Abstract
Objectives. To assess changes in US tuberculosis (TB) incidence rates by age, period, and cohort effects, stratified according to race/ethnicity and nativity.
Methods. We used US National Tuberculosis Surveillance System data for 1996 to 2016 to estimate trends through age-period-cohort models.
Results. Controlling for cohort and period effects indicated that the highest rates of TB incidence occurred among those 0 to 5 and 20 to 30 years of age. The incidence decreased by age for successive birth cohorts. There were greater estimated annual percentage decreases among US-born individuals (–7.3%; 95% confidence interval [CI] = –7.5, –7.1) than among non–US-born individuals (–4.3%; 95% CI = –4.5, –4.1). US-born individuals older than 25 years exhibited the largest decreases, a pattern that was not reflected among non–US-born adults. In the case of race/ethnicity, the greatest decreases by nativity were among US-born Blacks (–9.3%; 95% CI = –9.6, –9.1) and non–US-born Hispanics (–5.7%; 95% CI = –6.0, –5.5).
Conclusions. TB has been decreasing among all ages, races and ethnicities, and consecutive cohorts, although these decreases are less pronounced among non–US-born individuals.
Overall US tuberculosis (TB) incidence rates have decreased since the mid-20th century, from an estimated 52.6 cases per 100 000 individuals in 1952 to 2.9 cases per 100 000 in 2016.1 However, between 2013 and 2015 the annual decrease in incidence slowed, resulting in overall national incidence rates remaining at approximately 3.0 cases per 100 000 annually for the entire period.1 According to modeling studies, TB trends are explained in part by changes in age-specific TB rates over time.2,3 The influence of events experienced within birth cohorts independent of age-specific trends, however, is not well understood.
Estimating the independent effects of age at diagnosis, period (year of diagnosis), and birth cohort (year of birth) on changes in TB incidence within US groups over time can clarify the relative effects of aging, influential exposures shared by each birth cohort, and influential exposures experienced by all birth cohorts during a particular period on TB incidence over time. We analyzed trends in TB incidence in the United States during 1996 to 2016 by age, birth cohort, and period, stratified according to race/ethnicity and nativity.
METHODS
Our primary data source was the National Tuberculosis Surveillance System (NTSS), which is maintained by the Centers for Disease Control and Prevention.1 We identified all individuals with TB verified between January 1, 1996, and December 31, 2016, within the 50 US states and the District of Columbia.
In the NTSS, US-born individuals are identified as those who were eligible for US citizenship at birth, regardless of the geographic location where they were born. The surveillance system also includes demographic (e.g., age and self-reported race/ethnicity), clinical, and laboratory data for each patient.
Estimated Tuberculosis Incidence
To compute incidence rates, we obtained population estimates from the Integrated Public Use Microdata Series of the Current Population Survey,4 a cross-sectional monthly US household survey conducted by the US Census Bureau and the Bureau of Labor Statistics. Using the US Census Bureau’s 2010 standard population,5 we age standardized TB incidence rates according to calendar period to control for residual confounding by single years of age within the broad 10-year age groups used to calculate age-specific rates. We used SAS version 9.4 (SAS Institute Inc., Cary, NC) to conduct weighted analyses.
Case Characteristics and Other Regression Covariates
We stratified incident TB cases by nativity (US-born or non–US-born) and by race/ethnicity (Hispanic, non-Hispanic White or Black, or Asian/Pacific Islander). Asians/Pacific Islanders were classified as 1 group because, until 2003, the NTSS categorized these individuals as a single racial group.1 Because of limited numbers of cases, individuals who reported their race as Native American (accounting for less than 2% of TB cases in the United States), who reported more than 1 non-Hispanic race, or who reported unknown race/ethnicity were excluded from the race/ethnicity analysis but were included in non–race/ethnicity-stratified analyses. Patients older than 74 years were excluded from analysis to ensure consistency of the 3-year or 5-year age groups in all comparative analyses involving age groups.
To calculate age-specific TB incidence by birth cohort, we classified patients into 11 cohorts by decade of birth (i.e., 1920: 1922–1929; 1930: 1930–1939; and so forth until 2010: 2010–2016) on the basis of available data by age. We estimated age-adjusted TB incidence according to 7 calendar periods of 3 years each (1996–1998, 1999–2001, 2002–2004, 2005–2007, 2008–2010, 2011–2013, and 2014–2016), 6 age groups (0–4, 5–14, 15–24, 25–44, 45–64, and 65–74 years), nativity (US-born or non–US-born), and race/ethnicity.
Age-Period-Cohort Modeling
We used the age-period-cohort analysis tool6 to fit log-linear models of expected TB incidence rates adjusted to estimate independent additive effects (if any) of age, period, and cohort. Because of the collinearity of the 3 time scales (cohort = period − age), the tool developers partitioned the log-linear additive effects of age, period, and cohort into linear and nonlinear components (age-cohort and age-period) expressed in equations not shown here.6
Briefly, the models calculate trends in TB incidence rates for a specific age group by creating a regression line that best fits the rates within a specific group. We estimated cross-sectional age-specific rates for the reference period (2005–2007) and adjusted those rates for cohort deviations from the linear trend for each birth cohort from 1922 to 1924 through 2014 to 2016. We estimated age-specific rates for the reference birth cohort (1966–1969) and then adjusted each curve for nonlinear departures from the linear period trends to obtain longitudinal age-specific TB incidence curves for each of the other cohorts during the period considered (1996–2016). We computed 95% confidence intervals (CIs) for each TB incidence rate point estimate. We fit a separate age-period-cohort model for each race/ethnicity and nativity category.
Estimated Change in Tuberculosis Incidence
Although the estimated annual percentage change (EAPC) in TB incidence can be computed from the observed annual age-standardized rates, the EAPC can be computed from the fitted rates of the age-period-cohort models with substantially greater precision (narrower 95% CIs).6 We used the regression coefficients (slopes) from the fitted models to calculate the estimated annual percentage change in TB incidence.6
RESULTS
During 1996 to 2016, a total of 288 253 verified TB cases were reported to the NTSS. Of these cases, 33 471 (11.6%) were excluded from our analysis because the patients in question were not 0 to 74 years of age and 598 (0.2%) were excluded because the data did not contain nativity information. Of the remaining 254 184 cases, 249 337 (98.1%) occurred among individuals in one of the race/ethnicity categories assessed (White, Black, Asian/Pacific Islander, Hispanic).
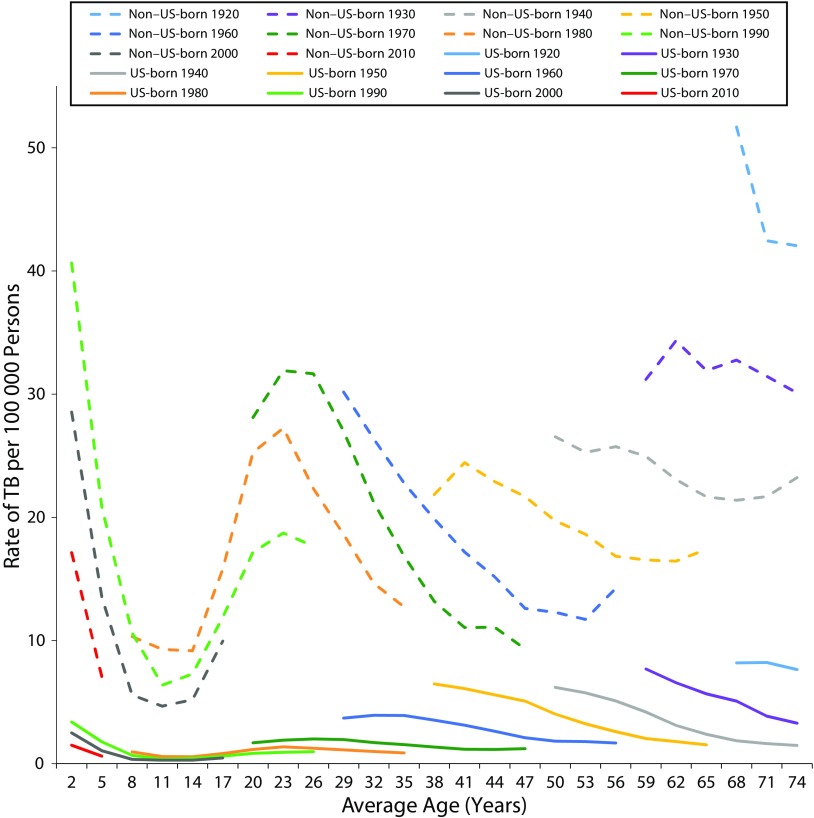
Cohort Effects
For all age groups and all birth cohorts, TB incidence rates were consistently higher among non–US-born individuals than among those born in the United States (Figure 1). Each successive birth cohort had a lower age-specific rate than the rates for all previous cohorts, indicative of strong birth-cohort effects. TB rates decreased as a birth cohort aged with the exception of higher incidence rates among adolescents and young adults.
FIGURE 1—
Age-Specific Incidence of Tuberculosis (TB), by Birth Cohort, Among US-Born and Non–US-Born Individuals: United States, 1996–2016
Note. The TB rate is per 100 000 individuals and covers 10 birth cohorts of 10 years each from 1920 to 2010.
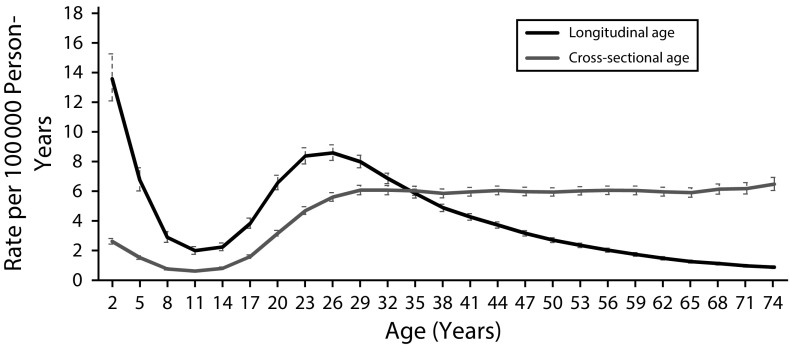
Cross-sectional and longitudinal age-specific TB rates diverged, indicating a strong cohort effect for TB cases reported in the United States (Figure 2). Cross-sectional age rates were higher than estimates of longitudinal age-specific rates after approximately the age of 35 years. Longitudinal, or life-course, rates were highest among children (0–5 years of age) and young adults (20–30 years of age).
FIGURE 2—
Cross-Sectional and Longitudinal Age-Specific Tuberculosis Incidence Rates: United States, 1996–2016
Note. The 95% confidence intervals are indicated by the upper and lower bars around the rate lines.
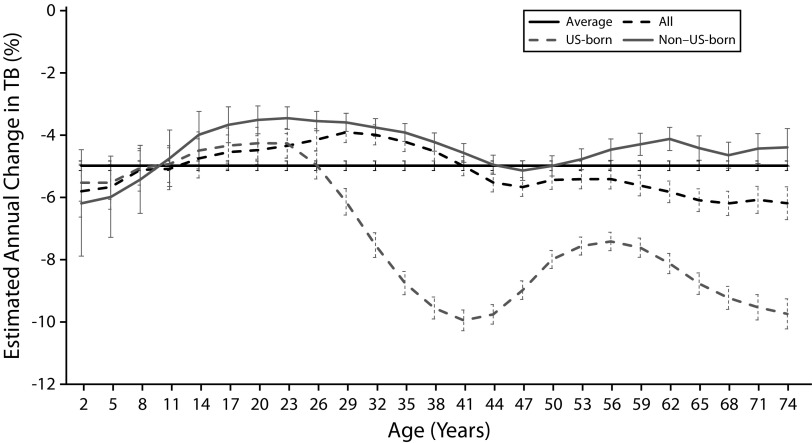
Age Effects
During 1996 to 2016, the EAPC in the overall US TB incidence rate decreased on average by 5.0% per year (95% CI = –5.1, –4.8%; Figure 3). Age-specific EAPCs revealed a larger decrease among individuals older than approximately 45 years, with the highest TB incidence decrease, 6.2% per year (95% CI = –6.7, –5.6%), among those 72 to 74 years of age.
FIGURE 3—
Estimated Annual Percentage Changes in Tuberculosis (TB) Incidence Rates, by Age and Nativity: United States, 1996–2016
Note. Estimates are for the overall annual percentage change (age in the figure legend) and annual percentage change by nativity among 3-year age groups (age in the figure legend; the oldest age for each age group represents each point on the x-axis) in TB rates. The 95% confidence intervals are indicated by the upper and lower bars around the rate lines.
Dichotomizing by nativity (Figure 3) revealed that the decrease in EAPCs for all age groups combined was larger among US-born (7.3% per year; 95% CI = –7.5, –7.1%) than non–US-born (4.3% per year; 95% CI = –4.5, –4.1%) individuals, primarily because of higher age-specific decreases among US-born individuals older than 25 years (the largest average decrease, 9.9% per year [95% CI = –10.3, –9.6], was among those 39–41 years of age). The largest decreases among non–US-born individuals occurred among children younger than 12 years, with the highest age-specific decrease among children 0 to 2 years of age (6.2% per year; 95% CI = –7.9, –4.4). Older non–US-born adults did not exhibit the same patterns of decreases in TB incidence as did those observed among US-born adults.
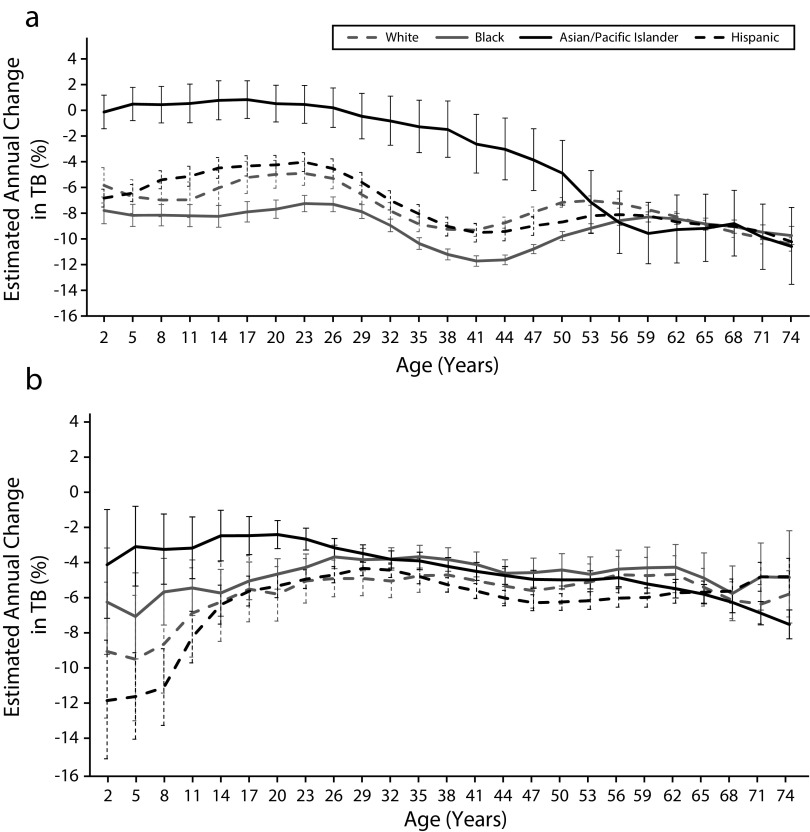
Age- and nativity-specific patterns of decreases were further reflected when the data were stratified by race/ethnicity, except among Asians/Pacific Islanders. Larger decreases occurred among US-born Whites, Blacks, and Hispanics than among members of the corresponding non–US-born racial/ethnic groups at or after approximately the age of 30 years (Figure 4). In the case of White and Hispanic individuals, EAPC patterns were similar among US-born and non–US-born individuals younger than approximately 30 years. EAPCs for Blacks diverged by nativity at a younger age, with US-born individuals experiencing a larger decrease than did non–US-born individuals from adolescence onward.
FIGURE 4—
Estimated Annual Percentage Changes in Tuberculosis (TB) Incidence Rates, by Race/Ethnicity and Age, Among (a) US-Born and (b) Non–US-Born Individuals: United States, 1996–2016
Note. The 95% confidence intervals are indicated by the upper and lower bars around the rate lines.
Asians/Pacific Islanders experienced similar patterns of decreases with the exception of smaller decreases among US-born individuals in their 20s and non–US-born individuals in their late 50s and early 60s. Among US-born individuals younger than approximately 50 years, Asians/Pacific Islanders exhibited a significantly lower decrease in incidence rates than did members of other racial/ethnic groups. Blacks experienced the highest decreases among those younger than approximately 50 years. Among non–US-born individuals, EAPC curves stratified by race/ethnicity were similar in patterns and rates of decrease, with Asians/Pacific Islanders experiencing the smallest decreases among children and among adults younger than approximately 24 years.
In terms of overall EAPCs by race/ethnicity and nativity, incidence rates decreased the most among US-born Blacks (–9.3%; 95% CI = –9.6, –9.1), followed by Whites (–7.6%; 95% CI = –7.9, –7.3), Hispanics (–7.4%; 95% CI = –7.8, –7.1), and Asians/Pacific Islanders (–3.2%; 95% CI = –4.1, –2.3). Race/ethnicity-specific EAPCs decreased slightly less among non–US-born individuals. Largest to smallest decreases by race/ethnicity were as follows: Hispanics, –5.7% (95% CI = –6.0, –5.5); Whites, –5.3% (95% CI = –5.8, –4.8); Blacks, –4.4% (95% CI = –4.8, –4.0); and Asians/Pacific Islanders, –4.1% (95% CI = –4.4, –3.8).
Period Effects
Age-standardized TB rates have been decreasing temporally among US-born and non–US-born individuals and among the majority of age and racial/ethnic groups (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Exceptions to this finding include fluctuations in rates among non–US-born Blacks 0 to 4 and 15 to 24 years old from 1996 to 2006 and among US-born Asians/Pacific Islanders aged 24 years or younger from 1996 to 2016.
Rate patterns were similar among US-born racial/ethnic group members with the exception of Asians/Pacific Islanders aged 24 years or younger. Before 2002, rates among Asians/Pacific Islanders aged 24 years or younger were lower than rates among Blacks and Hispanics; however, these rates increased (relative to those among all US-born racial/ethnic group members) from 2008 to 2016. A transition occurred in TB rates by age between non–US-born Blacks and Asians/Pacific Islanders aged 45 years or older from 1996 to 2016 (Figure A and Figure B, available as supplements to the online version of this article at http://www.ajph.org). Among individuals younger than 45 years, rates were higher among non–US-born Blacks than among members of other racial/ethnic groups from 1996 to 2016. Among non–US-born individuals aged 45 years or older for all years measured, rates were highest among Asians/Pacific Islanders, followed by Blacks.
DISCUSSION
TB incidence rates in the United States during 1996 to 2016 decreased among members of all racial/ethnic groups regardless of nativity, with independent age, period, and cohort effects. Our results demonstrate a decrease in age-specific TB incidence for every birth period cohort, a finding consistent with those of previous studies of the US population showing consecutive birth cohort decreases in TB mortality7 or latent TB infection.8 Lower TB rates for successive birth cohorts might represent success in the early diagnosis and complete and effective treatment of TB in the United States, which in turn might lead to reduced transmission.9 Each successive birth cohort is, therefore, exposed to a lesser risk for new infection.
Similarly, in our study TB incidence rates, age standardized and modeled, had a bimodal distribution with peaks in rates among young children (0–5 years of age) and younger adults (20–30 years of age). These results are comparable to those of a previous TB age-period-cohort analysis among patients in Hong Kong that demonstrated a similar bimodal pattern.10 The findings are in contrast with published cross-sectional data regarding US TB incidence rates by age,1 which frequently indicate that the highest rates are among older adults; however, these findings do not account for the decreasing rates of TB in each successive cohort.
TB incidence, regardless of age, was higher among non–US-born individuals throughout the study period, which is consistent with previously published data.1 Relative to US-born individuals, non–US-born individuals exhibited a slower decrease in age-specific case rates, particularly among those older than approximately 30 years. When further stratifying by race/ethnicity, we found that the overall EAPC decreases were the smallest among minority groups, regardless of nativity, with the exception of US-born Blacks and non–US-born Hispanics.
Among US-born individuals, the largest decreases were among Blacks. Hispanics exhibited the largest decreases among non–US-born individuals. Interestingly, age-specific EAPCs by nativity decreased similarly after adolescence regardless of race/ethnicity, except for US-born Asians/Pacific Islanders. This indicates that, among adults, changes in age-specific rates might not be influenced by race/ethnicity. Higher rates and smaller decreases in EAPCs among US-born Asians/Pacific Islanders might reflect small numbers of US-born Asians among individuals with newly diagnosed TB (e.g., 146 cases among Asians/Pacific Islanders in 2016) and continued high rates of TB among United States residents from US-affiliated Pacific islands.11
Finally, previous findings regarding race/ethnicity-specific TB incidence rates indicate that non–US-born Asians have the highest rate of TB incidence among non–US-born individuals.1 By contrast, our study determined that, when stratified according to nativity and age group, incidence rates are highest among non–US-born Asians/Pacific Islanders only in the 45- to 74-year age group. Among those younger than 45 years, rates are highest among non–US-born Blacks.
Strengths and Limitations
One of the main strengths of our study is the use of a robust data set that incorporates all reported TB case reports within the United States and includes data on age, race/ethnicity, and nativity. Furthermore, we used age-period-cohort modeling to estimate temporal percentage changes by nativity and race/ethnicity and to adjust incidence data for model effects. Our findings highlight disparities in rates of TB decrease between US- and non–US-born individuals and by race/ethnicity.
One limitation of this analysis is that we were unable to follow a single entire birth cohort because the data set contained only 21 years of TB incidence data, based on the availability of population denominators stratified by nativity. Also, we were unable to follow individuals’ entire life courses or to assess time since TB infection in relation to TB incidence. Moreover, although describing age, period, and cohort effects on decreasing TB incidence trends, our study does not explain the slowing of decreases during 2013 to 2015. Additional analyses to explain causal mechanisms for trends are needed.
In the case of US-born individuals, we did not consider parents’ place of birth or travel to TB-endemic areas; therefore, we cannot ascertain whether US-born children and adolescents with non–US-born parents might be at higher risk for TB because of travel or family history. Also, for individuals born outside the United States, the period of immigration and immigration patterns may have differed by race/ethnicity as well as birth cohort. In addition, from 2007 to 2013, the introduction of culture-based overseas screening for refugees and immigrants increased the number of TB cases detected prior to individuals’ arrival in the United States.12
Conclusions
We have shown that TB trends in the United States differ by nativity and race/ethnicity and according to age, period, and birth cohort. Although there have been decreases in TB rates, these decreases have been smaller among non–US-born individuals than US-born individuals in the case of all racial/ethnic groups as well as among those aged 30 years or older. Furthermore, the recent stabilization of rates among non–US-born individuals ensures that TB will remain a health concern for the United States.1 Maintaining effective TB control programs alongside screening and treatment of people at risk for TB or latent TB infection, particularly among those not born in the United States, is essential for reducing TB incidence.13
ACKNOWLEDGMENTS
We gratefully acknowledge the contributions of all state and local health departments whose staff collected and reported the data used in this article. We specifically acknowledge the editing contributions of C. Kay Smith.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not required because the data were collected and analyzed as part of routine tuberculosis surveillance.
REFERENCES
- 1.Reported Tuberculosis in the United States, 2016. Atlanta, GA: Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 2.Vynnycky E, Fine PE. The natural history of tuberculosis: the implications of age-dependent risks of disease and the role of reinfection. Epidemiol Infect. 1997;119(2):183–201. doi: 10.1017/s0950268897007917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frost WH. The age selection of mortality from tuberculosis in successive decades: 1939. Am J Epidemiol. 1995;141(1):4–9. doi: 10.1093/oxfordjournals.aje.a117343. [DOI] [PubMed] [Google Scholar]
- 4.Flood S, King M, Ruggles S, Warren JR. Integrated Public Use Microdata Series, Current Population Survey. Available at: https://www.ipums.org/doi/D030.V4.0.shtml. Accessed August 7, 2018.
- 5.US Census Bureau. Profile of general population and housing characteristics: 2010. Available at: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_DP_DPDP1&src=pt. Accessed August 7, 2018.
- 6.Rosenberg PS, Check DP, Anderson WF. A Web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23(11):2296–2302. doi: 10.1158/1055-9965.EPI-14-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doege TC. Tuberculosis mortality in the United States, 1900 to 1960. JAMA. 1965;192(12):1045–1048. doi: 10.1001/jama.1965.03080250023005. [DOI] [PubMed] [Google Scholar]
- 8.Winston CA, Navin TR. Birth cohort effect on latent tuberculosis infection prevalence, United States. BMC Infect Dis. 2010;10(1):206. doi: 10.1186/1471-2334-10-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lobato MN, Wang YC, Becerra JE, Simone PM, Castro KG. Improved program activities are associated with decreasing tuberculosis incidence in the United States. Public Health Rep. 2006;121(2):108–115. doi: 10.1177/003335490612100202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu P, Cowling BJ, Schooling CM et al. Age-period-cohort analysis of tuberculosis notifications in Hong Kong from 1961 to 2005. Thorax. 2008;63(4):312–316. doi: 10.1136/thx.2007.082354. [DOI] [PubMed] [Google Scholar]
- 11.Viney K, Hoy D, Roth A, Kelly P, Harley D, Sleigh A. The epidemiology of tuberculosis in the Pacific, 2000 to 2013. Western Pac Surveill Response J. 2015;6(3):59–67. doi: 10.5365/WPSAR.2015.6.3-059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y, Posey DL, Cetron MS, Painter JA. Effect of a culture-based screening algorithm on tuberculosis incidence in immigrants and refugees bound for the United States: a population-based cross-sectional study. Ann Intern Med. 2015;162(6):420–428. doi: 10.7326/M14-2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LoBue PA, Mermin JH. Latent tuberculosis infection: the final frontier of tuberculosis elimination in the USA. Lancet Infect Dis. 2017;17(10):e327–e333. doi: 10.1016/S1473-3099(17)30248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]