Abstract
Objectives
The aim of this systematic review was to provide an overview of time to return to work (RTW) after carpal tunnel release (CTR), including return to different occupations and working patterns.
Methods
A systematic search from inception to 2016 was conducted using nine electronic databases, trial registries and grey literature repositories. Randomized controlled trials and observational studies reporting RTW times after CTR were included. Study risk of bias was assessed using Cochrane risk of bias assessment tools. Time to RTW was summarized using median and range.
Results
Fifty-six relevant studies were identified: 18 randomized controlled trials and 38 observational studies. Only four studies were rated as low risk of bias. Reported return to work times ranged from 4-168 days. Few studies reported occupational information. Among six studies, median time to return to non-manual work was 21 days (range 7-41), compared with 39 days for manual work (range 18-101). Median time to return to modified or full duties was 23 days (ranges 12-50 and 17-64, respectively), as reported by three studies. There was no common method of defining, collecting or reporting RTW data.
Conclusions
This review highlights wide variation in reported RTW times after CTR. Whilst occupational factors may play a role, these were poorly reported and there is currently limited evidence to inform individual patients of their expected duration of work absence after CTR. A standardized definition of ‘return to work’ is needed, as well as an agreed method of collecting and reporting RTW data.
Key terms: Return to work, Elective hand surgery
Introduction
Carpal tunnel syndrome (CTS) is a common peripheral nerve entrapment disorder (1) and recommended treatment includes carpal tunnel release surgery (CTR) (2, 3). CTR has become a common elective operation, with more than 77 000 CTR procedures expected to be performed annually in the English NHS alone, by 2020 (4). Despite CTR being such a frequently performed procedure, there is currently no evidence-based guidance to inform patients and clinicians about when it is safe to return to work, or other activities, after their surgery. Extended work absence after CTR may have financial consequences for both the worker and employer, whereas returning to work too soon after surgery could be associated with reduced work performance, increased workplace risk due to altered grip and dexterity, or clinical complications.
Whilst there have been previous systematic reviews which included return to work (RTW) time after CTR as a measure of the effectiveness of different CTR interventions (5–9), these reviews have not explored the variation caused by occupational factors, such as the type of work, work pattern or whether participants were employed or self-employed. Moreover, ‘return to work’ may be defined in a number of ways and can include: return to full duties, return to amended duties, or return to modified working hours. To our knowledge, none of the existing reviews has considered this diversity. We therefore undertook a systematic review of the literature to address the following question: when do patients return to work after CTR, and how do occupational factors influence this timing?
Methods
The review protocol was pre-registered with PROSPERO (registration number: CRD42016034158) (10) and was carried out according to the PRISMA guidelines (11).
Selection criteria
Eligible studies were those reporting post-operative RTW time after CTR, using any surgical technique, in a working population. Randomized controlled trials (RCTs), cohort studies and case-control studies were eligible for inclusion (Table 1).
Table 1.
Review eligibility criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
Search strategy
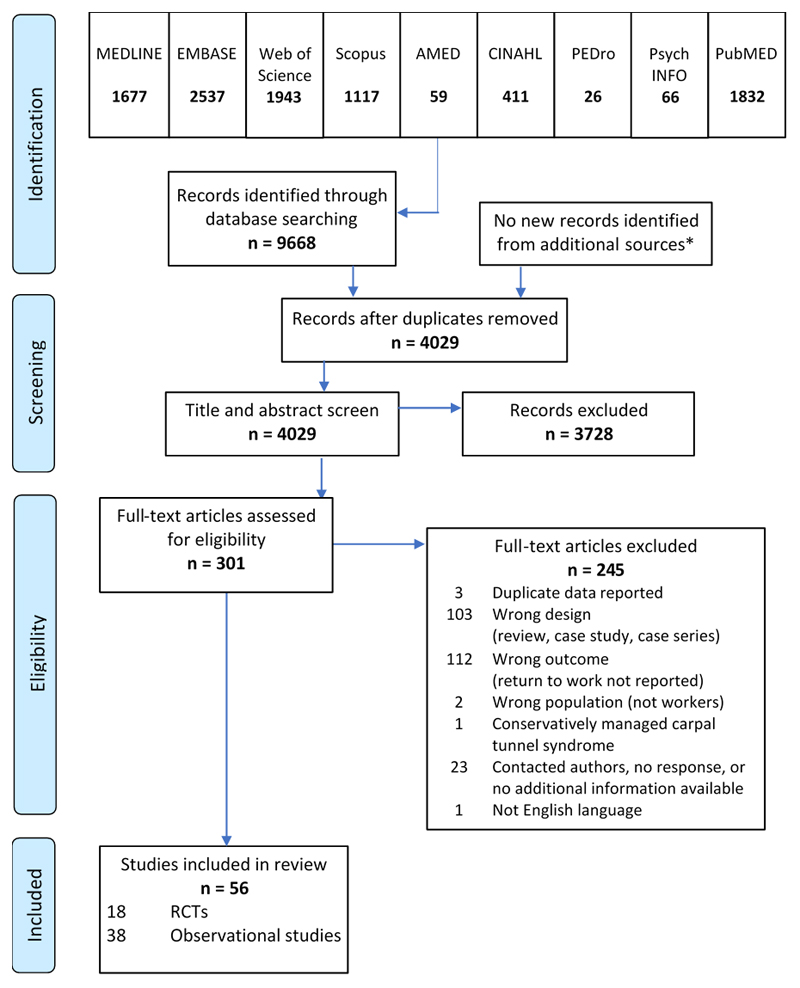
Twenty-four electronic sources were searched by the lead author between February and March 2016. These comprised electronic databases, trials registries, grey literature sources and the electronic records of four relevant journals (Figure 1). There were no restrictions for country of origin or date of publication, but due to time and resource limitations, studies were restricted to those available in the English language. The example search strategy for Medline is provided in Appendix A.
Figure 1.
Systematic review flow diagram.
Additional sources comprised:
1. Trials registries (Cochrane Central Register of Controlled trials, ClinicalTrials.gov, EU Clinical Trials Register, Alltrials.net, WHO International Clinical Trials Registry, NIHR UK Clinical Trials Gateway);
2. Grey literature databases (E-Theses Online Service, OpenThesis, ProQuest, OpenGrey, OpenDOAR;
3. Key journals (Journal of Hand Surgery [European], Journal of Hand Surgery [American], Occupational Medicine, Journal of Occupational Rehabilitation).
Eligibility assessment
Title and abstract screening was performed independently by two reviewers (LN and MS) using the Covidence web platform (www.covidence.org). Any disagreements were discussed and taken to an additional independent reviewer (KWB) if agreement was not reached. All reviewers agreed the final decision. Full text was retrieved for those articles selected from this initial screen and in cases where no abstract had been found. Full text screening was performed according to the review inclusion and exclusion criteria (Table 1), following the same process as above.
Data extraction
For the included studies, data extraction was performed independently by LN and MS using pre-piloted data extraction forms (Appendix B). Data extraction included year of publication, country of research, study population, study design, CTR surgical technique, information about workers’ compensation (or other insurance) status, post-operative management and measurement of return to work time. Where clarification or additional information were required, LN contacted the relevant author by email.
Methodological assessment
Study risk of bias was assessed independently by two reviewers (LN and KWB) using the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials and a modified version of the tool for non-randomized trials (12, 13). The items included in the risk of bias assessment are shown in Appendix C. For each item, RCTs were rated at low, unclear or high risk of bias and observational studies were rated at low, moderate, serious or critical risk of bias. When there was insufficient information to make a firm judgment about the risk of bias for an individual item, the rating ‘no information’ was used. Summary scores for observational studies were derived from the lowest score (highest risk of bias) for any single item (13). For RCTs, the absence of patient blinding was excluded from the summary score because of the difficulties with blinding patients in surgical trials. Studies were rated at low risk of bias if rated ‘low’ for all remaining domains; high risk of bias if rated ‘high’ for two additional domains; and ‘unclear’ for other scoring patterns. Following a pilot, the papers were reviewed independently and any differences in scoring were resolved and agreed by discussion.
Data synthesis
RTW data were reported in two ways: 1) the average time period from CTR to return to work; or 2) the proportion of individuals who had returned by specified time points. The duration until RTW was reported using a mixture of days, weeks and months. To enable direct comparison within the review, all durations have been reported in days. The basis of the conversion was that one week was equal to 7 days and one month equal to 30 days. In the absence of explicit information, an assumption was made that the reported RTW times included all seven days of a calendar week, regardless of the participants’ usual working pattern. Heterogeneity in both study methods and populations limited the review to a narrative analysis with summary descriptive statistics. Duration before RTW was summarized using the median and range. For each summary calculation, the number of studies and observations (study arms) that provided these data were documented. Due to inconsistent reporting of the number of workers in the included studies, summary data was not weighted for sample size.
Results
Study characteristics
Results for each stage of the literature search and reasons for exclusion are shown in Figure 1. A total of 4029 individual records were identified, of which 56 met the review inclusion criteria; 18 RCTs and 38 observational studies. Twenty-four authors were contacted for additional information, with only one providing clarification that enabled the study to be included (14). We found that two papers reported on the same study participants (15, 16), but as different RTW analyses were undertaken, both have been included in this review. Participant numbers and demographics were only counted once for these reports. The included research took place in 16 countries, primarily in North America and Europe, with three studies in Asia and one in Israel. Publication dates ranged from 1992-2016.
Participants
The 56 included studies comprised 14 335 CTR patients (1551 from RCTs, 7328 from cohort studies and 5456 from a single case control study). Seven studies did not report the age of participants (14, 17–22) and seven did not report the sex (18–21, 23–25). The mean age of CTR participants in the RCTs ranged between 44-60 years, as compared with 37-66 years in the cohort studies. The male/female ratio of participants was 1:2.4 for RCTs and cohort studies and 1:3 for the case-control study. Study characteristics and reported duration until RTW are shown in Appendix D.
We found that study inclusion and exclusion criteria varied widely between studies. For example, there were no consistently reported methods of CTS diagnosis. Furthermore, six studies included only unilateral CTS (26–31); seven included only bilateral CTS (32–38); 29 included individuals undergoing either unilateral or bilateral CTR (16, 20–25, 39–60); and 14 studies did not report whether participants had unilateral or bilateral CTS or CTR (14, 17–19, 48, 61–69).
Duration until RTW was reported by all included studies, however six RCTs (18, 32, 40, 42, 45, 63) and seven cohort studies (37, 38, 52, 54–56, 60) did not specify the number of individuals included in their RTW analyses. With the pragmatic assumption that, where unreported, all participants provided RTW data, this yielded a total of 1263 workers from RCTs, 7071 from cohort studies and 1529 from one case control study.
Methodological assessment
The risk of bias assessments are summarized in Appendix C. Overall, only four studies were rated at low risk of bias: one RCT (27), two cohort studies (48, 69) and one case control study (14). This compared with 27 studies rated at moderate or unclear risk of bias and 25 studies rated at high, serious or critical risk of bias. Common concerns centered on the assessment and reporting of RTW data; issues with the selection of participants for observational studies; and the lack of assessor blinding for RTW data in RCTs.
Measurement of return to work timescales
There was no common method of defining or collecting RTW data. Only 36 studies (64%) reported any information on how the period of post-operative work absence was calculated. Of these, three non-hierarchical categories were identified based on the method of RTW data collection: 1) regional/national databases (14, 27, 31); 2) patient reported questionnaires or telephone interviews (15–17, 22, 25, 29, 37, 40, 42, 48–50, 52, 60, 68); and 3) medical records. For the latter, RTW information was either recorded during clinical assessment (18, 20, 30, 35, 39, 44, 47, 51, 53, 63, 69) or was extracted retrospectively from the records (24, 38, 54, 56–58, 65).
Return to work timescales
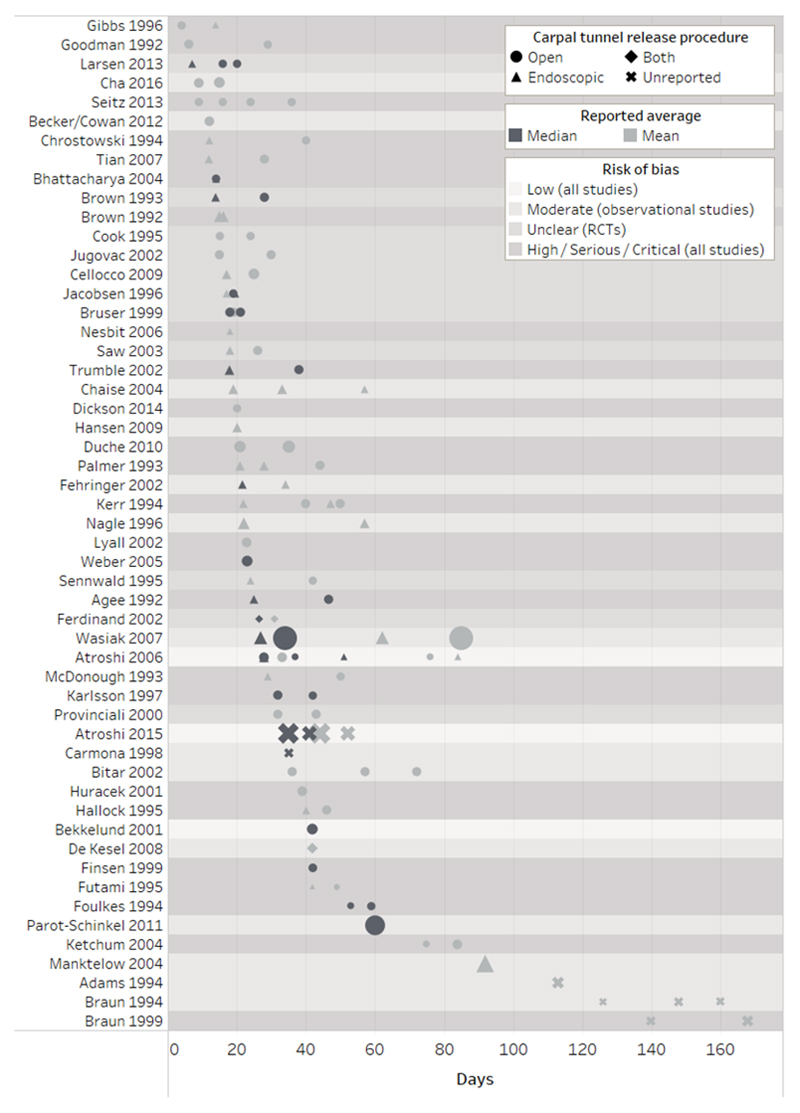
Figure 2 shows the average time to RTW for the included studies. Only 19 studies summarized RTW time as a median. Median RTW time in these studies ranged from 7-60 days with an overall median of 28 days. Forty-one studies reported mean RTW times, ranging from 4-168 days, with the overall median of 30 days (Table 2). Of the 56 included studies, only eight reported median RTW time and range or interquartile range (14, 27, 32, 35, 42, 46, 48, 55), while 24 studies provided a single point estimate with no measure of the spread of the data. Table 2 summarizes the reported duration to RTW according to different study characteristics: study type, CTR procedure, sample size, RTW data collection method, study location and risk of bias score. Details from the individual studies, including characteristics and reported RTW times are provided in Appendix D.
Figure 2.
Reported return to work times following carpal tunnel release according to surgical procedure, point estimate (median/mean) and study risk of bias.
Symbol size represents the number of study participants per study arm (range 3 to 1410).
Table 2.
Summary of reported return to work times according to methodological characteristics.
| Subgroup | Studies | Observations A | Return to work time reported as median (days) |
Studies | Observations A | Return to work time reported as mean (days) |
||
|---|---|---|---|---|---|---|---|---|
| Median | Range | Median | Range | |||||
| All studies | 19 | 35 | 28 | 7-60 | 41 | 81 | 30 | 4-168 |
| Study | ||||||||
| Randomised controlled trials | 11 | 24 | 26 | 7-59 | 11 | 23 | 25 | 12-84 |
| Observational study | 8 | 11 | 35 | 21.5-60 | 30 | 58 | 36 | 4-168 |
| CTR procedure | ||||||||
| Open CTR | 15 | 21 | 34 | 14-60 | 29 | 44 | 29.5 | 4-85 |
| Endoscopic CTR | 9 | 10 | 18.75 | 7-51 | 21 | 28 | 22 | 12-92 |
| Procedure not reported | 3 | 4 | 35 | 26.5-41 | 6 | 10 | 119.5 | 31-168 |
| Sample size | ||||||||
| <30 workers | 7 | 14 | 23.25 | 7-59 | 17 | 28 | 29 | 4-126 |
| 30-100 workers | 9 | 15 | 28 | 14-46.5 | 24 | 40 | 31 | 6-168 |
| >100 workers | 4 | 6 | 38 | 27-60 | 9 | 13 | 44 | 15-140 |
| Source of return to work data | ||||||||
| Regional or national databases | 3 | 8 | 34.5 | 27-51 | 3 | 8 | 57 | 28-85 |
| Questionnaires or interviews | 4 | 5 | 53 | 35-60 | 9 | 14 | 23 | 4-92 |
| Medical records | 3 | 4 | 22.25 | 14-28 | 15 | 32 | 36 | 6-160 |
| Not reported | 7 | 14 | 23 | 14-46.5 | 14 | 27 | 22 | 6-168 |
| Location | ||||||||
| Scandinavia | 8 | 18 | 30 | 7-51 | 5 | 10 | 34.5 | 17-84 |
| Europe (excluding Scandinavia) | 4 | 6 | 19.5 | 14-60 | 12 | 21 | 26 | 15-57 |
| North America | 8 | 13 | 28 | 13-59 | 22 | 44 | 37 | 4-168 |
| Other | - | - | - | - | 3 | 6 | 21.5 | 9-49 |
| Risk of bias | ||||||||
| Low (all studies) | 3 | 7 | 37 | 28-51 | 2 | 6 | 48 | 28-84 |
| Moderate (observational studies) | 4 | 5 | 34 | 13-60 | 12 | 21 | 57 | 9-160 |
| Unclear (randomised controlled trials) | 5 | 10 | 19.25 | 7-28 | 9 | 17 | 24 | 15-43 |
| High/serious/critical (all studies) | 7 | 13 | 38 | 14-59 | 18 | 37 | 29 | 4-168 |
Number of study arms;
any reported health insurance including national and personal schemes. For each summary calculation, the number of studies and observations (study arms) are reported. Summary data was not weighted for sample size.
Duration of work absence did not appear to increase or decrease consistently according to the hierarchy of risk of bias categories. Interestingly, the 11 RCTs rated at unclear risk of bias generally reported faster return to work times and showed less variability than the studies in other risk of bias categories (Table 2). RTW times varied when classified according to the method of data collection; median RTW times obtained from medical records tended to be earlier than those reported in databases or collected by interviews or questionnaires. In contrast, mean RTW times reported by interview/questionnaire were earlier than those recorded by the other methods (Table 2). We found no apparent relationship between reported RTW time and year of publication.
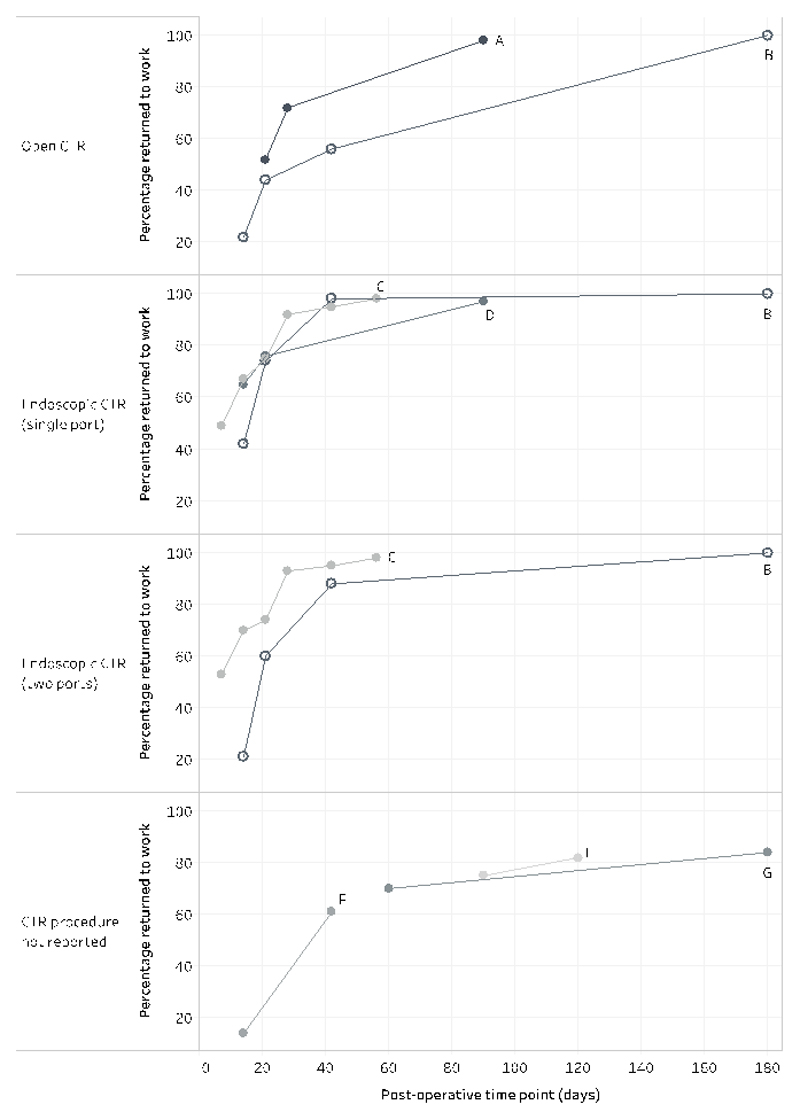
Return to work rates
Seven cohort studies reported the percentage of participants who had returned to work by different post-operative time points; however, there was minimal overlap in the timing of data collection for each study (17, 19, 29, 47, 49, 60, 69). The reported time points for at least 50% of study participants to return to work ranged from 7-42 days (Figure 3). Only one study recorded 100% return to work and this had occurred by 180 days (6 months) (60).
Figure 3.
Cumulative proportion of carpal tunnel release patients who had returned to work by the reported time points.
A. Ratzon et al. (17)
B. Palmer et al. (60)
C. Brown et al. (19)
D. Hansen et al. (29)
E. Adams et al. (47)
F. Carmona et al. (49)
G. Gimeno et al. (69)
CTR - carpal tunnel release.
Occupational information
Table 3 shows the summary RTW times for studies reporting occupational information. Six of the 56 studies reported RTW times for different job types (16, 27, 34, 50, 59, 67), and four studies distinguished between return to modified duties and return to full duties (15, 18, 35, 57). Neither the method of classifying occupation, nor the description of what constituted modified or full duties, were consistent across studies. For the purposes of this review, we classified desk-based, sedentary, white-collar or light work as ‘non-manual’; and light-repetitive, medium, heavy or blue-collar work as ‘manual’. We also defined a subgroup of ‘heavy manual’ workers which consisted of heavy manual and blue-collar work. Return to light duties, one-handed activity and light two-handed activity were classified as ‘modified duties’; return to normal or full duties were classified as ‘full duties’.
Table 3.
Summary return to work times according to reported occupational characteristics.
| Subgroup | Studies | Observations A | Return to work time reported as median (days) |
Studies | Observations A | Return to work time reported as mean (days) |
||
|---|---|---|---|---|---|---|---|---|
| Median | Range | Median | Range | |||||
| Work duties | ||||||||
| Modified duties | 1 | 1 | 13 | - | 4 | 6 | 20.5 | 12-50 |
| Full duties | 1 | 1 | 63 | - | 4 | 5 | 27 | 17-82 |
| Work type | ||||||||
| Non-manual | 1 | 1 | 21 | - | 6 | 11 | 21 | 7-49 |
| Manual | 1 | 1 | 36 | - | 6 | 14 | 39 | 18-101 |
| (Subgroup: heavy manual) | 1 | 1 | 36 | - | 3 | 4 | 46.5 | 22-101 |
| Employer | ||||||||
| Employed | - | - | - | - | 2 | 3 | 36 | 33-57 |
| Self-employed | - | - | - | - | 2 | 2 | 21 | 19-23 |
| Working pattern | ||||||||
| Part-time | - | - | - | - | 1 | 2 | 24.5 | 15-34 |
| Full-time | - | - | - | - | 1 | 2 | 12 | 10-14 |
| Workers’ compensation status | ||||||||
| Workers’ compensation | 4 | 6 | 56.5 | 27-114 | 16 | 29 | 56 | 23-160 |
| No workers’ compensation | 3 | 5 | 19 | 15-45.5 | 12 | 20 | 18.5 | 3-57 |
| Other health insurance B | 4 | 11 | 35 | 7-51 | 7 | 14 | 35 | 17-84 |
Number of study arms/subgroups. For each summary calculation, the number of studies and observations (study arms) are reported. Summary data was not weighted for sample size.
Only Gimeno et al. reported return to work rates for different levels of work functioning. They reported that by 2 months after surgery, 41% of study participants reported working normally, while 28% had work limitations. By 6 months, this had improved to 58% and 26%, respectively. At both time points, the remainder of participants had yet to return to work (69). Only one study reported RTW time separately for full- and part-time work (16) and two studies reported RTW times separately for self-employed and employed participants (50, 67).
Participants receiving workers’ compensation took longer to RTW in all studies reporting and comparing insurance types (23, 30, 35, 56, 59, 60, 65, 67). Where other insurance types were stated, such as national insurance schemes or private insurance, mean RTW times tended to be shorter than among those receiving workers’ compensation (67, 56).
Earlier RTW was found in: non-manual workers; those able to return to modified duties; full-time workers; individuals who were self-employed; and those not receiving workers’ compensation.
Return to work advice
Few studies reported that patients received any standardized return to work advice. Four studies recommended RTW as soon as possible (15, 16, 43, 60); others advised patients to return when able (26, 44) or after suture removal (39). Three studies reported that the surgeon was responsible for suggesting a RTW time (17, 21, 66); one study reported that this was the role of the General Practitioner (29); one study reported a combined decision between the surgeon and therapist (57); and two studies reported a combined decision between surgeon and patient (18, 41).
Discussion
This review systematically identified 56 studies reporting RTW timescales following CTR and compared their findings according to different occupational, clinical and study characteristics. Overall, our review points to substantial heterogeneity in the duration of work absence after CTR. Mean RTW times ranged from 4-168 days in 41 studies; median RTW times ranged from 14-60 days in 17 studies. Earlier return to work was reported following endoscopic CTR and in populations without workers’ compensation, findings that are consistent with those of previous systematic reviews (5–9, 70). We also found that return to modified duties occurred sooner than return to full duties and return to non-manual occupations were generally faster than return to manual roles. Where studies categorized the type of work, heavy manual work was associated with the longest period of work absence. This finding is supported by a recent review of the prognostic factors for RTW after CTR, which found that exposure to bending/twisting the hands at work, repetitive activities, heavy lifting and blue-collar work were all associated with delayed RTW (71).
Given that these findings might be expected, it was surprising how few studies adequately reported work-related information, such as occupation, working pattern (full-time or part-time), employment status (employed or self-employed) and availability of paid sick-leave. Only 36 studies gave a definition of RTW or described their method of collecting RTW data. Where this was defined, 50% used the participants’ medical records as their data source. Our observed lack of reporting of work-related information in the included studies may therefore be explained, in part, by an absence of routine collection, or recording, of work-related information in clinical practice.
Two studies reported return to work data for employed and self-employed individuals, and both found that those who were self-employed returned to work sooner than salaried workers (50, 67). A further two studies deliberately excluded self-employed individuals from their return to work analyses (24, 44), the assumption being that the return to work process would be notably different for these individuals. However, a recent systematic review of return to work after hip and knee arthroplasty found no difference in return to work times for employed and self-employed workers, although only two of the 19 included studies reported relevant data (72). The role of the type of work contract (permanent, fixed term, zero hours or self-employed) on RTW after elective surgery remains unclear and requires further examination in CTR populations, taking into account issues such as job security and sick-leave entitlement.
We only found one study that specifically compared individuals in full-time work with those working part-time (16). The authors reported shorter periods of post-operative sick-leave among full-time workers, however, it is unclear whether all calendar days, or just those where the participant would usually be working, were included in this estimation.
Interestingly, we found that studies with large sample sizes (>100 workers per study arm) tended to report longer RTW times than medium-sized (30-100) or small studies (<30). One explanation for this finding is the left-censoring of data in at least one of the large studies. Atroshi et al. (14) explicitly stated that their RTW data were obtained from a national database that registered work absences exceeding 14 days. Therefore, any individuals who returned to work within 14 days of their CTR would be omitted from this study. If every CTR patient had been included, the median time to RTW would be shorter. We could not ascertain whether a similar convention was adopted in the large study by Wasiak & Pransky, which also obtained RTW information from regional/national databases (31). Importantly, when the results were further examined, there was no clear association between RTW times and the method of obtaining RTW data. Moreover, we found no clear relationship between reported RTW times and risk of bias scoring.
Advice provided by healthcare professionals, particularly the surgeon, may be an important determinant of RTW time. Ratzon et al. found that surgeon’s advice was a strong predictor of RTW times among their cohort (17). However, we were unable to explore the role of advice in the current review because so few studies specified what advice had been given, and by whom.
The eligibility criteria for our review were deliberately broad to reflect the patients and CTR procedures seen in clinical practice. All studies purported to measure RTW duration after CTR, but key information, such as the definition of RTW, the method of assessment and the number of workers contributing data were frequently unreported. As a result, we provided descriptive summaries of the reported RTW times as the median and range. It is a limitation of the current review that we were unable to pool data for a formal meta-analysis with a sample size weighting.
In order to present the data consistently, all RTW durations were reported in days. In some cases, this involved a conversion from weeks or months to days, which may not truly reflect the timescales collected in the original dataset. It is also possible that some authors calculated RTW duration based on a 5-day working week, although this was not specified.
Time to RTW would not be expected to show a normal distribution because the presence of a few individuals who take much longer to RTW will cause a positive skew to the data. For this reason, summarizing RTW duration as the mean has the potential to inflate the point estimate, as seen in four of the five studies that reported both mean and median (14, 27, 31, 35). At the most extreme, the study by Wasiak & Pransky reported a mean return to work time after open CTR of 85 days as compared with a median of 34 days (31). This bias has obvious implications when interpreting the findings of our review, and for patients wishing to know the usual period of time it takes for someone to return to an occupation that is similar to their own. To generate more useful clinical information, future research should report RTW times as the median and range to better enable comparison between studies. Only eight of the studies in our review reported their data in this way and therefore consideration needs to be given to the probable positive skew of the studies which reported only mean RTW time, and the associated consequences of this on the summary data presented in this review.
Despite the weaknesses identified in many of the included studies, our review adds to the existing CTR literature by demonstrating a wide range of RTW times across a large number of international studies using different methodological approaches. Previous reviews have been restricted to either the smaller number of published RCTs that were designed to assess the clinical effectiveness of different interventions (5–9); or to studies of prognostic factors for RTW without an assessment of the duration of work absence (71).
Inconsistencies in the definition and measurement of time to RTW in CTR settings have been previously discussed (73). The authors called for standardized assessment of RTW, measured in days, and including information on type of work, insurance status and rehabilitation. The results of the current review show that this information is still not consistently reported and clear standards for the measurement and reporting of work-related outcomes in clinical studies need to be defined. In particular, we would argue for a clear statement of the number of workers in the study sample; provision of summary data on the spread of RTW times, rather than just a point estimate; documentation of the number of workers who had not returned to work by the end of the study period; capturing any subsequent, related periods of sick leave; and making a clear distinction between return to paid work and return to other activities. There is also a need to establish a definition for the assessment of return to modified and full work duties and a standardized categorization of occupational roles. In the current review only six studies provided information on return to work times for different types of occupation, but the classifications varied so widely that it was only feasible to group into discrete ‘manual’ and ‘non-manual’ categories for purposes of the review summary. As a result, the studies provide only limited information for clinicians to draw upon in advising individual patients of how long it might take to return to specific work roles.
We purposefully included research conducted in any country, and acknowledge the potential issues associated with the comparison of findings from different cultural, social, welfare and healthcare backgrounds. In fact, the majority of included studies were conducted in the USA and the results were spread across the range of reported RTW durations, including both the shortest and longest periods of work absence. Scandinavian studies reported longer return to work times than studies conducted in other parts of Europe. This finding might also be partly explained by the left-censoring of return to work data captured from national databases, as discussed above. One study included in this review specifically compared return to work times across two different geographical settings. Bitar et al. retrospectively assessed post-operative work absence in 81 female workers from USA (34 with workers’ compensation, 47 without) and 42 female workers from Sweden (65). Both groups from the USA took longer to return to work than the Swedish cohort. The availability of compensation or other paid sick leave is an important determinant of duration to RTW, however the influences of additional cultural and contextual factors on post-operative return to work timescales warrant further exploration.
The key factors underpinning the wide variation in reported RTW times remain unclear, largely due to the heterogeneity of the available studies and incomplete reporting. The findings of our review support the call for greater clarity in the reporting of work-related outcomes in relevant studies. ‘Return to work time’ needs to be measured consistently and include a description of influential factors, such as: type of occupation and employment status; RTW advice and return to modified or full duties. However, despite the limitations of the available studies, our findings suggest that occupational factors play an important role in RTW after CTR. The identified literature suggests longer periods of work absence among those who are employed (rather than self-employed); those who work part-time (rather than full-time); those who work in heavy manual occupations; and those required to return to full (rather than amended) duties. Further research is required to determine whether earlier RTW is appropriate for these groups, and if so, to determine the safest recommended timescales.
Supplementary Material
Summary.
Time to return to work after carpal tunnel release varied widely in the literature and was inconsistently measured. Few studies reported specific occupational information, such as return to work times for different duties or work schedules. It is currently not possible to provide evidence-based guidance for patients about when they might expect to return safely to their work.
Acknowledgements
The authors would like to thank: Paula Sands and Tom Wake of the University of Southampton Health Sciences Library for their assistance in obtaining full text articles for this review; Professor Keith Palmer and Dr Georgia Ntani for their assistance with the data syntheses; and Rob Wilson for his assistance with data visualisation.
Funding
LN was funded by an NIHR Doctoral Research Fellowship (Ref: DRF-2015-08-056). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Footnotes
Authors’ contributions
LN, KWB, JA and DW conceived the study and prepared the draft manuscript. LN and MS performed the literature screening and data extraction. LN and KWB performed the risk of bias assessments and data syntheses. All authors reviewed and contributed to the final manuscript.
Conflicts of interest
The authors declare no conflict of interest.
References
- 1.Lewis C, Mauffrey C, Newman S, Lambert A, Hull P. Current concepts in carpal tunnel syndrome: a review of the literature. Eur J Orthop Surg Traumatol. 2010;20:445–52. [Google Scholar]
- 2.American Academy of Orthopaedic Surgeons. Management of carpal tunnel syndrome evidence-based clinical practice guideline. Illinois: American Academy of Orthopaedic Surgeons; 2016. [DOI] [PubMed] [Google Scholar]
- 3.British Orthopaedic Association. Commissioning guide: Treatment of carpal tunnel syndrome. London: Royal College of Surgeons; 2017. [Google Scholar]
- 4.Bebbington E, Furniss D. Linear regression analysis of Hospital Episode Statistics predicts a large increase in demand for elective hand surgery in England. J Plast Reconstr Aesthet Surg. 2015;68:243–51. doi: 10.1016/j.bjps.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kohanzadeh S, Herrera FA, Dobke M. Outcomes of open and endoscopic carpal tunnel release: a meta-analysis. Hand. 2012;7:247–51. doi: 10.1007/s11552-012-9413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen L, Duan X, Huang X, Lv J, Peng K, Xiang Z. Effectiveness and safety of endoscopic versus open carpal tunnel decompression. Arch Orthop Trauma Surg. 2014;134:585–93. doi: 10.1007/s00402-013-1898-z. [DOI] [PubMed] [Google Scholar]
- 7.Sayegh ET, Strauch RJ. Open versus endoscopic carpal tunnel release: a meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2015;473:1120–32. doi: 10.1007/s11999-014-3835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vasiliadis HS, Nikolakopoulou A, Shrier I, Lunn MP, Brassington R, Scholten RJP, et al. Endoscopic and open release similarly safe for the treatment of carpal tunnel syndrome. A systematic review and meta-analysis. PLoS One. 2015;10:e0143683. doi: 10.1371/journal.pone.0143683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vasiliadis HS, Georgoulas P, Shrier I, Salanti G, Scholten RJ. Endoscopic release for carpal tunnel syndrome. Cochrane Database Syst Rev. 2014;1:CD008265. doi: 10.1002/14651858.CD008265.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newington L, Stevens M, Ntani G, Adams J, Warwick D, Walker-Bone K. Systematic review of return to work timescales and strategies to enhance return to work after carpal tunnel release (protocol) PROSPERO. 2016 CRD42016034158. [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sterne J, Higgins J, Reeves B, on behalf of the development group for ACROBAT-NRSI A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI) [updated 24 September 2014];2014 Version 1.0.0:[Available from: http://www.riskofbias.info/
- 14.Atroshi I, Zhou C, Joud A, Petersson IF, Englund M. Sickness absence from work among persons with new physician-diagnosed carpal tunnel syndrome: a population-based matched-cohort study. PLoS One. 2015;10:e0119795. doi: 10.1371/journal.pone.0119795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Becker SJ, Makanji HS, Ring D. Expected and actual improvement of symptoms with carpal tunnel release. J Hand Surg Am. 2012;37:1324–9. doi: 10.1016/j.jhsa.2012.03.039. [DOI] [PubMed] [Google Scholar]
- 16.Cowan J, Makanji H, Mudgal C, Jupiter J, Ring D. Determinants of return to work after carpal tunnel release. J Hand Surg Am. 2012;37:18–27. doi: 10.1016/j.jhsa.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 17.Ratzon N, Schejter-Margalit T, Froom P. Time to return to work and surgeons' recommendations after carpal tunnel release. Occup Med. 2006;56:46–50. doi: 10.1093/occmed/kqi194. [DOI] [PubMed] [Google Scholar]
- 18.Cook AC, Szabo RM, Birkholz SW, King EF. Early mobilization following carpal tunnel release. A prospective randomized study. J Hand Surg Br. 1995;20:228–30. doi: 10.1016/s0266-7681(05)80057-9. [DOI] [PubMed] [Google Scholar]
- 19.Brown MG, Keyser B, Rothenberg ES. Endoscopic carpal tunnel release. J Hand Surg Am. 1992;17:1009–11. doi: 10.1016/s0363-5023(09)91047-4. [DOI] [PubMed] [Google Scholar]
- 20.Chrostowski JH, Wolfe SW, Bernstein R. Endoscopic versus open carpal tunnel release: A retrospective review. Surg Forum. 1994;45:609–12. [Google Scholar]
- 21.Goodman RC. An aggressive return-to-work program in surgical treatment of carpal tunnel syndrome: A comparison of costs. Plast Reconstr Surg. 1992;89:715–7. doi: 10.1097/00006534-199204000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Parot-Schinkel E, Roquelaure Y, Ha C, Leclerc A, Chastang J-F, Raimbeau G, et al. Factors affecting return to work after carpal tunnel syndrome surgery in a large french cohort. Arch of Phys Med Rehabil. 2011;92:1863–9. doi: 10.1016/j.apmr.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Agee JM, McCarroll HR, Jr, Tortosa RD, Berry DA, Szabo RM, Peimer CA. Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. J Hand Surg Am. 1992;17:987–95. doi: 10.1016/s0363-5023(09)91044-9. [DOI] [PubMed] [Google Scholar]
- 24.Braun RM, Jackson WJ. Electrical studies as a prognostic factor in the surgical treatment of carpal tunnel syndrome. J Hand Surg Am. 1994;19:893–900. doi: 10.1016/0363-5023(94)90086-8. [DOI] [PubMed] [Google Scholar]
- 25.Manktelow RT, Binhammer P, Tomat LR, Bril V, Szalai JP. Carpal tunnel syndrome: cross-sectional and outcome study in Ontario workers. J Hand Surg Am. 2004;29:307–17. doi: 10.1016/j.jhsa.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Larsen MB, Sorensen AI, Crone KL, Weis T, Boeckstyns ME. Carpal tunnel release: a randomized comparison of three surgical methods. J Hand Surg Eur. 2013;38:646–50. doi: 10.1177/1753193412475247. [DOI] [PubMed] [Google Scholar]
- 27.Atroshi I, Larsson G-U, Ornstein E, Hofer M, Johnsson R, Ranstam J. Outcomes of endoscopic surgery compared with open surgery for carpal tunnel syndrome among employed patients: randomised controlled trial. BMJ. 2006;332:1473. doi: 10.1136/bmj.38863.632789.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cha SM, Shin HD, Ahn JS, Beom JW, Kim DY. Differences in the postoperative outcomes according to the primary treatment options chosen by patients with carpal tunnel syndrome: conservative versus operative treatment. Ann Plast Surg. 2016;77:80–4. doi: 10.1097/SAP.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 29.Hansen TB, Dalsgaard J, Meldgaard A, Larsen K. A prospective study of prognostic factors for duration of sick leave after endoscopic carpal tunnel release. BMC Musculoskelet Disord. 2009;10:144. doi: 10.1186/1471-2474-10-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seitz WH, Lall A. Open carpal tunnel release with median neurolysis and z-plasty reconstruction of the transverse carpal ligament. Curr Orthop Pract. 2013;24:53–7. [Google Scholar]
- 31.Wasiak R, Pransky G. The impact of procedure type, jurisdiction and other factors in workers' compensation on work-disability outcomes following carpal tunnel surgery. Work. 2007;28:103–10. [PubMed] [Google Scholar]
- 32.Bhattacharya R, Birdsall PD, Finn P, Stothard J. A randomized controlled trial of knifelight and open carpal tunnel release. J Hand Surg Br. 2004;29:113–5. doi: 10.1016/j.jhsb.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 33.Ferdinand RD, MacLean JG. Endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome. A prospective, randomised, blinded assessment. J Bone Joint Surg Br. 2002;84:375–9. doi: 10.1302/0301-620x.84b3.12224. [DOI] [PubMed] [Google Scholar]
- 34.Dickson DR, Boddice T, Collier AM. A comparison of the functional difficulties in staged and simultaneous open carpal tunnel decompression. J Hand Surg Eur. 2014;39:627–31. doi: 10.1177/1753193413509938. [DOI] [PubMed] [Google Scholar]
- 35.Fehringer EV, Tiedeman JJ, Dobler K, McCarthy JA. Bilateral endoscopic carpal tunnel releases: Simultaneous versus staged operative intervention. Arthroscopy. 2002;18:316–21. doi: 10.1053/jars.2002.30643. [DOI] [PubMed] [Google Scholar]
- 36.Futami T. Surgery for bilateral carpal tunnel syndrome. Endoscopic and open release compared in 10 patients. Acta Orthop Scand. 1995;66:153–5. doi: 10.3109/17453679508995510. [DOI] [PubMed] [Google Scholar]
- 37.Nesbitt KS, Innis PC, Dubin NH, Wilgis EF. Staged versus simultaneous bilateral endoscopic carpal tunnel release: an outcome study. Plast Reconstr Surg. 2006;118:139–45. doi: 10.1097/01.prs.0000221073.99662.39. [DOI] [PubMed] [Google Scholar]
- 38.Weber RA, Boyer KM. Consecutive versus simultaneous bilateral carpal tunnel release. Ann Plast Surg. 2005;54:15–9. doi: 10.1097/01.sap.0000139566.23908.2c. [DOI] [PubMed] [Google Scholar]
- 39.Brown RA, Gelberman RH, Seiler JG, Iii, Abrahamsson SO, Weiland AJ, Urbaniak JR, et al. Carpal tunnel release. A prospective, randomized assessment of open and endoscopic methods. J Bone Joint Surg Am. 1993;75:1265–75. doi: 10.2106/00004623-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Cellocco P, Rossi C, El Boustany S, Di Tanna GL, Costanzo G. Minimally invasive carpal tunnel release. Orthop Clin North Am. 2009;40:441–8. doi: 10.1016/j.ocl.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Finsen V, Andersen K, Russwurm H. No advantage from splinting the wrist after open carpal tunnel release. A randomized study of 82 wrists. Acta Orthop Scand. 1999;70:288–92. doi: 10.3109/17453679908997810. [DOI] [PubMed] [Google Scholar]
- 42.Foulkes GD, Atkinson RE, Beuchel C, Doyle JR, Singer DI. Outcome following epineurotomy in carpal tunnel syndrome: a prospective, randomized clinical trial. J Hand Surg Am. 1994;19:539–47. doi: 10.1016/0363-5023(94)90253-4. [DOI] [PubMed] [Google Scholar]
- 43.Jacobsen MB, Rahme H. A prospective, randomized study with an independent observer comparing open carpal tunnel release with endoscopic carpal tunnel release. J Hand Surg Br. 1996;21:202–4. doi: 10.1016/s0266-7681(96)80097-0. [DOI] [PubMed] [Google Scholar]
- 44.Saw NL, Jones S, Shepstone L, Meyer M, Chapman PG, Logan AM. Early outcome and cost-effectiveness of endoscopic versus open carpal tunnel release: a randomized prospective trial. J Hand Surg Br. 2003;28:444–9. doi: 10.1016/s0266-7681(03)00097-4. [DOI] [PubMed] [Google Scholar]
- 45.Tian Y, Zhao H, Wang T. Prospective comparison of endoscopic and open surgical methods for carpal tunnel syndrome. Chin Med Sci J. 2007;22:104–7. [PubMed] [Google Scholar]
- 46.Trumble TE, Diao E, Abrams RA, Gilbert-Anderson MM. Single-portal endoscopic carpal tunnel release compared with open release : a prospective, randomized trial. J Bone Joint Surg Am. 2002;84:1107–15. doi: 10.2106/00004623-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 47.Adams ML, Franklin GM, Barnhart S. Outcome of carpal tunnel surgery in Washington State workers' compensation. Am J Ind Med. 1994;25:527–36. doi: 10.1002/ajim.4700250407. [DOI] [PubMed] [Google Scholar]
- 48.Bekkelund SI, Pierre-Jerome C, Torbergsen T, Ingebrigtsen T. Impact of occupational variables in carpal tunnel syndrome. Acta Neurol Scand. 2001;103:193–7. doi: 10.1034/j.1600-0404.2001.103003193.x. [DOI] [PubMed] [Google Scholar]
- 49.Carmona L, Faucett J, Blanc PD, Yelin E. Predictors of rate of return to work after surgery for carpal tunnel syndrome. Arthritis Care Res. 1998;11:298–305. doi: 10.1002/art.1790110411. [DOI] [PubMed] [Google Scholar]
- 50.De Kesel R, Donceel P, De Smet L. Factors influencing return to work after surgical treatment for carpal tunnel syndrome. Occup Med. 2008;58:187–90. doi: 10.1093/occmed/kqn034. [DOI] [PubMed] [Google Scholar]
- 51.Duche R, Trabelsi A. The Canaletto implant for reconstructing transverse carpal ligament in carpal tunnel surgery. Surgical technique and cohort prospective study about 400 Canaletto cases versus 400 cases with open carpal tunnel surgery. Chir Main. 2010;29:352–9. doi: 10.1016/j.main.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 52.Gibbs KE, Rand W, Ruby LK. Open vs endoscopic carpal tunnel release. Orthopedics. 1996;19:1025–8. doi: 10.3928/0147-7447-19961201-09. [DOI] [PubMed] [Google Scholar]
- 53.Hallock GG, Lutz DA. Prospective comparison of minimal incision "open" and two-portal endoscopic carpal tunnel release. Plast Reconstr Surg. 1995;96:941–7. doi: 10.1097/00006534-199509001-00027. [DOI] [PubMed] [Google Scholar]
- 54.Huracek J, Heising T, Wanner M, Troeger H. Recovery after carpal tunnel syndrome operation: the influence of the opposite hand, if operated on in the same session. Arch Orthop Trauma Surg. 2001;121:368–70. doi: 10.1007/s004020100260. [DOI] [PubMed] [Google Scholar]
- 55.Karlsson MK, Lindau T, Hagberg L. Ligament lengthening compared with simple division of the transverse carpal ligament in the open treatment of carpal tunnel syndrome. Scand J Plast Reconstr Surg Hand Surg. 1997;31:65–9. doi: 10.3109/02844319709010507. [DOI] [PubMed] [Google Scholar]
- 56.Kerr CD, Gittins ME, Sybert DR. Endoscopic versus open carpal tunnel release: clinical results. Arthroscopy. 1994;10:266–9. doi: 10.1016/s0749-8063(05)80109-4. [DOI] [PubMed] [Google Scholar]
- 57.Lyall JM, Gliner J, Hubbell MK. Treatment of workers' compensation cases of carpal tunnel syndrome: an outcome study. J Hand Ther. 2002;15:251–9. doi: 10.1016/s0894-1130(02)70008-2. [DOI] [PubMed] [Google Scholar]
- 58.McDonough JW, Gruenloh TJ. A comparison of endoscopic and open carpal tunnel release. Wis Med J. 1993;92:675–7. [PubMed] [Google Scholar]
- 59.Nagle DJ, Fischer TJ, Harris GD, Hastings Hn, Osterman AL, Palmer AK, et al. A multicenter prospective review of 640 endoscopic carpal tunnel releases using the transbursal and extrabursal chow techniques. Arthroscopy. 1996;12:139–43. doi: 10.1016/s0749-8063(96)90001-8. [DOI] [PubMed] [Google Scholar]
- 60.Palmer DH, Paulson JC, Lane-Larsen CL, Peulen VK, Olson JD. Endoscopic carpal tunnel release: a comparison of two techniques with open release. Arthroscopy. 1993;9:498–508. doi: 10.1016/s0749-8063(05)80396-2. [DOI] [PubMed] [Google Scholar]
- 61.Bruser P, Richter M, Larkin G, Lefering R. The operative treatment of carpal tunnel syndrome and its relevance to endoscopic release. Eur J Plast Surg. 1999;22:80–4. [Google Scholar]
- 62.Jugovac I, Burgic N, Micovic V, Radolovic-Prenc L, Uravic M, Golubovic V, et al. Carpal tunnel release by limited palmar incision vs traditional open technique: randomized controlled trial. Croat Med J. 2002;43:33–6. [PubMed] [Google Scholar]
- 63.Provinciali L, Giattini A, Splendiani G, Logullo F. Usefulness of hand rehabilitation after carpal tunnel surgery. Muscle Nerve. 2000;23:211–6. doi: 10.1002/(sici)1097-4598(200002)23:2<211::aid-mus11>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 64.Sennwald GR, Benedetti R. The value of one-portal endoscopic carpal tunnel release: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 1995;3:113–6. doi: 10.1007/BF01552386. [DOI] [PubMed] [Google Scholar]
- 65.Bitar G, Alexandrides J, Missirian R, Sotereanos D, Nystrom A. Carpal tunnel release in the United States and Sweden: reimbursement patterns, cost for treatment, and return to work. Plast Reconstr Surg. 2002;109:1574–8. doi: 10.1097/00006534-200204150-00013. [DOI] [PubMed] [Google Scholar]
- 66.Braun RM, Doehr S, Mosqueda T, Garcia A. The effect of legal representation on functional recovery of the hand in injured workers following carpal tunnel release. J Hand Surg Am. 1999;24:53–8. doi: 10.1053/jhsu.1999.jhsu24a0053. [DOI] [PubMed] [Google Scholar]
- 67.Chaise F, Bellemere P, Fril JP, Gaisne E, Poirier P, Menadi A. Return-to-work interval and surgery for carpal tunnel syndrome. Results of a prospective series of 233 patients. J Hand Surg Br. 2004;29:568–70. doi: 10.1016/j.jhsb.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 68.Ketchum LD. A comparison of flexor tenosynovectomy, open carpal tunnel release, and open carpal tunnel release with flexor tenosynovectomy in the treatment of carpal tunnel syndrome. Plast Reconstr Surg. 2004;113:2020–9. doi: 10.1097/01.prs.0000122216.24878.1f. [DOI] [PubMed] [Google Scholar]
- 69.Gimeno D, Amick BC, Habeck RV, Ossmann J, Katz JN. The role of job strain on return to work after carpal tunnel surgery. Occup Environ Med. 2005;62:778–85. doi: 10.1136/oem.2004.016931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dunn JC, Kusnezov NA, Koehler LR, Vanden Berge D, Genco B, Mitchell J, et al. Outcomes following carpal tunnel release in patients receiving workers' compensation: a systematic review. Hand. 2018;13:137–42. doi: 10.1177/1558944717701240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Peters S, Johnston V, Hines S, Ross M, Coppieters M. Prognostic factors for return-to-work following surgery for carpal tunnel syndrome: a systematic review. JBI Database System Rev Implement Rep. 2016;14:135–216. doi: 10.11124/JBISRIR-2016-003099. [DOI] [PubMed] [Google Scholar]
- 72.Tilbury C, Schaasberg W, Plevier JW, Fiocco M, Nelissen RG, Vliet Vlieland TP. Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology. 2014;53:512–25. doi: 10.1093/rheumatology/ket389. [DOI] [PubMed] [Google Scholar]
- 73.Ayeni O, Thoma A, Haines T, Sprague S. Analysis of reporting return to work in studies comparing open with endoscopic carpal tunnel release: a review of randomized controlled trials. Can J Plast Surg. 2005;13:181–7. doi: 10.1177/229255030501300403. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.