate ratio.
Data suppressed because of small cell size or small subpopulation size.
Less than 50% of P&S syphilis cases contained information on sex of partners; state RR not reported and data did not contribute to national estimates.
Estimates of variability are derived based on county-level variation; the District of Columbia has no constituent counties and therefore no estimate of variability is presented.
At least 1 racial/ethnic group being compared had zero reported cases.
At least 50% but less than 70% of P&S syphilis cases contained information on sex of partners; state RR not reported but data contributed to national estimates.
Data not reported to the Centers for Disease Control and Prevention.
For P&S syphilis diagnoses in Black MSM, the highest state-specific disparity was in Alaska (RR = 17.11), and the lowest was in the District of Columbia (RR = 0.80; 1 of 2 jurisdictions with a Black–White RR < 1.0). Three of the 6 highest state-specific Black–White RRs for HIV diagnoses were in the South; 5 of the 7 highest Hispanic–White disparities for HIV diagnoses occurred in Northeastern states. For Black–White syphilis disparities, 6 of the 7 states with the lowest disparity were Western states. The scatterplots (Figures 1–3) illustrated that states with a specific level of disparity can have highly variable patterns of race-specific rates.
FIGURE 1—
HIV Diagnosis Rates Among Black and White Men Who Have Sex With Men (MSM) and Black–White Rate Ratios by State and decile of Disparity: United States, 2016
Note. WMSM = White men who have sex with men.
FIGURE 3—
Primary and Secondary (P&S) Syphilis Diagnosis Rates Among Black and White Men Who Have Sex With Men (MSM) and Black–White Rate Ratios by State and decile of Disparity: United States, 2016
Note. WMSM = White men who have sex with men.
FIGURE 2—
HIV Diagnosis Rates Among Hispanic and White Men Who Have Sex With Men (MSM) and Hispanic–White Rate Ratios by State and Sextile of Disparity: United States, 2016
Note. WMSM = White men who have sex with men.
DISCUSSION
Health disparity indictors are important indicators of population health and are useful for monitoring the progress of national and state goals to reduce health disparities in the United States.3 However, measurement of disparities is complex because there is no uniform standard of reporting, and it is particularly complex to calculate rates for hidden populations for which population size may be difficult to ascertain—especially in rural settings.24–27 For the first time, to our knowledge, we calculated state-level disparity measures for HIV and syphilis for MSM using state-level disease reports and state-level population-based estimates for MSM. Our analysis allows the discussion of disparities to move beyond national-level disparity measures and allows us to examine the data that are most relevant to state programs, which have primary public health responsibility and authority for disease control and treatment programs. National goals can be met only through the accumulation of many local successes—and these data are intended for state program use and program improvement. Our approach—illustrating the component rates for RRs—has practical implications for health departments and programs.
Examining disparities is a key metric for identifying health inequities, and in the case of sexual health, it is clear that Black MSM have the highest rates of HIV and syphilis and the largest disparities compared with White MSM. However, a measure of disparity by itself is not sufficient information to understand how states are doing in HIV prevention and how to focus programmatic and prevention efforts. By plotting the rates of HIV diagnoses in each subgroup and identifying the disparity category, we were able to identify more nuanced understandings of the heterogeneity of MSM’s epidemics in states. Across some states, such as North Carolina, Texas, and Oklahoma, HIV diagnosis rates for White MSM are similar, but the HIV diagnosis rates for Black MSM are very different, leading to widely varying RRs on the basis solely of the extent of the differences in rate between these states for Black MSM. The opposite is also true: Iowa, Nevada, and Louisiana have similar HIV rates for Black MSM but widely varying rates among White MSM, leading to broad variation in RRs driven by the differences among states in the White-specific rates.
Florida has a relatively low overall disparity ratio for HIV diagnoses between Black and White MSM but also has the seventh highest state-specific rate of HIV among White MSM. The picture is similar for the comparisons of HIV diagnoses between Hispanic MSM and White MSM: the overall national disparity is reflected in a range of disparity ratios that are greater than 1 in all states with enough data for this measure, but there are multiple race/ethnicity-specific rate scenarios that underlie these summary measures of disparity. For Black–White syphilis ratios (Figure 3), the cluster of states with the lowest disparities (< 2.0) largely represented states with low rates of syphilis for White MSM, with 1 exception: Hawaii, which represented the highest rate of syphilis diagnoses for White MSM.
Other factors associated with low or high disparity are not consistent; for example, 4 of the 5 areas with the lowest Black–White HIV diagnosis disparities (Rhode Island, Oklahoma, Oregon, Colorado) have proportions of Black residents lower than the national average; the fifth area (District of Columbia) has a higher proportion of Black residents than does any US state. The variability in rates among states might be attributable to historical differences in the prevalence of HIV and syphilis overall, to variability in the effectiveness of prevention programs, and to differences in state-level investments in prevention activities. Most states with high Hispanic–White disparities in HIV diagnoses were in the Northeast; this pattern might be related to differences in the country of origin of Hispanics in different US regions and variable prevalence of HIV in those countries of origin.28
These epidemic patterns translate to public priorities. States such as Arkansas, with high diagnosis rates in Black and White MSM, might consider focusing on examining their overall programmatic response for MSM. But states with high Hispanic-specific rates and low White-specific rates (e.g., Pennsylvania, New York) might consider evaluating existing prevention efforts for Hispanic MSM. States such as Nevada, with the second highest syphilis rate for White MSM and the third highest rate for Black MSM, should examine opportunities for increased syphilis screening and treatment of all MSM. Ultimately, each state has its own patterns of HIV and syphilis rates and disparity ratios, and on the basis of existing state programs, funding, and gaps, each state should develop a tailored program to address both the rates and the disparities. The data we have provided should be useful to states as part of a comprehensive set of data—including surveillance data, program monitoring data, and other state data sources—to develop a profile of programmatic needs. Data should be provided, with technical assistance, to community planning bodies, local prevention providers, and other stakeholders in HIV and STI prevention programs.
Although these data have programmatic utility, they are subject to limitations. The HIV diagnosis data we used reflect addresses at diagnosis, whereas the MSM denominators reflect current residence and sexual behavior in the previous 5 years. Our syphilis results are limited by heterogeneity in completeness of data on the gender of sexual partner among states and small cell sizes that precluded presentation of Hispanic rates and RRs. Hispanic ethnicity may represent different regional origins in different US states.
The denominator methodology is subject to both random error, which may be considerable in some jurisdictions, and systematic error introduced by key assumptions such as that the race distribution of MSM at the county level reflects that of males generally. Further, because the proportions of men who are MSM vary by state,16 some states might have apparently higher or lower rates among MSM because of the difference in MSM denominators. Our previous articles have extensively explored these assumptions.16,20
Because we combined race and ethnicity for Hispanic men, we were not able to describe some nuances in disparities for Hispanic MSM of varying races. In addition, although these disparities are important to report and follow in an ongoing manner, the actions needed to respond to various patterns of disparities across 2 different diseases is not immediately clear or straightforward. Similar analyses are needed for disparities in other STIs.
We have reported disparity ratios for Black MSM (HIV diagnoses and P&S syphilis) compared with White MSM and for Hispanic MSM (HIV diagnoses only) compared with White MSM for all states with sufficient data to be calculated. We have also reported a novel method of visual depiction of the component race/ethnicity-specific rates to provide further context to the interpretation of the RRs. These data can be updated annually to track progress and see changes in disparities. These data also can be used by states to focus programmatic efforts and to examine the impact of programmatic changes; in the future, data at more granular geographic levels can be developed. State progress in disease rates and disparities will both be needed to reduce HIV and syphilis rates and to meet national prevention goals.
ACKNOWLEDGMENTS
We acknowledge funding from the National Center for HIV, Viral Hepatitis, STDs, and TB Prevention Epidemic and Economic Modeling Agreement (grant U38 PS004646-01). This work was also supported by the Center for AIDS Research at Emory University (grant P30AI050409).
We thank members of the scientific and public health advisory groups of the Coalition for Applied Modeling for Prevention project for their input on this study, specifically those who reviewed a previous version of this article: Susan Blank, Jim Curran, David dowdy, Gregory Felzien, Jessica Frasure-Williams, David Harvey, and Jonathon Poe.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed for this analysis of public health surveillance data.
REFERENCES
- 1.Schulz AJ, Mullings LE. Gender, Race, Class, & Health: Intersectional Approaches. San Francisco, CA: Jossey-Bass; 2006. [Google Scholar]
- 2.Stall R, Mills TC, Williamson J et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. HIV.gov. National HIV/AIDS Strategy for the United States: Updated to 2020. 2015. Available at: https://www.hiv.gov/federal-response/national-hiv-aids-strategy/nhas-update. Accessed September 23, 2018.
- 4.Sullivan PS. Practical considerations for implementing a new syphilis action plan. Sex Transm Dis. 2018;45(9S suppl 1):S78–S79. doi: 10.1097/OLQ.0000000000000826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2016. HIV Surveillance Report. 2017. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2016-vol-28.pdf. Accessed September 23, 2018.
- 6. Centers for Disease Control and Prevention. NCHHSTP AtlasPlus. 2018. Available at: https://www.cdc.gov/nchhstp/atlas/index.htm. Accessed September 23, 2018.
- 7.Lynn W, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004;4(7):456–466. doi: 10.1016/S1473-3099(04)01061-8. [DOI] [PubMed] [Google Scholar]
- 8.Abara WE, Hess KL, Neblett Fanfair R, Bernstein KT, Paz-Bailey G. Syphilis trends among men who have sex with men in the United States and Western Europe: a systematic review of trend studies published between 2004 and 2015. PLoS One. 2016;11(7):e0159309. doi: 10.1371/journal.pone.0159309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forsyth AD, Valdiserri RO. A state-level analysis of social and structural factors and HIV outcomes among men who have sex with men in the United States. AIDS Educ Prev. 2015;27(6):493–504. doi: 10.1521/aeap.2015.27.6.493. [DOI] [PubMed] [Google Scholar]
- 10.Kelley CF, Vaughan AS, Luisi N et al. The effect of high rates of bacterial sexually transmitted infections on HIV incidence in a cohort of Black and White men who have sex with men in Atlanta, Georgia. AIDS Res Hum Retroviruses. 2015;31(6):587–592. doi: 10.1089/aid.2015.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sullivan PS, Rosenberg ES, Sanchez TH. Explaining racial disparities in HIV incidence in Black and White men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–454. doi: 10.1016/j.annepidem.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberg ES, Millett GA, Sullivan PS, Del Rio C, Curran JW. Understanding the HIV disparities between Black and White men who have sex with men in the USA using the HIV care continuum: a modeling study. Lancet HIV. 2014;1(3):e112–e118. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sullivan PS, Hamouda O, Delpech V. Reemergence of the HIV Epidemic among men who have sex with men in North America, Western Europe, and Australia, 1996–2005. Ann Epidemiol. 2009;19(6):423–431. doi: 10.1016/j.annepidem.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2015. 2016. Available at: https://www.cdc.gov/std/stats15/std-surveillance-2015-print.pdf. Accessed November 17, 2016.
- 15.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2016. 2017. Available at: https://www.cdc.gov/std/stats16/CDC_2016_STDS_Report-for508WebSep21_2017_1644.pdf. Accessed August 4, 2018.
- 16.Grey JA, Bernstein KT, Sullivan PS. Estimating the population sizes of men who have sex with men in US states and counties using data from the American Community Survey. JMIR Public Health Surveill. 2016;2(1):e14. doi: 10.2196/publichealth.5365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2014. HIV Surveillance Report. 2016. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2014-vol-26.pdf. Accessed September 23, 2018.
- 18.Nakashima AK, Fleming PL. HIV/AIDS surveillance in the United States, 1981–2001. J Acquir Immune Defic Syndr. 2003;32(suppl 1):S68–S85. [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2015. HIV Surveillance Report. 2016. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. Accessed September 23, 2018.
- 20.Grey JA, Bernstein KT, Sullivan PS et al. Rates of primary and secondary syphilis among White and Black non-Hispanic men who have sex with men, 2014. J Acquir Immune Defic Syndr. 2017;76(3):e65–e73. doi: 10.1097/QAI.0000000000001508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenberg ES, Grey JA, Sanchez TH, Sullivan PS. Rates of prevalent HIV infection, prevalent diagnoses, and new diagnoses among men who have sex with men in US states, metropolitan statistical areas, and counties, 2012–2013. JMIR Public Health Surveill. 2016;2(1):e22. doi: 10.2196/publichealth.5684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grey JA, Bernstein KT, Sullivan PS. Rates of primary and secondary syphilis among White and Black non-Hispanic men who have sex with men, US states, 2014. J Acquir Immune Defic Syndr. 2017;76(3):e65–e73. doi: 10.1097/QAI.0000000000001508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Efron B, Tibshirani R. An Introduction to the Bootstrap. Boca Raton, FL: Chapman & Hall/CRC; 1993.
- 24.Harper S, King NB, Meersman SC, Reichman ME, Breen N, Lynch J. Implicit value judgments in the measurement of health inequalities. Milbank Q. 2010;88(1):4–29. doi: 10.1111/j.1468-0009.2010.00587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman ME. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area–socioeconomic position and race-ethnicity, 1992–2004. Am J Epidemiol. 2008;167(8):889–899. doi: 10.1093/aje/kwn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chesson HW, Patel CG, Gift TL, Bernstein KT, Aral SO. Using reported rates of sexually transmitted diseases to illustrate potential methodological issues in the measurement of racial and ethnic disparities. Sex Transm Dis. 2017;44(9):513–518. doi: 10.1097/OLQ.0000000000000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pearcy JN, Keppel KG. A summary measure of health disparity. Public Health Rep. 2002;117(3):273–280. doi: 10.1016/S0033-3549(04)50161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Selik RM, Castro KG, Pappaioanou M, Buehler JW. Birthplace and the risk of AIDS among Hispanics in the United States. Am J Public Health. 1989;79(7):836–839. doi: 10.2105/ajph.79.7.836. [DOI] [PMC free article] [PubMed] [Google Scholar]