Highlights
-
•
Laparoscopic surgery as technique of choice in children for benign solid lesions of the spleen.
-
•
Multidisciplinary treatment of rare disease, Hamartoma of the spleen, in childhood.
-
•
Role of chemoembolization in the pre-operative surgical setting to reduce intraoperative bleeding.
-
•
Partial splenectomy as safe procedure to preserve hematological function of the spleen.
Keywords: Hamartoma, Laparoscopic splenectomy, Partial splenectomy, Pediatric surgery
Abstract
Introduction
To date, laparoscopic surgery has played a key role in the treatment of not only splenic hematologic pathologies but also solid ones.
Hamartoma is a rare disease; only twenty percent of them are of pediatric relevance; it is a benign tumor, but radiological features never allow proper differentiation from malignant neoplasms.
In children, hamartoma may be associated with other morbid conditions, such as sickle cell disease or other hematological alterations.
Presentation of the case
We report a case of hamartoma in a 7-year-old child treated with partial laparoscopic splenectomy.
After a multidisciplinary evaluation, the indication of laparoscopic splenectomy was decided; upon evaluating the age of the patient and the affected spleen portion, a partial splenectomy was proposed. The histological examination during surgery was performed to exclude any form of malignancy.
The intraoperative frozen section of the specimen was negative for malignancies, and a partial splenectomy was performed.
Discussion
Surgery remains the first choice in the definitive treatment of solid lesions of the spleen; minimally invasive technique, namely, laparoscopy, has set itself as the technique of choice for surgical treatment.
In this case, the possibility of obtaining an intraoperative pathological diagnosis by frozen section of the specimen, confirming the benign nature of the lesion, allowed the surgeon to decide in favor of a laparoscopic partial splenectomy.
Conclusion
Partial laparoscopic splenectomy can be considered a safe, effective and reproducible alternative in patients suffering from benign solid diseases, safeguarding the hematological functions of the organ itself in pediatric age.
1. Introduction
To date, laparoscopic surgery has played a key role in the surgical treatment of not only splenic hematologic pathologies but also solid ones, such as benign and malignant tumors [2,3].
Hamartoma, primarily described by Rokitansky in 1861 [4], is a rare disease, with few cases described in the literature; only twenty percent of them are of pediatric relevance [5]. Hamartoma is often diagnosed during autopsy or incidentally during radiological examinations for the study of other pathological conditions; it is considered a benign tumor, but radiological features never allow proper differentiation from malignant neoplasms. For this reason, proceeding to splenectomy is recommended.
In children, hamartoma may be associated with other morbid conditions, such as sickle cell disease or other hematological alterations [6]. It derives from a morphological alteration of the red pulp of the spleen [7].
The first open splenectomy for hamartoma was described in 1990; most recently, in 2012, total laparoscopic splenectomy for hamartoma was described [8].
In this article, we report a case of hamartoma in a 7-year-old child treated with partial laparoscopic splenectomy.
2. Presentation of case
In July 2017, a 7-year-old child was admitted to the pediatric emergency room for lumbar pain and fever; during the physical examination, mild pain was evoked from the lower abdominal quadrants. Urine tests showed a slight microhematuria. In the history, no allergies and no major diseases were described.
Standard hematological and blood chemistry tests didn’t show significant alterations.
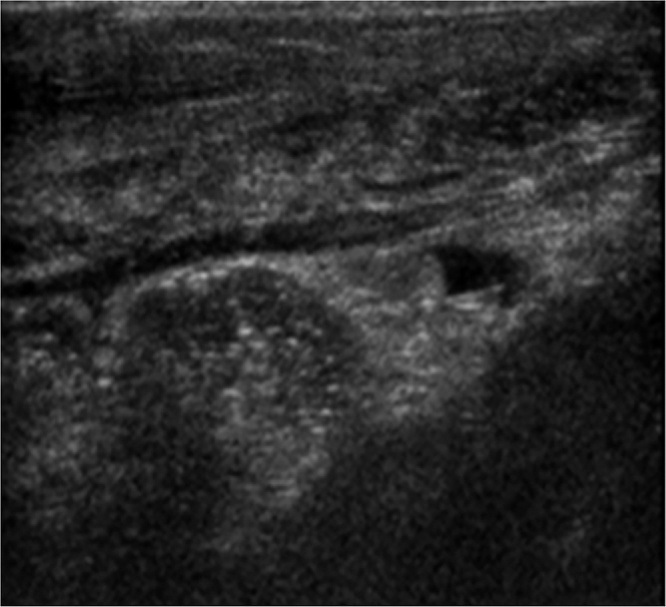
Abdominal ultrasound (US) highlighted a single solid lesion 5.5 × 6.5 cm in size with rounded morphology and sharp margins, occupying the middle third of the spleen. The structure showed hypoechoic and small intralesional hyperechoic spots suggestive of microcalcifications. The marked Doppler vascularization was both peripheral and intralesional (Fig. 1).
Fig. 1.
xxx.
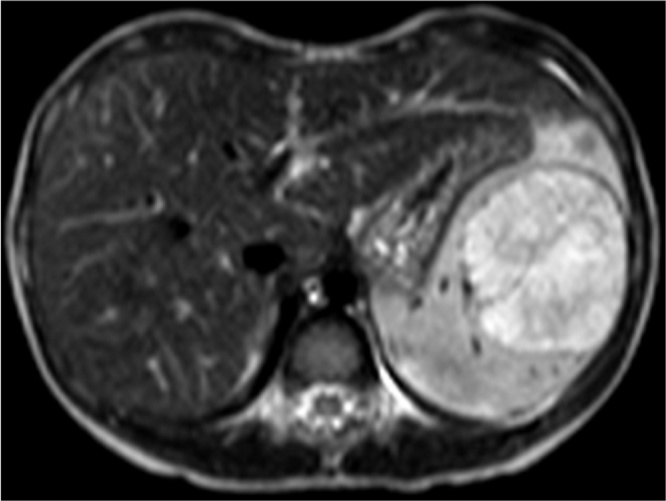
Magnetic resonance imagining (MRI) was performed to better investigate the lesion. The spleen had a bipolar diameter of 11 cm, the presence of a single round lesion with well-defined margins of 6.3 cm × 5.3 cm × 5.8 cm was confirmed. The lesion had an uneven, high-intensity T2 signal and isointensity in T1, with early and intense contrast. The radiologist concluded that the radiologic framework was compatible with a benign lesion, likely a hamartoma, although the diagnosis of atypical hemangioma could not be excluded (Fig. 2).
Fig. 2.
xxx.
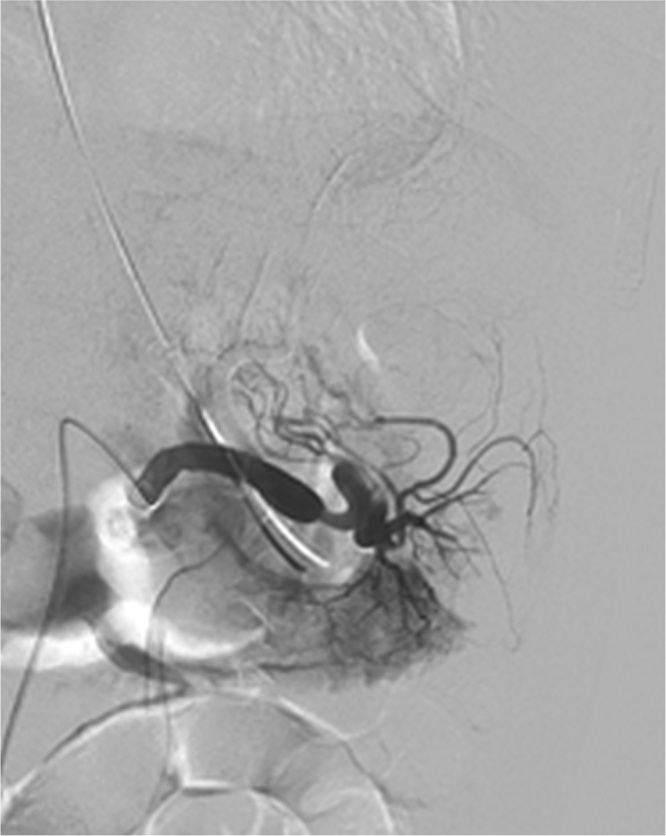
After a multidisciplinary evaluation, the indication of laparoscopic splenectomy was decided; upon evaluating the age of the patient and the affected spleen portion, a partial splenectomy was proposed, with preservation of the lower pole prior to frozen section histological examination during surgery to exclude any form of malignancy. The patient was subjected to segmental chemoembolization of the splenic artery (Fig. 3), preserving vessels of the lower pole, to minimize intraoperative blood loss. The intraoperative frozen section of the specimen was negative for malignancies, and a partial splenectomy was performed.
Fig. 3.
xxx.
The patient was placed in right semi-lateral decubitus; a 10-mm optical trocar was placed in the left para-rectal region on the transverse umbilical line. Three more trocars were positioned according to a concave line along the left subcostal margin 5 cm from the coastal arch.
An abdominal cavity inspection was performed. The spleen was dissected using an ultrasound scalpel. The section and sealing of segmental splenic vessels was performed using the scalpel plus titanium clips. Parenchymal transection was performed using bipolar forceps and an ultrasound scalpel. The upper pole and the middle section of the spleen was removed, maintaining a margin of about 1 cm from the lesion. The lower pole of the spleen and the segmental vessels to lower pole has been fully maintained Lastly the specimen was removed via an endobag through the left flank port enlarged up to 4 cm in size. Accurate hemostasis of the line of transection was made, and fibrin glue was applied to ensure sealing.
Before desufflation of the pneumoperitoneum, sprays of local anesthetic were applied to the hemidiagraphm to reduce the pain caused by muscle relaxation during the laparoscopy
No complications occurred during the post-operative course. An anti-thrombotic prophylaxis with enoxaparin sodium 2000 U.I./die was administered until discharge. An increase in the patient’s platelet count up to 900 migl / mmc within the first and second post-operative days occurred, with a count of 345 migl / mmc at discharge.
The remaining blood tests were within normal ranges. Refeeding was started on the first day after surgery, and good pain control was obtained with common pain relievers.
Before discharge, an abdominal ultrasound was performed, which showed minimal inflammatory fluid along the splenic loggia. The patient was discharged on the fifth post-operative day; an antibiotic therapy (amoxicillin) was prescribed for 7 days at home.
During the pathological examination, the specimen was represented by splenic parenchyma 8 cm × 6 cm × 3.5 cm in size, and the weight was 78 g. The nodule inside, roundish, had a diameter of 5.5 cm. The pre-operative diagnosis of splenic hamartoma was confirmed.
The patient underwent physical examination and blood tests every 3 months after discharge; after a year, the patient have a normal platelet count of 345 migl/mmc and no Howell-Jolly bodies were found.
3. Discussion
Hamartomas are solid spleen tumors and are rare and histologically benign; they are often asymptomatic, and diagnosis is occasional.
Imaging is becoming more and more refined in differentiating the solid lesions of parenchymatous organs. Several authors have described how hamartomas of the spleen radiologically appear; in this case, only US and MRI were used so as not to expose the patient to ionizing radiations, considering the patient’s age [9,10].
The role of biopsy of splenic lesions is controversial and is burdened by certain risks, such as bleeding and the risk of seeding of neoplastic cells into the abdominal cavity in case of malignancies [11,12].
Therefore, surgery remains the first choice in the definitive treatment of these lesions; minimally invasive technique, namely, laparoscopy, has set itself as the technique of choice for surgical treatment, offering the benefits of a minimally invasive approach with a very low conversion rate [13]. Moreover, the reduced risk of post-operative adhesions facilitates further surgery if required.
In particular, partial splenectomy is proposed in children with certain benign lesions, to preserve the immunological function of the organ such as Garza-Serna et al. have described partial splenectomy for splenic cysts [14,15]; however, for lesions for which there is no definitive pre-operative diagnosis, associated with technical limits, proceeding to complete splenectomy is the preferred course.
In this case, the possibility of obtaining an intraoperative pathological diagnosis by frozen section of the specimen, confirming the benign nature of the lesion, allowed the surgeon to decide in favor of a laparoscopic partial splenectomy.
The operator's experience in laparoscopic surgery, associated with the highly advanced nature of laparoscopic instruments and the improved understanding of vascular anatomy, all contribute to avoiding severe bleeding from the splenic parenchyma [16].
As far as the literature is concerned, this is the first case of partial laparoscopic splenectomy for hamartoma in a child.
In addition, an accurate pre-operative study of images was performed; the hypothesis that partial splenectomy could be performed has suggested the choice of performing an angiography to embolize the upper splenic pole to reduce the risk of bleeding during the splenic parenchymal dissection [17].
4. Conclusions
Proper integration between radiologists, pediatricians and surgeons resulted in the correct management of a pediatric patient suffering from a rare disease.
Partial laparoscopic splenectomy can be considered a safe, effective and reproducible alternative in patients suffering from benign solid diseases, safeguarding the hematological functions of the organ itself.
This procedure should be performed in centers in which the intraoperative frozen section of the specimen is available.
In the absence of a clear histologic diagnosis, it is necessary to proceed to complete splenectomy.
Conflicts of interest
No conflicts of interest.
Sources of funding
Non funding were used.
Ethical approval
In our institute, the approval of the ethics committee for the retrospective analysis of a clinical case is not required.
Consent
Written informed consent was obtained from the patient's parent for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Serra Francesco, MD: Data collection and author of methods and discussion.
Sorrentino Lorena, MD: Review of surgical technique literature and co-author of discussion.
Cabry Francesca, MD: Review of surgical technique literature and author of introduction.
Diego Biondini, MD: Consultant of the pediatric clinical case.
Pier Luca Ceccarelli, MD: Consultant of the pediatric clinical case.
Campanelli Michela, MD: Data collection.
Gelmini Roberta, MD PhD: Supervisor and co-author of entire manuscript.
Registration of research studies
The submitted case report is not a research study.
Guarantor
Gelmini Roberta.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
The work was written in line with the SCARE criteria [1].
Contributor Information
Francesco Serra, Email: serrafrancescomd@gmail.com.
Lorena Sorrentino, Email: lorena.sorrentino@live.it.
Francesca Cabry, Email: francesca.cabry@unimore.it.
Diego Biondini, Email: biondinidiego@gmail.com.
Pier Luca Ceccarelli, Email: ceccarelli.pierluca@unimore.it.
Michela Campanelli, Email: michelacampanelli@live.it.
Roberta Gelmini, Email: roberta.gelmini@unimore.it.
References
- 1.Agha R.A., Fowler A.J., Saeta A. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. Lond. Engl. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Habermalz B., Sauerland S., Decker G. Laparoscopic splenectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) Surg. Endosc. 2008;22:821–848. doi: 10.1007/s00464-007-9735-5. [DOI] [PubMed] [Google Scholar]
- 3.Otrock Z.K., Seoud M.A., Khalifeh M.J. Laparoscopic splenectomy for isolated parenchymal splenic metastasis of ovarian cancer. Int. J. Gynecol. Cancer. 2006;16:1933–1935. doi: 10.1111/j.1525-1438.2006.00662.x. [DOI] [PubMed] [Google Scholar]
- 4.Rokitansky K. Braumuller und seidel; Wien: 1861. About Splenomas Lehrbuch. Der Pathologishen Anatomie, Baud 1; p. 3. [Google Scholar]
- 5.Abramowsky C., Alvarado C., Wyly J.B., Ricketts R. “Hamartoma” of the spleen (splenoma) in children. Pediatr. Dev. Pathol. 2004;7:231–236. doi: 10.1007/s10024-003-9097-5. [DOI] [PubMed] [Google Scholar]
- 6.Elenga N., Labbé S., Leduc N. Asymptomatic multinodular splenoma (splenic hamartoma) in a child with sickle cell anemia. Int. Med. Case Rep. J. 2017;10:233–236. doi: 10.2147/IMCRJ.S125988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee H., Maeda K. Hamartoma of the spleen. Arch. Pathol. Lab. Med. 2009;133:147–151. doi: 10.5858/133.1.147. [DOI] [PubMed] [Google Scholar]
- 8.Pisani Ceretti A., Bislenghi G., Virdis M. Laparoscopic splenectomy for splenic hamartoma: a case report. Case Rep. Gastrointest. Med. 2012;2012:435802. doi: 10.1155/2012/435802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elsayes K.M., Narra V.R., Mukundan G. MR imaging of the spleen: spectrum of abnormalities. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2005;25:967–982. doi: 10.1148/rg.254045154. [DOI] [PubMed] [Google Scholar]
- 10.Ali T.Z., Beyer G., Taylor M. Splenic hamartoma: immunohistochemical and ultrastructural profile of two cases. Int. J. Surg. Pathol. 2005;13:103–111. doi: 10.1177/106689690501300116. [DOI] [PubMed] [Google Scholar]
- 11.Lee S.-H. Fine-needle aspiration cytology of splenic hamartoma. Diagn. Cytopathol. 2003;28:82–85. doi: 10.1002/dc.10230. [DOI] [PubMed] [Google Scholar]
- 12.Kumar P.V. Splenic hamartoma. A diagnostic problem on fine needle aspiration cytology. Acta Cytol. 1995;39:391–395. [PubMed] [Google Scholar]
- 13.Minkes R.K., Lagzdins M., Langer J.C. Laparoscopic versus open splenectomy in children. J. Pediatr. Surg. 2000;35:699–701. doi: 10.1053/jpsu.2000.6010. [DOI] [PubMed] [Google Scholar]
- 14.Hayes T.C., Britton H.A., Mewborne E.B. Symptomatic splenic hamartoma: case report and literature review. Pediatrics. 1998;101:E10. doi: 10.1542/peds.101.5.e10. [DOI] [PubMed] [Google Scholar]
- 15.Garza-Serna U., Ovalle-Chao C., Martinez D. Laparoscopic partial splenectomy for congenital splenic cyst in a pediatric patient: case report and review of literature. Int. J. Surg. Case Rep. 2017;33:44–47. doi: 10.1016/j.ijscr.2017.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee S.H., Lee J.S., Yoon Y.C., Hong T.H. Role of laparoscopic partial splenectomy for tumorous lesions of the spleen. J. Gastrointest. Surg. 2015;19:1052–1058. doi: 10.1007/s11605-015-2812-5. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y., Chen X.-M., Sun D.-L., Yang C. Treatment of hemolymphangioma of the spleen by laparoscopic partial splenectomy: a case report. World J. Surg. Oncol. 2014;12:60. doi: 10.1186/1477-7819-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]