Abstract
Background
Contrast-induced nephropathy (CIN) is a complication after the intravascular administration of a contrast medium injection. Previous studies have investigated statins as therapy for CIN due to its positive results in the prevention of contrast-induced acute kidney injury (CI-AKI). Nevertheless, the beneficial effects of rosuvastatin pretreatment in preventing CIN in patients with acute coronary syndromes still remain controversial. In this study, we performed a meta-analysis of randomized controlled trials (RCTs) to evaluate the beneficial impact of rosuvastatin in the prevention of CI-AKI in acute coronary syndrome patients.
Methods
PubMed, Embase, and Cochrane library were searched, for RCTs, updated on January 2018. The method was to evaluate rosuvastatin prior to angiography for the prevention of CI-AKI in patients undergoing coronary angiography, of which the main outcome was the incidence of CIN.
Results
A total of five RCTs were included in this analysis. Patients treated with rosuvastatin prior to invasive angiography had a significantly lower incidence of CI-AKI than controls (odds ratio [OR]: 0.53, 95% CI: 0.40–0.71, P<0.0001). Moreover, the subgroup analysis also showed that the benefit of rosuvastatin for patients with chronic kidney disease (OR: 0.49, 95% CI: 0.26–0.92, P=0.03) and diabetes mellitus (OR: 0.56, 95% CI: 0.38–0.83, P=0.004) which was consistent in compared with the respective control groups.
Conclusion
The findings of this meta-analysis suggest that the preoperative rosuvastatin treatment significantly reduces the risk of renal insufficiency of CIN in at-risk patients with chronic kidney disease or diabetes mellitus. Additional studies are needed to identify at-risk patients, provide optimum dose peri-procedural treatment, and reduce the incidence of CIN.
Keywords: contrast-induced nephropathy, coronary angiography, rosuvastatin, meta-analysis
Introduction
Contrast-induced nephropathy (CIN) is characterized by acute impairment of renal function after contrast exposure.1 Patients with acute coronary syndrome (ACS) undergoing primary percutaneous intervention (p-PCI) are at a higher risk of developing contrast-induced acute kidney injury (CI-AKI).2 Moreover, the incidence of contrast nephropathy was associated with patient characteristics that are risk factors for this disease.3,4 As CI-AKI is associated with increased short- and long-term morbidity and mortality, nonfatal cardiovascular events, and a longer hospital stay,5 the adoption of optimal therapeutic strategies is needed to prevent CIN, offering an opportunity to reduce patient morbidity and mortality.
In clinical practice, a number of studies have shown that the pleiotropic properties of statins exert a beneficial impact in the prevention of contrast nephropathy.6 Apart from their cholesterol-lowering effects, statins have anti-inflammatory, antithrombotic, and antioxidative properties and may exercise nephron-protective action, thereby improving the endothelial function and reducing vascular inflammation and oxidative stress.5 These favorable activities have a direct preventive effect against the development of CI-AKI.7,8 However, the results concerning the efficacy of statin therapy in the prevention of CI-AKI are inconsistent.6,9,10
The hydrophilic form of the statin rosuvastatin may have better potential for prevention of CIN than other statin forms, probably owing to its longer plasma half-life and stronger anti-inflammatory effect. Previous randomized controlled trials (RCTs) focused mainly on the application of the lipophilic form of rosuvastatin for the prevention of CIN, but conflicting results have been reported.
Therefore, in this study, we performed a meta-analysis of RCTs to evaluate the efficacy of rosuvastatin pretreatment for the prevention of CIN as compared with placebo treatment.
Methods
Search strategy
To find all related articles, two investigators independently searched electronic databases (PubMed, Embase, and Cochrane Library) up to January 2018. The keywords “rosuvastatin” and “contrast-induced acute kidney injury,” as well as relevant Medical Subject Heading terms were used in the search. We also checked the reference lists of all articles for additional eligible studies.
Eligibility criteria
To be included in the meta-analysis, the studies had to meet the following criteria: 1) RCTs comparing rosuvastatin pretreatment with placebo treatment in patients undergoing PCI; 2) they provided information about CI-AKI; 3) the outcome of interest was the incidence of CIN; 4) each paper had to be written in English.
Quality assessment
Two investigators independently rated the quality of the eligible RCTs. We choose the risk of bias items for RCTs recommended by The Cochrane Handbook for Systematic Reviews of Interventions.32
Data extraction
Two authors independently extracted the relevant data from each article. Any disagreement was resolved by consensus. The data extracted from the eligible studies included the following information: name of the first author, year of publication, characteristics of the trials, number of study patients, mean age, mean baseline SCr, and definition of CIN in each trial.
Statistical analysis
All outcome comparisons were conducted and estimates calculated using the Review Manager version 5.3 software (Revman; The Cochrane Collaboration, Oxford, UK). Odds ratios (ORs) and their 95% CIs were calculated to assess the CIN events and make comparisons between the rosuvastatin and the control groups. The ORs and their 95% CIs were also mentioned in the summary statistics in the pooled subgroup analysis for patients with chronic kidney disease (CKD) or diabetes mellitus (DM).
A sensitivity analysis was also performed to examine the overall impact of heterogeneity on meta-analysis results. The I2 test was employed to evaluate the heterogeneity of the results.11 An I2-value ≥50% was considered to indicate moderate and high heterogeneity, whereas an I2-value <50% showed low heterogeneity.12 A P-value <0.05 was considered statistically significant.
Results
Overview of literature search and study characteristics
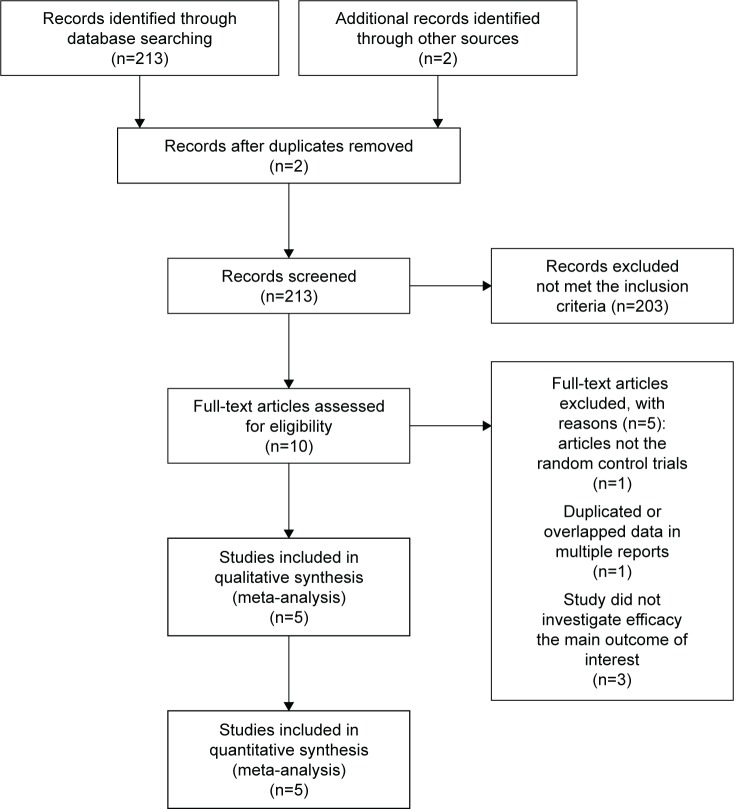
A total of 213 studies were identified and reviewed according to the criteria described in the methods, of which 10 publications were evaluated in more detail, but some did not provide information on the endpoint outcomes.
Thus, a total of five RCTs were finally included in the present analysis.13–17 The search process is illustrated in Figure 1. All included studies in this meta-analysis were considered to be at least of moderate quality. Detailed information on the medication protocols of the eligible studies is presented in Table 1.
Figure 1.
PRISMA flow chart of the selection process used to identify studies eligible for pooling.
Abbreviation: RCT, randomized controlled trial.
Table 1.
Detailed medication protocols of the eligible studies
| Study | Patients number
|
Inclusion criteria | Protocol | Definition of CIN | Mean age, years
|
Mean baseline SCr, µmol/L or mg/dL
|
|---|---|---|---|---|---|---|
| E/C | E/C | E/C | ||||
| Fahmy et al,13 | 100/100 | Patients undergoing CAG | Rosuvastatin 20 mg/d from 3 days before to 7 days after procedure vs placebo | ≥25% SCr or ≥44.2 µmol/L SCr within 48 hours | 54.8±11.0/52.1±10.7 | 0.81±0.2/0.81±0.3 mg/dL |
| Leoncini et al,14 2014 | 252/252 | NSTE-ACS patients undergoing CAG with or without PCI | Rosuvastatin 40 mg followed by 20 mg/d vs placebo | ≥25% SCr or ≥44.2 µmol/L SCr within 72 hours | 66.2±12.4/66.1±13.5 | 0.95±0.27/0.96±0.28 mg/dL |
| Abaci et al,15 2015 | 110/110 | Patients undergoing CAG | Rosuvastatin 40 mg within 24 hours before and 20 mg/d for 2 days vs placebo | ≥25% SCr or≥ 44.2 µmol/L SCr within 48–72 hours | 67.5±8.9/67.7±8.9 | 1.3±0.4/1.4±0.5 mg/dL |
| Msd et al,16 2012 | 67/68 | ACS patients undergoing PCI | Rosuvastatin 40 mg 2–6 hours before procedure vs placebo | ≥25% SCr or ≥44.2 µmol/L SCr within 24 hours | 59.4±8.6/62.2±9.8 | 0.89±0.24/0.98±0.21 mg/dL |
| Han et al,17 2014 | 1,498/1,500 | Patients with DM and CKD undergoing coronary/peripheral arterial diagnostic angiography, left ventriculography, or PCI were eligible | rosuvastatin,10 mg every evening, from 2 days before to 3 days after contrast medium administration (total dose of 50 mg of rosuvastatin over 5 days) or to a control group | ≥0.5 mg/dL (44.2 mmol/L) or ≥25% above baseline at 72 hours after exposure to the contrast medium | 61.45±8.64/61.44±8.64 | 95.08±22.92/94.95±20.84 mg/dL |
Abbreviations: CAG, coronary angiography; CIN, contrast-induced nephropathy; CKD, chronic kidney disease; DM, diabetes mellitus; PCI, percutaneous coronary intervention.
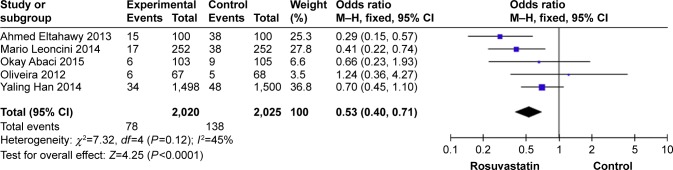
Effect of rosuvastatin on the incidence of CI-AKI
The data pooled from all five articles included in our research showed that the risk of CI-AKI (OR: 0.53, 95% CI: 0.40–0.71, P<0.0001) in the atorvastatin treatment group was lower than that in the control group (Figure 2).
Figure 2.
Effect of rosuvastatin on the incidence of CI-AKI.
Abbreviations: CI-AKI, contrast-induced acute kidney injury; OR, odds ratio.
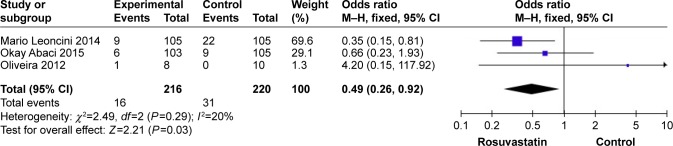
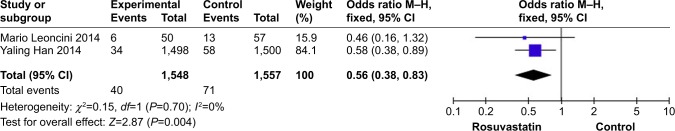
Subgroup analysis of the effect of rosuvastatin on the incidence of CI-AKI
Rosuvastatin reduced also the risk of CI-AKI in patients with CKD (OR: 0.45, 95% CI: 0.21–0.95, P=0.04) (Figure 3) and DM (OR: 0.56, 95% CI: 0.38–0.83, P=0.004) (Figure 4), as compared with that in the placebo group.
Figure 3.
Influence of rosuvastatin treatment on the incidence of CI-AKI in patients with CKD.
Abbreviations: CI-AKI, contrast-induced acute kidney injury; CKD, chronic kidney disease; OR, odds ratio.
Figure 4.
Impact of rosuvastatin administration on the incidence of CI-AKI in patients with DM.
Abbreviations: CI-AKI, contrast-induced acute kidney injury; DM, diabetes mellitus; OR, odds ratio.
Discussion
The pathophysiological mechanism of CIN is still not entirely clear. Multiple mechanisms may be involved; in particular, adenosine, angiotensin, vasopressin, and endothelin secretion after contrast exposure is a logical cause for the reduction in the synthesis of nitric oxide and the induction of oxidative stress, causing hypoxia in the renal medulla. More recently, other renal damage mechanisms have been associated with the development of cellular lesions, necrosis, interstitial inflammation, and tubular injury.5,7 It is noteworthy that the elevated preprocedural concentration of the high-sensitivity CRP was found to increase the risk of CIN in patients who had underwent PCI.18
In addition to their lipid-lowering activities, statins are also known to downregulate the angiotensin receptor, limit the production of endothelial nitric oxide synthase, and have antithrombotic and anti-inflammatory properties, which altogether constitutes their pleiotropic effects.9 Due to these multidirectional activities, statins are considered to exert also a renoprotective effect and that the pretreatment with statin can affect the progression of the CI-AKI pathogenesis.
Basing on the beneficial clinical results observed in various subgroups of patients, we analyzed the additional functions of rosuvastatin which showed acute pleiotropic effects.19 In one of the studies included in our research, healthy patients without hyperlipidemia (low-density lipoprotein cholesterol levels: <130 mg/dL) but with elevated high-sensitivity CRP levels (<2.0 mg/L)20 and patients with estimated eGFR <60 mL/min/1.73 m2 were found to be at the highest risk of CI-AKI.21 Furthermore, the short-term treatment with rosuvastatin was indicated to play a protective role by improving eGFR independently of the lipid fraction changes, suggesting that the pleiotropic effect of rosuvastatin included also renoprotective functions.22 The preventive impact of rosuvastatin on the magnitude of CIN reduction could be due to of its inhibitory influence on the synthesis of inflammatory mediators, a phenomenon observed in the JUPITER trial.20
Previous studies have shown the beneficial, preventive effects of statins against CI-AKI. For example, Leoncini et al14 established that rosuvastatin significantly reduced CI-AKI. However, Abaci et al15 found that the high-dose rosuvastatin treatment had no beneficial effects in decreasing the occurrence of CI-AKI in patients with suspected coronary artery disease.
Preexisting kidney disease is known to be the greatest risk for CI-AKI development, especially in patients with acute coronary syndrome because of their diminished renal reserve.23 Nevertheless, whether the short-term high-dose statin pretreatment in patients with stable coronary artery disease lowers the risk of CI-AKI and reduces the renal function still remains debatable, and thus additional research is needed to further elucidate this issue.24–26 Moreover, patients with DM are at the highest risk of CI-AKI due to the pathophysiologic changes caused by contrast materials, including increased production of reactive oxygen species, vascular endothelial injury, and dysregulated microcirculation. Thus, patients with CKD and DM are at increased risk of CI-AKI.27
In the current study, we found that the beneficial effects of rosuvastatin were consistent in patients with renal dysfunction and diabetes with a significant reduction of CI-AKI rate. The pathophysiology contributing to kidney injury in CIN is not completely understood. Given their multiple pleiotropic effects, statins are likely to exert a renoprotective effect and limit the injury of renal function over time.5 Preclinical studies have demonstrated that statins inhibit receptor-mediated endocytosis, which is responsible for the protein uptake in proximal tubular cells, in a dose-dependent manner.28,29
The latest meta-analysis published suggested that the moderate- or high-dose rosuvastatin treatment may have preventive effects against CIN in patients undergoing coronary angiography or PCI. As the data available on this dose-dependent influence are limited, in this meta-analysis, we did not assess the impact of the potentially hazardous high-dose rosuvastatin pretreatment.30
The main relative strength of our analysis as compared with previous meta-analyses on the same topic is the inclusion and analysis of the results of randomized controlled trials published in English. Nonetheless, several inherent flaws of the study should not be ignored as that might have led to potential bias. First, data were pooled from a number of RCTs with different inclusion criteria with insignificant heterogeneity among the included studies. Second, patients might have had differential responses to treatment with different doses of rosuvastatin. Third, the entire meta-analysis is based upon 5 RCTs, of which only three related to CKD and two related to DM, which limits the ability to statistically analyze the effect of rosuvastatin on the incidence of interested outcomes, so future research should be conducted to identify these subgroups.
Contrast administration is well-established in the literature as a risk factor for CI-AKI. The incidence of CI-AKI varies widely depending on the patient cohorts evaluated, definition criteria used, and preventive strategies adopted.31 In conclusion, the current evidence indicates that rosuvastatin prevents the occurrence of CIN in patients after an episode of CI-AKI, especially in high-risk patients with DM or CKD.
The best approaches established so far to prevent CIN are to identify at-risk patients, provide adequate therapeutic doses, and minimize the amount of contrast administered. However, the actual mechanism by which statins may lower the risk of contrast nephropathy remains uncertain. Therefore, further research is needed to better understand their underlying mechanisms of action.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Solomon R, Dauerman HL. Contrast-induced acute kidney injury. Circulation. 2010;122(23):2451–2455. doi: 10.1161/CIRCULATIONAHA.110.953851. [DOI] [PubMed] [Google Scholar]
- 2.Senoo T, Motohiro M, Kamihata H, et al. Contrast-induced nephropathy in patients undergoing emergency percutaneous coronary intervention for acute coronary syndrome. Am J Cardiol. 2010;105(5):624–628. doi: 10.1016/j.amjcard.2009.10.044. [DOI] [PubMed] [Google Scholar]
- 3.Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105(19):2259–2264. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 4.Sudarsky D, Nikolsky E. Contrast-induced nephropathy in interventional cardiology. Int J Nephrol Renovasc Dis. 2011;4:85–99. doi: 10.2147/IJNRD.S21393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mccullough PA. Radiocontrast-induced acute kidney injury. Nephron Physiol. 2008;109(4):p61–p72. doi: 10.1159/000142938. [DOI] [PubMed] [Google Scholar]
- 6.Pappy R, Stavrakis S, Hennebry TA, Abu-Fadel MS. Effect of statin therapy on contrast-induced nephropathy after coronary angiography: a meta-analysis. Int J Cardiol. 2011;151(3):348–353. doi: 10.1016/j.ijcard.2011.05.045. [DOI] [PubMed] [Google Scholar]
- 7.Tumlin J, Stacul F, Adam A, et al. Pathophysiology of Contrast-Induced Nephropathy. Am J Cardiol. 2006;98(6):14–20. doi: 10.1016/j.amjcard.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 8.Giusti-Paiva A, Martinez MR, Felix JV, et al. Simvastatin decreases nitric oxide overproduction and reverts the impaired vascular responsiveness induced by endotoxic shock in rats. Shock. 2004;21(3):271–275. doi: 10.1097/10.shk.0000115756.74059.ce. [DOI] [PubMed] [Google Scholar]
- 9.Patti G, Ricottini E, Nusca A, et al. Short-term, high-dose Atorvastatin pretreatment to prevent contrast-induced nephropathy in patients with acute coronary syndromes undergoing percutaneous coronary intervention (from the ARMYDA-CIN [atorvastatin for reduction of myocardial damage during angioplasty – contrast-induced nephropathy]) trial. Am J Cardiol. 2011;108(1):1–7. doi: 10.1016/j.amjcard.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Zhang L, Zhang L, Lu Y, et al. Efficacy of statin pretreatment for the prevention of contrast-induced nephropathy: a meta-analysis of randomised controlled trials. Int J Clin Pract. 2011;65(5):624–630. doi: 10.1111/j.1742-1241.2010.02588.x. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fahmy M, Eltahawy A, Enany BE. TCTAP A-037 Role of Rosuvastatin Pretreatment in Prevention of Contrast Induced Nephropathy in Patients Undergoing Coronary Angiography. J Am Coll Cardiol. 2014;63(12):S11. [Google Scholar]
- 14.Leoncini M, Toso A, Maioli M, et al. Early high-dose rosuvastatin and cardioprotection in the protective effect of rosuvastatin and antiplatelet therapy on contrast-induced acute kidney injury and myocardial damage in patients with acute coronary syndrome (PRATO-ACS) study. Am Heart J. 2014;168(5):792–797. doi: 10.1016/j.ahj.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 15.Abaci O, Arat Ozkan A, Kocas C, et al. Impact of Rosuvastatin on contrast-induced acute kidney injury in patients at high risk for nephropathy undergoing elective angiography. Am J Cardiol. 2015;115(7):867–871. doi: 10.1016/j.amjcard.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Msd O, Bomfim Araujo Martins K, Ribamar Costa J, et al. Impact on Renal Function of Rosuvastatin Preload Prior to Elective Percutaneous Coronary Intervention in Chronic Statin Users. Revista Brasileira de Cardiologia Invasiva. 2012;20(3):303–308. [Google Scholar]
- 17.Han Y, Zhu G, Han L, et al. Short-term rosuvastatin therapy for prevention of contrast-induced acute kidney injury in patients with diabetes and chronic kidney disease. J Am Coll Cardiol. 2014;63(1):62–70. doi: 10.1016/j.jacc.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 18.Briasoulis A, Pala M, Telila T, et al. Statins and contrast-induced nephropathy: a systematic review and meta-analysis. Curr Pharm Des. 2017 doi: 10.2174/1381612823666170913170527. [DOI] [PubMed] [Google Scholar]
- 19.Liuni A, Luca MC, Gori T, Parker JD. Rosuvastatin prevents conduit artery endothelial dysfunction induced by ischemia and reperfusion by a cyclooxygenase-2-dependent mechanism. J Am Coll Cardiol. 2010;55(10):1002–1006. doi: 10.1016/j.jacc.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 20.Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. The New England Journal of Medicine. 2008;359(21):2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 21.Ridker PM, Macfadyen J, Cressman M, Glynn RJ. Efficacy of rosuvastatin among men and women with moderate chronic kidney disease and elevated high-sensitivity C-reactive protein: a secondary analysis from the JUPITER (Justification for the Use of Statins in Prevention-an Intervention Trial Evaluating Rosuvastatin) trial. J Am Coll Cardiol. 2010;55(12):1266–1273. doi: 10.1016/j.jacc.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 22.Vidt DG, Harris S, Mctaggart F, Ditmarsch M, Sager PT, Sorof JM. Effect of short-term rosuvastatin treatment on estimated glomerular filtration rate. Am J Cardiol. 2006;97(11):1602–1606. doi: 10.1016/j.amjcard.2005.12.052. [DOI] [PubMed] [Google Scholar]
- 23.Marenzi G, Lauri G, Assanelli E, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004;44(9):1780–1785. doi: 10.1016/j.jacc.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 24.Jo SH, Koo BK, Park JS, et al. Prevention of radiocontrast medium-induced nephropathy using short-term high-dose simvastatin in patients with renal insufficiency undergoing coronary angiography (PROMISS) trial – a randomized controlled study. Am Heart J. 2008;155499(3):e491–e498. doi: 10.1016/j.ahj.2007.11.042. [DOI] [PubMed] [Google Scholar]
- 25.Toso A, Maioli M, Leoncini M, et al. Usefulness of atorvastatin (80 mg) in prevention of contrast-induced nephropathy in patients with chronic renal disease. Am J Cardiol. 2010;105(3):288–292. doi: 10.1016/j.amjcard.2009.09.026. [DOI] [PubMed] [Google Scholar]
- 26.Quintavalle C, Fiore D, de Micco F, et al. Impact of a high loading dose of atorvastatin on contrast-induced acute kidney injury. Circulation. 2012;126(25):3008–3016. doi: 10.1161/CIRCULATIONAHA.112.103317. [DOI] [PubMed] [Google Scholar]
- 27.Mccullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103(5):368–375. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 28.Agarwal R. Statin induced proteinuria: renal injury or renoprotection? J Am Soc Nephrol. 2004;15(9):2502–2503. doi: 10.1097/01.ASN.0000143720.71748.79. [DOI] [PubMed] [Google Scholar]
- 29.Harper CR, Jacobson TA. Managing dyslipidemia in chronic kidney disease. J Am Coll Cardiol. 2008;51(25):2375–2384. doi: 10.1016/j.jacc.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 30.Liang M, Yang S, Fu N. Efficacy of short-term moderate or high-dose rosuvastatin in preventing contrast-induced nephropathy: A meta-analysis of 15 randomized controlled trials. Medicine. 2017;96(27):e7384. doi: 10.1097/MD.0000000000007384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44(7):1393–1399. doi: 10.1016/j.jacc.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 32.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [Accessed October 19, 2018]. wepage on Internet. [updated March 2011]. Available from: www.handbook.cochrane.org.