Abstract
Background
The Nottingham Hip Fracture Score (NHFS) is validated as a predictive mortality tool in patients with hip fracture. However, it has not been modified or validated widely other than in the UK NHS health systems.
Material/Methods
We assessed the predictive capability of the NHFS for 30-day mortality after surgery for hip fracture in the Greek population and then compared the original model to a modified one. We applied the NHFS to the Greek population and created a modified model of the NHFS by including the New Mobility Score (NMS) (Parker and Palmer, 1993) to the evaluated parameters and excluding the parameter of institution.
We ran a prospective study over a period of 3 years in our institution, collecting full data from 349 patients. All data were analyzed using SPSS, version 20.
Results
From all 349 patients, with a mean age of 80.82 years, only 85 (24.4%) were men. All patients were followed up for at least 30 days and the NHFS and modified NHFS prediction were compared with the mortality rate of patients. The area under the ROC curve for both models suggested acceptable accuracy (original NHFS 0.83, modified NHFS 0.84). Calibration was acceptable for both models (Hosmer-Lemeshow p=0.31 and 0.11, respectively).
Conclusions
Both the original and the modified NHFS were significant predictors of 30-day mortality. A higher-power study might be able to show superiority of the modified one for the Greek population in the future.
MeSH Keywords: Decision Support Techniques, Hip Fractures, Risk Factors, Validation Studies
Background
Fractures of the neck of the femur are strongly associated with increased mortality rates, with a variation in the reported risk of death among patients in different studies. In the UK for the year 2016, the 30-day mortality was 6.7% [1,2]. Complete return to pre-injury mobility status is uncommon, and the financial and social costs all over the world are considerable [3,4]. They affect 1.5 million people per year worldwide (expected to increase to 4.5 million by 2050 due to the aging population) [5–7], which makes them a major healthcare problem.
Up to 13.3% of these patients are expected to die within the first months after the operation [8], and up to one-third of them will die within 1 year postoperatively [7].
In the UK, about 68 000 hip fractures in the 2-year period of 2008 to 2009 [9]. Approximately 23% of the UK population is predicted to be aged over 65 years by 2033 [10], which means an increased incidence of hip fractures, despite all primary and secondary preventive measures [11,12].
In Greece, there was a 100% increase in the incidence of hip fractures from 1977 to 2007 among people older than 50 years [13]. In 2007, there were 14 055 patients aged ≥50 years who sustained a fracture of the femur neck. Of these, 9850 (70.1%) were women and 4205 were (29.9%) men. In 2007, more than 50% of them were older than 80 years, whereas this percentage was only 22.5% in 1977, [13] showing a 2.81 times higher risk for people older than 80 years to sustain a hip fracture in 2007 compared to 1977 [13]. This might be the result of the aging population, increased life expectancy, or other factors. However, there is no National Hip Fracture Database in Greece and the estimate can rely only on assumptions.
An accurate assessment of mortality risk after a hip fracture would help with the management of the patient, allow appropriate discussions with patients and family members, and facilitate the comparison of similar patients in audit and research, and the need for such an assessment has become more and more apparent in recent years.
Several scales or scores have been reported to predict the perioperative mortality risk for elderly patients, like the American Society of Anaesthesiologists (ASA) classification [14], the Barthel index [15], the Goldman index [16], the Visual Analogue Scale for Risk (RISK-VAS) scale [17], the Donati score [18], the Charlson Comorbidity Index (CCI) [19], and the Orthopaedic Physiologic and Operative Severity Score for the enumeration of Mortality and Morbidity (O-POSSUM) [20,21]. Furthermore, the Estimation of Physiologic Ability and Surgical Stress (E-PASS) [22,23], a risk model by Jiang et al. [24], a model by Holt et al. [25], the recently published Almelo Hip Fracture Score (AHFS) (which classifies patients with hip fracture into low, medium, or high risk for early postoperative mortality) [26], and the Nottingham Hip Fracture Score (NHFS) [27], the use of which has been recommended by the Association of Anaesthetists of Great Britain and Ireland [28]. Only the last 4 models were designed for the hip fracture population.
Unlike in the UK [29,30], the NHFS has never been validated in Greece. The purpose of the present study was to assess the predictive capability of the original NHFS for 30-day mortality after surgery for a hip fracture in the Greek population and then to compare that with a modified model, adjusted to the elderly Greek way of life. The reason we chose the NHFS is that it is easy to use, can be calculated on admission, and does not require surgical or anesthetic data.
The NHFS and modified NHFS
The score is calculated based on age, sex, comorbidities, place of residence (i.e., home or institutional care), the abbreviated mental test score (AMTS), the level of haemoglobin on admission, and history of previous cancer (Table 1). The NHFS, as it was first designed, has been demonstrated to predict 30-day and 1-year mortality, as well as time to discharge from hospital to home, in studies of patients from the originating unit [27,31,32].
Table 1.
NHFS vs. modified NHFS.
| Variable | Value | Score | |
|---|---|---|---|
|
| |||
| NHFS | Modified NHFS | ||
| Age | Age | 66–85 | 3 |
| >85 | 4 | ||
|
| |||
| Sex | Sex | Male | 1 |
| Female | 0 | ||
|
| |||
| Admission Hb | Admission Hb | <10 g/dl | 1 |
| ≥10 g/dl | 0 | ||
|
| |||
| MMTS | MMTS | <6/10 | 1 |
| ≥7/10 | 0 | ||
|
| |||
| Institutionalized | Yes | 1 | |
| No | 0 | ||
|
| |||
| New Mobility Score | <6 | 1 | |
| ≥6 | 0 | ||
|
| |||
| Number of co-morbidities | Number of co-morbidities | ≥2 | 1 |
| <2 | 0 | ||
|
| |||
| Malignancy | Malignancy | Yes | 1 |
| No | 0 | ||
We applied the NHFS to the Greek population, and at the same time, a modified model of the NHFS by including the New Mobility Score (NMS) (Parker and Palmer, 1993) [33] to the evaluated parameters and excluding the parameter of the institution (Table 1).
The idea behind the exclusion of institution as a parameter was that, unlike in the UK, fewer Greek older adults lives in institutions. Most of them live with their children or alone (but still under their children’s care). Therefore, we thought that the factor “living in an institute” is not reliable enough for the Greek population. The New Mobility Score is focused on the “mobility status” of these patients and has been previously used to assess morbidity as a reliable indicator of general health status.
Moreover, Galiatsatos et al. (2014) showed that the most appropriate risk factor for the Greek population, between the New Mobility Score and the Institution factor, as described in the NHFS, is the first one [34]. Patients with a New Mobility Score of 6 and above can walk out of the house and go shopping even with the use of a cane, while patients with a score below 6 need help from another person.
Material and Methods
Study cohort
All patients admitted to the University Hospital of Alexandroupolis from April 2009 to November 2012 with a fracture of the femur neck were included in this study. This is a supra-regional hospital, which is located in North-Eastern Greece and serves a population of about 250 000 people annually. As per current guidelines, intracapsular fractures were treated with hemiarthroplasty, total hip replacement, or cannulated screws, whereas extracapsular fractures were fixed either with an intramedullary nail or a Dynamic Hip Screw. We excluded patients younger than 66 years, patients with a periprosthetic fracture, and those undergoing conservative treatment. All the required details/data were collected during admission either in A & E or the ward. The NHFS and modified NHFS were subsequently calculated for each admitted patient. These were: age, sex, AMTS, admission hemoglobin, history of malignancy, comorbidities, pre-fracture residence, and mobility status (Mobility Parker score). A contralateral fracture in the same patient at a different date was recorded as a separate case.
Our study and the use of clinical data were approved by the local medical ethics committee. Informed consent was unnecessary due to the observational character of the research.
During the study period, 385 consecutive hip fracture patients underwent surgery. Complete data were collected for 359 patients, and the other 26 were excluded. Thirty-day mortality, defined as death within 30 days following hip fracture surgery, was verified using our hospital administration records, clinical files, health insurance databases, and via family members. For 10 patients, we could not identify their condition on the 30th postoperative day. In the remaining 349 patients, the mean age was 80.82 years, and only 85 (24.4%) were men. There were 230 extracapsular and 119 intracapsular fractures. The NHFS and modified NHFS were calculated for each hip fracture.
Statistical analysis
The observed 30-day mortality of the cohort was compared with those predicted by the NHFS and the modified NHFS. SPSS version 20 was used to perform univariate logistic regression analysis for assessing the significance, and the odds ratio for every risk factor in our research. We measured model calibration with the Hosmer-Lemeshow statistic, defining a lack of fit as a p-value ≤0.05, and multinomial logistic regression analysis for predicting the suitability between 2 important models consisted of just about the same risk factors. We used the R statistical package version 3.4.3 to analyze data.
Results
At 30 days following surgery, 33 of 349 patients had died, giving a mortality of 9.45% overall. The predicted mortality was also 9.45% both for NHFS and modified NHFS (33.01/349 and 33/349, respectively). The observed mortality was similar to the predicted one for both scores. Univariate logistic analysis was carried out for the risk factors, and we found all the individual parameters were significant (p<0.05). NMS, admission AMTS, sex, age, and malignancy were the most critical factors in hip fracture according the multivariate analysis in both models. In the first model, we used the factor institution, and the model’s chi-square index was 62.78, whereas in the second model, with the participation of NMS, the chi-square score was 64.05 (Tables 2, 3). Odds ratio (OR) is also included in these tables.
Table 2.
The NHFS.
| Model 1 | P-Value=0.0 | χ2=62.78 | |
|---|---|---|---|
| P-Value | OR (odds ratio) | LB-UB (lower bound-upper bound) | |
| Age | 0.03 | 2.69 | 1.13–6.39 |
| Malignancy | 0.0 | 9.53 | 3.57–25.45 |
| Institution | 0.04 | 3.92 | 1.07–14.31 |
| Diseases | 0.05 | 4.65 | 0.98–22.06 |
| MMTS | 0.03 | 2.62 | 1.12–6.13 |
| Hb | 0.17 | 2.13 | 0.72–6.28 |
| Sex | 0.04 | 2.47 | 1.03–5.88 |
Table 3.
The modified NHFS.
| Model 2 | P-Value=0.0 | χ2=64.05 | |
|---|---|---|---|
| P-Value | OR (odds ratio) | LB-UB (lower bound-upper bound) | |
| Age | 0.03 | 2.59 | 1.08–6.18 |
| Malignancy | 0.0 | 6.71 | 2.55–17.7 |
| Institution | 0.02 | 3.32 | 1.18–9.33 |
| Diseases | 0.07 | 4.27 | 0.89–20.41 |
| MMTS | 0.11 | 2.04 | 0.86–4.86 |
| Hb | 0.29 | 1.81 | 0.60–5.47 |
| Sex | 0.01 | 3.28 | 1.36–7.92 |
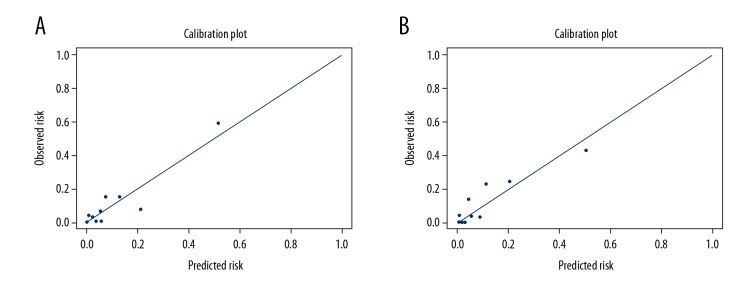
An overfitted model could be detected through an assessment of model calibration (Figure 1, Table 4) and discrimination (Figure 2). This may be done by dividing the patients into risk groups according to their predicted risk and comparing the proportion of patients who experienced the event in each group with the average predicted risk in that group, using a graph (calibration plot – Figure 1) or table (which leads to the Hosmer-Lemeshow test – Table 4). The Hosmer-Lemeshow statistic can be significant when predicted and observed outcomes are similar or close (Figure 1, Table 4). Both models predicted almost the same deaths at 30 postoperative days as that observed with calibration p-value=0.31 (χ2=11.74) for NHFS and p-value=0.11 (χ2=14.44) for modified NHFS, indicating good fit (Figure 1, Table 4).
Figure 1.
The observed vs. predicted 30-day mortalities for the Nottingham Hip Fracture (A) Score and the modified Nottingham Hip Fracture Score (B).
Table 4.
Observed and predicted 30 day mortality for 349 patients.
| NHFS | Modified NHFS | ||||
|---|---|---|---|---|---|
| Score | Observed | Predicted | Score | Observed | Predicted |
| 1,2 or 3 | 4/159 (2.5%) | 2.45/159 (1.54%) | 1,2 or 3 | 1/128 (0.78%) | 1.51/128 (1.17%) |
| 4 | 0/19 (0%) | 0.73/19 (3.9%) | 4 | 0/45 (0%) | 1.31/45 (2.91%) |
| 5 | 0/40 (0%) | 2.18/40 (5.5%) | 5 | 3/22 (13.6%) | 0.94/22 (4.27%) |
| 6 | 1/15 (6.7%) | 0.83/15 (5.53%) | 6 | 1/29 (3.44%) | 1.49/29 (5.13%) |
| 7 | 5/33 (15.2%) | 2.52/33 (7.63%) | 7 | 1/35 (2.85%) | 2.96/35 (8.45%) |
| 8,9 or 10 | 23/83 (27.71%) | 24.3/83 (29.2%) | 8,9 or 10 | 27/90 (30%) | 24.79/90 (27.54%) |
| Total | 33/349 | 33.01/349 | Total | 33/349 | 33/349 |
Figure 2.
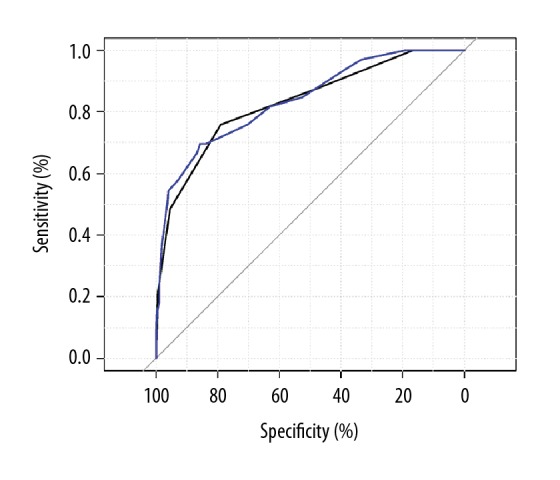
Receiver operator characteristic curves for the calibrated Nottingham Hip Fracture Score (blue line) and the calibrated modified Nottingham Hip Fracture Score (black line).
The graph (Figure 2) shows 2 ROC curves representing good tests plotted on the same graph. The accuracy of the test depends on how well it separates the group being tested into those with and without the disease in question. Accuracy is measured by the area under the ROC curve and shows the discrimination of the models. The curves were constructed by computing the sensitivity and specificity of increasing numbers of clinical findings. Both clinical models showed very good discrimination, as the area under the curve was 0.83 for NHFS and 0.84 for modified NHFS (Figure 2).
NHFS, as well as modified NHFS, demonstrate very good calibration and discrimination as hip fracture risk assessment tools. The NHFS model perfectly matches the UK population. Likewise, the modified NHFS seems to have a strong match to the Greek population by changing the institute with a New Mobility Score variable.
Discussion
Several scores have been developed before the NHFS to serve this purpose. Recent studies [35,36] showed that all the pre-NHFS developed score systems had an AUC below 0.80 and failed to provide quick and accurate risk counseling to the patient. ASA score evaluates the chronic physiological status of patients and is widely used to assess operative risk but has weak-to-moderate discriminant accuracy (AUC 0.60 to 0.71) [37].
The CCI score, which is a medical risk prediction tool adapted for surgical risk assessment, has a weak 90-day mortality prediction (AUC 0.59) [37]. The O-POSSUM score has been found to overestimate mortality in hip fractures [38], with AUC values ranging from 0.62 to 0.74 [37]. E-PASS has shown a better ability in predicting morbidity and mortality than O-POSSUM, but the fact that it requires intraoperative details, such as the amount of blood loss, operating time, and the extent of skin incision to calculate the final risk score for the patient, makes its use difficult, demanding, and complicated [22,23].
The recently introduced AHFS seems quite promising, but there are few studies supporting its value [26]. The NHFS, on the other hand, has been used for a few years now, mostly in the UK, and its prognostic value has been tested and validated for early hospital discharge [32], 30-day mortality [27], and 1-year mortality [31]. It has shown a moderate discriminant ability and a reasonable calibration [29,36,37,39]. It is simple to use, and data required for each patient are available on admission.
In our hospital, there is no trauma-dedicated theatre. That means that the patients with hip fractures are taken to the theatre as soon as possible, after the end of the elective lists and not later than 10 pm. Occasionally (and unfortunately not rarely) though, they can be operated on much later than 48 h after admission. The operations are done by Consultants or by supervised senior trainees. Consultant anaesthetists or supervised anaesthetic trainees give anaesthesia. Patients stay under the orthopedists’ care until they are discharged, and medical doctors (not orthogeriatricians, as there is no such specialty in Greece) are called to review patients if needed. Patients get mobilized by physiotherapists at 1 day after surgery, and they continue with physiotherapies at home if they can afford it or if their insurance can cover the service.
Although the above information reflects the working practices of a single hospital, we feel it is representative of the average hip trauma care in Greek hospitals. As seen in Table 5, this is an entirely different practice compared to the UK. The difference in practice between the 2 countries is significant and has become even wider due to the Greek financial crisis and austerity measures. However, the results of our study demonstrate that the NHFS and the modified NHFS quite accurately predict 30-day mortality following a fracture of the hip in an elderly Greek population and shows that the 7 predictors of mortality that the NHFS uses are truly independent. To the best of our knowledge, this is the first validation of the NHFS in Greece and the first attempt to modify the NHFS and adapt it for the Greek population. The result for the NHFS supports those from the originating center [27,29,31,32].
Table 5.
Differences in hip fractures treatment between UK and Greece.
| UK | Greece |
|---|---|
| Patient admitted under care of both Orthopaedic Surgeons and Orthogeriatricians | Patients admitted under Orthopaedic Surgeons Orthogeriatric is not a recognised specialty in Greece |
| Multidisciplinary assessment protocol | – |
| Hip fracture surgery within 36 h of admission | As soon as free theatre is found (if patient is good to go) |
| Assessed by orthogeriatricians within 72 h of admission | Review by other specialties, only if required |
| Falls and rehabilitation assessments | – |
| Assessment for osteoporosis and fracture prevention | – |
| Kept in a rehabilitation ward or transferred to a nursing/care home if needed until it is safe to go home. | Discharged home or under the children’s care. No long term rehabilitation. |
| NICE Guidelines | No guidelines |
The results for the modified NHFS suggest that it can be a useful tool for managing these patients in Greece. Currently, no risk assessment tool is regularly used in any Greek hospital for elderly patients with a hip fracture. Despite the high incidence of these fractures, no guidelines have been suggested or published by the Greek Health Ministry or the Greek Orthopaedic Association to allow or promote optimization of care for these patients. We believe that the modified NHFS score should be used regularly in Greek hospitals to allow early identification of high-risk patients and their need for higher levels of peri-operative care.
There are several limitations to this study: (a) The lack of accuracy and the completeness of the data recorded by the orthopedic staff in some cases or due the difficulty to reach some of the patients or their family members or their insurance database postoperatively; (b) The number of our patients, although small when compared to other studies [39], is satisfactory for a supra-regional hospital, but obviously, the adaptation of the study protocol by other hospitals all over Greece would deliver stronger evidence; and (c) The decision about replacing the parameter institution with the Parker NMS (and not another factor) could be questioned, but the results proved us correct. In the future, studies using another factor – or other factors – could increase the accuracy of the NHFS for use in Greece.
Conclusions
Although our study did not show any significant superiority of the modified NHFS to the original one, it did show a slightly higher accuracy or adaptability for the Greek population and, most importantly, it did not show any inferiority. This suggests that a future national study in a much larger population sample would show that use of the Parker mobility score (instead of institution) could achieve significantly higher adaptability to the Greek population, particularly considering the idea that this modification is based on, but this remains to be studied.
Moreover, our study could trigger further research in the UK with a modified NHFS, the same as ours or with other variables. There are predictive variables that are not currently used in the NHFS or any other mortality predictive model, such as red blood cell distribution on admission [40], albumin levels [41], and some inflammatory markers [42,43].
As the medical community has accepted the value and necessity of risk prediction scores, doctors need to work hard to improve the accuracy of our tools.
Footnotes
Source of support: Departmental sources
References
- 1.Pugely AJ, Martin CT, Gao Y, et al. A risk calculator for short-term morbidity and mortality after hip fracture surgery. J Orthop Trauma. 2014;28:63–69. doi: 10.1097/BOT.0b013e3182a22744. [DOI] [PubMed] [Google Scholar]
- 2.The National Hip Fracture Database: National Hip Fracture Database National report. 2017. No authors listed. https://www.nhfd.co.uk/files/2017ReportFiles/NHFD-AnnualReport2017.pdf.
- 3.White SM, Griffiths R. Projected incidence of proximal femoral fracture in England: a report from the NHS Hip Fracture Anaesthesia Network (HIPFAN) Injury. 2011;42:1230–33. doi: 10.1016/j.injury.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Lawrence TM, White CT, Wenn R, Moran CG. The current hospital costs of treating hip fractures. Injury. 2005;36:88–92. doi: 10.1016/j.injury.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: Injuries, healthcare costs, and long-term reduced quality of life. J Trauma. 2011;71:748–53. doi: 10.1097/TA.0b013e3181f6f5e5. [DOI] [PubMed] [Google Scholar]
- 6.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: A world-wide projection. Osteoporos Int. 1992;2:285–89. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 7.Abrahamsen B, van Staa T, Ariely R, et al. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633–50. doi: 10.1007/s00198-009-0920-3. [DOI] [PubMed] [Google Scholar]
- 8.Hu F, Jiang C, Shen J, et al. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43:676–85. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 9.The Improvement Centre for Health and Social Care. Hospital Episode Statistics. [16 February 2011 date last accessed]. http://www.hesonline.nhs.uk.; UK Statistics Authority, Office for National Statistics. [19 April 2010 date last accessed]. http://www.ons.gov.uk.
- 10.National Institute for Health and Clinical Excellence. Alendronate, Etidronate, Risedronate, Raloxifene and Strontium Ranelate for the Primary Prevention of Osteoporotic Fragility.
- 11.Fractures in Postmenopausal Women (Amended) London: National Institute for Health and Clinical Excellence; 2011. (NICE Technology Appraisal Guidance 160). [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. Alendronate, Etidronate, Risedronate, Raloxifene, Strontium Ranelate and Teriparatide for the Secondary Prevention of Osteoporotic Fragility Fractures in Postmenopausal Women. London: National Institute for Health and Clinical Excellence; 2011. (NICE Technology Appraisal Guidance 161). [Google Scholar]
- 13.Lyritis GP, Rizou S, Galanos A, Makras P. Incidence of hip fractures in Greece during a 30-year period: 1977–2007. Osteoporos Int. 2013;24(5):1579–85. doi: 10.1007/s00198-012-2154-z. [DOI] [PubMed] [Google Scholar]
- 14.American Society of Anesthesiologists. American Society of Anesthesiologists new classification of physical status. Anesthesiology. 1963;24:111. [Google Scholar]
- 15.Mahoney FI, Barthel DW. Functional evaluation: The Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 16.Goldman L, Caldera DL, Nussbaum SR. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–50. doi: 10.1056/NEJM197710202971601. [DOI] [PubMed] [Google Scholar]
- 17.Arvidsson S, Ouchterlongy J, Sjostedt L, Svărdsudd K. Predicting postoperative adverse events. Clinical efficiency of four general classification systems. The project perio-perative risk. Acta Anaesthesiol Scand. 1996;40:783–91. doi: 10.1111/j.1399-6576.1996.tb04533.x. [DOI] [PubMed] [Google Scholar]
- 18.Donati A, Ruzzi M, Adrario E. A new and feasible model for predicting operative risk. Br J Anaesth. 2004;93:393–99. doi: 10.1093/bja/aeh210. [DOI] [PubMed] [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.Mohamed K, Copeland GP, Boot DA, et al. An assessment of the POSSUM system in orthopaedic surgery. J Bone Joint Surg Br. 2002;84(5):735–39. doi: 10.1302/0301-620x.84b5.12626. [DOI] [PubMed] [Google Scholar]
- 21.Copeland GP, Jones D, Walters M. POSSUM: A scoring system for surgical audit. Br J Surg. 1991;78(3):355–60. doi: 10.1002/bjs.1800780327. [DOI] [PubMed] [Google Scholar]
- 22.Hirose J, Mizuta H, Ide J, et al. E-PASS for predicting postoperative risk with hip fracture: A multicenter study. Clin Orthop Relat Res. 2008;466(11):2833–41. doi: 10.1007/s11999-008-0377-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirose J, Mizuta H, Ide J, Nomura K. Evaluation of estimation of physiologic ability and surgical stress (E-PASS) to predict the postoperative risk for hip fracture in elder patients. Arch Orthop Trauma Surg. 2008;128(12):1447–52. doi: 10.1007/s00402-007-0551-0. [DOI] [PubMed] [Google Scholar]
- 24.Jiang HX, Majumdar SR, Dick DA, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20(3):494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 25.Holt G, Smith R, Duncan K, et al. Early mortality after surgical fixation of hip fractures in the elderly: An analysis of data from the scottish hip fracture audit. J Bone Joint Surg Br. 2008;90(10):1357–63. doi: 10.1302/0301-620X.90B10.21328. [DOI] [PubMed] [Google Scholar]
- 26.Nijmeijer WS, Folbert EC, Vermeer M, et al. Prediction of early mortality following hip fracture surgery in frail elderly: The Almelo Hip Fracture Score (AHFS) Injury. 2016;7(10):2138–43. doi: 10.1016/j.injury.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 27.Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–17. doi: 10.1093/bja/aen236. [DOI] [PubMed] [Google Scholar]
- 28.Association of Anaesthetists of Great Britain and Ireland. Griffiths R, Alper J, Beckingsale A, et al. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67:85–98. doi: 10.1111/j.1365-2044.2011.06957.x. [DOI] [PubMed] [Google Scholar]
- 29.Moppett IK, Parker M, Griffiths R, et al. Nottingham Hip Fracture Score: longitudinal and multi-assessment. Br J Anaesth. 2012;109:546–50. doi: 10.1093/bja/aes187. [DOI] [PubMed] [Google Scholar]
- 30.Rushton PR, Reed MR, Pratt RK. Independent validation of the Nottingham Hip Fracture Score and identification of regional variation in patient risk within England. Bone Joint J. 2015;97-B(1):100–3. doi: 10.1302/0301-620X.97B1.34670. [DOI] [PubMed] [Google Scholar]
- 31.Wiles MD, Moran CG, Sahota O, Moppett IK. Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br J Anaesth. 2011;106:501–4. doi: 10.1093/bja/aeq405. [DOI] [PubMed] [Google Scholar]
- 32.Moppett IK, Wiles MD, Moran CG, Sahota O. The Nottingham Hip Fracture Score as a predictor of early discharge following fractured neck of femur. Age Ageing. 2012;41:322–26. doi: 10.1093/ageing/afr142. [DOI] [PubMed] [Google Scholar]
- 33.Parker MJ, Palmer C. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75(5):797–98. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 34.Galiatsatos D, Anastassopoulos GC, Drosos G, et al. Volume 436 of the series IFIP Advances in Information and Communication Technology. 2014. Prediction of 30-day mortality after a hip fracture surgery using neural and bayesian networks. Chapter: Artificial intelligence applications and innovations; pp. 566–75. [Google Scholar]
- 35.Kau CY, Kwek EB. Can preoperative scoring systems be applied to Asian hip fracture populations? Validation of the Nottingham Hip Fracture Score (NHFS) and identification of preoperative risk factors in hip fractures. Ann Acad Med Singapore. 2014;43(9):448–53. [PubMed] [Google Scholar]
- 36.Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30-day mortality following hip fracture surgery: Evaluation of six risk prediction models. Injury. 2015;46(2):371–77. doi: 10.1016/j.injury.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 37.Marufu TC, Mannings A, Moppett IK. Risk scoring models for predicting peri-operative morbidity and mortality in people with fragility hip fractures: Qualitative systematic review. Injury. 2015;46(12):2325–34. doi: 10.1016/j.injury.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 38.Ramanathan TS, Moppett IK, Wenn R, Moran CG. POSSUM scoring for patients with fractured neck of femur. Br J Anaesth. 2005;94(4):430–33. doi: 10.1093/bja/aei064. [DOI] [PubMed] [Google Scholar]
- 39.Marufu TC, White SM, Griffiths R, et al. Prediction of 30-day mortality after hip fracture surgery by the Nottingham Hip Fracture Score and the Surgical Outcome Risk Tool. Anaesthesia. 2016;71(5):515–21. doi: 10.1111/anae.13418. [DOI] [PubMed] [Google Scholar]
- 40.Garbharran U, Chinthapalli S, Hopper I, et al. Red cell distribution width is an independent predictor of mortality in hip fracture. Age Ageing. 2012;6:1–4. doi: 10.1093/ageing/afs176. [DOI] [PubMed] [Google Scholar]
- 41.Steinberg EL, Amar E, Sagy Y, et al. The impact of serum albumin and serum protein levels on POSSUM score of patients with proximal femur fractures. Injury. 2014;45(12):1928–31. doi: 10.1016/j.injury.2014.07.030. [DOI] [PubMed] [Google Scholar]
- 42.Kieffer WK, Rennie CS, Gandhe AJ. Preoperative albumin as a predictor of one-year mortality in patients with fractured neck of femur. Ann Roy Coll Surg. 2013;95:26–28. doi: 10.1308/003588413X13511609954815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laulund AS, Lauritzen JB, Duus BR, et al. Routine blood tests as predictors of mortality in hip fracture patients. Injury. 2012;43:1014–20. doi: 10.1016/j.injury.2011.12.008. [DOI] [PubMed] [Google Scholar]