Abstract
Background and Objectives
Midlife adults are a “pivot” generation, responding to parents’ and grown children’s problems. Yet, some midlife adults may have families where multiple members suffer sorrows, whereas other midlife adults may have families with few problems. This study examined: (a) typologies of problems across generations and (b) associations between profiles of problems and midlife adults’ well-being.
Research Design and Methods
Midlife adults (N = 633) reported their own, each parent’s (n = 868), and grown child’s (n = 1,785) physical (e.g., injury, cancer), psychological (e.g., anxiety, addiction), and lifestyle problems (e.g., divorce, job loss), and parents’ functional disabilities. Midlife adults reported their own depressive symptoms.
Results
Latent profile analysis revealed four family typologies: (a) lowest problems across generations (n = 364), (b) offspring and midlife adult moderate problems, parent high physical problems and disability (n = 165), (c) offspring and parent moderate problems (n = 90), and (d) offspring highest problems (n = 14). Midlife adults in the lowest problems group (Profile a) reported higher income and fewer depressive symptoms than midlife adults in the other groups.
Discussion and Implications
Midlife adults cope with challenges when grown children or parents suffer problems, and their well-being may suffer as a result. In this study, regardless of the profile, higher problems in either generation were associated with more depressive symptoms for midlife adults.
Keywords: Intergenerational relationships, Parent–child ties, Intergenerational transmission, Life problems, Caregiving, Crisis, Young adulthood, Midlife, Emerging adulthood, Family, Latent profile analysis
Scholars refer to midlife adults as a “pivot” generation who often provide support to generations above and below when things go wrong (Attias-Donfut & Wolff, 2000; Fingerman et al., 2011; Grundy & Henretta, 2006). In midlife, grown children are sensitive to detrimental events an aging parent incurs such as health declines, widowhood, or financial strains (Bangerter, Zarit, & Fingerman, 2016). Recent research also has found that midlife adults report poorer well-being when their grown children suffer problems (Fingerman, Cheng, Birditt, & Zarit, 2012; Pillemer, Suitor, Riffin, & Gilligan, 2017; Umberson, Pudrovska, & Reczek, 2010). Yet, we know little about the constellation of problems across generations or how these constellations of problems may be associated with midlife adults’ depressive symptoms.
Indeed, some midlife adults may focus energies on one family member’s unique problems, whereas another midlife adult may rally to deal with widespread problems throughout the family. Difficulties may spread from parents to children due to genetic similarities or transmission of behaviors, stress, and risk (Agrawal & Lynskey, 2008; Kraft & Hunter, 2009). In some families, most members may be thriving, and in other families, parents may have problems but offspring may not. Midlife adults’ reactions to these constellations also may vary; some midlife adults may suffer depressive symptoms in response to many family members’ problems, whereas other midlife adults thrive with few family problems.
This study generated typologies of problems in three-generation families. We examined factors associated with family profiles of problems (e.g., socioeconomic status [SES]). Moreover, we asked how family profiles of problems are associated with midlife adults’ depressive symptoms.
Distributions of Problems Within Families
Researchers have distinguished lifestyle problems associated with behavior (e.g., divorce, job loss) as distinct from physical (e.g., injury, cancer) and psychological problems (e.g., anxiety disorder, addiction). Initial studies of life events suggested that physical or psychological health problems were uncontrollable, but lifestyle problems such as financial difficulties and relationship dissolution were controllable (Plomin, Lichtenstein, Pedersen, McClearn, & Nesselroade, 1990). In truth, the ability to control distinct types of life events and the implications of those events are complex (Rhee, in press), and thus, we examined psychological, physical, and lifestyle problems without implication of control. Prior research on parents’ and children’s problems has not differentiated between physical and psychological disorders (e.g., Birditt, Fingerman, & Zarit, 2010; Pillemer et al., 2007; Pillemer et al., 2017), but given potential differences in demands on family for such disorders, we did so here. We also considered functional disability in late life as distinct from physical health problems. Although the two types of events may co-occur, functional disabilities pertain to the inability to complete activities of daily life, thus necessitating ongoing family caregiving (Kim et al., 2017).
We asked how different types of problems cluster among parents and offspring in a given family. Recently, researchers have examined typologies of family characteristics. Typological studies have limitations; findings depend on the measures used to generate patterns and how scholars interpret the patterns. Yet, studies consistently have found that midlife adults’ ties to parents and children can be classified into four to six categories based on relationship qualities and support (Dykstra & Fokkema, 2011; Fiori et al., 2017; Hogerbrugge & Silverstein, 2015; Kim, Zarit, Fingerman, & Han, 2015). This is the first study to consider family typologies regarding parents’ and grown children’s problems.
Family Profiles
Several theories point to homogeneity in family problems across generations. Research has documented intergenerational transmission of belief, behaviors, and psychopathologies (e.g., Johnston, Schurer, & Shields, 2013). Genetic risk factors for physical and psychological problems and addiction have been identified (Agrawal & Lynskey, 2008; Kraft & Hunter, 2009). Furthermore, one family member’s problems may contribute to poor mental health via contagion (Christakis & Fowler, 2013) or empathetic distress (Knoester, 2003). Stress also may spread via demands of helping family members who suffer problems.
Lifestyle problems in particular may co-occur across generations. Homophily—similarity of values, life station, and behaviors—may generate similarity in problems among family members (McPherson, Smith-Lovin, & Cook, 2001). For example, divorce in one generation predicts a higher risk of divorce in the next generation (Wolfinger, 2011). Likewise, economic hardship occurs across generations in families (Fingerman et al., 2015; Torche, 2015). Indeed, familial risk patterns may begin in childhood when shared genetic vulnerabilities and disruptive psychosocial functioning contribute to life stressors (Repetti, Taylor, & Seeman, 2002). Then, cumulative disadvantage may snowball problems to persist across adulthood (Swartz, 2008).
Family systems theory and sociocontextual theories (e.g., Bronfenbrenner & Morris, 2006; Elder, 1998; Fingerman & Bermann, 2000) also suggest that some families may fit the axiom, “all good things clump together” and problems may be rare across generations. Benefits may cluster in these families due to shared privilege and cumulative advantage, high SES, or low-risk genetic dispositions (Swartz, 2008). In these families, parents may experience successful aging, low rates of disability, and have few other problems (Rowe & Kahn, 1997, 2015) and midlife and young adults may be thriving.
We also expected heterogeneous family constellations in which only some parents or grown children experience different types of problems (Birditt et al., 2010; Fingerman et al., 2012; Suitor et al., 2016). For example, offspring who are aware of problems in prior generations may take measures to avoid those problems. Furthermore, theory suggests problems vary across the life course and, thus, vary by generation. For example, in young adulthood, grown children experience more lifestyle problems (job loss, divorce) than older generations (Schulenberg, Sameroff, & Cicchetti, 2004). By contrast, older parents may incur more physical health problems and a greater likelihood of functional disability.
In sum, we expected homogeneous families to be most common and characterized by two typologies: (a) parents and grown children across generations may experience similar physical, psychological, lifestyle problems, and disability (and this may be particularly true for lifestyle problems) and (b) parents and grown children across generations may experience low rates of problems. We also expected some families to fit profiles reflecting heterogeneity in problems, that is, parents and children in these families experience different types of physical, psychological, lifestyle problems, or disability.
SES Associated With Profiles of Problems
We also expected socioeconomic position to be associated with constellations of family problems. Socioeconomic position in the United States is typically highly correlated across generations (Swartz, 2008). The United States has the lowest rate of economic mobility among major industrialized countries; thus, parental SES is strongly associated with offspring SES (Torche, 2015).
People in lower socioeconomic positions experience more lifestyle-associated problems such as job loss and divorce as well as increased risk of physical and psychological problems (Conger & Donnellan, 2007). Moreover, by late life, disability rates are higher among less educated and poorer older adults (Hayward, Hummer, & Sasson, 2015). Lack of resources and impoverished living circumstances generate an array of risk factors. Thus, we expected lower SES to be associated with membership in profiles of higher problems.
Family Problems and Midlife Adults’ Depressive Symptoms
Midlife adults’ well-being (e.g., depressive symptoms) might be associated with the constellation of problems in the family. Prior studies report that midlife adults suffer when members of generations above or below experience a variety of problems (Fingerman et al., 2012; Pillemer et al., 2017; Umberson et al., 2010). As such, we expected midlife adults in families with fewer problems to report fewer depressive symptoms, possibly because they are less burdened to provide support.
Moreover, prior research suggests family members’ lifestyle problems may be associated with poorer well-being more so than other types of problems. Regardless of actual controllability of events, midlife adults tend to blame their relatives for lifestyle problems and experience increased distress due to frustration with the relative (Birditt et al., 2010; Birditt, Kim, Zarit, Fingerman, & Loving, 2016; Suitor et al., 2016). Nevertheless, other types of problems also may be associated with depressive symptoms. For example, midlife adults might worry about their children’s health problems or provide caregiving for parents’ disabilities (Hay, Fingerman, & Lefkowitz, 2008; Knoester, 2003).
Furthermore, prior research has focused on problems either in the parent generation (e.g., Bangerter et al., 2016; Pinquart & Sörensen, 2003) or among grown children (e.g., Fingerman et al., 2012; Pillemer et al., 2017), but not problems in both generations. We expected that pivoting between generations suffering problems would be especially detrimental for midlife adults’ depressive symptoms. Yet, the intergenerational stake hypothesis suggests parents have a greater investment in children than the reverse (Birditt, Hartnett, Fingerman, Zarit, & Antonucci, 2015; Giarrusso, Feng, & Bengtson, 2005). Thus, typologies with young adult children experiencing problems may be particularly harmful for midlife adults’ depressive symptoms.
In sum, based on prior typology studies of families (e.g., Dykstra & Fokkema, 2011; Fiori et al., 2017; Kim et al., 2015), we expected to find four to six typologies of families grouped by physical, psychological, lifestyle problems, and parental disability. We expected most families to be distributed among homogeneous typologies involving: (a) low problems or (b) similar physical, psychological, and/or lifestyle problems across generations. We also expected to find typologies with heterogeneity in problems across generations. Based on life course distributions of problems, in these families, we expected more lifestyle problems in younger generations, and physical problems and functional disability in the oldest generation. We anticipated lower SES families would have a greater likelihood of membership in profiles suffering problems (i.e., upper SES families to fall in typologies characterized by lower problems). We also expected profiles of problems to be associated with the midlife adults’ depressive symptoms, particularly typologies with grown children suffering problems.
Methods
Sample
The sample included 633 midlife men (n = 301) and women (n = 332) aged 40–60 years (Mage = 50.70, SD = 4.99) who participated in the Family Exchanges Study 1 conducted in 2008. Participants resided in the greater Philadelphia area and had at least one living parent and one child aged 18 and older. Recruitment occurred via listed samples purchased from Genesys Corporation and random digit dialing in regional area codes. Heavy recruitment in high-density minority neighborhoods resulted in a sample that was 37% minority (primarily African American; see Fingerman et al., 2011).
Measures
Midlife participants reported on themselves, each grown child (n = 1,785) and each living parent (n = 868). They provided background information and reports of problems and disability for each family member.
Parents and Grown Children’s Problems
Drawing on prior research (Birditt et al., 2010; Fingerman, Miller, Birditt, & Zarit, 2009; Greenfield & Marks, 2006; Pillemer et al., 2017), participants indicated whether each parent and each grown child had experienced several problems in the past 2 years (1 = yes, 0 = no). The problem lists were similar, but also specific to position in the life course. For parents, participants indicated: serious health problems, emotional problems (e.g., anxiety, depression), drinking or drug addiction, financial loss, divorce or relationship problems, or death of a loved one. In addition, participants rated each parent’s health in the past year on a scale from 1 = poor to 5 = excellent. If participants indicated a parent had 1 = poor health, we considered that a problem coded as “poor health.”
To assess parents’ functional disabilities, participants answered items from the Community Disability Scale for each parent regarding functional disabilities requiring assistance with tasks of personal care, daily care, transportation, and finances (Bassett & Folstein, 1991). We treated this construct as distinct from physical problems for parents because functional disabilities require help from others; individuals with physical health problems may or may not require assistance.
Participants indicated similar problems for each young adult child. The list for children did not include death of a loved one. But the list for children also included trouble with the law and participants rated a single item for physical impairment for adult child.
We grouped items under the following categories: (a) physical problems (e.g., physical impairment, serious health problem, poor health), (b) psychological problems (e.g., emotional problem, alcohol or drug addiction), (c) lifestyle problems (e.g., financial difficulty, divorce, trouble with law, victim of crime, death of loved one), and (d) parental functional disability. Table 1 shows the distributions for each problem for parent and offspring, as well as the categories in bold (i.e., physical, psychological, lifestyle problems).
Table 1.
Proportion of Aging Parents, Midlife Adults, and Grown Children Suffering Each Type of Problem
| Adult children (n = 1,785) | Midlife adults (N = 633) | Aging parents (n = 868) | |
|---|---|---|---|
| Physical problems | .07 | .41 | .48 |
| Physical impairment | .03 | .09 | — |
| Serious health problem or injury | .05 | .38 | .50 |
| Poor physical healtha | .01 | .04 | .14 |
| Psychological problems | .10 | .14 | .17 |
| Emotional problem | .07 | — | .17 |
| Drinking or drug addiction | .04 | .02 | .03 |
| Depression problemb | — | .05 | — |
| Anxiety disorder | — | .11 | — |
| Lifestyle problems | .32 | .16 | .56 |
| Financial problem | .22 | .16 | .10 |
| Divorce or relationship problem | .09 | — | .07 |
| Trouble with law or police | .07 | — | — |
| Victim of a crime | .05 | — | .05 |
| Death of loved one | — | — | .49 |
| Functional disabilities | — | — | .32 |
Notes: All problems were coded as 1 = having this problem and 0 = not having this problem unless otherwise specified. Numbers in bold represent the category of problem entered in the latent profile analysis.
aPhysical health was rated from 1 = poor to 5 = excellent; we recoded as 1 = poor physical health and 0 = not in poor physical health for ratings > 1. bFive depressive symptoms from the Brief Symptom Inventory were rated from 1 = not at all, 2 = a little bit, 3 = moderately, 4 = quite a bit, and 5 = extremely; we recoded means across items > 3 as 1 = having a depression problem and 0 = no depression problem.
Participants’ Problems
Unfortunately, participants did not complete the same problems list for themselves as for their grown children or parents. Instead, participants completed a three-item problem list indicating whether they had experienced physical health problems, drinking or drug problems, and financial difficulties in the past year (1 = yes, 0 = no). In addition, they rated their own physical health in the past year (1 = poor to 5 = excellent); we recoded 1 = poor in the physical problems category. Participants indicated whether they had any enduring physical impairment (1 = yes, 0 = no). Participants completed the Patient Health Questionnaire (PHQ) anxiety scale (Spitzer, Kroenke, & Williams, 1999). We used the screening question for anxiety disorder whether the participant had an anxiety attack in the past month (1 = yes, 0 = no).
SES and Background Information
Participants provided their education in years. The sample was comparable to the general population of the Philadelphia area with regard to 2007 household income (M = 4.40, SD = 1.45, 1 = less than $10,000, 2 = $10,001–$25,000, 3 = $25,001–$40,000, 4 = $40,001–$75,000, 5 = $75,001–$100,000, and 6 = more than $100,000), though slightly better educated (M = 14.38 years of education; U.S. Census Bureau, 2008; see Fingerman et al., 2011).
Participants reported their own age, gender (1 = male, 0 = female), ethnicity/race (1 = ethnic or racial minority, 0 = non-Hispanic White), number of children, and number of living parents. Because participant age and ethnicity/race was highly correlated with parent and offspring age and ethnicity, we included participant variables for the family.
Depressive Symptoms
Participants also reported their depressive symptoms in the past 7 days using five items from the Brief Symptom Inventory (Derogatis & Melisaratos, 1983). Example items included feeling no interest in things and feelings of worthlessness. Items were rated from 1 = not at all to 5 = extremely. Scores were low on average (M = 1.47, SD = 0.65; α = .83).
Analytic Strategy
We conducted latent profile analysis (LPA) to identify family constellations of problems (Mplus 7.4; Asparouhov & Muthén, 2008). LPA allows continuous variables (e.g., proportion of parents or children suffering a problem) and categorical variables (e.g., whether participant suffered a problem) to generate probable profile membership using maximum likelihood techniques. We included indicators of problems for the parents’, participants’ and offspring’s physical, psychological, and lifestyle problems, as well as parental disability. Because each family had different numbers of family members, we used the proportion of parents or grown children who suffered from at least one problem in each category (e.g., lifestyle, physical, psychological for grown children; see Table 2). For participants, we used dichotomous indicators; whether participants suffered from at least one problem in the problem categories (yes/no).
Table 2.
Membership Probabilities and Item Response Means/Probabilities of the Four-Latent Profile Model
| Profile 1 | Profile 2 | Profile 3 | Profile 4 | F or χ2 | |
|---|---|---|---|---|---|
| Variable | Lowest problems (58%) | Parent physical problems and disability (26%) | Offspring and parent moderate physical problems (14%) | Offspring highest problems (2%) | |
| Young adult children | |||||
| Physical problemsa | .00 | .00 | .39 | .98 | 3,225.70*** |
| Psychological problemsb | .08 | .13 | .15 | .21 | 4.52** |
| Lifestyle problemsc | .29 | .37 | .39 | .45 | 3.55* |
| Midlife adults | |||||
| Physical problemsd | .39 | .40 | .49 | .57 | 4.86 |
| Psychological problemsd | .11 | .16 | .21 | .14 | 6.50 |
| Lifestyle problemsd | .12 | .19 | .21 | .21 | 6.64 |
| Aging parents | |||||
| Physical problemsc | .39 | .76 | .54 | .46 | 27.45*** |
| Psychological problemsa | .13 | .28 | .20 | .36 | 7.37*** |
| Lifestyle problemsb | .55 | .62 | .63 | .71 | 1.67 |
| Disabilitye | .08 | .98 | .34 | .32 | 577.45*** |
Note: ANOVA = analysis of variance. We used ANOVA to compare proportions of young adult children and parents who suffered different categories of problems across profiles. We used chi-square tests to compare proportions of midlife adults who suffered each category of problems.
aProportion of adult children or parents suffering a physical problem (i.e., physical impairment, serious health problem or injury, poor physical health). bProportion of adult children or parents suffering a psychological problem (i.e., emotional problem, drinking or drug problem). cProportion of adult children or parents suffering a lifestyle problem (i.e., financial problem, relationship problem or divorce, trouble with law/police, victim of a crime). dWhether midlife participants suffered a physical/psychological/lifestyle problem (1 = yes, 0 = no). eProportion of aging parents with functional disability (e.g., tasks of personal care, transportation, and finances).
*p < .05. **p < .01. ***p < .001.
First, we examined models with differing numbers of profiles and comparisons of the “fit” of those models to the data. We used various model fit indices to establish the optimal number of profiles, including log likelihood, Bayesian information criterion (BIC) and adjusted BIC (ABIC) across different models, Lo–Mendell–Rubin (LMR) test and Vuong–Lo–Mendell–Rubin (VLMR) test, and entropy.
LPA generates the probability of membership in each profile or estimates of the proportion of the sample that would be expected to belong to each latent category. We examined the profiles to understand how problems distribute over generations in different families.
We also used multinomial logistic regression to predict the “most-likely” profile membership based on the latent class posterior distribution from socioeconomic variables (e.g., income, education). Multinomial regression requires a referent category; we repeated this analysis using different profiles as the reference category to provide all possible comparisons.
Finally, we estimated a regression examining midlife participants’ depressive symptoms with profile membership as a predictor. Again, we repeated this analysis, with each of the profiles as the reference. In regression analyses, we treated midlife participant’s age, gender, minority status, number of children, and number of parents in the family as covariates.
Results
Profiles of Family Problems
As can be seen in Table 1, a third of offspring suffered lifestyle problems, but fewer than a tenth incurred psychological or physical problems. Many midlife adults suffered a physical problem, but fewer than one fifth suffered psychological or lifestyle problems. Approximately half of parents suffered lifestyle and physical problems and one third suffered functional disability, with fewer parents experiencing psychological problems.
We examined model fit statistics for two, three, and four profiles of family problems (see Supplementary Table 1). The model did not converge for five or more profiles. The four-profile model constituted the best possible fit.
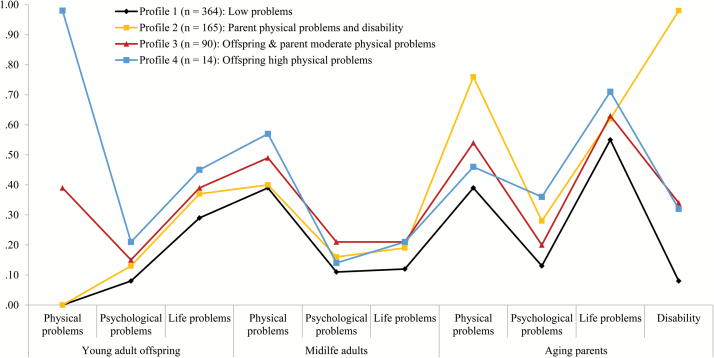
Figure 1 illustrates distributions of problems for grown children, midlife participants, and aging parents for the four profiles. The proportion of family members who suffered each type of problem is shown in Table 2, with analyses of variance (ANOVAs; with Tukey’s post hoc comparisons) and χ2 tests between profile membership and distributions for each category of problems.
Figure 1.
Item response means and probabilities of family problem indicators across generations (N = 633).
In describing profiles, we focus on significant differences. No significant differences emerged by profile for any type of midlife adults’ problems or for parents’ lifestyle problems. Thus, all profiles included midlife adults who suffered moderate physical problems (and lower lifestyle and psychological problems), and over half of parents suffered lifestyle problems. Labels for the profiles describe differences, but these similarities were shared across profiles (see Table 2).
Profile 1 (which accounted for 58% of families) fit an expected pattern of comparatively lower levels of problems. Tukey’s post hoc tests revealed that Profile 1 had lower distributions with regard to each type of problem with a significant ANOVA (i.e., offspring’s psychological, lifestyle, physical problems, parents’ psychological, physical, and disability problems).
Remaining families were distributed across three complex profiles that did not fit expected patterns. About a quarter of families fell in Profile 2 (26%), characterized by aging parents with the highest rates of physical and disability problems. In this profile, offspring had some psychological and lifestyle problems, but post hoc tests showed they did not differ from Profile 1 on any offspring problems.
Profile 3 (14%) included adult offspring and parents who suffered moderate problems. For offspring problems, 15% suffered psychological problems (compared to 8% in Profile 1) and 39% suffered physical problems (compared to 0% in Profiles 1 and 2). Some parents suffered physical problems (54%) and disability (34%; but fewer than in Profile 2 which had 98%). Thus, in these families, offspring and parents incurred moderate problems.
Profile 4 included few families (2%) and was distinguished by nearly all young adults in the family suffering physical problems (98%). Profile 4 also had significantly more offspring with psychological problems (36%) than the other groups. We note that more offspring appear to have lifestyle problems in Profile 4 and suspect the lack of significant difference reflects small group size (i.e., a larger sample may reveal offspring in this profile also differ on lifestyle problems). Parents in this profile had only moderate physical problems and disability compared with Profile 2 (but did not differ significantly from other profiles on psychological or lifestyle problems in post hoc tests). Due to low frequency, we did not include Profile 4 in subsequent analyses.
SES and Background Differences in Family Profiles
Using the first three profiles with adequate distributions, we estimated multinomial regressions treating each profile as the referent category. Interestingly, we only found significant differences in income for Profile 2 (parent physical and disability problems), compared with Profile 1 (lowest problems; see Table 3). Higher income was associated with greater likelihood of families falling in Profile 1 (lowest problems) than Profile 2 (parent physical problems and disability). There were no significant SES differences between Profile 3 (parents and offspring moderate problems) and the other profiles.
Table 3.
Multinomial Logistic Regression Comparing Profile Membership by Socioeconomic Status Indicators
| Profile 1 | Profile 2 | Profile 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Lowest problems (n = 364) | Parent physical problems and disability (n = 165) | Offspring and parent moderate physical problems (n = 90) | |||||||
| Variable | B | SE | OR | B | SE | OR | B | SE | OR |
| Intercept | (Ref.) | −3.57** | 1.20 | −3.83** | 1.48 | ||||
| Incomea | (Ref.) | −0.22** | 0.08 | 0.80 | −0.13 | 0.09 | 0.88 | ||
| Education in years | (Ref.) | 0.02 | 0.06 | 1.02 | 0.04 | 0.07 | 1.04 | ||
| Midlife adult covariates | |||||||||
| Age | (Ref.) | 0.08*** | 0.02 | 1.08 | 0.05* | 0.03 | 1.05 | ||
| Genderb | (Ref.) | −0.01 | 0.20 | 0.99 | −0.25 | 0.25 | 0.78 | ||
| Minorityc | (Ref.) | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 1.00 | ||
| Number of children | (Ref.) | −0.14* | 0.07 | 0.87 | −0.02 | 0.08 | 0.99 | ||
Note: OR = odds ratio; Ref. = reference profile. Midlife adult n = 619. Fourteen midlife adults were excluded because they were categorized in Profile 4 (i.e., offspring highest problems). Model fit statistics: −2 (pseudo) log likelihood = 1,055.8, McFadden’s pseudo-R2 = .03.
a1 = less than $10,000; 2 = $10,001–$25,000; 3 = $25,001–$40,000; 4 = $40,001–$75,000; 5 = $75,001–$100,000; and 6 = more than $100,000. b0 = female and 1 = male. c0 = non-Hispanic White and 1 = ethnic or racial minority.
*p < .05. **p < .01. ***p < .001.
These analyses also showed significant associations in the control variables with older age of participant (and family members) predicting greater likelihood of membership in Profile 2 or 3. Strangely, larger families were less likely to fall in Profile 2 compared with Profile 1.
Midlife Adults’ Depressive Symptoms
We first estimated a model examining the association between depressive symptoms and the control variables. The regression was not significant, and the adjusted R2 was zero. We then estimated a model predicting depressive symptoms as a function of profile membership treating Profile 1 (lowest problems) as the reference category along with the control variables. The regression including the profile comparisons was significant, and the adjusted R2 also differed significantly from the model with only the control variables. As can be seen in Table 4, participants in Profile 1 had fewer depressive symptoms than participants in Profiles 2 or 3, controlling for gender, age, minority status, and number of children. Profiles 2 and 3 did not differ in depressive symptoms when they were treated as reference categories.
Table 4.
Regression Predicting Midlife Adults’ Depressive Symptoms From Profile Membership
| Preliminary model | Primary model | |||
|---|---|---|---|---|
| Variable | B | SE | B | SE |
| Intercept | 1.60*** | 0.28 | 1.64*** | 0.28 |
| Profile membership | ||||
| Profile 2: Parent physical problems and disability | — | — | 0.13* | 0.06 |
| Profile 3: Offspring and parent moderate physical problems | — | — | 0.26** | 0.08 |
| Profile 1: Lowest problems | — | — | (Ref.) | (Ref.) |
| Covariates | ||||
| Midlife adults age | −0.00 | 0.01 | −0.00 | 0.01 |
| Midlife adults gendera | −0.07 | 0.05 | −0.06 | 0.05 |
| Midlife adults minorityb | 0.00 | 0.00 | 0.00 | 0.00 |
| Number of children | 0.00 | 0.02 | 0.00 | 0.02 |
| F | 0.67 | 2.59* | ||
| Adjusted R2 | .00 | .02 | ||
Note: Ref. = reference profile. Midlife adult n = 619. Fourteen midlife adults were excluded because they were categorized in Profile 4 (i.e., offspring highest problems). Depressive symptoms were rated from 1 = not at all to 5 = extremely.
a0 = female and 1 = male. b0 = non-Hispanic White and 1 = ethnic or racial minority.
*p < .05. **p < .01. ***p < .001.
Tests of Stability of Findings
We re-estimated analyses to assure stability of findings. Due to the small number of families in Profile 4, we attempted a three-profile solution. The three profiles were similar to Profiles 1 through 3 presented here, with the current Profile 4 regrouping into Profile 3. We also generated profiles regrouping the items into (a) physical/emotional and (b) lifestyle problems (Birditt et al., 2010). We still found four profiles, but those profiles were differentiated more so by parents’ level of disability and problems than by young adults’ problems.
Discussion
This study examined profiles of physical, psychological, and lifestyle problems and functional disability across three generations. We found families differ in the likelihood the middle generation will need to respond to problems among young adult children and aging parents, with four profiles best explaining problems across generations. Midlife adults with lower incomes were more likely to be in families where parents had physical problems and disabilities than midlife adults with higher income. Furthermore, midlife adults in profiles with grown children and parents suffering problems reported more depressive symptoms, suggesting that regardless of how they “pivot” (in response to parents or children), midlife adults’ well-being may suffer.
Distributions of Problems
This study provides partial support for Tolstoy’s famous quote, “All happy families are alike, but each unhappy family is unhappy in its own way.” Over half the families fit the happy family ideal, falling into the lowest problems profile. Nevertheless, these families were not problem free; nearly half the midlife adults had a health problem and over half the parents suffered a lifestyle problem even in the lowest problems profile. These findings are consistent with recent research showing that rates of disease (and mortality) have risen among many groups of midlife adults in the United States (Case & Deaton, 2015). But these lowest problems families had fewer problems than families in the other profiles. That is, fewer adult offspring had physical, psychological, or lifestyle problems, and a smaller proportion of parents suffered psychological and physical problems than in other profiles; and most aging parents were free of disability. As such, these “happy” families were generally well-off.
The remaining families were not each unhappy in their own way, however; rather, these families clustered in three profiles. In the second profile, most parents suffered functional disabilities, physical problems, and lifestyle problems and some offspring suffered lifestyle problems. The high rates of parental disability and problems are consistent with gerontological research showing such problems increase in late life, and are more likely to occur for some individuals (e.g., lower educated) than other individuals (Chiu & Wray, 2011; Fauth, Zarit, Malmberg, & Johansson, 2007). Findings from this study suggest that higher rates among older adults’ problems may distinguish certain families.
In a third profile, the parents and the offspring were moderately likely to have many types of problems. This third profile is consistent with studies regarding midlife adults’ support to multiple generations; midlife adults who support the older generation with health problems also often help grown children due to problems (Fingerman et al., 2011; Grundy & Henretta, 2006). This profile also may represent the greatest variability within families; the proportions suggest that some members of each generation suffered problems, whereas other members of that same generation did not.
The third and fourth profiles also provide insights into families when grown children were ill and suffered psychological and lifestyle problems. Research suggests that early adulthood is a period of heightened risk, particularly for lifestyle (e.g., job loss, relationship disbanding) and mental health (e.g., depression, drug addiction) problems (Schulenberg et al., 2004). Some young adults in each profile suffered lifestyle problems, but those in Profiles 3 and 4 were more likely to do so. Furthermore, Profiles 3 and 4 included grown children suffering physical problems (particularly Profile 4). Although most young adults are healthy, those who are not may disproportionately burden families. Given rising rates of cancer and diabetes (e.g., Siegel et al., 2017) in early adulthood, these physical health crises warrant additional attention.
Nevertheless, these families may not be as distinct as LPA findings suggest. Across profiles, midlife adults accrued problems and aging parents experienced lifestyle problems. The differences seem to be subtle, with some families more likely to have parents who suffer declines of late life and other families with moderate problems among parents and offspring. As such, whether these family types are truly distinct warrants additional research attention.
SES, Age, and Family Profiles
We had speculated that SES differences would account for variations in family typologies, but low income only differentiated Profile 2, involving the highest rates of parents’ physical problems and disability. Interestingly, this profile did not differ from the lowest problems profile with regard to the young adult generations. As such, SES did not differentiate problems across all generations.
The study was limited by the absence of information regarding income and assets in the parental generation, but assumed that midlife adults’ income is associated with parental SES (Torche, 2015). If so, findings are consistent with the observation that higher SES advantages health and deters disability in late life (Hayward et al., 2015; Schoeni, Martin, Andreski, & Freedman, 2005).
Findings regarding control variables revealed that older age was associated with greater likelihood of membership in either of the more problem-ridden profiles, compared with the lowest problems profile. The age association with Profile 2 (greater likelihood of parental health problems and disability) was not surprising, but the finding regarding Profile 3 (which included moderate offspring problems) was. We had predicted offspring lifestyle and psychological problems would be more likely in younger families due to heightened risks at the transition to adulthood (Schulenberg et al., 2004), but here, older families were more likely to have offspring with such problems. Indeed, this profile suggests adults may be more likely to end up as a pivot generation later in midlife, with parents and offspring who suffer problems. Longitudinal research is needed to understand whether this is a life course phenomenon that arises over time or is a persistent between-family difference.
Family Profiles and Midlife Adults’ Depressive Symptoms
Regarding midlife adults’ depressive symptoms, membership in the lowest problems families (Profile 1) was associated with fewer depressive symptoms than membership in the other profiles. Notably, many midlife adults in the lowest problems group still reported their own physical, psychological, or lifestyle problems, but lower depressive symptoms seemed to stem from the comparatively lower problems among their parents and offspring.
Prior research has shown that children’s problems are associated with poorer well-being for midlife parents (Fingerman et al., 2012; Suitor et al., 2017; Umberson et al., 2010). Based on the intergenerational stake (Birditt et al., 2015; Giarrusso et al., 2005), we had expected children’s problems to be more strongly associated with midlife adults’ depressive symptoms than parents’ problems. Here, profiles with either generations’ problems were associated with depressive symptoms in similar ways; children’s problems did not have a greater impact than parents’ problems. Future research should clarify whether any type of problems in the older and younger generations puts the middle generation at risk of diminished well-being.
Implications and Limitations of the Current Study
The study was limited in several respects. This study focused on between-family differences, but prior studies have shown that within the same family, some children suffer problems, whereas others do not (Fingerman et al., 2009; Pillemer et al., 2017; Suitor et al., 2016). To the best of our knowledge, only one study has examined within-family differences using typologies (Kim, Fingerman, Birditt, & Zarit, 2016). Such an analysis requires a measure of within-family variability (i.e., standard deviation in ratings). This study used dichotomous (yes/no) ratings of problems. Future research might include continuous ratings of intensity of problems to incorporate within-family differences.
In addition, the midlife adults provided information on all three generations’ problems, and findings may be influenced by bias in reporting. Nevertheless, the profiles suggest we did not merely capture a negativity bias (whereby midlife adults with a greater number of depressive symptoms perceive more problems across generations); rather, three profiles of problems were associated with more depressive symptoms. Indeed, midlife adults’ reports of their own problems did not differentiate groups. Of course, midlife adults did not complete the full list of problems for themselves (as they did for family members); future studies should include parallel measures.
Furthermore, despite a burgeoning literature using typology approaches (Dykstra & Fokkema, 2011; Fiori et al., 2017; Hogerbrugge & Silverstein, 2015; Kim et al., 2015), profiles are not completely stable and involve subjective interpretation. Here, we also estimated the profiles combining physical and emotional problems (Birditt et al., 2010; Pillemer et al., 2007); doing so generated slightly different profiles in which the older adults’ problems distinguished groups more so than the young adults’ problems. Nevertheless, the patterns were similar and findings regarding SES and midlife adults’ depressive symptoms were the same. Thus, typologies may provide insights into family demands midlife adults face.
In sum, regardless of their own problems, midlife adults in the “pivot generation” (Attias-Donfut & Wolff, 2000; Fingerman et al., 2011) may commonly respond to grown children and parents who encounter problems. Prior studies have taken a variable-centered approach examining problems in each generation separately. This study identified patterns of problems across multiple generations in families. Future research also should identify risk factors associated with each family typology to ascertain how different combinations of problems arise.
Supplementary Material
Supplementary data are available at The Gerontologist online.
Funding
This study was supported by grants from the National Institute on Aging (NIA), R01AG027769, Family Exchanges Study II (K. L. Fingerman, Principal Investigator) and R03AG048879, Generational Family Patterns and Well-Being (K. Kim, Principal Investigator). The MacArthur Network on an Aging Society (J. W. Rowe, Network Director) provided funds. This research also was supported by grant, 5 R24 HD042849 awarded to the Population Research Center (PRC) at the University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Conflict of Interest
None reported.
Supplementary Material
References
- Agrawal A., & Lynskey M. T (2008). Are there genetic influences on addiction: Evidence from family, adoption and twin studies. Addiction, 103, 1069–1081. doi:10.1111/j.1360-0443.2008.02213.x [DOI] [PubMed] [Google Scholar]
- Asparouhov T., & Muthén B (2008). Multilevel mixture models. In G. R. Hancock & K. M. Samuelsen (Eds.), Advances in latent variable mixture models (pp. 27–51). Charlotte, NC: Information Age Publishing, Inc. [Google Scholar]
- Attias-Donfut C., & Wolff F.-C (2000). The redistributive effects of generational transfers. In S. Arbur & C. Attias-Donfut (Eds.), The myth of generational conflict: The family and state in ageing societies (pp. 22–46). New York: Routledge. [Google Scholar]
- Bangerter L. R., Zarit S. H., & Fingerman K. L (2016). Moderators of mother’s problems on middle-aged offspring depressive symptoms. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71, 41–48. doi:10.1093/geronb/gbu081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassett S. S., & Folstein M. F (1991). Cognitive impairment and functional disability in the absence of psychiatric diagnosis. Psychological Medicine, 21, 77–84. doi:10.1017/S0033291700014677 [DOI] [PubMed] [Google Scholar]
- Birditt K. S., Fingerman K. L., & Zarit S. H (2010). Adult children’s problems and successes: Implications for intergenerational ambivalence. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65, 145–153. doi:10.1093/geronb/gbp125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt K. S., Hartnett C. S., Fingerman K. L., Zarit S., & Antonucci T. C (2015). Extending the intergenerational stake hypothesis: Evidence of an intraindividual stake and implications for well-being. Journal of Marriage and Family, 77, 877–888. doi:10.1111/jomf.12203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt K. S., Kim K., Zarit S. H., Fingerman K. L., & Loving T. J (2016). Daily interactions in the parent-adult child tie: Links between children’s problems and parents’ diurnal cortisol rhythms. Psychoneuroendocrinology, 63, 208–216. doi:10.1016/j.psyneuen.2015.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U., & Morris P. A (2006). The bioecological model of human development. In W. Damon & R. M. Lerner (Eds.), Handbook of child psychology, Vol. 1: Theoretical models of human development (6th ed., pp. 793–828). New York: Wiley. [Google Scholar]
- Case A., & Deaton A (2015). Rising morbidity and mortality in midlife among white and non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences of the United States of America, 112, 15078–15083. doi:10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu C. J., & Wray L. A (2011). Physical disability trajectories in older Americans with and without diabetes: The role of age, gender, race or ethnicity, and education. The Gerontologist, 51, 51–63. doi:10.1093/geront/gnq069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis N. A., & Fowler J. H (2013). Social contagion theory: Examining dynamic social networks and human behavior. Statistics in Medicine, 32, 556–577. doi:10.1002/sim.5408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger R. D., & Donnellan M. B (2007). An interactionist perspective on the socioeconomic context of human development. Annual Review of Psychology, 58, 175–199. doi:10.1146/annurev.psych.58.110405.085551 [DOI] [PubMed] [Google Scholar]
- Derogatis L. R., & Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13, 595–605. doi:10.1017/S0033291700048017 [PubMed] [Google Scholar]
- Dykstra P. A., & Fokkema T (2011). Relationships between parents and their adult children: A west European typology of late-life families. Ageing and Society, 31, 545–569. doi:10.1017/S0144686X10001108 [Google Scholar]
- Elder G. H., Jr (1998). The life course as developmental theory. Child Development, 69, 1–12. doi:10.1111/j.1467-8624.1998.tb06128.x [PubMed] [Google Scholar]
- Fauth E. B., Zarit S. H., Malmberg B., & Johansson B (2007). Physical, cognitive, and psychosocial variables from the Disablement Process Model predict patterns of independence and the transition into disability for the oldest-old. The Gerontologist, 47, 613–624. doi:10.1093/geront/47.5.613 [DOI] [PubMed] [Google Scholar]
- Fingerman K. L., & Bermann E (2000). Applications of family systems theory to the study of adulthood. International Journal of Aging and Human Development, 51, 5–29. doi:10.2190/7TF8-WB3F-TMWG-TT3K [DOI] [PubMed] [Google Scholar]
- Fingerman K. L., Cheng Y.-P., Birditt K., & Zarit S (2012). Only as happy as the least happy child: Multiple grown children’s problems and successes and middle-aged parents’ well-being. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 184–193. doi:10.1093/geronb/gbr086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman K. L., Kim K., Davis E. M., Furstenberg F. F. Jr., Birditt K. S., & Zarit S. H (2015). “I’ll give you the world”: Socioeconomic differences in parental support of adult children. Journal of Marriage and Family, 77, 844–865. doi:10.1111/jomf.12204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman K. L., Miller L., Birditt K., & Zarit S (2009). Giving to the good and the needy: Parental support of grown children. Journal of Marriage and Family, 71, 1220–1233. doi:10.1111/j.1741-3737.2009.00665.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman K. L., Pitzer L. M., Chan W., Birditt K., Franks M. M., & Zarit S (2011). Who gets what and why? Help middle-aged adults provide to parents and grown children. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66, 87–98. doi:10.1093/geronb/gbq009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiori K. L., Rauer A. J., Birditt K. S., Brown E., Jager J., & Orbuch T. L (2017). Social network typologies of Black and White married couples in midlife. Journal of Marriage and Family, 79, 571–589. doi:10.1111/jomf.12330 [Google Scholar]
- Giarrusso R., Feng D., & Bengtson V. L (2005). The intergenerational stake over 20 years. In M. Silverstein & K. W. Schaie (Eds.), Annual review of gerontology and geriatrics: Vol. 24. Intergenerational relations across time and place (pp. 55–76). New York: Springer. [Google Scholar]
- Greenfield E. A., & Marks N. F (2006). Linked lives: Adult children’s problems and their parents’ psychological and relational well-being. Journal of Marriage and Family, 68, 442–454. doi:10.1111/j.1741-3737.2006.00263.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy E., & Henretta J. C (2006). Between elderly parents and adult children: A new look at the intergenerational care provided by the “sandwich generation.” Ageing and Society, 26, 707–722. doi:10.1017/S0144686X06004934 [Google Scholar]
- Hay E. L., Fingerman K. L., & Lefkowitz E. S (2008). The worries adult children and their parents experience for one another. International Journal of Aging and Human Development, 67, 101–127. doi:10.2190/AG.67.2.a [DOI] [PubMed] [Google Scholar]
- Hayward M. D., Hummer R. A., & Sasson I (2015). Trends and group differences in the association between educational attainment and U.S. adult mortality: Implications for understanding education’s causal influence. Social Science and Medicine, 12, 8–18. doi:10.1016/j.socscimed.2014.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogerbrugge M. J., & Silverstein M. D (2015). Transitions in relationships with older parents: From middle to later years. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 481–495. doi:10.1093/geronb/gbu069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston D. W., Schurer S., & Shields M. A (2013). Exploring the intergenerational persistence of mental health: Evidence from three generations. Journal of Health Economics, 32, 1077–1089. doi:10.1016/j.jhealeco.2013.09.001 [DOI] [PubMed] [Google Scholar]
- Kim K., Bangerter L. R., Liu Y., Polenick C. A., Zarit S. H., & Fingerman K. L (2017). Middle-aged offspring’s support to aging parents with emerging disability. The Gerontologist, 57, 441–450. doi:10.1093/geront/gnv686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K., Fingerman K. L., Birditt K. S., & Zarit S. H (2016). Capturing between- and within-family differences in parental support to adult children: A typology approach. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71, 1034–1045. doi:10.1093/geronb/gbv029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K., Zarit S. H., Fingerman K. L., & Han G (2015). Intergenerational exchanges of middle-aged adults with their parents and parents-in-law in Korea. Journal of Marriage and Family, 77, 791–805. doi:10.1111/jomf.12185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoester C. (2003). Transitions in young adulthood and the relationship between parents and offspring well-being. Social Forces, 81, 1431–1458. doi:10.1353/sof.2003.0063 [Google Scholar]
- Kraft P., & Hunter D. J (2009). Genetic risk prediction – Are we there yet?The New England Journal of Medicine, 360, 1701–1703. doi:10.1056/NEJMp0810107 [DOI] [PubMed] [Google Scholar]
- McPherson M., Smith-Lovin L., & Cook J. M (2001). Birds of a feather: Homophily in social networks. Annual Review of Sociology, 27, 415–444. doi:10.1146/annurev.soc.27.1.415 [Google Scholar]
- Pillemer K., Suitor J. J., Mock S. E., Sabir M., Pardo T. B., & Sechrist J (2007). Capturing the complexity of intergenerational relations: Exploring ambivalence within later-life families. Journal of Social Issues, 63, 775–791. doi:10.1111/j.1540-4560.2007.00536.x [Google Scholar]
- Pillemer K., Suitor J. J., Riffin C., & Gilligan M (2017). Adult children’s problems and mothers’ well-being. Research on Aging, 39, 375–395. doi:10.1177/0164027515611464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M., & Sörensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250–267. doi:10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Plomin R., Lichtenstein P., Pedersen N. L., McClearn G. E., & Nesselroade J. R (1990). Genetic influence on life events during the last half of the life span. Psychology and Aging, 5, 25–30. doi:10.1037/0882-7974.5.1.25 [DOI] [PubMed] [Google Scholar]
- Repetti R. L., Taylor S. E., & Seeman T. E (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128, 330–366. doi:10.1037/0033-2909.128.2.330 [PubMed] [Google Scholar]
- Rhee S. H. (in press). Life events. In M. Borstein M. Arterberry K. L. Fingerman, & J. Lansford (Eds.), Encyclopedia of lifespan development. Thousand Oaks, CA: Sage. [Google Scholar]
- Rowe J. W., & Kahn R. L (1997). Successful aging. The Gerontologist, 37, 433–440. doi:10.1093/geront/37.4.433 [DOI] [PubMed] [Google Scholar]
- Rowe J. W., & Kahn R. L (2015). Successful Aging 2.0: Conceptual expansions for the 21st century. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70, 593–596. doi:10.1093/geronb/gbv025 [DOI] [PubMed] [Google Scholar]
- Schoeni R. F., Martin L. G., Andreski P. M., & Freedman V. A (2005). Persistent and growing socioeconomic disparities in disability among the elderly: 1982-2002. American Journal of Public Health, 95, 2065–2070. doi:10.2105/AJPH.2004.048744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg J. E., Sameroff A. J., & Cicchetti D (2004). The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology, 16, 799–806. doi:10.1017/S0954579404040015 [DOI] [PubMed] [Google Scholar]
- Siegel R. L., Fedewa S. A., Anderson W. F., Miller K. D., Ma J., Rosenberg P. S., & Jemal A (2017). Colorectal cancer incidence patterns in the United States, 1974–2013. Journal of the National Cancer Institute, 109, 1–6. doi:10/1093/jnci/djw322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R. L., Kroenke K., & Williams J. B (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA, 282, 1737–1744. doi:10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- Suitor J. J., Gilligan M., Peng S., Con G., Rurka M., & Pillemer K (2016). My pride and joy? Predicting favoritism and disfavoritism in mother-adult child relations. Journal of Marriage and Family, 78, 908–925. doi:10.1111/jomf.12288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suitor J. J., Gilligan M., Pillemer K., Fingerman K. L., Kim K., Silverstein M., & Bengtson V. L (2017). Applying within-family differences approaches to enhance understanding of the complexity of intergenerational relations. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. Advance online publication. doi:10.1093/geronb/gbx037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz T. T. (2008). Family capital and the invisible transfer of privilege: Intergenerational support and social class in early adulthood. New Directions for Child and Adolescent Development, 2008, 11–24. doi:10.1002/cd.206 [DOI] [PubMed] [Google Scholar]
- Torche F. (2015). Analyses of intergenerational mobility: An interdisciplinary review. The Annals of the American Academy of Political and Social Science, 657, 37–62. doi:10.1177/0002716214547476 [Google Scholar]
- Umberson D., Pudrovska T., & Reczek C (2010). Parenthood, childlessness, and well-being: A life course perspective. Journal of Marriage and Family, 72, 612–629. doi:10.1111/j.1741-3737.2010.00721.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (2008). 2007 American Community Survey. Retrieved October 20, 2008, from http://factfinder.census.gov [Google Scholar]
- Wolfinger N. H. (2011). More evidence for trends in the intergenerational transmission of divorce: A completed cohort approach using data from the general social survey. Demography, 48, 581–592. doi:10.1007/s13524-011-0025-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.